Abstract
Although intratumoral heterogeneity has been established in pediatric central nervous system tumors, epigenomic alterations at the cell type level have largely remained unresolved. To identify cell type-specific alterations to cytosine modifications in pediatric central nervous system tumors, we utilize a multi-omic approach that integrated bulk DNA cytosine modification data (methylation and hydroxymethylation) with both bulk and single-cell RNA-sequencing data. We demonstrate a large reduction in the scope of significantly differentially modified cytosines in tumors when accounting for tumor cell type composition. In the progenitor-like cell types of tumors, we identify a preponderance differential Cytosine-phosphate-Guanine site hydroxymethylation rather than methylation. Genes with differential hydroxymethylation, like histone deacetylase 4 and insulin-like growth factor 1 receptor, are associated with cell type-specific changes in gene expression in tumors. Our results highlight the importance of epigenomic alterations in the progenitor-like cell types and its role in cell type-specific transcriptional regulation in pediatric central nervous system tumors.
Subject terms: CNS cancer, Paediatric cancer, DNA methylation, Cancer genomics, Tumour heterogeneity
Cell type-specific epigenomic alterations and heterogeneity in paediatric central nervous system (CNS) tumours remain underexplored. Here, the authors integrate bulk DNA cytosine modification data with bulk and single-nucleus RNA-sequencing to explore cell type-specific epigenomic alterations and gene regulation in paediatric CNS tumours.
Introduction
Central nervous system (CNS) tumors are the leading cause of cancer death in the pediatric population1. While major progress has been made in reducing the mortality in pediatric cancers in the past few decades, the magnitude of reduction in the mortality rate of CNS tumors have not been as substantial2. Even among patients who survive childhood cancers, those who have survived CNS tumors have the highest cumulative burden of disease post-survival3. Craniospinal radiation and neuro-toxic therapy are major risk factors for the future burden on quality of life with late effects including neurocognitive impairments such as academic and memory decline, and adverse health outcomes like abnormal hearing and growth hormone deficiency4–9. Efforts to address discrepancies in the reduction of mortality rates and extensive chronic health burdens later in life have been made with the recent advances in technology that have allowed for better insight into the molecular characterization of pediatric CNS tumors10–22. Molecular biomarkers are progressively being incorporated into the diagnosis and management of certain pediatric CNS tumor types23.
One method to supplementally diagnose and subtype CNS tumors is DNA methylation24. Capper et al. developed a classification method to address previous issues in inter-observer variability for histopathological diagnosis of many CNS tumors24. Since the development of this method, DNA methylation classification is now used regularly for certain pediatric CNS tumor types, like ependymomas, to understand the prognosis and manage treatment decisions13,14. This method utilizes bisulfite-treated DNA, which does not distinguish between 5-methylcytosine (5mC) and 5-hydroxymethylcytosine, although it has been indicated only 5mC signal from oxidative bisulfite-treated DNA alters the classification from this method25,26. Moreover, while advancements have improved management strategies for some tumor types, many other pediatric CNS tumor types remain underexplored.
DNA methylation is one of the most well-studied epigenomic marks, primarily known for its role in regulating gene expression. DNA methylation occurs when a methyl group is added to the 5-carbon position of a cytosine in the context of a Cytosine-phosphate-Guanine (CpG) dinucleotides by DNA methyltransferases (DNMTs)27–32. Methylation of CpG island promoters is associated with repression of gene expression while methylation of gene bodies is associated with activation of gene expression33–35. 5mC many times co-exist with H3K9me3 marks and do not overlap with H3K4me3 marks and H2A.Z34,36,37. In addition, DNA methylation marks function as genome stabilizers by silencing transposable elements34,38. The main ways DNA methylation is altered in cancer include genome-wide hypomethylation in repetitive elements like retrotransposable elements39,40, hypermethylation of promoters40–43, and propensity for cytosines in CpG contexts to be mutated44–47.
Cytosines can also remain in a hydroxymethylated state (5-hydroxymethylcytosine, 5hmC). 5hmC is formed when 5mC is actively being demethylated by ten-eleven translocation (TET) enzymes48–50. TET enzymes add a hydroxyl group onto the methyl group to become 5-hydroxymethylcytosine, then add the hydroxyl group again to become 5-formylcytosine, then again to become 5-carboxylcytosine, which is excised to become unmethylated48–51. While 5hmC is an intermediate, it has been shown to have functional roles and be stable in the genome. Like 5mC, 5hmC has been associated with regulating transcription. It is enriched in gene bodies of active genes and in transcription start sites in which promoters are marked with H3K27me3 and H3K4me452,53. 5hmC has also been shown to play roles in maintaining pluripotency and tumorigenesis52,54. While generally 5hmC levels are relatively much lower than 5mC levels, higher levels of 5hmC are found in the brain tissue compared to other tissue and in embryonal stem cells developmentally programmed neuronal cells52,55–61. Although progress has been made since the discovery of TET enzymes producing 5hmC49–51, more investigation is needed to understand the functional roles of 5hmC. While alterations in hydroxymethylation patterns have not been as well examined, studies have indicated decreased hydroxymethylation across the genome in a variety of tumor types including adult and pediatric CNS tumors26,54,62–70, and mutations in hydroxymethylation-associated genes such as IDH1/2 and TET1/2/3 have been associated with certain tumor types like gliomas and acute myeloid leukemia62,71–74.
Numerous studies have established that brain tumors display intratumoral cellular heterogeneity17,19,20,75–85. While it is known that both DNA methylation and hydroxymethylation patterns are tissue type and cell type dependent52,53,86–90, limited research has addressed cell type-specific DNA cytosine modification alterations in these tumors. This gap exists largely due to the high cost and limitations in technologies to profile cytosine modifications at the cell type-specific scale91. While the importance of cell type composition effects in epigenome-wide association studies has been well documented92–96, single-cell methylation profiling strategies97–100 are slowly developing in comparison to more accessible and commercially available genome profiling technologies focused on gene expression or chromatin accessibility. To address these shortcomings, computational methods have been developed to deconvolute cell type composition using DNA methylation for certain tissue types91,101–109. While these methods have greatly improved our understanding of the cell type composition effects on many epigenome-wide association studies, they have not been utilized in investigating cell type composition effects on brain tumors due to some limited applicability in brain tissue.
In this study, we use a multi-omic approach to study cell type-level epigenomic alterations in pediatric CNS tumors to maximize the applicability of currently available methods. By integrating single nuclei RNA-seq and cytosine modification data, we provide a more complete picture of the cytosine modification alterations associated with pediatric CNS types and cytosine modifications that are associated with changes in transcription at the cell type level in pediatric CNS tumors.
Results
Our cohort included 32 tumor tissues (8astrocytomas, 6 embryonal tumors, 10 ependymomas, 8 glioneuronal/neuronal tumors) and 2 non-tumor tissue (Table 1). To assess the potential normal tissue margin in our tissues that may confound downstream analyses, we first determined the tumor purity of our pediatric CNS tumor samples that were used to measure DNA cytosine modifications. Tumor purity in our samples varied but did not significantly differ based on tumor type or grade (Supplementary Fig. 1). The genetic variants associated with each tumor can be found in ref. 110.
Table 1.
Subject demographics
| Tumor types | ||||||
|---|---|---|---|---|---|---|
| Total (N = 34) | Astrocytoma (N = 8) | Embryonal (N = 6) | Ependymoma (N = 10) | Glioneuronal/neuronal (N = 8) | Non-Tumor (N = 2) | |
| Sex | ||||||
| F | 14 (41 %) | 3 (38%) | 3 (50%) | 5 (50%) | 1 (12%) | 2 (100%) |
| M | 20 (59 %) | 5 (62%) | 3 (50%) | 5 (50%) | 7 (88%) | 0 (0%) |
| Age (years) | ||||||
| Mean (SD) | 8.5 (±5.3) | 5.6 (±4.5) | 9.2 (±5.4) | 9.5 (±4.3) | 10.5 (±6.5) | 5.8 (±7.4) |
| Grade | ||||||
| High | 12 (35 %) | 0 (0%) | 6 (100%) | 5 (50%) | 1 (12%) | 0 (0%) |
| Low | 18 (53 %) | 8 (100%) | 0 (0%) | 4 (40%) | 6 (75%) | 0 (0%) |
| NEC/NOS | 2 (6 %) | 0 (0%) | 0 (0%) | 1 (10%) | 1 (12%) | 0 (0%) |
| Missing | 2 (5.9%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (100%) |
| Location | ||||||
| Metastasis | 1 (3 %) | 1 (12%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Subtentorial | 19 (56 %) | 5 (62%) | 5 (83%) | 8 (80%) | 1 (12%) | 0 (0%) |
| Supratentorial | 14 (41 %) | 2 (25%) | 1 (17%) | 2 (20%) | 7 (88%) | 2 (100%) |
Epigenomic burden from altered cytosine modifications in pediatric CNS tumors
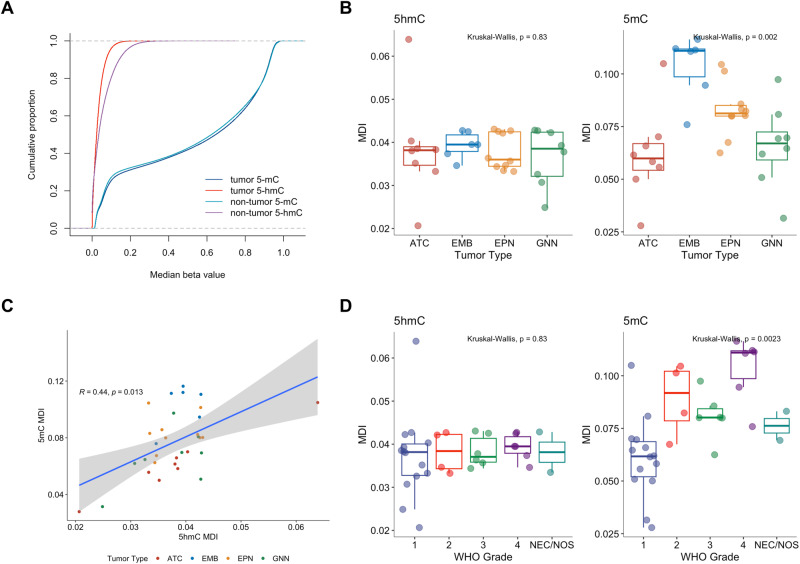
To determine the global epigenomic burden of altered cytosine modifications in pediatric CNS tumors compared to non-tumor pediatric brain tissue, we compared median beta values for both 5hmC and 5mC across samples at each CpG and determined the methylation dysregulation index (MDI). MDI is a summary measure of the epigenome-wide alteration of tumors compared to non-tumor tissue111. Tumor tissues (N = 32) displayed a decrease in median 5hmC beta values and a slight increase in median 5mC beta values compared to non-tumor tissue (Non-tumor tissue N = 2; KS test: 5mC: D = 0.019, p < 2.2e-16; 5hmC: D = 0.19, p < 2.2e-16; Fig. 1A). The 5hmC MDI values were not significantly different by tumor type (N = 8 (ATC), 6 (EMB), 10 (EPN), 8 (GNN)) or by tumor grade (N = 14 (G1), 5 (G2), 6 (G3), 6 (G4); Fig. 1B), whereas 5mC MDI values varied by tumor type. Embryonal tumors had the greatest extent of epigenome-wide alteration burden compared to non-tumor tissue, astrocytomas had the lowest burden of 5mC MDI compared to non-tumor tissue, and we observed increasing 5mC MDI with increasing tumor grade. 5hmC MDI and 5mC MDI were positively correlated (R = 0.44, p = 0.013, Fig. 1C). We repeated our analysis after removing one astrocytoma sample with an outlier 5hmC MDI value and observed consistent results (Supplementary Fig. 2). In addition, we determined MDI for distinct genomic contexts and again found consistent results in which 5mC MDI, but not 5hmC MDI values significantly varied among tumor types (Supplementary Fig. 3). Interestingly, both 5hmC MDI and 5mC MDI in gene body, enhancer and exon regions were slightly, but statistically significantly higher than 5hmC MDI and 5-MDI when adjusted for tumor types (Supplementary Table 2). For both 5hmC and 5mC, MDI were highest in enhancers, then gene body/exon regions, and were lowest in promoter CpGs. We tested and confirmed that the burden of observed epigenomic alterations was not due to differences in tumor purity (Supplementary Fig. 4, Supplementary Table 3A). However, we did observe significant differences in 5mC MDI by tumor grade (Supplementary Table 3B). While 5hmC is prevalent at only 6% of 5mC, the level of dysregulation of the hydroxymethylome is comparable to the level of dysregulation of the methylome with 5hmC MDI being 49% of 5mC MDI (Supplementary Table 4). Our results suggest that while 5hmC may not be as prevalent, epigenome-wide alterations of 5hmC in tumors are occurring at comparable levels to altered 5mC.
