Abstract
Background:
In Iran, the primary healthcare system is the front-line for society’s encounter with healthcare. Health planners aim to enhance quality and administer an accreditation program. This study examined program administration prerequisites through systematic review and meta-synthesis.
Methods:
We conducted a systematic review and meta-synthesis of qualitative literature using Thomas and Hudson’s framework. Peer-reviewed papers were searched in Scopus, PubMed, Web of Science, Google, and Google Scholar up to 2023.
Results:
The search found 1308 articles, with 37 relevant ones selected for review. Data extraction included setting, participants, study design, data collection, analysis, and themes. Thirteen qualitative subthemes were identified and were categorized under three elements of the Donabedian model.
Conclusion:
Before implementing a plan, it is crucial to consider its executive prerequisites. Revision and trial-and-error approaches can be costly and time-consuming, potentially hindering the plan’s effectiveness and diverting organizations from their primary goal, leading to failure.
Keywords: Prerequisites, Accreditation, Primary healthcare
Introduction
Primary healthcare is crucial for accessible healthcare for all. These services contribute to better healthcare outcomes, performance, social justice, equity, lower mortality rates, increased life expectancy, and a healthier population (1, 2). Quality improvement is pivotal in delivering primary healthcare. Measuring primary healthcare functions and quality is a global challenge (3).
Accreditation assesses quality independently through development programs. It involves multiple assessment processes for functions, organizations, and healthcare networks. The program follows checkpoints of measurement, assessment, evaluation, and auditing (4, 5). It is a comprehensive program worldwide, tailored to economic, social, local, cultural, and technological factors and national laws (6).
Many countries lack consistent systems for accrediting primary healthcare facilities, hindering quality improvement. Policymakers and beneficiaries prioritize adjustments in primary healthcare. The importance of enhancing and reinforcing PHC gained attention, especially considering the increasing prevalence of non-contagious diseases in the region (7). Consequently, assessment and quality improvement in PHC are now high-priority measures in many EMRO countries. Bahrain and Qatar have implemented accreditation programs for their PHC systems (2, 8).
Considering the WHO’s advice on healthcare facility accreditation and quality checks (9), implementing this program will face initial challenges due to its novelty and deficient administration in many countries, including Iran. Systematic measures in PHC accreditation are yet to be taken, making upcoming challenges unknown to enforcers and prerequisites unclear. We aimed to improve program implementation by identifying and assessing prerequisites.
Methods
This study was conducted as a systematic review and meta-synthesis aiming to identify and evaluate the requirements for the execution of the accreditation program for PHC facilities. This review evaluates and interprets the results of published qualitative studies on primary healthcare accreditation program prerequisites. The thematic synthesis as described by Bondas and Hall (10) and Thomas and Harden (11) was used to identify relevant literature for inclusion, critical appraisal, data extraction, analysis and synthesis of findings.
Search strategy and study selection
For the systematic review, keywords on accreditation and primary healthcare were searched in Scopus, PubMed, Web of Science, Google, and Google Scholar (up to 2023). English papers and reports were included, while exclusion criteria were non-descriptive sources on primary healthcare accreditation, non-English sources, and sources without full-text access.
The search strategy involved systematic use of English keywords in various combinations. General keywords used were (Accreditation OR Evaluate OR assess) AND (Primary AND Healthcare) AND Challenges AND (Policy OR Program OR Plan) AND Prerequisites.
Quality appraisal
The Critical Appraisal Skills Program (CASP, http://www.casp-uk.net/) was used to assess the 37 articles included in the analysis. Based on the research method and accuracy, none of the selected final articles was excluded from the study. Meta-synthesis
Thomas and Harden’s (11) approach was used for thematic synthesis in a three-step process: first, free-line coding in the texts, highlighting and naming conditional citations; second, identifying descriptive themes by categorizing quotes and adding identified themes until all are included using a tree structure; and thirdly, descriptive analytical headings from tree structures identified and synthesized under the three general themes (fields) of Donabedian Model (12): structure, process and outcome.
The three reviewers (S.E, R.D, M.H) discussed and reached a consensus supported by original data. A fourth team member (A.B.) reviewed the final themes. Topic disagreements were resolved through team meetings, resulting in a consensus. M.M conducted the final review, editing the themes, sub-themes, and the article text.
