Abstract
Partial posterior wall fractures are usually fixed with open reduction–internal fixation through an open posterolateral approach, but when the fragment may be fixed without a plate (with screws only), reduction and fixation may also be achieved via hip arthroscopy with the patient in the prone position. This article presents all the surgical steps to perform this procedure.
Technique Video
Isolated fractures involving the posterior wall are situated along the acetabular rim while keeping the posterior column intact; frequently, they are associated with multiple fragments, marginal impactions, or trapped pieces.1 In cases devoid of these features, selecting an appropriate treatment approach can be perplexing. Applying conservative methods for relatively minor, nondisplaced fractures carries its own set of challenges. Extended bed rest combined with continuous traction can lead to complications such as pressure ulcers, thromboembolism, infections along pin tracks, orthostatic pneumonia, and urinary tract infections.1,2 Furthermore, conservative management yields suboptimal results when displacement of the fragment is present.2,3
Although traditional open methods enable anatomic realignment and sturdy fixation, they come with significant drawbacks owing to the extensive exposure they necessitate. Complications can arise, encompassing infections, significant blood loss, wound-related issues, sciatic nerve damage, and weakening of the abductor muscles, as well as the formation of abnormal bone outside its usual location (heterotopic ossification).4 For specific cases involving less than 25% of the posterior wall and a solitary non-impacted fragment, an alternative minimally invasive option is warranted to mitigate surgical trauma while avoiding the risks associated with wide surgical exposure. Hip arthroscopy emerges as a suitable contender in these situations.5,6
Arthroscopy has proved its effectiveness in supporting the fixation of several intra-articular fractures, such as those of the tibial plateau and ankle, offering undisputed advantages such as direct visualization of the joint space, reduced invasiveness, and the capability to identify cartilage lesions and soft-tissue injuries.7,8 The realm of hip arthroscopy has undergone notable evolution over time, now being regarded as the standard procedure for diagnosing and treating multiple intra-articular issues such as femoroacetabular impingement, septic arthritis, and pigmented villonodular synovitis.9,10
Increasing evidence supports the safety and efficacy of arthroscopy in managing several traumatic hip conditions, including Pipkin fractures, intra-articular loose bodies, osteochondral lesions, and labral tears.11,12 The benefits brought by arthroscopy include direct and superior visualization of the joint and the ability to perform joint flushing and selective removal of damaged tissue, all while minimizing invasiveness and reducing the need for extensive surgical dissection.13 Nonetheless, there exist limited reports in the literature regarding labral fixation of posterior wall fractures, indicating its valuable role in enhancing overall outcomes through meticulous patient selection.6,14
In this article, we describe a surgical technique we have performed in a series of cases involving posterior wall fractures in which a single displaced fragment accounted for less than 25% of the posterior wall surface area and that were addressed through reduction and fixation using hip arthroscopy with the patient in the prone position. The objectives of our study are to delineate the surgical technique used, to provide a few tips we have developed during our learning curve, and to address the main limitations of this procedure in the fixation of these types of acetabular fractures.
Surgical Technique
The patient is placed in the prone position with the affected limb in traction. Gel pads are positioned under the patient’s shoulders and iliac spines following the standard technique for prone positioning in traction. It is essential to use a fully radiolucent traction table to obtain alar and obturator fluoroscopic views without interference from the metal of the table.
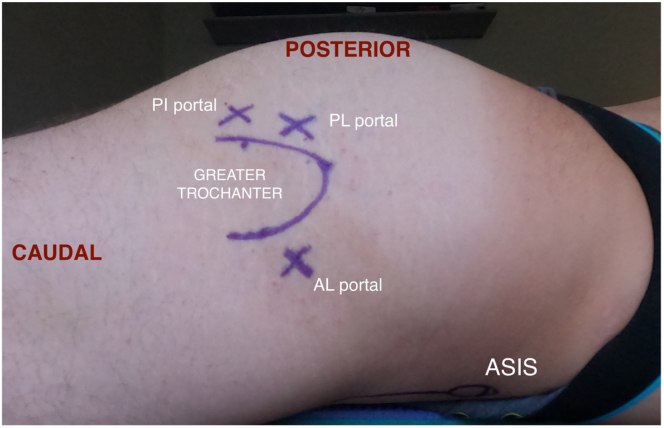
The operating room setup is shown in Figure 1. The affected limb is placed in traction to achieve sufficient distraction, similar to the technique used during supine elective hip arthroscopy. The fluoroscopy system with its monitor and the arthroscopic column are placed on the contralateral side of the traction table, facing the surgeon. Skin landmarks are drawn on the greater trochanter and anterior superior iliac spine (Fig 2). Three arthroscopic portals are used, the classic anterolateral (AL) (placed 1 cm proximal and 66 1 cm anterior to the tip of the greater thochanter) and posterolateral (PL) portals (placed 1 cm proximal 67 and 1 cm anterior to the tip of the greater trochanter), and an additional posterior portal located 68 about 2 to 4 cm distally to the PL portal. This last portal can be positioned more medially if the desired screw entry point is less peripheral on the acetabulum. However, it should be emphasized that this carries the risk of injuring the sciatic nerve and a possibly too vertical (and therefore intra-articular) direction.
