Abstract
Background
Understanding the complexity and multidimensional nature of chronic breathlessness is key to its successful management. The aim of this study was to explore illness perceptions, cognitive and behavioural responses to chronic breathlessness in individuals living with advanced respiratory disease.
Methods
This was a cross-sectional secondary analysis of data from a feasibility randomised control trial (SELF-BREATHE) for individuals living with chronic breathlessness due to advanced disease. All participants completed the following questionnaires: numerical rating scale (NRS) breathlessness severity, NRS distress due to breathlessness, NRS self-efficacy for managing breathlessness, Dyspnea-12 (D-12), Chronic Respiratory Disease Questionnaire (CRQ), Brief Illness Perception Questionnaire (Brief IPQ) and the Cognitive and Behavioural Responses Questionnaire, short version (CBRQ-S). The associations between the Brief IPQ and CBRQ-S with NRS breathlessness severity, distress and self-efficacy, D-12 and CRQ were examined using Spearman's rho correlation coefficient rs. A Spearman's rs of ≥0.50 was predefined as the threshold to denote important associations between variables. A p-value of <0.008 was considered statistically significant, to account for the number of comparisons performed.
Results
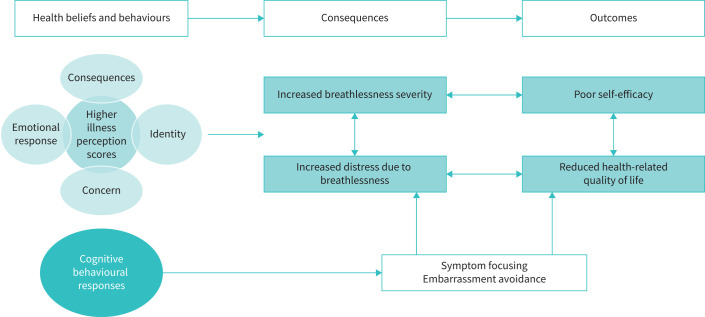
The illness perception items consequences, identity, concern and emotional response were associated with increased breathlessness severity, increased distress, reduced breathlessness self-management ability and lower health-related quality of life. Symptom focusing and embarrassment avoidance were identified as important cognitive responses to chronic breathlessness.
Conclusion
Interventions that directly target illness perceptions, cognitive and behavioural responses to chronic breathlessness may improve symptom burden, self-efficacy and health-related quality of life.
Shareable abstract
Interventions that directly target illness perceptions, cognitive and behavioural responses to chronic breathlessness may improve symptom burden, self-efficacy and health-related quality of life https://bit.ly/3I0aVp1
Introduction
Breathlessness is a significant global transdiagnostic problem, with more than 75 million people living with breathlessness, including >90% of the 65 million people with severe lung disease [1], >50% of the 10 million with incurable cancer and 50% of the 23 million with heart failure [2, 3]. More than two-thirds of those living with breathlessness have multimorbidity [4].
The burden of breathlessness on individuals, family, society and health systems is increasing with population ageing and multimorbidity, further amplified by the coronavirus disease 2019 (COVID-19) pandemic [5, 6]. Proactive approaches to the management of breathlessness are required to build capacity and resilience within healthcare systems, especially given rising health and social care costs, and workforce challenges [7–10].
Understanding the complexity and multidimensional nature of chronic breathlessness is key to its successful management. The American Thoracic Society defines dyspnoea (breathlessness) as “a subjective experience of breathing discomfort that consists of qualitatively distinct sensations that vary in intensity” [11]. The mechanisms of breathlessness are complex and incompletely understood [11]. Breathlessness derives from interactions between multiple physiological, psychological, social and environmental factors that may induce secondary physiological and behavioural responses [11]. When considering factors that influence outcomes and symptom burden in individuals living with chronic breathlessness, illness perceptions, cognitive and behavioural responses may be important determinants, especially in the context of self-management [12]. Leventhal's Common-Sense Model of Self-Regulation provides a framework to explore illness perceptions, cognitive and behavioural responses to chronic breathlessness in individuals living with chronic respiratory disease [13].
Leventhal's common-sense model of illness self-regulation is a prominent social cognition approach to describing the processes by which patients form lay beliefs (positive and negative) about health threats (e.g. symptoms), how these health beliefs impact coping procedures, and how subsequent appraisals of these procedures, iteratively and dynamically, update beliefs and responses to managing the perceived threat, consequently resulting in positive or negative outcomes [13, 14]. The model takes an individual perspective, recognising that illness management is dependent on individuals’ motivation to respond to and manage threat(s). Lay beliefs and associated coping responses (positive and negative) make sense to the individual, even though they may be inconsistent or contradictory to expert health advice [14]. Therefore, understanding patients’ health beliefs, cognitive and behavioural responses to chronic breathlessness in advanced respiratory disease is key to the development of new potential treatments for chronic breathlessness. We hypothesised that more negative health beliefs, cognitive and behavioural factors contribute to chronic breathlessness severity in patients with advanced disease.
Cognitive factors include beliefs about the dangers of undertaking activity (fear avoidance beliefs) and beliefs about self-efficacy, while behavioural factors include avoidance of activity, prolonged bed rest and all-or-nothing behaviour (i.e. periods of high activity followed by periods of inactivity), also referred to as “booming-and-busting” [15].
