Abstract
Background
Prior research capturing pharmacists’ perspectives on the discharge process has shown that their involvement is essential. Given the multidisciplinary nature of the hospital environment, it is important to understand the perspectives of nonpharmacist health care providers.
Objectives
To explore the perspectives of nonpharmacist health care providers concerning current discharge practices, components of an effective discharge plan, and perceived barriers to an optimal discharge, and to explore their expectations of pharmacists at discharge.
Methods
This qualitative study used key informant interviews of allied health professionals and prescribers at Vancouver General Hospital and North Island Hospital Comox Valley (British Columbia). Participants primarily working on general medicine, family practice, or hospitalist wards were invited to participate.
Results
A total of 16 health care providers participated, consisting of 12 allied health professionals and 4 prescribers. Thematic analysis of the interview transcripts revealed 5 themes for each group. The following 3 themes were common to both groups: systems-related barriers to an optimal discharge; patient- and community-related barriers to an optimal discharge; and patient involvement and education. For allied health professionals, themes of prioritization of patients for discharge and direct communication/teamwork were also key for an optimal discharge. Prescriber-specific themes were limitations related to technology infrastructure and inefficiency of existing collaborative processes. Key responsibilities expected of the pharmacist at discharge included preparing the discharge medication reconciliation and prescriptions, addressing medication-related cost concerns, organizing adherence aids/tools, and providing medication counselling.
Conclusions
Further studies are warranted to investigate optimization of the discharge process through implementation of standardized discharge protocols and electronic health record–related tools. The primary responsibilities of the pharmacist at discharge, as perceived by study participants, were consistent with previous literature.
Keywords: hospital pharmacists, pharmacy services, discharge planning
RÉSUMÉ
Contexte
Des recherches antérieures recueillant le point de vue de pharmaciens sur le processus associé au congé de l’hôpital ont démontré que leur implication est essentielle. Compte tenu de la nature multidisciplinaire du milieu hospitalier, il est important de comprendre les perspectives des prestataires de soins de santé non pharmaciens.
Objectifs
Étudier les points de vue des prestataires de soins de santé non pharmaciens au sujet des pratiques actuelles relatives au congé, des éléments d’un plan de congé efficace et des obstacles perçus à un congé optimal, et, enfin, prendre connaissance des attentes des prestataires à l’égard des pharmaciens au moment du congé.
Méthodologie
Cette étude qualitative a utilisé des entretiens avec des informateurs clés, des professionnels paramédicaux et des prescripteurs au Vancouver General Hospital et au North Island Hospital Comox Valley (en Colombie-Britannique). Les participants travaillant principalement dans les services de médecine générale, de médecine familiale ou d’hospitalisation ont été invités à participer.
Résultats
Au total, 16 prestataires de soins de santé ont participé, 12 professionnels paramédicaux et 4 prescripteurs. L’analyse thématique des transcriptions des entretiens a permis d’identifier 5 thèmes pour chaque groupe. Les 3 thèmes suivants étaient communs aux deux groupes: obstacles au congé optimal liés aux systèmes; obstacles au congé optimal liés aux patients et à la communauté; et participation et sensibilisation des patients. Pour les professionnels paramédicaux, les thèmes de la priorisation des patients pour le congé et de la communication directe/du travail d’équipe étaient essentiels pour un congé optimal. Les thèmes spécifiques aux prescripteurs étaient les limitations liées à l’infrastructure technologique et l’inefficacité des processus de collaboration existants. Les principales responsabilités attendues du pharmacien à la sortie comprenaient la préparation du bilan comparatif des médicaments et des ordonnances au moment du congé, la résolution des problèmes de coûts liés aux médicaments, l’organisation des aides/outils à l’observance et la fourniture de conseils en matière de médication.
Conclusions
D’autres études sont nécessaires pour étudier l’optimisation du processus associé au congé grâce à la mise en œuvre de protocoles standardisés et d’outils liés aux dossiers de santé électroniques. Les principales responsabilités du pharmacien au moment du congé, telles que perçues par les participants à l’étude, correspondaient à la littérature antérieure.
Mots-clés: pharmaciens hospitaliers, services de pharmacie, planification des congés hospitaliers
INTRODUCTION
Transitions of care, such as discharge from hospital, are critical points in a patient’s journey through the health care system, as they are associated with increases in the risk of patient harm and hospital readmission.1 In Canada, approximately 8.5% of patients were readmitted to the hospital within 30 days of discharge in 2010/11, costing the health care system $1.8 billion.1 Literature available at that time suggested that up to 59% of readmissions could potentially be prevented, if those at high risk were identified and their predischarge care improved. Similarly, Auerbach and others2 found that 27% of readmissions within 30 days were potentially preventable and recommended that efforts be made to better identify a patient’s readiness for discharge and to improve communication between health care providers and patients.
Several factors can contribute to medication-related problems at discharge, including intentional and unintentional medication nonadherence, adverse drug events, unintentional medication changes, and poor communication with patients and community health care providers about the discharge plan.3,4 Because of the significant burden that medication-related problems may place on patients and the health care system, pharmacists are in an ideal position to minimize these issues at the time of discharge.5 Previous studies have demonstrated that pharmacist involvement in the discharge process, which may include providing medication education, identifying medication discrepancies, and improving adherence, is vital to success of the discharge.3–6
Our research group has published 2 previous studies exploring the perceptions of British Columbian hospital pharmacists concerning the discharge process.7,8 The first study, which used focus groups, demonstrated that hospital pharmacists believe optimization of the discharge process requires a multifaceted, team-based approach.7 The second study was a survey of hospital pharmacists across British Columbia.8 When asked about key discharge interventions, pharmacists in both studies believed that performing medication reconciliation, providing patient medication education, and ensuring medication adherence were their most important responsibilities for a successful discharge.7,8
Given the multidisciplinary nature of the hospital setting, it is also important to understand the perspectives of nonpharmacist health care providers concerning the discharge process and their expectations of pharmacists at the time of discharge. Previous studies using quantitative methods to explore the opinions of health care providers about clinical pharmacy services9,10 found that pharmacists were expected to complete the medication reconciliation, prepare a patient-friendly medication list, and provide medication counselling, findings that are consistent with our prior research.7,8 However, qualitative methods, such as interviews, are often considered more exploratory in nature, allowing for a greater understanding of the overall situation and identification of behaviours, perceptions, and opinions.
