As novel mutations within the Omicron variant of the SARS-CoV-2 virus continue to drive COVID-19 cases globally, the prevalence of chronic complications following infection is likely to rise. Post-COVID-19 condition (or long COVID) is defined by WHO as new or persistent COVID-19 symptoms occurring three months after the onset of illness without an alternate diagnosis.1 Commonly, these include fatigue, dyspnoea, chest pain, headache, memory loss, and neuropsychiatric features such as depression, and anxiety.2
Post-COVID-19 condition affects females more than males and can develop in about 10%–30% of people following acute infection during pregnancy.3 Currently, there are no guidelines for managing obstetric patients with post-COVID-19 condition. We propose an approach to individuals with post-COVID-19 condition who are planning to conceive or are already pregnant (Fig. 1).
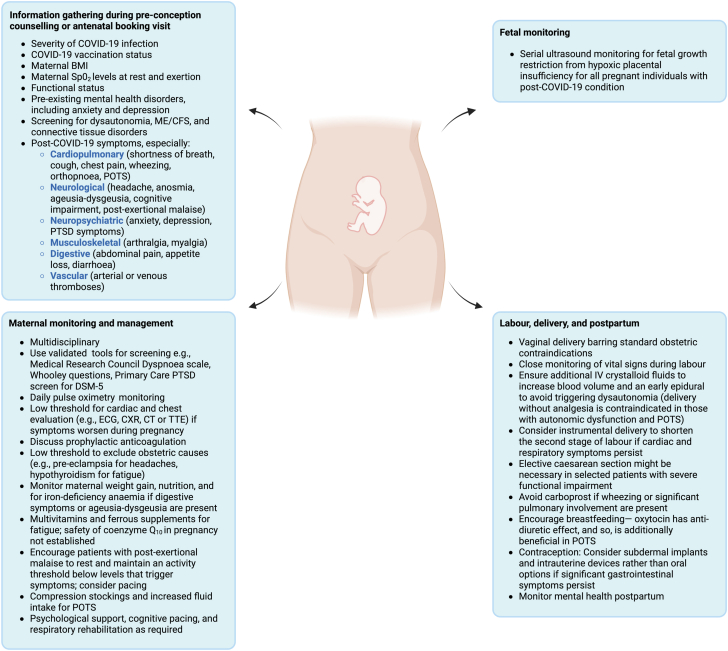
Fig. 1.
Management of post-COVID-19 condition in pregnancy. The management of post-COVID-19 condition in pregnancy is adapted from that in non-pregnant adults.2 BMI, body mass index; CT, computed tomography scan; CXR, chest x-ray; ECG, electrocardiogram; IV, intravenous; ME/CFS, myalgic encephalomyelitis/chronic fatigue syndrome; POTS, postural orthostatic tachycardia syndrome; PTSD, posttraumatic stress disorder; Sp02, peripheral capillary oxygen saturation; TTE, transthoracic echocardiogram. Figure created by the authors with BioRender.com and exported with publication and licensing rights.
Crucially, those with persistent dyspnoea or low oxygen saturations should be evaluated for chronic lung disease, cardiac dysfunction, and venous thromboembolism—sequelae which can occur after moderate-to-severe COVID-19 infection. Such patients must be monitored within a multi-disciplinary team for maternal deterioration with advancing gestation. Further, given that hypercoagulability can occur in post-COVID-19 condition owing to chronic endothelial inflammation, hyperactivated platelets, and fibrinaloid microclots, pregnancies should be assessed for fetal growth restriction from hypoxic placental insufficiency. While headache and chest discomfort are common in post-COVID-19 condition, worsening symptoms must be promptly assessed so as not to miss pregnancy-specific diagnoses such as pre-eclampsia.
In labour, early epidural analgesia and intravenous fluids could prevent autonomic instability in those with postural orthostatic tachycardia syndrome, while planned caesarean delivery might be necessary in individuals with severely reduced effort tolerance and fatigue. Additionally, prostaglandin F2-alpha agonists (carboprost) should be avoided when managing postpartum haemorrhage in patients with significant pulmonary involvement in post-COVID-19 condition, given the drug-related risk of major bronchospasm. Although there are no interventions to prevent the development of post-COVID-19 condition, observational data suggest symptoms might improve following the SARS-CoV-2 vaccine4; in the context of pregnancy, we believe maternal vaccination, including booster doses, with the mRNA or protein subunit COVID-19 vaccine will similarly benefit the pregnant individual and the child.
Finally, we advocate for reporting pregnant individuals with post-COVID-19 condition to international registries and call on obstetric units to prospectively study the impact of post-COVID-19 condition on maternal and neonatal outcomes.5
Contributors
EM, GF, IB, PD, AP, and DB conceptualized the manuscript. EM, PD, and DB did the original draft. EM, GF, IB, PD, AP, and DB wrote the manuscript. EM, GF, IB, PD, AP, and DB reviewed and edited the manuscript.
Declaration of interests
Alice Panchaud has received financial support from the Swiss Federal Office of Public Health to research COVID-19 during pregnancy and from the CHUV foundation for the COVI-PREG registry. Alice Panchaud has received two grants for research on COVID-19 vaccines and medications: i) Safety monitoring of COVID-19 vaccines in the EU—Reopening of competition no. 20 under a framework contract following procurement procedure EMA/2017/09/PE (Lot 3); ii) Efficacy and safety studies on Medicines EMA/2017/09/PE/11, Lot 4, WP 2 lead “Study on impact of COVID-19 infection and medicines in pregnancy”. Isabelle Boucoiran has received a grant from Ferring for a study on COVID-19 in pregnancy and consultant fees from Pfizer and Moderna for immunization in pregnancy unrelated to SARS-CoV-2. All other authors declare no conflicts of interest.
References
- 1.Soriano J.B., Murthy S., Marshall J.C., Relan P., Diaz J.V., WHO Clinical Case Definition Working Group on Post-COVID-19 Condition A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis. 2022;22(4):e102–e107. doi: 10.1016/S1473-3099(21)00703-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davis H.E., McCorkell L., Vogel J.M., Topol E.J. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol. 2023;21(3):133–146. doi: 10.1038/s41579-022-00846-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Munoz-Chapuli Gutierrez M., Prat A.S., Vila A.D., et al. Post-COVID-19 condition in pregnant and postpartum women: a long-term follow-up, observational prospective study. eClinicalMedicine. 2024;67 doi: 10.1016/j.eclinm.2023.102398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ayoubkhani D., Bosworth M.L., King S., et al. Risk of long COVID in people infected with severe acute respiratory syndrome coronavirus 2 after 2 doses of a coronavirus disease 2019 vaccine: community-based, matched cohort study. Open Forum Infect Dis. 2022;9(9) doi: 10.1093/ofid/ofac464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Panchaud A., Favre G., Pomar L., et al. An international registry for emergent pathogens and pregnancy. Lancet. 2020;395(10235):1483–1484. doi: 10.1016/S0140-6736(20)30981-8. [DOI] [PMC free article] [PubMed] [Google Scholar]