Results
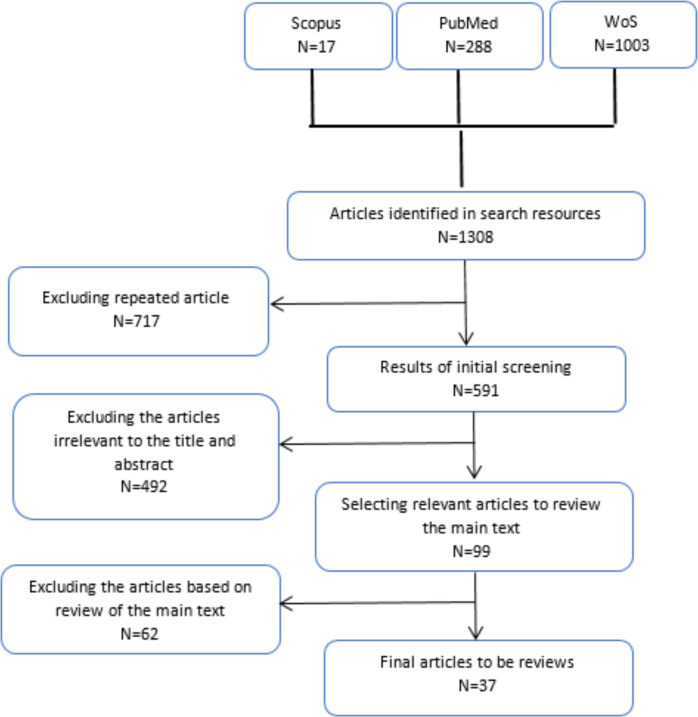
According to Fig. 1, 1308 articles were identified in search resources, and of these, the researchers studied 37 related documents including one report and 36 articles. The bibliographic information of the articles is shown in Table 1.
Fig. 1:
The selection of the articles was made according to the following PRISMA flow diagram
Table 1:
A summary of characteristics of included studies
| N. | First author | Document language | Country | Purpose of the study |
|---|---|---|---|---|
| 1 | Y Shaymaa(13); | English | Saudi Arabia | This study aimed to explore lessons for KSA from countries with implemented accreditation programs for PHCs. |
| 2 | JS.Tabrizi(14); | English | I.R Iran | This study aimed to develop a national accreditation model for primary healthcare in Iran, focusing on family practice. |
| 3 | QAL Saffer(15); | English | Saudi Arabia | Reviewing primary healthcare’s current state to guide policymakers and examining service distribution, infrastructure, and the primary healthcare workforce. |
| 4 | T. Drud Due (22); | English | Denmark | Assessing general practitioners and primary healthcare providers’ performance and understanding of accreditation standards, while providing solutions to enhance their awareness. |
| 5 | MB Kousgaard (27); | English | Denmark | Reviewing the experience of GPs and staff affected by mandatory accreditation in Denmark. |
| 6 | JS Tabrizi (16); | English | I.R Iran | Review the most appropriate accreditation models in PHC. |
| 7 | C Van Weel (17); | English | EMRO | Describing and analyzing primary healthcare systems in Bahrain, Egypt, Lebanon, Qatar, Sudan, and the United Arab Emirates. |
| 8 | A Ghareeb (18); | English | Qatar | Assess changes from integrating the Canada International Accreditation Program into Qatar’s Primary Healthcare Organization. |
| 9 | N Rider (19); | English | United States | Investigate how to achieve public health standards and increase readiness for accreditation. |
| 10 | F. Gharibi (20); | English | I.R Iran | Creating a national accreditation model for health education and promotion in Iran’s PHC system |
| 11 | MG. ALRubaey (21); | English | Iraq | Assessing the impact of accreditation on primary healthcare centers’ quality of care and identifying barriers to implementing PHC center accreditation in Iraq. |
| 12 | AM Saut (22); | English | Brazil | Assessing the impact of accreditation programs on Brazilian healthcare organizations. |
| 13 | MA Alsakkak (23); | English | Saudi Arabia | Studying and evaluating the initial phase of the Central Council for Accreditation of Primary Healthcare’s activities in the PHC center accreditation cycle. |
| 14 | SD Silva (24); | English | Portugal | Use of quality management tools and practices in designing an accreditation model for primary healthcare services. |
| 15 | D Debono (25); | English | Australia | Examining stakeholders’ perspectives and experiences in general practice accreditation to identify program strengths and improvement areas. |
| 16 | M Alyahya (26); | English | Jordan | Understanding accreditation perceptions among primary public healthcare centers using institutional theory. |
| 17 | AS O’Malley (27); | English | United States | Investigating challenges in measuring the comprehensiveness of primary care team services to patients. |
| 18 | E Nouwens (28); | English | Netherlands | Identifying determinants influencing the accreditation program through primary care professionals’ experiences. |
