Abstract
With advancements in both pharmacologic and non-pharmacologic treatments, significant changes have occurred in heart failure (HF) management. The previous Korean HF registries, namely the Korea Heart Failure Registry (KorHF-registry) and Korean Acute Heart Failure Registry (KorAHF-registry), no longer accurately reflect contemporary acute heart failure (AHF) patients. Our objective is to assess contemporary AHF patients through a nationwide registry encompassing various aspects, such as clinical characteristics, management approaches, hospital course, and long-term outcomes of individuals hospitalized for AHF in Korea. This prospective observational multicenter cohort study (KorHF III) is organized by the Korean Society of Heart Failure. We aim to prospectively enroll 7,000 or more patients hospitalized for AHF at 47 tertiary hospitals in Korea starting from March 2018. Eligible patients exhibit signs and symptoms of HF and demonstrate either lung congestion or objective evidence of structural or functional cardiac abnormalities in echocardiography, or isolated right-sided HF. Patients will be followed up for up to 5 years after enrollment in the registry to evaluate long-term clinical outcomes. KorHF III represents the nationwide AHF registry that will elucidate the clinical characteristics, management strategies, and outcomes of contemporary AHF patients in Korea.
Trial Registration
ClinicalTrials.gov Identifier: NCT04329234
Keywords: Heart failure, Acute heart failure, Registry, Hospitalization
INTRODUCTION
Heart failure (HF) represents a condition marked by significant morbidity and mortality rates.1,2,3,4,5) Many HF patients undergo acute decompensation episodes leading to hospitalization.6,7) Notably, HF-related hospital admissions are the primary cause of admittance in the US, Western nations, and Korea.3,8,9) Among individuals aged over 65 years, HF substantially contributes to hospitalization and mortality.10) In the United States alone, over 5.1 million individuals aged 20 years or older are affected by HF, as per the National Health and Nutrition Examination Survey.11)
With an aging society and an increasing prevalence of HF risk factors in Korea, the HF prevalence surged from 0.77% in 2002 to 2.24% in 2018, amounting to 1.16 million patients.3) Understanding HF is crucial for its effective management, prompting continuous efforts to acquire epidemiologic data on HF in Korea. Presently, there are two representative HF registries,12,13) each conducted every 10 years. The most recent, the Korean Acute Heart Failure (KorAHF) registry, enrolled 5,625 consecutive acute heart failure (AHF) patients from 10 centers in Korea between 2011 and 2014. Concerns arose regarding the limited participation of high-volume centers in these registries, potentially leading to selection bias. Furthermore, with the evolution of HF guidelines and the introduction of new pharmacological and non-pharmacological treatments,5,14,15,16) the previous registries did not capture these advancements.
The collective data from registries have revealed diverse regional characteristics among Korean HF patients, indicating improvements in guideline adherence and noteworthy enhancements in clinical outcomes over time.
Our objective is to establish the third HF registry in Korea, aiming to uncover shifts in clinical attributes, treatment methodologies, and in-hospital outcomes among Korean AHF patients over the last decade. This initiative seeks to contrast these findings with data from previous registries, providing valuable insights into the evolving landscape of HF management in Korea.
STUDY DESIGN
Overview
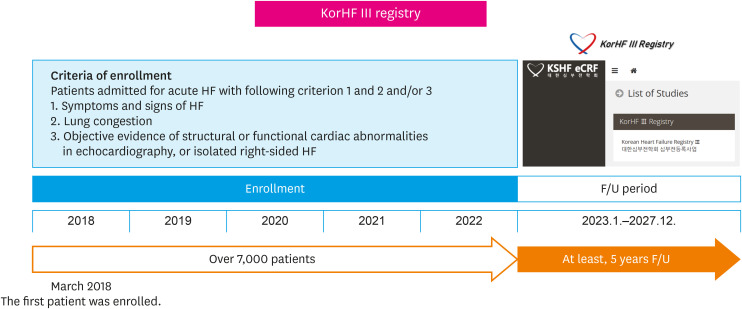
The Korean Heart Failure III (KorHF III) registry is a prospective multicenter cohort conducted across 47 tertiary hospitals in Korea (Figure 1). It aims to enroll consecutive patients admitted for acute HF, commencing in March 2018. The enrollment target is to reach 7,000 or more patients, with a follow-up period extending up to 5 years from their initial enrollment.
Figure 1. Study design of KorHF III registry.
KorHF III = Korean Heart Failure III; HF = heart failure; KSHF = Korean Society of Heart Failure; F/U = follow-up.