To date, research on the relationship between illness perceptions and coping, self-efficacy and health-related quality of life has been respiratory disease specific, e.g. asthma [16] and COPD [12, 17]. No studies have taken a transdiagnostic approach to chronic breathlessness. The move away from the single-diagnosis approach towards a transdiagnostic conceptualisation and treatment of chronic breathlessness represents a significant paradigm shift [10, 18]. The transdiagnostic approach focuses on identifying the common and core maladaptive temperamental, psychological, cognitive, emotional interpersonal and behavioural processes that underpin a broad array of diagnostic presentations/symptoms and targeting these factors in treatment(s) [18, 19]. Transdiagnostic treatments apply the same underlying treatment principles across diagnoses, without tailoring the treatment(s) to a specific diagnosis, and as such operate outside the traditional diagnostic boundaries [10, 18].
The aim of this study was to explore the associations between illness perceptions, cognitive and behavioural responses to chronic breathlessness in individuals living with advanced malignant and non-malignant respiratory disease to inform future studies and intervention development.
Methods
Design
This was a cross-sectional secondary analysis of data from a randomised, controlled, feasibility trial of an online, self-guided breathlessness supportive intervention (SELF-BREATHE) for individuals with chronic breathlessness due to advanced disease [10]. Ethical and local research and development approval was obtained prior to commencing this research (Research Ethics Committee/Health Research Authority reference 20/LO/1108). SELF-BREATHE was registered at ClinicalTrials.gov with identifier number NCT04574050.
Population
Patients living with chronic breathlessness due to advanced malignant or non-malignant disease.
Inclusion criteria
Adults aged ≥18 years.
Chronic breathlessness defined as breathlessness that persisted (>3 months) despite optimal pharmacological treatment of the underlying lung disease, including COPD, asthma, interstitial lung disease (ILD), chronic fibrotic lung disease following severe acute respiratory syndrome coronavirus 2 infection, bronchiectasis, cystic fibrosis and lung cancer.
Medical Research Council (MRC) dyspnoea score ≥2 (short of breath when hurrying on the level or walking up a slight hill) [20].
Access to a computer or tablet or smartphone with internet access.
Able to provide informed consent.
Exclusion criteria
Breathlessness of unknown cause.
Primary diagnosis of chronic hyperventilation syndrome.
Currently participating in a rehabilitation programme, e.g. pulmonary/cardiac rehabilitation.
Patient demographic and characterisation data
At baseline participants were asked to self-complete a demographic questionnaire which included the following: age, sex, ethnicity, educational level, employment status smoking status, MRC dyspnoea score and living status (alone versus living with others).
Patient-reported outcome measures
Breathlessness severity: worst over the last 24 h was assessed on a 0–10 numerical rating scale (NRS) (0=no shortness of breath, 10=worse possible) [10].
Dyspnoea 12 (D-12) quantifies breathlessness using 12 descriptors that tap the physical and affective aspects of dyspnoea [21].
Distress due to breathlessness over the last 24 h was assessed on a 0–10 NRS (0=no distress, 10=worse possible distress).
Self-efficacy for managing breathlessness was measured using the question “How confident are you that you can keep your shortness of breath from interfering with what you want to do?” scored on a 0–10 NRS (0=not at all confident, 10=totally confident) [10].
The Chronic Respiratory Disease Questionnaire (CRQ) is a 20-item validated health-related quality of life questionnaire across four domains: dyspnoea, fatigue, emotion and mastery, which is applicable across respiratory diseases. Experiences are rated on 7-point scales ranging from 1 (maximum impairment) to 7 (no impairment) [22].
Patients’ illness perceptions, cognitive and behavioural responses to chronic breathlessness were assessed using the validated Brief Illness Perception Questionnaire (Brief IPQ) and Cognitive and Behavioural Responses Questionnaire, short version (CBRQ-S).
The Brief IPQ is an eight-item questionnaire designed to rapidly assess cognitive and emotional representations of illness: consequences, timeline, personal control, treatment control, identity, concern, coherence and emotional response. Each item is rated on a 0–10 scale, with higher scores indicating a more threatening perception of the illness [23].
The CBRQ-S explores patient's cognitive and behavioural responses to their symptoms [24]. The CBRQ-S has four cognitive subscales (fear avoidance beliefs (e.g. “Physical activity makes my symptoms worse”), embarrassment avoidance beliefs (e.g. “I worry that people will think badly of me because of my symptoms”), symptom focusing (e.g. “My symptoms are always at the back of my mind”) and damage beliefs/catastrophising (e.g. “The severity of my symptoms must mean that there is something serious going on in my body”)) and two behavioural subscales (avoidance/resting behaviour (e.g. “I stay in bed to control my symptoms”) and all-or-nothing behaviour (e.g. “I find myself rushing to get things done before I crash”)). The cognitive subscales items are scored from 0 (strongly disagree) to 4 (strongly agree), while the behavioural subscales are scored from 0 (never) to 4 (all the time). Item scores are summed together to obtain a total score for each subscale. Higher scores indicate more negative cognitive responses to a symptom on the cognitive subscales. Higher scores on the behavioural subscales indicate greater use of avoidance and/or all-or-nothing behaviours in response to a symptom [25].
Data analysis
Patient demographics, characteristics and completed outcome measures were summarised using descriptive statistics. The associations between the Brief IPQ and CBRQ-S with NRS breathlessness severity, distress and self-efficacy, D-12, CRQ health-related quality of life and CRQ mastery were examined using Spearman's rho correlation coefficient rs. A Spearman's rs of ≥0.50 was predefined as the threshold to denote important associations between variables. A p-value of <0.008 was considered statistically significant. A Bonferroni correction was applied to an α-level of <0.05 (0.05/6=0.008) to allow for the number of comparisons performed between individual items on the Brief IPQ and CBRQ-S with variables of interest. Statistical analysis of the data was performed using SPSS for Windows version 28 (IBM, Armonk, NY, USA).