| 19 | L Saprii (29); | English | India | Analyze the opportunities and challenges faced by social health activists and staff to play their role in rural India. |
| 20 | JS. Tabrizi (30); | English | I.R Iran | Designing a quality assessment model for primary healthcare training centers using the Delphi method |
| 21 | SM Diab (31); | English | Jordan | Investigating the impact of primary healthcare accreditation standards on care and staff satisfaction. |
| 22 | R Pineault (32); | English | Canada | Assess and describe the extent of change in primary healthcare organizations following reforms. |
| 23 | SS Saleh (33); | English | Lebanon | Evaluating accreditation as a quality improvement strategy for primary healthcare in middle- and low-income countries. |
| 24 | D. Greenfield (34); | English | Australia | Identify process, resources, and expertise for accreditation program; Review standards and implementation reports. |
| 25 | F. El-Jardali (35); | English | Lebanon | Assess PHC centers’ readiness for accreditation standards; Review challenges, activities, and strategies. |
| 26 | M. Almasabi (36); | English | Saudi Arabia | Review of quality and accreditation in the health sector in Saudi Arabia |
| 27 | R. Bailie (37); | English | Australia | Describing primary healthcare accreditation model, outcomes, challenges, and research questions. |
| 28 | O’Beirne (38); | English | Canada | Research on the current state of accreditation of primary care |
| 29 | CD Shaw (39); | English | Canada | Examining global healthcare accreditation patterns, identifying sustainability factors and quality improvement opportunities. |
| 30 | M O’Beirne (38); | English | Canada, United States, England, India, Denmark, Australia and News land | Investigating the status of implementation of accreditation program in the primary care delivery system. |
| 31 | JS. Tabrizi (40); | English | I.R Iran | Development of a national accreditation model for rural health centers in the Iranian health system |
| 32 | J Braithwaite (41); | English | Low- and middle-income countries | Investigate and describe accreditation program attributes in LMICs compared to HICs, identifying contextual factors for sustainability or barriers. |
| 33 | J. Szecsenyi (42); | English | Germany | Evaluate accreditation program effectiveness in improving primary healthcare management, focusing on quality and safety. |
| 34 | B Sibthorpe (12); | English | Australia | Provide a conceptual model for evaluating the performance of the PHC system. |
| 35 | Word Health Organization (4); | English | World Health Organization | Describes global structures and activities promoting healthcare quality, catalogs quality concepts and tools used internationally, reviews health service accreditation initiatives and analyzes national programs worldwide. |
| 36 | S A Buetow (43); | English | Australia and New Zealand | Examining the Challenges and Accreditation Lessons of General Practitioners Providing Primary Healthcare |
| 37 | E. SCRIVENS (44); | English | England | Address the issues raised in the field of quality development, review and evaluate the progress made |
After the qualitative analysis of the articles, Researchers classified the extracted codes using the inductive approach into 13 subthemes and arranged the subthemes under the three general themes (fields) of Donabedian Model (12): structure, process, and outcome (Table 2).
