Abstract
Chronic illness (CI) is a major cause of morbidity and mortality for Indigenous people. In Montana, Indigenous communities disproportionately experience CI, a legacy of settler colonialism. For over two decades, Messengers for Health, an Apsáalooke (Crow Indian) non-profit, and Montana State University have partnered to improve community health using a community-based participatory research (CBPR) approach. We developed Báa nnilah, an intervention utilizing community strengths, to improve CI self-management. This manuscript describes the protocol for a cluster randomized trial with two arms: an intervention group and a wait list control group, who both participated in the Báa nnilah program. Enrollment occurred through family/clan networks and community outreach and attended to limitations of existing CI self-management interventions by using an approach and content that were culturally consonant. Participants received program materials, attended seven gatherings focused on improving CI management, and received and shared health information through storytelling based on a conceptual framework from the Apsáalooke culture and incorporating CI self-management strategies. Participant support occurred within partnership dyads during and between gatherings, from community mentors, and by program staff. The study used mixed methods to evaluate the intervention, with qualitative measures including the Short Form Health Survey (SF-12), Patient Health Questionnaire (PHQ-9), Patient Activation Measure (PAM), and a suite of PROMIS measures, various physical tests and qualitative survey responses, semi-structured interviews, and outcomes shared by participants with program staff. We hypothesized that Báa nnilah would significantly improve participant health outcome measures across multiple dimensions with quality of life (QoL) as the primary outcome.
Trial registration: ClinicalTrials.gov: NCT03036189. Registered on 30 January 2017. (From https://clinicaltrials.gov/ct2/show/NCT03036189).
Keywords: CBPR, Cluster randomized trial, Indigenous, Chronic illness, Self-management, Community resilience
1. Introduction
Chronic Illness (CI) affects 6 in 10 adults in the United States [15], contributing to premature death, disability, and lower individual and familial quality of life (QoL) [3,6,14,30,66,91]. Compared to other US racial groups, Indigenous1 people experience the highest prevalence of CI [13]. Disparities are due in large part to the legacies of settler colonialism [54,84], including impacts of the reservation system [55,89], forced changes in food systems [47], historical and current loss [46,69], and chronic underfunding of healthcare[86,95].
In Montana, racial inequities between Indigenous and white populations are reflected in years of potential life lost due to diabetes (17 vs. 13.5, respectively), heart disease (16.3 vs 11.8), stroke (14.3 vs 12.1), and chronic liver disease (25.4 vs 17.1) [50]. Big Horn County, the location of the intervention, where 66% of residents identify as Indigenous [85], ranks in the lowest quartile for health in Montana, with 26% of individuals reporting poor health, 17% diagnosed with diabetes, and triple the state rate of potential life lost before age 75 [72]. Life expectancy for Indigenous individuals in Big Horn County is 62.6 years compared to 78.1 for white individuals and the rate of preventable hospitalization is 2.7 times higher for Indigenous individuals [72]. Due to the burden of CI in the Apsáalooke community, the Community Advisory Board (CAB) of our Community-Based Participatory Research (CBPR) partnership chose to focus our efforts on supporting tribal members with CI.
We decided to develop a program for community members using a CBPR approach so the program would be more relational, effective, and well-received. CBPR approaches equitably involve all partners in the development, implementation, evaluation, and dissemination of health interventions [45,57]. These approaches provide effective solutions to health problems and avoid replication of damaging colonial relationships between predominantly white institutions and Indigenous populations [69,87]. The gold standard evidence-based program for CI self-management, the Chronic Disease Self-Management Program (CDSMP) [93], was developed in a predominantly white population and has been difficult to sustain in Indigenous communities [46,63,81,82]. The CDSMP was not appropriate for use with the Apsáalooke community due to the structure and approach not being culturally consonant and because program content did not include important influencers of CI self-management in this community.
2. Partnership context
The partnership between the Apsáalooke non-profit organization, Messengers for Health (Messengers) and faculty and students at Montana State University (MSU) began in 1996. Decision-making is done collaboratively between partners. Formalized in 2001, our community advisory board (CAB) consists of Elders, community members working in health and education, and individuals with CI. Messengers serves the community with the support of the Crow Tribal Government through a resolution from the Tribal Legislature. The tribe is regularly briefed on the partnership’s activities and provided letters of support for the grant applications to fund the development, implementation, and evaluation of the Báa nnilah program.
3. Conceptual framework
In 2013, we gathered information on the community experience of CI. One community partner interviewed 20 men and women who shared their stories of living with CI. We developed a new method to analyze the stories because available qualitative methods were not consonant with Apsáalooke culture [36]. The process involved the CAB and research team listening to the interviews and having iterative discussions that wove interviewee experiences with team member reflections resulting in a conceptual framework for understanding and improving CI self-management [38,77]. The title of the intervention, Báa nnilah, translates to advice or instructions for life that are received from others, often in a story form. Our conceptual framework of influencers of CI self-management, their role in the Báa nnilah program, and outcome measures related to the influencers is shown in Fig. 1.
Fig. 1.
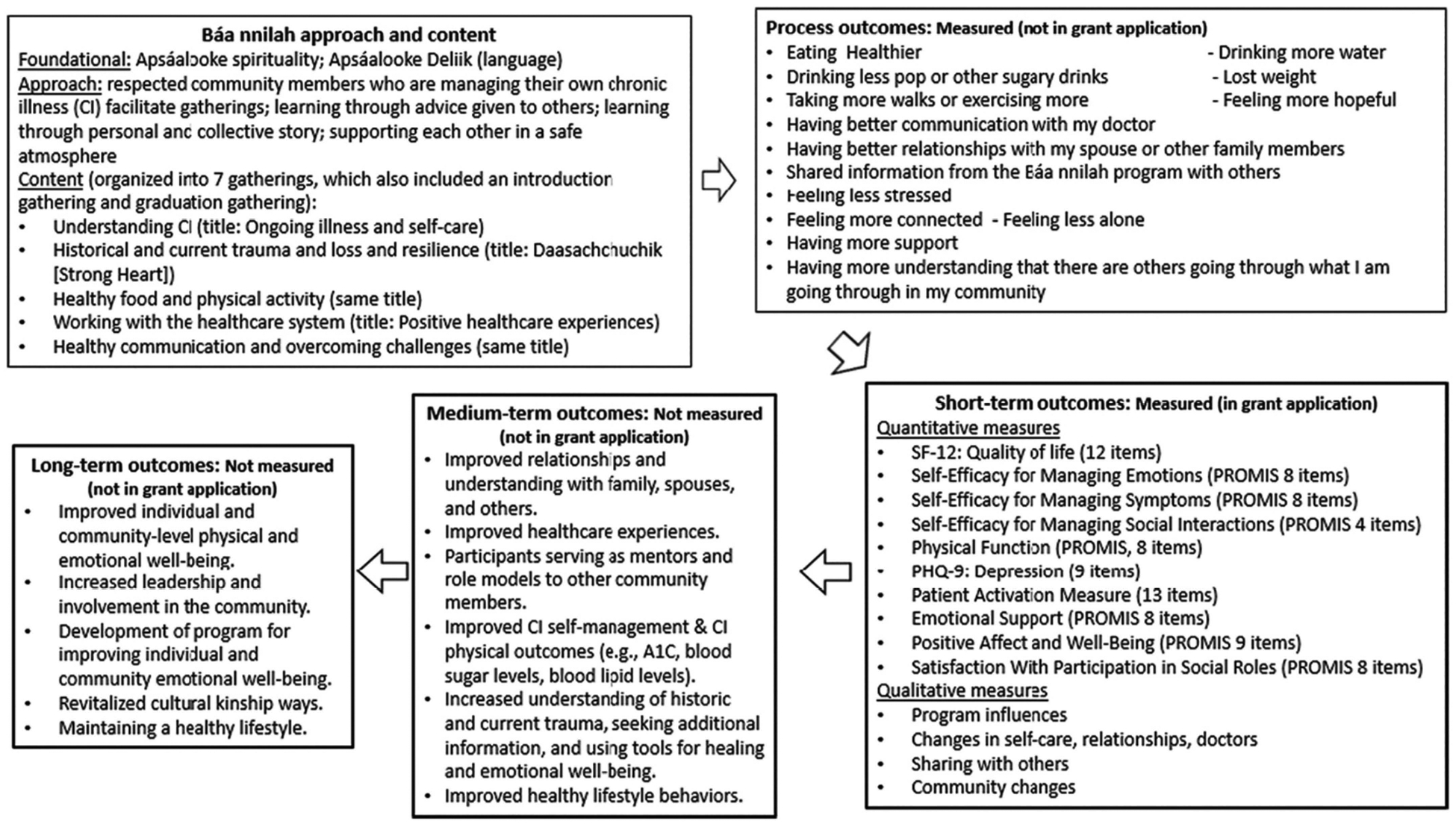
Framework for Approach, Content and Outcomes (measured and unmeasured).
