Abstract
Background and Hypothesis
Loneliness, the subjective experience of feeling alone, is associated with physical and psychological impairments. While there is an extensive literature linking loneliness to psychopathology, limited work has examined loneliness in daily life in those with serious mental illness. We hypothesized that trait and momentary loneliness would be transdiagnostic and relate to symptoms and measures of daily functioning.
Study Design
The current study utilized ecological momentary assessment and passive sensing to examine loneliness in those with schizophrenia (N = 59), bipolar disorder (N = 61), unipolar depression (N = 60), remitted unipolar depression (N = 51), and nonclinical comparisons (N = 82) to examine relationships of both trait and momentary loneliness to symptoms and social functioning in daily life.
Study Results
Findings suggest that both trait and momentary loneliness are higher in those with psychopathology (F(4,284) = 28.00, P < .001, ηp2 = 0.27), and that loneliness significantly relates to social functioning beyond negative symptoms and depression (β = −0.44, t = 6.40, P < .001). Furthermore, passive sensing measures showed that greater movement (β = −0.56, t = −3.29, P = .02) and phone calls (β = −0.22, t = 12.79, P = .04), but not text messaging, were specifically related to decreased loneliness in daily life. Individuals higher in trait loneliness show stronger relationships between momentary loneliness and social context and emotions in everyday life.
Conclusions
These findings provide further evidence pointing to the importance of loneliness transdiagnostically and its strong relation to social functioning. Furthermore, we show that passive sensing technology can be used to measure behaviors related to loneliness in daily life that may point to potential treatment implications or early detection markers of loneliness.
Keywords: loneliness, social functioning, ecological momentary assessment, depression, bipolar disorder, schizophrenia, mobile sensing
Introduction
Loneliness is estimated to affect up to 20% of the general population with even higher rates in those with psychopathology.1,2 It has been linked to current and future psychopathology3 and identified as a public health crisis.4–6 There is remarkably little research assessing trait and momentary loneliness in those with serious mental illness. A better understanding of the experience of loneliness in daily life is crucial for identifying an unmet treatment need, to determine who may benefit from interventions, and to develop effective interventions. Here, we focus on understanding whether trait loneliness relates to loneliness measured in daily life in those with psychotic and mood disorders. Furthermore, we examine contextual factors of when momentary loneliness occurs and its relationship to symptoms and functioning.
Loneliness is the experience of distress one feels when dissatisfied in one’s social relationships.7 The bulk of research on loneliness utilizes trait measures which ask people to rate their general feelings of loneliness and social isolation. Studies of trait loneliness have identified loneliness as a worldwide phenomenon linked to poor physical and psychological health. For example, trait loneliness is elevated in those with mood8,9 and psychotic disorders.10–14 Elevated trait loneliness has also been shown in psychosis.10–14 In fact, in a survey of people with psychosis, 80% of participants reported feeling lonely and almost 40% identified loneliness as a top challenge.15
Further work is needed to understand how loneliness unfolds in daily life to understand its contexts and correlates better and identify potential treatment paths. Ecological momentary assessment (EMA) studies in psychosis have found that people with psychosis report higher levels of momentary loneliness in daily life relative to nonclinical comparisons16 and that trait loneliness is related to decreased happiness and intimacy during social interactions.14 One study found people with schizophrenia reported lower levels of momentary loneliness when with family and friends suggesting that loneliness may depend on social context.11
Recent work has examined the role passive sensing can play in enhancing our understanding of loneliness.17 While the bulk of this research has taken place in community samples, 1 group found that trait loneliness was related to visiting fewer locations outside the home in those with schizophrenia.13 These studies suggest that movement and time away from home may be important to understanding trait loneliness, however, work must extend these findings to examine the daily experience of loneliness.
Another gap in our knowledge is the relationship between trait and momentary loneliness. The differential reactivity hypothesis18 suggests that those with high trait loneliness respond differently to environments. For example, young adults with high trait loneliness derived less satisfaction from social experiences19 relative to those lower in trait loneliness. Other work suggests that those with high trait loneliness may receive greater benefit from social interactions. For example, older adults with high trait loneliness showed greater decreases in momentary feelings of loneliness following social interactions relative to those with lower trait loneliness.20 Similarly, those with high trait loneliness reported larger boosts of pleasure following positive events.21 It is unclear whether trait loneliness is an important moderator for momentary loneliness in those with serious mental illness.
Current Study
The current study sought to fill several key gaps in the literature by examining both trait and momentary loneliness across mood and psychotic disorders. We hypothesized that: (1) loneliness would be transdiagnostic with greater trait and momentary loneliness in those with mood and psychotic disorders relative to the nonclinical comparison group; (2) trait and momentary loneliness would be positively correlated with depression, experiential negative symptoms, and negative affect; (3) loneliness would relate to interpersonal functioning even when accounting for other symptoms; (4) in daily life, social contact with close others, social contact via phone calls and text messaging, and physical activity would be related to reduced momentary loneliness across participants; and (5) relationships between momentary loneliness, symptoms and functioning would be stronger in those with higher trait loneliness, consistent with the differential reactivity hypothesis.
Methods
Participants
Study participants included: (1) 59 people with schizophrenia/schizoaffective disorder (SZ), (2) 60 people with current major depressive disorder (MDD), (3) 51 people with at least 1 previous episode of major depression remitted for at least 1 month (rMDD), (4) 61 people with bipolar I disorder (BD); and (5) 82 nonclinical comparison participants (CON). Exclusion criteria included: (1) DSM-5 diagnosis of substance abuse or dependence in the past 6 months; (2) IQ less than 70 as measured by the Wechsler Test of Adult Reading22; and (3) history of severe head trauma and/or loss of consciousness. Additional exclusion criteria for clinical groups included: (1) medication changes in the month prior to study participation; (2) inpatient or partial hospital status. Additional criteria for CON included: (1) no personal or immediate relative with a history of schizophrenia, schizoaffective disorder, or bipolar disorder and (2) no current or past major depression. All participants provided written informed consent to the protocol approved by the Washington University Institutional Review Board. Demographics for all groups are in table 1.