Fig. 1. Global methylation dysregulation, but not global hydroxymethylation dysregulation, is associated with tumor type and grade.
A Cumulative proportion of median 5hmC and median 5mC in tumors (N = 32) and non-tumor tissue (N = 2). B Methylation dysregulation index of 5-mC and 5mC by tumor type (N = 8 (ATC), 6 (EMB), 10 (EPN), 8 (GNN)) and (D) grade (N = 14 (G1), 5 (G2), 6 (G3), 6 (G4)). Differences in MDI were calculated using the rank-based Kruskal-Wallis test. C Correlation between 5hmC MDI and 5mC MDI calculated using Spearman rank correlation. Linear regression line is indicated by the blue line. 95% confidence interval of the linear regression line indicated by gray bands. Color of each point indicates tumor type. In the boxplots of (B) and (D), the low ends of the segment indicate the minimum and the high ends of the segment indicate the maximum. Lower bounds of the box indicate the 25th percentile and the higher bounds of the box indicate the 75th percentile. Segment in the middle is the median. Source data are provided as a Source Data file.
Cell type composition influences bulk-omics comparisons between pediatric CNS tumors and non-tumor pediatric brain tissue
We utilized our single nuclei RNA-seq data to identify the cell type composition of pediatric CNS tumor tissue and non-tumor pediatric brain tissue110. The cell types identified in our cohort like radial glial cells (RGC) in ependymoma were similar to comparable pediatric CNS tumors in previous literature22,112. As we wanted to account for major cell types present that may confound comparisons between the epigenomes of tumors and non-tumors, we identified the cell types present with most variability. Based on the cell type proportion distributions for all of our samples, we identified neuronal-like cells (NEU), neural stem cells (NSC), oligodendrocyte precursor cells (OPC), RGC, and unipolar brush cells (UBC) as having the most variance from PCA analysis (Supplementary Fig. 5A, B). For each tumor type we compared proportions of cell types with non-tumor pediatric brain tissue. Supporting our principal component analysis, the cell types with the greatest differences were NEU, NSC, OPC, RGC, and UBC (Supplementary Fig. 5C).
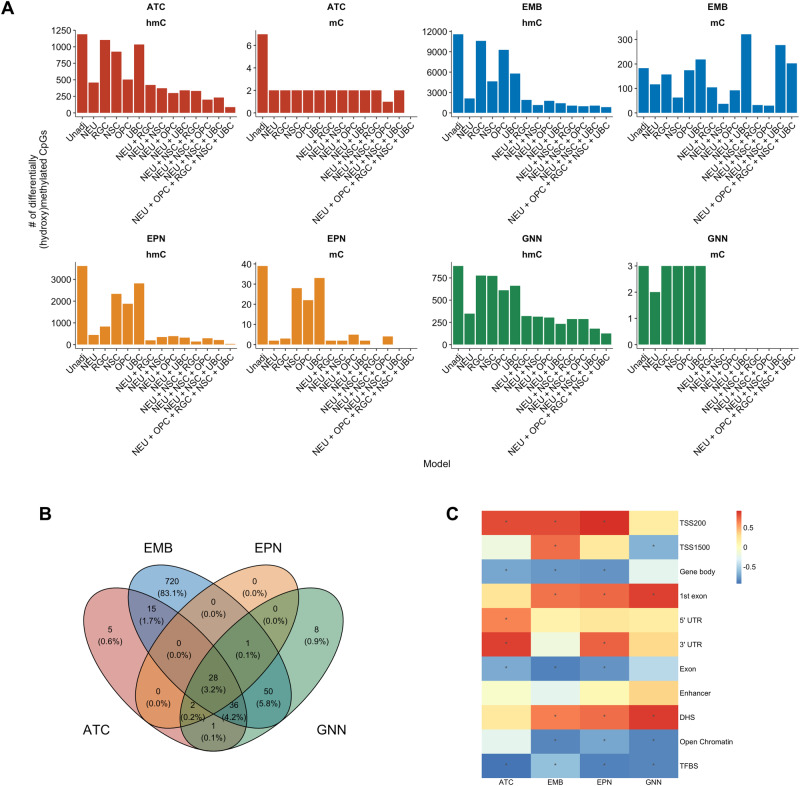
We conducted an epigenome-wide association study to determine the differential hydroxymethylated and methylated CpGs associated with each tumor type (N = 8 (ATC), 6 (EMB), 10 (EPN), 8 (GNN)) compared to non-tumor pediatric brain tissue (N = 2). To reduce potential confounding by cell type composition, we incorporated cell type proportions as covariates in a stepwise manner to each series of linear models. Age at diagnosis, sex, and tumor purity were adjusted to reduce potential confounding from these variables in these linear models. Due to sample size, tumor location was not included in the model. Importantly, as the number of cell type proportion covariates included in the models increased, the scope of differentially hydroxymethylated and differentially methylated CpGs associated with each tumor type decreased (Fig. 2A, Table 2, Supplementary Figs. 6–9, Supplementary Data 1–8). In addition, across our models in different tumor types, the extent of differentially hydroxymethylated CpGs (dhmCpGs) was far greater than that of differentially methylated CpGs (dmCpGs). When all five cell types (NEU, NSC, OPC, RGC, and UBC) were incorporated into the model, we observed low number of dmCpGs associated with each tumor type. Embryonal tumors had the greatest number of dhmCpGs, and the 83.1% were specific to the embryonal tumors (Fig. 2B). In the model with all five cell types included, 87 dhmCpGs were associated with astrocytoma, 850 dhmCpGs were associated with embryonal tumors, 31 dhmCpGs were associated with ependymoma, and 126 dhmCpGs were associated with glioneuronal/neuronal tumors. We identified 90 dhmCpGs (10.4%) that were shared across two or three of the tumor types and 28 dhmCpGs (3.2%) that were shared across all tumor types (Fig. 2B, Supplementary Table 5). The 28 shared CpGs were located predominantly in island (42.9%) and open sea (42.9%) regions in relation to CpG islands (Supplementary Table 6). In addition, 64.3% of the shared dhmCpGs were in DNase hypersensitive sites (DHS) (Supplementary Table 7). The shared CpGs tracked to genes including ESRRG, HECA, THBD, and TJP1 (Supplementary Table 5).
Fig. 2. Adjusting for proportions of cell types of interest reduces the number of differentially hydroxymethylated and methylated CpGs across tumor types compared to non-tumor pediatric brain tissue.
A The number of differentially hydroxymethylated (hmC) and methylated (mC) CpGs under q < 0.05 threshold in astrocytoma (ATC), embryonal tumors (EMB), ependymoma (EPN), and glioneuronal/neuronal tumors (GNN) compared to non-tumor pediatric brain tissue. X-axes indicate each cell type proportion included in the model. Each model, even ‘unadjusted’ models, includes sex and age at diagnosis in the linear model. B Venn diagram of the differentially hydroxymethylated CpGs among the different tumor types. C Heatmap of correlation between number of cell types included in model and proportion of dhmCpGs per genomic context. Correlation calculated by Spearman rank test. Heatmap cells with * indicate statistically significant correlation at p < 0.05. Source data are provided as a Source Data file.
Table 2.
Summary of dmCpGs in unadjusted and five-cell type adjusted EWAS model
| Unadjusted model dmCpGs N (%) |
dmCpGs that are also dhmCpGs N (%) |
Adjusted model dmCpGs N (%) |
dmCpGs that are also dhmCpGs N (%) |
|
|---|---|---|---|---|
| Astrocytoma (ATC) | 7 (0.001%) | 3 (42.9%) | 0 (0%) | 0 (0%) |
| Embryonal (EMB) | 183 (0.04%) | 90 (49.1%) | 202 (0.04%) | 15 (7.4%) |
| Ependymoma (EPN) | 39 (0.008%) | 25 (64.1%) | 0 (0%) | 0 (0%) |
| Glioneuronal/neuronal (GNN) | 3 (0.0006%) | 1 (33.3%) | 0 (0%) | 0 (0%) |
We then investigated if specific genomic regions were associated with the changes in the number of dhmCpGs by assessing the relationship between the proportion of the dhmCpGs for each genomic context with each model using Spearman rank tests. We identified positive relationship between number of cell types included in the model and the proportion of dhmCpGs in regions within 200 bps of the transcription start sites (TSS200) and 1st exon regions (Fig. 2C, Supplementary Fig. 10). Moreover, we found negative relationship between the number of cell types included in the model and the proportion of dhmCpGs in gene body, open chromatin, and transcription factor binding sites. Our results suggest that epigenome-wide association studies comparing bulk pediatric CNS tumor tissue to non-tumor pediatric tissue are considerably influenced by the cell type composition, especially in promoter and gene body genomic regions. Moreover, it was quite unexpected that the observed differences were almost solely in hydroxymethylation and not in methylation.
We then compared transcriptome data from bulk RNA-seq in each of the tumor types (N = 8 (ATC), 6 (EMB), 10 (EPN), 8 (GNN)) with non-tumor pediatric brain tissue (N = 2). The differential expression testing model included the same covariates (sex, age at diagnosis, and tumor purity) and the same five cell type proportions used for the EWAS analysis. Including proportions of major cell types of interest led to differences in an average of around 702 genes (range: 536–892) detected as significantly differentially expressed. In astrocytoma and glioneuronal/neuronal tumors, the adjusted model identified more genes that were significantly differentially expressed. In embryonal tumors and ependymomas, the adjusted model identified fewer genes that were significantly differentially expressed. Some key tumor progression-associated genes like PTEN in astrocytoma and in embryonal tumors, MYCN in ependymoma, and BRCA2 in glioneuronal/neuronal tumors would not otherwise have been identified as significantly differentially expressed in the tumors had the cell type proportions not been adjusted for.
As we reduced potential confounding effects from cell type composition differences, we sought to explore genes with differential expression that were specifically associated with the tumors. Across all tumor types, the majority of differentially expressed genes were increased in expression compared to the non-tumor pediatric brain tissue (Supplementary Fig. 11A, 12–15, Supplementary Data 9–16). Almost half (43%, 3020 genes) of all genes with increased expression were shared across all tumor types (Supplementary Fig. 11B). Among the genes with shared increases in expression in tumors were IRX5, MYOSLID, CWH43, ITGA2, and HOXA3. Genes with increased expression across all tumor types were associated with biological oxidations and keratinization among other pathways (Supplementary Fig. 11D). There were 253 genes (13.6%) that had decreased expression shared across tumor types (Supplementary Fig. 11C), including NPTXR, SCG2, B4GAT1, and ATRN. Genes that were decreased in expression across all tumor types were associated with the insulin receptor signaling and ion channel transport among other pathways (Supplementary Fig. 11E). Our results suggest potential non-cell type-specific avenues for therapy that may be shared across the pediatric CNS tumor types.
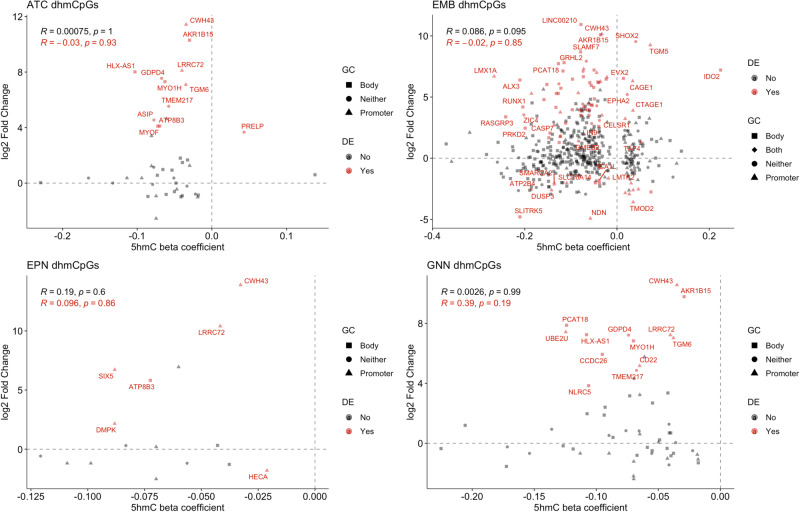
To identify potentially important gene regulation by differential hydroxymethylation we compared changes in hydroxymethylation in dhmCpGs from the five-cell type-adjusted model with gene expression in each tumor type (N = 8 (ATC), 6 (EMB), 10 (EPN), 8 (GNN)). The genes we identified in our differential gene expression analysis were used in comparisons to changes in 5hmC. Generally, genes with decreased hydroxymethylation levels had increased gene expression across tumor types compared to non-tumor pediatric brain tissue (Fig. 3). When correlations between changes in 5hmC and changes in gene expression were performed to assess any directional relationship, the correlation coefficients across all tumor types were non-existent and not statistically significant even for genes that had statistically significant changes in gene expression (R, p = −0.03, 0.93 (ATC); −0.02, 0.85 (EMB); 0.096, 0.86 (EPN); 0.39, 0.19 (GNN), Fig. 3).
