Abstract
Spigelian hernias are difficult to detect and palpate during physical examination due to their deeper location. They can be asymptomatic or present with acute complications such as incarceration, strangulation, or bowel obstruction. Here we present a case of a 58-year-old female with history of palpable swelling over the left iliac fossa region with abdominal distension. A computed tomography with oral contrast revealed features suggestive of incarcerated Spigelian hernia with small bowel obstruction, which was later managed with laparoscopic ventral hernia repair and repair of seromuscular tear of the small bowel. Computed tomography is the gold standard for diagnosing the condition and assessing bowel status. Conservative treatment is not effective due to the high likelihood of complications, and surgery is the mainstay of management. The approach to surgery depends on the patient's characteristics, the type of hernia, and the surgeon's experience. Mesh repair is advocated regardless of approach.
Keywords: Computed tomography, Hernia, Incarceration, Mesh, Spigelian, Strangulation
Introduction
Spigelian hernia is a rare type of hernia typically seen in individuals between the ages of 50 and 60 years. While most Spigelian hernias are asymptomatic, they are prone to complications. Spigelian hernia is named after Adrian Van der Spighel, who described the semilunar line (linea spigeli) in 1645 [1], and Klinkosch first described the hernia in 1764 [2]. Spigelian hernia is anterior wall defect in the transverses abdominis muscle lateral to the anterior rectus sheath border along the semilunar line in close proximity to the arcuate line. As this point lacks a posterior rectus sheath owing to be the weakest point [2]. Based on a comprehensive literature review, incarcerated Spigelian hernias are less commonly reported. Therefore, we are presenting a case of a 58-year-old female with posthysterectomy status diagnosed with an incarcerated Spigelian hernia with small bowel obstruction. The patient was managed with laparoscopic ventral wall hernia repair.
Case Presentation
A 58-year-old female presented to the outpatient department with complaints of a painless swelling over the left iliac fossa region that was progressively increasing in size. The swelling was previously reducible but had not been reduced for the past 3 days. She also reported multiple episodes of vomiting, although she had been passing stool and flatus regularly. There was no history of abdominal distension, fever, or shortness of breath. She had a history of total abdominal hysterectomy performed 5 years ago and no history of past medical comorbidities such as COPD, diabetes mellitus, chronic cough, or pelvic organ prolapse. On examination, she was conscious, well-oriented to time, place, and person. Her vitals were normal. Abdominal examination showed a nondistended, nontender abdomen with swelling in the left iliac fossa region. The swelling was nonreducible, firm in consistency, and without a cough impulse. There was a midline scar from previous surgery.
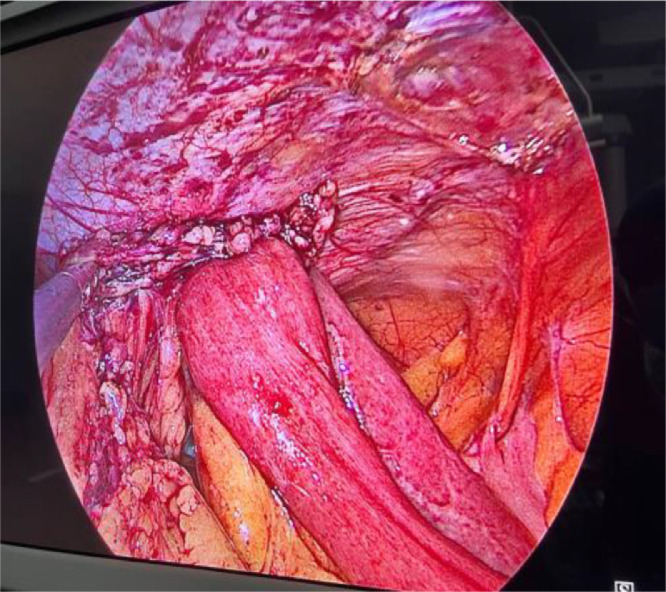
Her routine blood investigations, including complete blood counts, renal function tests, and liver function tests, were within the normal range. X-rays of the abdomen and pelvis in supine and erect views showed dilated bowel loops with air-fluid level. Ultrasound of the abdomen and pelvis showed ∼22 mm defect along peritoneum in the left iliac fossa region with protrusion of intra-abdominal content(bowel loops) through it. There was a dilemma between a Spigelian hernia and an incisional hernia as the patient had a history of total abdominal hysterectomy. Subsequent contrast-enhanced computed tomography (CECT) of the abdomen and pelvis showed a defect of size ∼27.0 mm lateral to the left rectus abdominis muscle along the semilunar lines, transverse abdominis muscle, and internal oblique muscle in the left iliac fossa region with evidence of protrusion of intraabdominal content (distal jejunal bowel loop with its mesentery and omentum). There was dilatation of proximal jejunal loops(Maximum dilatation measures∼ 3.7 cm) with multiple foci of trapped air in between valvulae conniventes with collapsed distal bowel loops. However, there was no evidence of pneumoperitoneum and free fluid in abdomen. Findings were suggestive of Spigelian hernia with small bowel obstruction (Figs. 1 A and B) and patient was planned for surgery. The intraoperative findings revealed a left-sided incarcerated Spigelian hernia with dense omental adhesions containing bowel loops (jejunum), mesentery, and omentum as content (Fig. 2). Bowel loops were found to be viable after reduction from the hernial sac. She underwent laparoscopic ventral hernia repair with repair of the seromuscular layer of the bowel loops for serosal tear (Fig. 3). The postoperative period was uneventful. She was started on oral feeding on the fourth postoperative day. The drain was removed on the fifth postoperative day, and she was discharged on the fifth postoperative day. The patient presented on the 12th postoperative day for staple removal and is recovering well.