4. Study aims and hypotheses
Study aims included: 1) Refining and strengthening the community-based, culturally appropriate Báa nnilah intervention and study protocol and 2) Testing the effects of the refined intervention versus usual care using a pragmatic CRT with a wait-list control (WLC) arm among Indigenous community members. We hypothesized that intervention participants would have significant improvement in QoL using the Short Form Health Survey-12 (SF-12), compared to WLC participants, immediately following the intervention, and at 6- and 12-months post-intervention. We also hypothesized that, compared to the WLC participants, intervention participants would show significant improvements in: a) measures of physical function, b) self-efficacy for managing CI symptoms, c) depression, d) patient activation, e) emotional support, 0 self-efficacy for managing emotions and social interactions, g) positive affect and well-being, and h) satisfaction with participation in social roles, immediately following the intervention and at 6- and 12-months post-intervention.
5. Materials and methods
5.1. Study design
This CRT protocol is presented in accordance with Good Clinical Practice, Standard Protocol Items: Recommendation for Intervention Trials (SPIRIT) and Consolidated Standards of Reporting Trials (CONSORT) guidelines [10,16]. This CRT had two arms (intervention and WLC) to test the effectiveness of a bi-monthly, seven-gathering intervention compared to usual care that community members received from various healthcare providers. The CAB requested this design because of a desire for all participants to receive the program. CRTs are considered the “gold standard” for evaluating interventions delivered to communities [60,61]. The clinical trial registration number is NCT03036189. See Table 1 for the intervention and data collection time points.
Table 1.
Intervention Timeline.
| Intervention and data collection time points (T = time) | ||||||||
|---|---|---|---|---|---|---|---|---|
| T1 | Intervention | T2 | WLC | T3 | T4 | T5 | ||
| 10/2017–4/2018 | 4/2018–8/2018 | 9/2018–1/2019 | 4/2019–8/2019 | 10/2019–1/2020 | ||||
| Recruit and Randomize | Intervention Group | Pre | Attend Báa nnilah program | Immediate post | – | 6-months post | 12-months post | – |
| WLC Group | Pre | – | Pre | Attend Báa nnilah program | Immediate post | 6-months post | 12-months post | |
5.2. Sample: inclusion/exclusion criteria
Inclusion criteria for study participants included a) age ≥ 25 years, b) Indigenous, c) living on or near the Apsáalooke Reservation and d) diagnosed by a medical provider with a CI. We chose a younger age threshold than some CI self-management studies because Indigenous people are more likely to report risk factors for, and prevalence of, CI at a younger age compared to other racial/ethnic groups [2,4,39,42,48,59]. Participants were excluded if they had an advanced terminal condition that precluded participation.
5.3. Recruitment and enrollment
We aimed to recruit at least 200 participants and the 10 intervention facilitators (Aakbaabaaniilea – ones who give advice) were each asked to recruit 10 community members for each study arm from within their family, clan, and community. Aakbaabaaniilea were encouraged to share information about the program including program format, content, and information on participation incentives such as gas cards and health-relat when community members: 1) observed data collection in the community and expressed interest in becoming a participant, 2) were informed of the program by previously recruited participants and invited to join an ongoing or future data collection, or 3) were attending a concurrent event in the same facility as a data collection event and invited to join by Aakbaabaaniilea.
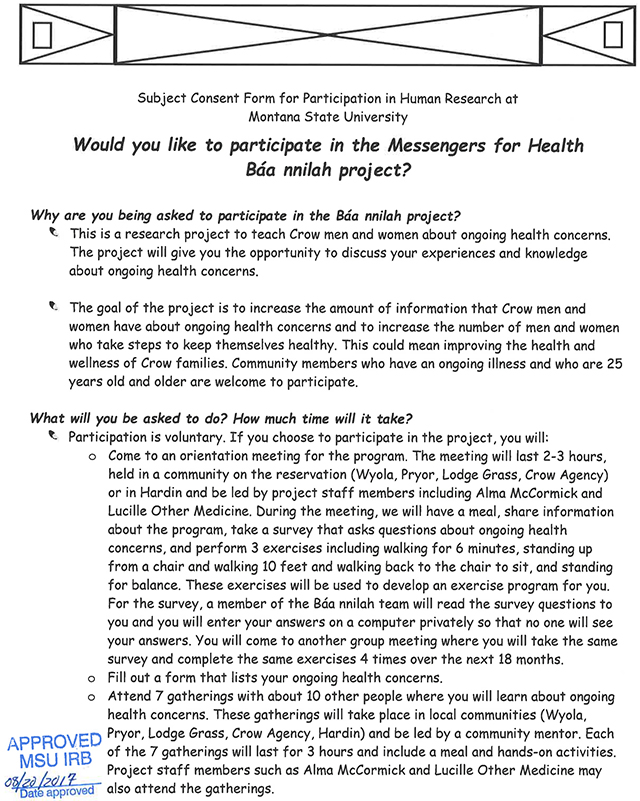
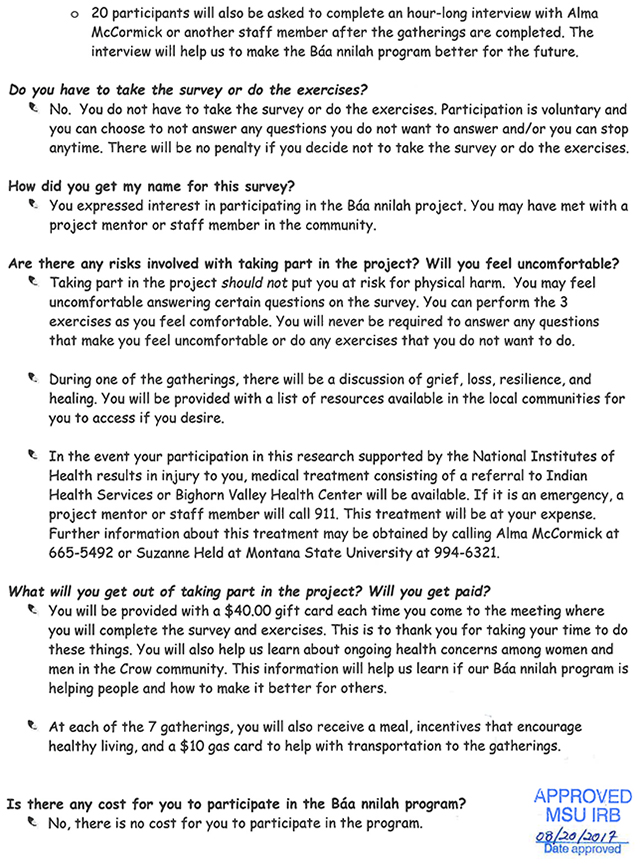
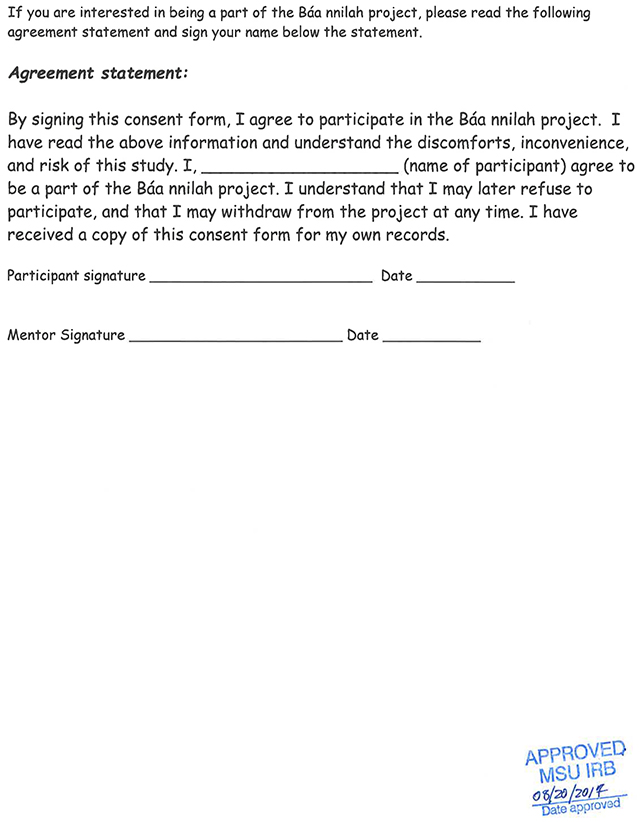
5.4. Informed consent/IRB
Participants consented to participate prior to the first data collection event by Aakbaabaaniilea or at during the first data collection event by program staff. Participants signed and received a copy of the consent form, which was written in plain language and designed to be easily understood. Institutional Review Board (IRB) approval was obtained from MSU. There was not a registered IRB through the US Office for Human Research Protections on the Apsáalooke Reservation at the time of this study.
