ABSTRACT
While fluconazole use is generally considered safe and well-tolerated, there has been an increasing number of reports regarding several adverse events. Therefore, the present study aimed to present a unique case in which photobiomodulation therapy (PBMT) was employed to manage bullous erythema multiforme lesions secondary to fluconazole intake. A 32-year-old female patient sought emergency dental care due to painful orofacial lesions that had developed two days after oral fluconazole use for recurrent vulvovaginal candidiasis. Given the acute clinical features, a diagnosis of bullous erythema multiforme secondary to fluconazole was established. Prednisone 20 mg was then prescribed for five days, and fluconazole intake was immediately discontinued. As the initial treatment strategies failed to show improvement in the clinical condition, three PBMT sessions were proposed every other day. Within seven days, almost complete wound healing was observed, and any pain complaints were no longer present. The resolution of orofacial lesions within a short period suggests that PBMT could be a promising tool for managing drug-induced bullous erythema multiforme. However, more studies are needed to confirm this statement.
Keywords: Case report, erythema multiforme, fluconazole, low-level laser
INTRODUCTION
Although fluconazole use is thought to be safe and well-tolerated, it may interact with other drugs,[1] and reports of several adverse events have been increasing over time.[2] Mild gastrointestinal, hepatic, hematologic, neurologic, cutaneous, endocrine, and metabolic effects are commonly described in patients receiving fluconazole; however, very serious and fatal cases have already been presented as well.[3]
Among these adverse effects, severe allergy and hypersensitivity reactions to fluconazole are of great clinical concern despite being very uncommon. Fixed drug eruptions,[4,5] Steven–Johnson Syndrome,[6] toxic epidermal necrolysis, angioedema,[2] and even anaphylactic reaction[7] are conditions that doctors may face in daily clinical routine when prescribing this antifungal medication. Erythema multiforme (EM), a reactive mucocutaneous disorder of variable severity and extension, may be triggered by a hypersensitivity reaction to a drug[8] but, to date, there is no report on the relationship between oral manifestations of EM and the fluconazole use.
In light of these facts, the present study aims to present a unique case in which photobiomodulation therapy (PBMT) was used to manage bullous EM lesions secondary to fluconazole intake.
CASE REPORT
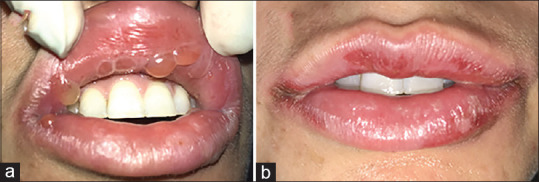
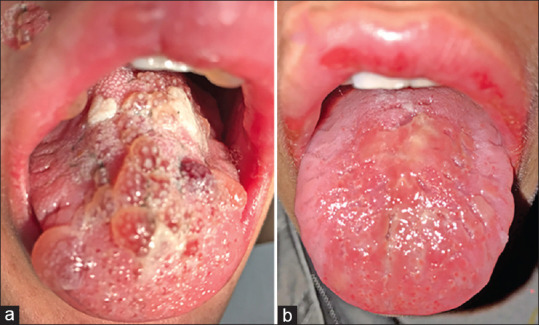
A 32-year-old female sought emergency dental care from a private office due to painful orofacial lesions that had arisen two days earlier. The patient reported a medical history of recurrent vulvovaginal candidiasis with symptoms for which she attempted self-treatment with fluconazole (150 mg daily). No other medication intake or systemic conditions were reported. She noted that similar lesions, but less severe, had occurred at the same orofacial sites in the last vulvovaginal infection, which was also treated with fluconazole. Clinical examination revealed several blistering lesions on both lips [Figure 1a] and the dorsum of the tongue [Figure 2a] associated with diffuse edema and an erythematous target lesion on the ventral aspects of the hand. According to her medical history and conventional clinical features, the diagnosis of bullous EM was established for the orofacial lesions and fixed drug eruption for the hand lesion, with no other differential diagnosis to be considered. No specific diagnostic testing was asked because of the patient’s economic status and the need for prompt relief of the acute symptoms from the lesions.
Figure 1.
The clinical course of the lesions on the tongue. (a) Initial clinical aspects. (b) Clinical aspects on the 7th day after photobiomodulation therapy
Figure 2.