Fig 1.
Intraoperative patient positioning. Under general anesthesia, the patient is placed in the prone decubitus position with the operative limb (right leg) in traction on a radiolucent table. A distraction pad (pink pad) is placed under the patient to prevent sliding and achieve bottomless traction. The C-arm and arthroscopy monitor are on the contralateral side of the table.
Fig 2.
Skin landmarks for prone hip arthroscopy of the right leg. (AL, anterolateral portal; ASIS, anterior superior iliac spine; PI, posteroinferior portal; PL, posterolateral portal.)
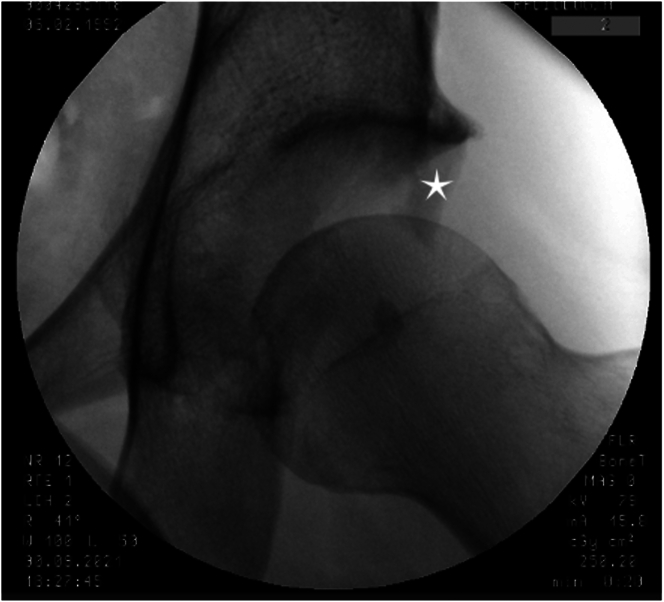
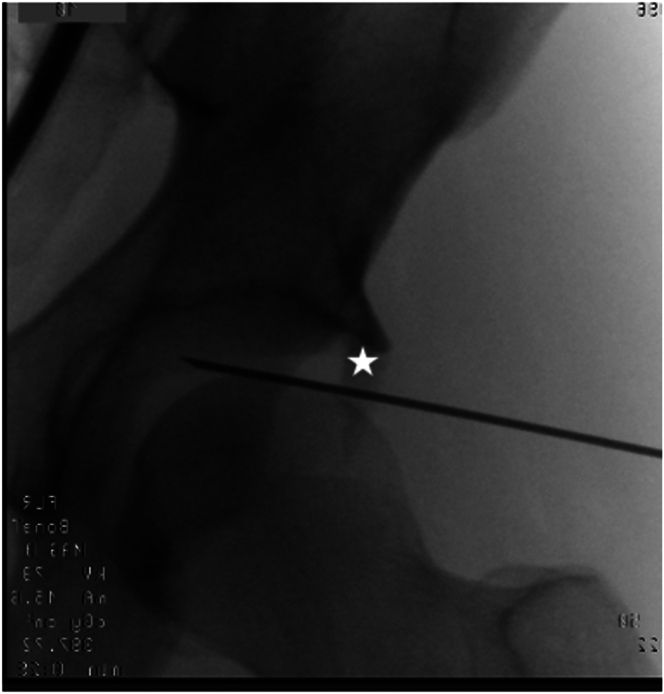
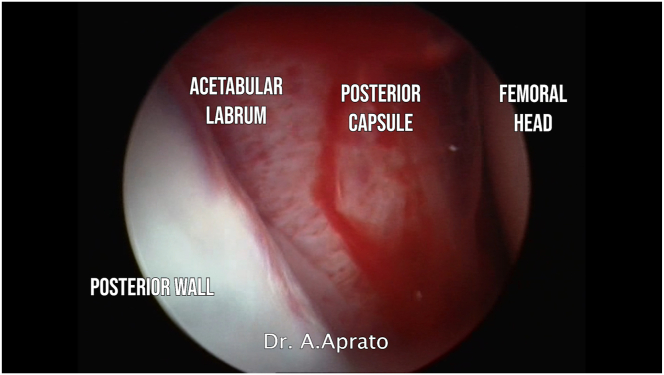
The first portal (AL) is obtained under fluoroscopic guidance. Space in the hip joint is created throughout distraction with the traction table (Fig 3). A nitinol wire is used to penetrate the hip capsule and access the central compartment of the hip (Fig 4). Then, with guided instruments, the arthroscope is positioned, allowing joint visualization. The AL and PL portals are used throughout the procedure for visualization and allow viewing of the entire joint (Fig 5), including the smaller fragments usually located in the fovea (Fig 6).
