Abstract
Background
Plantar vein thrombosis (PVT) is a rare condition. Less than 50 cases have been described in the literature. Evidence from interventional and observational studies is sparse or lacking.
Objectives
To describe a consecutive cohort of patients diagnosed with PVT at a single academic institution over the past 17 years.
Methods
We searched medical charts from patients managed at the University Hospital Zurich between 2005 and 2022. PVT was detected through sonography (eg, in the presence of a noncompressible deep vein) and/or magnetic resonance (eg, a vein with a filling defect on non–contrast-enhanced or contrast-enhanced imaging). The study was approved by the local ethics commission.
Results
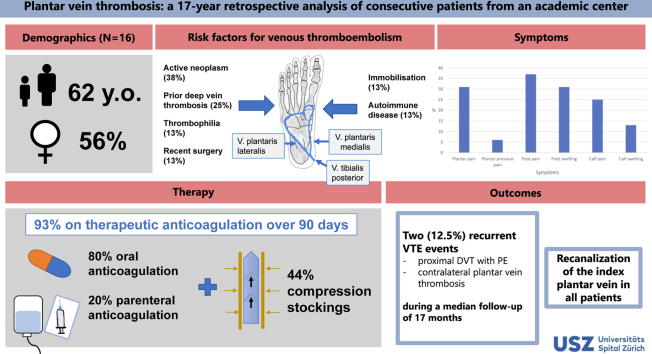
We identified 45 patients who had been assessed for PVT. After manual check of these cases, we selected 16 patients with a confirmed, objective diagnosis. Median age was 62 (25th-75th percentiles, 46-73) years, and 9 (56%) patients were women. All patients were symptomatic, usually reporting local pain in the foot (100%) and swelling (67%). The most frequent risk factors were cancer (n = 6; 38%) and prior deep vein thrombosis (n = 4; 25%). Overall, 80% of patients received oral anticoagulation and 20% received parenteral anticoagulation for a median of 90 days. Over a median follow-up of 17 months, 2 (12.5%) recurrent venous thromboembolism events were recorded following the discontinuation of anticoagulation. Index vein recanalization occurred in all 15 survivors. One patient died from cancer 2 years after PVT diagnosis.
Conclusion
We provided initial information on the clinical characteristics, treatment, and course of PVT, which partly resembles that of distal deep vein thrombosis.
Keywords: anticoagulants, venous thrombosis, plantar vein thrombosis, pulmonary embolism, doppler ultrasonography
Graphical abstract
Essentials
-
•
Plantar vein thrombosis (PVT) is a rare and often misdiagnosed clinical entity.
-
•
We analyzed consecutive patients treated for PVT at an academic center over 17 years.
-
•
Among 16 patients with confirmed PVT, cancer was the principal risk factor.
-
•
Therapeutic anticoagulation for 3 months was the most commonly utilized treatment.
1. Introduction
Plantar vein thrombosis (PVT) is a rare vascular disorder involving the plantar venous plexus, which is composed of multiple large-diameter veins that span the arch of the foot. The plantar metatarsal veins drain into the deep plantar arch, with the medial and lateral plantar veins running near the corresponding arteries in the intermuscular space. Each of the plantar veins has valves that communicate with the cutaneous venous arch draining in the saphenous veins and posterior tibial veins.
No more than 50 cases have been reported in the medical literature over the last 2 decades [1], encompassing several case reports and a single cohort study of 22 patients [2]. Challenges in accurately diagnosing PVT, leading to both overdiagnosis and underdiagnosis, may obscure its true prevalence and impact. Pain, swelling, and sensation of heaviness have been described as typical symptoms [[1], [2], [3], [4], [5]] in patients in whom other conditions, ie, plantar fasciitis, bone fractures, tendon abnormalities, and Morton neuroma, have been excluded.
Diagnostic methods have not been tested in this setting. Compression ultrasound and contrast-enhanced magnetic resonance imaging (MRI) may serve to confirm diagnosis [[1], [2], [3], [4], [5], [6]]. Due to the absence of clinical data, even from cohorts of patients with distal deep vein thrombosis (DVT), no standard treatment has been established. A common approach involves the use of anticoagulants [1,2]. Evidence for the use of compression stockings for PVT is lacking.