The clinical course of the lesions on both lips. (a) Initial clinical aspects. (b) Clinical aspects on the 7th day after photobiomodulation therapy
Prednisone 20 mg was initially prescribed for five days, and fluconazole intake was interrupted immediately. On the next day of follow-up, the hand lesion was completely resolved, but the orofacial lesions did not. Thus, three PBMT sessions were proposed every other day. For that, the device Therapy XT® (DMC, São Carlos SP, Brazil) was used in contact mode, perpendicularly to the tissues, at 660 nm, 100 mW, with 10 seconds and 1 J per point, totaling 15 points (10 on the tongue and 5 on both lips). After every session of laser irradiation, progressive analgesia was reported without any adverse effect. Within seven days, almost complete wound healing was observed, and any pain complaint was no longer present [Figures 1b and 2b]. The patient was advised for gynecological evaluation and has been under follow-up with no more signs or symptoms.
DISCUSSION
Chronic recurrent vulvovaginal candidiasis affects 5%–8% of women during their fertile years, and the treatment may be challenging, which generally requires drugs such as fluconazole or other antimycotics.[9] Fluconazole, the first azole antifungal compound commercially produced, is used for treating not only superficial mycoses but also systemic fungal infections[10] due to its selectivity for fungal cytochrome P45014a-demethylase (P45014DM).[5]
EM is an acute, immune-mediated, mucocutaneous condition often related to a viral infection, but it may also occur during medication use,[11] including antifungal agents. Although the classification of severe forms of EM is still a matter of debate and confusion among authors, especially when considering the differential diagnosis of Steven–Johnson Syndrome and toxic epidermal necrolysis, the patient herein presented was diagnosed with the bullous variant since the clinical mucocutaneous detachment was below 10% of the body surface area and raised atypical targets were observed.[12]
The treatment of EM varies according to the etiology, clinical presentation/involvement, chronicity, and severity.[13,14] Most cases are mild and acute and show spontaneous regression within a few weeks with only conservative care directed towards symptoms (e.g., adequate nutrition, analgesics, anesthetics, and even corticosteroids, antihistamines, and antibiotics). In drug-induced cases, rapid identification and drug withdrawal are essential.[15,16] As the majority of treatment recommendations rely on case series or expert opinion, the management of severe cases is still unclear, which includes many systemic agents and even hospitalization.[14]
The rationale behind the present case report was that laser therapies have shown good results in previous reports of virus-induced orofacial lesions with similar clinical presentations.[17,18,19] PBMT, specifically, is popular among clinicians due to its capacity to modulate inflammation, relieve pain, and promote healing.[18,19] Moreover, it is non-invasive,[20] safe, and painless,[21] reasons why it was well tolerated by the patient, leading to excellent treatment adherence.
To the best of the authors’ knowledge, there are no other similar case reports both on the use of PBMT for the management of oral bullous EM and on the occurrence of oral bullous EM induced by fluconazole, which makes this case report valuable even considering all the limitations inherent to this type of study (e.g., lack of generalization, impossibility to establish a cause-effect relationship, overinterpretation or misinterpretation).[22]
CONCLUSION
Given that the orofacial lesions were resolved in a short period, PBMT seems to be a promising tool for the management of drug-induced bullous EM. More studies, however, are needed to confirm this statement.
Ethics statement
The patient gave informed consent. Patient anonymity was assured.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Heikkil H, Timonen K, Stubb S. Fixed drug eruption due to fluconazole. J Am Acad Dermatol. 2000;42:883–4. doi: 10.1016/s0190-9622(00)90262-7. [DOI] [PubMed] [Google Scholar]
- 2.Craig TJ. Adverse reactions to fluconazole: Illustrative case with focus on desensitization. J Osteopath Med. 1997;97:584. doi: 10.7556/jaoa.1997.97.10.584. [DOI] [PubMed] [Google Scholar]
- 3.Amichai B, Grunwald MH. Adverse drug reactions of the new oral antifungal agents –terbinafine, fluconazole, and itraconazole. Int J Dermatol. 1998;37:410–5. doi: 10.1046/j.1365-4362.1998.00496.x. [DOI] [PubMed] [Google Scholar]