Table 1.
Participant Demographic and Clinical Measures
| CON (n = 82) |
SZ (n = 59) |
BD (n = 61) |
MDD (n = 60) |
rMDD (n = 51) |
Group Diffs (P Value) | Pattern | |
|---|---|---|---|---|---|---|---|
| Gender (M:W:NB) | 34:48:0 | 25:34:0 | 21:40:0 | 23:36:1 | 22:29:0 | .71 | |
| Race/ethnicity (n) | <.001 | ||||||
| African American | 40 | 33 | 11 | 22 | 10 | ||
| Caucasian | 38 | 25 | 45 | 37 | 39 | ||
| Additional races | 4 | 0 | 5 | 1 | 2 | ||
| Age | 35.54 (8.89) | 36.15 (8.78) | 37.23 (8.61) | 33.65 (8.39) | 35.57 (8.43) | .25 | |
| Education (y) | 15.54 (2.48) | 13.71 (2.28) | 15.16 (2.51) | 15.07 (2.24) | 16.49 (2.43) | <.001 | rMDD = CON = BD > MDD > SZ |
| Parental education (y) | 13.06 (2.51) | 14.02 (2.64) | 14.79 (3.09) | 15.17 (2.69) | 16.06 (2.98) | <.001 | rMDD > CON = SZ = BD; BD = MDD > HC |
| WTAR FSIQ | 104.28 (9.82) | 100.07 (12.94) | 106.89 (9.88) | 104.53 (10.76) | 109.86 (8.51) | <.001 | BD = rMDD > SZ; rMDD > CON |
| Unmedicated (%) | 100% | 10% | 16% | 29% | 50% | ||
| Antidepressant (%) | 0 | 54% | 70% | 68% | 48% | ||
| Mood stabilizer (%) | 0 | 15% | 59% | 7% | 6% | ||
| Antipsychotic (%) | 0 | 83% | 38% | 10% | 4% | ||
| CPZ | — | 524.43 (426.96) | 333.97 (211.45) | 167.7 (111.7) | 175.0 (35.4) | ||
| CAINS-MAP | — | 14.66 (7.95) | 11.34 (6.46) | 14.45 (5.51) | 9.43 (5.44) | <.001 | SZ = MDD > BD = rMDD |
| CAINS-EXP | — | 2.76 (3.36) | 1.15 (2.39) | 1.65 (1.97) | 1.41 (1.88) | .003 | SZ > BD = MDD = rMDD |
| BPRS Depression | — | 10.07 (4.16) | 10.20 (4.59) | 13.37 (3.18) | 9.10 (3.51) | <.001 | MDD > SZ = BD = rMDD |
| BPRS Positive | — | 10.07 (4.55) | 4.13 (2.10) | 3.45 (0.98) | 3.39 (0.96) | <.001 | SZ > BD = MDD = −rMDD |
| CES-D | 5.13 (3.01) | 11.83 (6.64) | 12.30 (6.07) | 15.23 (5.44) | 10.18 (5.08) | <.001 | MDD > SZ = BD > rMDD > CON |
| MAP-SR | 39.99 (9.71) | 32.31 (12.01) | 32.98 (10.75) | 29.88(9.41) | 36.53 (8.94) | <.001 | MDD < SZ = BD = rMDD < CON |
| UCLA Loneliness | 36.81 (8.65) | 52.77 (11.53) | 51.04 (10.69) | 53.64 (11.05) | 46.53 (12.04) | <.001 | MDD = SZ = BD > rMDD > CON |
Note: BD, bipolar disorder; BPRS, Brief Psychiatric Rating Scale; CAINS-EXP, expression subscale; CAINS-MAP, Clinical Assessment Interview for Negative Symptoms Motivation and Pleasure Subscale; CES-D, Center for Epidemiologic Studies-Depression; CON, nonclinical comparison; CPZ, Chlorpromazine equivalent dose; MAP-SR, Motivation and Pleasure Scale—Self-Report; MDD, current major depressive disorder; rMDD, remitted major depressive disorder; gender and race were self-reported; SZ, schizophrenia; UCLA Loneliness Scale; WTAR, Wechsler Test of Adult Reading.
Diagnostic and Symptom Assessment
Diagnostic status was confirmed using the Structured Clinical Interview for DSM-5 conducted by masters or PhD-level clinicians. Clinician-rated negative symptoms were assessed in all clinical groups using the Clinical Assessment Interview for Negative Symptoms (CAINS),23 which includes a Motivation and Pleasure (MAP) and Expression (EXP) subscale. General psychiatric symptoms were assessed using the Brief Psychiatric Rating Scale (BPRS)24 which includes a subscale of psychotic symptoms and depression.
Participants completed the UCLA Loneliness Scale—Revised to measure trait loneliness.25 Participants completed the Motivation and Pleasure Scale (MAP-SR)26 with higher scores equaling more motivation and pleasure across the week. Depression was assessed using the Center for Epidemiological Studies Depression Scale (CES-D).27 Participants completed the self-report version of the Specific Levels of Functioning Scale (SLOF).28 The SLOF includes subscales for functioning in interpersonal relationships, social acceptability, and participation in community/work activities, with higher scores meaning better functioning.
Procedure
Participants completed session 1 which included a diagnostic interview and clinician-rated assessment of symptoms in clinical groups and were trained on the EMA survey. In addition to EMA surveys, participants that had Android phones were enrolled in an additional study component that assessed passive sensing for 2 weeks. These participants were trained to use the Garmin and Crosscheck app at their session. Following 2 weeks of EMA, participants completed self-reported assessments of prior week symptoms.
Ecological Momentary Assessment
The EMA questionnaire included questions related to behaviors and emotions (table 2). Participants were prompted to complete the EMA questionnaire 4 times per day for 14 days between 9:30 am and 8:30 pm on their smartphone. Questionnaires occurred pseudorandomly approximately every 3 hours. Only questionnaires that were submitted within 20 minutes of EMA prompt were included in the current analyses. Mean response rates were 84% (SD = 18%) and did not differ by group (F(4,295) = 0.83, P = .51). All participants included completed at least 33% of surveys.