Fig. 1.
CECT abdomen and pelvis axial (A) and Sagittal (B) section showing defect of size 27.0 mm (white arrow) with evidence of protrusion of intraabdominal content (distal jejunal bowel loop with its mesentery and omentum) causing the dilatation of proximal jejunal loops with multiple foci of trapped air in between valvulae conniventes with collapsed ileal loops, features suggestive of Spigelian hernia with small bowel obstruction.
Fig. 2.
Intraoperative picture showing protrusion of jejunal loop with its mesentry and omentum likely obstructive Spigelian hernia.
Fig. 3.
Laparoscopic view showing the mesh repair (green arrow) of Spigelian hernia with repair of serosal tear of jejunal loop (white arrow).
Discussion
Spigelian hernias constitute about 0.12% to 0.2% of all abdominal hernias. Most commonly, these hernias are seen between the ages of 50 and 60 years, affecting both sides and both sexes equally [3] as in our case she is a 58 years female. Spigelian hernias are located between the muscle layers of the abdominal wall along the semilunar line. Many terms like lateral ventral [4], interparietal, intermuscular, or intramural hernias [5,6] have been used to describe this entity. The Spigelian aponeurosis is part of the aponeurosis of the transverse abdominal muscle between the linea semilunaris laterally and the lateral edge of the rectus muscle medially [6]. Spigelian hernias are commonly located in the so-called Spigelian hernia belt, a transverse zone of 6 cm located above the interspinal plane [6,7]. Obesity, chronic obstructive pulmonary disease (COPD), abdominal trauma, and abdominal surgery are predisposing factors for the development of Spigelian hernia [8]. The hernia sac usually contains the greater omentum; however, the small intestine, colon, stomach, gallbladder, Meckel's diverticulum, appendix, ovaries, and testes are also observed as contents [9]. The presenting symptoms range from abdominal pain and intermittent swelling in the anterior abdominal wall to signs of intestinal obstruction. As many as 21% may present with small bowel incarceration [10]. Due to its location deep to the external oblique aponeurosis, this type of hernia is complex and challenging to detect and palpate on a physical exam [11]. This kind of hernia is not amenable to conservative treatment due to the high likelihood of complications such as incarceration, strangulation, or bowel obstruction [11]. A computerized tomography (CT) scan of the abdomen with contrast has become the best imaging method for confirming the diagnosis, especially in a diagnostic dilemma [12]. In addition, bowel strangulation can be better identified on a CT [13].In our scenario Contrast Enhanced CT has helped a lot for diagnosis and planning of management . Surgery remains the mainstay of treatment and can be performed through an open or laparoscopic approach. The approach depends upon the patient's characteristics, the type of hernia, and the surgeons experience [14,15]. It was in 1992 when Carter and Mizes performed the first intra-abdominal laparoscopic repair of a Spigelian hernia using sutures to close the defect [16]. The laparoscopic approach has been widely utilized in both elective and emergency repair of the hernia using intra-peritoneal on-lay mesh (IPOM), trans-abdominal preperitoneal (TAPP), and total extra-peritoneal (TEP) techniques. Faster recovery, shorter hospital stays, and lower morbidity render the laparoscopic approach superior to the open approach [17]. According to recent European Hernia Society (EHS) guidelines, mesh repair is recommended regardless of the approach to reduce recurrence [18,19]
Conclusion
Spigelian hernias are difficult to diagnose clinically due to their deeper location. Presentations can vary from asymptomatic to complicated hernias such as incarceration, obstruction, and strangulations. A high degree of suspicion should be maintained for anterior abdominal wall swelling with signs of obstruction. Computed tomography is always the investigation of choice. Surgery remains the mainstay of management; however, the approach depends on the patient's characteristics, the type of hernia, and the surgeon's experience. European Hernia Society (EHS) guidelines recommend mesh repair regardless of the approach to reduce recurrence.