Therefore, to thoroughly characterize the discharge process and to explore the expectations of pharmacists at discharge, a qualitative methodology is preferred. In the study reported here, we sought to explore the perspectives of nonpharmacist health care providers concerning current discharge practices, components of an effective discharge plan, and perceived barriers to an optimal discharge, and also to explore their expectations of pharmacists at discharge and their perceptions of pharmacists’ responsibilities.
METHODS
Study Population and Recruitment
A qualitative study design involving key informant interviews was used. Prescribers (physicians and nurse practitioners) and allied health professionals (care management leaders, bedside nurses, social workers, transition services coordinators, patient care coordinators, physiotherapists, and occupational therapists) from the general medicine, family practice, and hospitalist wards at Vancouver General Hospital (VGH) and North Island Hospital Comox Valley (CVH) were eligible to participate. A care management leader is a registered nurse who leads “iCARE rounds” (interdisciplinary rounds for disposition planning), confirms action plans and follow-up for barriers related to care or discharge planning, and initiates tasks to ensure an ideal transition to home. CVH is a community hospital with 150 acute care beds and a hybrid paper-and-electronic medical records system, whereas VGH is a tertiary care teaching hospital with 1000 acute beds and a fully electronic records system.11,12 Discharge supports at VGH include a designated care management leader on each unit, to coordinate disposition planning, and specialized health care providers, known as transition services teams, that primarily focus on helping patients with complex care needs transition to home. Health care providers holding exclusively leadership positions (managers, directors, etc.) and those working in emergency, intensive care, surgical, or outpatient settings were excluded. A $10 Starbucks gift card was offered as an honorarium to each participant.
Hospital administrators used email to send invitations to participate (including a letter of initial contact and a consent form) to staff in their respective areas of responsibility. Study recruitment posters were also posted on the units. Interested staff members contacted the study team directly and were screened by 2 of the authors (P.Y., K.D.) for eligibility. Once the signed consent forms were collected, the link to the baseline demographic survey was distributed by email; participants were instructed to complete this survey before scheduling their interview. Participants were stratified into 2 groups: allied health professionals and prescribers.
Data Collection
All participants completed the baseline demographic survey using the University of British Columbia January 2023 version of Qualtrics software. All interviews were facilitated virtually by the first author (P.Y.) through the primary investigator’s (K.D.) Zoom (version 5.14.10) account. The interview facilitator asked each participant a series of preapproved interview questions (described below). All study material (ID# H22-02496) was approved by the University of British Columbia Behavioural Research Ethics Board and Harmonized Partner Boards (Fraser Health and Island Health). Each interview was audio-recorded using the Zoom recording function and transcribed verbatim by P.Y. The audio files were deleted once the transcriptions had been reviewed by P.Y. and the interviewee for accuracy and authenticity, with corrections made as needed.
Development of Interview Guide
The interview questions (Appendix 1) were developed following a detailed literature search.13–15 The questions were then refined by the research team and circulated to previously identified stakeholders for further refinement. Two interview guides were created, one for allied health professionals and the other for prescribers. The main difference between the interview guides was that the prescribers (but not the allied health professionals) were asked to specify, from a predefined list, what they thought were the most and least important discharge interventions.
Within the investigator team, K.D. and M.L. have prior experience in qualitative research and key informant interview methodology. P.Y., K.D., M.L., C.I., and K.R. are clinical pharmacists; J.T. has experience as a front-line nurse; D.F. and L.C. are physicians; and all are familiar and experienced with the patient discharge process.
Data Analysis
Descriptive statistical analyses were used to calculate frequencies and percentages for the baseline demographic data. All interview transcripts were analyzed using thematic analysis. One investigator (P.Y.) independently coded the transcripts using NVivo qualitative data analysis software (QSR International). The research group discussed the codes until the final code list had been created. P.Y. then used the final code list to develop overall themes, which were discussed within the research team during 2 separate meetings until consensus was reached concerning the final theme list.
