Abstract
Objectives
We aimed to examine the extent to which health plan expenditures for infertility services differed by whether women resided in states with mandates requiring coverage of such services and by whether coverage was provided through a self-insured plan subject to state mandates versus fully-insured health plans subject only to federal regulation.
Methods
This retrospective cohort study used individual-level, de-identified health insurance claims data. We included women 19–45 years of age who were continuously enrolled during 2011 and classified them into three mutually exclusive groups based on highest treatment intensity: in vitro fertilization (IVF), intrauterine insemination (IUI), or ovulation-inducing (OI) medications. Using generalized linear models, we estimated adjusted annual mean, aggregate, and per member per month (PMPM) expenditures among women in states with an infertility insurance mandate and those in states without a mandate, stratified by enrollment in a fully-insured or self-insured health plan.
Results
Of the 6,006,017 women continuously enrolled during 2011, 9199 (0.15%) had claims for IVF, 10,112 (0.17%) had claims for IUI, and 23,739 (0.40%) had claims for OI medications. Among women enrolled in fully insured plans, PMPM expenditures for infertility treatment were 3.1 times higher for those living in states with a mandate compared with states without a mandate. Among women enrolled in self-insured plans, PMPM infertility treatment expenditures were 1.2 times higher for mandate versus non-mandate states.
Conclusions for Practice
Recorded infertility treatment expenditures were higher in states with insurance reimbursement mandates versus those without mandates, with most of the difference in expenditures incurred by fully-insured plans.
Keywords: In vitro fertilization, Infertility, Artificial insemination, Assisted reproductive technologies, Ovulation induction, Expenditures, Insurance
Introduction
Infertility, commonly defined as the inability of couples become pregnant after 12 months of trying, is a disease that is estimated to affect between 6.0 and 15.5% of reproductive aged women in the U.S. (Chandra et al. 2013; Thoma et al. 2013). The use of medical interventions to overcome infertility has become increasingly common over time with approximately 6.9 million U.S. women 25–44 years of age reporting having ever used infertility services between 2006 and 2010 (Chandra et al. 2014). Infertility treatments can be costly, depending on the frequency and intensity of services used and the degree to which the treatments are covered by health insurance. Findings from one study indicated that median out-of-pocket expenses (i.e., those not paid by health insurance) for an 18-month period were $912 for couples using medications only, $2623 for those using intrauterine insemination (IUI), and $19,324 for those using in vitro fertilization (IVF) (Katz et al. 2011).
Historically, insurance coverage of infertility treatments has been limited because such procedures were not considered medically necessary (Neumann 1997; Johnston et al. 2014). Indeed, data from a 2005 survey indicated that, among US employers with 500 or more employees, only 37% covered ovulation-inducing (OI) medications, and 19% covered IVF (William M Mercer, Inc. 2006). To expand access to infertility services, 15 states enacted an infertility insurance mandate between 1977 and 2001 (Henne and Bundorf 2008; Bitler and Schmidt 2012). The scope of the mandates varies widely across states, with some states requiring that insurers provide coverage for certain types of infertility treatments and others only requiring that insurers offer health plans that include some type of infertility benefit (Henne and Bundorf 2008; Martin et al. 2011; Bitler and Schmidt 2012). Furthermore, state insurance laws do not apply to most self-insured employers because the federal Employee Retirement Income Security Act (ERISA) pre-empts state regulation of such plans (Jensen and Morrisey 1999). Large employers are typically self-insured, with health plans merely administering claims, whereas smaller employers usually purchase coverage from fully-insured health plans. In 2011, approximately 58% of U.S. workers in the private sector who were enrolled in employer-sponsored health insurance were enrolled in self-insured plans (Agency for Healthcare Research and Quality 2011). In addition, some self-insured employers are in the public sector, and state insurance mandates may apply to self-insured health plans covering state employees (Barry et al. 2017).
Infertility insurance mandates have been shown to increase use of infertility services in studies using the Society for Assisted Reproductive Technologies (SART) clinical data reported to the Centers for Disease Control and Prevention and the National Survey of Family Growth (Henne and Bundorf 2008; Bitler and Schmidt 2012; Hamilton and McManus 2012). However, while several studies assessed expenditures associated with IVF (Collins et al. 1995; Griffin and Panak 1998; Chambers et al. 2009; Katz et al. 2011; Wu et al. 2014) and other types of infertility treatments (Katz et al. 2011; Wu et al. 2014) from a societal perspective, the extent to which health plan expenditures differ for women residing in states with and without a mandate has not been studied. Therefore, the purpose of our study was to examine the magnitude by which infertility treatment expenditures incurred by health plans are higher in states with mandates requiring coverage of such services differentially for fully-insured plans subject to state mandates and self-insured health plans which in principle are subject only to federal regulation. We aimed to use claims data from a large employer sponsored health insurance claims database to compare aggregate and per-member-per-month (PMPM) costs by mandate status for fully-insured and self-insured plans. Claims data are uniquely suited to assess that question, and as far as is known, this is the first study to use claims data for this purpose.
