Distal pancreatectomy has received relatively less attention than the eponymous Whipple operation (pancreatoduodenectomy). However, increasing attention to detail in pancreatic surgery in general, and the development of minimally invasive techniques and better appreciation of benign, premalignant, and malignant pancreatic disease entities, has changed appreciation of the details. This has resulted in the need for a more refined consideration of distal pancreatectomy—increasingly referred to as ‘left-sided pancreatectomy’. Two current studies in BJS1,2 add to the knowledge base, and come as timely additions to recently evolving evidence on optimal management in distal pancreatectomy in the Journal3–5.
Of note, although several aspects of open and minimally invasive surgery in distal pancreatectomy have been entertained, in addition to the role of drains6 and risk of postoperative fistulas7, several other questions remain unanswered. One is the definition of ‘left’ in left-sided pancreatectomy. Another is the question of what else can, or even should, be left (behind): the spleen? lymph nodes? peripancreatic tissue?
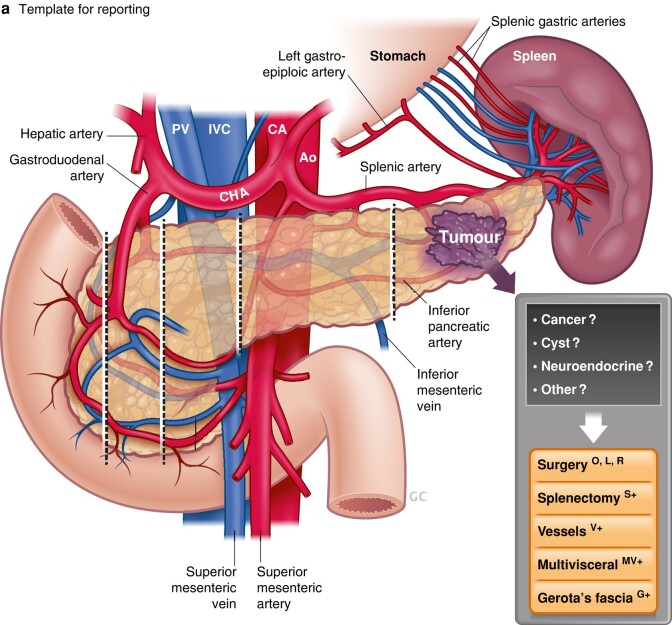
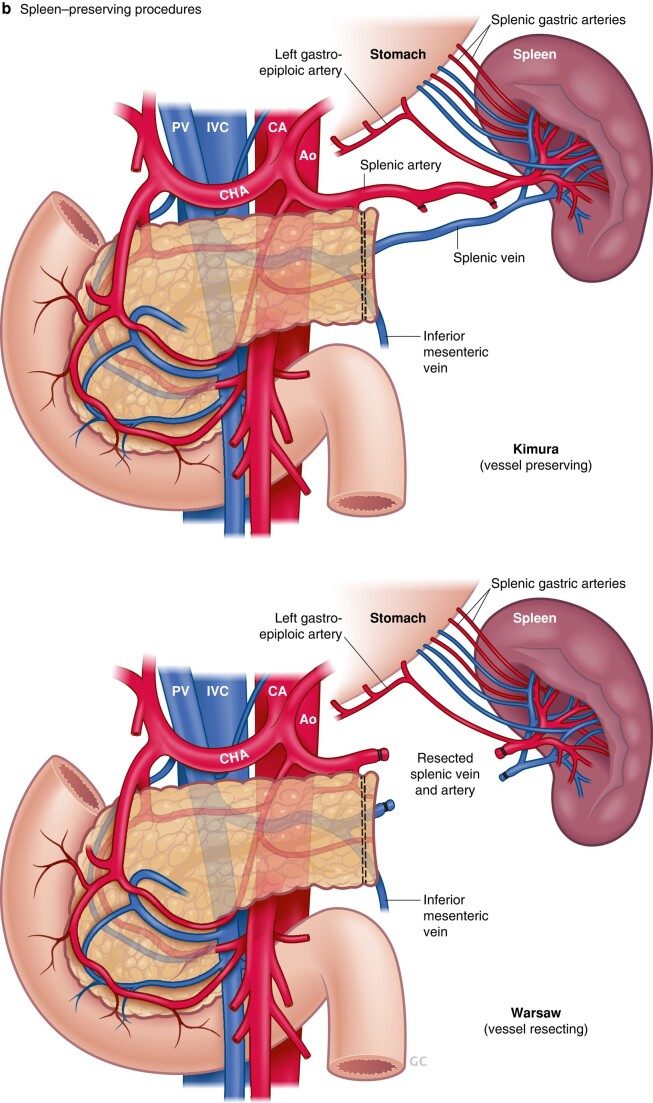
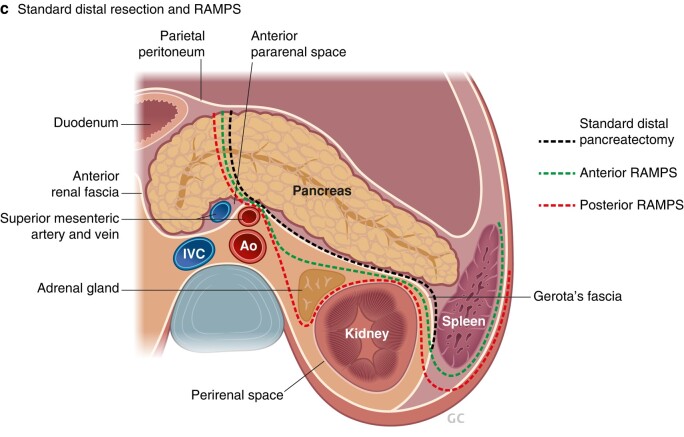
Until recently, the definition of ‘left’ in left-sided pancreatectomy has been rather undeclared. In the past, the term ‘distal pancreatectomy’ was applied to any resection from a peripheral tail resection to a subtotal pancreatectomy. However, as shown in a large single-centre study8, there is considerable risk variation depending on the extent of resection. Hence, it is timely to see the novel definition and new terminology proposed in BJS by an international