Abstract
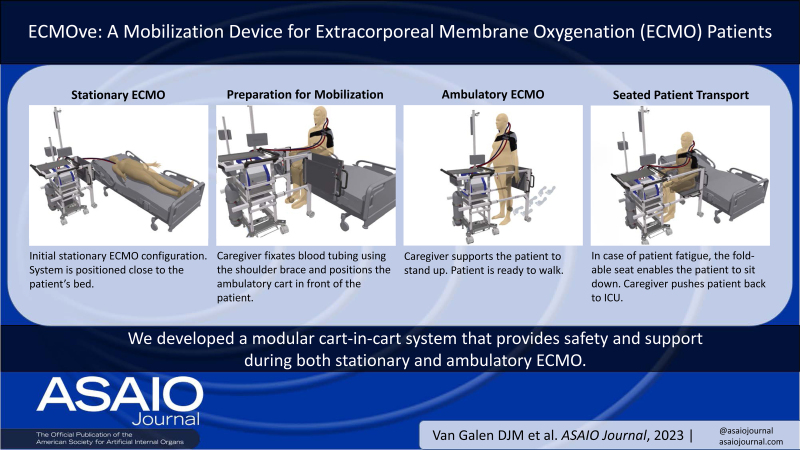
Extracorporeal membrane oxygenation (ECMO) is a temporary lifesaving treatment for critically ill patients with severe respiratory or cardiac failure. Studies demonstrated the feasibility of in-hospital mobilizing during and after ECMO treatment preventing neuromuscular weakness and impaired physical functioning. Despite more compact mobile ECMO devices, implementation of ambulatory ECMO remains labor-intensive, complex, and challenging. It requires a large multidisciplinary team to carry equipment, monitor and physically support the patient, and to provide a back-up wheelchair in case of fatigue. Moreover, there is no adequate solution to ensure the stability of the patient’s cannula and circuit management during ambulation. We developed a system contributing to improvement and innovation of current ambulatory ECMO patient programs. Our modular cart-in-cart system carries necessary ECMO equipment, features an extendable walking frame, and contains a folding seat for patient transport. An adjustable shoulder brace with lockable tubing-connectors enables safe fixation of the blood tubing. ECMOve provides safety, support, and accessibility while performing ambulatory ECMO for both patient and caregiver. Prototype evaluation in a simulated intensive care unit showed feasibility of our design, but needs to be evaluated in clinical care.
Keywords: patient mobility, early mobilization, rehabilitation, awake ECMO, physical therapy modalities, patient safety, intensive care unit
Extracorporeal membrane oxygenation (ECMO) is a temporary lifesaving treatment for critically ill patients suffering from severe respiratory or cardiac failure.1,2 Over the past years, a paradigm shift has taken place from keeping intensive care unit (ICU) patients under deep sedation and immobilization toward participation and mobilized patients.3 Awake ECMO treatment may avoid the use of heavy long-term sedation required for mechanical ventilation. This strategy prevents prolonged mechanical ventilation and associated complications including delirium and longer stay in ICU.4,5 Extracorporeal membrane oxygenation use without mechanical ventilation allows for active patient rehabilitation and is associated with improved patient survival rates compared to mechanical ventilation-based bridging strategies.6
Physical therapy during ICU stay of critically ill patients has been shown to be safe and effective in preventing neuromuscular weakness and impaired physical functioning.7–10 Subsequently, active rehabilitation during ECMO progressed toward studies showing the feasibility and safety of early mobilization in ECMO patients,11–18 and is in line with active in-hospital mobilization strategies after cardiac surgery.19 A positive response to early mobilization during ECMO has been associated with improved clinical outcomes such as lower mortality, decreased length of hospital stay, and improved level of independence after hospital discharge.11,20–23 These improved patient outcomes may lead to lower hospital costs compared to nonambulatory ECMO.23 New technologies and innovations have led to more compact ECMO devices with increased mobility.24,25 Despite these improvements, ambulatory ECMO remains labor-intensive, challenging, and risky. A highly trained multidisciplinary team is needed.26 Patient fall incidents, cannula-related complications, and fatigue are serious risks and may result in life-threatening situations.7,15–18,27–29 These conditions may prevent ICUs, especially low-volume centers, from using ambulatory ECMO.22 A compilation of ambulatory ECMO videos reveals the aforementioned challenges that need to be addressed.30 Indeed, adequate solutions for safety and stability of patient’s cannula and circuit management are lacking. Additionally, multiple not strictly necessary devices (eg, heater-cooler unit) are transported during mobilization, which further complicates the situation.
We designed and developed ECMOve: a modular system for improvement of current ambulatory ECMO patient programs. This system provides safety, support, and accessibility while performing ambulatory veno-venous (VV) ECMO for both patient and caregiver.
Materials and Methods
Extracorporeal membrane oxygenation mobilization support system development was performed according to the V-model.31 For each module, detailed user requirements were defined to develop a system that complies with the user’s needs. Actual ECMO patients were not involved in the design process. Instead, scientific publications and openly available online video content were used to determine the limitations and needs of current ambulatory ECMO practice.26,30 Unstructured, multiperspective feedback was collected and integrated throughout the development process, including feedback from the ASAIO community.32 A risk analysis was performed to identify risks for both patient and caregiver. Where necessary, countermeasures to minimize the probability of occurrence were defined and translated into additional design requirements.
Video 1.
General Requirements
User requirements were defined based on the limitations of current clinical ambulatory ECMO care. This design focuses on adult ICU patients receiving VV-ECMO support through a dual lumen cannula placed in the jugular vein and receive ambulation by walking. Extracorporeal membrane oxygenation treatment was classified into two treatment situations: stationary (bed-bound) and ambulatory (walking) ECMO.
Six key user requirements were defined at the start of the project to set the scope for the design process. A component to provide:
Transport of ECMO equipment necessary for both stationary and ambulatory situations. This equipment includes ECMO device (eg, Cardiohelp, CARL, Mobybox, etc.), oxygen cylinder, emergency drive unit, emergency kit, perfusor pump(s), and drip(s).
Transport of ECMO equipment only necessary for stationary situation. This equipment includes gas blender, flow meter, and heater-cooler unit.
Physical patient support during walking and in case of sudden events such as patient fatigue or unexpected hemodynamic instability.