Table 2:
The extracted codes classified into 13 subthemes and the subthemes arranged under the three general themes
| Theme | Subthemes |
|---|---|
| Structure | Supporting and patronaging/sponsoring the program (12, 16, 20, 21, 23, 24, 26, 30, 31, 33, 35, 37, 39, 44) Providing the infrastructure (4, 12–14, 16, 20, 22, 26, 29, 34, 35, 37, 41, 42, 45) Recourse’s allocation (4, 13–15, 20–22, 25, 26, 34–39, 43, 44) Evaluator’s Features (35, 39, 43, 44) Designing Accreditation Motivational System (for Organization and Staff) (13, 25, 26, 34, 35, 37, 38, 41, 44) |
| Process | Interpretation of Knowledge (18, 35, 38) Empowering the personnel (4, 16–18, 21–23, 30, 35, 36, 38, 41, 42, 46) Justification of stakeholders (16, 17, 20, 25, 29, 30, 34, 35) Designing and assessment of accreditation’s standards (12–14, 16, 19–21, 24, 27, 28, 31–35, 38, 40, 43–45, 47) Time and duration of implementation (4, 12, 16, 18, 19, 22, 23, 27, 32–35, 38, 42, 44, 46) |
| Outcome | The result of the feedback system (28, 30, 34, 35, 43–44) Evidence-based management and decision making (14, 17, 25, 30, 34, 35, 37) The mechanism of exploiting the results (20, 22, 24, 25, 30, 34, 35, 43) |
Structure subthemes: 1) Supporting the program: Government and higher authorities’ support for accreditation. 2) Infrastructure provision: Electronic systems, equipment, and necessary supplies for facilities and the Ministry of Health and Medical Education for surveillance and continuous monitoring. 3) Resource contribution: Identifying necessary resources for program implementation. 4) Assessor characteristics: Training and education for assessors to gather and report qualitative information and evaluate facilities effectively. 5) Motivational system: Establishing a reward and punishment system to enhance performance in organizations and among personnel involved in accreditation.
Process subthemes: 1) Knowledge interpretation: Clarifying and interpreting evidence in various professional fields for administrators to make informed decisions. 2) Personnel empowerment: Providing necessary training to familiarize individuals with standards, ensuring efficient application and process improvement. 3) Beneficiary justifications: Vital for proper program execution and interaction with beneficiaries in any organization. 4) Accreditation standards: Setting standards to measure goal achievement and the gap between expected and obtained results. 5) Execution timespan estimation: Determining the time-line for notifying facilities about measurements, executing the accreditation program, and conducting necessary assessments.
Outcome subthemes: 1) Feedback system: Necessary to assess program impacts and determine needed changes. 2) Evidence-based administration: Important for making suitable decisions that align with the situation. 3) Utilizing accreditation results: Beneficial for assessed facilities and higher authorities in developing accurate and realistic policies.
Discussion
The study examines prerequisites for administering the program through a systematic review. The accreditation program requires necessities for enforcement and success. In its simplest form, quality improvement programs include structure, process, outcome (48). Structural factors are vital for program success. Program initiation without them is nearly impossible. Success relies on higher authorities’ support, which guarantees program execution. Initially, low-rank authorities resist program administration, but with support from higher authorities and executives, this issue is resolved. Studies confirm that financial support is crucial (36, 49).
Studies confirm that quality enhancement is an ongoing task (50, 51). Based on accreditation experiences in healthcare and education, accreditation should not be limited to short-term assessments. Instead, integrated facilities should regularly report quality issues to higher authorities. Continuous evaluations are also essential. Quality enhancement projects can be conducted without extra expenses. However, for an accreditation program, proper financial support and a flexible budget are necessary. Financial support is a significant factor in the accreditation program, as mentioned in other studies (17, 52).
To accredit facilities, assessors are essential. As highlighted in previous studies (53–55), assessors play a fundamental role in hospital accreditation, and their performance significantly affects result validity. The properties and characteristics of assessors are crucial for an accurate and unbiased assessment. Program assessment and evaluation affect success rates in achieving goals. Training individuals with sufficient knowledge and professional ethics to scrutinize quality aspects is crucial. Assessors’ technical, perceptual, and personal competence must be confirmed before program execution.
Another factor in program design is the regulatory system, which serves as the program’s reward and punishment mechanism. The regulator’s performance quality should be considered, with measures in place to reward or punish organizations based on their performance. Previous studies highlight the significance of this issue and recommend using the reward and punishment system for continuous quality improvement, preventing decline, and deterring low-quality services (26, 35, 56, 57). The regulatory can be financial or nonfinancial, applied at an organizational or individual level, emphasizing its importance.