Methods
The data used for this study were derived from the 2011 Truven Health MarketScan Commercial Claims and Encounters Databases. These administrative data are composed of individual-level, de-identified health insurance claims from employers across the U.S. that offer private health insurance to employees as well as their spouses and dependents. Medical claims for inpatient and outpatient services are linked to outpatient prescription drug claims and person-level enrollment information. Individuals can be tracked longitudinally using unique identifiers. A variety of insurance plan types are represented, including fee-for-service, preferred provider organizations, and capitated health plans. In 2011, the MarketScan Commercial Databases contained information on more than 52 million insured individuals with employer-sponsored insurance with data contributed by over 150 self-insured employers and 21 fully-insured health plans.
We restricted the analysis to women 19–45 years of age with information on prescription drug claims who were continuously enrolled (≥ 11 months) during 2011. Women < 19 years and > 45 years of age were excluded due to low frequency of IVF use. We classified the women into three mutually exclusive groups based on the highest level of infertility treatment intensity reported on claims filed during the calendar year: IVF, IUI, or OI medications. Accordingly, if a woman had claims for both OI medications and IUI, she would be included in the IUI group. IVF treatments were identified by the presence of an International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) code for an IVF visit (V26.81) or a current procedural terminology (CPT) code for oocyte retrieval (58970) or embryo transfer (58974, 58976) on an outpatient service claim. IUI treatments were identified by an ICD-9-CM code for an IUI visit (V26.1) or a CPT code for artificial insemination (58321, 58322) on an outpatient service claim. We used outpatient prescription claims data to ascertain the use of OI medications including clomiphene citrate, follicle stimulating hormone, luteinizing hormone, human chorionic gonadotropin, human menopausal gonadotropin, gonadotropin releasing hormone (GnRH), GnRH agonists, GnRH antagonists, aromatase inhibitors, metformin, estradiol, and progesterone. The medication claims were detected using National Drug Codes associated with the generic product names (S1 Table); all formulations were included. To reduce potential misclassification in the group of women using OI medications without any corresponding report of IVF or IUI treatments during a given calendar year, we only included those women with report of an infertility diagnosis (ICD-9-CM codes 628.0–628.4, 628.8, 628.9) or infertility testing (ICD-9-CM code V26.21) in the 6 months prior to first filled prescription. In addition, women with one or more filled estradiol prescriptions but no other OI medication claim were only included if there was a concomitant claim for progesterone 6 weeks before or after the estradiol claim as progesterone alone may be used for indications other than infertility. Women with claims for progesterone only were not included.
To characterize the study population, we examined the distribution of age, infertility diagnosis, use of infertility testing, insurance type (comprehensive, preferred provider or exclusive provider organization, health maintenance organization or capitated point-of-service, non-capitated point-of-service, and consumer driven health plan or high deductible health plan), health plan type (fully-insured or self-insured), and region of residence for each of the infertility treatment groups and for women without claims for infertility treatment. We also assessed the proportion of women living in a state with an infertility insurance mandate (Arkansas, California, Connecticut, Hawaii, Illinois, Louisiana, Maryland, Massachusetts, Montana, New Jersey, New York, Ohio, Rhode Island, Texas, and West Virginia) and those living in states without a mandate. All state mandates were enacted by 2005. Data were missing for ≤ 1% of all characteristics except insurance type (5%).
For each treatment type, we calculated adjusted annual estimates of mean health plan expenditures per women with ≥ 1 relevant claim. We included all outpatient service claims with ICD-9-CM codes for IUI or IVF visits and claims with CPT codes for procedures specific to IVF or IUI (S2 Table). We estimated medication expenditures by assessing filled outpatient prescription medication claims for all aforementioned OI medications, including progesterone. Claims for outpatient visits were aggregated by date of service. Expenditures included total net payments for a particular service and represented plan or employer liability; expected out-of-pocket payments and coordination of benefits were excluded. We used generalized linear models with a log-link function and gamma distribution to estimate adjusted mean and aggregate estimates of annual expenditures, after controlling for patient age and region of residence. Per member per month (PMPM) expenditures were calculated by dividing aggregate annual expenditures by the total number of continuously enrolled women 19–45 years of age multiplied by 12. We also calculated the unadjusted mean number of treatment visits and medication claims and 95% confidence intervals for infertility treatments. We stratified all estimates according to the presence or absence of a state mandate and by enrollment in a self-insured or fully-insured health plan.
Among states with mandates, only eight (Arkansas, Connecticut, Hawaii, Illinois, Maryland, Massachusetts, New Jersey, and Rhode Island) require that plans cover IVF treatment; in addition, the amount of coverage differs substantially among states. To further examine differences in IVF-related claims, we restricted the study population to women in the IVF group that lived in any of the eight states with mandated IVF coverage. We compared IVF expenditures for women living in Illinois, Massachusetts, New Jersey and Rhode Island, states with a comprehensive mandate that require coverage of at least four IVF cycles, with those for women living in the remaining four states with more limited IVF mandates. These estimates were also calculated separately for fully-insured and self-insured health plan types.
We used Pearson chi-squared tests to compare the distribution of patient characteristics among the infertility treatment groups. Because the infertility expenditure data were right skewed, we used the Wilcoxon rank-sum test to assess differences in the distributions between states with and without an infertility insurance mandate for each infertility treatment group. An alpha of 0.05 was used to determine statistical significance. All analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC) and Stata 14 (College Station, TX). Because the MarketScan data are de-identified, this study was determined to be exempt from review by the Center for Disease Control and Prevention’s institutional review board.