Fig. 3. Hypo-hydroxymethylation of CpGs is associated with changes in gene expression.
Association between differentially hydroxymethylated CpG beta coefficients and log2 fold changes in gene expression for astrocytoma, embryonal tumors, ependymoma, and glioneuronal/neuronal tumors. Red points indicate significantly differentially expressed genes. Shapes indicate genomic context of CpGs. Correlations were calculated using the Pearson method. Differential hydroxymethylated CpGs were identified from linear regression model and significant dhmCpGs were identified using q < 0.05 significance threshold. Log2 fold changes in gene expression were identified from negative binomial regression model and significantly differentially expressed genes were identified using adjusted p value threshold <0.05. Source data are provided as a Source Data file.
Only one dhmCpGs associated with ependymoma had significant decreased expression. The dhmCpGs with differential expression did not generally favor promoters or gene body regions (Fig. 3, Supplementary Table 8). Only embryonal tumors displayed slightly varying associations. While many of the dhmCpGs associated with embryonal tumors followed similar patterns of decreased 5hmC levels and increased gene expression, there were some CpGs with decreased 5hmC and decreased gene expression, as well as CpGs with increased 5hmC with increased or decreased gene expression levels. Embryonal tumor associated dhmCpGs with significantly increased gene expression were less likely to be in promoter regions compared to dhmCpGs with significantly decreased gene expression (OR = 0.23, 95% CI = 0.064–0.78, p = 0.01). On the contrary, embryonal tumor associated dhmCpGs with significant increased expression were marginally more likely to be in gene body regions (OR = 2.81, 95% CI = 0.84–10.34, p = 0.06). We could not test for associations between promoter or gene body regions for other tumor types due to the limited number of dhmCpGs.
Interestingly, there were two CpGs with decreased 5hmC levels and increased gene expression in astrocytoma, ependymoma, and glioneuronal/neuronal tumors: cg18280362 located in the promoter region of CWH43 and cg08278401 located in the promoter region of LRRC72. In addition, we investigated the association between changes in 5mC methylation and gene expression in the embryonal tumors where there were 24 dmCpGs associated with significant changes in gene expression (Supplementary Fig. 16). Unlike dhmCpGs, magnitude of changes in 5mC levels were negatively associated with magnitude of changes in gene expression for genes that did not have statistically significant gene expression changes (R = −0.45, p = 0.029) and genes with statistically significant gene expression changes (R = −0.41, p = 0.0002, Supplementary Fig. 16). While we could not conduct statistical tests to test for an enrichment of promoter/gene body regions for shared dhmCpGs with increased gene expression, there were 18 dhmCpGs with increased gene expression in non-promoter regions and 3 dhmCpGs with increased gene expression in promoter regions. Moreover, there were 9 dhmCpGs with increased gene expression not in gene body regions and 12 dhmCpGs in gene body regions. Our results suggest potential roles of hydroxymethylation in regulating gene expression of certain pediatric CNS tumor-associated genes, that require further investigation to validate.
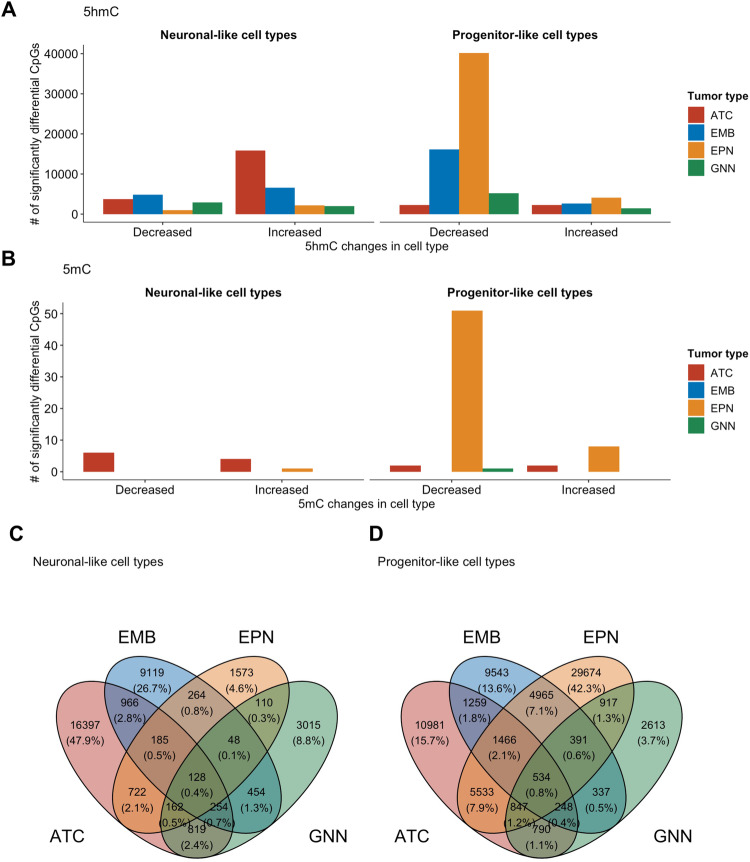
Molecular alterations in pediatric CNS tumors occur in a cell type-specific and tumor type-specific manner
One of the major questions that remains unanswered in many epigenome-wide association studies is whether altered cytosine modification can be ascribed to a specific cell type. With data from single nuclei RNA-seq for these pediatric CNS tumors and non-tumor pediatric brain tissues, we sought to identify epigenomic alterations at a cell type-specific level. To reduce the number of covariates in our analysis we focused on neuronal-like and progenitor-like cell types (Supplementary Table 9). The progenitor-like cells were an aggregation of NSC, RGC, OPC, and UBC. We used an approach developed by ref. 103 called CellDMC to identify cell-type-specific differentially hydroxymethylated and methylated CpGs. We compared the epigenome of each tumor type to non-tumor tissue and used CellDMC to identify which cell type was driving the change in 5hmC and 5mC in the tumors compared to the non-tumor tissue. Overall, we identified abundant dhmCpGs for each cell type and tumor type, far greater than the scope of CpGs identified with bulk tissue EWAS (Fig. 4A, Supplementary Figs. 17–20, Supplementary Table 10, Supplementary Data 17–20). While there were a relatively lower number of dmCpGs compared to the dhmCpGs, there were some dmCpGs detected in the cell type-specific model (Fig. 4B). Majority of the cell type-specific dhmCpGs were tumor-type-specific (Fig. 4C, D, Supplementary Fig. 21). However, 128 dhmCpGs were observed in the neuronal-like cell types and 534 dhmCpGs were observed to be driven by the progenitor-like cell types across all four tumor types. While some neuronal-like cell-specific driven dhmCpGs were acting on the same genes as the progenitor-like cell-specific dhmCpGs, genes that had decreased 5hmC in the progenitor-like cells were exclusive (Supplementary Fig. 22).
Fig. 4. 5hmC is altered in cell type-specific and tumor type-specific manner.
Cell type driven differentially (A) hydroxymethylated and (B) methylated CpGs in each tumor type identified by epigenome wide association study adjusted for cell type proportions. Significantly differentially hydroxymethylated and methylated CpGs were defined by q < 0.05. Venn diagram of shared differentially hydroxymethylated CpGs in (C) neuronal-like cell types and (D) progenitor-like cell types across the four tumor types. Number of cell type driven differential CpGs were statistically significant under adjusted p < 0.05. ATC Astrocytoma, EMB Embryonal tumors, EPN Ependymoma, GNN Glioneuronal/neuronal tumors. Source data are provided as a Source Data file.
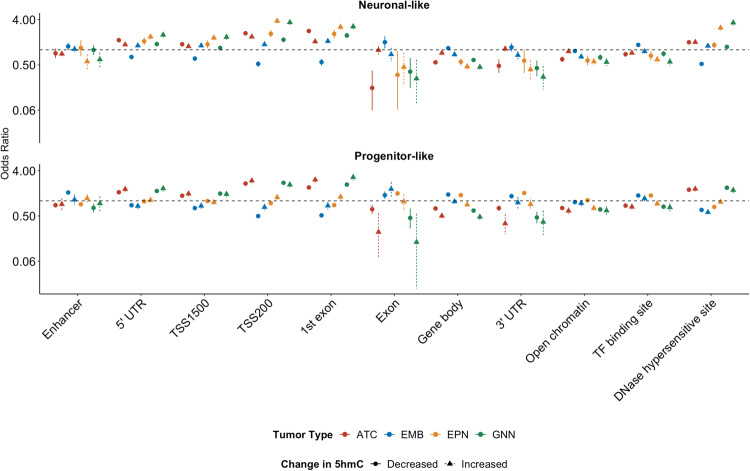
We then assessed the genomic context of cell type-specific dhmCpGs and tested for enrichment to various genomic contexts stratified by the direction of differential hydroxymethylation. Interestingly, both increased and decreased dhmCpGs in neuronal-like and progenitor-like cell types of astrocytoma and glioneuronal/neuronal tumors were enriched in similar contexts at DHS, 1st exons, promoter regions (TSS200, TSS1500), and 5’ UTR regions (Fig. 5, Supplementary Data 21). dhmCpGs in ependymoma were dependent on the cell type in which it was occurring. Ependymoma-associated dhmCpGs in the NEU and CpGs with increased 5hmC in progenitor-like cells were enriched in similar regions as the astrocytoma and glioneuronal/neuronal tumors. On the contrary, ependymoma-associated CpGs with decreased 5hmC in the progenitor-like cells were enriched in transcription factor binding sites (TFBS), 3’ UTR, gene body, and exon regions. The dhmCpGs, especially for those occurring in the progenitor-like cell types, in embryonal tumors were enriched in distinct genomic contexts compared to the other tumor types. Progenitor-like cell type-specific dhmCpGs were enriched in the transcription factor binding sites, 3’ UTR, gene body, exons, and enhancers.
Fig. 5. Cell type-specific differential hydroxymethylation tumor type-specific.
Enrichment of differentially hydroxymethylated CpGs at specific genomic contexts by tumor type and direction of differential methylation as represented by odds ratios and 95% confidence intervals. Odds ratio points and confidence intervals colored by tumor type. The direction of 5hmC change is indicated by the shape indicating the odds ratio. Odds ratios were calculated by Mantel-Haenszel test. Source data are provided as a Source Data file.
Our findings indicate that hydroxymethylation alterations are driven by different cell types in different tumor types.