Fig 3.
Under fluoroscopic guidance, the hip joint of the left leg is distracted to gain the proper working space. The star indicates the main posterior wall fragment.
Fig 4.
A nitinol wire is used as a guide to enter the central compartment of the left leg. The star indicates the main posterior wall fragment.
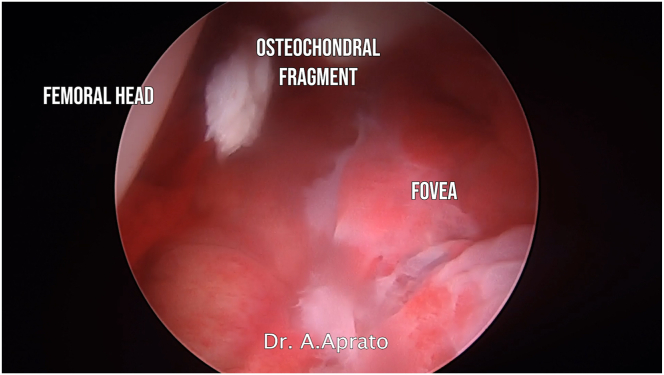
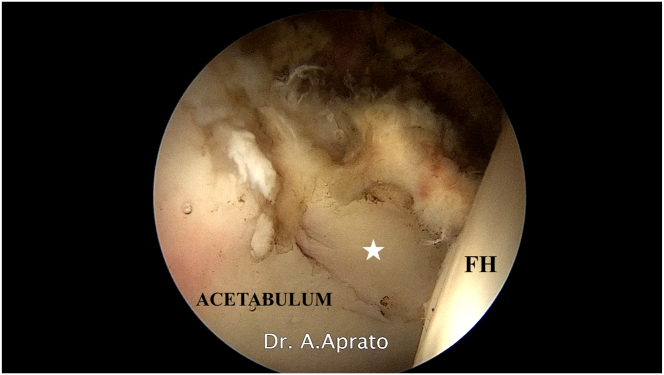
Fig 5.
Hip joint of the left leg view (intracapsular) through anterolateral portal. The anatomic structures are labeled.
Fig 6.
View from anterolateral portal (left leg). Small fracture fragments can be identified during the arthroscopic diagnostic phase.
The second portal (PL) is created with a standard technique through direct visualization from the AL portal and allows removal of the initial hematoma, as well as extraction of any free fragments that cannot be fixed, and fracture reduction (Fig 7), at the end the fracture line, should be clearly visible. Hematoma removal can be achieved using a large-diameter soft-tissue shaver (e.g., 3.5 mm). Once a good view is obtained, the posterior wall fragment is mobilized (it is recommended to perform the arthroscopic procedure shortly after trauma because scar tissue can complicate reduction). Mobilization is usually made challenging by the intact labrum, but if it is possible to avoid releasing the fragment from the labrum, the reduction will be easier. Under direct visualization, the posteroinferior (PI) portal is then created, considering the desired screw direction.
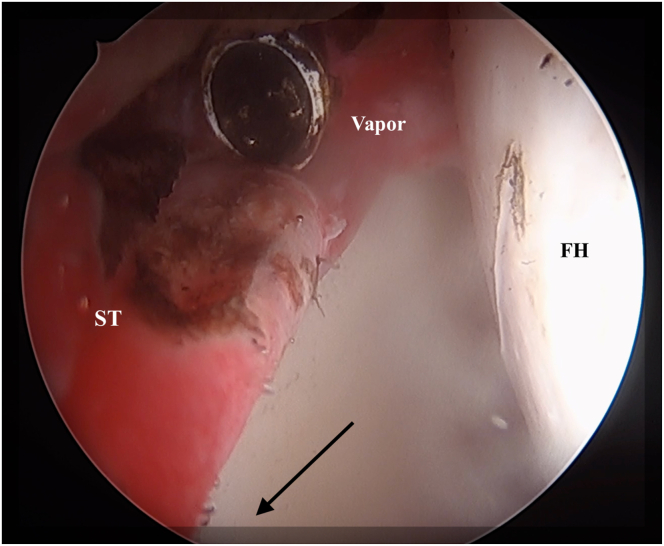
Fig 7.