5.5. Assignment
Using a computer-generated randomization program, family/clan members were cluster randomized, with each cluster comprised of participants belonging to the same family/clan. The clusters enrolled by each Aaakbaabaaniilea were sorted by size and then randomly assigned to one of the study groups. There were also individuals randomized to one of the two groups. Allocation was not concealed, and participants and program staff were not blinded. Twelve participants randomized to the intervention group who had not attended any sessions were invited to and joined the WLC group. All participants received usual care from existing healthcare providers, without standardization of usual care across participants. During the intervention and wait list period, all participants were sent monthly newsletters on topics unrelated to Báa nnilah content.
5.6. Intervention format
5.6.1. Intervention facilitators (Aakbaabaaniilea)
Interview analyses resulted in selecting program facilitators who were community members with a CI who were actively engaged in their health care and were viewed as role models for managing their Cl. Each Aakbaabaaniilea led an intervention group and a WLC group and were selected to represent different Apsáalooke communities. Aakbaabaaniilea were provided with a monthly stipend of $350 while the intervention was running.
5.6.2. Training for Aakbaabaaniilea
We held monthly meetings with Aakbaabaaniilea and the CAB to pilot test aspects of the intervention, receive feedback and provide training in recruitment and facilitation. Aakbaabaaniilea were given a training manual that included suggestions for recruitment, advice for preparing and facilitating gatherings, and tips for retaining participants. They received a program facilitation manual, with lists of materials to bring to each gathering and detailed information for facilitating each of the seven gatherings. Aakbaabaaniilea practiced facilitating each of the seven gatherings with program staff at a weekend retreat prior to the intervention. Before the WLC group started, Aakbaabaaniilea facilitated three gatherings during a retreat, which allowed each to determine what they wanted to practice.
5.6.3. Facilitation style
The facilitation style emerged from the oral story-telling tradition of the Apsáalooke. Aakbaabaaniilea were encouraged to read and become familiar with the program manual and then use their own words and lived experience, with the program manual as an aid. Aakbaabaaniilea were given the freedom to speak in their language and to foster a comfortable, yet structured format for content delivery.
5.6.4. Intervention delivery
Baa nnilah was delivered face-to-face in groups of approximately 10 participants and one Aakbaabaaniilea. There were seven gatherings, occurring roughly every other week and each lasting approximately 3 h in local community settings, such as schools, community and senior citizen centers, and churches. Participants were partnered into dyads to provide support to each other between the gatherings and were encouraged to meet face-to-face, or use text message, phone, or email communication, a minimum of once per week. Dyad support was not measured.
Gatherings were comprised of six sections. The first section included a prayer, meal, and visiting, and allowed for the strengthening of relationships. In the second section, a story related to the gathering topic was read out loud. In the third section, Aakbaabaaniilea shared information. The fourth section was devoted to a sharing circle where Aakbaabaaniilea shared a personal story of challenges and solutions to the gathering topic and then participants shared their stories. The fifth section included a partnership check-in and gathering-specific activity. In this section, supportive partners discussed prior and future goals, represented as feathers within a culturally consonant goal setting tool, Counting Coup, that was developed for the program ([19]). The final section was a closing prayer. Table 2 contains details about the gatherings.
Table 2.
Báa nnilah gathering sequence and session content.
|
Gathering 1: Introductory gathering “The intent of this gathering is to share how the program grew from the desires and interests of the Crow community to provide support and encouragement to community members with ongoing illnesses. We want members to become familiar with the program, and to foster and encourage an atmosphere of safety and hope.” Story: Through the eyes of the eagle. A story about hope and health and transformation. Mentor provides information: Creating norms/ground rules for the gatherings, Counting Coup journals, confidentiality. Sharing circle: Sharing personal health stories. Supportive partnerships activity: “My partner has my back”. Selecting a partner for the duration of the program, sharing contact information and how they will support each other outside of the meetings. Counting Coup: selecting feathers (goals) they would like to receive over the next two weeks. Incentive gifts: Counting Coup journal, Báa nnilah tote bag |
|
Gathering 2: Ongoing conditions and self-care (Understanding chronic illness) “The intent of this gathering is to help Apsáalooke gain knowledge of ongoing health conditions and how to practice self-care for healing and resilience. It is important for you to have knowledge about your ongoing health conditions, medicines, and treatment We encourage each of you to use our own cultural resources on your healing journey.” Story: Coyote falls from grace. A story about humility and forgiveness of self and others while working on making healthy changes. Mentor provides information: Ongoing health conditions (what they are, risk factors, prevention, self-care), resourcing, Walking a good path exercise Sharing circle: Stories of what we are doing as a part of personal self-care. Supportive partnerships activity: Counting Coup check in, review Healing Circle, and select self-care activities, including medication log. Incentive gift: Laminated medication log and dry erase pen |
|
Gathering 3: Düchikaatah (Taking good care of yourself through healthy communication) “Today’s gathering will focus on practicing Düchikaatah (taking good care of yourself through healthy communication). We have learned many things over the past two gatherings that we are applying to our lives toward better health. The changes we are working to make can come with challenges, and today we are going to build skills for taking on those challenges with confidence. It is helpful for patients with ongoing health conditions to speak and act for themselves and their families for better health and to do so in a good way that maintains the honor and respect for others that we were taught Today we will explore ways to find our voice and develop healthy communication skills. We will also develop tools for overcoming challenges that arise as we make changes in our lives and there’s an activity for practicing Düchikaatah that you can do on your own time.” Story: Victory Dance. A story about working together with families, friends, and co-workers. Mentor provides information: Speaking and acting for ourselves and our families, healthy communication. Sharing circle: Stories about when you spoke up for yourself or faced a challenge concerning your health and found a way to overcome it. Supportive partnerships activity: Counting Coup check in, practicing health communication and healthy conflict resolution skills, problem solving to overcome a current challenge, and self-kindness. Incentive gift: Living a healthy life with chronic conditions book |
|
Gathering 4: Daasachchuchik (Strong Heart) “The intent of this gathering is to better understand the personal impacts of historical and current trauma, loss and how traditional cultural values and resilience help to heal and overcome loss and trauma.” Story: Old man coyote kills the monster. A story about overcoming symbolic monsters such as substance abuse and shame in our healing journey. Mentor provides information: Historical and current grief, loss, and stress, daasachchuchik (resilience), symptom cycle; not ignoring reality of poverty and difficult situations Sharing circle: Stories of loss/trauma and strength. Supportive partnerships activity: Counting Coup check in, skill building on grief/loss/stress/pain/fatigue management tools. Incentive gift: Ground. Breathe. Settle, bracelet and wallet card |
|
Gathering 5: Healthy food and physical activity “The intent of this gathering is healthy eating habits and physical activity. We learned that eating healthy and being physically active can help in managing many ongoing illnesses. Today we will share information and activities about healthy food and how to be physically active. ” Story: Fox is lifted up. A story about lifting each other up and taking care of the community. Mentor provides information: Healthy eating and physical activity including how to shop for healthy food, metabolic syndrome, reading a nutrition label, meal planning, and benefits of physical activity. Sharing circle: Stories of what we do to eat healthy and be physically active. Supportive partnerships activity: Counting Coup check in, Rethink your drink activity to visualize sugar, practicing exercises with stretchy bands. Incentive gifts: Exercise bands, activity tracker |
|
Gathering 6: Positive healthcare experience “The intent of this gathering is show how important positive interactions with our healthcare providers are and how to establish a healthy relationship with our healthcare providers. Another purpose is to show that we have to do our part in taking care of ourselves outside of the doctor’s office in order to stay healthy.” Story: Coyote steals fire. A story about wholeness. Mentor provides information: How to receive good healthcare including picking a primary care provider, communicating with them, and how to have positive healthcare visits. Sharing circle: Stories of having a positive interaction with the health care system and providers. Supportive partnerships activity: Counting Coup check in, skill building activity around having a good visit with a healthcare provider including making lists of questions for providers and things to bring to a doctor visit. Incentive gift: Preparing for a doctor’s visit dry erase board, doctor’s visit wallet card |
|
Gathering 7: Closing and Graduation Celebration “The intent of this gathering is to better understand the personal impacts of the program and how you will transition from the program into the community. This is a time to share how you plan to maintain what you have learned and how you will continue to stay in connection with each other. This is a time to share the resources you will use to sustain and improve your health. Finally, it is a time to honor your progress, effort, and commitment to the path of good health.” Mentor provides information: How each participant can now be a mentor and spread this information into the community. Sharing circle: Stories of what you have gained from the program. Supportive partnerships activity: Counting Coup check in, development of an individual action plan. Incentive gift: Graduation certificate, program t-shirt Source materials for gathering content and activities included publications from government agencies (e.g., Centers for Disease Control and Prevention, Indian Health Service, US Department of Health and Human Services), health-related organizations (e.g., Mayo Clinic, American Indian Cancer Foundation, Billings Clinic, Fooducate), manuals from other health promotion programs (e.g., The Good Road of Life: Curriculum for Native Families [80], ENHANCE Project from University of Hawaii School of Nursing and Dental Hygiene [43]), journal articles, and books (e.g., My Body, My Earth [29]). |
5.6.5. Materials
At the first gathering, participants were provided with a 250-page printed program manual. We incorporated materials from prior Messengers for Health projects and developed materials specifically for the Báa nnilah program. Additionally, we utilized or adapted materials and activities from outside sources, as noted in Table 2.