Safety and stability of the patient’s cannula and circuit management during ambulatory ECMO.
Easy switching between wall-mounted gas and bottled gas.
Easy attachment and detachment of devices needed for stationary ECMO.
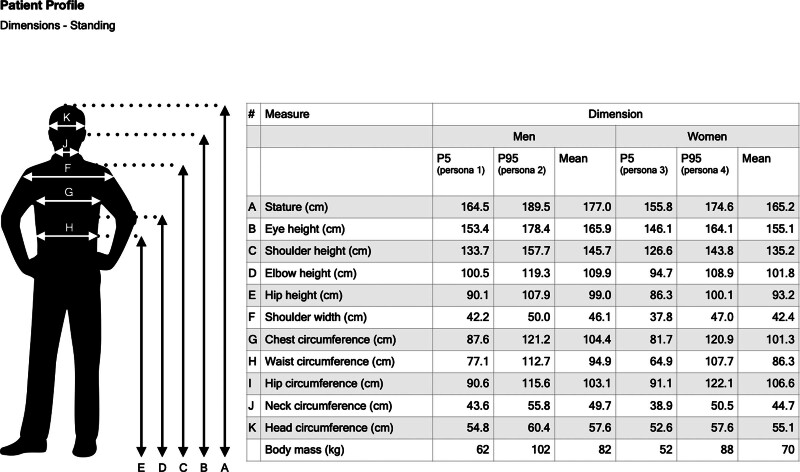
Patient-Centered Requirements
To design a patient-centered system suitable for a wide range of patients, anthropometric data were used to create four different personas. Anthropometric data were collected using the DINED anthropometric database of Technical University (TU) Delft.33 Measures were based on a Dutch population with an age of 31–60 years. Two male and two female profiles were generated. For both genders, anthropometric data for the P5 (5th percentile) and P95 (95th percentile) were defined (Figure 1). This resulted in a small and a large patient profile for both genders. Multiple body measures were considered to generate a three-dimensional (3D) computer-aided design (CAD) profile for each persona and were used to further define the design requirements of the system.
Figure 1.
Creation of four personas for patient profiling through anthropometric data analysis. Anthropometric data were sourced from the TU Delft DINED database, covering human measurements from Dutch adults. The data, depicting the 90% range (5th–95th percentile), pertains to individuals aged 31–60 years and is visualized in the left panel. TU, Technical University.
User requirements for patient types were established based on the profile data generated. The main user requirements regarding patient type include that the product shall be designed for patients with a weight of 52–102 kg, height of 156–190 cm, and chest circumference of 82–121 cm.
System Design
The developed system was divided into six modules. Each module solves a specific problem originating from the corresponding key user requirement. Morphological schemes were used for preconcept generation of the modules. Each preconcept was evaluated by weighing its pros and cons without using a dedicated scoring system. Thereafter, one concept was selected for further development. Subsequently, two-dimensional (2D) sketches of the chosen preconcept were elaborated and transformed into 3D models using Shapr3D for MacOS (Shapr3D Zrt., Budapest, Hungary). Multiple design iterations were performed to generate the final design of each module. All 3D model designs were optimized for prototype assembly. Only the final module designs are elaborated in this article.
Prototype Fabrication
The ECMOve prototype was built by combining prefabricated components with custom-made parts. Custom-made sheet materials were obtained with laser cutting 3 mm thick steel, 6 mm high-pressure laminate, and 12 mm plywood. Other custom parts were fabricated with selective laser sintering.
Design Verification