Through the posterolateral portal (left leg), with classic arthroscopic instruments (shaver, radiofrequency probe, and hooks), the surgeon can address the soft tissue (paying attention not to injure the acetabular labrum) to free the main fragment. The arrow indicates the position of the main posterior wall fragment. (FH, femoral head; ST, soft tissue surrounding main fragment.)
As shown in Video 1, the fragment can now be reduced using a pointed cruciate clamp or a microfracture pick through the PL portal (Fig 8). The quality of the reduction is evaluated by direct visualization of the articular surface. Once reduced, temporary synthesis is performed using long K-wires with a diameter of 1.4 to 1.6 mm under fluoroscopic guidance from the PI portal (Fig 9). If the achieved reduction is satisfactory, definitive synthesis can be achieved using 4.5-mm cannulated screws (Citieffe Rondo) (Fig 10). We recommend using 4.5-mm cannulated screws because of the usually more rigid K-wires, simplifying both the reduction (also used as joysticks) and the fixation, reducing the risk of bending or breaking during screw insertion. Additionally, the 4.5-mm screwdriver is longer, allowing easier insertion, especially in patients with larger thighs (Fig 6).
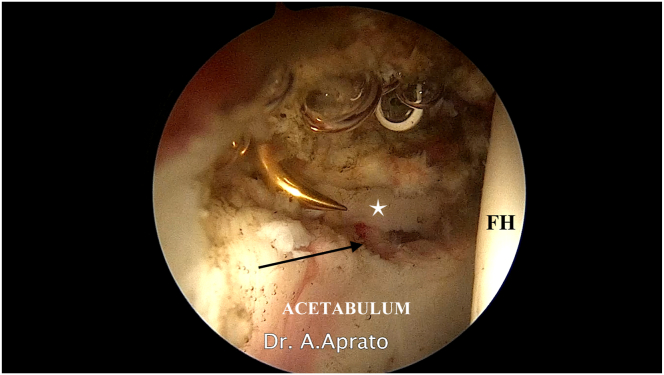
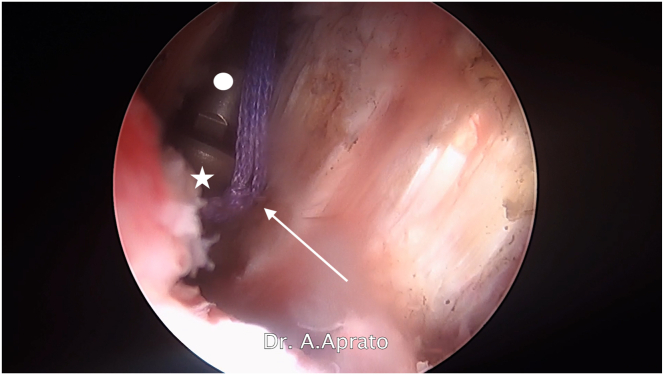
Fig 8.
View from anterolateral portal (left leg). Through posterolateral (blunt hook) and posteroinferior (radiofrequency probe) portals, with a combination of instruments, the main fragment (star) is mobilized to obtain fracture reduction. The arrow indicates the fracture site. (FH, femoral head.)
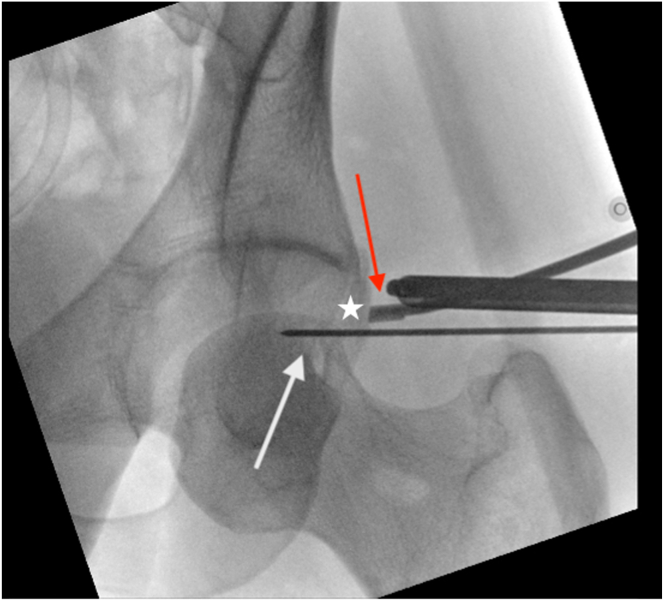
Fig 9.