Delphi consensus group on left-sided pancreatectomy1. The new proposed terminology (Fig. 1a) defines the level of division of the pancreatic gland at defined anatomical landmarks, and allows a structured report of the procedure with additional parts included, such as splenectomy (designated S+) or spleen-preserving procedure (Fig. 1b) with vessel resection (designated V+)1. Multivisceral resection is designated MV+ and resection of Gerota’s fascia G+, as included in the radical antegrade modular pancreatosplenectomy (RAMPS) procedure9 (Fig. 1c), a still much debated topic. Hence, there is an opportunity to report and compare future studies that use this definition, and relate this to endpoints and assessment of outcomes.
Fig. 1.
Novel terminology and definitions
a Lesion in distal pancreas, level of resection, and template for reporting. PV, portal vein; IVC, inferior vena cava; CA, coeliac artery; Ao, aorta; CHA, common hepatic artery. b Spleen-preserving procedures, according to Kimura or Warshaw (S+). c Standard distal resection; anterior radical antegrade modular pancreatosplenectomy (RAMPS), which includes resection of Gerota’s fascia (S+ G+); and posterior RAMPS, also including adrenal gland (S+ G+ MV).
Of note, the splenic vessels are not considered as part of ‘borderline’ or ‘locally advanced’ definitions in pancreatic cancer for tumours located in the body or tail10, even though cancers in this region also may be subject to more complex resectional procedures11. A lack of ‘borderline’ resectable terminology may also contribute to a lower likelihood of such tumours being considered for neoadjuvant chemotherapy, despite being associated with higher recurrence and lower survival rates10.
