Abstract
BACKGROUND
Early venous drainage is a critical diagnostic feature of arteriovenous malformations (AVMs) and arteriovenous fistulas (AVFs). However, other conditions associated with early venous drainage can mimic AVMs and AVFs and mislead the treating physician team.
OBSERVATIONS
The authors present a unique case of a 56-year-old man with new left hemianopsia. Workup with magnetic resonance imaging and magnetic resonance angiography had revealed cortical enhancement and early venous drainage, possibly caused by an AVF or AVM. Catheter angiography confirmed the presence of early venous drainage of specifically the right occipital lobe. The early venous drainage occurred as the result of local hyperperfusion limited to the right occipital lobe. Subsequent electroencephalography confirmed focal seizure activity in the right occipital lobe. After seizure control with multiple antiepileptic medications, the patient regained his vision. Repeat digital subtraction angiography revealed restoration of normal cerebral blood flow.
LESSONS
Early venous drainage observed during catheter angiography can be associated with seizure activity. Differentiation from other conditions, such as AVM, AVF, or ischemic stroke, is critical to facilitate prompt and appropriate treatment.
Keywords: focal seizure, early venous drainage, hyperperfusion, EEG, DSA, hemianopsia
ABBREVIATIONS: AVF = arteriovenous fistula, AVM = arteriovenous malformation, DSA = digital subtraction angiography, EEG = electroencephalography, MRI = magnetic resonance imaging, SPECT = single-photon emission computed tomography
Early venous drainage is one of the diagnostic cornerstones of arteriovenous malformations (AVMs) and arteriovenous fistulas (AVFs).1,2 However, other conditions associated with early venous drainage can mimic AVMs and AVFs and mislead the treating physician team. We report a unique case of a patient in whom angiography was performed while the patient was symptomatic from a focal seizure. Digital subtraction angiography (DSA) and electroencephalography (EEG) findings were correlated.
Illustrative Case
Clinical Presentation
A 56-year-old man presented with left homonymous hemianopsia for 1 week associated with intense headaches. The patient had no self- or family-reported history of recent seizures, although the patient admitted to a similar episode 4 years prior. Workup at another hospital had included contrast-enhanced magnetic resonance imaging (MRI) of the brain, which revealed abnormal cortical right occipital lobe enhancement. Magnetic resonance angiography showed an occipital vein with arterialized signal. The patient was referred for catheter angiography and treatment of a possible dural AVF.
Catheter Angiography
Diagnostic cerebral angiography by DSA was performed with the patient under moderate sedation via right radial artery access. Injections of the right common carotid artery revealed engorged parietal middle cerebral artery branches. The capillary phase of the occipital lobe occurred early, ahead of all other lobes. This was followed by early venous drainage off the occipital lobe, ahead of all remaining vascular territories (Fig. 1). Drainage was via the normal superficial and tentorial veins. Of note, the physiological sequence of arterial to capillary to venous phase was preserved, just accelerated. No nidus or fistulous connections were identified. Instead, the findings were consistent with focal hyperperfusion of the right occipital lobe with the presence of “early” venous drainage.
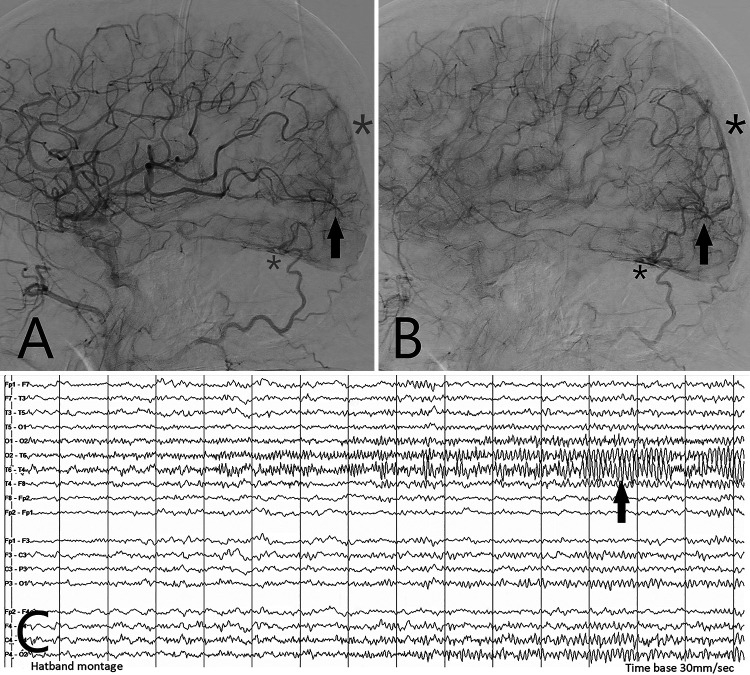
FIG. 1.