Fluoroscopic image of reduction maneuver. A 1.4-mm K-wire is inserted through the posteroinferior portal (left leg) and used to temporarily stabilize the main fragment. A pointed cruciate clamp or a microfracture clamp is used to help in the reduction. The white arrow indicates the 1.4-mm K-wire stabilizing the fragment; red arrow, microfracture pick helping in reduction; and star, main fragment.
Fig 10.
Arthroscopic view of reduction from anterolateral portal (left leg). The star indicates the main fragment. (ACETABULUM, posterior part of acetabulum; FH, femoral head.)
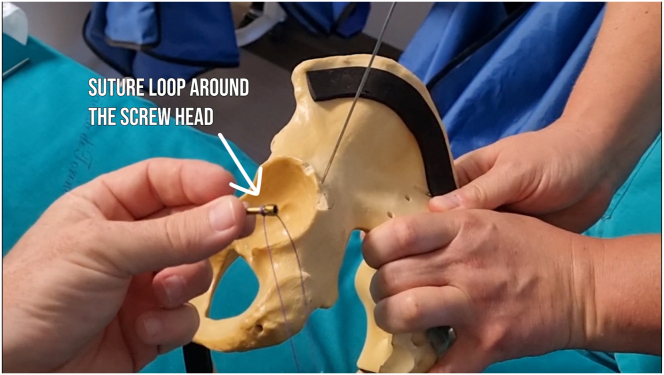
To avoid the risk of misplaced screws, a pointed cannulated guide handle for 4.5-mm screws, normally used for inserting the femoral nail’s head screw, can also be used (Citieffe Endovis femoral trocar [EBA-0025] for cephalic screw). To prevent possible screw loss into the soft tissues, it is suggested to use a loop-knotted wire around the proximal part of the screw, as described in other procedures. This wire is cut at the end of the procedure (Figs 11 and 12).
Fig 11.
View from anterolateral portal (left leg). Screw insertion is performed through the posteroinferior portal. The star indicates the screw head; circle, screwdriver; and arrow, suture loop knotted around screw head.
Fig 12.
A loop-knotted wire is placed around the screw to prevent screw loss into the joint (left leg).
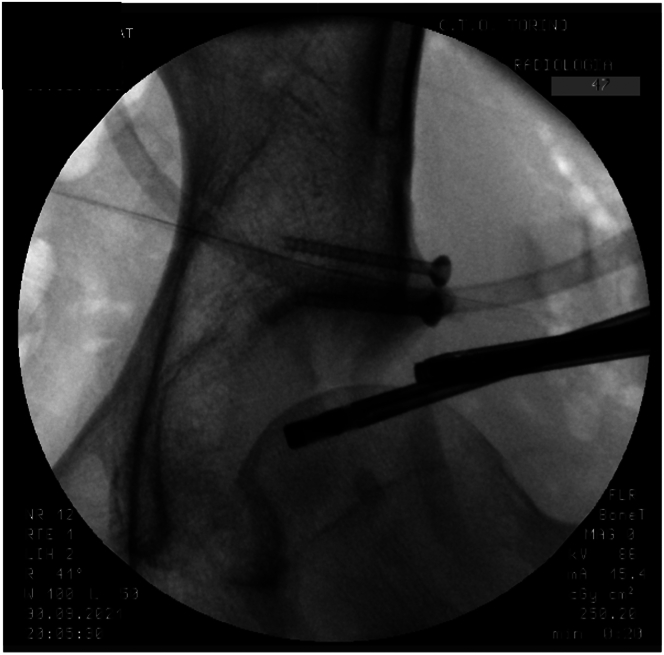
Once the screws are placed, a final fluoroscopic evaluation is performed in 3 projections (anteroposterior, alar, and obturator) (Fig 13). Once satisfactory fixation is obtained, fluids are drained out from the joint and traction is released. Skin is closed with silk suture wire or a stapler. The patient is then gently positioned supine for the awakening procedure with the anesthesiologist. The patient is advised to perform toe-touch weight bearing with crutches for 30 days without restriction of range of motion.
Fig 13.
Fluoroscopic evaluation of screw position (left leg). The fracture is anatomically reduced, and the joint surface is restored.