Results
A total of 6,006,017 women 19–45 years of age were continuously enrolled during 2011; of those, 48.1% were enrolled in fully-insured plans. Within the population of continuously enrolled women, 9199 (0.15%) had one or more IVF claims, 10,112 (0.17%) had one or more IUI claims, and 23,736 (0.40%) had one or more claims for OI medications (Table 1). Approximately 2.2% of women in the IVF group were 19–25 years of age, compared with 3.6% and 7.9% in the IUI and OI medication groups, respectively. Infertility of unspecified origin was the most commonly reported diagnosis for all treatment types. Anovulation was reported more frequently in the OI medication group than the IUI or IVF group (26.3% vs. 19.2% and 13.2%, respectively).
Table 1.
Characteristics of commercially insured women 19–45 years of age with claims for infertility treatments during 2011
| In vitro fertilizationa |
Intrauterine insemination |
Ovulation-inducing medications only |
All enrollees |
|||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | |
|
| ||||||||
| Total | 9919 | 10,112 | 23,736 | 6,006,017 | ||||
| Ageb | ||||||||
| 19–25 | 216 | 2.2 | 368 | 3.6 | 1872 | 7.9 | 1,388,382 | 23.1 |
| 26–30 | 1733 | 17.5 | 2440 | 24.1 | 6848 | 28.9 | 951,800 | 15.9 |
| 31–35 | 3519 | 35.5 | 3826 | 37.8 | 7825 | 33.0 | 1,099,298 | 18.3 |
| 36–40 | 3153 | 31.8 | 3647 | 26.2 | 5318 | 22.4 | 1,244,443 | 20.7 |
| 41–45 | 1298 | 13.1 | 831 | 8.2 | 1873 | 7.9 | 1,322,094 | 22.0 |
| Infertility diagnosis | ||||||||
| Anovulationb | 1313 | 13.2 | 1943 | 19.2 | 6249 | 26.3 | 17,931 | 0.3 |
| Pituitary-hypothalamic origin | 67 | 0.7 | 57 | 0.6 | 122 | 0.5 | 402 | 0.01 |
| Tubal originb | 826 | 8.3 | 567 | 5.6 | 1313 | 5.5 | 6812 | 0.1 |
| Uterine originb | 175 | 1.8 | 138 | 1.4 | 182 | 0.8 | 870 | 0.01 |
| Cervical originb | 58 | 0.6 | 72 | 0.7 | 84 | 0.4 | 373 | 0.01 |
| Other origin—specifiedb | 3043 | 30.7 | 2270 | 22.5 | 3005 | 12.7 | 12,929 | 0.2 |
| Unspecified originb | 8825 | 88.9 | 8112 | 80.2 | 16,034 | 67.6 | 63,897 | 1.1 |
| Any infertility diagnosisb | 9533 | 96.1 | 9203 | 91.0 | 20,344 | 85.7 | 81,259 | 1.4 |
| Had infertility testingb | ||||||||
| Yes | 3152 | 31.8 | 3244 | 32.1 | 6150 | 25.9 | 23,812 | 0.4 |
| No | 6767 | 68.2 | 6868 | 67.9 | 17,586 | 74.1 | 5,982,205 | 99.6 |
| Insurance typec | ||||||||
| PPO/EPO | 7336 | 76.1 | 6258 | 65.4 | 15,029 | 67.3 | 3,738,164 | 66.2 |
| HMO/ capitated POS | 778 | 8.1 | 1693 | 17.7 | 3646 | 16.3 | 952,546 | 16.9 |
| POS (non-capitated) | 667 | 6.9 | 681 | 7.1 | 1708 | 7.6 | 410,388 | 7.3 |
| CDHP/HDHP | 844 | 8.8 | 887 | 9.3 | 1825 | 8.2 | 506,720 | 9.0 |
| Comprehensive | -d | 46 | 0.5 | 135 | 0.6 | 42,756 | 0.8 | |
| Health plan typeb | ||||||||
| Self-insured | 5820 | 58.7 | 6256 | 61.9 | 14,026 | 59.1 | 3,120,316 | 52.0 |
| Fully-insured | 4099 | 41.3 | 3856 | 38.1 | 9710 | 40.9 | 2,885,701 | 48.1 |
| Regionb | ||||||||
| Northeast | 2627 | 26.7 | 2691 | 26.8 | 4682 | 20.1 | 935,328 | 15.9 |
| North central | 3221 | 32.7 | 2629 | 26.2 | 5865 | 25.2 | 1,414,192 | 24.1 |
| South | 2530 | 25.7 | 2542 | 25.4 | 9059 | 38.9 | 2,427,750 | 41.3 |
| West | 1477 | 15.0 | 2166 | 21.6 | 3698 | 15.9 | 1,103,992 | 18.9 |
| Infertility insurance mandateb,e | ||||||||
| Yes | 6373 | 64.7 | 5894 | 58.8 | 11,410 | 49.0 | 2,780,252 | 47.3 |
| No | 3482 | 35.3 | 4134 | 41.2 | 11,895 | 51.0 | 3,103,726 | 52.8 |
PPO preferred provider organization, EPO exclusive provider organization, HMO health maintenance organization, POS point-of-service, CDHP consumer-driven health plan, HDHP health deductible health plan
Includes in vitro fertilization with or without intrauterine insemination
P value < .05 for comparison of distribution of the characteristic across infertility treatment groups
Insurance type missing for 5% of study population
N < 30; data not reported
Resides in a state with an infertility insurance mandate (Arkansas, California, Connecticut, Hawaii, Illinois, Louisiana, Maryland, Massachusetts, Montana, New Jersey, New York, Ohio, Rhode Island, Texas, and West Virginia); residence missing for < 2% of study population
Less than one-third of women in each treatment group had an infertility testing claim during 2011. The most common type of benefit plan was a preferred provider or exclusive provider organization; however, a greater proportion of women in the IUI and OI medication groups were enrolled in capitated plans than women in the IVF group (17.7% and 16.3% vs. 8.1%, respectively). About 60% of women receiving infertility treatment were covered by a self-insured plan, compared with 52% of all women. Nearly 65% of women in the IVF group lived in a state with an infertility insurance mandate, compared with 59% of women in the IUI group and 49% of women in the OI medication group.