- 4.Nakai N, Katoh N. Fixed drug eruption caused by fluconazole: A case report and mini-review of the literature. Allergol Int. 2013;62:139–41. doi: 10.2332/allergolint.12-LE-0464. [DOI] [PubMed] [Google Scholar]
- 5.Tavallaee M, Rad MM. Fixed drug eruption resulting from fluconazole use: A case report. J Med Case Rep. 2009;3:7368. doi: 10.4076/1752-1947-3-7368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Craythorne E, Creamer D. Stevens-Johnson syndrome due to prophylactic fluconazole in two patients with liver failure. Clin Exp Dermatol. 2009;34:e389–90. doi: 10.1111/j.1365-2230.2009.03365.x. [DOI] [PubMed] [Google Scholar]
- 7.Neuhaus G, Pavic N, Pletscher M. Anaphylactic reaction after oral fluconazole. BMJ. 1991;302:1341. doi: 10.1136/bmj.302.6788.1341-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ayangco L, Rogers RS. Oral manifestations of erythema multiforme. Dermatol Clin. 2003;21:195–205. doi: 10.1016/s0733-8635(02)00062-1. [DOI] [PubMed] [Google Scholar]
- 9.Benedix F, Schilling M, Schaller M, Röcken M, Biedermann T. A young woman with recurrent vesicles on the lower lip: Fixed drug eruption mimicking herpes simplex. Acta Derm Venereol. 2008;88:491–4. doi: 10.2340/00015555-0519. [DOI] [PubMed] [Google Scholar]
- 10.Eşkut N, Gedizlioğlu M, Ünal O, Özlü C, Ergene U. Acute fluconazole toxicity: A case presenting with protean manifestations including systemic and neurologic symptoms. Postgrad Med. 2021;133:250–2. doi: 10.1080/00325481.2020.1840830. [DOI] [PubMed] [Google Scholar]
- 11.Kashfi S, Radparvar AA, Ventura Y, Sharma S, Sharma S. Bullous erythema multiforme secondary to trimethoprim-sulfamethoxazole use, treated with cyclosporine in a 91-year-old male. Cureus. 2021;13:e18239. doi: 10.7759/cureus.18239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bastuji-Garin S, Rzany B, Stern RS, Shear NH, Naldi L, et al. Clinical classification of cases of toxic epidermal necrolysis, Stevens-Johnson syndrome, and erythema multiforme. Arch Dermatol. 1993;129:92–6. [PubMed] [Google Scholar]
- 13.Soares A, Sokumbi O. Recent updates in the treatment of erythema multiforme. Medicina (B Aires) 2021;57:921. doi: 10.3390/medicina57090921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Trayes KP, Love G, Studdiford JS. Erythema multiforme: Recognition and management. Am Fam Physician. 2019;100:82–8. [PubMed] [Google Scholar]
- 15.Mtiri A, Bouslama G, Messouad NB, Abidi I, Youssef SB, Sriha B. Erythema multiforme attributable to herpes simplex virus: Clinical aspects and treatment. Case Rep Dent. 2021;2021:1–4. doi: 10.1155/2021/6692495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fan X, Luo Y, Lu J, Xu J, Chen Q, Guo H, et al. Erythema multiforme major associated with community-acquired pneumonia: Lessons from a case report. Front Pediatr. 2021;9:698261. doi: 10.3389/fped.2021.698261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Teixeira IS, Leal FS, Tateno RY, Palma LF, Campos L. Photobiomodulation therapy and antimicrobial photodynamic therapy for orofacial lesions in patients with COVID-19: A case series. Photodiagnosis Photodyn Ther. 2021;34:102281. doi: 10.1016/j.pdpdt.2021.102281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berlingieri G, Alvares CMA, Serrano RV, Palma LF, Campos L. Phototherapies for COVID-19-associated opportunistic oral infections. Photodiagnosis Photodyn Ther. 2022;37:102678. doi: 10.1016/j.pdpdt.2021.102678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rezende SB, Campos L, Palma LF, Tateno RY, Simões A, Macedo MC, da Silva RL. Antimicrobial photodynamic therapy for recurrent herpes labialis in chronic graft-versus-host disease: A case report. Photodermatol Photoimmunol Photomed. 2021;37:321–3. doi: 10.1111/phpp.12655. [DOI] [PubMed] [Google Scholar]
- 20.Kazemikhoo N, Pour SH, Nilforoushzadeh MA, Mokmeli S, Dahmardehei M. The efficacy of carbon dioxide laser debridement along with low-level laser therapy in treatment of a grade 3 necrotic burn ulcer in a paraplegic patient (a case report) J Lasers Med Sci. 2019;10:338–41. doi: 10.15171/jlms.2019.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vahdatinia F, Gholami L, Karkehabadi H, Fekrazad R. Photobiomodulation in endodontic, restorative, and prosthetic dentistry: A review of the literature. Photobiomodul Photomed Laser Surg. 2019;37:869–86. doi: 10.1089/photob.2019.4707. [DOI] [PubMed] [Google Scholar]
- 22.Nissen T, Wynn R. The clinical case report: A review of its merits and limitations. BMC Res Notes. 2014;7:264. doi: 10.1186/1756-0500-7-264. [DOI] [PMC free article] [PubMed] [Google Scholar]