Prototype verification was performed in a simulated ICU environment at TechMed Simulation Centre (University of Twente, Enschede, the Netherlands). Usability and functionality of the ECMOve were assessed for use in a clinical setting. Multiple user scenarios were simulated using voluntary healthy subjects (n = 5, written consent given) with varying body profiles (weight: 50–88 kg, body height: 162–189 cm, chest circumference: 80–98 cm) to check for suitability across a wide range of patients. The use of a Cardiohelp ECMO system (Getinge AB, Rastatt, Germany), and a heater-cooler device (HICO-Aquatherm 660; pfm medical hico GmbH, Köln, Germany) enabled realistic simulation testing.
Results
Final Concept
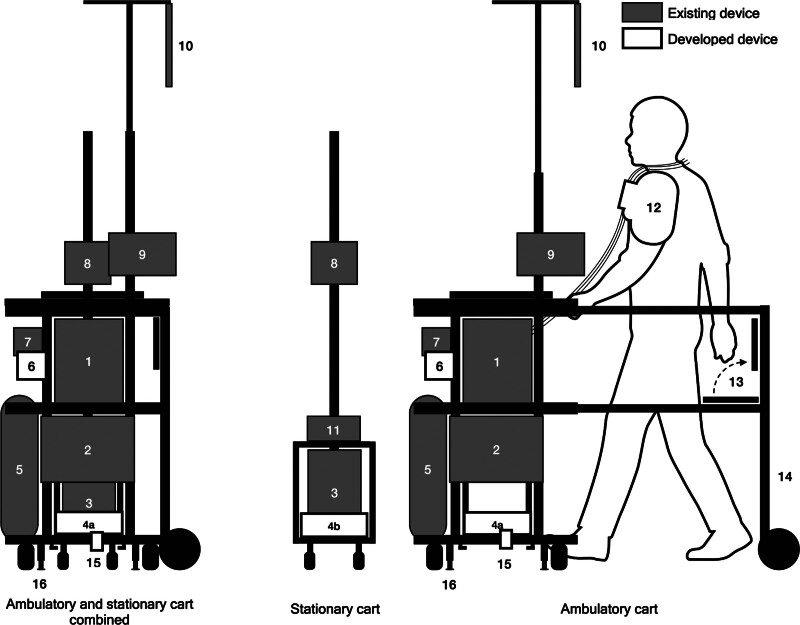
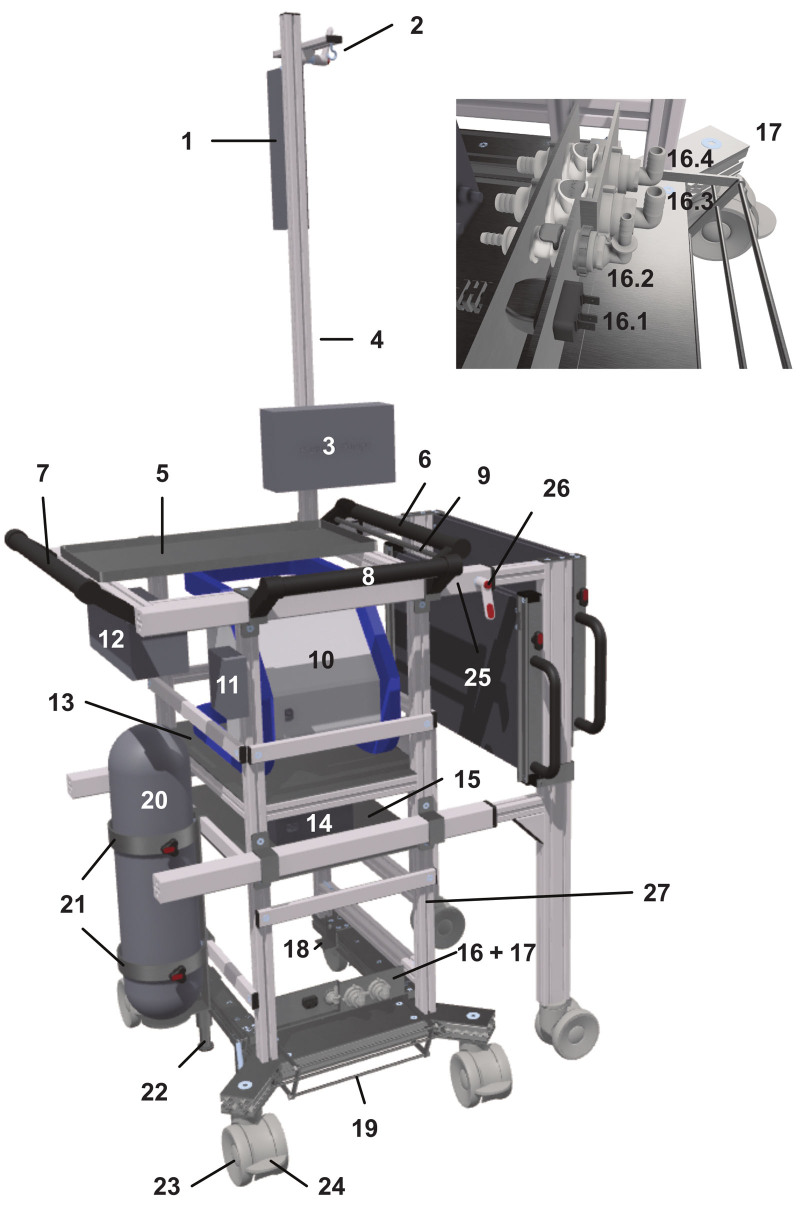
The final concept of ECMOve as depicted in Figure 2 comprises a modular cart-in-cart system consisting of two distinct carts—a stationary cart and the ambulatory cart. The stationary cart carries devices not required during ambulation and remains in the ICU next to the patient’s bed. The ambulatory cart carries all necessary devices during ambulation and features an extendable walking frame (Figure 2, component 14) that ensures safe walking support for the patient. The foldable seat (13) allows the patient to sit and facilitates transport back to the ICU in case of patient fatigue or in-hospital transport. A safety brake system (16) prevents unintentional movement of the ambulatory cart. Devices on both carts can be (dis)connected through a multi-connector hub (4a, 4b), enabling easy configuration of necessary fluids (tempered water from heater-cooler unit), gases, and electricity. A connection between the stationary and ambulatory cart is maintained by a pedal-controlled lift mechanism (15) that prevents accidental disconnection of the multi-connector and enables transport of both carts simultaneously. The system also features a gas switch (6) that allows for convenient switching between wall-mounted gas and bottled gas. A prefabricated universal shoulder brace (12) (Bracefox, Breda, the Netherlands) combined with an integrated blood tubing connector that can be adjusted to the patient via Velcro closure, facilitates secure fixation of the blood tubing, and minimizes strain on the cannula.
Figure 2.
Final concept of the developed ECMOve system comprising an ECMO device (1), emergency kit (2), heater-cooler unit (3), multi-connector—ambulatory part (4a), multi-connector—stationary part (4b), oxygen bottle (5), gas splitter (6), emergency drive for blood pump (7), gas blender and flow meter (8), perfusor pump(s) (9), drip(s) (10), power hub (11), blood tubing and cannula fixation device (12), folding seat (13), walking frame (14), foot pedal for actuation of lift mechanism (15), and (de)braking safety system (16). ECMO, extracorporeal membrane oxygenation.
Module Specification
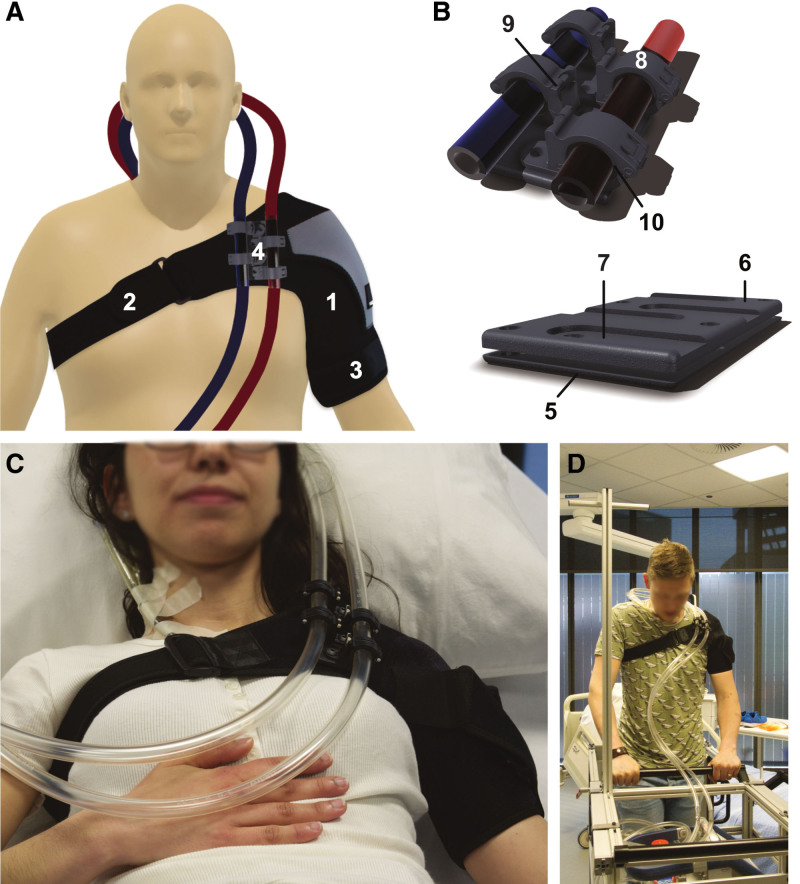
Module A—blood tubing fixation module
The aim of the blood tubing fixation module is to provide safety and stability of patient’s cannula and tubing management during ambulatory ECMO. The resulting concept design is depicted in Figure 3.