In light of the existing aforementioned uncertainties, we performed a longitudinal analysis of consecutive PVT cases diagnosed at a single academic institution over the past 17 years.
2. Methods
We screened all patients with suspected PVT followed at the University Hospital Zurich between 2005 and 2021. The diagnosis of PVT was confirmed in the presence of any deep vein segment distally from the ankle that was noncompressible on compression ultrasound or that presented a filling defect on MRI.
The aim of this descriptive study was to evaluate the characteristics of PVT in consecutive patients followed at an academic institution and provide information of the clinical course of the disease.
The screening strategy included an electronic search of multiple keywords (Supplementary Text) across all medical charts from the Department of Angiology and the Department of Radiology to identify patients with suspected (or confirmed) PVT with optimized sensitivity and to remove duplicates. In order to do so, all charts mentioning the plantar veins (or synonyms) were searched. Subsequently, all files were manually screened to select those with a confirmed diagnosis of PVT. We extracted information on baseline characteristics, including age, sex, ethnicity, body mass index, potential risk factors for thrombosis, symptoms, location of thrombosis, and baseline medications, as well as data on clinical course, including pulmonary embolism (PE), bleeding, death, and used therapy.
The study was approved by the cantonal ethical commission (protocol BASEC-Nr. 2021-02262) and by an internal committee deputed to hospital electronic searches. For this retrospective study, the ethical committee approved the use of deidentified clinical data from patients diagnosed before 2015 without requiring retrospective informed consent. Since 2015, patients were asked to give general informed consent for their clinical data to be used for research purposes, and only patients who consented have been included in the study.
The statistical analysis was performed following the general principles of descriptive, noninferential statistics with appropriate reporting of measures of central tendency and risks. Categorical data were reported as frequencies, while quantitative data were reported as mean and SD for normal distributed variables or median and 25th-75th percentiles (Q1-Q3) for skewed distributed variables. All the data were managed and analyzed with an SPSS spreadsheet (IBM SPSS Statistics for Windows, version 28.0).
3. Results and Discussion
Our electronic screening identified medical charts from 45 patients mentioning PVT over a 17-year period. In 29 patients, PVT was ruled out by compression ultrasound or other noninvasive imaging techniques (Figure 1). Six (13%) patients presented with unexplained foot pain, eventually attributed to musculoskeletal causes. In 5 (11%) patients, PVT was initially suspected based on clinical presentation but was subsequently excluded by imaging, with no further causes identified. In 1 (6%) patient, PVT was investigated and ultimately not confirmed as part of a preoperative workup based on the personal history. Finally, 17 (38%) patients underwent PVT screening due to prior vascular diseases such as superficial venous insufficiency, proximal DVT, Buerger disease, and venous aneurysms. These data emphasize the nonspecific nature of PVT symptoms in the presence of unilateral foot pain and swelling.
Figure 1.
Patient screening and selection flowchart. PVT, plantar vein thrombosis.
A total of 16 (36%) patients were objectively diagnosed with PVT. Median age was 62 (Q1-Q3, 46-73) years, and 9 (56%) patients were women (Table 1). Symptoms were present in all patients with a median duration of 10 days, usually consisting of foot and plantar pain or local swelling and previously referred to musculoskeletal conditions like fasciitis plantaris. Pain and swelling in the calf were also present in 4 (25%) and 2 (13%) patients, respectively (Visual Abstract).
Table 1.
Patient baseline characteristics.