Table 2.
Ecological Momentary Assessment Questionnaire and Responses
| EMA Domains Assessed | Responses |
|---|---|
| Social contact | |
| Who are you with right now? | Alone, Stranger, Family, Friend, Partner, Coworker Coded alone (−1): alone/stranger; Close others (1): family/friend/partner |
| Momentary loneliness | |
| How lonely do you feel right now? | Not at all (1) to Extremely (5) |
| EMA-MAP Composite (average of current and anticipated MAP questions at each time point) | |
| Current MAP: (1) How interested are you in these activities? (2) How much are you enjoying these activities? | Not at all (1) to Extremely (5) |
| Anticipated MAP: (1) How interested do you think you will be in these activities? (2) How much do you think you will enjoy these activities? | Not at all (1) to Extremely (5) |
| Positive emotion (average of all 3 questions at each time point) | |
| (1) How happy are you right now? (2) How excited are you right now? (3) How hopeful are you right now? | Not at all (1) to Extremely (5) |
| Negative emotion (average of all 3 questions at each time point) | |
| (1) How anxious are you right now? (2) How angry are you right now (3) How sad are you right now? | Not at all (1) to Extremely (5) |
Note: EMA, ecological momentary assessment; MAP, motivation and pleasure.
Passive Sensing
Participants that had Android phones capable of measuring passive sensing were included in the present study to investigate passive sensing data during the 2-week EMA period. This subset of participants (51 CON, 40 SZ, 44 BD, and 47 MDD) provided passive sensing using the Crosscheck29 platform including geolocation measures of the number of unique places visited daily and phone calls/text messaging. Crosscheck is a smartphone sensing application that runs in the background on Android phones and passively collects data. Participants also wore a Garmin Vivosmart 4 fit watch on their nondominant arm to track steps, heart rate, and sleep throughout the 2-week EMA assessment period. We focused on daily step count as a measure of physical activity and on the number of phone calls made/received and number of text messages sent/received as a measure of social behavior. Demographic information for just those in the Passive Sensing Group is presented in supplementary table 1.
Data Analysis
Trait Level Analyses
A univariate ANOVA with total score on the UCLA Loneliness Scale as a dependent variable and diagnostic group (CON, SZ, BD, MDD, and rMDD) as an independent variable examined group differences in trait loneliness. Multiple regression analyses with UCLA trait loneliness as the dependent variable and symptoms as predictors examined relationships between symptoms and loneliness, with group as a factor. Multiple regression analyses were conducted with the SLOF subscales as dependent variables and UCLA Loneliness, CAINS MAP and EXP, BPRS depression, and BPRS Psychotic symptoms as predictors to determine the independent association between loneliness and functioning accounting for other symptoms.
EMA Analyses/Sensing Data Analysis
We used multilevel modeling in the lme4 package for R to investigate relationships between within-subject observations of EMA (level 1) and between-subject observations including symptoms and levels of functioning (level 2), investigating the following questions: (1) does momentary loneliness differ across groups, (2) does trait level loneliness relate to momentary loneliness, (3) do momentary symptoms and emotions relate to momentary loneliness, (4) does who a person is with (close others vs alone/strangers) relate to momentary loneliness, and (5) do passive sensing measures (activity, unique location, phone contact via calls/texts) relate to momentary loneliness. Group was included as a factor. Momentary loneliness was the dependent variable with predictor variables that varied randomly across participants. To test the differential reactivity hypothesis, we ran all models with trait loneliness as a cross-level interaction. We also examined whether interactions between group and trait loneliness improved the model fit.
Results
Demographic Differences
As shown in table 1, there were significant differences in race/ethnicity, education, parental education, and WTAR by group. We examined whether demographic variables were related to outcome measures and found no significant associations between demographic variables and trait loneliness (age: r = .030, P = .57; WTAR: r = −.007, P = .91; parental education: r = −.024, P = .68; personal education: r = −.005, P = .94; race: r = .04, P = .54). Furthermore, there were no significant associations between demographic variables and momentary loneliness (age: β = 0.005, P = .42; WTAR: β = 0.003, P = .62; parental education: β = −0.02, P < .19; personal education: β = −0.03, P = .16; race: β = −0.11, t = 9.09, P = .18).
Group Differences in Trait Loneliness
We found a main effect of Group (F(4,284) = 31.19.00, P < .001, ηp2 = 0.30) with all clinical groups (SZ, BD, MDD, and rMDD) reporting higher levels of trait loneliness relative to CON (figure 1). The rMDD group reported greater trait loneliness than the nonclinical comparison group, but less relative to all other clinical groups (Ps > .15). There were no significant differences between SZ, BD, and MDD (Ps > .20). There were no significant relationships between demographic variables and loneliness.
Fig. 1.
All clinical groups report higher trait-level loneliness as measured by the UCLA Loneliness scale, relative to nonclinical comparisons. Those with remitted depression (rMDD) report less trait loneliness, relative to active clinical groups.
Trait Loneliness, Symptoms, and Functioning
In clinical groups, a regression with CAINS MAP, CAINS EXP, BPRS Positive Symptoms, BPRS Depression, and Group to predict trait loneliness was significant (r = .57, r2 = .32, F(5,255) = 20.24, P < .001) with CAINS MAP, BPRS Positive, and BPRS Depression domains simultaneously significantly predicting loneliness (ts > 2.87, Ps < .005), while CAINS EXP was not a significant predictor (t = −1.53, P = .13). Group was not a significant predictor of loneliness (r = .10, P = .17), and did not interact with symptom measures (Ps < .14), indicating transdiagnostic relations. Both self-reported depression (t = 9.89, β = 0.48, P < .001) and motivation and pleasure (t = −7.11, β = −0.33, P < .001) significantly predicted loneliness (overall model: r = .74, r2 = .55, F(3,307) = 123.92, P < .001). There were no significant interactions between symptoms and group (Ps > .20). Thus, depression and motivation and pleasure were related to trait loneliness across people regardless of diagnostic status.