Results
52 participants with chronic breathlessness, across a wide range of ages and disease severity, were recruited; mean±sd age 63±13 years, of which 31% were >71 years of age, and MRC dyspnoea score 2.4±1, of which 40.5% had an MRC ≥4 (table 1).
TABLE 1.
Baseline demographics and characteristics of participants (n=52)
| Age (years) | 63±13 |
| Age category | |
| <40 years | 3 (5.8) |
| 41–50 years | 5 (9.6) |
| 51–60 years | 8 (15.4) |
| 61–70 years | 20 (38.5) |
| 71–80 years | 12 (23.1) |
| 81–90 years | 4 (7.7) |
| MRC dyspnoea score# | 2.4±1 |
| MRC dyspnoea score category# | |
| MRC 2 | 10 (19.2) |
| MRC 3 | 21 (40.4) |
| MRC 4 | 13 (25) |
| MRC 5 | 8 (15.5) |
| Sex | |
| Male | 31 |
| Female | 21 |
| Ethnicity ¶ | |
| White | 42 (80.8) |
| Asian or Asian British | 4 (7.7) |
| Black, African, Caribbean or Black British | 1 (1.9) |
| Mixed | 2 (3.8) |
| Other | 3 (5.8) |
| Primary diagnosis | |
| COPD | 31 (59.6) |
| Interstitial lung disease | 5 (9.6) |
| Bronchiectasis | 9 (17.3) |
| Cancer | 2 (3.8) |
| Asthma | 1 (1.9) |
| Cystic fibrosis | 1 (1.9) |
| Long COVID | 3 (5.8) |
| Smoking status | |
| Never-smoker | 13 (25) |
| Ex-smoker | 36 (69.2) |
| Current smoker | 3 (5.8) |
| Living situation | |
| Living alone | 25 (48.1) |
| Living with significant other/family | 27 (51.9) |
| Support provided by a carer | |
| Yes | 29 (55.8) |
| No | 23 (44.2) |
| Breathlessness severity | |
| NRS worst breathlessness in last 24 h# | 6.7±2.3 |
| Dyspnea-12 total score# | 18.4±8.8 |
| NRS distress due to breathlessness# | 5.3±2.8 |
| Health-related quality of life | |
| CRQ+ | 62±19 |
| Breathlessness self-management | |
| NRS confidence in breathlessness self-management+ | 4.3±2.7 |
| CRQ mastery+ | 3.8±1.4 |
Data are reported as mean±sd, n (%) or n. MRC: Medical Research Council; NRS: numerical rating scale (0−10); CRQ: Chronic Respiratory Disease Questionnaire. #: higher score worse; ¶: self-reported; +: higher score better.
Illness perceptions
Descriptive information on illness perceptions in individuals living with chronic breathlessness due to advanced disease is summarised in table 2. High illness perception scores (reflecting a more threatening view of illness) were reported specifically for the items timeline, concern and consequences, and low scores for the items personal control and treatment control over their illness/breathlessness (table 2). Patients believed that their illness severely affected their life, that it was long lasting; they were very concerned about the illness and moderately affected emotionally.
TABLE 2.
Illness perception in individuals living with chronic breathlessness due to advanced respiratory disease (n=52): Brief Illness Perception Questionnaire (Brief IPQ)
| Brief IPQ item | Mean±sd | Median (range) |
|
Consequences (0–10) How much does your illness affect your life? |
8.02±2.04 | 8.5 (2–10) |
|
Timeline (0–10) How long do you think your illness will continue? |
9.41±1.25 | 10 (3–10) |
|
Personal control (0–10) How much control do you feel you have over your illness? |
3.87±2.67 | 3 (0–10) |
|
Treatment control (0–10) How much do think your treatment can help your illness? |
5.34±2.40 | 5 (0–10) |
|
Identity (0–10) How much do you experience symptoms from your illness? |
7.29±2.01 | 8 (3–10) |
|
Concern (0–10) How concerned are you about your illness? |
8.12±2.25 | 9 (0–10) |
|
Coherence (0–10) How well do you feel you understand your illness? |
7.48±2.41 | 8 (2–8) |
|
Emotional response (0–10) How much does your illness affect you emotionally? (e.g. does it make you angry, scared, upset or depressed) |
6.21±3.25 | 7 (0–10) |
Higher scores reflect a more threatening view of illness.
The illness perception items consequences, identity, concern and emotional response were associated with increased breathlessness severity, increased distress, reduced breathlessness self-management ability and lower health-related quality of life (table 3).
TABLE 3.