Reduce the number of words in the following text without changing its meaning (57, 58), facilities and organizations have become specialized, with professionals working in their respective fields. This is also true for healthcare organizations, where personnel continuously generate evidence and experiences for future decision-making. However, administrators face challenges in thoroughly reviewing and considering all the produced evidence and research due to technical issues and time constraints. Therefore, having sufficient human resources, either as individuals or as a dedicated department, to provide advice, summarize, and simplify the evidence and feedback from personnel in different fields is crucial. Empowering human resources is another process-related issue. Achieving quality goals requires the efforts of administrators, up-to-date technologies, and active participation from all organization personnel. Personnel assistance is essential for quality improvement and adherence to standards. This highlights the importance of attending to this group within an organization, as emphasized in other studies and various sources (16, 18, 35, 59).
Considering beneficiaries is vital for success and goal achievement in healthcare facilities. Government-run healthcare facilities aim to provide healthcare services to members of society, involving various internal and external beneficiaries. These include human resources, healthcare-related individuals and organizations, and entities contributing to healthcare infrastructure (e.g., law enforcement, municipalities, county offices, Red Crescent, etc.). Studies emphasize the importance of earning the approval and support of beneficiaries (60, 61). Organizations strive to provide the best means of earning support, reducing potential threats and resistance.
Setting proper, clear, valid, and complete standards is a fundamental process-related issue in every system. These standards should analyze all qualitative aspects according to the assessment program goals. They must be valid, reliable, and flexible enough to accommodate new needs (16, 35). Inadequate standard design results in time and cost implications, requiring redesign and re-instruction of facilities and assessors. Hence, designing and setting standards is highly important. Accreditation standards should be localized, suitable for the health department and country conditions, agreed upon by all parties, and prioritize aspects to differentiate between facilities with different capabilities.
In the accreditation program for integrated primary healthcare facilities, it is crucial to provide sufficient time for facilities to apply standards, complete measurements, and prepare for comprehensive accreditation (62, 18). The assessment process should be carefully planned to cover all qualitative factors, such as services, expenses, and accounting. Consideration should be given to the fiscal year and workload of facilities during the accreditation period. Encouraging continuous internal audits and institutionalizing the practice of continuous quality improvement is preferable to avoid last-minute efforts to meet annual accreditation criteria.
Feedback is a crucial factor mentioned in various studies. It provides corrective responses and opportunities for learning and change to both the giving and receiving organizations. Feedback aids the Ministry of Health in improving performance, increasing responsibility, and enhancing management. It is also necessary for revising standards (16). Additionally, feedback helps facilities identify weaknesses, implement measures for improvement, enhance staff understanding of their roles in quality improvement, make changes to their duties, identify educational needs, and take action to improve themselves.
Administration and evidence-based decision-making are crucial outcome factors. Evidence-based decision-making revolutionizes management by utilizing clear, efficient, and tested rationalization. It enables administrators to make accurate decisions, standardize facilities, and plan future actions for the accreditation program. Efficient utilization of program results, gathering data on program shortcomings and advantages, and using the information for further development and quality enhancement are essential. This ensures that assessed facilities, as the frontline of society’s healthcare system, operate optimally.
Conclusion
Continuous quality improvement is a significant concern in the healthcare system. Managers and administrators have always been interested in quality control and assessment. The accreditation program systematically evaluates the application of standards and service quality using predetermined parameters. In the field of health and primary healthcare, this system is relatively new and requires further research. Sufficient time is necessary for tasks such as planning, execution, receiving feedback, and learning from other professional fields and regions/countries. This study aimed to guide planners and administrators by examining accreditation program prerequisites based on international studies and activities. It also provides the necessary knowledge to enhance the program’s effectiveness and efficiency.
Journalism Ethics considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
This research did not receive any grant. This article is the result of the first phase of the Master’s thesis, carried out under the code of ethics “IR.KMU.REC.1400.390” in the Faculty of Management and Medical Information at Kerman University of Medical Sciences.
Footnotes
Conflict of interests
None to declare.