Images illustrating the correlation among cerebral hyperperfusion, early venous drainage, and focal seizure activity. A patient with hemianopsia underwent a right common carotid artery DSA (lateral views). During the midarterial phase (A), engorged parietal middle cerebral arteries can be appreciated. Note early capillary hyperperfusion centered on the occipital lobe (arrow). A hint of early venous drainage is already apparent (faint asterisks). In the late arterial phase (B), the early venous drainage is clearly visible (solid asterisks). The main draining veins include occipital surface veins superiorly (large asterisks) and tentorial veins inferiorly (small asterisks). Corresponding surface EEG (C) shows maximum synchronized waves in leads T6 (right posterior temporal) and O2 (right occipital), consistent with a focal occipital lobe seizure. After seizure control with multiple antiepileptic agents, the patient regained his vision, and his cerebral blood flow returned to normal, confirmed by repeat catheter angiography.
Electroencephalography
After further prompting, the patient then recalled occasional flashes of light in his left visual field. The waxing and waning nature of these symptoms raised the possibility of seizures. Continuous EEG monitoring was initiated while the patient was both awake and asleep. The EEG was significant for right-sided focal seizures. The seizures started as rhythmic theta wave activity with definite evolution. The seizures happened at frequencies of 1–6 per hour, each seizure lasting up to 2 minutes (Fig. 1). Occasionally, the seizures were symptomatic with head jerking and head turning to the left. However, most seizures did not have an obvious clinical correlate except for the patient’s ongoing hemianopsia.
Outcome
The patient was treated with multiple antiepileptic drugs. This resulted in resolution of the seizure activities. Concurrently, the patient recovered his vision completely. Contrast-enhanced MRI at hospital day 10 revealed significantly decreased right occipital lobe gyral enhancement compared with the first brain MRI. A second DSA study was performed with resolution of the previously seen occipital lobe abnormalities associated with the focal seizure.
Patient Informed Consent
The necessary patient informed consent was obtained in this study.
Discussion
Observations
The main observation of this report is that catheter angiography can demonstrate early venous drainage related to seizure activity without another underlying lesion. This differential diagnosis for an angiographically early draining vein is not established in the literature but is critical to recognize by the treating team of neurologists, neurosurgeons, and interventionalists alike.
Early Venous Drainage with AVM, AVF, or Stroke
Early venous drainage is generally the hallmark of AVMs or AVFs.1,2 As a result of the arteriovenous shunting, venous drainage can be seen early in the arterial phase with AVMs or AVFs. Catheter angiography remains the gold-standard test for definitive workup of these lesions. More recently, early venous drainage has increasingly been recognized in association with ischemic stroke.3 The early venous drainage can be seen around an ischemic core (“luxury perfusion”).4 Alternatively, early venous drainage can be noted during reperfusion after successful recanalization.4
Early Venous Drainage with Seizures
Seizure activity as a potential cause for early venous drainage is easily overlooked or confused with an actual arteriovenous shunt. The phenomenon is not well described in the literature. We found only one report from 1975 mentioning this possibility. McDonald et al.5 reported a case of cerebral hypervascularity and early venous opacification in a patient with status epilepticus. The patient died. The absence of an underlying lesion was confirmed by autopsy. In our case, we observed focal hyperperfusion limited to the occipital lobe, the focus of the seizure. Venous drainage of the occipital lobe occurred early relative to all other areas of the brain.
Cerebral Perfusion Abnormalities with Seizures
The association between cerebral hyperperfusion and epilepsy has been documented more clearly. A cohort of 51 children with epilepsy monitored with transcranial Doppler sonography demonstrated a positive correlation between arterial flow dynamics, including both hyperperfusion and hypoperfusion.6 These flow changes depended on the type of seizure. Tonic-clonic seizures showed hyperperfusion with blood flow increases to nearly 200% of baseline. Absence seizures were linked to hypoperfusion down to about 70% of baseline.