Spearman's rho correlation coefficient rs between the Brief Illness Perception Questionnaire (Brief IPQ) and selected measures (n=52)
| Brief IPQ item | Consequences | Outcomes | ||||
| Breathlessness severity | Distress | Health-related quality of life | Self-management | |||
| NRS worst breathlessness over 24 h | Dyspnea-12 | NRS distress due to breathlessness | Health-related quality of life | NRS self-efficacy for managing breathlessness | CRQ mastery | |
| Consequences |
rs=0.57,
p<0.001* |
rs=0.57,
p<0.001* |
rs=0.47, p<0.001* |
rs= −0.54,
p<0.001* |
rs= −0.53,
p<0.001* |
rs= −0.58,
p<0.001* |
| Timeline | rs= −0.08, p=0.602 |
rs=0.06, p=0.683 |
rs= −0.16, p=0.249 |
rs=0.06, p=0.682 |
rs= −0.15, p=0.295 |
rs=0.01, p=0.947 |
| Personal control | rs= −0.22, p=0.116 |
rs= −0.16, p=0.285 |
rs= −0.26, p=0.158 |
rs=0.05, p=0.740 |
rs=0.28, p=0.045 |
rs=0.22, p=0.120 |
| Treatment control | rs= −0.12, p=0.416 |
rs=0.00, p=0.994 |
rs=0.04, p=0.962 |
rs= −0.10, p=0.486 |
rs=0.12, p=0.416 |
rs=0.02, p=0.872 |
| Identity |
rs=0.61,
p<0.001* |
rs=0.76,
p<0.001* |
rs=0.60,
p<0.001* |
rs= −0.65,
p<0.001* |
rs= −0.50,
p<0.001* |
rs= −0.65,
p<0.001* |
| Concern | rs=0.41, p=0.002* |
rs=0.61,
p<0.001* |
rs=0.41, p=0.003* |
rs= −0.54
p<0.001* |
rs= −0.59,
p<0.001* |
rs= −0.62,
p<0.001* |
| Coherence | rs=0.03, p=0.817 |
rs=0.04, p=0.772 |
rs= −0.07, p=0.643 |
rs=0.04, p=0.754 |
rs= −0.04, p=0.783 |
rs= −0.06, p=0.535 |
| Emotional response |
rs=0.50,
p<0.001* |
rs=0.79,
p<0.001* |
rs=0.76,
p<0.001* |
rs= −0.81,
p<0.001* |
rs= −0.38, p<0.001* |
rs= −0.78,
p<0.001* |
rs= ±1: perfect correlation; rs= ±0.50–0.99: strong correlation; rs= ±0.30–0.49: medium correlation; rs< ±0.29: small correlation; rs=0: no correlation. A Spearman's rs of ≥0.50 was predefined as the threshold to denote important associations between variables, highlighted in bold. *: correlation significant at p<0.008 level (two-tailed). NRS: numerical rating scale (0–10); CRQ: Chronic Respiratory Disease Questionnaire.
Cognitive and behavioural responses
Cognitive and behavioural responses to chronic breathlessness in advanced disease are reported in table 4. Participants reported high scores for cognitive response and symptom focusing, and low scores for behavioural response avoidance/resting behaviour (table 4). Symptom focusing (attention) and embarrassment avoidance were associated with breathlessness severity (table 4). In addition, symptom focusing was associated with distress due to breathlessness, lower health-related quality of life and reduced breathlessness self-management (table 5 and figure 1).
TABLE 4.
Cognitive and behavioural responses to chronic breathlessness in advanced disease: Cognitive Behavioural Responses Questionnaire, short version (CBRQ-S)
| CBRQ-S subscale | Mean±sd | Median (range) |
| Fear avoidance (0–12) | 6.33±1.84 | 6 (3–11) |
| Embarrassment avoidance (0–12) | 5.86±3.20 | 7 (0–12) |
| All-or-nothing behaviour (0–12) | 5.48±3.2 | 5 (0–11) |
| Damage beliefs (0–12) | 6.94±1.43 | 7 (3–9) |
| Symptom focusing (0–12) | 8.07±3.08 | 8 (0–12) |
| Avoidance/resting behaviour (0–12) | 3.53±3.14 | 3 (0–12) |
TABLE 5.
Spearman's rho correlation coefficient rs between the Cognitive Behavioural Responses Questionnaire, short version (CBRQ-S) and selected measures (n=52)
| CBRQ-S subscale | Consequences | Outcomes | ||||
| Breathlessness severity | Distress | Health-related quality of life | Self-management | |||
| NRS worst breathlessness over 24 h | Dyspnea-12 | NRS distress due to breathlessness | Health-related quality of life | NRS self-efficacy for managing breathlessness | CRQ mastery | |
| Fear avoidance | rs=0.06, p=0.673 |
rs=0.27, p=0.067 |
rs=0.25, p=0.080 |
rs= −0.33, p=0.012 |
rs= −0.10, p=0.472 |
rs= −0.32, p=0.025 |
| Embarrassment avoidance | rs=0.26, p=0.064 |
rs=0.50,
p<0.001 * |
rs=0.19, p=0.198 |
rs= −0.40, p=0.003* |
rs= −0.36, p=0.010 |
rs= −0.39, p=0.004* |
| All-or-nothing behaviour | rs=0.29, p=0.043 |
rs=0.24, p=0.115 |
rs=0.28, p=0.050 |
rs= −0.41, p=0.003* |
rs= −0.11, p=0.455 |
rs= −0.134, p=0.357 |
| Damage beliefs | rs=0.20, p=0.146 |
rs=0.13, p=0.385 |
rs=0.00, p=0.997 |
rs= −0.07, p=0.608 |
rs= −0.08, p=0.567 |
rs= −0.02, p=0.881 |
| Symptom focusing |
rs=0.50,
p<0.001* |
rs=0.50,
p<0.001* |
rs=0.52,
p<0.001* |
rs= −0.60,
p<0.001* |
rs= −0.27, p<0.049 |
rs= −0.54,
p<0.001* |
| Avoidance/resting behaviour | rs=0.16, p=0.250 |
rs=0.287, p=0.051 |
rs=0.32, p=0.023 |
rs= −0.22, p=0.116 |
rs= −0.08, p=0.566 |
rs= −0.22, p=0.120 |
rs= ±1: perfect correlation; rs= ±0.50–0.99: strong correlation; rs= ±0.30–0.49: medium correlation; rs< ±0.29: small correlation; rs=0: no correlation. A Spearman's rs of ≥0.50 was predefined as the threshold to denote important associations between variables, highlighted in bold. *: correlation significant at p<0.008 level (two-tailed). NRS: numerical rating scale (0–10); CRQ: Chronic Respiratory Disease Questionnaire.