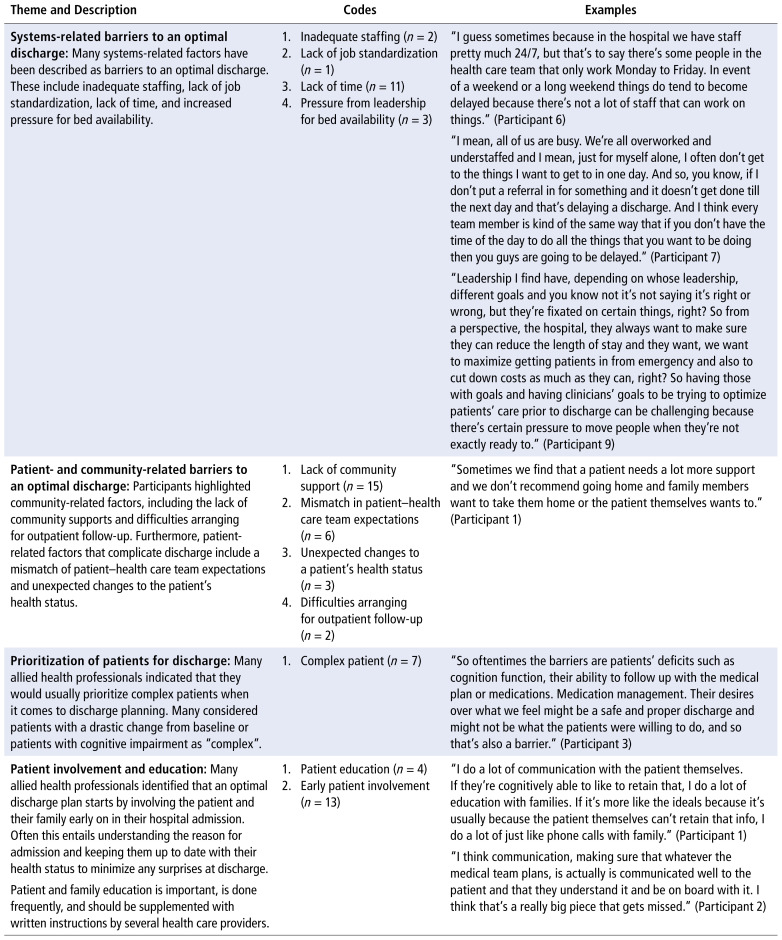
RESULTS
A total of 16 health care providers consented to participate in this study; 12 were allied health professionals and 4 were prescribers. Complete baseline demographic data are presented in Table 1. All interviews were conducted from January to March 2023, and the average interview duration was 21 minutes. Thematic analysis of the interview transcripts generated 13 and 14 codes for the allied health participants and prescribers, respectively; these were organized into 5 themes for each group (Table 2 and Table 3). The following 3 themes were common to the 2 groups: systems-related barriers to an optimal discharge; patient- and community-related barriers to an optimal discharge; and patient involvement and education. Themes specific to allied health participants were prioritization of patients for discharge and direct communication and teamwork are key for an optimal discharge. Prescriber-specific themes were limitations related to technology infrastructure and inefficiency of existing collaboration processes.
TABLE 1.
Baseline Characteristics of Participants
| Characteristic | Study Group; No. (%) of Respondents | |
|---|---|---|
|
| ||
| Allied Health (n = 12) | Prescribers (n = 4) | |
| Occupation | ||
| Care management leader | 5 (41) | NA |
| Bedside nurse | 2 (17) | NA |
| Occupational therapist | 2 (17) | NA |
| Physiotherapist | 3 (25) | NA |
| Physician | NA | 4 (100) |
|
| ||
| Practice setting | ||
| Vancouver General Hospital | 11 (92) | 0 |
| North Island Hospital Comox Valley | 1 (8) | 4 (100) |
|
| ||
| Time in practice (years) | ||
| < 5 | 6 (50) | 0 |
| 5–10 | 2 (17) | 0 |
| 10–15 | 2 (17) | 1 (25) |
| >15 | 2 (17) | 3 (75) |
|
| ||
| Average no. of patients per day | ||
| < 10 | 4 (33) | 1 (25) |
| 10–20 | 0 | 3 (75) |
| 21–30 | 7 (59) | 0 |
| > 30 | 1 (8) | 0 |
|
| ||
| Average no. of discharges per week | ||
| < 5 | 1 (8) | 2 (50) |
| 5–10 | 2 (17) | 2 (50) |
| 11–15 | 5 (42) | 0 |
| > 15 | 4 (33) | 0 |
|
| ||
| % of discharge participationa | ||
| < 25% | 2 (17) | NA |
| 25%–50% | 2 (17) | NA |
| 50%–75% | 4 (33) | NA |
| > 75% | 4 (33) | NA |
|
| ||
| Average time to complete a patient discharge (min) | ||
| < 15 | 1 (8) | 0 |
| 15–30 | 3 (25) | 0 |
| 30–45 | 6 (50) | 3 (75) |
| > 45 | 2 (17) | 1 (25) |
NA = not applicable.
Refers to percentage of discharges in which the allied health professional participates.
TABLE 2.
Key Themes, Descriptions, and Relevant Codes for Allied Health Participants
| Theme and Description | Codes | Examples |
|---|---|---|
| Systems-related barriers to an optimal discharge: Many systems-related factors have been described as barriers to an optimal discharge. These include inadequate staffing, lack of job standardization, lack of time, and increased pressure for bed availability. |
|
“I guess sometimes because in the hospital we have staff pretty much 24/7, but that’s to say there’s some people in the health care team that only work Monday to Friday. In event of a weekend or a long weekend things do tend to become delayed because there’s not a lot of staff that can work on things.” (Participant 6) “I mean, all of us are busy. We’re all overworked and understaffed and I mean, just for myself alone, I often don’t get to the things I want to get to in one day. And so, you know, if I don’t put a referral in for something and it doesn’t get done till the next day and that’s delaying a discharge. And I think every team member is kind of the same way that if you don’t have the time of the day to do all the things that you want to be doing then you guys are going to be delayed.” (Participant 7) “Leadership I find have, depending on whose leadership, different goals and you know not it’s not saying it’s right or wrong, but they’re fixated on certain things, right? So from a perspective, the hospital, they always want to make sure they can reduce the length of stay and they want, we want to maximize getting patients in from emergency and also to cut down costs as much as they can, right? So having those with goals and having clinicians’ goals to be trying to optimize patients’ care prior to discharge can be challenging because there’s certain pressure to move people when they’re not exactly ready to.” (Participant 9) |
| Patient- and community-related barriers to an optimal discharge: Participants highlighted community-related factors, including the lack of community supports and difficulties arranging for outpatient follow-up. Furthermore, patient-related factors that complicate discharge include a mismatch of patient–health care team expectations and unexpected changes to the patient’s health status. |
|
“Sometimes we find that a patient needs a lot more support and we don’t recommend going home and family members want to take them home or the patient themselves wants to.” (Participant 1) |
| Prioritization of patients for discharge: Many allied health professionals indicated that they would usually prioritize complex patients when it comes to discharge planning. Many considered patients with a drastic change from baseline or patients with cognitive impairment as “complex”. |
|
“So oftentimes the barriers are patients’ deficits such as cognition function, their ability to follow up with the medical plan or medications. Medication management. Their desires over what we feel might be a safe and proper discharge and might not be what the patients were willing to do, and so that’s also a barrier.” (Participant 3) |
|
Patient involvement and education: Many allied health professionals identified that an optimal discharge plan starts by involving the patient and their family early on in their hospital admission. Often this entails understanding the reason for admission and keeping them up to date with their health status to minimize any surprises at discharge. Patient and family education is important, is done frequently, and should be supplemented with written instructions by several health care providers. |
|
“I do a lot of communication with the patient themselves. If they’re cognitively able to like to retain that, I do a lot of education with families. If it’s more like the ideals because it’s usually because the patient themselves can’t retain that info, I do a lot of just like phone calls with family.” (Participant 1) “I think communication, making sure that whatever the medical team plans, is actually is communicated well to the patient and that they understand it and be on board with it. I think that’s a really big piece that gets missed.” (Participant 2) |