We next examined whether trait loneliness related to interpersonal functioning while taking other symptoms into account. Even with BPRS depression, BPRS psychosis, and CAINS MAP in the model, loneliness significantly predicted interpersonal functioning across all clinical groups (table 3). For SLOF Social Acceptability, only trait loneliness was a significant predictor of functioning.
Table 3.
Symptoms and Loneliness Predicting Functioning
| Predictor | Standardized Beta | t | P |
|---|---|---|---|
| Model 1: Interpersonal Relationships | |||
| CAINS-MAP | −0.28 | −4.06 | <.001 |
| BPRS Depression | −0.02 | −0.28 | .78 |
| BPRS Psychosis | 0.04 | 0.70 | .49 |
| UCLA Loneliness | −0.44 | −6.40 | <.001 |
| Model 2: Social Acceptability | |||
| CAINS-MAP | 0.03 | 0.40 | .69 |
| BPRS Depression | −0.09 | −1.06 | .29 |
| BPRS Psychosis | −0.04 | −0.46 | .65 |
| UCLA Loneliness | −0.20 | −2.20 | .03 |
| Model 3: Community Functioning | |||
| CAINS-MAP | −0.24 | −2.91 | .004 |
| BPRS Depression | −0.07 | −0.84 | .40 |
| BPRS Psychosis | −0.58 | −3.47 | <.001 |
| UCLA Loneliness | −0.11 | −1.32 | .19 |
Note: BPRS, Brief Psychiatric Rating Scale; CAINS-MAP, Clinical Assessment Interview for Negative Symptoms Motivation and Pleasure Subscale.
Thus, all clinical groups reported higher levels of trait loneliness relative to the nonclinical comparison group, and loneliness was related to depression and motivation and pleasure negative symptoms across diagnostic groups. Loneliness predicted social and interpersonal functioning even when other symptoms were included in models, suggesting an independent relationship between trait loneliness and social functioning across diagnostic groups.
Loneliness in Daily Life
Consistent with trait-level analyses, people with mood and psychotic disorders reported more loneliness throughout their day relative to CON (Ps < .01). There were no significant relationships between demographic variables and momentary loneliness (Ps > .12). The BD group (β = 0.27, t = 2.13, P = .03) and MDD group (β = 0.31, t = 2.43, P = .02) reported significantly more loneliness in daily life relative to the rMDD group. There were no significant differences between the SZ, BD, and MDD groups (Ps > .18). Trait loneliness significantly related to momentary loneliness (β = 0.34, t = 9.77, P < .0001) suggesting convergent validity. Both trait loneliness and the group factor continued to predict momentary loneliness (all Ps < .005) when in the same model, with all of the clinical groups reporting greater momentary loneliness than CON even when accounting for trait loneliness. There were no significant interactions between trait loneliness and group.
Momentary Loneliness, Symptoms, Functioning, and Emotion
In a model across all participants (clinical and nonclinical groups) using both CES-D depression and MAP-SR motivation and pleasure self-reports to predict momentary loneliness, depressive symptoms related to momentary loneliness (β = 0.40, t = 9.09, P < .001) while motivation and pleasure did not (β = −0.001, t = −0.03, P = .98). However, there was a significant interaction between depression and motivation and pleasure symptoms (β = −0.12, t = −4.24, P < .0001) with momentary loneliness greater in those with both high depression and low motivation and pleasure. There were no interactions or main effects of group (Ps > .19) suggesting a transdiagnostic relationship between depression, motivation, and pleasure and momentary loneliness.
In regards to emotion in daily life, both lower momentary positive emotion (β = −0.13, t = −18.58, P < .0001) and greater negative emotion (β = 0.31, t = 41.95, P < .0001) related to greater momentary loneliness across both clinical and nonclinical comparison groups. There were no interactions with group suggesting transdiagnostic effects of positive and negative emotion on loneliness. EMA-MAP ratings were also significantly related to momentary loneliness (β = −0.15, t = −22.50, P < .0001) such that when individuals felt more motivation and pleasure they simultaneously felt less momentary loneliness even when group was in the model. There were also significant interactions between EMA-MAP and each clinical group (Ps < .0001) suggesting that the link between momentary loneliness and motivation/pleasure was stronger in the clinical groups relative to the nonclinical comparison groups.
In terms of functioning, SLOF Social Interaction scale scores significantly related to momentary loneliness (β = −0.13, t = −2.90, P = .004) as did SLOF Social Acceptability scores (β = −0.11, t = −2.48, P = .01). There were no interactions with group and functioning. Thus, across all participant groups, domains of functioning relating to social interaction and communication related to momentary loneliness in daily life even across group boundaries.
Does Trait Loneliness Moderate Relationships With Momentary Loneliness
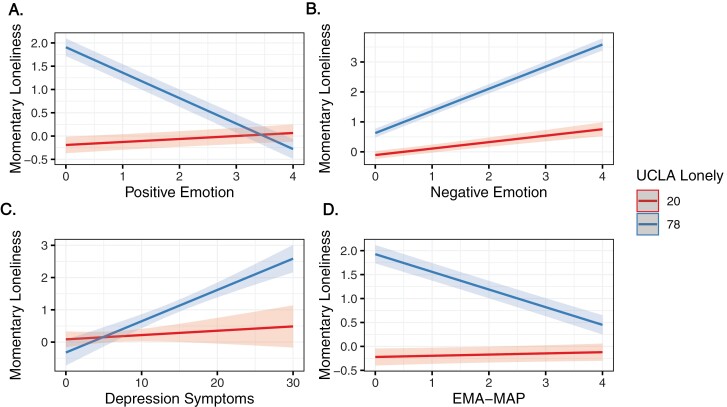
We then examined whether predictors of momentary loneliness differed in those with high vs lower trait loneliness to test the differential reactivity hypothesis. There were interactions of trait loneliness with both MAP-SR (β = −0.10, t = −3.04, P = .003) and depression (β = 0.10, t = 3.42, P = .0007)—in both cases symptoms and momentary loneliness were more strongly related in those with high trait loneliness. Trait loneliness also interacted with both positive (β = −0.13, t = −17.37, P < .0001) and negative affect (β = 0.08, t = 11.58, P < .0001), such that those with high trait loneliness got a bigger boost in positive affect when feeling less lonely and a bigger increase in negative affect when feeling lonelier (figure 2). EMA-MAP showed a similar interaction (β = −0.08, t = −11.86, P < .0001), with EMA-MAP again being most relevant to momentary loneliness in those with high trait loneliness. There was only a single nominally significant interaction with group (negative affect), and all models with group interactions fit the model worse than the models without interaction terms.