Study population
Patients were eligible if they exhibited symptoms and signs of HF along with lung congestion and/or objective evidence of structural or functional cardiac abnormalities in echocardiography, or if they presented with isolated right-sided HF. Lung congestion was characterized as chest radiograph congestion or the presence of rales during physical examination. Patients were classified as either having de novo HF (new-onset acute HF in a patient without previously known cardiac dysfunction) or experiencing acute decompensation of chronic HF, as per the 2021 guidelines from the European Society of Cardiology.14) The registry did not document instances of high-output HF.
Each patient’s informed consent was obtained, either directly from the patient or through a legally appointed representative in situations where the patient's condition hindered their capacity to provide consent.
Data
The attending physician utilized the Electronic Data Capture System to fill out a web-based case report form, often with the assistance of a clinical research coordinator. Baseline data, encompassing laboratory results and the initial presentation at the emergency department (ED) for patients who entered through the ED, were collected. The case report form and the definition of variables in the KorHF III registry are described in the Supplementary Table 1.
Of particular emphasis in the variable collection of the KorHF III registry, we sought to collect information on the use of angiotensin receptor-neprilysin inhibitors (ARNI) and sodium-glucose cotransporter 2 (SGLT2) inhibitors, which are relatively new drugs in HF.14,15,16) We also collected information on left ventricular assist devices, which have been increasingly utilized in Korea in recent years. In addition, we sought to collect information on the iron profile, including ferritin, serum iron and total iron binding capacity, as the diagnosis and treatment of iron deficiency in HF has been emphasized.5,17)
After discharge, the registry monitored overall mortality, mortality resulting from HF exacerbation, and readmissions due to HF exacerbation. Follow-up assessments conducted at 30 days post-discharge and then at intervals of 3, 6, 12, 24, 36, 48, and 60 months. These visits included the collection of up-to-date clinical details, biochemical markers and information on prescribed medications. Physicians acquired follow-up data directly from patients, entering them into a web-based case report system. For patients who did not have in-person follow-ups, outcome data were collected through telephone interviews.
The research protocol received approval from the ethics committees and Institutional Review Boards of all involved facilities (Seoul National University Bundang Hospital: B-1807-483-302). Comprehensive information about the study's objectives, design, and participant demographics was provided in the clinical trial registration (ClinicalTrial.gov NCT04329234). Adherence to the principles outlined in the Declaration of Helsinki was ensured throughout the study process. Funding for this study was provided by the Korean Society of Heart Failure.
Study management and data validation
Executive committee
The KorHF III registry is governed and managed by a committee comprising healthcare professionals specializing in HF. This committee was responsible for developing the study protocol and case report forms. Additionally, they oversaw all aspects pertaining to publications utilizing the aggregated database.
Data Safety Monitoring Board (DSMB)
The DSMB operates autonomously and holds responsibility for overseeing the data. They conduct evaluations by meticulously reviewing outliers in continuous variables and unexpected values in categorical variables using predefined criteria. In case of detecting any inconsistencies, the original institution is promptly contacted to verify the data. Moreover, comprehensive source document verification is carried out as an additional precautionary measure.
Clinical event committee
A distinguished clinical event committee, consisting of independent HF specialists who were not involved in patient enrollment, meticulously supervised and authenticated all clinical events, encompassing deaths (both cardiovascular and all-cause) and rehospitalizations for HF.
Variables and statistical analysis
Descriptive statistics summarized demographic and clinical characteristics, hospital care, and patient outcomes. Continuous variables were depicted as mean ± standard deviation or median with range, while categorical variables were presented as counts (percentages). Statistical significance was determined using Student’s t-test for normally distributed continuous data, Wilcoxon’s rank sum test for non-normally distributed continuous data, χ2 test, and Fisher’s exact test for categorical variables as appropriate.
To predict in-hospital all-cause mortality, we will utilize both univariable and multivariable Cox proportional hazards regression models employing backward selection. Variables demonstrating p<0.05 in the univariable analysis will be incorporated into the multivariable model. We will calculate hazard ratios with 95% confidence intervals. All analyses will be 2-sided, and statistical significance will be established at p<0.05.
DISCUSSION
HF poses significant healthcare burden due to its high morbidity and mortality rates, alongside its increasing prevalence.1,2,3,4) Understanding HF is pivotal for its effective management. To achieve this goal, numerous efforts have been made to establish multicenter registries.18) However, initial attempts began with a limited number of participating centers, resulting in regional variations in patient characteristics. More importantly, over the past 30 years, there have been significant advancements in both pharmacological and non-pharmacological therapies, leading to improved clinical outcomes for HF patients.14,15,16) Despite these advancements, concerns persist regarding the representativeness of existing registries due to their limited participating centers and the absence of updated treatment data. Thus, there arises a need for a new, comprehensive HF registry. KorHF III registry aims to illuminate the shifts in clinical attributes, treatment approaches, and in-hospital outcomes among Korean patients experiencing AHF over the past decade. Its objective is to contrast these findings with data from previous registries, intending to capture the evolving landscape of HF management.