FIGURE 1.
Illness perception, cognitive and behavioural responses, resultant consequences, and outcomes in patients living with chronic breathlessness due to advanced respiratory disease. Leventhal's Common-Sense Model of Self-Regulation states that patient health beliefs (positive and negative) determine behavioural responses and coping strategies in response to illness, consequently resulting in positive or negative outcomes [13]. Interventions that target modifiable factors, i.e. patient health beliefs and behaviours, may improve patient outcomes. Bidirectional arrows highlight the interaction between consequences and outcomes.
Discussion
Key findings
This is the first study to explore illness perceptions, cognitive and behavioural responses to chronic breathlessness in individuals living with advanced malignant and non-malignant respiratory disease. Participant's illness perception scores showed a high level of understanding of their main condition (coherence) coupled with high scores (reflecting a more threatening view of illness) on the items timeline, concern and consequences. Personal control beliefs were low, indicating that most participants did not believe they had any influence on the course of their breathlessness.
In relation to illness perception items, more extreme scores on consequences, identity, concern and emotional response were associated with increased breathlessness severity, increased distress, reduced breathlessness self-management ability and lower health-related quality of life. Symptom focusing and embarrassment avoidance were identified as important cognitive responses to chronic breathlessness.
Relevance of findings
Comparing our findings with reference groups in the literature for patients with COPD and asthma [12], our cohort reported more strongly affected illness perceptions, they perceived more negative consequences, less personal and treatment control, and increased identity, concern and emotional response [12]. Interestingly, the scores in our cohort and the COPD and asthma reference groups for timeline and coherence were similar [12].
Our findings are in keeping with other studies in chronic conditions where illness perceptions have been found to relate to patients' quality of life and other clinical outcomes [16, 26, 27]. For example, patients who perceived high control of their illness were less likely to have unplanned hospital attendance [16, 26, 27]. This is of particular importance in the context of chronic breathlessness management, as data suggest that one-fifth of emergency department presentations by ambulance in the UK are due to acute-on-chronic breathlessness [8, 28]. Illness perceptions influence patients' motivation to adopt specific strategies to manage their emotions and increase control over symptoms [13].
We found that symptom focusing was associated with increased breathlessness severity. Symptom focusing leads to enhanced attention to and/or hypervigilance of one's breathing pattern and breathlessness. Consequently, individuals interpret any change in their breathing awareness and/or breathlessness as a signal of impending harm. This inadvertently creates a vicious cycle where the increased attention results in exaggerated or catastrophic perceptions of their breathing. Inefficient breathing adaptations are then adopted, which leads to a worsening of breathlessness [13, 29, 30]. A strength of this study was the multidimensional battery of outcome measures used, resulting in novel data on the potential importance of attention/hypervigilance in breathlessness severity.
Reflecting inclusion criteria of previously published clinical trials of breathlessness supportive services [31] and referral criteria to clinical services in the UK, such as pulmonary rehabilitation, we included patients with an MRC dyspnoea score of ≥2. Individuals with an MRC dyspnoea score of 2 accounted for 19% of the cohort. Our findings highlight that even without severely disabling breathlessness these associations are important to consider, and therefore potentially applicable and transferable to patients earlier as well as later in the disease trajectory.
In understanding the complexity of living with chronic breathlessness it is vital to understand the importance of cognitive and behavioural factors associated with chronic breathlessness. While it is important to acknowledge the distressing nature of breathlessness in patients with serious disease, it is also important to understand the cognitive factors that are adding to distress, poor quality of life and low self-efficacy, because these factors are amenable to change. Evidence suggests that non-pharmacological treatments [31, 32] and self-management interventions improve health status and outcomes in patients with chronic breathlessness. Outcomes could be further enhanced by targeting symptom focusing specifically. Attentional training, a brief metacognitive treatment, is designed to re-orient patients’ attention, reduce symptom focusing and produce a shift away from self-focus. This could lead to a reduction in breathlessness or at least pre-occupation with it [33, 34].
Given the high scores reported on the items timeline and concern on the Brief IPQ, in addition to the fact that patients’ quality of life is adversely affected, a focus on values-based goals is warranted. Third-wave psychotherapies such as acceptance and commitment therapy (ACT) have been evaluated in the context of several long-term conditions and found to improve a range of outcomes [35]. ACT focuses on helping people to respond flexibly to symptoms, accept what cannot be changed, and focus on values and life goals.
Patients' willingness, motivation and ability to participate in these self-management interventions will vary, but discussing the role of perceptions and cognitive behavioural responses explicitly with patients may enhance motivation [13].