Fig. 2.
Plots showing models testing differential reactivity hypothesis. Models testing the differential reactivity hypothesis examining whether predictors of momentary loneliness differ in those with high vs lower trait loneliness. Trait loneliness interacted with both positive and negative affect when relating to momentary loneliness such that those with high trait loneliness showed a tighter link between affect and momentary loneliness (panels A and B). Similarly, motivation and pleasure and depression symptoms were more strongly related to momentary loneliness (panels C and D). All findings were similar across groups.
In assessing relationships between functioning and trait loneliness, there was no significant interaction between SLOF Interpersonal and trait loneliness (β = −0.04, t = −1.06, P = .29). However, SLOF Social Acceptability interacted with trait loneliness (β = 0.08, t = 2.01, P = .046) with stronger relations to momentary loneliness in those with low trait loneliness. There were no interactions with group and the model including group interactions fit the data worse than those without.
Thus, overall, even when accounting for group status and trait loneliness, symptoms, and momentary affect related to momentary loneliness in daily life. Furthermore, interactions with trait loneliness suggest that these relationships were especially strong in those with high trait loneliness for most relations.
Relationships Between Momentary Loneliness and Social Context
Consistent with previous research, there was a main effect of social context (β = −0.19, t = −15.17, P < .001) suggesting that across groups people reported feeling lonelier when alone or with strangers relative to when they were with close others. Furthermore, there was an interaction between context and each clinical group (β = −0.33, t = −8.91, P < .001), such that relationships were stronger in the clinical groups than in CON. There was also a significant interaction with trait loneliness, such that social context mattered more for momentary loneliness for those with high trait loneliness (β = −0.09, t = −7.34, P < .001).
Relationships Between Momentary Loneliness and Passive Sensing
Both daily steps (β = −0.56, t = −3.29, P = .02) and unique locations (β = −0.19, t = −2.37, P = .03) significantly predicted loneliness such that more movement and places visited throughout a day related to lower loneliness in daily life across all participants regardless of group status. There were no interactions with group or trait loneliness in these models. Furthermore, only number of phone calls (β = −0.22, t = −2.79, P = .04) related to lower levels of loneliness across participants while the number of text messages (β = −0.001, t = 0.29, P = .77) was not related to state loneliness. There were no significant interactions between group or trait loneliness (β = 0.01; P = .50).
Discussion
Loneliness is a worldwide epidemic associated with premature mortality and psychopathology30 including being recognized as a profound threat to physical and mental well-being in the 2023 US Surgeon General Report.6 Indeed, feelings of loneliness predict future psychopathology, poorer functioning, and increased risk of hospitalization.4,31 While loneliness is recognized as a public health crisis, there is limited understanding of how loneliness unfolds in daily life in those with serious mental illness. We found strong evidence that despite not being a symptom of mood and psychotic disorders, both trait and momentary loneliness are elevated in these groups relative to the nonclinical comparisons. Loneliness was related to reduced functioning independent of other symptoms, pointing to the critical need for assessing and targeting loneliness. Furthermore, we found that passive sensing measures obtained via mobile technology relate to self-reported loneliness pointing to potential outlets for both assessment and intervention. Across most analyses, relationships between affect, symptoms, and momentary loneliness were strongest in those with high trait loneliness. This provides strong support for the differential reactivity hypothesis suggesting that those with high trait loneliness show differential patterns of responding to social experiences relative to those low in trait loneliness.
The current study is the first to our knowledge that examines both trait and momentary loneliness in daily life across mood and psychotic disorders. Consistent with our hypotheses, we found that each clinical group showed elevated trait and momentary loneliness relative to the comparison group. It is perhaps remarkable that loneliness is so prevalent across all clinical groups in this study. However, given that mood and psychotic disorders are characterized by social impairments it is perhaps understandable. Given the stigma of mental illness, it may be that those in the clinical groups feel this sense of loneliness in part by being perceived as different or not understood. Indeed, in a qualitative study of young adults with depression, research showed that stigma from others and internal stigma was related to feelings of loneliness and isolation.32
Even though people with remitted depression reported less loneliness than clinical groups with active symptoms, they reported greater levels of loneliness relative to the comparison group. This is consistent with work demonstrating that those with remitted depression show continued social impairments33 and show increased negative affect to social stress.34 Given that loneliness is a predictor of future mood episodes in a general population35 and a risk factor for maintenance of depression,8 it will be important for future research to examine whether loneliness in remitted depression predicts future episodes.
Strikingly, there were no significant differences in loneliness across the other clinical groups, and very few interactions with group. Furthermore, trait loneliness was predictive of social acceptability and interpersonal functioning even after accounting for depression, negative symptoms, and psychosis across disorders. While the social acceptability scale reflects a tendency to get into verbal or physical altercations, the interpersonal functioning scale assesses one’s ability to initiate and maintain communication and friendships with others. It will be important to consider other factors that may relate to loneliness that may be driving these relationships, such as comfort with others, social anxiety, and paranoia. For example, it may be that those with high social anxiety score lower on measures of interpersonal relationships and also report feelings of loneliness. Identifying these relationships and potential constructs that relate to loneliness may help identify potential treatment targets. These findings highlight the importance of better understanding how loneliness unfolds in daily life and identifying potential treatments for addressing loneliness across diagnoses along with detecting related constructs that might be mediating or maintaining these relationships. Indeed, while loneliness has been identified as a top treatment need by people with psychosis,15 it is not a component of most standard treatments for psychosis or mood disorders.