Cell type-specific gene expression changes associated with changes in hydroxymethylation
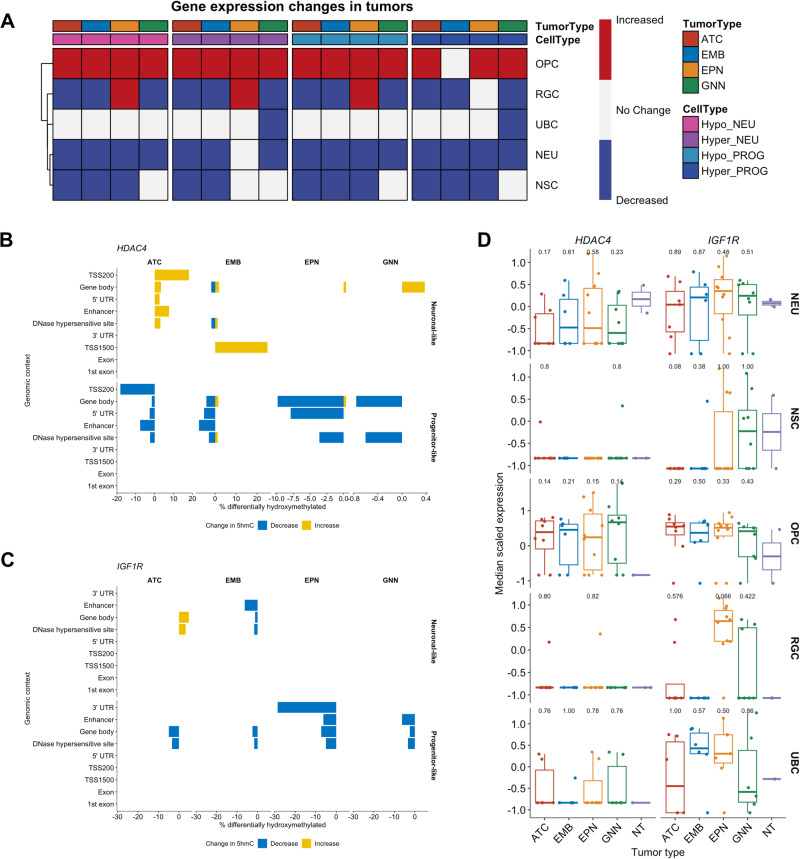
We next evaluated cell-specific gene expression changes for genes with cell-type-specific changes in hydroxymethylation. We calculated gene expression scores for genes associated with CpGs with differentially hydroxymethylated CpGs in the neuronal-like cells and progenitor-like cells for each granular cell types incorporated in our analysis for each tumor type (Supplementary Figs. 23–26). Interestingly, for all tumor types, the expression scores for genes associated with CpGs with increased or decreased hydroxymethylation were increased in the OPCs of the tumors compared to non-tumor pediatric brain tissue (Fig. 6A). Only the OPCs in embryonal tumors did not show a statistically significant increase in the expression of genes with increased 5hmC in the progenitor-like cells. On the contrary, gene expression levels for each of the gene sets with cell type-specific alterations in 5hmC were decreased in each of the cell types for all tumors compared to the non-tumor pediatric brain tissue.
Fig. 6. Alterations in hydroxymethylation are associated with cell type-specific changes in gene expression.
A Summary heatmap of changes in gene expression in the gene sets with differentially hydroxymethylated CpGs per cell type. The proportion of differentially hydroxymethylated CpGs associated with (B) HDAC4 and (C) IGF1R at each genomic context across the different tumor types in neuronal-like cell types and progenitor-like cell types. Blue bars indicate the proportion of hydroxymethylated CpGs that are decreased in the tumors. Yellow bars indicate the proportion of hydroxymethylated CpGs that are increased in the tumors. D Gene expression levels of HDAC4 and IGF1R for each cell type across the tumor types and non-tumor tissue. Sample size: ATC = 8, EMB = 6, EPN = 10, GNN = 8. Differences between each tumor type to non-tumor tissue were determined by Wilcoxon rank sum test. Number above the boxplot indicates p value from the Wilcoxon rank sum test. In the boxplots of (D), the low ends of the segment indicate the minimum and the high ends of the segment indicate the maximum. Lower bounds of the box indicate the 25th percentile and the higher bounds of the box indicate the 75th percentile. Segment in the middle is the median. Source data are provided as a Source Data file.
HDAC4, established as associated with cancer progression and poor prognosis in a variety of tumor types113–121, was one gene with cell type-specific dhmCpGs across all four tumor types. Interestingly, the majority of the CpGs with decreased 5hmC were associated with progenitor-like cell types, while the majority of the CpGs with increased 5hmC were associated with the neuronal-like cell types in the tumor tissue (Fig. 6B). More than 50% of the dhmCpGs in HDAC4 for each tumor type were in the gene body (Table 3). There were few dhmCpGs in the 5’ UTR, TSS200, and DHS. The neuronal-like cell types had lower expression of HDAC4 across all tumor types compared to the non-tumor tissue (Fig. 6D). On the contrary, the progenitor-like cell types had higher levels of HDAC4 expression. However, these differences in gene expression in each cell type of each tumor type compared to the same cell types in non-tumor tissues were not statistically significant which was likely due limitations from sample size (Fig. 6D).
Table 3.
Genomic context of dhmCpGs in (A) HDAC4 and (B) IGF1R for each tumor type
| A) HDAC4 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| TSS200 | TSS1500 | Gene body | 1st exon | 5’ UTR | 3’ UTR | Exon bound | Enhancer | DHS | dhmCpG total | |
| ATC | 2 (15%) | 0 (0%) | 10 (77%) | 0 (0%) | 1 (8%) | 0 (0%) | 0 (0%) | 1 (8%) | 5 (38%) | 13 |
| EMB | 0 (0%) | 1 (5%) | 16 (84%) | 0 (0%) | 2 (11%) | 0 (0%) | 0 (0%) | 1 (5%) | 9 (47%) | 19 |
| EPN | 0 (0%) | 0 (0%) | 27 (90%) | 0 (0%) | 3 (10%) | 0 (0%) | 0 (0%) | 0 (0%) | 6 (20%) | 30 |
| GNN | 0 (0%) | 0 (0%) | 2 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (50%) | 2 |
| B) IGF1R | ||||||||||
| ATC | 0 (0%) | 0 (0%) | 4 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (50%) | 4 |
| EMB | 0 (0%) | 0 (0%) | 3 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (33%) | 2 (67%) | 3 |
| EPN | 0 (0%) | 0 (0%) | 6 (75%) | 0 (0%) | 0 (0%) | 2 (25%) | 0 (0%) | 1 (13%) | 3 (38%) | 8 |
| GNN | 0 (0%) | 0 (0%) | 2 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (50%) | 2 (100%) | 2 |
IGF1R had dhmCpGs across all tumor types and is associated with tumorigenesis, therapy resistance, and poor survival in different cancer types, including in some pediatric CNS tumor types122–132. Most of the dhmCpGs with decreased 5hmC were associated with the progenitor-like cell types in the tumor tissue while only a couple dhmCpGs were in the neuronal-like cell types of the tumor tissue (Fig. 6C). Like HDAC4, the dhmCpGs in IGF1R were mostly located in the gene body and DHS, with a few scattered in the enhancer and 3’ UTR regions (Table 4). Consistent with the lack of changes in hydroxymethylation in the neuronal-like cell types of the tumors, gene expression levels of IGF1R did not differ between tumors and the non-tumor tissue among neuronal-like cell types (Fig. 6D). However, following the decreases in hydroxymethylation, IGF1R gene expression levels were higher in the progenitor-like cell types, particularly the OPCs, in the tumors than in the progenitor-like cell types of non-tumor tissue. As with HDAC4, the differences between each cell type of each tumor type and same cell type of non-tumor tissues were also not statistically significant (Fig. 6D). EWAS results from bulk tumor tissue identified only one or two CpGs in HDAC4 and IGF1R as differentially hydroxymethylated in either cell type-adjusted or unadjusted model (Table 4).
Table 4.
Comparison of the number of differentially hydroxymethylated CpGs in HDAC4 and IGF1R identified by bulk tissue EWAS and CellDMC for each tumor type
| Tumor type | Bulk EWAS (CT unadjusted) | Bulk EWAS (CT adjusted) | CellDMC (Neuronal-like) | CellDMC (Progenitor-like) | |
|---|---|---|---|---|---|
| HDAC4 | ATC | 0 | 0 | 12 | 7 |
| EMB | 1 | 1 | 11 | 17 | |
| EPN | 1 | 0 | 1 | 30 | |
| GNN | 0 | 0 | 1 | 2 | |
| IGF1R | ATC | 0 | 0 | 4 | 4 |
| EMB | 2 | 0 | 1 | 2 | |
| EPN | 1 | 0 | 0 | 8 | |
| GNN | 0 | 0 | 0 | 2 |
Our results suggest potential roles of hydroxymethylation of CpGs located within the gene body regions in affecting the gene expression of critical cancer genes, like HDAC4 and IGF1R. However as statistical significance levels were not reached in cell type specific differences in gene expression levels likely due to limited sample size, further experimentation is needed to validate these results.
Discussion
In this study, we investigated the cell type-specific cytosine modification alterations in pediatric central nervous system tumors with a multi-omic approach. We described the cell type composition effects that occur in epigenome-wide association studies using bulk pediatric central nervous system tumors and non-tumor pediatric brain tissue. We identified that there were more differentially hydroxymethylated CpGs associated with each tumor type, particularly in the progenitor-like cell types, rather than differentially methylated CpGs. Lastly, we show that the cell type-specific changes in hydroxymethylation are associated with cell type-specific gene expression changes in pediatric central nervous system tumors.
Based on methods to classify tumor subtypes and the predominant focus on DNA methylation, it was unexpected that there were very few differentially methylated CpGs associated with each tumor type. One possible explanation for this phenomenon may be that as these are pediatric tissues, there is still ongoing development with which 5hmC is associated. As our results suggest the epigenome-wide alterations of 5hmC in these tumors, it may be critical to distinguish between 5mC and 5hmC to better understand the molecular underpinnings of these pediatric CNS tumors. Furthermore, it may be beneficial to incorporate 5hmC into cytosine modification-based classification methods to improve performance.
Pediatric tumors are known not to have substantial genetic alterations133. Our results suggest that pediatric CNS tumors may be characterized by non-mutational epigenomic reprogramming134,135. We identified a substantial number of differentially hydroxymethylated CpGs associated with progenitor-like cell types of each tumor type. Additionally, even among the shared differentially hydroxymethylated CpGs in the progenitor-like cell types, numerous differentially hydroxymethylated CpGs were located within different genes that regulate epigenetic patterns, such as DNMT3A, HDAC4, MLLT3, and KAT2B. Furthermore, pediatric brain cancers have been shown to contain somatic mutations in epigenetic regulator genes such as H3F3A, KDM6A, and MLL3136–138. Considering the dysregulation of the epigenome may be important when developing innovative therapeutic strategies for these tumors.
While much more investigation has been conducted into how DNA methylation regulates gene expression, less is known about how DNA hydroxymethylation can also be associated with changes in gene expression. We identified relationships between cell type-specific hydroxymethylation patterns and cell type-specific gene expression in our pediatric CNS tumors. Our findings indicate that hydroxymethylation changes in the gene body regions can alter gene expression. Previous studies have found positive associations between DNA methylation in gene body regions and gene expression changes33,44. However, many genome-wide DNA methylation studies use the traditional bisulfite treatment approach to measure 5mC. Because bisulfite treatment alone cannot distinguish between 5mC and 5hmC25, some methylation signals may have been from 5hmC. Further studies that explicitly distinguish between 5hmC and 5mC are needed to gain a clearer understanding of the effects of DNA cytosine modifications on gene expression.
We identified two genes, HDAC4 and IGF1R, in our pediatric CNS tumors that were both epigenetically and transcriptionally altered in comparison to non-tumor pediatric brain tissue. HDAC4 and IGF1R had differentially hydroxymethylated CpGs and increased expression in OPCs across all four of our tumor types. Our results suggest a potential role of hydroxymethylation regulating genes associated with tumorigenesis. With these targets already having been studied in adult cancers, there are pharmacological inhibitors that already exist for these targets. Our study expands previously suggested ideas of targeting HDAC4 and IGF1R in certain pediatric CNS tumor types127,139,140.
Accruing a large sample size for pediatric CNS tumors is particularly difficult as they are very rare in the general population. The limited sample size prevented us from including other potential variables like tumor location. As different parts of the brain may be composed of differing cell types, not adjusting for tumor location introduces limitations in our conclusions. However, as we compare the epigenome within major cell types, we believe that some limitations of not including tumor location were addressed. Furthermore, the limited sample size reduced our statistical power in our analyses. While our study does incorporate a reasonable sample size for these rare tumors, the smaller sample size limited the inclusion of other variables and cell types that may affect methylation and transcription into our models. Moreover, our study incorporates multiple genome-wide and epigenome-wide molecular features of the matched tumor sample to give a more comprehensive landscape of each tumor type. Multi-omic approaches involving single nuclei RNA-seq, bulk RNA-seq, 5mC, 5hmC epigenome profiles of different pediatric CNS tumors have been limited in investigations to our knowledge.