Figure 3.
Design of the blood tubing fixation module (A and B) providing safety and stability of the patient’s cannula and tubing management. The blood tubing fixation module comprises a (1) universal shoulder brace, (2) adjustable Velcro chest closure, (3) adjustable Velcro upper arm closure, (4) blood tubing connector, (5) bottom plate, (6) base plate, (7) countersink for tubing clamp mounting, (8) blood tubing clamp—two per tube, (9) locking pin, (10) antislip rings—two per clamp. Simulated ECMO patients wearing the prototype during lying in bed (C), walking with the ambulatory cart (D). Permission was obtained for use of this photograph for publication. ECMO, extracorporeal membrane oxygenation.
Module B—ambulatory device transport module
The aim of the ambulatory device transport module is to provide transport of devices necessary in both stationary and ambulatory conditions. The design of the ambulatory device transport module is shown in Figure 4.
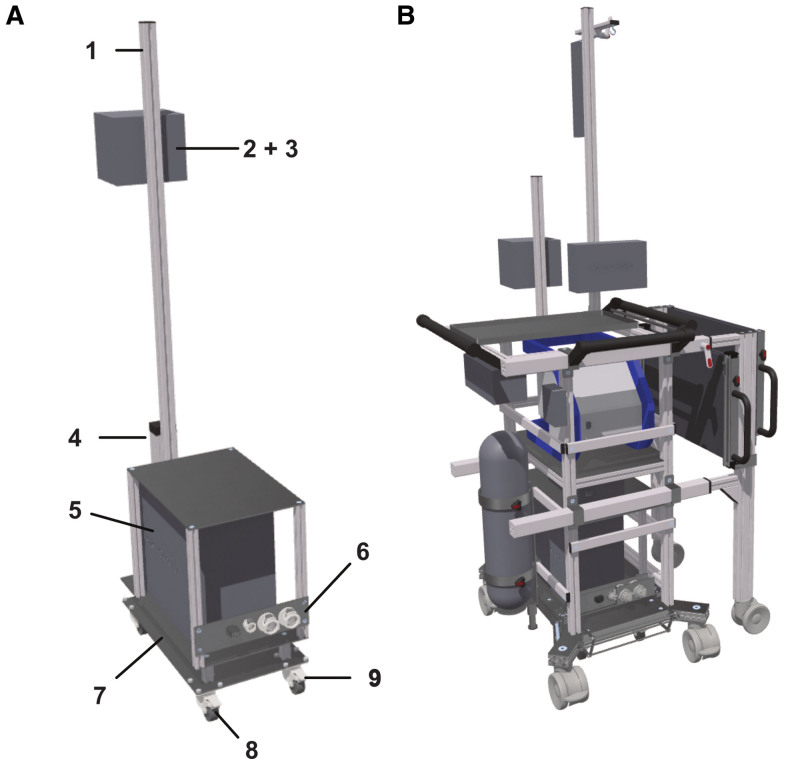
Figure 4.
Design of ambulatory device transport module providing transport of devices necessary in both stationary and ambulatory conditions. This module comprises a (1) drip, (2) drip connection pole, (3) perfusor pump(s), (4) perfusor pump connection pole, (5) tray for additional accessories, (6) patient pushing handle, (7) main pushing handle for caregiver, (8) side handle for caregiver, (9) (de)braking handles, (10) ECMO device, (11) gas splitter (module e), (12) emergency drive for blood pump, (13) tray for ECMO device placement, (14) power hub, (15) tray for power hub, (16) ambulatory hub plate mounting all ambulatory connectors containing: (16.1) electricity connector, (16.2) gas connector, (16.3) water connectors (inlet) for heater-cooler unit inlet/outlet, (16.4) water connector (outlet) for heater-cooler unit, (17) multi-connector hub (module f, stationary and ambulatory hub part), (18) lift mechanism for secure device connection, (19) foot pedal for lift mechanism actuation, (20) oxygen bottle, (21) oxygen bottle holder, (22) (de)braking safety system, (23) swiveling wheels, (24) parking brake, (25) extendable frame of patient support module, (26) handle for (un)locking the extendable frame, (27) main ambulatory cart frame. ECMO, extracorporeal membrane oxygenation.
Module C—stationary device transport module
The aim of the stationary device transport module is to provide transport of devices only necessary in stationary conditions. Figure 5 shows the design of the stationary device transport module.
Figure 5.
Design of stationary device transport module (A) providing transport of devices only necessary in stationary conditions, and ambulatory ECMO cart combined with the stationary cart as used in stationary ECMO conditions (B). The stationary device transport module comprises a (1) connection pole for gas blender, flow meter, and multiple socket outlet, (2) gas blender, (3) flow meter, (4) multiple socket outlet, (5) heater-cooler unit, (6) stationary hub plate containing electricity connector, gas connector, and water connectors (inlet/outlet) for heater-cooler unit, (7) double bottom for cable and line organization, (8) swiveling wheels, and (9) parking brake. ECMO, extracorporeal membrane oxygenation.