|
Direct communication and teamwork are key for an optimal discharge: Most allied health professionals identified direct communication as a key factor in an optimal discharge, as the results of their discussions are immediate and actionable. Daily rounds help keep the team up to date with the status of all patients and the likely discharges for the day. Having overlap in responsibilities during the discharge process was described as helpful, especially when certain providers were too busy to manage their workload. |
|
“We also have rounds every day on our unit for about an hour where the focus is on barriers to discharge. So usually things like that come up there just verbally and then there are emails if we need like community partners involved. But if it’s just within the team, then we tend to just like talk, you know in person on the unit.” (Participant 1) |
TABLE 3.
Key Themes, Descriptions, and Relevant Codes for Prescribers
| Theme and Description | Codes (Frequency) | Example |
|---|---|---|
| Systems-related barriers to an optimal discharge: Many systems-related factors have been described as barriers to an optimal discharge. Some of these are logistic issues involving inadequate staffing, the lack of a discharge coordinator, and physicians being scheduled to discharge a patient when they have just received them recently into their care. |
|
“But yeah, I’d say the ideal would be to tell one person what is needed to get a patient out of hospital and then do my part and then have them tell me when that stuff was put to place … I love the team, but I feel like I have to talk to the physio, talk to the Home Care liaison, talk to the family and you know, go over all these things.” (Participant 15) “Oh, 100%, 100%. And the unpredictability of our patients. So you go to do a discharge and then somebody on the other side of the hospital has a heart attack. Well, that discharge just isn’t happening now. People are waiting for me to deal with somebody’s heart attack. So to get somebody [else] out the door for discharge … so barrier to discharge is, yeah, definitely time.” (Participant 15) |
| Limitations related to technology infrastructure: Another issue involves the inability of the electronic health record to electronically create a discharge medication reconciliation and prescription. This often becomes a time-consuming task which is prone to medication errors. |
|
“One thing I would like to see is some way of like printing off the medication list in preparation for discharge, so I don’t have to write everything and potentially make a transcription error. Having a like a form that it gets downloaded from Cerner [EHR], or whatever, would be great.” (Participant 8) |
| Patient- and community-related barriers to an optimal discharge: Participants highlighted community-related factors, including the lack of community supports and difficulties arranging for outpatient follow-up. Furthermore, patient-related factors that complicate discharge include patients simply not understanding the circumstances of their care. |
|
“I mean overall lack of resources everywhere. A lot of our patients, our home care supply here is incredibly short. So community services is a barrier to discharge.” (Participant 15) “Well, I think the ideal discharge process would be one in which the patient and everybody else is well informed about what’s supposed to happen and things are organized such that things don’t fall through the crack or there’s uncertainties.” (Participant 14) |
| Patient involvement and education: Many prescribers identified that an optimal discharge starts by involving the patient and their family. Often this entails a thorough discussion near the time of discharge, along with providing information on follow-up testing, follow-up with outpatient providers, and discharge prescriptions. This is often supplemented with written instructions. |
|
“Yeah, the patient education and counselling. I would take that to mean patient and family? OK, because that’s a big part and it could be a very time-consuming part as well. But again, I don’t think that that can be done by another provider. I think it has to be done by the person who knows the core issues.” (Participant 15) “Well, from the time that they come into hospital, you talk about goals of care. You know, how do you know that you’ve met your goals of care. And so that’s one way. And another way for me is to have patients go on passes home and you know, be living out in the community as they would with supports in place and having that go well I think is another step that I like to take for a successful discharge.” (Participant 8) |
| Inefficiency of existing collaboration processes: Often prescribers are unable to participate in daily rounds with the allied health team to discuss potential discharges. This perceived lack of collaboration can be inferred, as the usual mode of communication for prescribers seems to be through written documentation or speaking with individual providers when necessary. |
|
“My first instinct is that people should stick to their roles because (A) that’s what they know best and (B) if there’s overlap and somebody might not do it. I mean, there is a lot of overlap. The nurses overlap with almost everybody. Because the nurses mobilize patients, the nurses deliver medications. They do assessments. They do part my job, part rehab job. But in general, I feel like everybody should have their designated duties because they are the ones that do them best.” (Participant 15) |
Common Themes for Allied Health Participants and Prescribers
Systems-Related Barriers to an Optimal Discharge
Many of the study participants identified systems-related issues, including factors that are often out of the individual’s immediate control but may nevertheless affect the discharge process, such as a lack of staff on weekends and holidays, lack of a discharge coordinator, and inconsistencies in discharge responsibilities across different wards. The most frequently cited barrier was a lack of time. Participants also acknowledged that they felt some patients were discharged prematurely because of limited bed availability and pressure from leadership.