Future studies with an expanded cohort of pediatric CNS patients will allow us to assess the epigenomic alterations in additional cell types of interest, such as glial cells. Moreover, following our findings of cell type-specific changes in DNA cytosine modifications in these pediatric CNS tumors, other tumor types may also have cell type-specific that have yet to be detected. Tools to understand the cell type composition of tissues should be incorporated in bulk epigenome-wide association studies to discriminate the cell type composition effects.
Our study addresses gaps that currently exist in understanding epigenomic alterations at the cell type level in pediatric central nervous system tumors. Changes in hydroxymethylation were particularly drastic in progenitor-like cells and were associated with cell type level alterations in transcription. We highlight the relevance of epigenome dysregulation in pediatric central nervous system tumors that may lead us to more effective therapeutic targets.
Methods
This study complies with all Dartmouth Hitchcock Medical Center Institutional Review Board regulations. This study was approved by the Dartmouth Hitchcock Medical Center Institutional Review Board Study #00030211. Parents/legal guardians of the subjects provided consent for the use of tissues for research purposes.
Sample information
Cytosine modifications, bulk tissue gene expression, and single nuclei gene expression were measured in 32 pediatric CNS tumors of various types and 2 non-tumor pediatric brain tissues (Table 1, Supplementary Table 1). Only samples with all four molecular measurements were included in downstream analyses. The samples were collected from patients being treated at Dartmouth-Hitchcock Medical Center and the Dartmouth Cancer Center from 1993 to 2017. For each tumor type, the number of samples was distributed evenly with 8 samples for astrocytoma, 6 for embryonal tumors, 10 for ependymoma, and 8 for glioneuronal/neuronal tumors. Pathological re-review for the histopathologic tumor type and grade were done according to the 2021 World Health Organization CNS tumor classification system, then categorized into broader tumor types. The non-tumor pediatric brain tissues were obtained from patients who underwent surgical resection for epilepsy.
Data collection and pre-processing
Single nuclei RNA-sequencing
Nuclei were isolated from fresh frozen tissue samples following the Nuclei Pure Prep nuclei isolation kit (Sigma-Aldrich, St. Louis, MO) with some modifications The samples were first washed with PBS to remove extraneous OCT the samples were frozen in. The tissue was homogenized with both wide and narrow pestles submerged in 2.5 mL of the lysis buffer in a Dounce homogenizer. The lysate mixed with 4.5 mL 1.8 M sucrose cushion were gently layered on top of the 2.5 mL of 1.8 M sucrose cushion in Beckman ultracentrifuge tubes. Samples were centrifuged for 45 min at 22,673 g at 4 °C in an ultracentrifuge. Each sample was multiplexed with lipid-tagged oligonucleotides following the MULTI-seq protocol141. Libraries for single nuclei RNA-seq were prepared following the 10X Genomics Single Cell Gene Expression workflows (10X Genomics, Pleasanton, CA). Libraries were pooled and sequenced using the Illumina NextSeq500 instrument. 10X Cell Ranger software was used to align sequences to the GRCh38 pre-mRNA reference genome.
Low-quality nuclei, as defined as having greater than 10,000 and less than 2000 features and more than 5% of reads that map to mitochondrial genes, were removed for analyses. Samples were demultiplexed using an integrative approach, combining barcode based demultiplexing and genotype-based demultiplex method142,143. Pooled nuclei were demultiplexed by hashtag oligonucleotides using HTODemux function in Seurat v4142,144–146. Pooled samples were also demultiplexed using Vireo, a genotype based demultiplexing method143. We performed genetic demultiplexing analysis using genotype data following the methods described in ref. 147, implemented in a Nextflow workflow148. Briefly, bulk RNA-seq reads from each sample were mapped to the reference genome (GRCh38.p13) using STAR149. Pooled single-nuclei RNA-seq reads were mapped to the reference genome using STARsolo150. Variants among the samples within each pool were identified and genotyped with bcftools mpileup151 using the mapped bulk reads. Individual cells were then genotyped only at the sites identified using the bulk RNA using cellsnp-lite (mode 1a)152. Cell genotypes were used to identify the sample of origin for each cell using Vireo143. Code for the genetic demultiplexing workflow can be found at https://github.com/AlexsLemonade/alsf-scpca/tree/main/workflows/genetic-demux.
To integrate the methods, we first used sample identity assigned from the hashtag oligonucleotides. If the nuclei were confidently assigned a sample, it was compared to the genotype-based sample assignment. Those that did not match the same sample were filtered out. If the nuclei were assigned as a doublet or to none of the samples, the nuclei were assigned to a sample based on the genotype-based approach. 84,700 nuclei with confident sample assignment were used in analysis.
Downstream analyses for single nuclei-RNA seq were done with the Seurat package v4 in R142,144–146. Cell types for the nuclei were assigned by expression levels for classical markers for brain cell types such as GFAP and AQP4 for astrocytes and MOG and PLP1 for oligodendrocytes. The cell types were then validated by using the Variance-adjusted Mahalnobis method, a gene set enrichment testing developed to be specific to singe cell RNA-seq data, with gene sets derived from specific brain cell types153. Further details for single cell RNA-seq pre-processing and analysis are detailed in ref. 110.
Bulk RNA-sequencing
Unused nuclei from our single nuclei RNA-seq experiment were used for bulk RNA-sequencing. RNA was isolated following the RNeasy Plus kit (Qiagen, Hilden, Germany). Libraries for bulk RNA-seq were prepared following the Takara Pico v3 low-input protocol (Takara Bio, Kusatsu, Japan).
Quality control for raw single-end RNA-seq data was checked using FastQC v0.11.8154. Reads were trimmed of polyA sequences and low-quality bases using Cutadapt v2.4155. Reads were aligned to the human pre-mRNA genome GRCh38 with STAR v2.7.7a149. Quality control of aligned reads was confirmed with CollectRNASeqMetrics in the Picard software v2.18.29156. Duplicate reads were identified with MarkDuplicates function in the Picard software156. One sample with an exceedingly high duplicate read percentage was removed from downstream analyses. Counts per gene were estimated using the htseq-count function in the HTseq software v0.11.2157.
DNA methylation and hydroxymethylation
In total, DNA from 32 paired pediatric brain tumor and 2 non-tumor brain samples was treated with tandem bisulfite and oxidative bisulfite conversion followed by hybridization to Infinium HumanMethylationEPIC BeadChips to measure DNA methylation (5mC) and hydroxymethylation (5hmC). Raw BeadArray data were preprocessed using the SeSAMe pipeline (v1) from Bioconductor, including data normalization and quality control158. Cross-reactive probes, SNP-related probes, sex chromosome probes, non-CpG probes, and low-quality probes (pOOBHA > 0.05) were masked in the analysis159. The oxBS.MLE function was used to infer 5mC and 5hmC levels160.
Tumor purity estimates
Tumor purity for the tissue samples with DNA cytosine modifications was estimated using the getPurity function with the non-tumor pediatric tumor tissue as our non-tumor reference and the low-grade glioma option as our cancer type in the InfiniumPurify package v1.3.1 in R161.
Statistical analyses
Distribution of tumor tissues 5mC and 5hmC were compared to distribution of non-tumor 5mC and 5hmC, respectively, using a Kolmogorov-Smirnov tests. Distributions were considered to be statistically significant at p < 0.05 threshold. Outliers for MDI were determined using the Grubb’s test for outliers at statistical significance threshold of p < 0.05. Linear regression models were used to determine association between 5hmC and 5mC Methylation Dysregulation Index values with genomic context and tumor type. Linear regression models were run with the lm function in the stats package in R.
Epigenome-wide association studies
Linear regression models, adjusting for sex, age at diagnosis, and tumor purity in all models, were used to identify differentially methylated and hydroxymethylated CpGs associated with each tumor type compared to the non-tumor tissue. Due to sample size, tumor location was not adjusted for in the linear regression models. Multiple linear regression models, with adjustments for different cell type proportions identified from the single nuclei RNA-seq data, were added to the models. Linear regression models were fit by using lmFit and eBayes functions in the limma (v3.54.2) package in R162. CpGs were considered differentially methylated or hydroxymethylated under the q-value threshold of 0.05.
Cell type-specific differential hydroxymethylation and methylation for each tumor type were identified using CellDMC103. CellDMC is a statistical model that identifies both differentially methylated CpGs and which cell type drives the differential methylation by incorporating cell type proportions as interaction terms in the linear regression model in the epigenome wide association study103. CellDMC was conducted within the EpiDISH (v2.14.1) R package103. Proportions of cell types of interest (neurons and progenitor-like cell types) were pulled from the single nuclei RNA-seq dataset. To limit overfitting the model in our relatively smaller sample size, we aggregated the progenitor-like cell types into a single cell type category. The progenitor-like cell types included NSC, RGC, OPC, and UBC. UBCs were included due to the high levels of stemness score in the cell types identified previously. Separate models to compare each tumor type to the non-tumor tissue were run with the same cell types (progenitor-like and neuronal-like cell types) included in each model.
Differential gene expression testing
Negative binomial regression models were used to identify the differential expressed genes in each tumor type compared to non-tumor tissue. One model was fit adjusting for age at diagnosis and sex. The other model was fit adjusting for age at diagnosis, sex, and the proportions for cell types of interest (NEU, NSC, RGC, OPC, UBC). Negative binomial models were fit by using DESeq function in the DESeq2 package v1.36.0 in R163. Genes were considered as differentially expressed under the adjusted p-value threshold of 0.05.
Pathways enrichment testing
Reactome pathways enrichment associated with differentially expressed genes in each tumor type were identified using the enrichPathway function in the ReactomePA package v1.40.0 in R164.
Genomic context enrichment test
Enrichment tests for genomic context for differentially hydroxymethylated CpGs were conducted using the Mantel-Haenszel (MH) test. The MH test was adjusted for the type of probe (Type I or Type II) used for the CpG in the Illumina Methylation EPIC array.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Supplementary information
Description of Additional Supplementary Files
Source data
Acknowledgements
This work was supported by a Prouty Pilot award from the Dartmouth Cancer Center and a Single-cell Pediatric Cancer Atlas (ScPCA) grant from the Alex’s Lemonade Stand Foundation. M.K.L. was supported by the Burroughs-Wellcome Fund: Big Data in the Life Sciences at Dartmouth. N.A. was supported by the S.M. Tenney Fellowship at Dartmouth. This work was also supported by National Institutes of Health (R01CA216265, R01CA253976, and P20GM104416 – 6369) to B.C.C. and P20 GM104416-09/8299 and CDMRP/Department of Defense (W81XWH-20-1-0778) to L.A.S. Single nuclei RNA-seq experiments were conducted in the Genomics and Molecular Biology Shared Resource (GMBSR) at Dartmouth, which is supported by NCI Cancer Center Support Grant 5P30CA023108 and NIH S10 (1S10OD030242) awards. Single-nuclei RNA experiments were also supported through the Dartmouth Center for Quantitative in collaboration with the GMBSR with support from NIGMS (P20GM130454) and NIH S10 (S10OD025235) awards.
Author contributions
M.K.L., N.A., and B.C.C. designed the study. N.A., G.J.Z., and L.N. identified subject populations and collected tissue samples. M.K.L., N.A., and L.P. performed experiments to collect cytosine modification and gene expression data. M.K.L., N.A., and F.W.K. performed experiments to collect single nuclei-RNA seq data. M.K.L. and Z.Z. processed data for downstream analyses. M.K.L. performed statistical analyses under the supervision of L.A.S. and B.C.C. B.C.C. supervised the project. All authors reviewed the manuscript.
Peer review
Peer review information
Nature Communications thanks Xiao-Nan Li, and the other anonymous reviewer for their contribution to the peer review of this work. A peer review file is available.
Data availability
The raw single nuclei-RNA seq data and the processed data for single nuclei-RNA seq generated in this study are available in the Gene Expression Omnibus under accession code GSE211362. The raw hydroxymethylation/methylation data generated in this study have been deposited in the Gene Expression Omnibus under accession code GSE152561. The raw bulk RNA-seq data generated in this study have been deposited in the Gene Expression Omnibus under accession code GSE241396. Source data are provided as a Source Data file. All larger size source data files are available at https://figshare.com/projects/Associations_in_cell_type-specific_hydroxymethylation_and_transcriptional_alterations_of_pediatric_central_nervous_system_tumors/193781. GRCH38 reference data are available in the National Library of Medicine database (https://www.ncbi.nlm.nih.gov/datasets/genome/GCF_000001405.26/). Source data are provided with this paper.