Module D—patient support module
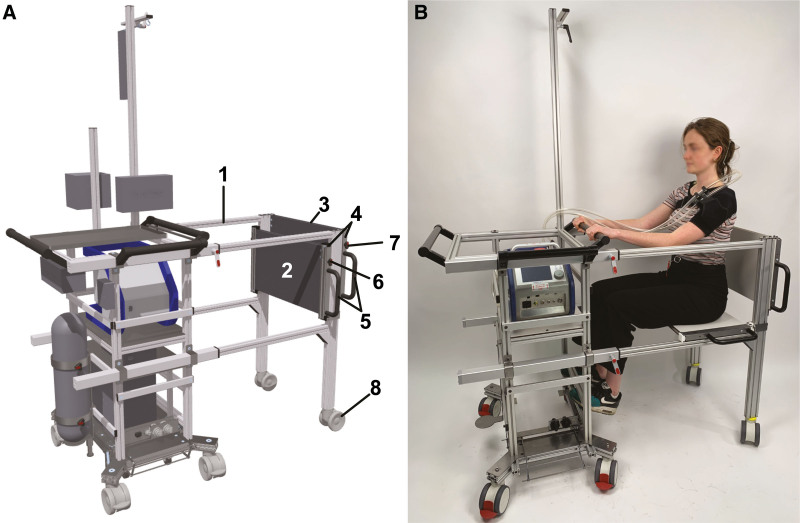
The aim of the patient support module is to provide physical patient support during walking and in case of sudden events such as patient fatigue or unexpected hemodynamic instability. The design of the patient support module is shown in Figure 6.
Figure 6.
Design of patient support module providing physical patient support during walking (A) and the prototype demonstrating sitting support (B) for sudden events such as patient fatigue or hemodynamic instability. The patient support module comprises a (1) extendable walking frame surrounding the patient for safe and unobstructed walking support, (2) folding seat facilitating seated patient transport, (3) backrest, (4) sliding opening/closing mechanism for seat and backrest, (5) handgrips, (6) seat locking mechanism, (7) backrest locking mechanism, and (8) swiveling wheels. Permission was obtained for use of this photograph for publication.
Module E—gas splitter
The aim of the gas splitter is to provide easy switching between wall-mounted gas and bottled gas.
The proposed concept involves a gas splitter consisting of two inlets and one outlet. One of the inlets is intended for the oxygen cylinder. The oxygen flow needs to be regulated using a medical flow regulator before it enters the gas splitter inlet. The other inlet is meant for the wall gas mixture. The outlet of the gas splitter is connected to the gas inlet of the oxygenator. The gas splitter must be capable of switching between the two inlets, necessitating the incorporation of a change-over valve. Moreover, when one inlet is in use, the other inlet must be blocked. The change-over valve can be implemented using either a solenoid valve or a mechanical mechanism. A conceptual artwork and further information on this concept can be found in Supplement A, Supplemental Digital Content, http://links.lww.com/ASAIO/B213.
Module F—multi-connector hub
The aim of the multi-connector hub is to provide easy attachment and detachment of devices needed for stationary ECMO.
To facilitate easy configuration of necessary fluids, gases, and electricity between devices required for stationary ECMO a multi-connector hub was designed as depicted in Figure 4. This hub comprises two parts: a stationary part and an ambulatory part. In stationary conditions, the two parts must be connected to each other, whereas in ambulatory conditions, they must be disconnected. Both the stationary and ambulatory hub parts consist of a plate in which the necessary valved connectors are mounted. These connectors are valved to prevent leakage when disconnected.
When the two carts are pushed together, the connectors of both hub parts will slide into each other and connect. A lifting mechanism lifts the stationary cart to ensure no positional displacement between the stationary and ambulatory connectors.
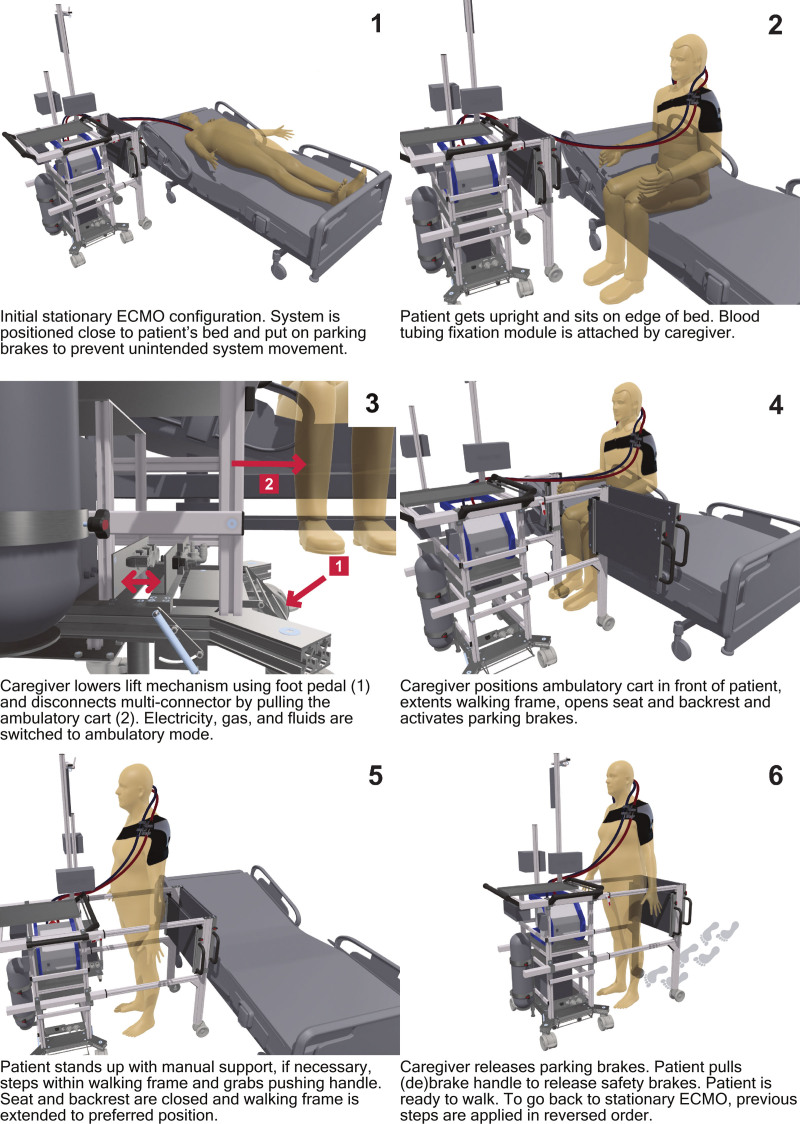
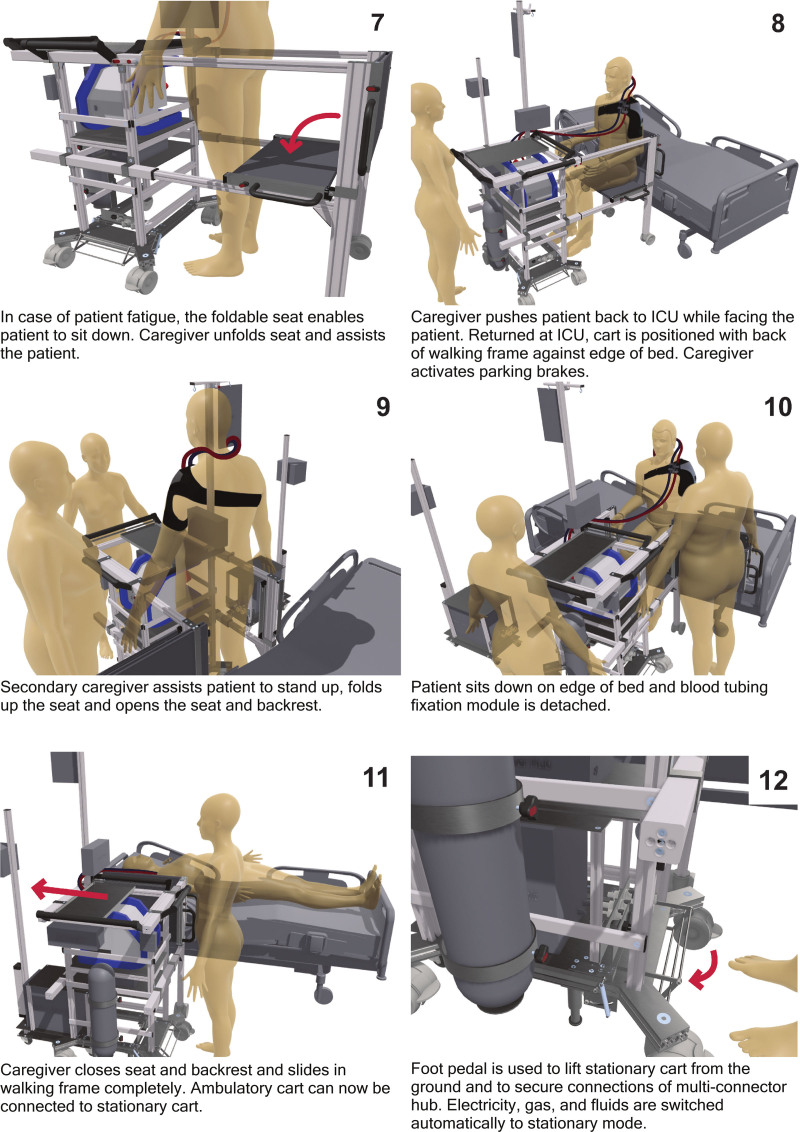
ECMOve Patient Scenario
To describe the intended use of the system, a user scenario of an ICU patient on ECMO has been described (Figures 7 and 8).
Figure 7.
Product user scenario, part 1.
Figure 8.
Product user scenario, part 2.
Design Verification at Simulated Intensive Care Unit Environment