This study focuses on a transdiagnostic approach. Given the small sample size for conditions such as ILD (n=5), bronchiectasis (n=9) and cancer (n=2), we were unable to assess the potential influence of disease-specific diagnoses on illness perceptions, cognitive and behavioural responses to chronic breathlessness. A limitation of this study is that we do not have any data on illness and breathlessness symptom duration. Onset/duration of chronic breathlessness is not routinely documented in clinical notes. With hindsight we could have asked subjectively how long individuals had been living with/experiencing breathlessness. However, it must be acknowledged that there are challenges and limitations with this approach, especially regarding patient recall [36].
This is a cross-sectional secondary analysis of baseline data from a feasibility randomised controlled trial of an online breathlessness self-management intervention (SELF-BREATHE), the results of which have been published in ERJ Open Research [10]. As this was a feasibility study, it was not powered to conduct any pre- versus post-interventional analysis. We acknowledge that there are limitations with this cross-sectional secondary data analysis approach. Future prospective studies should seek to understand cause/effect relationships. However, it is important to highlight that mediation analysis will help discern mechanisms of change [37, 38]. Our data highlight the importance of including the illness perceptions and the cognitive and behavioural responses questionnaires repeatedly within clinical trials testing interventions for chronic breathlessness, so that mechanisms can be investigated [37, 38].
Both males and females were well represented in our study. However, our sample was predominantly White. Under-representation of minority ethnic groups in medical research is an ongoing issue in the UK and beyond [39, 40]. Ensuring equity, inclusion and diversity of participants must be a priority in planning subsequent studies.
We have developed a complex intervention for breathlessness: SELF-BREATHE. SELF-BREATHE is a complex, transdiagnostic, breathlessness, supportive digital intervention co-developed with patients [10, 41, 42], theoretically underpinned by Leventhal's common-sense model of illness self-regulation [10, 13, 43, 44]. It targets negative health beliefs and behavioural responses to chronic breathlessness via education and self-management non-pharmacological approaches, e.g. breathing exercises, pacing and goal setting [10]. The next step in our programme of research is to carry out a multicentre randomised controlled trial to test SELF-BREATHE.
Our findings provide a testable hypothesis that improving patient's illness perceptions, cognitive and behavioural responses via SELF-BREATHE will improve symptom burden, symptom control and health-related quality of life in adults living with chronic breathlessness due to advanced disease.
Conclusion
The illness perception items consequences, identity, concern and emotional response were associated with increased breathlessness severity, increased distress, reduced breathlessness self-management ability and lower health-related quality of life. Symptom focusing and embarrassment avoidance were identified as important cognitive responses to chronic breathlessness. These data provide a testable hypothesis that interventions targeting illness perceptions, cognitive and behavioural responses to chronic breathlessness will improve symptom burden, self-efficacy and health-related quality of life.
Acknowledgements
We thank all the patients who participated in this research, and everybody who identified and screened patients for this study, especially the respiratory medicine and physiotherapy departments at King's College Hospital (London, UK).
Provenance: Submitted article, peer reviewed.
SELF-BREATHE is registered at ClinicalTrials.gov with identifier number NCT04574050.
Ethics statement: Ethical and local research and development approval was obtained prior to commencing this research (Research Ethics Committee/Health Research Authority reference 20/LO/1108).
Author contributions: C.C. Reilly was the grant award holder (ICA-CL-2018-04-ST2-001) and chief investigator. Conception and design: C.C. Reilly, T. Chalder and I.J. Higginson. Data acquisition: C.C. Reilly. Data analysis and interpretation was led by C.C. Reilly, I.J. Higginson and T. Chalder. All authors contributed to the integration of the interpretation of the data and provided critical revision of the manuscript for important intellectual content. All authors read and approved the final manuscript.
Conflict of interest: C.C. Reilly reports support for the present manuscript from NIHR Clinical Lectureship (ICA-CL-2018-04-ST2-001), which funds all aspects of this research; and grants or contracts from King's Together multi and interdisciplinary research scheme, and Royal Brompton Hospital–King's Health Partnership Transformation funding, outside the submitted work.
Conflict of interest: I.J. Higginson reports grants or contracts from the NIHR, UKRI, Cicely Saunders International and Marie Curie, outside the submitted work.
Conflict of interest: T. Chalder reports support for the present manuscript by receiving salary support from the NIHR Mental Health Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King's College London. The views expressed in this article are those of the authors and not necessarily those of the NIHR or the NHS.
Support statement: A National Institute for Health and Care Research (NIHR) Clinical Lectureship (ICA-CL-2018-04-ST2-001) supports C.C. Reilly. I.J. Higginson is supported by the NIHR Applied Research Collaboration South London (NIHR ARC South London) at King's College Hospital NHS Foundation Trust. I.J. Higginson is an NIHR Senior Investigator Emeritus. This publication presents independent research funded by the NIHR. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, NIHR or the Department of Health and Social Care. Funding information for this article has been deposited with the Crossref Funder Registry.