Code availability
Code used for analysis is available at https://github.com/sarahmklee/IntegrativePCNS.
Competing interests
B.C.C. is an advisor to Guardant Health which had no role in this work. All other authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Min Kyung Lee, Email: sarahminkyunglee@gmail.com.
Brock C. Christensen, Email: Brock.Christensen@dartmouth.edu
Supplementary information
The online version contains supplementary material available at 10.1038/s41467-024-47943-9.
References
- 1.Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. Ca Cancer J. Clin. 2022;72:7–33. doi: 10.3322/caac.21708. [DOI] [PubMed] [Google Scholar]
- 2.Smith MA, Altekruse SF, Adamson PC, Reaman GH, Seibel NL. Declining childhood and adolescent cancer mortality. Cancer. 2014;120:2497–2506. doi: 10.1002/cncr.28748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhakta N, et al. The cumulative burden of surviving childhood cancer: an initial report from the St Jude Lifetime Cohort Study (SJLIFE) Lancet. 2017;390:2569–2582. doi: 10.1016/S0140-6736(17)31610-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Palmer SL, et al. Patterns of intellectual development among survivors of pediatric medulloblastoma: a longitudinal analysis. J. Clin. Oncol. 2001;19:2302–2308. doi: 10.1200/JCO.2001.19.8.2302. [DOI] [PubMed] [Google Scholar]
- 5.Robinson KE, et al. A quantitative meta‐analysis of neurocognitive sequelae in survivors of pediatric brain tumors. Pediatr. Blood Cancer. 2010;55:525–531. doi: 10.1002/pbc.22568. [DOI] [PubMed] [Google Scholar]
- 6.Ellenberg L, et al. Neurocognitive status in long-term survivors of childhood CNS malignancies: a report from the childhood cancer survivor study. Neuropsychology. 2009;23:705–717. doi: 10.1037/a0016674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Merchant TE, et al. Critical combinations of radiation dose and volume predict intelligence quotient and academic achievement scores after craniospinal irradiation in children with medulloblastoma. Int. J. Radiat. Oncol. Biol. Phys. 2014;90:554–561. doi: 10.1016/j.ijrobp.2014.06.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pinto MD, Conklin HM, Li C, Merchant TE. Learning and memory following conformal radiation therapy for pediatric craniopharyngioma and low-grade glioma. Int. J. Radiat. Oncol. Biol. Phys. 2012;84:e363–e369. doi: 10.1016/j.ijrobp.2012.03.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ris MD, et al. Intellectual and academic outcome following two chemotherapy regimens and radiotherapy for average‐risk medulloblastoma: COG A9961. Pediatr. Blood Cancer. 2013;60:1350–1357. doi: 10.1002/pbc.24496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Taylor MD, et al. Molecular subgroups of medulloblastoma: the current consensus. Acta Neuropathol. 2012;123:465–472. doi: 10.1007/s00401-011-0922-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Northcott PA, et al. The whole-genome landscape of medulloblastoma subtypes. Nature. 2017;547:311–317. doi: 10.1038/nature22973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Juraschka K, Taylor MD. Medulloblastoma in the age of molecular subgroups: a review: JNSPG 75th Anniversary Invited Review Article. J. Neurosurg. Pediatr. 2019;24:353–363. doi: 10.3171/2019.5.PEDS18381. [DOI] [PubMed] [Google Scholar]
- 13.Pajtler KW, et al. Molecular classification of ependymal tumors across all CNS compartments, histopathological grades, and age groups. Cancer Cell. 2015;27:728–743. doi: 10.1016/j.ccell.2015.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Witt H, et al. DNA methylation-based classification of ependymomas in adulthood: implications for diagnosis and treatment. Neuro-Oncol. 2018;20:1616–1624. doi: 10.1093/neuonc/noy118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jessa S, et al. Stalled developmental programs at the root of pediatric brain tumors. Nat. Genet. 2019;51:1702–1713. doi: 10.1038/s41588-019-0531-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang L, et al. Single-cell transcriptomics in medulloblastoma reveals tumor-initiating progenitors and oncogenic cascades during tumorigenesis and relapse. Cancer Cell. 2019;36:302–318.e7. doi: 10.1016/j.ccell.2019.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gojo J, et al. Single-cell RNA-seq reveals cellular hierarchies and impaired developmental trajectories in pediatric ependymoma. Cancer Cell. 2020;38:44–59.e9. doi: 10.1016/j.ccell.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gillen AE, et al. Single-cell RNA sequencing of childhood ependymoma reveals neoplastic cell subpopulations that impact molecular classification and etiology. Cell Rep. 2020;32:108023. doi: 10.1016/j.celrep.2020.108023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hovestadt V, et al. Resolving medulloblastoma cellular architecture by single-cell genomics. Nature. 2019;572:74–79. doi: 10.1038/s41586-019-1434-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Filbin MG, et al. Developmental and oncogenic programs in H3K27M gliomas dissected by single-cell RNA-seq. Science. 2018;360:331–335. doi: 10.1126/science.aao4750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vladoiu MC, et al. Childhood cerebellar tumours mirror conserved fetal transcriptional programs. Nature. 2019;572:67–73. doi: 10.1038/s41586-019-1158-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reitman ZJ, et al. Mitogenic and progenitor gene programmes in single pilocytic astrocytoma cells. Nat. Commun. 2019;10:3731. doi: 10.1038/s41467-019-11493-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Louis DN, et al. The 2021 WHO classification of tumors of the central nervous system: a summary. Neuro-Oncol. 2021;23:1231–1251. doi: 10.1093/neuonc/noab106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Capper D, et al. DNA methylation-based classification of central nervous system tumours. Nature. 2018;555:469–474. doi: 10.1038/nature26000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Booth MJ, et al. Oxidative bisulfite sequencing of 5-methylcytosine and 5-hydroxymethylcytosine. Nat. Protoc. 2013;8:1841–1851. doi: 10.1038/nprot.2013.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Azizgolshani N, et al. DNA 5-hydroxymethylcytosine in pediatric central nervous system tumors may impact tumor classification and is a positive prognostic marker. Clin. Epigenetics. 2021;13:176. doi: 10.1186/s13148-021-01156-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sinsheimer RL. The action of pancreatic desoxyribonuclease: I. Isolation of mono- and dinucleotides. J. Biol. Chem. 1953;208:445–459. doi: 10.1016/S0021-9258(18)65663-7. [DOI] [PubMed] [Google Scholar]
- 28.Gold M, Hurwitz J, Anders M. The enzymatic methylation of RNA and DNA, II. on the species specificity. Proc. Natl Acad. Sci. 1963;50:164–169. doi: 10.1073/pnas.50.1.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Billen D, Hewitt R. Influence of starvation for methionine and other amino acids on subsequent bacterial deoxyribonucleic acid replication. J. Bacteriol. 1966;92:609–617. doi: 10.1128/jb.92.3.609-617.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Billen D. Methylation of the bacterial chromosome: an event at the “replication point”? J. Mol. Biol. 1968;31:477–486. doi: 10.1016/0022-2836(68)90422-1. [DOI] [PubMed] [Google Scholar]
- 31.Lark C. Studies on the in vivo methylation of DNA in Escherichia coli 15T−. J. Mol. Biol. 1968;31:389–399. doi: 10.1016/0022-2836(68)90416-6. [DOI] [PubMed] [Google Scholar]
- 32.Srinivasan PR, Borek E. Enzymatic alteration. Science. 1964;145:548–553. doi: 10.1126/science.145.3632.548. [DOI] [PubMed] [Google Scholar]
- 33.Jones PA. Functions of DNA methylation: islands, start sites, gene bodies and beyond. Nat. Rev. Genet. 2012;13:484–492. doi: 10.1038/nrg3230. [DOI] [PubMed] [Google Scholar]
- 34.Petryk N, Bultmann S, Bartke T, Defossez P-A. Staying true to yourself: mechanisms of DNA methylation maintenance in mammals. Nucleic Acids Res. 2020;49:gkaa1154. doi: 10.1093/nar/gkaa1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ambrosi C, Manzo M, Baubec T. Dynamics and context-dependent roles of DNA methylation. J. Mol. Biol. 2017;429:1459–1475. doi: 10.1016/j.jmb.2017.02.008. [DOI] [PubMed] [Google Scholar]
- 36.Rose NR, Klose RJ. Understanding the relationship between DNA methylation and histone lysine methylation. Biochim. Biophys. Acta. 2014;1839:1362–1372. doi: 10.1016/j.bbagrm.2014.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zilberman D, Coleman-Derr D, Ballinger T, Henikoff S. Histone H2A.Z and DNA methylation are mutually antagonistic chromatin marks. Nature. 2008;456:125–129. doi: 10.1038/nature07324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Deniz Ö, Frost JM, Branco MR. Regulation of transposable elements by DNA modifications. Nat. Rev. Genet. 2019;20:417–431. doi: 10.1038/s41576-019-0106-6. [DOI] [PubMed] [Google Scholar]
- 39.Hansen KD, et al. Increased methylation variation in epigenetic domains across cancer types. Nat. Genet. 2011;43:768–775. doi: 10.1038/ng.865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Berman BP, et al. Regions of focal DNA hypermethylation and long-range hypomethylation in colorectal cancer coincide with nuclear lamina–associated domains. Nat. Genet. 2012;44:40–46. doi: 10.1038/ng.969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Moarii M, Boeva V, Vert J-P, Reyal F. Changes in correlation between promoter methylation and gene expression in cancer. BMC Genom. 2015;16:873. doi: 10.1186/s12864-015-1994-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ng JM-K, Yu J. Promoter hypermethylation of tumour suppressor genes as potential biomarkers in colorectal cancer. Int. J. Mol. Sci. 2015;16:2472–2496. doi: 10.3390/ijms16022472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liyanage C, et al. Promoter hypermethylation of tumor-suppressor genes p16INK4a, RASSF1A, TIMP3, and PCQAP/MED15 in salivary DNA as a quadruple biomarker panel for early detection of oral and oropharyngeal cancers. Biomol. 2019;9:148. doi: 10.3390/biom9040148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Baylin SB, Jones PA. Epigenetic determinants of cancer. Csh Perspect. Biol. 2016;8:a019505. doi: 10.1101/cshperspect.a019505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pfeifer GP. p53 mutational spectra and the role of methylated CpG sequences. Mutat. Res. 2000;450:155–166. doi: 10.1016/S0027-5107(00)00022-1. [DOI] [PubMed] [Google Scholar]
- 46.You Y-H, Li C, Pfeifer GP. Involvement of 5-methylcytosine in sunlight-induced mutagenesis. J. Mol. Biol. 1999;293:493–503. doi: 10.1006/jmbi.1999.3174. [DOI] [PubMed] [Google Scholar]
- 47.Rideout WM, Coetzee GA, Olumi AF, Jones PA. 5-methylcytosine as an endogenous mutagen in the human LDL receptor and p53 genes. Science. 1990;249:1288–1290. doi: 10.1126/science.1697983. [DOI] [PubMed] [Google Scholar]
- 48.Ito S, et al. Role of Tet proteins in 5mC to 5hmC conversion, ES-cell self-renewal and inner cell mass specification. Nature. 2010;466:1129–1133. doi: 10.1038/nature09303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ito S, et al. Tet proteins can convert 5-methylcytosine to 5-formylcytosine and 5-carboxylcytosine. Science. 2011;333:1300–1303. doi: 10.1126/science.1210597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tahiliani M, et al. Conversion of 5-methylcytosine to 5-hydroxymethylcytosine in mammalian DNA by MLL partner TET1. Science. 2009;324:930–935. doi: 10.1126/science.1170116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.He Y-F, et al. Tet-mediated formation of 5-carboxylcytosine and its excision by TDG in mammalian DNA. Science. 2011;333:1303–1307. doi: 10.1126/science.1210944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shi D-Q, Ali I, Tang J, Yang W-C. New insights into 5hmC DNA modification: generation, distribution and function. Front. Genet. 2017;8:100. doi: 10.3389/fgene.2017.00100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nestor CE, et al. Tissue type is a major modifier of the 5-hydroxymethylcytosine content of human genes. Genome Res. 2012;22:467–477. doi: 10.1101/gr.126417.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Thomson JP, Meehan RR. The application of genome-wide 5-hydroxymethylcytosine studies in cancer research. Epigenomics. 2017;9:77–91. doi: 10.2217/epi-2016-0122. [DOI] [PubMed] [Google Scholar]