5.7. Participant retention and adherence
The close-knit nature of Apsáalooke relationships informed our methods for encouraging retention and adherence for the study. Most program participants knew each other and Aakbaabaaniilea encouraged them to develop deeper relationships with each other. Familiarity and commitment to each other’s wellbeing helped create a comfortable and supportive space for sharing, based on mutual love and concern. Other approaches to support adherence and retention included: 1) sending email/phone/text reminders, 2) offering healthy meals and beverages at gatherings, 3) providing gas cards ($10 value) at each gathering and gift cards ($40 value) at each data collection meeting, and 4) offering health-related incentives during program gatherings. These approaches arose out of literature searches, experiences from past interventions in the community, and knowledge from Apsáalooke staff. Adherence and retention rates were calculated through participant attendance records [28].
5.8. Data collection
Data were collected pre- and immediate post-intervention as well as 6 and 12 month follow up to assess program outcomes. Trained program staff gathered data for each of the data collection time points, using digital surveys on tablet computers. Follow-up occurred primarily in group reunion settings, where participants visited and shared a meal in addition to completing data collection. Additionally, data collection sessions were arranged for individuals and small groups to maximize participant retention. Qualitative outcome data included comments added during quantitative data gathering on tablets, comments made by participants to program staff and Aakbaabaaniilea, and interviews with a random sample of participants following their completion of the intervention.
5.9. Measures/tools
We utilized the SF-12 to assess our primary outcome, QoL. Secondary outcome surveys were from the Patient Reported Outcomes Measurement Information System (PRO MIS), the Patient Health Questionnaire-9 (PHQ-9), the Patient Activation Measure (PAM) and several physical health measures. Apsáalooke project staff and the CAB reviewed all measures to ensure consonance with Apsáalooke culture and understandability and were found to be acceptable for use with modifications as noted below. See Table 3 for detailed descriptions of measures, modifications, and Cronbach’s alpha data when available.
Table 3.
Data Instruments.
| Demographics health data | Data collected included year of birth, sex, marital status, highest achieved educational level/degree, employment status, annual household income (from 1 = Under $10,000 to 8 = $100,000 and higher), number of people in the household, insurance or health coverage (Yes/No for each of Indian Health Service, Medicare/Medicaid, and Private Insurance), participation in food assistance programs (Yes/No), number of miles traveled to primary healthcare, number of doctor visits in the past four months, and self-reported CI conditions. |
|
Measures [Cronbach’s a] SF-12 [0.72–0.89] [25] 12 questions regarding function in physical and mental health domains. The normed score range is from 0 to 100 with 50 representing an average score and lower scores indicating poorer health and increased physical and mental limitations. |
Changes Activities deleted were bowling and playing golf and activities that were added were carrying a small child, walking for exercise, or round dancing/push dancing (Native American traditional dances). |
|
PHQ-9 [0.86–0.89] [37] 9 questions asked participants to respond to statements pertaining to the frequency of depression symptoms in the preceding two weeks. The score range for the instrument is from 0 to 27, with higher scores indicating higher levels of depression symptoms. |
None |
|
Patient Activation Measure (PAM) [0.87] [79] 13 questions assess participant beliefs, perceptions, knowledge, and confidence regarding management of their health condition. |
Minor changes were made to 11 of 13 questions to assist with understandability. For example, the question “I have been able to maintain the lifestyle changes for my health that I have made.” was changed to “I have been able to maintain (keep up with) lifestyle changes, like eating right or exercising.” |
| PROMIS Measures [Cronbach’s a] | |
|
Satisfaction with Social Roles and Activities [α = 0.976] ([33]; [35]) Self-Efficacy for Managing Symptoms [α = 0.968] [32] Emotional Support [α = 0.976] [34] Positive Affect and Well-Being [α = 0.965] [74] Physical Function [α = 0.947] ([18]; [32]) Self-Efficacy for Managing Emotions [α = 0.961] ([32]; [53]) Self-Efficacy for Managing Social Interactions [α = 0.905] [32] |
| Physical Activity Tests | Changes | |
|---|---|---|
| Timed Up and Go (TUG) [64]. | Participants are timed as they rise from a seated position in a chair, walk for 3 m, turn around and return to a seated position. Participants performed the TUG twice and were scored with the mean time. | Due to an error in communication between a consultant who assisted with this measure and the research team, the distance that individuals walked during this test was modified from 3 m to 10 m, therefore prior validation data may not apply. |
| Modified Balance Error Scoring System (mBESS) ([7]; [49]; | Participants stood with hands on hips and eyes closed, balancing for 20 s in 3 standing positions: a double-leg stance, a single-leg stance, and tandem stance. Test observers counted up to 10 errors per stance, including opening eyes, taking hands off hips, stepping, putting a hand out to a chair or wall, or making other large corrections, which led to a stance score ranging from 0 to 10 with a maximum total of 30. Participants who could not complete a position for balance reasons, were given a score of 10. | Changes made for our data collection include testing single-leg stance with the dominant foot, as opposed to non-dominant foot as instructed by mBESS, and allowing participants to determine lead foot during the tandem stance; therefore, prior validation data may not apply. |
| 6 Minute Walk Test ([8];[52];[71]) | Staff measured the cumulative distance participants walked at a comfortable pace along a 100-ft tape measure for six minutes. | The distance participants walked before turning around was adapted to the unique space and weather conditions of the various data collection sites. |
Short Form Health Survey-12 (SF-12), Physical and Mental (version 1) The SF-12 was deemed the best fit for measuring quality of life and was previously validated with a cohort of Indigenous participants [25,70]. We received approval to change question two to encapsulate moderate activities more applicable to our study population [1].
Patient Health Questionnaire-9 (PHQ-9), Depression The PHQ-9 is widely used to measure symptoms of depression. It is applicable as a screening tool and serial assessment instrument in research and primary care [51] and has shown adequate construct validity for Indigenous populations [37].
Patient Reported Outcome Measurement Information System (PROMIS) measures We used validated NIH PROMIS measures to assess relevant aspects of health and QoL related to symptoms and function across CI conditions in diverse cultural contexts and formats. No validation data for Indigenous populations were available [9,11,12,18,73]. Selected PROMIS measures aligned with aspects of CI self-management identified within our conceptual framework.
Patient Activation Measure (PAM) Developed by Insignia Health, this short form has been validated to assess patient knowledge, skill, and confidence for self-management of health conditions [40].
Physical Activity Tests We used three common physical activity tests, the Timed Up and Go, modified Balance Error Scoring System, and the 6-min walk test, to assess impacts of the intervention, detailed in Table 3.