A lot of my role is it feels like just getting patients like good enough to be able to leave hospital to have more beds open up … I feel like there’s a few times I can think of like a patient would benefit … from just like a little bit more time rehabbing. (Participant 13)
It’s definitely time, like most people in acute care feel they’re drowning with the current assignments that they have. (Participant 3)
I think there’s a lack of standardization across the organization on a whole … from unit to unit is a different picture of who has the responsibility and who is accountable for what. (Participant 9)
Patient- and Community-Related Barriers to an Optimal Discharge
Most participants indicated a lack of community support as a major barrier within this theme:
Community resources. So not having proper support like home support or nursing staff. One of the pharmacy resources that I come across this week, that is, there’s a barrier with somebody going home on insulin and is not able to do the insulin themself and family isn’t able to do it. (Participant 7)
Furthermore, prescribers specified that it was a lack of family physicians that made continuity of care challenging:
So many of these patients don’t have family doctors anymore, which is a huge problem. That is an enormous deterrent to a good discharge because there’s, you know, a family physician is supposed to be sort of the central crossroads of information that should be receiving reports of everything that’s been done. (Participant 14)
Prescribers also found that patients’ poor understanding of their medication changes contributed to a difficult discharge:
I think it’s quite common for patients to end up at home with some confusion about what it is they’re supposed to be taking and then they realize there was some pill that they had at home that wasn’t given to them in the hospital and should they still be taking that or not. (Participant 14)
Patient Involvement and Education
The majority of participants agreed that patient education was important to an optimal discharge. Participants noted that such education was most effective when it was started early, repeated throughout the admission, and supplemented with written instructions:
I talked to the patient and the family and sort out the plan for them going home … Sometimes I’ll give them a little handwritten sort of checklist, you know, here’s what’s going to happen. (Participant 14)
Themes Specific to Allied Health Participants
Prioritization of Patients for Discharge
One of the themes specific to allied health participants was prioritization of patients for discharge interventions. Most participants in this group agreed that the need for prioritization was a consequence of a demanding workload and was done primarily out of necessity. Participants stated that patient prioritization was determined by the complexity of each patient’s medical situation, including factors such as changes from baseline or history of cognitive impairment.
My immediate priority would be equipment needs. So, if I’m seeing someone or if anyone has a drastic change in function, I’d immediately prioritize them for discharge. (Participant 1)
Direct Communication and Teamwork Are Key for an Optimal Discharge
Most participants identified direct communication as a key factor in an optimal discharge, as the results of discussions within the health care team are immediate and actionable. Daily rounds help health care providers involved in discharges stay informed of any evolving needs of patients before their transition to home.
We do rounds every day with the whole team and kind of go through every patient and talk about what’s going on and what our plans are moving forward so they can be discharged … I try and have face-to-face conversations with people. I find that that works best for us. (Participant 7)
Themes Specific to Prescribers
Limitations Related to Technology Infrastructure
All prescribers agreed that preparing the discharge medication reconciliation was time-consuming and prone to errors. They indicated that the current electronic heath record (EHR) system does not allow a discharge prescription to be printed; instead, they had to prepare the discharge prescription by hand or create a separate electronic document.
I think with medication reconciliation, that’s what takes time … I have to type in those new medications and tick the right box on the Word document … it’s not automatic. It’s not fail-safe. (Participant 11)
Inefficiency of Existing Collaboration Processes
Another theme was the perceived lack of collaboration between prescribers and allied health professionals. Prescribers expressed that they would ideally like to be involved in daily interprofessional rounds; however, there was a consensus that their demanding workload made attending difficult:
And there’s a structured team meeting in the morning, but that’s at a time that the physicians can’t always attend because it’s first thing in the morning to determine discharges. (Participant 15)
Furthermore, most prescribers acknowledged there was a lack of direct communication, given that their usual mode of communication was through written chart notes:
Right, so written progress note is one thing … “Please ask physiotherapy to assess mobility”, right then the unit clerk calls them … I don’t usually have time to call all those people individually. (Participant 14)
Responsibilities Expected of the Pharmacist
Both allied health participants and prescribers agreed that the responsibilities expected of the pharmacist at discharge should include preparing the discharge medication reconciliation and prescription, addressing concerns about medication costs, organizing adherence aids/tools, and providing medication counselling
Key Components of a Discharge Plan
Prescribers reported 4 components that they believed were essential to a successful discharge plan: coordination of care with the interdisciplinary team, discharge dictation, discharge prescription, and liaison with outpatient providers.
DISCUSSION
This study explored the perspectives of various health care providers concerning current discharge practices, barriers to an optimal discharge plan, and key responsibilities of the pharmacist.
Prescribers suggested several components that make up an effective discharge plan. Despite most prescribers agreeing that coordination of care with the interdisciplinary team was essential, time limitations often prevented them from participating in discharge rounds. Furthermore, allied health participants frequently cited a need to prioritize patient discharges as a direct consequence of a lack of time. Some participants described inconsistency in their responsibilities across different wards, which suggests a lack of standardization in the discharge process. These findings, which highlight potential system-wide problems that could limit efficient collaboration processes, were consistent with previous literature suggesting the need to improve staffing and identify strategies to promote collaboration.13–15 In Ontario, Canada, a provincial agency created a standardized discharge planning tool to facilitate discharge planning by health care staff, with the goal of reducing hospital readmissions.16 This protocol subdivides each discharge into 3 stages (pre-transition, transition planning, and post-transition), each with specific practices and goals. This proactive approach allows practitioners to identify ongoing patient care needs, implement individualized care plans, and ensure continuity of care after the discharge.16 The implementation of a standardized discharge protocol not only facilitates clear and consistent roles for each health care provider, but also promotes collaboration.