For women receiving reimbursement for services through fully-insured plans, health plan expenditures for all types of infertility treatments per woman with a relevant claim were higher for women living in a state with an infertility insurance mandate compared with their counterparts in states without a mandate (Table 2). For example, the adjusted annual mean expenditures for IVF treatment among women living in the mandate states were $12,664 compared with $9791 for women living in states without a mandate.
Table 2.
Mean, aggregate and per member per month expenditures for infertility treatments among commercially insured women 19–45 years receiving reimbursement from a fully-insured health plan, 2011
| Mandate |
No mandate |
Ratio of PMPM expendituresb | |||||
|---|---|---|---|---|---|---|---|
| Adjusteda mean expenditures (SE) | Aggregate expenditures | PMPM expenditures | Adjusted mean expenditures (SE) | Aggregate expenditures | PMPM expenditures | ||
|
| |||||||
| In vitro fertilization | n = 3128 | n = 912 | |||||
| Expenditures for treatment visits | $7926 (16.3) | $24,793,807 | $1.42 | $5984 (12.3) | $5,457,145 | $0.25 | 5.6 |
| Expenditures for medication claims | $4748 (13.9) | $14,852,983 | $0.85 | $3782 (11.1) | $3,448,923 | $0.16 | 5.3 |
| Total expenditures for treatment | $12,664 (29.8) | $39,613,367 | $2.27 | $9791 (23.0) | $8,929,714 | $0.42 | 5.5 |
| Intrauterine insemination | n = 2488 | n = 1290 | |||||
| Expenditures for treatment visits | $2366 (10.2) | $5,886,175 | $0.34 | $1594 (6.9) | $2,055,861 | $0.10 | 3.5 |
| Expenditures for medication claims | $1486 (10.1) | $3,696,165 | $0.21 | $1066 (7.2) | $1,375,083 | $0.06 | 3.3 |
| Total expenditures for treatment | $3866 (19.4) | $9,618,451 | $0.55 | $2651 (13.3) | $3,419,262 | $0.16 | 3.5 |
| Ovulation-inducing medications | n = 4958 | n = 4331 | |||||
| Expenditures for treatment visits | $953 (4.3) | $4,724,684 | $0.27 | $711 (3.2) | $3,080,261 | $0.14 | 1.9 |
| Expenditures for medication claims | $871 (7.8) | $4,320,672 | $0.25 | $853 (7.6) | $3,694,987 | $0.17 | 1.4 |
| Total expenditures for treatment | $1830 (11.3) | $9,071,137 | $0.52 | $1515 (9.4) | $6,562,349 | $0.31 | 1.7 |
| All infertility treatments | n = 10,574 | n = 6533 | |||||
| Expenditures for treatment visits | $3092 (9.7) | $32,689,965 | $1.87 | $1863 (5.9) | $12,169,209 | $0.57 | 3.3 |
| Expenditures for medication claims | $2032 (9.2) | $21,491,158 | $1.23 | $1465 (6.6) | $9,573,948 | $0.45 | 2.8 |
| Total expenditures for treatment | $5115 (18.7) | $54,082,626 | $3.10 | $3320 (12.2) | $21,687,652 | $1.01 | 3.1 |
The total number of fully insured enrollees was 1,453,824 in mandate states and 1,790,541 in non-mandate states. P value < .05 for all comparisons between mandate and no mandate groups except for medication claims among those using ovulation-inducing medications only
SE standard error, PMPM per member per month
Adjusted for enrollee age and region of residence
PMPM expenditures for women living in mandate states divided by those for women living in states without a mandate
PMPM expenditures estimate the impact of the mandate on insurance plans and account for potential differences in enrollment between women living in mandate states and those living in non-mandate states. For all infertility treatments, there was a threefold difference in the PMPM expenditures ($3.10 vs. $1.01) associated with residency in a mandate state. The PMPM expenditures for IVF were 5.5 times higher for women living in a state with a mandate compared with women living in states without a mandate.