5.10. Qualitative measurements
Our mixed-methods evaluation design included three sets of qualitative data to assess the impact of the program. Our primary dataset comprised in-depth qualitative interviews performed by co-author Knows His Gun McCormick with a random sample of approximately 10% of participants post intervention. Questions were designed to facilitate participants’ reflections on how the program impacted them and the community and to receive their ideas on improving the program. Our second dataset included open-ended response to the question, “Please share what you gained or learned from the program and what changes in your health or behavior you made because of the program?” This was the last question participants entered responses into tablet computers for the post-intervention quantitative data collections. Our third dataset included non-solicited, informal information shared by participants in conversations with program staff both during and after the intervention regarding program impacts.
5.11. Fidelity assessment
Two assessments were conducted to evaluate treatment fidelity. A random 10% sample of gatherings was evaluated with a check list assessment of whether each gathering component was not completed, partially competed, or fully completed and if new components were included that were not in the original protocol. The assessor also commented on Aakbaabaaniilea responsibilities such as communication with participants, bringing all necessary materials, and being on-time, interactional style such as speaking Crow, facilitation style, food choices, humor, and empathy, and participant or environmental factors such as health conditions, weather, deaths, and presence of non-participants at program gatherings.
For the second fidelity assessment, a graduate student researcher conducted semi-structured qualitative interviews with all Aakbaabaaniilea following completion of the intervention and WLC group programs. Interviews included questions on preparing to lead gatherings, what it meant to be a mentor, support received from program staff, personalizing gatherings, and what made them feel confident and comfortable leading gatherings.
5.12. Qualitative data analysis
Qualitative data was analyzed using a culturally consonant method developed by this team [36] that kept interviewee stories intact versus breaking stories apart into themes. Interviews were transcribed and a sub-group of the partnership team read the transcripts and held multiple analysis discussion sessions. From this process a conceptual model to represent participant and broader outcomes naturally emerged.
5.13. Quantitative data analysis
Sample size was calculated based on the longitudinal design with one between-subject factor (intervention condition: intervention vs. WLC) and one within-subject factor (time) using G*Power [27]. A review of outcomes of CI self-management interventions [65] showed small effect sizes (ES) of CI self-management interventions for clinical markers, depression, and physical function (median ES was f = 0.1 to 0.16), and moderate (f = 0.3) ES for self-efficacy. Similarly, an evaluation of the effectiveness of a self-management intervention for persons with diabetes [94] indicated a small ES for QoL (Cohen’s f = 0.11). Therefore, we used a small ES (f = 0.11) for the power analysis for the primary hypothesis and small to moderate effects for the secondary hypotheses. Our power analysis showed that to achieve 80% power for detecting overall intervention condition differences in the primary outcome, 200 participants were needed. We determined this sample size would yield at least 80% power for the secondary outcomes, with a conservatively estimated 0.6 correlation between repeated measures, Intraclass Correlation (ICC) ofO.l, and a 20% attrition rate [60]. Our power analysis further showed that a sample size of 200 would provide at least 80% power to detect a small (f = 0.1) intervention-by-time interaction in a primary or secondary outcome.
Survey data were de-identified and analyses were conducted using R [41,68,75]. Because we used CRT, the data structure was multilevel in nature (i.e., observations across time were nested within individuals and individuals were nested within family/clan clusters) and a positive ICC among observations of members of the same cluster was expected. Thus, we used random coefficient modeling [21,61] to analyze each primary and secondary outcome in this longitudinal and multilevel data set. Proper covariance structure was specified based on goodness-of-fit of an unconditional means model. An individual growth model was evaluated for overall intervention vs. WLC study group difference, linear/nonlinear change over time, group differences and group-by-time interaction effects. Model parameters were estimated with and without potential covariates including demographic variables thereby yielding unbiased estimates of intervention effects. As a follow-up heterogeneity of treatment effect (HTE) test, we examined two-way interactions between study group and each of the covariates, and, where appropriate, three-way interactions among group, time, and each covariate (i.e., moderation). We analyzed incomplete data using the intent-to-treat approach. Multiple imputation (MI) and full information maximum likelihood (FIML) estimation were used to handle missing data [26,31,76].
5.14. Data management
Quantitative data and one qualitative datapoint were collected digitally using tablet computers and uploaded to a central repository, accessible via password to program staff. Hard copy attendance records from Aaakbaabaaniilea and qualitative data, including digital recordings of interviews and resultant transcripts, were centralized, and stored in a locked cabinet in a locked room either on Montana State University campus or the Messengers office in Crow Agency.
5.15. Data safety and monitoring
A data safety monitoring plan was included in the grant application. The Data Safety Monitoring Committee (DSMC), consisting of program staff, with independent representatives, conducted periodic reviews of the trial such as the aggregated data, adverse events, and logistics of participant enrollment and participation. Two external representatives of the committee provided an independent review and recommendations. The DSMC met regularly during the data collection phase of the trial. Primary potential harms due to the intervention itself included possible experience of psychologic distress when completing surveys or discussing traumas or painful subjects in sharing circles, as well as during review of content focused on historical trauma and loss. Potential harms could have occurred when completing physical tests. The DSMC met regularly to review adverse events and determine whether there was a need to modify the study protocol. No specific criteria for discontinuation or modification were detailed in the DSMC protocol.
5.16. Steering committee
An annual Steering Committee meeting was held per requirements of the National Institutes of Health (NIH) U0l funding mechanism. Participants included the co-Principal Investigators, CAB Chair, NIH Project Scientist, and two external members (an Indigenous public health-trained Executive Director of a health-related non-profit organization and an Apsáalooke education-trained tribal college faculty member and elder). CAB members and community and university research partners, including student researchers, were invited to participate in annual meetings, where staff members presented progress of and plans for the project and received and addressed suggestions and comments.
6. Discussion
Indigenous communities experience CI at disparate rates [13]. It is essential that self-management programs are culturally consonant, positively impact CI self-management of participants, and are adaptable to variations across Indigenous nations. As no such examples were available, we developed our own culturally consonant intervention and study protocol. The protocol for the Báa nnilah program, which is now complete, is being shared at this time to provide details of the study to other communities who may want to implement a similar program and to support a forthcoming results paper. Here we present strengths and limitations of our trial as well as future directions.
The process used to develop the intervention tested in this trial was unique in that community members who had Cis shared their health stories, which included influencers of their CI self-management. These stories were shared with the co-PI who is a tribal member. Project staff then used a culturally consonant qualitative data analysis method [36] to develop our conceptual framework and the program content and approach. Since the conceptual framework, content, and approach arose directly from the stories of Apsáalooke tribal members, Báa nnilah is likely to improve CI self-management within this population [17,58,92].
Essential aspects of Báa nnilah’s content and approach are not included in current CI self-management programs and address crucial differences between Indigenous and non-Indigenous views of health and disease [5,20,22], responding to impacts of colonization and the reservation system on health outcomes. Historical and on-going trauma and loss are known barriers to effective CI self-management for Indigenous populations [90]. Trauma-informed principles were integrated throughout Báa nnilah and one gathering is devoted to understanding and healing from trauma and loss and cultivating resilience.
This study protocol reflects calls for improving the design and implementation of pragmatic trials that fit the needs of communities [96]. Compared to RCTs where individual participants are randomly assigned to study groups, CRT designs allow for a balance between maximizing the number of clusters (i.e., to increase statistical power) and minimizing “premature” information sharing across study groups. We used a WLC arm, recommended by community members, as an ethical way to ensure that all participants receive the intervention. This helped community members endorse the study as a value to the community.
A strength of this trial is that a CBPR approach was used to co-design and implement all aspects of the intervention protocols, recruitment, adherence, fidelity, and measurement and data collection strategies. Recruitment occurred in close-knit communities through clan and kinship ties. We utilized adherence and retention strategies based on lessons from our long-standing partnership, and included layered supportive relationships, multi-modal gathering reminders for participants, shared meals, and program incentives. While adapting program delivery to participant circumstances and community events, Báa nnilah included culturally appropriate fidelity assessments to ensure understanding of treatment variations. Strengths of outcome assessment included a mixed methods design.
Limitations of the Báa nnilah evaluation include a relatively short follow-up period of 12 months, lack of acceptable physiological assessments due to funding constraints, lack of intermediate outcome measurement and the lack of available culturally appropriate outcome measures with documented psychometric properties. Our study highlights the need for multi-year longitudinal research for the evaluation of CI self-management interventions and the need for developing and testing culturally appropriate outcome assessments among Indigenous populations [88].