The chronology of HF registries in Korea commenced in 1980, reflecting diverse methodologies and patient cohorts across different time frames.18) The Hallym HF registry (1987–1997, n=1,657) was a retrospective study involving 4 hospitals, providing insight into a historical cohort of HF patients.18) Following this, the Korean Multicenter HF study (1998–2003, n=1,759) offered a prospective, observational view across nine hospitals specifically focusing on AHF cases, shedding light on a different era of HF management.19) Following this, the Korean Heart Failure (KorHF) registry (2004–2009, n=3,200) emerged as a prospective multicenter registry, providing comprehensive data limited to AHF patients and offering unique insights into a specific timeframe.12) Finally, the Korean Acute Heart Failure (KorAHF) registry (2011–2014, n=5,625), supported by the Korea Centers for Disease Control and Prevention, included a broader spectrum of 10 hospitals. It continued the trend of prospective, observational approaches, representing the most recent and extensive dataset of AHF patients.13,20) Each registry signifies distinct periods and methodologies, progressively contributing to the evolving landscape of HF management in Korea. These registries highlight changes and patterns in patient characteristics, treatment strategies, and outcomes over time (Table 1).
Table 1. Differences between HF registries in Korea.
| Variables | Korean Heart Failure (KorHF) Registry | Korean Acute Heart Failure (KorAHF) Registry | Korean Heart Failure III (KorHF III) registry |
|---|---|---|---|
| Region | Korea | Korea | Korea |
| Time period | June 2004–April 2009 | March 2011–February 2014 | March 2018–ongoing |
| Number of participating hospitals | 24 | 10 | 47 |
| Sample size | 3,200 | 5,625 | Over 7,000 |
| Follow-up | Median 1.7 years | Median 4.3 years | Over 5 years |
| Male sex (%) | 50.0 | 53.2 | - |
| Age (yr) | 67.6±14.3 | 68.5±14.5 | - |
| LVEF (%) | 38.5±15.7 | 37.7±15.6 | - |
| Ischemic etiology (%) | 52.3 | 37.6 | - |
| In-hospital mortality (%) | 6.4 | 4.8 | - |
| 1-year mortality (%) | 15.0 | 18.2 | - |
HF = heart failure; LVEF = left ventricular ejection fraction.
The KorHF III registry stands as a pioneering prospective observational multicenter cohort study. Covering a cohort of more than 7,000 consecutive patients hospitalized for AHF across 47 tertiary hospitals in Korea, this registry began in March 2018 and boasts an extensive follow-up duration. Distinguished as the most contemporary HF registry, KorHF III aims to comprehensively capture patient characteristics, treatment patterns, and outcomes, providing crucial insights into HF management. This initiative is poised to offer essential data, acting as a fundamental resource for healthcare professionals and policymakers, facilitating informed decision-making processes in both healthcare and policy realms.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the KorHF III investigators; Seoul National University Hospital (Hyun-Jai Cho), Severance Cardiovascular Hospital (Seok-Min Kang), Samsung Medical Center (Jin Oh Choi), Kangnam Sacred Heart Hospital (Seonghoon Choi), Gangnam Severance Hospital (Eui-Young Choi), Kangdong Sacred Heart Hospital (Il Suk Sohn), Kangdong Sacred Heart Hospital (Dae-Gyun Park), Kangbuk Samsung Hospital (Ki-Chul Sung), Konkuk University Medical Center (Sung Hea Kim), Kyung Hee University Hospital (Hyemoon