The average expenditures for infertility treatments per woman with a relevant claim were also higher for women covered by self-insured plans living in a state with a mandate compared with their counterparts living in states without a mandate (Table 3). The adjusted annual mean expenditures for IVF treatment for women living in the mandate states was $12,337 compared with $11,422 for women living in states without a mandate. The PMPM expenditures were 1.4 times as high for those living in mandate versus non-mandate states and the ratio did not differ considerably according to the type of treatment received. The ratio of PMPM expenditures for fully-insured versus self-insured plans varied by treatment intensity with the largest difference observed among women undergoing IVF (5.5 vs. 1.4). Average expenditures for infertility treatments per woman with a relevant claim were slightly higher for women living in a state with a comprehensive mandate compared with women living in a state with a limited mandate (16,508 vs. 13,874, respectively) (Table 4). No differences by mandate type were observed for women covered by self-insured plans.
Table 3.
Mean, aggregate and per member per month expenditures for infertility treatments among commercially insured women 19–45 years receiving reimbursement from a self-insured health plan, 2011
| Mandate |
No mandate |
Ratio of PMPM expendituresb | |||||
|---|---|---|---|---|---|---|---|
| Adjusteda mean expenditures (SE) | Aggregate expenditures | PMPM expenditures | Adjusteda mean expenditures (SE) | Aggregate expenditures | PMPM expenditures | ||
|
| |||||||
| In vitro fertilization | n = 3245 | n = 2570 | |||||
| Expenditures for treatment visits | $7545 (12.8) | $24,484,593 | $1.54 | $7000 (11.9) | $17,990,334 | $1.14 | 1.3 |
| Expenditures for medication claims | $4793 (8.3) | $15,553,090 | $0.98 | $4420 (7.7) | $11,358,683 | $0.72 | 1.4 |
| Total expenditures for treatment | $12,337 (19.9) | $40,034,019 | $2.52 | $11,422 (18.4) | $29,354,540 | $1.86 | 1.4 |
| Intrauterine insemination | n = 3406 | n = 2844 | |||||
| Expenditures for treatment visits | $2558 (10.2) | $8,714,074 | $0.55 | $2100 (8.4) | $5,971,851 | $0.38 | 1.4 |
| Expenditures for medication claims | $1731 (9.3) | $5,894,420 | $0.37 | $1298 (7.0) | $3,691,614 | $0.23 | 1.6 |
| Total expenditures for treatment | $4299 (18.1) | $14,641,788 | $0.92 | $3395 (14.3) | $9,655,033 | $0.61 | 1.5 |
| Ovulation-inducing medications | n = 6452 | n = 7564 | |||||
| Expenditures for treatment visits | $1334 (7.6) | $8,605,452 | $0.54 | $1183 (6.8) | $8,944,506 | $0.57 | 1.0 |
| Expenditures for medication claims | $1289 (7.7) | $8,314,673 | $0.52 | $1163 (7.0) | $8,799,489 | $0.56 | 0.9 |
| Total expenditures for treatment | $2627 (14.7) | $16,947,223 | $1.06 | $2327 (13.0) | $17,601,322 | $1.12 | 1.0 |
| All infertility treatments | n = 13,103 | n = 12,978 | |||||
| Expenditures for treatment visits | $3093 (7.6) | $40,533,934 | $2.55 | $2615 (6.5) | $33,942,103 | $2.15 | 1.2 |
| Expenditures for medication claims | $2200 (6.3) | $28,831,291 | $1.81 | $1898 (5.4) | $24,635,294 | $1.56 | 1.2 |
| Total expenditures for treatment | $5292 (13.6) | $69,347,523 | $4.36 | $4515 (11.6) | $58,591,089 | $3.72 | 1.2 |
Total number of self-insured enrollees was 1,326,428 in mandate states and 1,313,185 in non-mandate states. P value < .05 for all comparisons between mandate and no mandate groups
SE standard error, PMPM per member per month
Adjusted for enrollee age and region of residence
PMPM expenditures for women living in mandate states divided by those for women living in states without a mandate
Table 4.
Mean, aggregate and per member per month expenditures for in vitro fertilization among commercially insured women living in a state with a comprehensive or limited mandate to cover in vitro fertilization, 2011
| Comprehensive mandatea |
Limited mandateb |
Ratio of PMPM expendituresd | |||||
|---|---|---|---|---|---|---|---|
| Adjustedc mean expenditures (SE) | Aggregate expenditures | PMPM expendi tures | Adjustedc mean expenditures (SE) | Aggregate expenditures | PMPM expenditures | ||
|
| |||||||
| Fully-insured | n = 2064 | n = 256 | |||||
| Expenditures for infertility treatment visits | $8781 (8.5) | $18,123,899 | $3.96 | $9808 (9.5) | $2,510,881 | $3.04 | 1.3 |
| Expenditures for medication claims | $5091 (8.7) | $10,508,427 | $2.29 | $6801 (11.6) | $1,741,079 | $2.10 | 1.1 |
| Total expenditures for infertility treatment | $13,874 (14.1) | $28,635,709 | $6.25 | $16,508 (16.8)e | $4,225,971 | $5.11 | 1.2 |
| Self-insured | n = 897 | n = 264 | |||||
| Expenditures for infertility treatment visits | $8269 (17.2) | $7,417,420 | $2.27 | $9205 (19.1) | $2,429,996 | $2.07 | 1.1 |
| Expenditures for medication claims | $5230 (7.2) | $4,691,205 | $1.43 | $5119 (7.0) | $1,351,302 | $1.15 | 1.2 |
| Total expenditures for infertility treatment | $13,480 (21.0) | $12,091,991 | $3.70 | $14,369 (22.3) | $3,793,490 | $3.22 | 1.1 |
The total number of fully insured enrollees was 381,696 in comprehensive mandate states and 68,927 in limited mandate states. Total number of self-insured enrollees was 272,482 in comprehensive mandate states and 98,032 in limited mandate states
SE standard error, PMPM per member per month
Comprehensive mandate states defined as those covering at least 4 IVF cycles and included Illinois, Massachusetts, New Jersey, and Rhode Island
Limited mandate states defined as those covering less than 4 IVF cycles and included Arkansas, Connecticut, Hawaii, and Maryland
Adjusted for enrollee age and region of residence
PMPM expenditures for women living in states with a comprehensive mandate divided by per enrollee expenditures for women living in states with a limited mandate
P value < .05 for comparison between comprehensive and limited mandate groups
Among women undergoing any infertility treatment, the mean numbers of visits and medication claims were consistently higher for those living in states with a mandate versus those in states without a mandate, regardless of plan type. In addition, differences were more pronounced in the fully-insured group (Fig. 1).