During ambulation, the shoulder brace and blood tubing connector remained in position. The shoulder brace was successfully tested on both a large man and a small woman. Simulation tests show that the ambulatory cart moves smoothly on flat hospital floors, with little force required to initiate movement. The cart’s maneuverability is enhanced by its ability to move sideways, allowing for easy positioning in all directions. Applying the wheel brakes is simple and necessary to prevent the cart from moving when the patient uses it to stand up. The current height of the pushing handle is suitable for taller patients, but should be redesigned for a broader scope of patients. During testing, it was confirmed that the cart remains stable and does not tilt when the patient applies full body weight to the pushing handle. Additionally, attaching of different equipment to the cart and lifting the ECMO machine in and out of the cart was also successfully performed by a large man and a small woman. A video of prototype testing is available in Supplement B, Supplemental Digital Content.
Discussion
The aim of this study was to develop a system that contributes to the improvement of current ambulatory ECMO. A proof of concept was developed and tested in a simulated ICU environment. Most of the user requirements (4/6) were met during verification testing.
Cannula and Tubing Management
The simulation tests suggest that the shoulder brace is a convenient tool for safely attaching blood tubing to patients, as it can be easily attached to a supine patient by a single caregiver. The double strain relief of the blood tubing connector prevents the cannula from any tension even when strong forces are applied on the tubing between the blood tubing connector and the oxygenator. Although the shoulder brace was safely used for both patient profiles, a smaller version would be more comfortable and better suited for smaller patients. To define the ideal position for the blood tubing connector, a Velcro connection between the connector and the shoulder brace is being used. In a future prototype, it is recommended to fixate the blood tubing connector on the shoulder brace to prevent accidental disconnection. However, an additional securing of the cannula itself to the patient might still be necessary to overcome the stiffness of the cannula and the tubing between the canulation site and our blood tubing connector.
If the patient wears the shoulder brace while lying in bed, tubing behind the head of the patient could lead to decubitus. Therefore, it is important that the blood tubing is positioned above the patient’s head when the shoulder brace is used in stationary conditions. This still fixates the blood tubing, but prevents friction behind the head of the patient. The tubing length between the cannulation site and the blood tubing fixation module can be adjusted accordingly by opening and (re)closing the blood tubing fixation clamps.
Equipment Transport
The stationary cart easily moves in all directions when the ambulatory cart is detached. The pole attached to the back of the stationary cart allows for placement of multiple devices required in stationary conditions (eg, gas blender, flow meter, etc.). The ambulatory cart successfully detaches from the stationary cart by lowering the lift mechanism using the foot pedal. It is recommended to increase the diameter of the foot pedal axes for more stability and durability. The lift mechanism lifts the stationary cart just enough to minimize the contact of the stationary cartwheels with the ground. A slight enlargement of several components would provide more lifting height, eliminating the likelihood of accidental ground contact due to uneven ground.