7. Conclusion
CI self-management relies on relationships that cultivate healthy behaviors and build collective resilience. Báa nnilah connects community values and strengths with CI self-management best practices in the context of a partnership that used a CBPR approach. Báa nnilah has the potential to benefit individuals with CI and the larger community through storytelling, oral transmission of health information through intergenerational relationships, and connections with support that fosters improved quality of life.
Acknowledgments
The authors express appreciation for the following financial support: Improving Chronic Illness Management with the Apsáalooke Nation: The Báa nnilah Project, NIH, U01MD010619; our Community Advisory Board, the Montana Healthcare Foundation; the Mountain West Clinical Translational Research Program, NIH U54GM104944. The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health.
Appendix A. Informed consent materials
Appendix B. Notes on statistics
Numerical and graphical descriptive statistics, as well as 95% confidence intervals, summarized the results of recruitment, attendance, and properties of the measures. Effect sizes were estimated to quantify the impacts of the intervention in terms of primary and secondary outcomes. Sample demographics and all outcome measures were summarized by graphical and numerical descriptive statistics with 95% confidence intervals. Bivariate tests (e.g., independent t-tests for continuous and chi-square tests for discrete variables) were used to examine the distributional properties of baseline data within and between the study groups. Outliers and multivariate assumptions of normality, linearity, and homoscedasticity were checked and handled properly as needed.
Multiple Imputation (MI) replaces each missing value with a set of plausible values that represent random errors in the imputation process, so that the standard statistical models of interest (e.g., general linear models) can be estimated based on each imputed (or, “complete”) data set, with parameter estimates and their standard errors eventually combined. All measured variables and information on groups and measurement waves were incorporated into the imputation model and FIML estimation as auxiliary variables, which allowed for greater recovery of the missing data.
Appendix C. Post-program qualitative interview questions
Báa nnilah post-program qualitative interview questions
- How did participating in the Báa nnilah program influence your life?
- Probe if needed: Can you tell me more about that?
- Probe if needed: Can you give me an example?
- How did your Báa nnilah program mentor influence your life?
- What did you learn from your mentor?
- How did the mentor’s teaching style influence your learning?
- What have you shared about the program with family members, community members and others?
- Could you give me some of examples of how you have shared about this program?
- What have you changed about your self-care after participating in the Báa nnilah program?
- What information/tips/techniques from the Báa nnilah program did you apply or are you applying to your own life?
In what ways, if at all, has attending the Báa nnilah program changed how you share about your health with others?
What has changed in your relationships with your family and friends since being in the Báa nnilah program?
- Have you seen your doctor since participating in the program?
- If no, go to “How has this program…”
- If yes, continue to the next question.
- What has changed in your relationship with your doctor since being in the Báa nnilah program?
- How has the communication between you and your doctor changed?
- How has your doctor’s attitude changed since being in Báa nnilah?
- Probe if they don’t mention these: how about their concern and thoroughness?
- How has the doctor’s behavior and treatment toward you changed?
How has this program influenced your feelings of hope toward your health?
Participant was given the list of gathering topics for the next set of questions.
Which parts of the program (which gathering) were most helpful?
Which parts of the program (which gathering) was least helpful?
- What would you change to make the program better for the future?
- What would you add?
- What would you get rid of?
Since starting with the Báa nnilah program, what other support in addition to being in the program has made a difference for your health?
What changes have you noticed in the community as a result of this program?
What do you see for your health for the future?
What information/tips/techniques from the program will you use in the future?
What ideas do you have for the future of the Báa nnilah program in the Crow community?
Footnotes
Confidentiality
Confidentiality statements were signed by each participant, following the review of the confidentiality within the intervention discussed by groups. Aakbaabaaniilea and program staff signed confidentiality agreements.
Public access to data
Data will not be made public, as it is community owned.
Ancillary and post-trial care
No formal ancillary or post-trial care are involved in this intervention.
Dissemination policy
For nearly 25 years, our partnership has a consistent record of disseminating both the processes and the outcomes of our projects to both the local and broader communities. We regularly present our work to the Apsáalooke community in open gatherings and in written form in local publications. We present our work in venues for Indigenous Nations interested in developing community-based research that respects and honors tribal sovereignty and Indigenous strengths. Finally, we submit our work in peer-reviewed journals and book chapters, deliver regional and national presentations, and engage Native American high school, undergraduate, graduate, and post-doctoral students in the research process.
Communication plans for trial results
A publication discussing trial results is in development.
Authorship eligibility statement
Within our CBPR partnership, all authors must have made substantial contributions to the following to be included as an author: 1. Conception and design, or analysis and interpretation 2. Drafting the article or reviewing it critically for important content; and 3. Approval of final version to be published. Individuals with less experience writing for publication qualify as co-authors if, either individually with the lead author or with the entire working group, they are involved with conceptual discussions about the work or interpretation of findings; review and make comments on at least one draft of the paper; and review the final version and give approval.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
To enact critical methodology and pedagogy, scholars and educators recommend using identifiers preferred by specific Indigenous communities (e. g., Crow). However, such usage can be complicated, since individuals within those communities may not identify using the majority affiliation and/or they may prefer a more general term (e.g., Native). We use “Indigenous” and “Native” to encourage solidarity across Nations and to advance broad scale action as well as tribal affiliations when speaking about specific nations (e.g., “Crow” and “Apsáalooke”). Although we occasionally use “Indian” or “American Indian” to align with policy language, we recognize these terms are problematic given their history. Throughout this paper, we use various terms deemed appropriate for specific contexts by Indigenous partners and mentors. Furthermore, we defer to these partners for advice regarding specific spellings of traditional names (e.g., Apsáalooke). We also use the Apsáalooke language throughout as a purposeful way to respect the community and bring it into and lndigenize a colonizing space.
References
- [1].Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, Leon AS, Compendium of physical activities: an update of activity codes and MET intensities, Medicine and science in sports and exercise 32 (9, SUPP/1) (2000) S498–S504. [DOI] [PubMed] [Google Scholar]
- [2].Amparo P, Farr SL, Dietz PM, Peer reviewed: chronic disease risk factors among American Indian/Alaska native women of reproductive age, Prev. Chronic Dis 8 (6) (2011). [PMC free article] [PubMed] [Google Scholar]
- [3].Baanders AN, Heijmans MJ, The impact of chronic diseases: the partner’s perspective, Family & Community Health 30 (4) (2007) 305–317. [DOI] [PubMed] [Google Scholar]
- [4].Barnes PM, Adams PF, Powell-Griner E, Health characteristics of the American Indian or Alaska native adult population, United States (2010) 2004–2008. [PubMed] [Google Scholar]
- [5].Bartlett JG, Iwasaki Y, Gottlieb B, Hall D, Mannell R, Framework for Aboriginal-guided decolonizing research involving Metis and First Nations persons with diabetes, Soc. Sci. Med 65 (11) (2007) 2371–2382. Epub 2007/08/11, 10.1016/j.socscimed.2007.06.011. [DOI] [PubMed] [Google Scholar]
- [6].Bauer UE, Briss PA, Goodman RA, Bowman BA, Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA, Lancet 384 (9937) (2014) 45–52, 10.1016/s0140-6736(14)60648-6. [DOI] [PubMed] [Google Scholar]
- [7].Bell DR, Guskiewicz KM, Clark MA, Padua DA, Systematic review of the balance error scoring system, Sports Health 3 (3) (2011) 287–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Benavent-Caballer V, Lisón JF, Rosado-Calatayud P, Amer-Cuenca JJ, Segura-Orti E, Factors associated with the 6-minute walk test in nursing home residents and community-dwelling older adults, J. Phys. Ther. Sci 27 (11) (2015) 3571–3578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Bjomer JB, Rose M, Gandek B, Stone AA, Junghaenel DU, Ware JE Jr, Method of administration of PRO MIS scales did not significantly impact score level, reliability, or validity, J. Clin. Epiderniol 67 (1) (2014) 108–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Campbell MK, Piaggio G, Elboume DR, Altman DG, for the CONSORT Group, Consort 2010 statement: extension to cluster randomised trials, BMJ (345) (2012), e5661. [DOI] [PubMed] [Google Scholar]
- [11].Cella D, Yount S, Rothrock N, Gershon R, Cook K, Reeve B, Rose M, The Patient-Reported Outcomes Measurement Information System (PROMIS): progress of an NIH Roadmap cooperative group during its first two years, Med. Care 45 (5 Suppl. 1) (2007) S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, PROMIS Cooperative Group, The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008, J. Clin. Epidemiol 63 (11) (2010) 1179–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Centers for Disease Control and Prevention, Tribal Health: Chronic Diseases, Retrieved from, https://www.cdc.gov/tribal/data-resources/information/chronic-diseases.html, 2018.