Fig. 1.
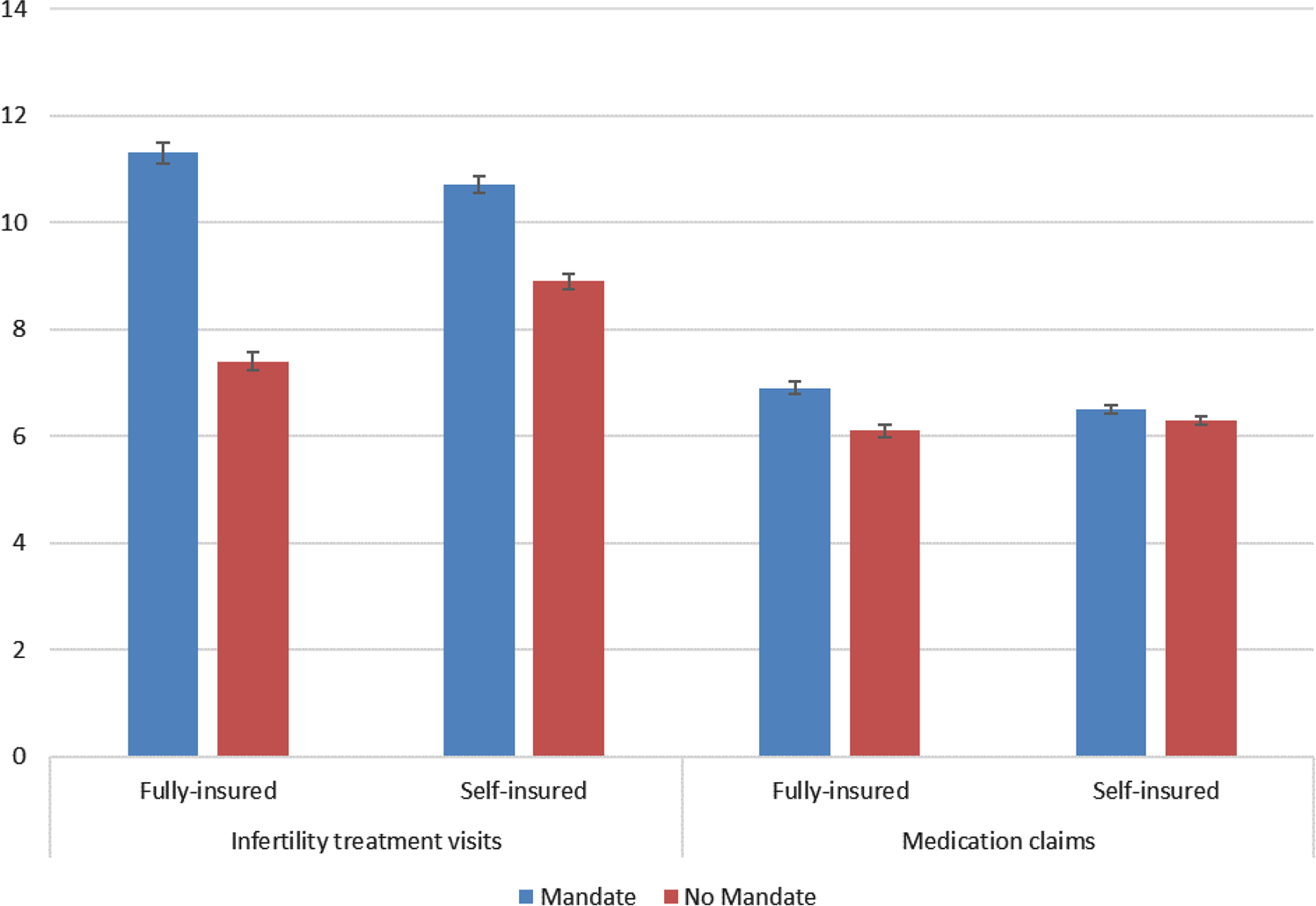
Mean number of visits and medication claims and 95% confidence intervals for all types of infertility treatments by health plan type, mandate versus non-mandate states. Wilcoxon rank sum P value < .01 for all comparisons between mandate and no mandate groups
Discussion
We found that infertility treatment expenditures per enrollee, particularly for IVF, were higher for women living in states with a mandate compared with those living in states without a mandate. This finding is consistent with other studies of the effect of mandates that used other types of data to assess expenditures on covered infertility services (Collins et al. 1995; Griffin and Panak 1998; Chambers et al. 2009; Katz et al. 2011; Wu et al. 2014). Similarly, we observed increased numbers of infertility treatment visits and medication claims for women living in mandate states compared with their counterparts in non-mandate states.