Patients’ poor understanding of their medications and their discharge plan was a frequently highlighted patient-related barrier. With their extensive medication background, pharmacists are uniquely positioned to help address this barrier. The pharmacists who participated in our previous 2 studies7,8 and participants in the current study agreed that patient education, including medication counselling, was one of the key responsibilities on which pharmacists should focus at discharge. However, time has often been cited as a limitation: in previous studies, pharmacists were observed to spend most of their time assessing patients and developing care plans, attending bedside rounds, and implementing recommendations, with only 3% of their time allocated to counselling patients.7,8,17 Enhanced communication methods, such as postdischarge follow-up, have also been identified as crucial components of an effective discharge plan and continuity of care.3,4 Furthermore, specialized transition-of-care teams have been implemented to streamline care coordination and reduce readmission rates.18 For example, Hitch and others19 found an 8.9% reduction in 30-day readmission rates with a 3-step discharge approach consisting of referral to a nurse case manager, medication reconciliation completed by a pharmacist, and outpatient follow-up appointments with a physician. Similarly, Dizon and Reinking20 observed a 2.3% reduction in 30-day readmission rates with a multidisciplinary transition-of-care program. Although tertiary care hospitals such as VGH may have already implemented additional supports for discharge planning (e.g., care management leader, transition services teams), stakeholders at community hospital sites should consider implementing such initiatives to improve continuity of care after discharge.
In the current study, prescribers highlighted an EHR- related challenge to an optimal discharge, suggesting that the integration of discharge-related tools may help to optimize the discharge process. However, these results are related specifically to the limited technology infrastructure at the community hospital, CVH (where all of the prescriber participants were based), whereas discharge prescriptions are generated automatically at the tertiary care hospital, VGH. Nonetheless, previous studies have shown the effectiveness of discharge optimization tools in enhancing interdisciplinary communication and minimizing discharge delay. As one example of the potential value of discharge optimization tools, Kelly and Cardy21 described the implementation of a colour-coded “dot” system to represent anticipated time until discharge (e.g., green = discharge in < 12 hours; yellow = anticipated discharge in 12–24 hours; red = anticipated discharge in 24–48 hours); after introduction of the system, hospital length of stay for postoperative surgical patients declined from 8.73 days to 7.31 days, and physicians’ satisfaction with communication increased from 3 to 4 (on a 5-point Likert scale). Similarly, when the same system was implemented in a pediatric hospital, the proportion of discharges occurring before noon increased from 16.4% to 19.3%.22 As technology advances, we can anticipate the implementation of fully electronic medical records systems across more community and tertiary care hospitals. Automating administrative tasks that pertain to discharge planning can increase efficiency and accuracy, possibly allowing more time for health care professionals to focus on other patient care activities.
In this study, participants’ expectations of the role of the pharmacist at discharge were consistent with the interventions that pharmacists believe to be their primary responsibilities (i.e., discharge medication reconciliation and patient medication education).7,8 These interventions have been demonstrated to have important impacts; for example, pharmacy-led medication reconciliation resulted in a 66% reduction in medication discrepancies, and a meta-analysis found a reduction in the odds of readmission with pharmacy-supported transition-of-care interventions, including medication reconciliation, patient education, and patient-centred follow-up.3,23
This study had several limitations. First, all of the prescribers were recruited from CVH, a community hospital, which had limited technology infrastructure pertaining to the usability of its EHR. This may limit the generalizability of these results to other clinical settings. Second, all participants were recruited from either a tertiary care or community hospital in a specific geographic location, with unique practice models and support systems at each site, which could further limit the generalizability of the results. Lastly, we assumed that theoretical data saturation was achieved despite the small sample size. However, there may be additional thoughts and perceptions of allied health professionals and prescribers that were not captured in this study.
CONCLUSION
Several barriers to an optimal discharge plan were identified, and further studies looking into the optimization of the discharge process with the implementation of standardized discharge protocols and EHR-related tools are therefore warranted. Overall, participants in this study believed that the primary responsibilities of the pharmacist at the time of discharge should include completing the discharge medication reconciliation and providing patient medication education, findings that are consistent with previous literature.
APPENDIX 1. Survey questions
PRESCRIBERS
Baseline survey questions (to be completed on Qualtrics prior to each session)
-
What is your current occupation?
Physician
Nurse Practitioner
Other:
-
At which hospital do you perform the majority of your work?
Vancouver General Hospital
North Island Hospital Comox Valley
Other:
-
How long have you been practicing (in years)?
< 5
5–10
10–15
> 15
-
Which speciality describes you the best?
Family Physician
Hospitalist
Internist
Medical Resident
Nurse Practitioner
Other:
-
What is the daily average number of hospital patients you care for in the clinical area where you work?
< 10
10–20
21–30
> 30
-
On average, how many patients are discharged from the clinical area that you cover each week?
< 5
5–10
11–15
> 15
-
Are there defined discharge roles for different health care professionals?
Yes
No
-
Are there formal discharge rounds?
Yes
No
-
(If yes) do you regularly participate in formal discharge rounds?
Yes
No
-
What are the key components of a patient discharge plan (select all that apply)?
Coordinating care with the interdisciplinary team
Discharge dictation
Discharge prescription
Liaising with outpatient providers
Outpatient lab requisition
Patient education/counselling
Other:
-
On average, how long does it take you to complete a patient discharge (in minutes)?
< 15
15–30
30–45
> 45
-
Do you currently liaise on a regular basis with any outpatient health care professionals to provide continuity of care when discharging your patients (select all that apply)?
Community pharmacists
Family physicians
Primary care networks
Relevant specialists
Other:
-
Rank the following interventions related to hospital discharge from most to least important.