Laich et al.7 evaluated clinical signs, EEG studies, and ictal cerebral blood flow by single-photon emission computed tomography (SPECT). Ictal SPECT showed unilateral predominance of hyperperfusion of the sensorimotor area in all patients, concordant with lateralizing clinical signs, lateralization of ictal scalp EEG, or the site of ictal onset of seizures, obtained from intracranial electrodes. Kim et al.8 evaluated cerebral blood flow using arterial spin labeling perfusion MRI in patients with clinical seizure activity. These authors were able to predict the location of the seizure foci on the basis of perfusion abnormalities in 33 (75%) of 44 patients. Manganotti et al.9 studied 481 patients with acute neurological deficits. Eleven had seizures. Eight of the 11 patients had a similar pattern of hyperperfusion by computed tomography (CT) perfusion.
In summary, cerebral hyperperfusion can be commonly encountered during epilepsy. Angiographically, the key finding is early venous drainage relative to that of the remaining brain. The blood flow pattern does follow the physiological sequence from arterial to capillary to venous phase. This differentiates the early venous drainage associated with epilepsy from an AVF or AVM. The absence of a nidus rules out an AVM, and the presence of the capillary phase rules out an AVF.
Lessons
Early venous drainage identified by catheter angiography can also be associated with seizure activity. Differentiation from other conditions, such as AVM, AVF, or ischemic stroke, is critical to facilitate prompt and appropriate treatment.
Author Contributions
Conception and design: Hauck. Acquisition of data: all authors. Analysis and interpretation of data: Hauck, Bibawy. Drafting the article: Hauck, Holman, Bibawy. Critically revising the article: Hauck, Morgenlander. Reviewed submitted version of manuscript: Hauck, Holman, Wadi, Morgenlander. Approved the final version of the manuscript on behalf of all authors: Hauck. Statistical analysis: Hauck. Administrative/technical/material support: Hauck. Study supervision: Hauck.
References
- 1. Spetzler RF, Martin NA. A proposed grading system for arteriovenous malformations. J Neurosurg. 1986;65(4):476–483. doi: 10.3171/jns.1986.65.4.0476. [DOI] [PubMed] [Google Scholar]
- 2. Cognard C, Gobin YP, Pierot L, et al. Cerebral dural arteriovenous fistulas: clinical and angiographic correlation with a revised classification of venous drainage. Radiology. 1995;194(3):671–680. doi: 10.1148/radiology.194.3.7862961. [DOI] [PubMed] [Google Scholar]
- 3. Zaidat OO, Yoo AJ, Khatri P, et al. Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke. 2013;44(9):2650–2663. doi: 10.1161/STROKEAHA.113.001972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dorn F, Kuntze-Soderqvist A, Popp S, et al. Early venous drainage after successful endovascular recanalization in ischemic stroke — a predictor for final infarct volume? Neuroradiology. 2012;54(7):745–751. doi: 10.1007/s00234-011-0966-8. [DOI] [PubMed] [Google Scholar]
- 5. McDonald EJ, Jr, Goodman PC, Nielsen SL, Winestock DP. Cerebral hypervascularity and early venous opacification in status epilepticus. A case report. Radiology. 1975;117(1):87–88. doi: 10.1148/117.1.87. [DOI] [PubMed] [Google Scholar]
- 6. Bode H. Intracranial blood flow velocities during seizures and generalized epileptic discharges. Eur J Pediatr. 1992;151(9):706–709. doi: 10.1007/BF01957579. [DOI] [PubMed] [Google Scholar]
- 7. Laich E, Kuzniecky R, Mountz J, et al. Supplementary sensorimotor area epilepsy. Seizure localization, cortical propagation and subcortical activation pathways using ictal SPECT. Brain. 1997;120(Pt 5):855–864. doi: 10.1093/brain/120.5.855. [DOI] [PubMed] [Google Scholar]
- 8. Kim BS, Lee ST, Yun TJ, et al. Capability of arterial spin labeling MR imaging in localizing seizure focus in clinical seizure activity. Eur J Radiol. 2016;85(7):1295–1303. doi: 10.1016/j.ejrad.2016.04.015. [DOI] [PubMed] [Google Scholar]
- 9. Manganotti P, Furlanis G, Ajčević M, et al. CT perfusion and EEG patterns in patients with acute isolated aphasia in seizure-related stroke mimics. Seizure. 2019;71:110–115. doi: 10.1016/j.seizure.2019.07.005. [DOI] [PubMed] [Google Scholar]