Our finding of larger differences in PMPM infertility treatment expenditures for fully-insured plans than for self-insured plans was as expected. However, this finding has not been previously reported because previous studies of state infertility mandates were not able to distinguish between women enrolled in self-insured versus fully-insured employer-sponsored health plans. This disparity was most pronounced for women undergoing IVF and likely reflects low levels of coverage for this treatment among fully-insured private health plans in the absence of a mandate. Although some observed differences in average expenditures overall between mandate and non-mandate states might be explained by variations in standards of care across states or other state-level factors, such factors would not be expected to result in differences in expenditures by type of plan.
Higher per-enrollee infertility treatment expenditures for self-insured employers in states with mandates could be either causal or artifactual. The latter could result from confounding by differences between states in the demand for infertility services leading to the adoption of mandates (Bitler and Schmidt 2012). For example, it is possible that a subset of self-insured employers in states with higher demand for infertility services might have voluntarily covered such services prior to the adoption of mandates and that those employers might not have opposed the adoption of mandates in those states. Insurance mandates could have a causal or spillover effect on expenditures by fully-insured plans for two reasons. First, self-insured plans that cover state employees may be required by states to pay for infertility treatments despite those plans not being subject to state regulation. This finding has been documented in a study of the impact of state autism services insurance mandates (Barry et al. 2017). That is technically not a spillover effect although it would appear as such in studies like ours that are unable to distinguish state employee plans from self-insured private employers. Second, some self-insured private employers in mandate states may opt to include coverage for infertility services in order to avoid complaints from employees.
In states with mandates to cover IVF, comprehensive mandates (those covering at least four IVF cycles) have been found to increase use of IVF while limited mandates have little or no effect (Henne and Bundorf 2008; Hamilton and McManus 2012). Although we were unable to evaluate access to IVF, we found that among women who used infertility treatments, the expenditures per enrollee did not differ substantially between states with comprehensive versus limited mandates for women enrolled in either fully-insured or self-insured plans. Thus, whereas per-enrollee expenditures were considerably higher for women living in mandate states compared with those living in non-mandate states, the type of mandate did not appear to influence IVF expenditures among women living in a state with a mandate.
The primary strength of our study is the use of a large sample of privately insured women with information on type of infertility treatments. However, our findings are subject to several limitations. The primary limitation of our study is that we were unable to account for state differences in factors that led to the adoption of mandates in some states and not others, differences which may confound our conclusions regarding mandate effects. That is because the mandates studied were adopted prior to the beginning of the claims data used in this analysis. Difference-in-difference statistical models using panel data typically use the change before and after a policy is adopted in some states with the same temporal period to control for confounding by differences between states. However, as noted previously, the heterogeneity of findings for fully-insured versus self-insured plans suggest that state characteristics do not fully explain our findings.
Another limitation is that we assessed infertility service use over a 12-month period, which may include multiple cycles of IVF, IUI and stimulation. Women may undergo multiple infertility treatments over a long period before achieving pregnancy; as such, our estimates do not reflect the total expenditures associated with a successful treatment outcome. Also, because we classified the groups according to highest level of treatment intensity, the IVF group included women who used both IVF and IUI, which accounted for 25.6% of the IVF group. In addition, because we only evaluated infertility treatments during a given calendar year, some degree of misclassification occurred if the treatment began in 1 year and continued into a subsequent year.
Furthermore, our expenditure estimates will likely understate actual expenditures because we could not accurately ascertain claims for procedures that were related to the infertility treatment but were not coded as an infertility visit (e.g. baseline ultrasound, blood collection, cervical dilation, or hysteroscopy). In addition, we could not evaluate donor IVF cycles as a distinct group. In our study donor cycles were either classified as IVF (if a transfer was reported) or as OI only (if the patient paid out of pocket for transfer); however, donor cycles are often excluded from coverage and would not be captured in the database. Likewise, treatments for same sex couples would largely be excluded from our analysis. Our analysis was limited to expenditures related to infertility treatment and did not consider costs associated with neonatal outcomes such as multiple birth that occur more frequently in women using infertility treatments than the general population. Finally, due to missing claims information for patients that paid out-of-pocket for treatment, our analysis was necessarily limited to payments by health plans and do not reflect total gross payments for infertility services including out-of-pocket spending.
Conclusions
Not surprisingly, we found that average health plan expenditures for infertility treatments were higher in states with insurance mandates to cover infertility treatments. What is new in this study is that expenditures were higher for both fully-insured and self-insured plans, although to a lesser extent for the latter. The presence of a mandate is positively associated with infertility coverage even for employers that self-insure although the latter may include state employee health plans that are subject to state insurance mandates. There could also be a spill-over effect of the mandates or to the higher expenditures for self-insured plans could reflect confounding by state differences in both mandates and standards of care. The bulk of recorded expenditures on infertility services in states with mandates were incurred by the fully-insured plans that were known to be subject to the state mandates.