References
- 1.Al Rashidi B, Al Wahaibi AH, Mahomed O, et al. (2020). Assessment of Key Performance Indicators of the Primary Health Care in Oman: A Cross-Sectional Observational Study. J Prim Care Community Health, 11:2150132720946953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Glazier R, North American Primary Care Research Group (2008). Mapping the future of primary healthcare research in Canada. Ann Fam Med, 6(1): 89–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Desta BF, Azeb A, Ismael BA, et al. (2020). Leadership, governance and management for improving district capacity and performance: the case of USAID Transform: Primary Health Care. BMC Fam Pract, 21 (1):252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization (2003). Quality and accreditation in health care services: a global review. [Google Scholar]
- 5.Shaw C. (2004). The external assessment of health services. World Hosp Health Serv, 40 (1):24–7, 50, 51. [PubMed] [Google Scholar]
- 6.Bahadori M, Ravangard R, Alimohammadzadeh K. (2015). The accreditation of hospitals in Iran. Iran J Public Health, 44 (2): 295–96. [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization (2008). The world health report 2008: primary health care now more than ever. Available from: https://www.who.int/director-general/speeches/detail/primary-health-care---now-more-than-ever
- 8.World Health Organization (2010). The world health report: health systems financing: the path to universal coverage: executive summary. [DOI] [PMC free article] [PubMed]
- 9.EMRO, W (2015). Expert consultation on improving the quality of care at primary health care level through the implementation of quality indicators and standards. Summary report.
- 10.Bondas T, Hall EO. (2007). Challenges in approaching metasynthesis research. Qual Health Res, 17 (1):113–21. [DOI] [PubMed] [Google Scholar]
- 11.Thomas J, Harden A. (2008). Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol, 8:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sibthorpe B, Gardner K. (2007). A conceptual framework for performance assessment in primary health care. Aust J Prim Health, 13 (2):96–103. [Google Scholar]
- 13.Alotaibi S. Y. (2023). Accreditation of primary health care centres in the KSA: Lessons from developed and developing countries. J Taibah Univ Med Sci, 18(4): 711–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tabrizi JS, Gharibi F. (2021). Developing national functional accreditation model for primary healthcares with emphasis on family practice in Iran. Korean J Fam Med, 42 (3):232–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Al Saffer Q, Al-Ghaith T, Alshehri A, et al. (2021). The capacity of primary health care facilities in Saudi Arabia: infrastructure, services, drug availability, and human resources. BMC Health Serv Res, 21 (1):365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tabrizi JS, Gharibi F. (2019). Primary healthcare accreditation standards: a systematic review. Int J Health Care Qual Assur, 32(2): 310–20. [DOI] [PubMed] [Google Scholar]
- 17.Van Weel C, Alnasir F, Farahat T, et al. (2018). Primary healthcare policy implementation in the Eastern Mediterranean region: Experiences of six countries. Eur J Gen Pract, 24 (1):39–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ghareeb A, Said H, El Zoghbi M. (2018). Examining the impact of accreditation on a primary healthcare organization in Qatar. BMC Med Educ, 18 (1):216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rider N, Frazier CM, McKasson S, et al. (2018). Achieving public health standards and increasing accreditation readiness: findings from the National Public Health Improvement Initiative. J Public Health Manag Pract, 24 (4):392–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gharibi F, Tabrizi JS. (2018). Development of an accreditation model for health education and promotion programs in the Iranian primary healthcare system: a Delphi study. Health Promot Perspect, 8 (2):155–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.ALRubaey MG, Farhan AR, Kadhem HJ. (2018). The impact of accreditation of primary healthcare centers on quality of care as perceived by healthcare providers and directors in Baghdad. Iraqi J Community Med, 31(1): 1–5. [Google Scholar]
- 22.Saut AM, Berssaneti FT, Moreno MC. (2017). Evaluating the impact of accreditation on Brazilian healthcare organizations: a quantitative study. Int J Qual Health Care, 29 (5):713–21. [DOI] [PubMed] [Google Scholar]