Patient consent
Written informed consent was obtained from patients for publication of this case report and accompanying images. A copy of the written consents is available for review by the Editor in chief of this journal on request.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Pinna A, Cossu ML, Paliogiannis P, Ginesu GC, Fancellu A, Porcu A. Spigelian hernia: a series of cases and literature review. Ann Ital Chir. 2016;87:306–311. [PubMed] [Google Scholar]
- 2.Kelly M.E., Courtney D., McDermott F.D., Heeney A., Maguire D., Geoghegan J.G., et al. Laparoscopic spigelian hernia repair: a series of 40 patients. Surg Laparosc Endosc Percutan Tech. 2015;25(3):e86–e89. doi: 10.1097/SLE.0000000000000112. [DOI] [PubMed] [Google Scholar]
- 3.Citgez B, Yetkin G, Uludag M, Akgun I, Karakoc S. Spigelian hernias treatment and diagnosis in our experience. Ann Ital Chir. 2014;85:610–612. [PubMed] [Google Scholar]
- 4.Houlihan TJ. A review of Spigelian hernias. Am J Surg. 1976;131(6):734–735. doi: 10.1016/0002-9610(76)90191-4. [DOI] [PubMed] [Google Scholar]
- 5.Bennett D., Fitzgibbons RJ., Jr . In: Nyhus and condon's hernia. 5th ed. Greenburg AG, editor. Lippincott Williams & Wilkins; Philadelphia: 2002. Incidence and management of primary abdominal wall hernias: umbilical, epigastric, and spigelian; pp. 389–414. eds. [Google Scholar]
- 6.Spangen L. Spigelian hernia. World J Surg. 1989;13:573–580. doi: 10.1007/BF01658873. [DOI] [PubMed] [Google Scholar]
- 7.Vos DI, Scheltinga MRM. Incidence and outcome of surgical repair of spigelian hernia. Br J Surg. 2004;91:640–644. doi: 10.1002/bjs.4524. [DOI] [PubMed] [Google Scholar]
- 8.Pinna A, Cossu ML, Paliogiannis P, Ginesu GC, Fancellu A, Porcu A. Spigelian hernia. Ann Ital Chir. 2016;87(4):306–311. [PubMed] [Google Scholar]
- 9.Spinelli C., Strambi S., Pucci V., Liserre J., Spinelli G., Palombo C. Spigelian hernia in a 14-year-old girl: a case report and review of the literature. Eur J Pediatr Surg Rep. 2014;2(1):58–62. doi: 10.1055/s-0034-1370771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Srivastava K.N., Agarwal A. Spigelian hernia: a diagnostic dilemma and laparoscopic management. Indian J Surg. 2015;77(Suppl 1):35–37. doi: 10.1007/s12262-014-1085-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huttinger R, Sugumar K, Baltazar-Ford KS. StatPearls Publishing; Treasure Island, FL: 2021. Spigelian hernia. [PubMed] [Google Scholar]
- 12.Foster D., Nagarajan S., Panait L. Richter-type Spigelian hernia: a case report and review of the literature. Int J Surg Case Rep. 2014;11(6):160–162. doi: 10.1016/j.ijscr.2014.10.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xu L, Dulku G, Ho R. A rare presentation of spigelian hernia involving the appendix. Eur J Radiol Open. 2017;9(4):141–143. doi: 10.1016/j.ejro.2017.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hanzalova I, Schäfer M, Demartines N, Clerc D. Spigelian hernia: current approaches to surgical treatment—a review. Hernia. 2021:1–7.. doi: 10.1007/s10029-021-02511-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de la Hermosa AR, Prats IA, Liendo PM, Noboa FN, Calero AM. Spigelian hernia. Personal experience and review of the literature. Rev Esp Enferm Dig. 2010;102(10):5836. doi: 10.4321/s1130-01082010001000003. [DOI] [PubMed] [Google Scholar]
- 16.Patterson A.L., Thomas B., Franklin A., Connor C., Pullatt R. Transabdominal preperitoneal repair of spigelian hernia. Am Surg. 2016;82(1):18–19. [PubMed] [Google Scholar]
- 17.Mittal T., Kumar V., Khullar R., Sharma A., Soni V., Baijal M., et al. Diagnosis and management of spigelian hernia: a review of literature and our experience. J. Minimal Access Surg. 2008;4(4):95–98. doi: 10.4103/0972-9941.45204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Henriksen NA, Kaufmann R, Simons MP, Berrevoet F, East B, Fischer J, et al. AHS guidelines for treatment of primary ventral hernias in rare locations or special circumstances. BJS open. 2020;4(2) doi: 10.1002/bjs5.50252. :342–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Takayama Y., Okada S., Nakatani K., Matsumoto R., Suganuma T., Rikiyama T. The advantage of laparoscopic surgery in the treatment of Spigelian hernia: a report of two cases. Int J Surg Case Rep. 2021;82 doi: 10.1016/j.ijscr.2021.105903. [DOI] [PMC free article] [PubMed] [Google Scholar]