Discussion
Hip arthroscopy for hip trauma has gained increasing interest as a dependable and less invasive option, and its popularity has grown over the years owing to a widening array of applicable scenarios.2,11 Our findings suggest that hip arthroscopy could be a suitable choice for treating specific cases of posterior wall fractures. All patients treated with described technique showed notable clinical and radiologic enhancements at least 1 year after the initial operation, with no significant complications reported that affected functional outcomes. It is important to note that, to our knowledge, the use of screws for fixation has not been documented before.
In the existing literature, there are only a few articles that have discussed the arthroscopic treatment of posterior wall fractures—and fewer that have described screw fixation. For example, Shi et al.6 presented a case report involving a 14-year-old boy with an acetabular posterior wall fracture treated with arthroscopic anchor-based fixation. Two anchors were positioned at the upper and lower edges of the fracture site, with threads secured around the fragment, and a third anchor was inserted into the fragment, with all 3 anchor threads intertwined. The patient exhibited complete union in 3 months per follow-up radiographs, although long-term outcomes were not reported.6 Stabile15 et al.16 recounted the case of a 46-year-old woman who experienced a posterior acetabular fracture-dislocation due to a motor vehicle collision. After reduction, a computed tomography scan revealed a non-concentric reduction and trapped loose bodies. Through hip arthroscopy, the loose bodies were removed, and during joint evaluation, an osseous bucket-handle labral tear was identified. The labral-osseous fragment was repositioned using a switching stick and affixed with a combination of anchors and loop sutures. However, the authors did not provide details about the patient’s postoperative outcome. Vale et al. presented a case report of a posterior wall acetabular fracture treated with a combination of a posterolateral mini-invasive approach (4 in) to the hip with arthroscopic assistance for assessing articular reduction and subsequent fixation with two 4-mm cannulated screws, with good results. Zhong et al.14 reported on a series of 9 patients with a diagnosis of a posterior labral tear accompanied by an attached bony fragment after traumatic posterior hip dislocation. These cases were addressed by hip arthroscopic techniques, using suture anchor fixation for the fragment without the use of screws. Additional procedures in some patients included the removal of loose bodies or microfracture of the exposed subchondral bone. All cases achieved uneventful union, with a mean modified Harris Hip Score of 81.8 (standard deviation, 2) at the 1-year postoperative mark.14 Hwang et al.17 recently published a case series of 13 patients who received arthroscopic fixation of acetabular posterior wall fractures with cannulated screws, in the lateral decubitus position, addressing this procedure as a good alternative option with good radiographic and clinical outcomes, convenient removal of intra-articular loose bodies, and low complication rates.
The arthroscopic technique itself has its own limitations that warrant discussion. Careful patient and case selection is of utmost importance when considering fractures suitable for arthroscopic fixation, giving its limited reduction capabilities; in cases of acetabular fractures featuring substantial posterior wall fragments and significant hip instability, opting for formal open reduction–internal fixation is advisable. However, for partial posterior wall fractures lacking major displacement and not requiring fixation with a plate for biomechanical reasons, open reduction introduces unnecessary risks of complications.18,19 Notably, there is currently no specific set of headless screws with the desired dimensions available on the market; the existing ones have guiding wires that are too small and flexible. Moreover, the prolonged surgical time and the surgeon’s learning curve must be taken into consideration.
Conversely, arthroscopy can facilitate precise anatomic realignment and secure screw fixation with minimal invasiveness. Additionally, it offers the advantages of evaluating joint congruity through direct joint visualization, diagnosing and addressing associated lesions such as labral tears, and managing intra-articular loose bodies—common findings in hips with posterior wall fractures, especially in instances of hip dislocation.20,21 It is associated with lower risks of femoral head avascular necrosis.
Advantages and disadvantages of arthroscopic fixation of acetabular posterior wall fractures are summarized in Table 1. The operating room setting is of utmost importance. To obtain proper projections, the C-arm should be perpendicular to the patient; as a result, the arthroscopic column is shifted distally, conversely to the elective setting. In addition, we have experienced benefits in placing the operative portal (PI portal) more distal and more medial than initially thought; this allows to have a better direction for reduction tools and to fire the screws with good direction. Frequently, articular impaction can be observed; even if limited, we advocate strictly following the chondral articular reduction of the fragment even if the outer cortical bone has some mismatch.
Table 1.