- 55.Song C-X, Yi C, He C. Mapping recently identified nucleotide variants in the genome and transcriptome. Nat. Biotechnol. 2012;30:1107–1116. doi: 10.1038/nbt.2398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.He B, et al. Tissue-specific 5-hydroxymethylcytosine landscape of the human genome. Nat. Commun. 2021;12:4249. doi: 10.1038/s41467-021-24425-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kriaucionis S, Heintz N. The nuclear DNA base 5-hydroxymethylcytosine is present in Purkinje neurons and the brain. Science. 2009;324:929–930. doi: 10.1126/science.1169786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kinde B, Gabel HW, Gilbert CS, Griffith EC, Greenberg ME. Reading the unique DNA methylation landscape of the brain: non-CpG methylation, hydroxymethylation, and MeCP2. Proc. Natl Acad. Sci. 2015;112:6800–6806. doi: 10.1073/pnas.1411269112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Thomson JP, et al. Comparative analysis of affinity-based 5-hydroxymethylation enrichment techniques. Nucleic Acids Res. 2013;41:e206–e206. doi: 10.1093/nar/gkt1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Spada F, et al. Active turnover of genomic methylcytosine in pluripotent cells. Nat. Chem. Biol. 2020;16:1411–1419. doi: 10.1038/s41589-020-0621-y. [DOI] [PubMed] [Google Scholar]
- 61.Stoyanova E, Riad M, Rao A, Heintz N. 5-Hydroxymethylcytosine-mediated active demethylation is required for mammalian neuronal differentiation and function. Elife. 2021;10:e66973. doi: 10.7554/eLife.66973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jin S-G, et al. 5-Hydroxymethylcytosine is strongly depleted in human cancers but its levels do not correlate with IDH1 mutations. Cancer Res. 2011;71:7360–7365. doi: 10.1158/0008-5472.CAN-11-2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Liu C, et al. Decrease of 5-hydroxymethylcytosine is associated with progression of hepatocellular carcinoma through downregulation of TET1. PloS One. 2013;8:e62828. doi: 10.1371/journal.pone.0062828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kudo Y, et al. Loss of 5‐hydroxymethylcytosine is accompanied with malignant cellular transformation. Cancer Sci. 2012;103:670–676. doi: 10.1111/j.1349-7006.2012.02213.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lian CG, et al. Loss of 5-hydroxymethylcytosine is an epigenetic hallmark of melanoma. Cell. 2012;150:1135–1146. doi: 10.1016/j.cell.2012.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chen K, et al. Loss of 5-hydroxymethylcytosine is linked to gene body hypermethylation in kidney cancer. Cell Res. 2016;26:103–118. doi: 10.1038/cr.2015.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Park J-L, et al. Decrease of 5hmC in gastric cancers is associated with TET1 silencing due to with DNA methylation and bivalent histone marks at TET1 CpG island 3′-shore. Oncotarget. 2015;6:37647–37662. doi: 10.18632/oncotarget.6069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Orr BA, Haffner MC, Nelson WG, Yegnasubramanian S, Eberhart CG. Decreased 5-hydroxymethylcytosine is associated with neural progenitor phenotype in normal brain and shorter survival in malignant glioma. Plos One. 2012;7:e41036. doi: 10.1371/journal.pone.0041036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ficz G, Gribben JG. Loss of 5-hydroxymethylcytosine in cancer: cause or consequence? Genomics. 2014;104:352–357. doi: 10.1016/j.ygeno.2014.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Johnson KC, et al. 5-Hydroxymethylcytosine localizes to enhancer elements and is associated with survival in glioblastoma patients. Nat. Commun. 2016;7:13177. doi: 10.1038/ncomms13177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Figueroa ME, et al. Leukemic IDH1 and IDH2 mutations result in a hypermethylation phenotype, disrupt TET2 function, and impair hematopoietic differentiation. Cancer Cell. 2010;18:553–567. doi: 10.1016/j.ccr.2010.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lu C, et al. IDH mutation impairs histone demethylation and results in a block to cell differentiation. Nature. 2012;483:474–478. doi: 10.1038/nature10860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rampal R, et al. DNA hydroxymethylation profiling reveals that WT1 mutations result in loss of TET2 function in acute myeloid leukemia. Cell Rep. 2014;9:1841–1855. doi: 10.1016/j.celrep.2014.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Duncan CG, et al. A heterozygous IDH1R132H/WT mutation induces genome-wide alterations in DNA methylation. Genome Res. 2012;22:2339–2355. doi: 10.1101/gr.132738.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Qazi MA, Bakhshinyan D, Singh SK. Deciphering brain tumor heterogeneity, one cell at a time. Nat. Med. 2019;25:1474–1476. doi: 10.1038/s41591-019-0605-1. [DOI] [PubMed] [Google Scholar]
- 76.Sottoriva A, et al. Intratumor heterogeneity in human glioblastoma reflects cancer evolutionary dynamics. Proc. Natl Acad. Sci. 2013;110:4009–4014. doi: 10.1073/pnas.1219747110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hoffman, M. et al. Intratumoral genetic and functional heterogeneity in pediatric glioblastoma. Cancer Res.79, 2111–2123 (2019). [DOI] [PMC free article] [PubMed]
- 78.Kim EL, et al. Intratumoral heterogeneity and longitudinal changes in gene expression predict differential drug sensitivity in newly diagnosed and recurrent glioblastoma. Cancers. 2020;12:520. doi: 10.3390/cancers12020520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Qazi MA, et al. Intratumoral heterogeneity: pathways to treatment resistance and relapse in human glioblastoma. Ann. Oncol. 2017;28:1448–1456. doi: 10.1093/annonc/mdx169. [DOI] [PubMed] [Google Scholar]
- 80.Gularyan SK, et al. Investigation of Inter- and intratumoral heterogeneity of glioblastoma using TOF-SIMS. Mol. Cell Proteom. 2020;19:960–970. doi: 10.1074/mcp.RA120.001986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Patel AP, et al. Single-cell RNA-seq highlights intratumoral heterogeneity in primary glioblastoma. Science. 2014;344:1396–1401. doi: 10.1126/science.1254257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Larsson I, et al. Modeling glioblastoma heterogeneity as a dynamic network of cell states. Mol. Syst. Biol. 2021;17:e10105. doi: 10.15252/msb.202010105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Berens ME, et al. Multiscale, multimodal analysis of tumor heterogeneity in IDH1 mutant vs wild-type diffuse gliomas. PloS One. 2019;14:e0219724. doi: 10.1371/journal.pone.0219724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lopes MB, Vinga S. Tracking intratumoral heterogeneity in glioblastoma via regularized classification of single-cell RNA-Seq data. BMC Bioinform. 2020;21:59. doi: 10.1186/s12859-020-3390-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lam KHB, Valkanas K, Djuric U, Diamandis P. Unifying models of glioblastoma’s intra-tumoral heterogeneity. Neuro-Oncol. Adv. 2020;2:vdaa096. doi: 10.1093/noajnl/vdaa096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Meissner A, et al. Genome-scale DNA methylation maps of pluripotent and differentiated cells. Nature. 2008;454:766–770. doi: 10.1038/nature07107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sproul D, et al. Tissue of origin determines cancer-associated CpG island promoter hypermethylation patterns. Genome Biol. 2012;13:R84. doi: 10.1186/gb-2012-13-10-r84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zhou J, et al. Tissue-specific DNA methylation is conserved across human, mouse, and rat, and driven by primary sequence conservation. BMC Genom. 2017;18:724. doi: 10.1186/s12864-017-4115-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zhang B, et al. Functional DNA methylation differences between tissues, cell types, and across individuals discovered using the M&M algorithm. Genome Res. 2013;23:1522–1540. doi: 10.1101/gr.156539.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Moss J, et al. Comprehensive human cell-type methylation atlas reveals origins of circulating cell-free DNA in health and disease. Nat. Commun. 2018;9:5068. doi: 10.1038/s41467-018-07466-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Rahmani E, et al. Cell-type-specific resolution epigenetics without the need for cell sorting or single-cell biology. Nat. Commun. 2019;10:3417. doi: 10.1038/s41467-019-11052-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kim S, et al. Enlarged leukocyte referent libraries can explain additional variance in blood-based epigenome-wide association studies. Epigenomics. 2016;8:1185–1192. doi: 10.2217/epi-2016-0037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Jaffe AE, Irizarry RA. Accounting for cellular heterogeneity is critical in epigenome-wide association studies. Genome Biol. 2014;15:R31. doi: 10.1186/gb-2014-15-2-r31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Christensen BC, et al. Aging and environmental exposures alter tissue-specific DNA methylation dependent upon CpG island context. Plos Genet. 2009;5:e1000602. doi: 10.1371/journal.pgen.1000602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.You C, et al. A cell-type deconvolution meta-analysis of whole blood EWAS reveals lineage-specific smoking-associated DNA methylation changes. Nat. Commun. 2020;11:4779. doi: 10.1038/s41467-020-18618-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Reinius LE, et al. Differential DNA methylation in purified human blood cells: implications for cell lineage and studies on disease susceptibility. PloS One. 2012;7:e41361. doi: 10.1371/journal.pone.0041361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Angermueller C, et al. Parallel single-cell sequencing links transcriptional and epigenetic heterogeneity. Nat. Methods. 2016;13:229–232. doi: 10.1038/nmeth.3728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Clark SJ, Lee HJ, Smallwood SA, Kelsey G, Reik W. Single-cell epigenomics: powerful new methods for understanding gene regulation and cell identity. Genome Biol. 2016;17:72. doi: 10.1186/s13059-016-0944-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Schwartzman O, Tanay A. Single-cell epigenomics: techniques and emerging applications. Nat. Rev. Genet. 2015;16:716–726. doi: 10.1038/nrg3980. [DOI] [PubMed] [Google Scholar]
- 100.Smallwood SA, et al. Single-cell genome-wide bisulfite sequencing for assessing epigenetic heterogeneity. Nat. Methods. 2014;11:817–820. doi: 10.1038/nmeth.3035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Salas LA, et al. An optimized library for reference-based deconvolution of whole-blood biospecimens assayed using the Illumina HumanMethylationEPIC BeadArray. Genome Biol. 2018;19:64. doi: 10.1186/s13059-018-1448-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Salas LA, et al. Enhanced cell deconvolution of peripheral blood using DNA methylation for high-resolution immune profiling. Nat. Commun. 2022;13:761. doi: 10.1038/s41467-021-27864-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Zheng SC, Breeze CE, Beck S, Teschendorff AE. Identification of differentially methylated cell types in epigenome-wide association studies. Nat. Methods. 2018;15:1059–1066. doi: 10.1038/s41592-018-0213-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Teschendorff AE, Zheng SC. Cell-type deconvolution in epigenome-wide association studies: a review and recommendations. Epigenomics. 2017;9:757–768. doi: 10.2217/epi-2016-0153. [DOI] [PubMed] [Google Scholar]
- 105.Houseman EA, et al. DNA methylation arrays as surrogate measures of cell mixture distribution. BMC Bioinform. 2012;13:86. doi: 10.1186/1471-2105-13-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Rahmani E, et al. BayesCCE: a Bayesian framework for estimating cell-type composition from DNA methylation without the need for methylation reference. Genome Biol. 2018;19:141. doi: 10.1186/s13059-018-1513-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Rahmani E, et al. Sparse PCA corrects for cell type heterogeneity in epigenome-wide association studies. Nat. Methods. 2016;13:443–445. doi: 10.1038/nmeth.3809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Waite LL, et al. Estimation of cell-type composition including T and B cell subtypes for whole blood methylation microarray data. Front. Genet. 2016;7:23. doi: 10.3389/fgene.2016.00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Zhang Z, et al. HiTIMED: hierarchical tumor immune microenvironment epigenetic deconvolution for accurate cell type resolution in the tumor microenvironment using tumor-type-specific DNA methylation data. J. Transl. Med. 2022;20:516. doi: 10.1186/s12967-022-03736-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Lee, M. K. et al. Identifying tumor type and cell type-specific gene expression alterations in pediatric central nervous system tumors. Nat. Commun.10.1038/s41467-024-47712-8 (2024). [DOI] [PMC free article] [PubMed]
