Tumour necrosis factor (TNF)αa is thought to play a central role in promoting and perpetuating inflammation in sarcoidosis, and treatment with TNF-α inhibitors has been reported to be successful.1-3 We present a patient with quiescent sarcoidosis who relapsed shortly after beginning treatment with a TNF-α inhibitor for an unrelated medical condition.
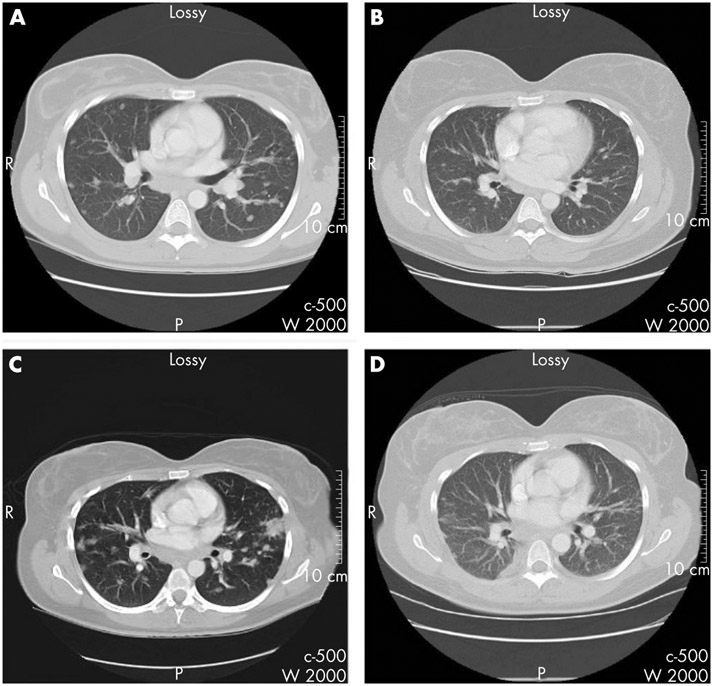
A 35-year-old woman with a history of sarcoidosis, in remission while on no treatment, and ankylosing spondylitis experienced a severe flare of inflammatory back pain that was not responsive to non-steroidal anti-inflammatory drugs. Treatment with etanercept 50 mg subcutaneously weekly was begun with marked symptomatic improvement in her back pain. Three weeks after starting etanercept, she developed dry cough, exertional dyspnoea, blurred vision with photopsia of the right eye, fatigue and fevers to 38.9°C. Etanercept was discontinued. Computed tomography of the chest showed extensive pulmonary nodules, peripherally based infiltrates, and paratracheal, subcarinal, mediastinal and bilateral hilar lymphadenopathy. Bronchoscopy revealed highly friable bronchial mucosa with scattered endobronchial nodular granulomas. Cultures of bronchoalveolar lavage fluid and lung tissue were negative. Lung biopsy demonstrated non-necrotising granulomas consistent with sarcoidosis. Treatment with prednisone 0.5 mg/kg per day and prednisolone acetate 1% ophthalmic solution resulted in prompt resolution of her anterior uveitis, respiratory and constitutional symptoms. Follow-up computed tomography scan of the chest 3 months later showed improvement (fig 1). One year after relapse of sarcoidosis, she remains in clinical remission on tapering doses of prednisone.
Figure 1.
Chest computed tomography scans. (A) Initial presentation of sarcoidosis. (B) Asymptomatic after months of treatment with corticosteroids. (C) Relapse of sarcoidosis after exposure to etanercept. (D) Resolution after discontinuation of etanercept and treatment with corticosteroids.
Contrary to previously reported cases of successful treatment of active sarcoidosis with TNF-α inhibitors, our patient experienced relapse of sarcoidosis 3 weeks after initiating etanercept to treat active ankylosing spondylitis. She had prompt clinical and radiographic improvement after discontinuation of etanercept and treatment with corticosteroids. This case adds to a few recent reports of the development of sarcoidosis after treatment with TNF-α inhibitors.4-6 Recent clinical trials of TNF-α inhibitors for the treatment of sarcoidosis have reported mixed results. Infliximab resulted in 2.5% improvement in forced vital capacity at 24 weeks, although there was no clinical improvement.7 Etanercept failed to improve sarcoidosis in 11 of 17 patients examined over 12 months.8 By evaluating only patients with active sarcoidosis, these studies were not able to observe worsening of quiescent disease upon treatment with TNF-α inhibitors.