- 23.Alsakkak MA, Alwahabi SA, Alsalhi HM, et al. (2017). Outcome of the first Saudi Central Board for Accreditation of Healthcare Institutions (CBAHI) primary health care accreditation cycle in Saudi Arabia. Saudi Med J, 38 (11):1132–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Silva SD, Fonseca A. (2017). Portuguese primary healthcare–sustainability through quality management. Int J Qual Reliab Manag, 34(2), 251–64. [Google Scholar]
- 25.Debono D, Greenfield D, Testa L, et al. (2017). Understanding stakeholders’ perspectives and experiences of general practice accreditation. Health Policy, 121 (7):816–22. [DOI] [PubMed] [Google Scholar]
- 26.Alyahya M, Hijazi H, Harvey H. (2018). Explaining the accreditation process from the institutional isomorphism perspective: a case study of Jordanian primary healthcare centers. Int J Health Plann Manage, 33 (1):102–20. [DOI] [PubMed] [Google Scholar]
- 27.O’Malley AS, Rich EC. (2015). Measuring comprehensiveness of primary care: challenges and opportunities. J Gen Intern Med, 30 Suppl 3(Suppl 3):S568–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nouwens E, Van Lieshout J, Wensing M. (2015). Determinants of impact of a practice accreditation program in primary care: a qualitative study. BMC Fam Pract, 16:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Saprii L, Richards E, Kokho P, et al. (2015). Community health workers in rural India: analysing the opportunities and challenges Accredited Social Health Activists (ASHAs) face in realising their multiple roles. Hum Resour Health, 13:95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tabrizi J-S, Farahbakhsh M, Shahgoli J, et al. (2015). Designing excellence and quality model for training centers of primary health care: a Delphi Method study. Iran J Public Health, 44 (10):1367–75. [PMC free article] [PubMed] [Google Scholar]
- 31.Diab SM. (2015). The Effect of Primary Health Accreditation Standards on the Primary Health Care Quality and Employees Satisfaction in the Jordanian Health Care Centers. Int J Acad Res Bus Soc Sci, 5 (4):157–63. [Google Scholar]
- 32.Pineault R, Da Silva RB, Prud’homme A, et al. (2014). Impact of Québec’s healthcare reforms on the organization of primary healthcare (PHC): a 2003–2010 follow-up. BMC Health Serv Res, 14: 229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Saleh SS, Alameddine MS, Natafgi NM. (2014). Beyond accreditation: a multi-track quality-enhancing strategy for primary health care in low-and middle-income countries. Int J Health Serv, 44 (2):355–72. [DOI] [PubMed] [Google Scholar]
- 34.Greenfield D, Civil M, Donnison A, et al. (2014). A mechanism for revising accreditation standards: a study of the process, resources required and evaluation outcomes. BMC Health Serv Res, 14: 571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.El-Jardali F, Hemadeh R, Jaafar M, et al. (2014). The impact of accreditation of primary healthcare centers: successes, challenges and policy implications as perceived by healthcare providers and directors in Lebanon. BMC Health Serv Res, 14:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Almasabi12 MH. (2013). An overview of quality and accreditation in the health sector within Saudi Arabia. Int J Health Res Innov, 1 (3): 1–5. [Google Scholar]
- 37.Bailie R, Matthews V, Brands J, et al. (2013). A systems-based partnership learning model for strengthening primary healthcare. Implement Sci, 8:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.O’Beirne M, Zwicker K, Sterling PD, et al. (2013). The status of accreditation in primary care. Qual Prim Care, 21 (1):23–31. [PubMed] [Google Scholar]
- 39.Shaw CD, Braithwaite J, Moldovan M, et al. (2013). Profiling health-care accreditation organizations: an international survey. Int J Qual Health Care, 25 (3):222–31. [DOI] [PubMed] [Google Scholar]
- 40.Tabrizi JS, Gharibi F, Pirahary S. (2013). Developing of national accreditation model for rural health centers in Iran health system. Iran J Public Health, 42 (12):1438–45. [PMC free article] [PubMed] [Google Scholar]
- 41.Braithwaite J, Shaw CD, Moldovan M, et al. (2012). Comparison of health service accreditation programs in low-and middle-income countries with those in higher income countries: a cross-sectional study. Int J Qual Health Care, 24 (6):568–77. [DOI] [PubMed] [Google Scholar]