References
- 1.Sorenson HM. Palliative care for lung disease: start early, stay late. Lancet Respir Med 2013; 1: 279–280. doi: 10.1016/S2213-2600(13)70083-3 [DOI] [PubMed] [Google Scholar]
- 2.Solano JP, Gomes B, Higginson IJ. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage 2006; 31: 58–69. doi: 10.1016/j.jpainsymman.2005.06.007 [DOI] [PubMed] [Google Scholar]
- 3.Austin J, Williams R, Ross L, et al. Randomised controlled trial of cardiac rehabilitation in elderly patients with heart failure. Eur J Heart Fail 2005; 7: 411–417. doi: 10.1016/j.ejheart.2004.10.004 [DOI] [PubMed] [Google Scholar]
- 4.Sandberg J, Ekström M, Börjesson M, et al. Underlying contributing conditions to breathlessness among middle-aged individuals in the general population: a cross-sectional study. BMJ Open Respir Res 2020; 7: e000643. doi: 10.1097/SPC.0000000000000568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.D'Cruz RF, Waller MD, Perrin F, et al. Chest radiography is a poor predictor of respiratory symptoms and functional impairment in survivors of severe COVID-19 pneumonia. ERJ Open Res 2021; 7: 00655-2020. doi: 10.1183/23120541.00655-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cares-Marambio K, Montenegro-Jiménez Y, Torres-Castro R, et al. Prevalence of potential respiratory symptoms in survivors of hospital admission after coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis. Chron Respir Dis 2021; 18: 14799731211002240. doi: 10.1177/14799731211002240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kelly AM, Keijzers G, Klim S, et al. An observational study of dyspnea in emergency departments: the Asia, Australia, and New Zealand Dyspnea in Emergency Departments Study (AANZDEM). Acad Emerg Med 2017; 24: 328–336. doi: 10.1111/acem.13118 [DOI] [PubMed] [Google Scholar]
- 8.Hutchinson A, Pickering A, Williams P, et al. Breathlessness and presentation to the emergency department: a survey and clinical record review. BMC Pulm Med 2017; 17: 53. doi: 10.1186/s12890-017-0396-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Currow DC, Chang S, Ekström M, et al. Health service utilisation associated with chronic breathlessness: random population sample. ERJ Open Res 2021; 7: 00415-2021. doi: 10.1183/23120541.00415-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reilly CC, Maddocks M, Chalder T, et al. A randomised, controlled, feasibility trial of an online, self-guided breathlessness supportive intervention (SELF-BREATHE) for individuals with chronic breathlessness due to advanced disease. ERJ Open Res 2023; 9: 00508-2022. doi: 10.1183/23120541.00508-2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Parshall MB, Schwartzstein RM, Adams L, et al. An official American Thoracic Society statement: update on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care Med 2012; 185: 435–452. doi: 10.1164/rccm.201111-2042ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tiemensma J, Gaab E, Voorhaar M, et al. Illness perceptions and coping determine quality of life in COPD patients. Int J Chron Obstruct Pulmon Dis 2016; 11: 2001–2007. doi: 10.2147/COPD.S109227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leventhal H, Phillips LA, Burns E. The Common-Sense Model of Self-Regulation (CSM): a dynamic framework for understanding illness self-management. J Behav Med 2016; 39: 935–946. doi: 10.1007/s10865-016-9782-2 [DOI] [PubMed] [Google Scholar]
- 14.Hagger MS, Orbell S. The common sense model of illness self-regulation: a conceptual review and proposed extended model. Health Psychol Rev 2022; 16: 347–377. doi: 10.1080/17437199.2021.1878050 [DOI] [PubMed] [Google Scholar]
- 15.Loades ME, Vitoratou S, Rimes KA, et al. Psychometric properties of the Cognitive and Behavioural Responses Questionnaire (CBRQ) in adolescents with chronic fatigue syndrome. Behav Cogn Psychother 2020; 48: 160–171. doi: 10.1017/S1352465819000390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cai Q, Jin M, Li X, et al. Effect of illness perceptions on asthma control and quality of life amongst adult outpatients with asthma in China. BMC Psychol 2023; 11: 68. doi: 10.1186/s40359-023-01097-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.An J, Zhou H, Yang T, et al. Relationship of psychological factors with daily activities and quality of life in patients with chronic obstructive pulmonary disease in a Chinese rural population. Ann Palliat Med 2021; 10: 1675–1684. doi: 10.21037/apm-20-1151 [DOI] [PubMed] [Google Scholar]
- 18.Newby JM, McKinnon A, Kuyken W, et al. Systematic review and meta-analysis of transdiagnostic psychological treatments for anxiety and depressive disorders in adulthood. Clin Psychol Rev 2015; 40: 91–110. doi: 10.1016/j.cpr.2015.06.002 [DOI] [PubMed] [Google Scholar]
- 19.Barlow DH, Allen LB, Choate ML. Toward a unified treatment for emotional disorders – republished article. Behav Ther 2016; 47: 838–853. doi: 10.1016/j.beth.2016.11.005 [DOI] [PubMed] [Google Scholar]
- 20.Bestall JC, Paul EA, Garrod R, et al. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax 1999; 54: 581–586. doi: 10.1136/thx.54.7.581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res 2016; 26: 1753–1760. doi: 10.1177/1049732315617444 [DOI] [PubMed] [Google Scholar]
- 22.Schünemann HJ, Puhan M, Goldstein R, et al. Measurement properties and interpretability of the Chronic respiratory disease questionnaire (CRQ). COPD 2005; 2: 81–89. doi: 10.1081/COPD-200050651 [DOI] [PubMed] [Google Scholar]
- 23.Broadbent E, Petrie KJ, Main J, et al. The Brief Illness Perception Questionnaire. J Psychosom Res 2006; 60: 631–637. doi: 10.1016/j.jpsychores.2005.10.020 [DOI] [PubMed] [Google Scholar]