| Total N = 16 | |
|---|---|
| Women,n (%) | 9 (56) |
| Age (y), median (Q1-Q3) | 62 (46-73) |
| Caucasian ethnicity,n (%) | 15 (94) |
| Active neoplasm,n (%) | 6 (38) |
| Plasma cell neoplasm | 3 (19) |
| Melanoma | 1 (6) |
| Acute myeloid leukemia | 1 (6) |
| Prostate carcinoma | 1 (6) |
| Thrombophilia, n (%) | 2 (13) |
| Factor V G1691A | 1 (6) |
| Protein C or S deficiency | 1 (6) |
| Antiphospholipid syndrome | 0 (0) |
| Prothrombin G20210A | 0 (0) |
| Antithrombin deficiency | 0 (0) |
| Diabetes mellitus, n (%) | 2 (13) |
| Arterial hypertension, n (%) | 4 (25) |
| Chronic heart failure, n (%) | 2 (13) |
| Coronary artery disease, n (%) | 2 (13) |
| Previous pulmonary embolism, n (%) | 1 (6) |
| Previous DVT, n (%) | 4 (25) |
| Previous PVT, n (%) | 1 (6) |
| Venous malformation, n (%) | 1 (6) |
| Surgery in last 3 months, n (%) | 2 (13) |
| Immobilization, n (%) | 2 (13) |
| Autoimmune disease, n (%) | 2 (13) |
| Smoking, n (%) | 1 (6) |
DVT, deep vein thrombosis; PVT, plantar vein thrombosis.
Even if PVT is thought to be usually unprovoked [1,2,4], a substantial proportion of patients from our cohort had, in fact, at least 1 risk factor for venous thromboembolism (VTE; Table 1). Cancer was known in 6 (38%) patients at the time of PVT diagnosis, and a previous VTE was described in 4 (25%). These data are in line with prior studies of patients with DVT and PE [7]. As opposed to prior studies [5], none of our patients had recent physical strain in the sole. In 1 case, PVT occurred in a patient with a small venous malformation 6 years after prior invasive treatment of varices.
PVT was diagnosed by ultrasound in all patients but 1 who underwent MRI. Exemplary sonography images from 4 patients are provided in Figure 2. The use of MRI to diagnose PVT was not considered standard at our institution. During the study period, PVT was mentioned in 4 MRI reports from patients with foot pain and swelling, primarily to exclude musculoskeletal conditions: PVT was excluded in 3 patients and confirmed in 1. In 10 (63%) patients, both the medial plantar vein and the lateral plantar vein were involved (Table 2). This appears to contrast with previous reports, where an involvement of both vessels occurred in only about one-third of cases, and the lateral plantar vein appeared to be more commonly affected than the medial plantar vein [8]. In 6 (38%) patients, PVT was associated with thrombosis of the posterior tibial vein, while a proximal vein, notably the popliteal vein, was involved in only 1 (6%) case.
Figure 2.
Ultrasonographic images of thrombosed plantar veins.
Table 2.
Location of the thrombosis.
| Affected vein | Total N = 16 |
|---|---|
| Left plantar vein, n (%) | 6 (38) |
| Right plantar vein, right, n (%) | 9 (56) |
| Medial plantar vein, n (%) | 12 (75) |
| Lateral plantar vein, n (%) | 11 (69) |
| Fibular vein, n (%) | 2 (13) |
| Posterior tibial vein, n (%) | 6 (38) |
| Soleus vein, n (%) | 2 (13) |
| Popliteal vein, n (%) | 1 (6) |
| Any superficial vein in the calf, n (%) | 3 (19) |
Anticoagulant treatment regimens are shown in Table 3 and usually consisted of therapeutic-dosed anticoagulation (14 of 15 patients with available data), with the remaining 1 receiving intermediate-dosed anticoagulation. Oral anticoagulants were used in 12 (80%) patients, whereas the remaining ones received low-molecular-weight heparin (Visual Abstract). The median duration of anticoagulant treatment was 90 (Q1-Q3, 90-90) days. Only 2 patients affected by hematologic malignancy (acute myeloid leukemia and multiple myeloma, respectively) received extended anticoagulation beyond 3 months, reflecting prior management strategies for distal DVT. It was only recently shown that patients with cancer-associated isolated DVT have a substantial risk of recurrence [[9], [10], [11]] and may be considered for long-term anticoagulation treatment. Compression stockings were prescribed in 7 (44%) patients for 1 year.
Table 3.