Supplementary Material
Significance.
What is already known on this subject?
Use of infertility services is increased in states with an infertility insurance mandate compared with states without a mandate. Most self-insured employers are exempt from state insurance mandates whereas fully insured plans are subject to the mandate.
What this study adds?
For women enrolled in self-insured plans, infertility expenditures were 1.2 times higher for those living in states with versus without a mandate. In contrast, there was threefold difference for women enrolled in fully-insured plans, suggesting that these plans incur greater expenditures in the context of an insurance mandate.
Footnotes
Electronic supplementary material The online version of this article (https://doi.org/10.1007/s10995-018-2675-y) contains supplementary material, which is available to authorized users.
References
- Agency for Healthcare Research and Quality. (2011). Percent of private-sector enrollees that are enrolled in self-insured plans at establishments that offer health insurance by firm size and state: United States, 2011. Center for Financing, Access and Cost Trends. http://meps.ahrq.gov/mepsweb/data_stats/summ_tables/insr/state/series_2/2011/tiib2b1.pdf. Accessed 21 Dec 2018. [Google Scholar]
- Barry CL, Epstein AJ, Marcus SC, Kennedy-Hendricks A, Candon MK, Xie M, & Mandell DS (2017). Effects of state insurance mandates on health care use and spending for autism spectrum disorder. Health Affairs, 36(10), 1754–1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bitler MP, & Schmidt L (2012). Utilization of infertility treatments: The effects of insurance mandates. Demography, 49(1), 125–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambers GM, Sullivan EA, Ishihara O, Chapman MG, & Adamson GD (2009). The economic impact of assisted reproductive technology: A review of selected developed countries. Fertility and Sterility, 91(6), 2281–2294. [DOI] [PubMed] [Google Scholar]
- Chandra A, Copen CE, & Stephen EH (2013). Infertility and impaired fecundity in the United States, 1982–2010: Data from the National Survey of Family Growth. National Health Statistics Reports, 67, 1–18. [PubMed] [Google Scholar]
- Chandra A, Copen CE, & Stephen EH (2014). Infertility service use in the United States: Data from the National Survey of Family Growth, 1982–2010. National Health Statistics Reports, 73, 1–21. [PubMed] [Google Scholar]
- Collins JA, Bustillo M, Visscher RD, & Lawrence LD (1995). An estimate of the cost of in vitro fertilization services in the United States in 1995. Fertility and Sterility, 64(3), 538–545. [DOI] [PubMed] [Google Scholar]
- Griffin M, & Panak WF (1998). The economic cost of infertility-related services: An examination of the Massachusetts infertility insurance mandate. Fertility and Sterility, 70(1), 22–29. [DOI] [PubMed] [Google Scholar]
- Hamilton BH, & McManus B (2012). The effects of insurance mandates on choices and outcomes in infertility treatment markets. Health Economics, 21(8), 994–1016. [DOI] [PubMed] [Google Scholar]
- Henne MB, & Bundorf MK (2008). Insurance mandates and trends in infertility treatments. Fertility and Sterility, 89(1), 66–73. [DOI] [PubMed] [Google Scholar]
- Jensen GA, & Morrisey MA (1999). Employer-sponsored health insurance and mandated benefit laws. The Milbank Quarterly, 77(4), 425–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston J, Gusmano MK, & Patrizio P (2014). Preterm births, multiples, and fertility treatment: Recommendations for changes to policy and clinical practices. Fertility and Sterility, 102(1), 36–39. [DOI] [PubMed] [Google Scholar]
- Katz P, Showstack J, Smith JF, Nachtigall RD, Millstein SG, Wing H, … Adler N (2011). Costs of infertility treatment: Results from an 18-month prospective cohort study. Fertility and Sterility, 95(3), 915–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin JR, Bromer JG, Sakkas D, & Patrizio P (2011). Insurance coverage and in vitro fertilization outcomes: A U.S. perspective. Fertility and Sterility, 95(3), 964–969. [DOI] [PubMed] [Google Scholar]
- Mercer Health and Benefits LLC. (2006). Employer experience with, and attitudes toward, coverage of infertility treatment. Accessed August 28, 2018, from https://resolve.org/wp-content/uploads/2017/09/Mercer_-_Resolve_Final_Report.pdf. [Google Scholar]
- Neumann PJ (1997). Should health insurance cover IVF? Issues and options. Journal of Health Politics, Policy and Law, 22(5), 1215–1239. [DOI] [PubMed] [Google Scholar]
- Thoma ME, McLain AC, Louis JF, King RB, Trumble AC, Sundaram R, & Louis GMB (2013). Prevalence of infertility in the United States as estimated by the current duration approach and a traditional constructed approach. Fertility and Sterility, 99(5), 1324–1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu AK, Odisho AY, Washington SL 3rd, Katz PP, & Smith JF (2014). Out-of-pocket fertility patient expense: Data from a multicenter prospective infertility cohort. The Journal of Urology, 191(2), 427–432. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