- 24.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol 2000; 55: 68–78. doi: 10.1037/0003-066X.55.1.68 [DOI] [PubMed] [Google Scholar]
- 25.Picariello F, Chilcot J, Chalder T, et al. The Cognitive and Behavioural Responses to Symptoms Questionnaire (CBRQ): development, reliability and validity across several long-term conditions. Br J Health Psychol 2023; 28: 619–638. doi: 10.1111/bjhp.12644 [DOI] [PubMed] [Google Scholar]
- 26.Rijken M, Valderas JM, Heins M, et al. Identifying high-need patients with multimorbidity from their illness perceptions and personal resources to manage their health and care: a longitudinal study. BMC Fam Pract 2020; 21: 75. doi: 10.1186/s12875-020-01148-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Borge CR, Moum T, Puline Lein M, et al. Illness perception in people with chronic obstructive pulmonary disease. Scand J Psychol 2014; 55: 456–463. doi: 10.1111/sjop.12150 [DOI] [PubMed] [Google Scholar]
- 28.Hutchinson A, Allgar V, Cohen J, et al. Mixed-methods feasibility cluster randomised controlled trial of a paramedic-administered breathlessness management intervention for acute-on-chronic breathlessness (BREATHE): study findings. ERJ Open Res 2022; 8: 00257-2022. doi: 10.1183/23120541.00257-2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Steinmann J, Lewis A, Ellmers TJ, et al. Validating the Breathing Vigilance Questionnaire for use in dysfunctional breathing. Eur Respir J 2023; 61: 2300031. doi: 10.1183/13993003.00031-2023 [DOI] [PubMed] [Google Scholar]
- 30.Vlemincx E. Dysfunctional breathing: a dimensional, transdiagnostic perspective. Eur Respir J 2023; 61: 2300629. doi: 10.1183/13993003.00629-2023 [DOI] [PubMed] [Google Scholar]
- 31.Higginson IJ, Bausewein C, Reilly CC, et al. An integrated palliative and respiratory care service for patients with advanced disease and refractory breathlessness: a randomised controlled trial. Lancet Respir Med 2014; 2: 979–987. doi: 10.1016/S2213-2600(14)70226-7 [DOI] [PubMed] [Google Scholar]
- 32.Brighton LJ, Miller S, Farquhar M, et al. Holistic services for people with advanced disease and chronic breathlessness: a systematic review and meta-analysis. Thorax 2019; 74: 270–281. doi: 10.1136/thoraxjnl-2018-211589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Knowles MM, Foden P, El-Deredy W, et al. A systematic review of efficacy of the attention training technique in clinical and nonclinical samples. J Clin Psychol 2016; 72: 999–1025. doi: 10.1002/jclp.22312 [DOI] [PubMed] [Google Scholar]
- 34.Wells A. Panic disorder in association with relaxation induced anxiety: an attentional training approach to treatment. Behav Ther 1990; 21: 273–280. doi: 10.1016/S0005-7894(05)80330-2 [DOI] [Google Scholar]
- 35.Graham CD, Gouick J, Krahé C, et al. A systematic review of the use of Acceptance and Commitment Therapy (ACT) in chronic disease and long-term conditions. Clin Psychol Rev 2016; 46: 46–58. doi: 10.1016/j.cpr.2016.04.009 [DOI] [PubMed] [Google Scholar]
- 36.Laws MB, Lee Y, Taubin T, et al. Factors associated with patient recall of key information in ambulatory specialty care visits: results of an innovative methodology. PLoS One 2018; 13: e0191940. doi: 10.1371/journal.pone.0191940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hayes AM, Laurenceau JP, Feldman G, et al. Change is not always linear: the study of nonlinear and discontinuous patterns of change in psychotherapy. Clin Psychol Rev 2007; 27: 715–723. doi: 10.1016/j.cpr.2007.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kazdin AE. Mediators and mechanisms of change in psychotherapy research. Annu Rev Clin Psychol 2007; 3: 1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432 [DOI] [PubMed] [Google Scholar]
- 39.Ainsworth B, Greenwell K, Stuart B, et al. Feasibility trial of a digital self-management intervention ‘My Breathing Matters’ to improve asthma-related quality of life for UK primary care patients with asthma. BMJ Open 2019; 9: e032465. doi: 10.1136/bmjopen-2019-032465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Smart A, Harrison E. The under-representation of minority ethnic groups in UK medical research. Ethn Health 2017; 22: 65–82. doi: 10.1080/13557858.2016.1182126 [DOI] [PubMed] [Google Scholar]
- 41.Reilly CC, Bristowe K, Roach A, et al. “The whole of humanity has lungs, doesn't it? We are not all the same sort of people”: patient preferences and choices for an online, self-guided chronic breathlessness supportive intervention: SELF-BREATHE. ERJ Open Res 2022; 8: 00093-2022. doi: 10.1183/23120541.00093-2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Reilly CC, Bristowe K, Roach A, et al. “You can do it yourself and you can do it at your convenience”: internet accessibility and willingness of people with chronic breathlessness to use an internet-based breathlessness self-management intervention during the COVID-19 pandemic. ERJ Open Res 2022; 8: 00557-2021. doi: 10.1183/23120541.00557-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mummah SA, Robinson TN, King AC, et al. IDEAS (Integrate, Design, Assess, and Share): a framework and toolkit of strategies for the development of more effective digital interventions to change health behavior. J Med Internet Res 2016; 18: e317. doi: 10.2196/jmir.5927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Skivington K, Matthews L, Simpson SA, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ 2021; 374: n2061. doi: 10.1136/bmj.n2061 [DOI] [PMC free article] [PubMed] [Google Scholar]