A second recurring discussion concerns the spleen, as this has commonly been considered as a part of a distal pancreatectomy, often en passant rather than according to indication, and with considerable variation in splenic salvage rates between institutions12. One reason for doing splenectomy routinely, rather than attempting a spleen-preserving procedure (Fig. 1b), may have been technical difficulties in dissection off the splenic vessels, particularly as practised in laparoscopic surgery. However, spleen preservation avoids the need for postsplenectomy vaccinations and the life-long increased infection risk. The introduction of robotically assisted minimally invasive surgery may facilitate spleen preservation, as demonstrated in one large study13 that showed higher spleen preservation rates (81% for robotic versus 63% laparoscopic procedures; P = 0.001). The spleen can be left after distal pancreatectomy by either sparing all the splenic vessels (Kimura procedure) or, even if the splenic vessels are difficult to dissect free (embedded in the pancreatic tissue, or involved by the tumour), by dividing and resecting the vessels (new terminology S+) and relying on the remaining blood flow from the gastrosplenic arteries (Warshaw procedure) (Fig. 1b).
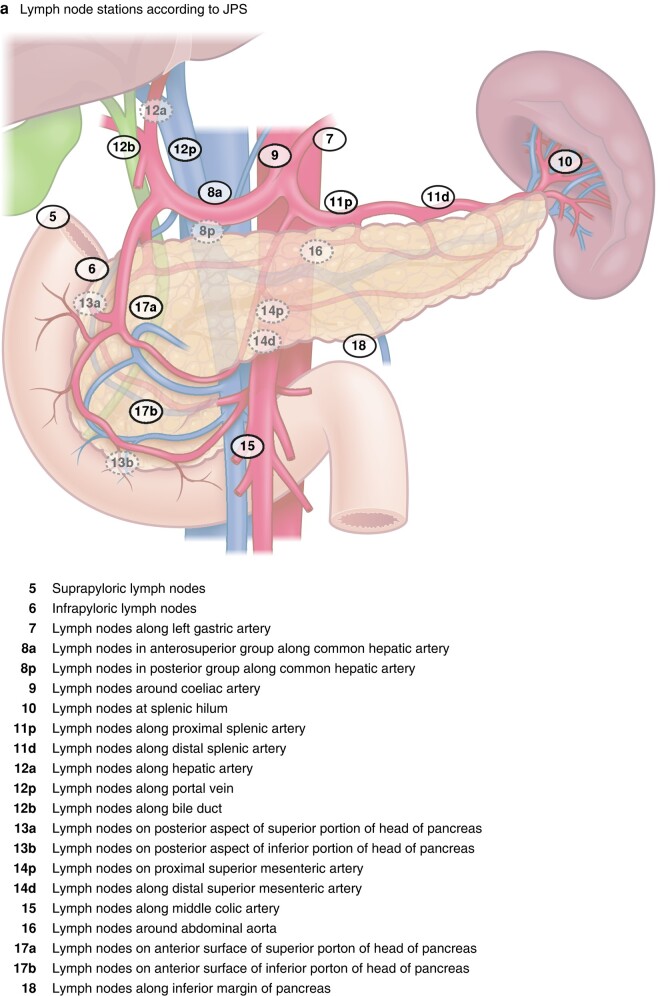
With an increasing number of premalignant lesions considered for surgery, in particular neuroendocrine tumour and intraductal papillary mucinous neoplasia (IPMN), the indication for splenectomy has become less clear, if not obsolete from an oncological viewpoint. Indeed, in one of the largest cohort studies2 to date on IPMN, less than 7% of patients had lymph nodes with metastasis in the splenic hilum. What the study does not address is the risk of having isolated lymph node metastasis in the splenic hilum alone (station 10, and hence the need for splenectomy to remove these nodes), without any other lymph node metastases along the pancreatic surface, considering the lymphatic drainage routes of the pancreas (Fig. 2). As nodal harvest may be viewed as a staging (and not curative) procedure, it may be considered to avoid extensive node sampling in premalignant and not clinically overt cancer diseases. Of note, this topic is bound to stir debate until further evidence can be produced to support one decision over the other. A further extended debate in this regard is the need for perirenal fat clearance (referred to as RAMPS9) to achieve an oncologically safe operation for advanced cancers of the body and tail of the pancreas (Fig. 1c).