- [14].Centers for Disease Control and Prevention, Health and Economic Costs of Chronic Diseases, Retrieved from, https://www.cdc.gov/chronicdisease/about/costs/index.htm, 2020.
- [15].Centers for Disease Control and Prevention, About Chronic Diseases, Retrieved from, https://www.cdc.gov/chronicdisease/about/index.htm, 2021.
- [16].Chan A-W, Tetzlaff JM, Altman DG, Laupacis A, Gøtzsche PC, Krleža-Jerić K, Hróbjartsson A, Mann H, Dickersin K, Berlin J, Doré C, Parulekar W, Summerskill W, Groves T, Schulz K, Sox H, Rockhold FW, Rennie D, Moher D, SPIRIT 2013 Statement: defining standard protocol items for clinical trials, Ann. Intern. Med 158 (3) (2013) 200–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Cochran PA, Marshall CA, Garcia-Downing C, Kendall E, Cook D, Mccubbin L, Gover RMS, Indigenous ways of knowing: implications for participatory research and community, Am. J. Public Health 98 (1) (2008) 22–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Cook KF, Jensen SE, Schalet BD, Beaumont JL, Amtmann D, Czajkowski S, Cella D, PROMIS measures of pain, fatigue, negative affect, physical function, and social function demonstrated clinical validity across a range of chronic conditions, J. Clin. Epidemiol 73 (2016) 89–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Dáakuash I, Birdhat-Howe R, McCormick AKHG, Keene S, Hallett J, Held S, Developing an Indigenous goal-setting tool: counting coup, Turtle Island journal of indigenous health 1 (1) (2020) 49. [PMC free article] [PubMed] [Google Scholar]
- [20].Donatuto JL, Satterfield TA, Gregory R, Poisoning the body to nourish the soul: prioritising health risks and impacts in a Native American community, Health Risk Soc. 13 (2) (2011) 103–127, 10.1080/13698575.2011.556186. [DOI] [Google Scholar]
- [21].Donner A, Klar N, Design and Analysis of Cluster Randomization Trials in Health Research, 2000.
- [22].Duran B, The promise of health equity: advancing the discussion to eliminate disparities in the 21st century, in: 32nd Annual Minority Health Conference 8, Chapel Hill, NC, 2011. [Google Scholar]
- [25].Edwards SL, McFadden M, Lanier AP, Murtaugh MA, Ferucci ED, Redwood DG, Slattery ML, Construct validity of the SF-12 among American Indian and Alaska native people using two known scoring methods, J. Health Care Poor Underserved 23 (3) (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Enders CK, Applied Missing Data Analysis, Guilford Press, 2010. [Google Scholar]
- [27].Faul F, Erdfelder E, Lang A-G, Buchner A, G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences, Behav. Res. Methods 39 (2007) 175–191. [DOI] [PubMed] [Google Scholar]
- [28].Fimbel L, Pitts M, Schure M, McCormick A, Held S, Recruitment, retention, and intervention adherence for a chronic illness self-management intervention with the Apsáalooke Nation, 5, 1st ed. Public Health Rev. (2022). [PMC free article] [PubMed] [Google Scholar]
- [29].Gibson R, My body, my earth: The practice of somatic archaeology. IUniverse, 2008. [Google Scholar]
- [30].Golics CJ, Basra MKA, Finlay AY, Salek S, The impact of disease on family members: a critical aspect of medical care, J. R. Soc. Med 106 (10) (2013) 399–407, 10.1177/0141076812472616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Graham JW, Cumsille PE, Shevock AE, Methods for Handling Missing Data, 2013.
- [32].Gruber-Baldini AL, Velozo C, Romero S, Shulman LM, Validation of the PROMIS® measures of self-efficacy for managing chronic conditions, Qual. Life Res 26 (7) (2017) 1915–1924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Hahn EA, DeVellis RF, Bode RK, Garcia SF, Castel LD, Eisen SV, Cella D, Measuring social health in the patient-reported outcomes measurement information system (PROMIS): item bank development and testing, Qual. Life Res 19 (7) (2010) 1035–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Hahn EA, Cella D, Bode RK, et al. , Measuring social well-being in people with chronic illness, Soc. Indic. Res 96 (2010) 381–401, 10.1007/sl1205-009-9484-z. [DOI] [Google Scholar]
- [35].Hahn EA, DeWalt DA, Bode RK, Garcia SF, DeVellis RF, Correia H, Cella D, New English and Spanish social health measures will facilitate evaluating health determinants, Health Psychol. 33 (5) (2014) 490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Hallett J, Held S, McCormick AKHG, Simonds V, Real Bird S, Martin C, Trottier C, What touched your heart? Collaborative story analysis emerging from an Apsáalooke cultural context, Qual. Health Res 27 (9) (2017) 1267–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Harry ML, Waring SC, The measurement invariance of the patient health Questionnaire-9 for American Indian adults, J. Affect. Disord 254 (2019) 59–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Held S, Hallett J, Schure M, McCormick AKHG, Allen S, Milne-Price S, Inouye J, Improving chronic illness self-management with the Apsáalooke Nation: development of the Báa nnilah program, Soc. Sci. Med 242 (2019), 112583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Heron MP, Deaths: Leading Causes for 2010, U.S. Department of Health and Human Services, 2013. [Google Scholar]
- [40].Hibbard JH, Mahoney ER, Stockard J, Tusler M, Development and testing of a short form of the patient activation measure, Health Serv. Res 40 (6pl) (2005) 1918–1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].IBM Corporation, IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0, IBM Corp, Armonk, NY, 2013. [Google Scholar]
- [42].Indian Health Service, Disparities, Indian Health Service, Rockville, MD, 2019. Retrieved from, https://www.ihs.gov/newsroom/factsheets/disparities/. [Google Scholar]
- [43].Inouye J, Enhancing Diabetes Self-Management (Researcher’s Manual, Group A) (Version 7.2), University of Hawai’i School of Nursing and Dental Hygiene, Honolulu, 2005. [Google Scholar]
- [45].Israel BA, Eng E, Schulz AJ, Parker EA, Introduction to Methods for CBPR for Health (No. 4–42), Jossey-Bass, San Francisco, CA, 2013. Retrieved from, http://site.ebrary.com/id/10606033. [Google Scholar]
- [46].Jernigan VB, Community-based participatory research with Native American communities: the Chronic Disease Self-Management Program, Health Promot. Pract 11 (6) (2010) 888–899, 10.1177/1524839909333374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Joe JR, Young RS, Diabetes as a Disease of Civilization: The Impact of Culture Change on Indigenous Peoples 50, Walter de Gruyter, 1994. [Google Scholar]
- [48].Kaufman P, Dicken C, Williams R, Measuring Access to Healthful, Affordable Food in American Indian and Alaska Native Tribal Areas (No. 1476-2017-3886), 2014.
- [49].Kleffelgård I, Langharnmer B, Sandhaug M, Soberg HL, Reliability and validity of the balance error scoring system-BESS, Physiotherapy 101 (2015) e764–e765. [Google Scholar]
- [50].Koch T, Ringel M, 2018 Montana Vital Statistics, 2019. Retrieved from Montana Department of Health and Human Services.