Coordinating care with the interdisciplinary team
Coordinating care with outpatient providers
Medication reconciliation on discharge
Patient education/counselling
Post-discharge follow-up
Key informant interview questions
How would you describe the usual discharge process at the site where you practice?
-
How would you describe the ideal discharge process?
What are some of the barriers to implementing this?
Do you feel like time is a barrier for an optimal discharge plan?
-
From the initial survey you were asked to rank discharge interventions from most to least important. The interventions included were coordinating care with the interdisciplinary team, coordinating care with outpatient providers, medication reconciliation on discharge, patient education/counselling, and post-discharge follow-up.
Can you tell me which intervention you ranked as most important? Why do you think this is?
Can you tell me which intervention you ranked as least important? Why do you think this is?
Is there anything else missing from this list that you think should be included?
-
(If not already mentioned in Q3) How do you coordinate discharge planning with the interdisciplinary team?
In person? By phone? Through written documentation?
Is this method effective?
-
How do you coordinate discharge planning (e.g., education, follow-up appointments, lab requisitions) with the patient?
By speaking directly to them? Do you delegate this task?
-
Should there be defined discharge roles for different healthcare professionals?
What should each profession be responsible for?
How would this help the current discharge process?
-
Specific to pharmacy, in the setting where you work are there hospital pharmacists who assist with any of the aspects of the discharge process? Are there discharge interventions (e.g., discharge medication reconciliation, medication education/counselling) that you think hospital pharmacists should prioritize?
How do you see pharmacists helping you in these interventions?
Is there anything else about this topic that wasn’t discussed today that your think is important for us to be aware of?
NON-PRESCRIBERS
Baseline survey questions (to be completed on Qualtrics prior to each session)
-
What is your current occupation?
Care management leader
Bedside nurse
Social worker
Transition services coordinator
Patient care coordinator
Other:
-
At which hospital do you perform the majority of your work?
Vancouver General Hospital
North Island Hospital Comox Valley
Other:
-
How long have you been practicing (in years)?
< 5
5–10
10–15
> 15
-
What is the daily average number of hospital patients you care for in the clinical area where you work?
< 10
10–20
21–30
> 30
-
On average, how many patients are discharged from the clinical area that you cover each week?
< 5
5–10
11–15
> 15
-
What percentage of the total number of discharges in your clinical area do you actively participate in each week?
< 25%
25%–50%
50%–75%
> 75%
-
Are there defined discharge roles for different healthcare professionals?
Yes
No
-
Are there formal discharge rounds?
Yes
No
-
(If yes) do you regularly participate in formal discharge rounds?
Yes
No
-
On average, how long does it take you to complete a patient discharge (in minutes)?
< 15
15–30
30–45
> 45
Key informant interview questions
What is your role in the discharge process?
-
How would you describe the ideal discharge process?
What are some of the barriers to implementing this?
Do you feel like time is a barrier for an optimal patient discharge plan?
-
Do you prioritize certain patients for discharge planning?
If yes – what types of patients do you prioritize?
-
What do you believe are the key components of a patient discharge plan?
Which discharge interventions are you involved with? Which one do you think is most important?
Do you participate in any discharge interventions that involve medications? Can you describe these interventions?
-
How do you coordinate discharge planning with the interdisciplinary team?
In person? By phone? Through written documentation?
Is this method effective?
-
How do you coordinate discharge planning (e.g., education, follow-up appointments) with the patient?
By speaking directly to them? Do you delegate this task?
-
Should there be defined discharge roles for different healthcare professionals?
What should each profession be responsible for?
How would this help the current discharge process?
-
Specific to pharmacy, in the setting where you work are there hospital pharmacists who assist with any of the aspects of the discharge process? Are there discharge interventions (e.g., medication education/counselling) that you think hospital pharmacists should prioritize?
How do you see pharmacists helping you in these interventions?
Is there anything else about this topic that wasn’t discussed today that you think is important for us to be aware of?
Funding Statement
The honoraria for participants were funded from the unrestricted start-up research funds of the primary investigator (K.D.).
Footnotes
Competing interests: For projects unrelated to the work reported here, Karen Dahri has received grants from the Canadian Institutes of Health Research, the UBC Students as Partners Fund, and the BC Ministry of Health; consulting fees from TRC Healthcare; honoraria from Pear Tree Healthcare, UBC Continuing Pharmacy Professional Development, and the Pharmacists in Primary Care Network; and support for travel related to her role as the BC delegate for the Canadian Society of Hospital Pharmacists. No other competing interests were declared.
Funding: The honoraria for participants were funded from the unrestricted start-up research funds of the primary investigator (K.D.). No other funding was received.