We also examined whether social contact may be important for understanding momentary loneliness. Momentary loneliness in those with mood and psychotic disorders was reduced when around close others, consistent with work demonstrating this effect in schizophrenia11 and in aging adults.20 The number of phone calls made/received throughout the day also related to reduced momentary loneliness, while number of text messages made/received was not. This distinction in contact type may suggest that social contact requiring a higher level of engagement and depth of conversation may have more impact on momentary loneliness. These findings are consistent with other work suggesting that level of engagement may be particularly tied to momentary loneliness11 and that social engagement relates to reduced trait loneliness.14 Furthermore, both the number of unique places visited and number of steps taken in a day related to reduced momentary loneliness. These findings point to potential treatments for loneliness and specifically argue for treatments geared toward engaging in activities with close others. Consistent with some studies investigating links between physical activity and loneliness,36 physical activity may be a potential intervention for loneliness. However, it will be important to clarify the active ingredient. As some have hypothesized, social activity (eg, group class, coach) during physical activity may moderate relationships found between reduced loneliness and physical activity.37
Finally, the differential reactivity hypothesis suggests that those with high trait loneliness respond differently to social environments relative to those with low trait loneliness.18,38 Our findings are consistent with this idea, showing that emotion and social context are more tightly linked to momentary loneliness in those high in trait loneliness. For example, being around close others seems to be more influential in modulating momentary loneliness and thus significantly reducing momentary loneliness in those with higher trait loneliness. These relationships did not differ or interact with group, suggesting important transdiagnostic relationships. These findings point to the potential for interventions to target momentary loneliness by suggesting that momentary loneliness can be modulated especially in those with high trait loneliness. This is the first study to our knowledge to extend this theory to those with mood and psychotic disorders and highlights the need for understanding both trait and momentary loneliness.
There are a number of important future directions from the current findings. For example, we did not include a measure of current social network or assess desire for change in social relationships. While one might assume that feeling lonely is related to having a small social network, the feeling of loneliness is defined as the subjective experience of feeling alone, thus it may or may not be consistent with an individual’s actual social network. Mechanisms driving loneliness are also important to consider. For example, Cacioppo and Hawkley39 posited that those with high trait loneliness view the social world as more threatening and have negative cognitive appraisals about others, which may serve to reinforce isolation and feelings of loneliness. Indeed, work has found that lonely individuals tend to pay more attention to negative social stimuli40 and a study including functional imaging showed increased activation in the visual cortex when viewing negative social stimuli relative to negative nonsocial stimuli among those reporting loneliness.41 Studies that assess cognitive biases and attention to negative social stimuli both at trait and momentary levels as they unfold in daily life level would help identify potential mechanisms that serve to maintain loneliness. Should such cognitive appraisals be driving loneliness, interventions could involve identifying maladaptive cognitions and challenging such thought processes. Similarly, we did not have a measure of social anxiety in the current study. While previous work has shown that loneliness shows a distinct neural and behavioral pattern relative to social anxiety,42 it will be important to examine the relationship between social anxiety and loneliness in daily life. Finally, an important next step will be examining feelings of momentary loneliness as social interactions unfold. While the current findings suggest that more phone calls are related to reduced momentary loneliness, novel EMA designs should assess emotional responses following these social interactions to get a more fine-grained idea of how emotions and levels of momentary loneliness may be impacted, and how other mechanisms such as social anxiety are related to more immediate social interactions.
The present study had several limitations. First, the study tracked momentary response over a relatively short period (2 weeks). Future research is needed to assess relations over larger time intervals. Second, the measure of the quality of social context (social closeness) was limited by the categorization of close others. While this is similar to previous research, it would be beneficial to have participants categorize the closeness of the relationship and the quality of the interactions themselves to further our understanding of how quality of interaction relates to feelings of loneliness. Finally, we did not collect height and weight measurements for participants, thus could not examine the relationships between body mass index and loneliness. Given previous research suggesting a potential link between loneliness and obesity,43 this will be an important future direction.
In summary, the current findings point to people with psychosis and mood disorders experiencing greater levels of both trait and momentary loneliness which is related to important markers of daily functioning. Despite loneliness not being an official diagnostic symptom of mood or psychotic disorders, it represents a critical target for intervention. Indeed, loneliness was identified as one of the top challenges people with psychosis face during recovery.44,45 Interventions incorporating time spent with close others, engaging in activities such as phone calls that require a certain level of engagement, and movement may be particularly helpful. The findings also suggest that those with high trait loneliness may show stronger links between various daily contexts and momentary loneliness thus suggesting intervention may be particularly beneficial toward those high in trait loneliness.
Supplementary Material
Acknowledgments
We thank the participants in this study who gave generously of their time. We also thank those that helped with all aspects of data collection including Julia Ermel, Stephanie Gombas, Sofia Mora, Katie Pereira, Eric Prager, and Emily Thomason. Parts of this article have been reported in presentation at the Society for Research in Psychopathology conference. The authors have declared that there are no conflicts of interest in relation to the subject of this study.
Contributor Information
Erin K Moran, Department of Psychological & Brain Sciences, Washington University in St. Louis, St. Louis, MO, USA.
Madelyn Shapiro, Department of Psychological & Brain Sciences, Washington University in St. Louis, St. Louis, MO, USA.
Adam J Culbreth, Department of Psychiatry, Maryland Psychiatric Research Center, University of Maryland, Baltimore, MD, USA.
Subigya Nepal, Department of Computer Science, Dartmouth College, Hanover, NH, USA.