- [51].Kroenke K, Spitzer RL, Williams JB, The PHQ-9: validity of a brief depression severity measure, J. Gen. lntern. Med 16 (9) (2001) 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Lee MC, Validity of the 6-minute walk test and step test for evaluation of cardiorespiratory fitness in patients with type 2 diabetes mellitus, J. Exerc. Nutr. Biochem 22 (1) (2018) 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Lee MJ, Romero S, Liu R, Velozo CA, Gruber-Baldini AL, Shulman LM, Multidimensional PROMlS self-efficacy measure for managing chronic conditions, Appl. Res. Qual. Life (2020) 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Madley Benjamin, Reexamining the American genocide debate: meaning, historiography, and new methods, Am. Hist. Rev 120 (1) (February 2015), 10.1093/ahr/120.l.98. Pages 98–139. [DOI] [Google Scholar]
- [55].Marley TL, Ambiguous jurisdiction: governmental relationships that affect American Indian health care access, J. Health Care Poor Underserved 30 (2) (2019) 431–441, 10.1353/hpu.2019.0039. [DOI] [PubMed] [Google Scholar]
- [57].Minkler M, Wallerstein N, Community-Based Participatory Research for Health: From Process to Outcomes, 2nd edition, Jossey-Bass, San Francisco, CA: San Francisco, CA, 2008. [Google Scholar]
- [58].Mohatt GV, Hazel KL, Allen J, Stachelrodt M, Hensel C, Fath R, Unheard Alaska: culturally anchored participatory action research on sobriety with Alaska Natives, Am. J. Community Psychol 33 (3–4) (2004) 263–273. [DOI] [PubMed] [Google Scholar]
- [59].Moulton P, McDonald L, Muus K, Knudson A, Wakefield M, Ludtke R, Prevalence of Chronic Disease among American lndian and Alaska Native Elders, Center for Rural Health, University of North Dakota, Grand Forks, 2005. [Google Scholar]
- [60].Murray DM, Design and Analysis of Group-Randomized Trials 29, Oxford University Press, USA, 1998. [Google Scholar]
- [61].Murray E, Davis H, Tai SS, Coulter A, Gray A, Haines A, Randomised controlled trial of an interactive multimedia decision aid on benign prostatic hypertrophy in primary care, BMJ 323 (7311) (2001) 493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Narayan K, Hoskin M, Kozak D, Kriska A, Hanson RL, Pettitt DJ, Knowler WC, Randomized clinical trial of lifestyle interventions in Pima Indians: a pilot study, Diabet. Med 15 (1) (1998) 66–72. [DOI] [PubMed] [Google Scholar]
- [64].Nightingale CJ, Mitchell SN, Butterfield SA, Validation of the timed up and go test for assessing balance variables in adults aged 65 and older, J. Aging Phys. Act 27 (2) (2019) 230–233. [DOI] [PubMed] [Google Scholar]
- [65].Nolte S, Osborne RH, A systematic review of outcomes of chronic disease self-management interventions, Qual. Life Res 22 (7) (2013) 1805–1816. [DOI] [PubMed] [Google Scholar]
- [66].Raghupathi W, Raghupathi V, An empirical study of chronic diseases in the United States: a visual analytics approach, lnt. J. Environ. Res. Public Health 15 (3) (2018) 431, 10.3390/ijerphl5030431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].RDevelopment CORE TEAM, A Language and Environment for Statistical Computing, R Foundation for Statistical Computing, Vienna, Austria, 2010. URL, http://www.R-project.org. [Google Scholar]
- [69].Real Bird S, Held S, McCormick A, Hallett J, Martin C, Trottier C, The impact of historical and current loss on chronic illness: perceptions of crow (Apsáalooke) people, lnt J Indig Health 11 (1) (2016) 198–210, 10.18357/ijihl11201614993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Resnick B, Parker R, Simplified scoring and psychometrics of the revised 12-item short-form health survey, Outcomes management for nursing practice 5 (4) (2001) 161–166. [PubMed] [Google Scholar]
- [71].Rikli RE, Jones CJ, The reliability and validity of a 6-minute walk test as a measure of physical endurance in older adults, J. Aging Phys. Act 6 (4) (1998) 363–375. [Google Scholar]
- [72].Robert Wood Johnson Foundation, County Health Rankings & Roadmaps, Retrieved September 13, 2021, from, https://www.countyhealthrankings.org/app/montana/2021/rankings/big-horn/county/outcomes/overall/snapshot, 2021. [Google Scholar]
- [73].Rothrock NE, Hays RD, Spritzer K, Yount SE, Riley W, Cella D, Relative to the general US population, chronic diseases are associated with poorer health-related quality of life as measured by the Patient-Reported Outcomes Measurement lnformation System (PROMIS), J. Clin. Epidemiol 63 (11) (2010) 1195–1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Salsman JM, Lai JS, Hendrie HC, Butt Z, Zill N, Pilkonis PA, Cella D, Assessing psychological well-being: self-report instruments for the NIH Toolbox, Qual. Life Res 23 (1) (2014) 205–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].SAS lnstitute, SAS/IML 9.3 User’s Guide, SAS Institute, 2011. [Google Scholar]
- [76].Schafer JL, Graham JW, Missing data: our view of the state of the art, Psychol. Methods 7 (2) (2002) 147. [PubMed] [Google Scholar]
- [77].Schure M, Allen S, Trottier C, McCormick A, Medicine LO, Castille D, Held S, Daasachchuchik: a trauma-informed approach to developing a chronic illness self-management program for the Apsáalooke people, J. Health Care Poor Underserved 31 (2) (2020) 992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Skolasky RL, Green AF, Scharfstein D, Boult C, Reider L, Wegener ST, Psychometric properties of the patient activation measure among multimorbid older adults, Health Serv. Res 46 (2) (2011) 457–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Small C, The Good Road of Life: Curriculum for Native Families, Retrieved from: http://www.nativeprideus.org/programs.html, 2010.
- [81].Stillwater, Living Well Alaska: Alaska Section of Chronic Disease Prevention and Health Promotion Chronicle, Retrieved from, https://dhss.alaska.gov/dph/Chronic/Documents/Publications/assets/ChroniclesVl-1.pdf, 2007.
- [82].Stillwater, Living Well Alaska: An Evaluation of a Distance Delivery Project, Retrieved from, https://dhss.alaska.gov/dph/Chronic/Documents/Publications/assets/ChroniclesV4-1.pdf, 2012.
- [84].Tuck E, Yang KW, Decolonization is not a Metaphor, Retrieved from, http://decolonization.org/index.php/des/article/view/18630, 2012.
- [85].University of Wisconsin Population Health Institute, Big Hom County, Montana 2021, Retrieved from: https://www.countyhealthrankings.org/app/montana/2021/rankings/big-hom/county/outcomes/overall/snapshot, 2021.
- [86].US Commission on Civil Rights, Broken Promises: Continuing Federal Funding Shortfall for Native Americans, Retrieved from, https://www.usccr.gov/pubs/2018/12-20-Broken-Promises.pdf, 2018.
- [87].Wallerstein N, Duran B, Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity, Am. J. Public Health 100 (Sl) (2010) S40–S46, 10.2105/ajph.2009.184036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [88].Walters K, Johnson-Jennings M, Stroud S, Rasmus S, Charles B, Simeon J, Allen J, Keawe’aimoku Kaholokula J, Look MA, de Silva M, Lowe J, Baldwin JA, Lawrence G, Brooks J, Noonan CW, Belcourt A, Quintana E, Semmens EO, Boulafentis J, Growing from our roots: strategies for developing culturally grounded health-promotion interventions in American Indian, Alaska native, and native Hawaiian communities, Prevention Science 21 (Suppl. 1) (2020) 54–64, 10.1007/sl1121-018-0952-z. Jan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [89].Warne D, Frizzell LB, American Indian health policy: historical trends and contemporary issues, Am. J. Public Health 104 Suppl 3 (Suppl. 3) (2014) S263–S267, 10.2105/AJPH.2013.301682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Warren K, Coulthard F, Harvey P, Elements of successful chronic condition self-management program for Indigenous Australians, in: Proceedings of the Eighth National Rural Health Conference, 2005. [Google Scholar]
- [91].Waters H, Graf M, The Costs of Chronic Disease in the US, 2020. Retrieved from Santa Monica, CA. [Google Scholar]
- [92].Wilson S, Research is Ceremony: Indigenous Research Methods, Femwood Publishing, 2008. [Google Scholar]
- [93].Woodcock C, Korda H, Erdem E, Pedersen S, Klco M, Tollefson E, Chronic Disease Self-management Program (CDSMP) Process Evaluation, IMPAQ International, 2013. [Google Scholar]
- [94].Wu SFV, Liang SY, Wang TJ, Chen MH, Jian YM, Cheng KC, A self-management intervention to improve quality of life and psychosocial impact for people with type 2 diabetes, J. Clin. Nurs 20 (17–18) (2011) 2655–2665. [DOI] [PubMed] [Google Scholar]
- [95].Zuckerman S, Haley J, Roubideaux Y, Lillie-Blanton M, Health service access, use, and insurance coverage among American Indians/Alaska natives and whites: what role does the Indian Health Service play? Am. J. Public Health 94 (1) (2004) 53–59, 10.2105/ajph.94.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Zwarenstein M, Treweek S, Gagnier JJ, Altman DG, Tunis S, Haynes B, Moher D, Improving the reporting of pragmatic trials: an extension of the CONSORT statement, BMJ 337 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]