- 111.O’Sullivan DE, Johnson KC, Skinner L, Koestler DC, Christensen BC. Epigenetic and genetic burden measures are associated with tumor characteristics in invasive breast carcinoma. Epigenetics. 2016;11:344–353. doi: 10.1080/15592294.2016.1168673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Taylor MD, et al. Radial glia cells are candidate stem cells of ependymoma. Cancer Cell. 2005;8:323–335. doi: 10.1016/j.ccr.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 113.Gruhn B, et al. The expression of histone deacetylase 4 is associated with prednisone poor-response in childhood acute lymphoblastic leukemia. Leuk. Res. 2013;37:1200–1207. doi: 10.1016/j.leukres.2013.07.016. [DOI] [PubMed] [Google Scholar]
- 114.Kang Z-H, et al. Histone deacetylase HDAC4 promotes gastric cancer SGC-7901 cells progression via p21 repression. PloS One. 2014;9:e98894. doi: 10.1371/journal.pone.0098894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kaowinn S, Kaewpiboon C, Koh SS, Krämer OH, Chung Y-H. STAT1-HDAC4 signaling induces epithelial-mesenchymal transition and sphere formation of cancer cells overexpressing the oncogene, CUG2. Oncol. Rep. 2018;40:2619–2627. doi: 10.3892/or.2018.6701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Mottet D, et al. HDAC4 represses p21WAF1/Cip1 expression in human cancer cells through a Sp1-dependent, p53-independent mechanism. Oncogene. 2009;28:243–256. doi: 10.1038/onc.2008.371. [DOI] [PubMed] [Google Scholar]
- 117.Cheng W, et al. HDAC4, a prognostic and chromosomal instability marker, refines the predictive value of MGMT promoter methylation. J. Neuro-oncol. 2015;122:303–312. doi: 10.1007/s11060-014-1709-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Cheng C, et al. HDAC4 promotes nasopharyngeal carcinoma progression and serves as a therapeutic target. Cell Death Dis. 2021;12:137. doi: 10.1038/s41419-021-03417-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Cai J-Y, et al. Histone deacetylase HDAC4 promotes the proliferation and invasion of glioma cells. Int. J. Oncol. 2018;53:2758–2768. doi: 10.3892/ijo.2018.4564. [DOI] [PubMed] [Google Scholar]
- 120.Wilson AJ, et al. HDAC4 promotes growth of colon cancer cells via repression of p21. Mol. Biol. Cell. 2008;19:4062–4075. doi: 10.1091/mbc.e08-02-0139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zeng L-S, et al. Overexpressed HDAC4 is associated with poor survival and promotes tumor progression in esophageal carcinoma. Aging. 2016;8:1236–1248. doi: 10.18632/aging.100980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Creighton CJ, et al. Insulin-like growth factor-I activates gene transcription programs strongly associated with poor breast cancer prognosis. J. Clin. Oncol. 2008;26:4078–4085. doi: 10.1200/JCO.2007.13.4429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Farabaugh SM, Boone DN, Lee AV. Role of IGF1R in breast cancer subtypes, stemness, and lineage differentiation. Front. Endocrinol. 2015;6:59. doi: 10.3389/fendo.2015.00059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Maris C, et al. IGF-IR: a new prognostic biomarker for human glioblastoma. Br. J. Cancer. 2015;113:729–737. doi: 10.1038/bjc.2015.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Doepfner KT, Spertini O, Arcaro A. Autocrine insulin-like growth factor-I signaling promotes growth and survival of human acute myeloid leukemia cells via the phosphoinositide 3-kinase/Akt pathway. Leukemia. 2007;21:1921–1930. doi: 10.1038/sj.leu.2404813. [DOI] [PubMed] [Google Scholar]
- 126.Chng WJ, Gualberto A, Fonseca R. IGF-1R is overexpressed in poor-prognostic subtypes of multiple myeloma. Leukemia. 2006;20:174–176. doi: 10.1038/sj.leu.2403997. [DOI] [PubMed] [Google Scholar]
- 127.Svalina MN, et al. IGF1R as a key target in high risk, metastatic medulloblastoma. Sci. Rep. 2016;6:27012. doi: 10.1038/srep27012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Tirrò E, et al. Prognostic and therapeutic roles of the insulin growth factor system in glioblastoma. Front. Oncol. 2021;10:612385. doi: 10.3389/fonc.2020.612385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Vewinger N, et al. IGF1R Is a potential new therapeutic target for HGNET-BCOR brain tumor patients. Int J. Mol. Sci. 2019;20:3027. doi: 10.3390/ijms20123027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Zhang Y, et al. Pan-cancer analysis of IGF-1 and IGF-1R as potential prognostic biomarkers and immunotherapy targets. Front. Oncol. 2021;11:755341. doi: 10.3389/fonc.2021.755341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Wang, P., Mak, V. C. Y. & Cheung, L. W. T. Drugging IGF-1R in cancer: new insights and emerging opportunities. Genes Dis.10, 199–211 (2022). [DOI] [PMC free article] [PubMed]
- 132.Hua H, Kong Q, Yin J, Zhang J, Jiang Y. Insulin-like growth factor receptor signaling in tumorigenesis and drug resistance: a challenge for cancer therapy. J. Hematol. Oncol. 2020;13:64. doi: 10.1186/s13045-020-00904-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Gröbner SN, et al. The landscape of genomic alterations across childhood cancers. Nature. 2018;555:321–327. doi: 10.1038/nature25480. [DOI] [PubMed] [Google Scholar]
- 134.Hanahan D. Hallmarks of cancer: new dimensions. Cancer Discov. 2022;12:31–46. doi: 10.1158/2159-8290.CD-21-1059. [DOI] [PubMed] [Google Scholar]
- 135.Allis CD, Jenuwein T. The molecular hallmarks of epigenetic control. Nat. Rev. Genet. 2016;17:487–500. doi: 10.1038/nrg.2016.59. [DOI] [PubMed] [Google Scholar]
- 136.Savary C, et al. Depicting the genetic architecture of pediatric cancers through an integrative gene network approach. Sci. Rep. 2020;10:1224. doi: 10.1038/s41598-020-58179-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Huether R, et al. The landscape of somatic mutations in epigenetic regulators across 1,000 paediatric cancer genomes. Nat. Commun. 2014;5:3630. doi: 10.1038/ncomms4630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Lawlor ER, Thiele CJ. Epigenetic changes in pediatric solid tumors: promising new targets. Clin. Cancer Res. 2012;18:2768–2779. doi: 10.1158/1078-0432.CCR-11-1921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Ecker J, Witt O, Milde T. Targeting of histone deacetylases in brain tumors. CNS Oncol. 2013;2:359–376. doi: 10.2217/cns.13.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Bielen A, et al. Enhanced efficacy of IGF1R inhibition in pediatric glioblastoma by combinatorial targeting of PDGFRα/β. Mol. Cancer Ther. 2011;10:1407–1418. doi: 10.1158/1535-7163.MCT-11-0205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.McGinnis CS, et al. MULTI-seq: sample multiplexing for single-cell RNA sequencing using lipid-tagged indices. Nat. Methods. 2019;16:619–626. doi: 10.1038/s41592-019-0433-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Hao Y, et al. Integrated analysis of multimodal single-cell data. Cell. 2021;184:3573–3587.e29. doi: 10.1016/j.cell.2021.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Huang Y, McCarthy DJ, Stegle O. Vireo: Bayesian demultiplexing of pooled single-cell RNA-seq data without genotype reference. Genome Biol. 2019;20:273. doi: 10.1186/s13059-019-1865-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Satija R, Farrell JA, Gennert D, Schier AF, Regev A. Spatial reconstruction of single-cell gene expression data. Nat. Biotechnol. 2015;33:495–502. doi: 10.1038/nbt.3192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Stuart T, et al. Comprehensive integration of single-cell data. Cell. 2019;177:1888–1902.e21. doi: 10.1016/j.cell.2019.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Butler A, Hoffman P, Smibert P, Papalexi E, Satija R. Integrating single-cell transcriptomic data across different conditions, technologies, and species. Nat. Biotechnol. 2018;36:411–420. doi: 10.1038/nbt.4096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Weber LM, et al. Genetic demultiplexing of pooled single-cell RNA-sequencing samples in cancer facilitates effective experimental design. Gigascience. 2021;10:giab062. doi: 10.1093/gigascience/giab062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Tommaso PD, et al. Nextflow enables reproducible computational workflows. Nat. Biotechnol. 2017;35:316–319. doi: 10.1038/nbt.3820. [DOI] [PubMed] [Google Scholar]
- 149.Dobin A, et al. STAR: ultrafast universal RNA-seq aligner. Bioinformatics. 2013;29:15–21. doi: 10.1093/bioinformatics/bts635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Kaminow, B., Yunusov, D. & Dobin, A. STARsolo: accurate, fast and versatile mapping/quantification of single-cell and single-nucleus RNA-seq data. Biorxiv 2021.05.05.442755 10.1101/2021.05.05.442755 (2021).
- 151.Danecek P, et al. Twelve years of SAMtools and BCFtools. Gigascience. 2021;10:giab008. doi: 10.1093/gigascience/giab008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Huang X, Huang Y. Cellsnp-lite: an efficient tool for genotyping single cells. Bioinformatics. 2021;37:4569–4571. doi: 10.1093/bioinformatics/btab358. [DOI] [PubMed] [Google Scholar]
- 153.Frost HR. Variance-adjusted Mahalanobis (VAM): a fast and accurate method for cell-specific gene set scoring. Nucleic Acids Res. 2020;48:e94. doi: 10.1093/nar/gkaa582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Andrews, S. FastQC. http://www.bioinformatics.babraham.ac.uk/projects/fastqc/ (2010).
- 155.Martin M. Cutadapt removes adapter sequences from high-throughput sequencing reads. EMBnet J. 2011;17:10–12. doi: 10.14806/ej.17.1.200. [DOI] [Google Scholar]
- 156.Institute, B. Picard Toolkit. https://broadinstitute.github.io/picard/ (2019).
- 157.Anders S, Pyl PT, Huber W. HTSeq—a Python framework to work with high-throughput sequencing data. Bioinformatics. 2015;31:166–169. doi: 10.1093/bioinformatics/btu638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Zhou W, Triche TJ, Laird PW, Shen H. SeSAMe: reducing artifactual detection of DNA methylation by Infinium BeadChips in genomic deletions. Nucleic Acids Res. 2018;46:e123. doi: 10.1093/nar/gky691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Zhou W, Laird PW, Shen H. Comprehensive characterization, annotation and innovative use of Infinium DNA methylation BeadChip probes. Nucleic Acids Res. 2017;45:e22–e22. doi: 10.1093/nar/gkw967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Xu Z, Taylor JA, Leung Y-K, Ho S-M, Niu L. oxBS-MLE: an efficient method to estimate 5-methylcytosine and 5-hydroxymethylcytosine in paired bisulfite and oxidative bisulfite treated DNA. Bioinformatics. 2016;32:3667–3669. doi: 10.1093/bioinformatics/btw527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Qin Y, Feng H, Chen M, Wu H, Zheng X. InfiniumPurify: an R package for estimating and accounting for tumor purity in cancer methylation research. Genes Dis. 2018;5:43–45. doi: 10.1016/j.gendis.2018.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Ritchie ME, et al. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015;43:e47–e47. doi: 10.1093/nar/gkv007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Love MI, Huber W, Anders S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014;15:550. doi: 10.1186/s13059-014-0550-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Yu G, He Q-Y. ReactomePA: an R/Bioconductor package for Reactome pathway analysis and visualization. Mol. Biosyst. 2015;12:477–479. doi: 10.1039/C5MB00663E. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of Additional Supplementary Files
Data Availability Statement
The raw single nuclei-RNA seq data and the processed data for single nuclei-RNA seq generated in this study are available in the Gene Expression Omnibus under accession code GSE211362. The raw hydroxymethylation/methylation data generated in this study have been deposited in the Gene Expression Omnibus under accession code GSE152561. The raw bulk RNA-seq data generated in this study have been deposited in the Gene Expression Omnibus under accession code GSE241396. Source data are provided as a Source Data file. All larger size source data files are available at https://figshare.com/projects/Associations_in_cell_type-specific_hydroxymethylation_and_transcriptional_alterations_of_pediatric_central_nervous_system_tumors/193781. GRCH38 reference data are available in the National Library of Medicine database (https://www.ncbi.nlm.nih.gov/datasets/genome/GCF_000001405.26/). Source data are provided with this paper.
Code used for analysis is available at https://github.com/sarahmklee/IntegrativePCNS.