Chung), Korea University Guro Hospital (Eung Ju Kim), Korea University Anam Hospital (Seong-Mi Park), Boramae Medical Center (Myung-A Kim), Seoul St. Mary Hospital (Jong-Chan Youn), Asan Medical Center (Junho Hyun), Ewha Womans University Medical Center (Kyung-Jin Kim), Seoul, Seoul National University Bundang Hospital (Dong-Ju Choi), Seongnam, Dongtan Sacred Heart Hospital (Seong Woo Han), Hwaseong, Bucheon Sejong Hospital (Seok-Geon Hong), Bucheon St. Mary's Hospital (Sang-Hyun Ihm), Bucheon SoonChunHyang University Hospital (Min Gyu Kong), Bucheon, Ilsan Paik Hospital (Sung Woo Cho), National Cancer Center (Jae-Kyung Kim), Goyang, Pyeongchon Sacred Heart Hospital (Sang-Ho Jo), Anyang, Ajou University Hospital (Joon-Han Shin), Uijeongbu St. Mary's Hospital (Hyo-Suk Ahn), Uijeongbu, Wonju Severance Cardiovascular Hospital (Byung-Su Yoo), Wonju, Kangwon National University Hospital (Dong Ryeol Ryu), Chuncheon Sacred Heart Hospital (Kyeong-Sun Hong), Chuncheon, Gil Medical Center (Mi-Seung Shin), Incheon Sejong Hospital (Kyung-Hee Kim), Incheon St. Mary's Hospital (Mi-Jeong Kim), Inha University Hospital (Sung-Hee Shin), Incheon, Kyungpook National University (Dong Heon Yang), Dongsan Hospital (Hyung-Seop Kim), Yeungnam University Medical Center (Jong-Ho Nam), Deagu, Ulsan University Hospital (Shin-Jae Kim), Kosin University Gospel Hospital (Bong-Joon Kim), Pusan University Hospital (Jung Hyun Choi), Inje University Busan Paik Hospital (Jeong-Sook Seo), Busan, Pusan National University Yangsan Hospital (Yong-Hyun Park), Chungbuk National University Hospital (Myeong-Chan Cho), Cheongju, Chungnam National University Hospital (Jin-Ok Jeong), Daejeon, Gyeongsang National University Hospital (Seok Jae Hwang), Jinju, Chonnam National University Hospital (Kye Hun Kim), Gwangju, Jeonbuk National University Hospital (Sun Hwa Lee), Jeonju, Jeju University Hospital (Seung Jae Joo).
Footnotes
Funding: This research was funded by the Korean Society of Heart Failure and supported by Heart Failure Registry TFT.
Conflict of Interest: The authors have no financial conflicts of interest.
- Conceptualization: Kim EJ, Han SW, Park SM, Kim IC, Cho MC, Ahn HS, Shin MS, Hwang SJ, Yang DH, Kim JJ, Choi JO, Cho HJ, Yoo BS, Kang SM, Choi DJ.
- Data curation: Yoon M, Kim EJ, Han SW, Park SM, Kim IC, Cho MC, Ahn HS, Shin MS, Hwang SJ, Jeong JO, Yang DH, Kim JJ, Choi JO, Cho HJ, Yoo BS, Kang SM, Choi DJ.
- Formal analysis: Yoon M, Kim EJ, Han SW, Park SM, Kim IC, Cho MC, Ahn HS, Shin MS, Hwang SJ, Jeong JO, Yang DH, Kim JJ, Choi JO, Cho HJ, Yoo BS, Kang SM, Choi DJ.
- Funding acquisition: Cho HJ, Choi DJ.
- Investigation: Yoon M, Kim EJ, Han SW, Park SM, Kim IC, Cho MC, Ahn HS, Shin MS, Hwang SJ, Jeong JO, Yang DH, Kim JJ, Choi JO, Cho HJ, Yoo BS, Kang SM, Choi DJ.
- Methodology: Yoon M, Kim EJ, Han SW, Park SM, Kim IC, Cho MC, Ahn HS, Shin MS, Hwang SJ, Jeong JO, Yang DH, Kim JJ, Choi JO, Cho HJ, Yoo BS, Kang SM, Choi DJ.
- Project administration: Cho HJ, Choi DJ.
- Resources: Yoon M, Kim EJ, Han SW, Park SM, Kim IC, Cho MC, Ahn HS, Shin MS, Hwang SJ, Jeong JO, Yang DH, Kim JJ, Choi JO, Cho HJ, Yoo BS, Kang SM.
- Software: Yoon M.
- Supervision: Cho HJ, Choi DJ.
- Visualization: Yoon M, Choi DJ.
- Writing - original draft: Yoon M, Cho HJ.
- Writing - review & editing: Yoon M, Kim EJ, Han SW, Park SM, Kim IC, Cho MC, Ahn HS, Shin MS, Hwang SJ, Jeong JO, Yang DH, Kim JJ, Choi JO, Cho HJ, Yoo BS, Kang SM, Choi DJ.