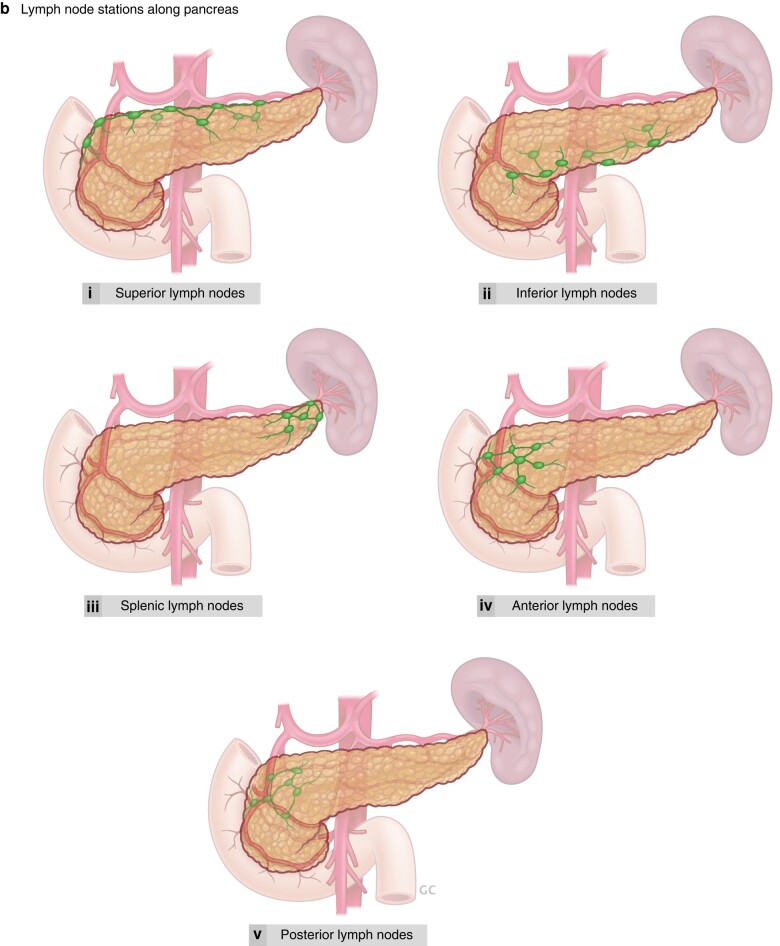
Fig. 2.
Lymph nodes of the pancreas
a Named lymph node stations according to the proposed terminology of the Japanese Society of Pancreatology (JPS). b Lymph node stations along pancreatic gland as anatomically described and defined: i superior lymph nodes—named owing to their location along superior border of head, body, and neck of pancreas; ii inferior lymph nodes—named owing to their location along inferior border of head, body, and neck of pancreas; iii splenic lymph nodes—drain nodes long the distal part of the pancreas, hilum of the spleen, and splenorenal ligament; iv anterior lymph nodes—comprise pyloric, anterior pancreatoduodenal, and mesenteric lymph nodes; v posterior lymph nodes—include posterior pancreatoduodenal lymph nodes, which are also a common site for drainage of the (common) bile duct and hepatopancreatic ampulla (of Vater) lymphatic vessels.
Taken together, considering what is ‘left’ in left-sided pancreatectomy has now been defined by consensus1. To consider, tongue in cheek, what else should be left, is still a matter of debate, but with some emerging data to support decisions. The spleen may be left (spleen-preserving procedure) for benign lesions such as IPMN2, as the risk of metastasis to the splenic lymph nodes is low (and with uncertainty whether spread is seen isolated in this area). Further data may be accrued using the novel proposed definitions and terminology1, with the hope of increasing the knowledge base in decision-making for left-sided pancreatectomy.
Contributor Information
Kjetil Søreide, Division of Surgery and Oncology, Department of Clinical Science, Intervention and Technology, Karolinska Institutet, Karolinska University Hospital, Stockholm, Sweden; Department of Gastrointestinal Surgery, Hepatopancreatobiliary Unit, Stavanger University Hospital, Stavanger, Norway; Department of Clinical Medicine, University of Bergen, Bergen, Norway.
Ernesto Sparrelid, Division of Surgery and Oncology, Department of Clinical Science, Intervention and Technology, Karolinska Institutet, Karolinska University Hospital, Stockholm, Sweden.
Funding
The authors have no funding to declare.