The movement of the stationary and ambulatory cart together works as intended, allowing for easy transport of both carts including all devices. To demonstrate the (de-)coupling of connectors between the stationary and ambulatory hub, nonfunctional 3D printed connectors were used. Although the positioning of both hub parts is successfully demonstrated, the hub system requires redesign and optimization to enable simultaneous mechanical (un-)locking of electricity, gas, and water connectors. A functional prototype of the gas splitter was not produced. The risk analysis indicated that a solenoid-based solution may be prone to errors. Therefore, a mechanically actuated switch is recommended and gas supply safety must be well monitored and equipped with a safety alarm.
Clamps can be used to provide a neat solution for blood tubing management on the ambulatory cart. The same clamps used on the shoulder brace could be used. During testing, the height of the ECMO device tray was raised for better visibility of the device’s display during ambulation and easier placement of the ECMO device. Locking pins would secure the ECMO device in a predefined position allowing for better access to the ECMO device and lowering the risk of tube kinking when placing the device on the cart. Additionally, this will create space for an extra support tray or a storage drawer. Ninety degrees quick-couplings should be used to prevent kinking in the water lines of the oxygenator. The accessory holder at the back of the cart should be repositioned to allow easier removal of the oxygenator from the ECMO device. However, in case of device failure, oxygenator and pump can be removed and attached to a manual pump drive fixated to the ambulatory cart pole. A removable top tray was designed to facilitate extra working surface on the ambulatory cart, but was not included in this first prototype.
Patient Support
Simulated patients can easily move the ECMOve themselves, resulting in a solid and safe walking experience. Very weak patients may require steering assistance from the caregiver by making use of the side handle. Additionally, the (de)braking system is not implemented in this first prototype, but necessary to prevent unintended movement of the cart during ambulation.
The walking frame unlocks and extends as intended. However, it is challenging to align the left and right part of the walking frame. The walking frame should be revised and adjusted accordingly to solve this issue. Preliminary tests suggest that in worst-case scenarios the walking frame prevents the patient from falling to the back, sides, and front. This reduces the risk of tension on the blood tubing and improves patient safety. The seat and backrest are sturdy and ensure safe patient transport. Applying the seat is quick and easy, allowing patients to sit down immediately without a deep squat and be moved back to the ICU including all equipment by one caregiver.
The seat and backrest slide open as intended, but do not run smoothly due to friction. The seat and backrest could be made less wide to improve comfort, without compromising safety. A fabric-type seat would be preferred to optimize the open/close mechanism. The backrest does need a rigid connection to lend stability to the walking frame.
Limitations
Although our prototype was successfully tested on healthy volunteers, no formal and structured user evaluation was conducted. Moreover, results from real debilitated patients are essential to confirm effectiveness in critically ill patients. Therefore, it is important to conduct a structured stakeholder analysis in the future, including patients, to validate our design choices. The ECMOve was developed with a focus on VV-ECMO patients utilizing jugular cannulation. However, the dual-lumen jugular technology is only part of the cannulation configurations used in clinical practice. Future designs will be tailored to ECMO patients having other cannulation strategies as well. Additionally, tracheostomy ventilated patients were not taken into account for current prototype development. Moreover, current device design is based on patient characteristics ranging from the 5th to the 95th percentile. However, patients outside this range may still be eligible for using the device as long as weight limits are not exceeded due to safety concerns. Further testing and optimization of the device aim for broader cannulation-strategy and patient suitability.
Conclusion
We developed a modular cart-in-cart system that provides safety and support during both stationary and ambulatory ECMO. Preliminary tests in a simulated ICU environment with healthy volunteers yielded promising results for the suitability of the ECMO mobilizing device in a clinical setting. However, full verification and validation, including realistic testing with patients in a clinical environment, is still required to fully determine the device’s capabilities. Although further testing and optimization are necessary, the design and development of ECMOve represent an important step forward in mobilizing ECMO patients.
Acknowledgment
The authors thank Maquet Cardiopulmonary/Getinge for kindly loaning us a Cardiohelp machine for the realistic testing of our prototype. The patent for this invention has been filed and is currently pending.
Supplementary Material
Footnotes
Disclosure: Maquet cardiopulmonary/Getinge provided a Cardiohelp for realistic testing of our device free of charge. D.J.M.v.G., Q.M., and J.A. filed a patent on the device on behalf of their employer, the University of Twente, Enschede, the Netherlands.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML and PDF versions of this article on the journal’s Web site (www.asaiojournal.com).