Advantages and Disadvantages of Arthroscopic Posterior Wall Reduction and Fixation
| Advantages | Disadvantages |
|---|---|
| Minimally invasive | Limited reduction capabilities |
| Direct control of articular reduction | Lighter fixation |
| No risk of iatrogenic avascular necrosis | Slightly longer surgical time |
| Possibility of treating associated lesions | Lack of dedicated screw set |
One of the challenges of our technique is managing the rotation of the fragment; the surgeon should take care to ensure its delicate mobilization, avoiding flipping it over. The surgeon should always check for accidental intra-articular placement of the screws directly with the scope because traction frequently rotates the pelvis, making oblique projections less accurate. Pearls and pitfalls are described in Table 2.
Table 2.
Pearls and Pitfalls of Arthroscopic Posterior Wall Reduction and Fixation
| Pearls | Pitfalls |
|---|---|
| Distal and medial placement of posterior portal | Intra-articular screw placement |
| Follow articular reduction, not cortical | Fragment derotation |
| Retain cannulated screw with suture | Distal proximity of sciatic nerve |
| Consider use of long pointed sleeves for safe placement of wire and screws | Pelvic tilt due to prone traction |
We propose the consideration of arthroscopic fixation for selected posterior wall fractures. Specifically, a displaced single fragment that constitutes less than 25% of the posterior wall surface can be effectively addressed arthroscopically using 2 screws. This approach is recommended for surgeons who regularly handle a substantial caseload of either acetabular fractures or hip arthroscopy procedures. Further studies are necessary to compare this approach with the established gold standard in terms of outcome scores and complications, ideally supported by a higher level of evidence.
Disclosures
The authors report no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Footnotes
This reseach was fund by the University of Turin.
Supplementary Data
Hip arthroscopy (left leg) is performed on a traction table with the patient in the prone position (Fig 1). A standard arthroscopic technique is used to access the central compartment using the anterolateral (AL) and posterolateral (PL) portals; an accessory portal (more distal to the PL portal) is used for fracture fixation. The AL portal is used to visualize the procedure, while a horizontal capsulotomy is performed through the PL portal with posterior enlargement of the capsulotomy; the fragment is then isolated with radiofrequency and a shaver without detaching it from the labrum. The fracture is reduced with a ball spike or a microfracture pick, pushing it against the healthy part of the acetabulum from the external border (Fig 7). If an appropriate reduction is not achieved, 2 Herbert screw guide pins are placed in the free fragment and used as joysticks to reduce the fracture. Eventually, the fragment is fixed with 2 cannulated Herbert screws with specific attention to avoid intra-articular penetration (Fig 11, Fig 12). The only postoperative restriction is to avoid weight bearing on the affected side for 40 days.
References
- 1.Baumgaertner M.R. Fractures of the posterior wall of the acetabulum. J Am Acad Orthop Surg. 1999;7:54–65. doi: 10.5435/00124635-199901000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Yamamoto Y., Ide T., Ono T., Hamada Y. Usefulness of arthroscopic surgery in hip trauma cases. Arthroscopy. 2003;19:269–273. doi: 10.1053/jars.2003.50033. [DOI] [PubMed] [Google Scholar]
- 3.Magu N.K., Rohilla R., Arora S. Conservatively treated acetabular fractures: A retrospective analysis. Indian J Orthop. 2012;46:36–45. doi: 10.4103/0019-5413.91633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kaempffe F.A., Bone L.B., Border J.R. Open reduction and internal fixation of acetabular fractures: Heterotopic ossification and other complications of treatment. J Orthop Trauma. 1991;5:439–445. doi: 10.1097/00005131-199112000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Yang J.H., Chouhan D.K., Oh K.J. Percutaneous screw fixation of acetabular fractures: Applicability of hip arthroscopy. Arthroscopy. 2010;26:1556–1561. doi: 10.1016/j.arthro.2010.04.068. [DOI] [PubMed] [Google Scholar]
- 6.Shi R.M., Yuan L.B., Tan C.J., et al. Hip arthroscopic reduction and fixation for adolescent acetabular posterior wall fracture: A case report. Orthop Surg. 2021;13:1934–1938. doi: 10.1111/os.13051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chan Y.S., Chiu C.H., Lo Y.P., et al. Arthroscopy-assisted surgery for tibial plateau fractures: 2- to 10-year follow-up results. Arthroscopy. 2008;24:760–768. doi: 10.1016/j.arthro.2008.02.017. [DOI] [PubMed] [Google Scholar]