Dror Ben-Zeev, Department of Psychiatry, BRiTE Center, University of Washington, Seattle, WA, USA.
Andrew Campbell, Department of Computer Science, Dartmouth College, Hanover, NH, USA.
Deanna M Barch, Department of Psychological & Brain Sciences, Washington University in St. Louis, St. Louis, MO, USA; Department of Psychiatry, Washington University School of Medicine, St. Louis, MO, USA; Department of Radiology, Mallinckrodt Institute of Radiology, Washington University School of Medicine, St. Louis, MO, USA.
Funding
This work was supported by the National Institute of Mental Health R37 MH066031.
References
- 1. Masi CM, Chen HY, Hawkley LC, Cacioppo JT.. A meta-analysis of interventions to reduce loneliness. Personal Soc Psychol Rev. 2011;15(3):219–266. doi: 10.1177/1088868310377394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Surkalim DL, Luo M, Eres R, et al. The prevalence of loneliness across 113 countries: systematic review and meta-analysis. BMJ. 2022;376:e067068. doi: 10.1136/bmj-2021-067068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA.. Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychol Aging. 2006;21(1):140–151. doi: 10.1037/0882-7974.21.1.140 [DOI] [PubMed] [Google Scholar]
- 4. Jeste DV, Lee EE, Cacioppo S.. Battling the modern behavioral epidemic of loneliness: suggestions for research and interventions. JAMA Psychiatry. 2020;77(6):553–554. doi: 10.1001/jamapsychiatry.2020.0027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Na PJ, Jeste DV, Pietrzak RH.. Social disconnection as a global behavioral epidemic—a call to action about a major health risk factor. JAMA Psychiatry. 2023;80(2):101–102. doi: 10.1001/jamapsychiatry.2022.4162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Murthy V. Our Epidemic of Loneliness and Isolation: The U.S. Surgeon General’s Advisory on the Healing Effects of Social Connection and Community. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service, Office of the Surgeon General; 2023. [PubMed] [Google Scholar]
- 7. Hawkley LC, Cacioppo JT.. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40(2):218–227. doi: 10.1007/s12160-010-9210-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Erzen E, Çikrikci O.. The effect of loneliness on depression: a meta-analysis. Int J Soc Psychiatry. 2018;64(5):427–435. doi: 10.1177/0020764018776349 [DOI] [PubMed] [Google Scholar]
- 9. Lee CN, Huang YL, Chang HH, et al. Associations of emotion recognition, loneliness, and social functioning in euthymic patients with bipolar disorder. Kaohsiung J Med Sci. 2022;38(7):703–711. doi: 10.1002/kjm2.12539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Badcock JC, Shah S, Mackinnon A, et al. Loneliness in psychotic disorders and its association with cognitive function and symptom profile. Schizophr Res. 2015;169(1):268–273. doi: 10.1016/j.schres.2015.10.027 [DOI] [PubMed] [Google Scholar]
- 11. Culbreth AJ, Barch DM, Moran EK.. An ecological examination of loneliness and social functioning in people with schizophrenia. J Abnorm Psychol. 2021;130(8):899–908. doi: 10.1037/abn0000706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Eglit GML, Palmer BW, Martin AS, Tu X, Jeste DV.. Loneliness in schizophrenia: construct clarification, measurement, and clinical relevance. PLoS One. 2018;13(3):e0194021. doi: 10.1371/journal.pone.0194021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fulford D, Mote J, Gonzalez R, et al. Smartphone sensing of social interactions in people with and without schizophrenia. J Psychiatr Res. 2021;137:613–620. doi: 10.1016/j.jpsychires.2020.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mote J, Gard DE, Gonzalez R, Fulford D.. How did that interaction make you feel? The relationship between quality of everyday social experiences and emotion in people with and without schizophrenia. PLoS One. 2019;14(9):e0223003. doi: 10.1371/journal.pone.0223003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Stain HJ, Galletly CA, Clark S, et al. Understanding the social costs of psychosis: the experience of adults affected by psychosis identified within the second Australian national survey of psychosis. Aust N Z J Psychiatry. 2012;46(9):879–889. doi: 10.1177/0004867412449060 [DOI] [PubMed] [Google Scholar]
- 16. Kimhy D, Vakhrusheva J, Jobson-Ahmed L, Tarrier N, Malaspina D, Gross JJ.. Emotion awareness and regulation in individuals with schizophrenia: implications for social functioning. Psychiatry Res. 2012;200(2–3):193–201. doi: 10.1016/j.psychres.2012.05.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Qirtas MM, Zafeiridi E, Pesch D, White EB.. Loneliness and social isolation detection using passive sensing techniques: scoping review. JMIR MHealth UHealth. 2022;10(4):e34638. doi: 10.2196/34638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cacioppo JT, Hawkley LC, Berntson GG.. The anatomy of loneliness. Curr Dir Psychol Sci. 2003;12(3):71–74. [Google Scholar]
- 19. Hawkley LC, Burleson MH, Berntson GG, Cacioppo JT.. Loneliness in everyday life: cardiovascular activity, psychosocial context, and health behaviors. J Pers Soc Psychol. 2003;85(1):105–120. doi: 10.1037/0022-3514.85.1.105 [DOI] [PubMed] [Google Scholar]
- 20. Zhaoyang R, Harrington KD, Scott SB, Graham-Engeland JE, Sliwinski MJ.. Daily social interactions and momentary loneliness: the role of trait loneliness and neuroticism. J Gerontol B Psychol Sci Soc Sci. 2022;77(10):1791–1802. doi: 10.1093/geronb/gbac083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wolf LD, Davis MC.. Loneliness, daily pain, and perceptions of interpersonal events in adults with fibromyalgia. Health Psychol. 2014;33(9):929–937. doi: 10.1037/hea0000059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wechsler D. Wechsler: Wechsler Test of Adult Reading: WTAR. New York, NY: Psychological Corporation; 2001. [Google Scholar]
- 23. Kring AM, Gur RE, Blanchard JJ, Horan WP, Reise SP.. The Clinical Assessment Interview for Negative Symptoms (CAINS): final development and validation. Am J Psychiatry. 2013;170(2):165–172. doi: 10.1176/appi.ajp.2012.12010109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Overall JE, Gorham DR.. The brief psychiatric rating scale. Psychol Rep. 1962;10(3):799–812. doi: 10.2466/pr0.1962.10.3.799 [DOI] [Google Scholar]
- 25. Russell D, Peplau L, Ferguson ML.. UCLA Loneliness Scale. J Pers Assess. 1978. https://psycnet.apa.org/doiLanding?doi=10.1037%2Ft05974-000. Accessed June 28, 2023.