Treatment of plantar venous thrombosis.
| Treatment | Total N = 16 |
|---|---|
| Intermediate-dosed anticoagulation, n (% of total with available data) | 1 (7) |
| Therapeutic-dosed anticoagulation, n (%) | 14 (93) |
| Oral anticoagulation | 12 (80) |
| Vitamin K antagonist, n (%) | 1 (7) |
| Rivaroxaban, n (%) | 7 (47) |
| Apixaban, n (%) | 2 (13) |
| Edoxaban, n (%) | 1 (7) |
| Parenteral anticoagulation | 3 (20) |
| Low-molecular-weight heparin, n (%) | 3 (20) |
| Length of anticoagulation (d), median (IQR) | 90 (90-90) |
| Nonsteroidal anti-inflammatory drug, n (%) | 0 (0) |
| Compression therapy, n (%) | 7 (44) |
The median time of first follow-up was 94 (Q1-Q3, 85-119) days. After a median of 17 (Q1-Q3, 5-70) months, index vein recanalization occurred in all 15 survivors. The high recanalization rate observed in the initially involved veins confirms prior results from PVT patients, and this outcome seems more favorable compared with that observed in patients with cancer-associated distal DVT [1,2,12]. Information on the resolution of symptoms was not routinely collected.
Some authors previously reported that an apparently unprovoked PVT might represent a marker for occult malignancy [2]. In this study, no new cancer diagnosis was made after PVT. Precancerous skin lesions were diagnosed 2 and 7 years after PVT; the clinical causality between these 2 events could not be determined. One patient died from the complications of multiple myeloma and acute myeloid leukemia nearly 2 years after being diagnosed with PVT.
During follow-up, 2 (12.5%; 95% CI, 3.5%-36.0%) recurrent VTE events were recorded following the discontinuation of anticoagulation. One patient without known VTE risk factors had a new-onset PVT in the contralateral leg 4 months after index PVT. One patient with melanoma had a recurrent thrombosis of the popliteal vein associated with acute PE 10 months after index PVT. No PVT recurrence at the same site was recorded. As described in a case report [13], PE is a rare but possible complication of PVT. No bleeding events were recorded during anticoagulation.
Such highly recurrent VTE rates can be interpreted in the context of the high prevalence of risk factors and the short-term use of anticoagulation. In this small cohort, therapeutic-dose direct oral anticoagulant or low-molecular-weight heparin for 3 months appeared to be effective and safe as long as anticoagulation was continued. Other reports have suggested that a management strategy not relying on anticoagulants but rather on nonsteroidal anti-inflammatory drugs alone or combined with compression stockings could be an alternative approach [[1], [2], [3],5]. Our results appear to be in line with recent findings indicating that the outcome after distal DVT secondary to major risk factors, notably cancer, may be as severe as that following proximal DVT [14].
This study bears several limitations, including a small patient sample and the retrospective design of the analysis. Moreover, the follow-up time was not homogeneous and predefined for all patients beyond the first 90 days. Uncertainty about the diagnostic accuracy of ultrasound for PVT remains, and our study cannot provide additional information in this respect. Finally, this cohort necessarily represents a group of patients who were diagnosed with PVT, whereas we cannot describe the clinical characteristics of those in whom PVT was missed.
In conclusion, we provided initial information on the clinical characteristics, treatment, and course of PVT, a condition for which almost no longitudinal data are available. The establishment of a multicenter registry on rare VTE manifestations is the next logical step to enhance our understanding also on this condition.
Acknowledgments
The study was conducted at the University Hospital Zurich and was not funded. We would like to thank Dr Spescha, Ms Probst, Ms Ackermann, and Ms Roth from the University Hospital Zurich for the support with data collection and management and Dr Zbinden for the critical comments provided.
Author contributions
M.S.: Software, Data collection, Formal analysis, Writing – original draft, Writing – review & editing, Visualization. P.A.K.: Data collection, Writing – original draft. R.M.F.: Writing – review & editing. A.K.: Review & editing. N.K.: Conceptualization, Methodology. S.B.: Data curation, Investigation, Methodology, Project administration, Writing – review & editing, Supervision.