- 8.Ono A., Nishikawa S., Nagao A., Irie T., Sasaki M., Kouno T. Arthroscopically assisted treatment of ankle fractures: Arthroscopic findings and surgical outcomes. Arthroscopy. 2004;20:627–631. doi: 10.1016/j.arthro.2004.04.070. [DOI] [PubMed] [Google Scholar]
- 9.Jamil M., Dandachli W., Noordin S., Witt J. Hip arthroscopy: Indications, outcomes and complications. Int J Surg. 2018;54:341–344. doi: 10.1016/j.ijsu.2017.08.557. [DOI] [PubMed] [Google Scholar]
- 10.Larson C.M., Swaringen J., Morrison G. A review of hip arthroscopy and its role in the management of adult hip pain. Iowa Orthop J. 2005;25:172–179. [PMC free article] [PubMed] [Google Scholar]
- 11.Niroopan G., De Sa D., MacDonald A., Burrow S., Larson C.M., Ayeni O.R. Hip arthroscopy in trauma: A systematic review of indications, efficacy, and complications. Arthroscopy. 2016;32:692–703. doi: 10.1016/j.arthro.2015.12.029. [DOI] [PubMed] [Google Scholar]
- 12.Aprato A., Buzzone M., Di Benedetto P., Massè A. Surgical hip dislocation vs arthroscopy for fixation of subfoveal femoral head fractures: A new technique for Pipkin type 1 fractures. Acta Biomed. 2021;92 doi: 10.23750/abm.v92iS3.11724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khanna V., Harris A., Farrokhyar F., Choudur H.N., Wong I.H. Hip arthroscopy: Prevalence of intra-articular pathologic findings after traumatic injury of the hip. Arthroscopy. 2014;30:299–304. doi: 10.1016/j.arthro.2013.11.027. [DOI] [PubMed] [Google Scholar]
- 14.Zhong M., Xie H., Fu Z., Lu W., Zhu W., Ouyang K. Arthroscopic treatment of acetabular rim fracture after traumatic posterior hip dislocation: A case series study. Orthop Surg. 2021;13:1828–1834. doi: 10.1111/os.13106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vale J., Diniz S., Santos Leite P., Soares D. Surgical treatment of acetabular posterior wall fracture with hip arthroscopy: A case report. Hip Pelvis. 2022;34:62–67. doi: 10.5371/hp.2022.34.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stabile K.J., Neumann J.A., Mannava S., Howse E.A., Stubbs A.J. Arthroscopic treatment of bucket-handle labral tear and acetabular fracture. Arthrosc Tech. 2014;3:e283–e287. doi: 10.1016/j.eats.2014.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hwang J.M., Lee C.W., Kim P.S., Ha Y.C. Arthroscopic reduction and internal fixation in patients with acetabular posterior wall fractures. Clin Orthop Surg. 2023;15:718–724. doi: 10.4055/cios22199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Foulk D.M., Mullis B.H. Hip dislocation: Evaluation and management. J Am Acad Orthop Surg. 2010;18:199–209. doi: 10.5435/00124635-201004000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Mandell J.C., Marshall R.A., Banffy M.B., Khurana B., Weaver M.J. Arthroscopy after traumatic hip dislocation: A systematic review of intra-articular findings, correlation with magnetic resonance imaging and computed tomography, treatments, and outcomes. Arthroscopy. 2018;34:917–927. doi: 10.1016/j.arthro.2017.08.295. [DOI] [PubMed] [Google Scholar]
- 20.Park M.S., Yoon S.J., Choi S.M. Hip arthroscopic management for femoral head fractures and posterior acetabular wall fractures (Pipkin type IV) Arthrosc Tech. 2013;2:e221–e225. doi: 10.1016/j.eats.2013.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morris A.C., Yu J.C., Gilbert S.R. Arthroscopic treatment of traumatic hip dislocations in children and adolescents: A preliminary study. J Pediatr Orthop. 2017;37:435–439. doi: 10.1097/BPO.0000000000000670. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Hip arthroscopy (left leg) is performed on a traction table with the patient in the prone position (Fig 1). A standard arthroscopic technique is used to access the central compartment using the anterolateral (AL) and posterolateral (PL) portals; an accessory portal (more distal to the PL portal) is used for fracture fixation. The AL portal is used to visualize the procedure, while a horizontal capsulotomy is performed through the PL portal with posterior enlargement of the capsulotomy; the fragment is then isolated with radiofrequency and a shaver without detaching it from the labrum. The fracture is reduced with a ball spike or a microfracture pick, pushing it against the healthy part of the acetabulum from the external border (Fig 7). If an appropriate reduction is not achieved, 2 Herbert screw guide pins are placed in the free fragment and used as joysticks to reduce the fracture. Eventually, the fragment is fixed with 2 cannulated Herbert screws with specific attention to avoid intra-articular penetration (Fig 11, Fig 12). The only postoperative restriction is to avoid weight bearing on the affected side for 40 days.