Author contributions
Kjetil Søreide (Conceptualization, Investigation, Methodology, Project administration, Resources, Supervision, Visualization, Writing—original draft, Writing—review & editing), and Ernesto Sparrelid (Conceptualization, Formal analysis, Investigation, Project administration, Supervision, Validation, Writing—review & editing)
Disclosure
The authors declare no conflict of interest.
References
- 1. Van Ramshorst TME, van Hilst J, Boggi U, Dokmak S, Edwin B, Keck Tet al. Definitions and terminology of left-sided pancreatic resections: an international Delphi consensus. Br J Surg 2024. in press [DOI] [PubMed] [Google Scholar]
- 2. Gorris M, van Bodegraven EA, Abu Hilal M, Bolm L, Busch OR, Del Chiaro Met al. Outcomes after distal pancreatectomy with or without splenectomy for intraductal papillary mucinous neoplasm: international multicentre cohort study. Br J Surg 2024;111:znad424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Giani A, van Ramshorst T, Mazzola M, Bassi C, Esposito A, de Pastena Met al. Benchmarking of minimally invasive distal pancreatectomy with splenectomy: European multicentre study. Br J Surg 2022;109:1124–1130 [DOI] [PubMed] [Google Scholar]
- 4. Nickel F, Distler M, Limen EF, Wise PA, Kowalewski KF, Tritarelli PMet al. Initial learning curves of laparoscopic and robotic distal pancreatectomy compared with open distal pancreatectomy: multicentre analysis. Br J Surg 2023;110:1063–1067 [DOI] [PubMed] [Google Scholar]
- 5. van Ramshorst TME, Giani A, Mazzola M, Dokmak S, Ftériche FS, Esposito Aet al. Benchmarking of robotic and laparoscopic spleen-preserving distal pancreatectomy by using two different methods. Br J Surg 2022;110:76–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. van Bodegraven EA, van Ramshorst TME, Balduzzi A, Hilal MA, Molenaar IQ, Salvia Ret al. Routine abdominal drainage after distal pancreatectomy: meta-analysis. Br J Surg 2022;109:486–488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bonsdorff A, Ghorbani P, Helanterä I, Tarvainen T, Kontio T, Belfrage Het al. Development and external validation of DISPAIR fistula risk score for clinically relevant postoperative pancreatic fistula risk after distal pancreatectomy. Br J Surg 2022;109:1131–1139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Loos M, Mack CE, Xu ATL, Hassenpflug M, Hinz U, Mehrabi Aet al. Distal pancreatectomy: extent of resection determines surgical risk categories. Ann Surg 2024;279:479–485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Strasberg SM, Linehan DC, Hawkins WG. Radical antegrade modular pancreatosplenectomy procedure for adenocarcinoma of the body and tail of the pancreas: ability to obtain negative tangential margins. J Am Coll Surg 2007;204:244–249 [DOI] [PubMed] [Google Scholar]
- 10. Kang JS, Choi YJ, Byun Y, Han Y, Kim JH, Lee JMet al. Radiological tumour invasion of splenic artery or vein in patients with pancreatic body or tail adenocarcinoma and effect on recurrence and survival. Br J Surg 2021;109:105–113 [DOI] [PubMed] [Google Scholar]
- 11. Nakamura T, Okada KI, Ohtsuka M, Higuchi R, Takahashi H, Nagai Ket al. Insights from managing clinical issues in distal pancreatectomy with en bloc coeliac axis resection: experiences from 626 patients. Br J Surg 2023;110:1387–1394 [DOI] [PubMed] [Google Scholar]
- 12. Søreide K, Nymo LS, Kleive D, Olsen F, Lassen K. Variation in use of open and laparoscopic distal pancreatectomy and associated outcome metrics in a universal health care system. Pancreatology 2019;19:880–887 [DOI] [PubMed] [Google Scholar]
- 13. Lof S, van der Heijde N, Abuawwad M, Al-Sarireh B, Boggi U, Butturini Get al. Robotic versus laparoscopic distal pancreatectomy: multicentre analysis. Br J Surg 2021;108:188–195 [DOI] [PubMed] [Google Scholar]