- 42.Szecsenyi J, Campbell S, Broge B, et al. (2011). Effectiveness of a quality-improvement program in improving management of primary care practices. CMAJ, 183 (18):E1326–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Buetow S, Wellingham J. (2003). Accreditation of general practices: challenges and lessons. Qual Saf Health Care, 12 (2):129–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Scrivens E. (1998). Widening the scope of accreditation–issues and challenges in community and primary care. Int J Qual Health Care, 10 (3):191–97. [DOI] [PubMed] [Google Scholar]
- 45.Kousgaard MB, Thorsen T, Due TD. (2019). Experiences of accreditation impact in general practice–a qualitative study among general practitioners and their staff. BMC Fam Pract, 20 (1):146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Al-Mhasnah A, Salleh F, Afthanorhan A, et al. (2018). The relationship between services quality and customer satisfaction among Jordanian healthcare sector. Manag Sci Lett, 8 (12):1413–20. [Google Scholar]
- 47.Due TD, Thorsen T, Kousgaard MB. (2019). Understanding accreditation standards in general practice–a qualitative study. BMC Fam Pract, 20 (1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McCullough K, Andrew L, Genoni A, et al. (2023). An examination of primary health care nursing service evaluation using the Donabedian model: A systematic review. Res Nurs Health, 46(1):159–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yassoub R, Hashimi S, Awada S, et al. (2014). Responsiveness of Lebanon’s primary healthcare centers to non-communicable diseases and related healthcare needs. Int J Health Plann Manage, 29 (4):407–21. [DOI] [PubMed] [Google Scholar]
- 50.Ettorchi-Tardy A, Levif M, Michel P. (2012). Benchmarking: a method for continuous quality improvement in health. Healthc Policy, 7 (4):e101–19. [PMC free article] [PubMed] [Google Scholar]
- 51.Shortell SM, O’Brien JL, Carman JM, et al. (1995). Assessing the impact of continuous quality improvement/total quality management: concept versus implementation. Health Serv Res, 30 (2):377–401. [PMC free article] [PubMed] [Google Scholar]
- 52.Van Weel C, Kassai R, Qidwai W, et al. (2016). Primary healthcare policy implementation in South Asia. BMJ Glob Health, 1 (2):e000057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jaafaripouyan E, Mosadeghrad A, Salarvand A. (2018). Performance of accreditation surveyors in Tehran hospitals: Strengths and weaknesses. Journal of Hospital, 17 (3):31–43 [In Persian] [Google Scholar]
- 54.Mosadeghrad A, Shakibaei E. (2017). Hospital accreditation implementation prerequisites. Journal of Hospital, 16 (3):43–45 [In Persian] [Google Scholar]
- 55.Mosadeghrad AM, Yousefinezhadi T. (2019). Evaluation of hospital accreditation implementation in Iran. Payesh (Health Monitor), 18 (1):23–35. [In Persian]. [Google Scholar]
- 56.Santoso KA, Dewi A. (2020). Differences in the Level of Understanding Patient Safety in the Accredited and Not Accredited Primary Healthcare Facilities. Int J Sci Healthc Res, 5 (4):338–42. [Google Scholar]
- 57.Straus SE, Tetroe J, Graham I. (2009). Defining knowledge translation. CMAJ, 181 (3–4):165–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Straus S, Tetroe J, Graham ID. (2013). Knowledge translation in health care: moving from evidence to practice. 2nd ed. John Wiley & Sons. [Google Scholar]
- 59.Hemadeh R, Kdouh O, Hammoud R, et al. (2020). The primary healthcare network in Lebanon: a national facility assessment. East Mediterr Health J, 26 (6): 700–707. [DOI] [PubMed] [Google Scholar]
- 60.de Brún T, O’Reilly-de Brún M, van Weel-Baumgarten E, et al. (2017). Using Participatory Learning & Action (PLA) research techniques for inter-stakeholder dialogue in primary healthcare: an analysis of stakeholders’ experiences. Res Involv Engagem, 3:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Norman WV, Dunn S, Guilbert E, et al. (2011). Developing a National Family Planning Primary Healthcare Research Program: Opportunities and Priorities Identified through Stakeholder and Expert Consultations. Vancouver : University of British Columbia Library.
- 62.Al Tehewy M, Salem B, Habil I, et al. (2009). Evaluation of accreditation program in nongovernmental organizations’ health units in Egypt: short-term outcomes. Int J Qual Health Care, 21 (3):183–9. [DOI] [PubMed] [Google Scholar]