SUPPLEMENTARY MATERIAL
Case report form and definition of variables in KorHF III registry
References
- 1.Savarese G, Becher PM, Lund LH, Seferovic P, Rosano GM, Coats AJ. Global burden of heart failure: a comprehensive and updated review of epidemiology. Cardiovasc Res. 2023;118:3272–3287. doi: 10.1093/cvr/cvac013. [DOI] [PubMed] [Google Scholar]
- 2.Ambrosy AP, Fonarow GC, Butler J, et al. The global health and economic burden of hospitalizations for heart failure: lessons learned from hospitalized heart failure registries. J Am Coll Cardiol. 2014;63:1123–1133. doi: 10.1016/j.jacc.2013.11.053. [DOI] [PubMed] [Google Scholar]
- 3.Park JJ, Lee CJ, Park SJ, et al. Heart failure statistics in Korea, 2020: a report from the Korean Society of Heart Failure. Int J Heart Fail. 2021;3:224–236. doi: 10.36628/ijhf.2021.0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee HH, Cho SM, Lee H, et al. Korea heart disease fact sheet 2020: analysis of nationwide data. Korean Circ J. 2021;51:495–503. doi: 10.4070/kcj.2021.0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cho JY, Cho DH, Youn JC, et al. Korean Society of Heart Failure guidelines for the management of heart failure: definition and diagnosis. Int J Heart Fail. 2023;5:51–65. doi: 10.36628/ijhf.2023.0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Setoguchi S, Stevenson LW, Schneeweiss S. Repeated hospitalizations predict mortality in the community population with heart failure. Am Heart J. 2007;154:260–266. doi: 10.1016/j.ahj.2007.01.041. [DOI] [PubMed] [Google Scholar]
- 7.Metra M, Tomasoni D, Adamo M, et al. Worsening of chronic heart failure: definition, epidemiology, management and prevention. A clinical consensus statement by the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2023;25:776–791. doi: 10.1002/ejhf.2874. [DOI] [PubMed] [Google Scholar]
- 8.Bui AL, Horwich TB, Fonarow GC. Epidemiology and risk profile of heart failure. Nat Rev Cardiol. 2011;8:30–41. doi: 10.1038/nrcardio.2010.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Curtis LH, Whellan DJ, Hammill BG, et al. Incidence and prevalence of heart failure in elderly persons, 1994-2003. Arch Intern Med. 2008;168:418–424. doi: 10.1001/archinternmed.2007.80. [DOI] [PubMed] [Google Scholar]
- 10.Krumholz HM, Chen YT, Wang Y, Vaccarino V, Radford MJ, Horwitz RI. Predictors of readmission among elderly survivors of admission with heart failure. Am Heart J. 2000;139:72–77. doi: 10.1016/s0002-8703(00)90311-9. [DOI] [PubMed] [Google Scholar]
- 11.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choi DJ, Han S, Jeon ES, et al. Characteristics, outcomes and predictors of long-term mortality for patients hospitalized for acute heart failure: a report from the Korean Heart Failure registry. Korean Circ J. 2011;41:363–371. doi: 10.4070/kcj.2011.41.7.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee SE, Cho HJ, Lee HY, et al. A multicentre cohort study of acute heart failure syndromes in Korea: rationale, design, and interim observations of the Korean Acute Heart Failure (KorAHF) registry. Eur J Heart Fail. 2014;16:700–708. doi: 10.1002/ejhf.91. [DOI] [PubMed] [Google Scholar]
- 14.McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42:3599–3726. doi: 10.1093/eurheartj/ehab368. [DOI] [PubMed] [Google Scholar]
- 15.Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;79:e263–e421. doi: 10.1016/j.jacc.2021.12.012. [DOI] [PubMed] [Google Scholar]
- 16.Youn JC, Kim D, Cho JY, et al. Korean Society of Heart Failure guidelines for the management of heart failure: treatment. Int J Heart Fail. 2023;5:66–81. doi: 10.36628/ijhf.2023.0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Park JJ, Yoon M, Cho HW, et al. Iron deficiency in Korean patients with heart failure. J Korean Med Sci. 2023;38:e177. doi: 10.3346/jkms.2023.38.e177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Park JJ, Choi DJ. Current status of heart failure: global and Korea. Korean J Intern Med. 2020;35:487–497. doi: 10.3904/kjim.2020.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Han SW, Ryu KH, Chae SC, et al. Multicenter analysis of clinical characteristics and prognostic factors of patients with congestive heart failure in Korea. Korean Circ J. 2005;35:357–361. [Google Scholar]
- 20.Lee SE, Lee HY, Cho HJ, et al. Clinical characteristics and outcome of acute heart failure in Korea: results from the Korean Acute Heart Failure registry (KorAHF) Korean Circ J. 2017;47:341–353. doi: 10.4070/kcj.2016.0419. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Case report form and definition of variables in KorHF III registry