References
- 1.All-cause readmission to acute care and return to the emergency department. Canadian Institute for Health Information; 2012. [cited 2022 Jul 4]. Available from: https://publications.gc.ca/collections/collection_2013/icis-cihi/H118-93-2012-eng.pdf. [Google Scholar]
- 2. Auerbach AD, Kripalani S, Vasilevskis EE, Sehgal N, Lindenauer PK, Metlay JP, et al. Preventability and causes of readmissions in a national cohort of general medicine patients. JAMA Intern Med. 2016;176(4):484–93. doi: 10.1001/jamainternmed.2015.7863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rodrigues CR, Harrington AR, Murdock N, Holmes JT, Borzadek EZ, Calabro K, et al. Effect of pharmacy-supported transition-of-care interventions on 30-day readmissions: a systematic review and meta-analysis. Ann Pharmacother. 2017;51(10):866–89. doi: 10.1177/1060028017712725. [DOI] [PubMed] [Google Scholar]
- 4. Mekonnen AB, McLachlan AJ, Brien JE. Effectiveness of pharmacist-led medication reconciliation programmes on clinical outcomes at hospital transitions: a systematic review and meta-analysis. BMJ Open. 2016;6(2):e010003. doi: 10.1136/bmjopen-2015-010003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Foot H, Scott I, Sturman N, Whitty JA, Rixon K, Connelly L, et al. Impact of pharmacist and physician collaborations in primary care on reducing readmission to hospital: a systematic review and meta-analysis. Res Social Adm Pharm. 2021;18(6):2922–43. doi: 10.1016/j.sapharm.2021.07.015. [DOI] [PubMed] [Google Scholar]
- 6. Daliri S, Boujarfi S, El Mokaddam A, Scholte Op Reimer WJM, Ter Riet G, Den Haan C, et al. Medication-related interventions delivered both in hospital and following discharge: a systematic review and meta-analysis. BMJ Qual Saf. 2021;30(2):146–56. doi: 10.1136/bmjqs-2020-010927. [DOI] [PubMed] [Google Scholar]
- 7. Ladhar S, Dahri K, Inglis C, Sambrielaz A, Raza H, Legal M. Insights into British Columbian hospital pharmacists perspectives on the discharge process. Innov Pharm. 2022;13(4):20. doi: 10.24926/iip.v13i4.5093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rahnama K, Dahri K, Legal M, Inglis C. Characterizing current and optimal involvement of hospital pharmacists in the discharge process – a survey of pharmacists in British Columbia. Can J Hosp Pharm. 2024;77(1):3433. doi: 10.4212/cjhp.3433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chevalier B, Neville HL, Thompson K, Nodwell L, MacNeil M. Health care professionals’ opinions and expectations of clinical pharmacy services on a surgical ward. Can J Hosp Pharm. 2016;69(6):439–48. doi: 10.4212/cjhp.v69i6.1606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hias J, Walgraeve K, Tournoy J, Flamaing J, Spriet I, Van der Linden L. Physician’s feedback on a clinical pharmacy program on geriatric wards. Acta Clin Belg. 2020;75(5):321–8. doi: 10.1080/17843286.2019.1629054. [DOI] [PubMed] [Google Scholar]
- 11.Divisions of Family Practice: Comox Valley Hospital, North Island Hospital - Comox Valley Campus [webpage] Family Practices Services Committee; [cited 2023 Aug 2]. Available from: https://divisionsbc.ca/comox-valley/live-work-play/our-hospitals. [Google Scholar]
- 12.Emergency Department VGH. About us [webpage] VGH Emergency Department; [cited 2023 Aug 2]. Available from: https://www.vghemergency.com/about/ [Google Scholar]
- 13. Wong EL, Yam CH, Cheung AW, Leung MC, Chan FW, Wong FY, et al. Barriers to effective discharge planning: a qualitative study investigating the perspectives of frontline healthcare professionals. BMC Health Serv Res. 2011;11:242. doi: 10.1186/1472-6963-11-242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pinelli V, Stuckey HL, Gonzalo JD. Exploring challenges in the patient’s discharge process from the internal medicine service: a qualitative study of patients’ and providers’ perceptions. J Interprof Care. 2017;31(5):566–74. doi: 10.1080/13561820.2017.1322562. [DOI] [PubMed] [Google Scholar]
- 15. Davis MM, Devoe M, Kansagara D, Nicolaidis C, Englander H. “Did I do as best as the system would let me?” Healthcare professional views on hospital to home care transitions. J Gen Intern Med. 2012;27(12):1649–56. doi: 10.1007/s11606-012-2169-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adopting a common approach to transitional care planning: helping health links improve transitions and coordination of care. Health Quality Ontario; n.d. [cited 2023 Aug 15]. Available from: https://www.hqontario.ca/Portals/0/documents/qi/health-links/bp-improve-package-traditional-care-planning-en.pdf. [Google Scholar]
- 17. Wong D, Feere A, Yousefi V, Partovi N, Dahri K. How hospital pharmacists spend their time: a work-sampling study. Can J Hosp Pharm. 2020;73(4):272–8. [PMC free article] [PubMed] [Google Scholar]
- 18. Zimmerman WD, Grenier RE, Palka SV, Monacci KJ, Lantzy AK, Leutbecker JA, et al. Transitions of care coordination intervention identifies barriers to discharge in hospitalized stroke patients. Front Neurol. 2021;12:573294. doi: 10.3389/fneur.2021.573294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hitch B, Parlier AB, Reed L, Galvin SL, Fagan EB, Wilson CG. Evaluation of a team-based, transition-of-care management service on 30-day readmission rates. N C Med J. 2016;77(2):87–92. doi: 10.18043/ncm.77.2.87. [DOI] [PubMed] [Google Scholar]
- 20. Dizon ML, Reinking C. Reducing readmissions: nurse-driven interventions in the transition of care from the hospital. Worldviews Evid Based Nurs. 2017;14(6):432–9. doi: 10.1111/wvn.12260. [DOI] [PubMed] [Google Scholar]
- 21. Kelly ST, Cardy C. Discharge optimization tool to decrease length of stay and improve satisfaction related to advanced practice provider communication. Heart Lung. 2023;60:59–65. doi: 10.1016/j.hrtlng.2023.02.026. [DOI] [PubMed] [Google Scholar]
- 22. Perry MF, Macias C, Chaparro JD, Heacock AC, Jackson K, Bode RS. Improving early discharges with an electronic health record discharge optimization tool. Pediatr Qual Saf. 2020;5(3):e301. doi: 10.1097/pq9.0000000000000301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mekonnen AB, Mclachlan AJ, Brien JE. Pharmacy-led medication reconciliation programmes at hospital transitions: a systematic review and meta-analysis. J Clin Pharm Ther. 2016;41(2):128–44. doi: 10.1111/jcpt.12364. [DOI] [PubMed] [Google Scholar]