References
- 1.Abrams D, Brodie D: Extracorporeal membrane oxygenation for adult respiratory failure: 2017 update. Chest. 152: 639–649, 2017. [DOI] [PubMed] [Google Scholar]
- 2.Abrams D, Garan AR, Brodie D: Awake and fully mobile patients on cardiac extracorporeal life support. Ann Cardiothorac Surg. 8: 44–53, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nydahl P, Eggmann S: Walking on ECMO—Don’t try this at home. Intensive Crit Care Nurs. 72: 103260, 2022. [DOI] [PubMed] [Google Scholar]
- 4.Temesgen N, Chekol B, Tamirie T, Eshetie D, Simeneh N, Feleke A: Adult sedation and analgesia in a resource limited intensive care unit—A systematic review and evidence based guideline. Ann Med Surg (2012). 66: 102356, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ely EW, Shintani A, Truman B, et al. : Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 291: 1753–1762, 2004. [DOI] [PubMed] [Google Scholar]
- 6.Schechter MA, Ganapathi AM, Englum BR, et al. : Spontaneously breathing extracorporeal membrane oxygenation support provides the optimal bridge to lung transplantation. Transplantation. 100: 2699–2704, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abrams D, Javidfar J, Farrand E, et al. : Early mobilization of patients receiving extracorporeal membrane oxygenation: A retrospective cohort study. Crit Care. 18: R38, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Needham DM: Mobilizing patients in the intensive care unit: Improving neuromuscular weakness and physical function. JAMA. 300: 1685–1690, 2008. [DOI] [PubMed] [Google Scholar]
- 9.Hashem MD, Nelliot A, Needham DM: Early mobilization and rehabilitation in the ICU: Moving back to the future. Respir Care. 61: 971–979, 2016. [DOI] [PubMed] [Google Scholar]
- 10.Schweickert WD, Pohlman MC, Pohlman AS, et al. : Early physical and occupational therapy in mechanically ventilated, critically ill patients: A randomised controlled trial. Lancet. 373: 1874–1882, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rehder KJ, Turner DA, Hartwig MG, et al. : Active rehabilitation during extracorporeal membrane oxygenation as a bridge to lung transplantation. Respir Care. 58: 1291–1298, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wells CL, Forrester J, Vogel J, Rector R, Tabatabai A, Herr D: Safety and feasibility of early physical therapy for patients on extracorporeal membrane oxygenator: University of Maryland medical center experience. Crit Care Med. 46: 53–59, 2018. [DOI] [PubMed] [Google Scholar]
- 13.Ferreira DDC, Marcolino MAZ, Macagnan FE, Plentz RDM, Kessler A: Safety and potential benefits of physical therapy in adult patients on extracorporeal membrane oxygenation support: A systematic review. Rev Bras Ter Intensiva. 31: 227–239, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pasrija C, Mackowick KM, Raithel M, et al. : Ambulation with femoral arterial cannulation can be safely performed on venoarterial extracorporeal membrane oxygenation. Ann Thorac Surg. 107: 1389–1394, 2019. [DOI] [PubMed] [Google Scholar]
- 15.Braune S, Bojes P, Mecklenburg A, et al. : Feasibility, safety, and resource utilisation of active mobilisation of patients on extracorporeal life support: A prospective observational study. Ann Intensive Care. 10: 161, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ko Y, Cho YH, Park YH, et al. : Feasibility and safety of early physical therapy and active mobilization for patients on extracorporeal membrane oxygenation. ASAIO J. 61: 564–568, 2015. [DOI] [PubMed] [Google Scholar]
- 17.Boling B, Dennis DR, Tribble TA, Rajagopalan N, Hoopes CW: Safety of nurse-led ambulation for patients on venovenous extracorporeal membrane oxygenation. Prog Transplant. 26: 112–116, 2016. [DOI] [PubMed] [Google Scholar]
- 18.Nydahl P, Sricharoenchai T, Chandra S, et al. : Safety of patient mobilization and rehabilitation in the intensive care unit. Systematic review with meta-analysis. Ann Am Thorac Soc. 14: 766–777, 2017. [DOI] [PubMed] [Google Scholar]
- 19.Halfwerk FR, Wielens N, Hulskotte S, Brusse-Keizer M, Grandjean JG: A mobilization poster stimulates early in-hospital rehabilitation after cardiac surgery: A prospective sequential-group study. J Cardiothorac Surg. 18: 83, 2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Polastri M, Loforte A, Dell’Amore A, Nava S: Physiotherapy for patients on awake extracorporeal membrane oxygenation: A systematic review. Physiother Res Int. 21: 203–209, 2016. [DOI] [PubMed] [Google Scholar]
- 21.Mayer KP, Pastva AM, Du G, et al. : Mobility levels with physical rehabilitation delivered during and after extracorporeal membrane oxygenation: A marker of illness severity or an indication of recovery? Phys Ther. 102: pzab301, 2022. [DOI] [PubMed] [Google Scholar]
- 22.Investigators E-PS, International EN: Early mobilisation during extracorporeal membrane oxygenation was safe and feasible: A pilot randomised controlled trial. Intensive Care Med. 46: 1057–1059, 2020. [DOI] [PubMed] [Google Scholar]
- 23.Bain JC, Turner DA, Rehder KJ, et al. : Economic outcomes of extracorporeal membrane oxygenation with and without ambulation as a bridge to lung transplantation. Respir Care. 61: 1–7, 2016. [DOI] [PubMed] [Google Scholar]
- 24.Beyersdorf F, Trummer G, Benk C, Pooth JS: Application of cardiac surgery techniques to improve the results of cardiopulmonary resuscitation after cardiac arrest: Controlled automated reperfusion of the whole body. JTCVS Open. 8: 47–52, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kau M, Steltner JC, Lepper PM, et al. : First use of a new extracorporeal membrane oxygenation system in COVID19-associated adult respiratory distress syndrome: The MobyBox device. ASAIO J. 68: 996–1001, 2022. [DOI] [PubMed] [Google Scholar]
- 26.Polastri M, Eden A, Loforte A, et al. : Physiotherapy for patients on extracorporeal membrane oxygenation support: How, when, and who. An international EuroELSO survey. Perfusion. 39: 162–173, 2022. [DOI] [PubMed] [Google Scholar]
- 27.Haji JY, Mehra S, Doraiswamy P: Awake ECMO and mobilizing patients on ECMO. Indian J Thorac Cardiovasc Surg. 37(suppl 2): 309–318, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eden A, Purkiss C, Cork G, et al. : In-patient physiotherapy for adults on veno-venous extracorporeal membrane oxygenation—United Kingdom ECMO Physiotherapy Network: A consensus agreement for best practice. J Intensive Care Soc. 18: 212–220, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abrams D, Madahar P, Eckhardt CM, et al. ; MORE-PT Investigators: Early mobilization during extracorporeal membrane oxygenation for cardiopulmonary failure in adults: Factors associated with intensity of treatment. Ann Am Thorac Soc. 19: 90–98, 2022. [DOI] [PubMed] [Google Scholar]
- 30.Gazzato A, Scquizzato T, Franco A, Zangrillo A, Scandroglio AM: Walking on ECMO support: An analysis of videos shared on social media. Intensive Crit Care Nurs. 72: 103253, 2022. [DOI] [PubMed] [Google Scholar]
- 31.Graessler I, Hentze J, Bruckmann T: V-models for interdisciplinary systems engineering, in Proceedings of the DESIGN 2018 15th International Design Conference, The Design Society, 2018, pp 747–756. V-MODELS FOR INTERDISCIPLINARY SYSTEMS ENGINEERING / The Design Society [Google Scholar]
- 32.van Galen DJ, Meinders Q, Halfwerk F, Arens J: P69: ECMO mobilizing device. ASAIO J. 69(suppl 2): 148, 2023. [Google Scholar]
- 33.Delft TU: DINED 1D Anthropometric database—Dataset: dined2004, 2004.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.