Relationship disclosure
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Footnotes
Handling Editor: Nick van Es
The online version contains supplementary material available at https://doi.org/10.1016/j.rpth.2024.102396
Supplementary material
References
- 1.Edwards S.R., Wood O.D. Plantar vein thrombosis. Phlebology. 2021;36:26–31. doi: 10.1177/0268355520946620. [DOI] [PubMed] [Google Scholar]
- 2.Czihal M., Röling J., Rademacher A., Schröttle A., Kuhlencordt P., Hoffmann U. Clinical characteristics and course of plantar vein thrombosis: a series of 22 cases. Phlebology. 2015;30:714–718. doi: 10.1177/0268355514555385. [DOI] [PubMed] [Google Scholar]
- 3.Edwards S.R. Plantar vein thrombosis masquerading as plantar fasciitis: a case report. Phlebology. 2021;36:160–162. doi: 10.1177/0268355520953327. [DOI] [PubMed] [Google Scholar]
- 4.Karam L., Tabet G., Nakad J., Gerard J.L. Spontaneous plantar vein thrombosis: state of the art. Phlebology. 2013;28:432–437. doi: 10.1177/0268355513477087. [DOI] [PubMed] [Google Scholar]
- 5.Geiger C., Rademacher A., Chappell D., Sadeghi-Azandaryani M., Heyn J. Plantar vein thrombosis due to busy night duty on intensive care unit. Clin Appl Thromb Hemost. 2011;17:232–234. doi: 10.1177/1076029609351878. [DOI] [PubMed] [Google Scholar]
- 6.Siegal D.S., Wu J.S., Brennan D.D., Challies T., Hochman M.G. Plantar vein thrombosis: a rare cause of plantar foot pain. Skeletal Radiol. 2008;37:267–269. doi: 10.1007/s00256-007-0419-y. [DOI] [PubMed] [Google Scholar]
- 7.Timp J.F., Braekkan S.K., Versteeg H.H., Cannegieter S.C. Epidemiology of cancer-associated venous thrombosis. Blood. 2013;122:1712–1723. doi: 10.1182/blood-2013-04-460121. [DOI] [PubMed] [Google Scholar]
- 8.Barros M.V., Labropoulos N. Plantar vein thrombosis--evaluation by ultrasound and clinical outcome. Angiology. 2010;61:82–85. doi: 10.1177/0003319709338175. [DOI] [PubMed] [Google Scholar]
- 9.Valerio L., Ambaglio C., Barone M., Ciola M., Konstantinides S.V., Mahmoudpour S.H., et al. Recurrence risk after first symptomatic distal versus proximal deep vein thrombosis according to baseline risk factors. TH Open. 2019;3:e58–e63. doi: 10.1055/s-0039-1683374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Galanaud J.P., Sevestre M.A., Pernod G., Genty C., Richelet S., Kahn S.R., et al. Long-term outcomes of cancer-related isolated distal deep vein thrombosis: the OPTIMEV study. J Thromb Haemost. 2017;15:907–916. doi: 10.1111/jth.13664. [DOI] [PubMed] [Google Scholar]
- 11.Dentali F., Pegoraro S., Barco S., di Minno M.N.D., Mastroiacovo D., Pomero F., et al. Clinical course of isolated distal deep vein thrombosis in patients with active cancer: a multicenter cohort study. J Thromb Haemost. 2017;15:1757–1763. doi: 10.1111/jth.13761. [DOI] [PubMed] [Google Scholar]
- 12.Dentali F., Barco S., Pegoraro S., Di Minno M.N.D., Mastroiacovo D., Pomero F., et al. Residual vein obstruction in patients diagnosed with acute isolated distal deep vein thrombosis associated with active cancer. J Thromb Thrombolysis. 2018;46:404–408. doi: 10.1007/s11239-018-1708-0. [DOI] [PubMed] [Google Scholar]
- 13.Barros M., Nascimento I., Barros T., Labropoulos N. Plantar vein thrombosis and pulmonary embolism. Phlebology. 2015;30:66–69. doi: 10.1177/0268355514520850. [DOI] [PubMed] [Google Scholar]
- 14.Galanaud J.P., Trujillo-Santos J., Bikdeli B., Bertoletti L., Di Micco P., Poénou G., et al. Clinical presentation and outcomes of patients with cancer-associated isolated distal deep vein thrombosis. J Clin Oncol. 2024;42:529–537. doi: 10.1200/JCO.23.00429. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.