Granuloma formation in sarcoidosis begins with a T cell and macrophage-mediated response to an unknown stimulus.9 Activated CD4+ T cells generate interleukin-2 and interferon (IFN)-γ, which result in recruitment of mononuclear cells to the alveoli. TNF-γ, secreted by activated macrophages and present in high concentrations in bronchoalveolar fluid of patients with active sarcoidosis, is believed to promote the formation of granuloma. Inhibition of TNF-α in our patient resulted in relapse of quiescent disease, suggesting the hypothesis that TNF-α functions to contain active inflammation in sarcoidosis, rather than itself being the primary pathogenic mediator. Case reports suggest that sarcoidosis can develop after IFN-α treatment.10 The ability of IFN-α to stimulate IFN-γ production by activated CD4+ T cells suggests that IFN-γ may be the primary pathogenic cytokine. Treatment of our patient with etanercept may have derepressed this system, resulting in a relapse of sarcoidosis in a manner analogous to the activation of latent tuberculosis observed in patients treated with TNF-α inhibitors.11
Acknowledgements:
We thank Dr John O’Shea for reviewing the manuscript.
Funding:
Supported by the Intramural Research Program of the National Institute of Arthritis and Musculoskeletal and Skin Diseases at the National Institutes of Health.
Footnotes
Competing interests: None.
Patient consent: Informed consent has been obtained for the publication of the details in this report.
REFERENCES
- 1.Baughman RP, Lower EE, du Bois RM. Sarcoidosis. Lancet 2003;361:1111–18. [DOI] [PubMed] [Google Scholar]
- 2.Yee AMF, Pochapin MB. Treatment of complicated sarcoidosis with infliximab antitumor necrosis factor-α therapy. Ann Intern Med 2001;135:27–31. [DOI] [PubMed] [Google Scholar]
- 3.Pritchard C, Nadarajah K. Tumour necrosis factor α inhibitor treatment for sarcoidosis refractory to conventional treatments: a report of five patients. Ann Rheum Dis 2004;63:318–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gonzalez-Lopez MA, Blanco R, Gonzalez-Vela MC, Fernandez-Llaca H, Rodriguez-Valverde V. Development of sarcoidosis during etanercept therapy. Arthritis Rheum 2006;55:817–20. [DOI] [PubMed] [Google Scholar]
- 5.Verschueren K, Van Essche E, Verschueren P, Taelman V, Westhovens R. Development of sarcoidosis in etanercept-treated rheumatoid arthritis patients. Clin Rheumatol 2007;26:1969–71. [DOI] [PubMed] [Google Scholar]
- 6.O’Shea FD, Marras TK, Inman RD. Pulmonary sarcoidosis developing during infliximab therapy. Arthritis Rheum 2006;55:978–81. [DOI] [PubMed] [Google Scholar]
- 7.Baughman RP, Drent M, Kavuru M, Judson MA, Costabel U, du Bois R, et al. Infliximab therapy in patients with chronic sarcoidosis and pulmonary involvement. Am J Respir Crit Care Med 2006;174:795–802. [DOI] [PubMed] [Google Scholar]
- 8.Utz JP, Limper AH, Kalra S, Specks U, Scott JP, Vuk-Pavlovic Z, Schroeder DR. Etanercept for the treatment of stage II and III progressive pulmonary sarcoidosis. Chest 2003;124:177–85. [DOI] [PubMed] [Google Scholar]
- 9.Ziegenhagen MW, Muller-Quernheim J. The cytokine network in sarcoidosis and its clinical relevance. J Intern Med 2003;253:18–30. [DOI] [PubMed] [Google Scholar]
- 10.Doyle MK, Berggren R, Magnus JH. Interferon-induced sarcoidosis. J Clin Rheumatol 2006;12:241–8. [DOI] [PubMed] [Google Scholar]
- 11.Winthrop KL, Siegel JN, Jereb J, Taylor Z, Iademarco MF. Tuberculosis associated with therapy against tumor necrosis factor alpha. Arthritis Rheum 2005;52:2968–74. [DOI] [PubMed] [Google Scholar]