- 26. Llerena K, Park SG, McCarthy JM, Couture SM, Bennett ME, Blanchard JJ.. The Motivation and Pleasure Scale-Self-Report (MAP-SR): reliability and validity of a self-report measure of negative symptoms. Compr Psychiatry. 2013;54(5):568–574. doi: 10.1016/j.comppsych.2012.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- 28. Schneider LC, Struening EL.. SLOF: a behavioral rating scale for assessing the mentally ill. Soc Work Res Abstr. 1983;19(3):9–21. doi: 10.1093/swra/19.3.9 [DOI] [PubMed] [Google Scholar]
- 29. Wang R, Aung MSH, Abdullah S, et al. CrossCheck: toward passive sensing and detection of mental health changes in people with schizophrenia. In: Proceedings of the 2016 ACM International Joint Conference on Pervasive and Ubiquitous Computing, UbiComp’16. New York, NY: Association for Computing Machinery; 2016:886–897. doi: 10.1145/2971648.2971740 [DOI] [Google Scholar]
- 30. Cacioppo JT, Cacioppo S.. The growing problem of loneliness. Lancet. 2018;391(10119):426. doi: 10.1016/S0140-6736(18)30142-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Badcock JC, Di Prinzio P, Waterreus A, Neil AL, Morgan VA.. Loneliness and its association with health service utilization in people with a psychotic disorder. Schizophr Res. 2020;223:105–111. doi: 10.1016/j.schres.2020.05.059 [DOI] [PubMed] [Google Scholar]
- 32. Prizeman K, Weinstein N, McCabe C.. Effects of mental health stigma on loneliness, social isolation, and relationships in young people with depression symptoms. BMC Psychiatry. 2023;23(1):527. doi: 10.1186/s12888-023-04991-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Saris IMJ, Aghajani M, van der Werff SJA, van der Wee NJA, Penninx BWJH.. Social functioning in patients with depressive and anxiety disorders. Acta Psychiatr Scand. 2017;136(4):352–361. doi: 10.1111/acps.12774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. van Winkel M, Nicolson NA, Wichers M, Viechtbauer W, Myin-Germeys I, Peeters F.. Daily life stress reactivity in remitted versus non-remitted depressed individuals. Eur Psychiatry. 2015;30(4):441–447. doi: 10.1016/j.eurpsy.2015.02.011 [DOI] [PubMed] [Google Scholar]
- 35. Mann F, Wang J, Pearce E, et al. Loneliness and the onset of new mental health problems in the general population. Soc Psychiatry Psychiatr Epidemiol. 2022;57(11):2161–2178. doi: 10.1007/s00127-022-02261-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Pels F, Kleinert J.. Loneliness and physical activity: a systematic review. Int Rev Sport Exerc Psychol. 2016;9(1):231–260. doi: 10.1080/1750984X.2016.1177849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ahn J, Kim Y, Jang D.. Physical activity intention-behavior gap during the COVID-19 pandemic: the moderating role of motivation and health-belief. Int J Sport Exerc Psychol. January 19, 2023. doi: 10.1080/1612197X.2023.2168723 [DOI] [Google Scholar]
- 38. van Roekel E, Verhagen M, Engels RCME, Scholte RHJ, Cacioppo S, Cacioppo JT.. Trait and state levels of loneliness in early and late adolescents: examining the differential reactivity hypothesis. J Clin Child Adolesc Psychol. 2018;47(6):888–899. doi: 10.1080/15374416.2016.1146993 [DOI] [PubMed] [Google Scholar]
- 39. Cacioppo JT, Hawkley LC.. Perceived social isolation and cognition. Trends Cogn Sci. 2009;13(10):447–454. doi: 10.1016/j.tics.2009.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Cacioppo S, Balogh S, Cacioppo JT.. Implicit attention to negative social, in contrast to nonsocial, words in the Stroop task differs between individuals high and low in loneliness: evidence from event-related brain microstates. Cortex. 2015;70:213–233. doi: 10.1016/j.cortex.2015.05.032 [DOI] [PubMed] [Google Scholar]
- 41. Cacioppo JT, Norris CJ, Decety J, Monteleone G, Nusbaum H.. In the eye of the beholder: individual differences in perceived social isolation predict regional brain activation to social stimuli. J Cogn Neurosci. 2009;21(1):83–92. doi: 10.1162/jocn.2009.21007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lieberz J, Shamay-Tsoory SG, Saporta N, et al. Behavioral and neural dissociation of social anxiety and loneliness. J Neurosci. 2022;42(12):2570–2583. doi: 10.1523/JNEUROSCI.2029-21.2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hajek A, Kretzler B, König HH.. The association between obesity and social isolation as well as loneliness in the adult population: a systematic review. Diabetes Metab Syndr Obes. 2021;14:2765–2773. doi: 10.2147/DMSO.S313873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Badcock JC, Adery LH, Park S.. Loneliness in psychosis: a practical review and critique for clinicians. Clin Psychol Sci Pract. 2020;27(4):e12345. doi: 10.1111/cpsp.12345 [DOI] [Google Scholar]
- 45. Morgan VA, Waterreus A, Carr V, et al. Responding to challenges for people with psychotic illness: updated evidence from the survey of high impact psychosis. Aust N Z J Psychiatry. 2017;51(2):124–140. doi: 10.1177/0004867416679738 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.