Abstract
We compared the alpha/beta interferon (IFN-α/β) sensitivities of the TC-83 vaccine strain and 24 enzootic and epizootic Venezuelan equine encephalitis (VEE) isolates. The IFN-resistant or -sensitive phenotype correlated well with epizootic or enzootic potential. IFN-α/β resistance of Trinidad donkey (TRD) virus correlated with virulence determinants in the 5′ noncoding region and glycoproteins. Infection of mice lacking a functional IFN system with the IFN-sensitive TC-83 virus resulted in disease equivalent to that produced by the virulent, IFN-resistant TRD virus, further demonstrating that IFN resistance contributes to VEE virus virulence and is a biological marker of epizootic potential.
Major epizootics of Venezuelan equine encephalitis (VEE) have occurred in northern South America (5, 9). Epizootic VEE viruses, classified antigenically as subtype 1, varieties AB (1AB) and C (1C), have not been isolated during interepizootic periods. Phylogenetic studies suggest that epizootic 1C strains may evolve from subtype 1, variety D (1D), enzootic strains maintained in sylvatic cycles (17, 26, 29, 38). Three monophyletic groups of epizootic viruses within the Colombia/Peru/Venezuela lineage have been delineated, indicating that VEE has emerged at least three times, possibly through mutations that generate viruses with similar equine virulence phenotypes (26).
Epizootic VEE viruses achieve higher viremias than enzootic viruses in experimental animals, which is an important determinant of mosquito transmission (19, 37). As a first line of defense the interferon (IFN) system is a significant barrier to virus replication (24). IFN-α and IFN-β might represent a selective barrier to the evolution of virulence and epizootic potential of VEE viruses.
The effects of IFN priming on the replication of a virulent, epizootic 1AB VEE virus, Trinidad donkey (TRD) virus, and its attenuated vaccine derivative, TC-83 virus, have been investigated with L cells (12). Regardless of the multiplicity of infection, the TC-83 virus was inhibited more than TRD virus, even though TRD virus elicited higher IFN production following infection. In hamsters and BHK-21 cells, the enzootic Pixuna (strain BeAr 35645, antigenic subtype 4) VEE virus was more sensitive than TRD virus to hamster IFN (10).
We used an in vitro assay to compare the IFN-α/β sensitivities of TC-83 virus and 24 antigenically classified enzootic and epizootic isolates (Table 1). A tissue culture cytopathic effect (CPE) reduction assay (21, 31) was chosen for its economy, efficiency, and reliability for screening large numbers of samples and was based on previously described assays used to define IFN sensitivity phenotypes of Mengo viruses (1, 14, 32, 33). The reliability of this assay was confirmed by examining the reproducibility of phenotypes between multiple experimental sets, by comparison with methods using plaque reduction and viral yield reduction as end points, and by statistical analysis. All viruses were of low passage number (range, 2 to 11), and titers were determined on Vero cell monolayers (8, 16) and stored at −80°C before use.
TABLE 1.
IFN-α/β sensitivity of VEE viruses
| Virus | Subtypea | Host species | Country/yr of isolation | 50% Inhibition (U of IFN/ml)b | Clusterc |
|---|---|---|---|---|---|
| TRD | 1AB | Donkey | Trinidad/43 | 100 | R |
| TC-83 | 1AB | —d | 3.1–12.5 | S | |
| Beck/Wyckoff | 1AB | Horse | Venezuela/38 | 100 | R |
| PTF-39 | 1AB | Human | Guatemala/69 | 50 | I |
| P676 | 1C | Mosquito | Venezuela/63 | 100–200 | R |
| V178 | 1C | Horse | Colombia/61 | 200 | R |
| V198 | 1C | Human | Colombia/62 | 200 | R |
| B80371V | 1C | Human | Colombia/95 | 100 | R |
| 125573 | 1C | Human | Venezuela/93 | 100 | R |
| 243884 | 1C | Horse | Venezuela/92 | 25–50 | I |
| SH5 | 1C | Human | Venezuela/92 | 50 | I |
| V209A | 1D | Mouse | Colombia/60 | 200 | R |
| 3880 | 1D | Human | Panama/61 | 25–50 | I |
| CoAn 9004 | 1D | Hamster | Colombia/69 | 50 | I |
| R16880 | 1D | Hamster | Ecuador/76 | 50 | I |
| IQT 1101 | 1D | Human | Peru/95 | 50 | I |
| 24138 | 1D | Hamster | Ecuador/76 | 12.5 | S |
| DEI 5191 | 1D | Human | Peru/94 | 12.5 | S |
| Mena II | 1E | Human | Panama/62 | 1.6 | S |
| 93-42124 | 1E | Horse | Mexico/93 | 100 | R |
| Everglades (Fe3-7c) | 2 | Mosquito | United States (Fla.)/63 | 3.1 | S |
| Mucambo (BeAn8) | 3A | Monkey | Brazil/54 | 0 | S |
| 71D-1252 | 3C | Mosquito | Peru/71 | 0.1 | S |
| Pixuna (BeAr35645) | 4 | Mosquito | Brazil/61 | 6.3 | S |
| AG80-663 | 6 | Mosquito | Argentina/80 | 0 | S |
Concentration at which degree of mean CPE at 5 days postinoculation was reduced by >50% in IFN-primed L929 cells relative to that in unprimed virus-infected cells.
Cluster analysis of FA data from four different experimental sets, for IFN concentrations from 25 to 200 U/ml at 5 days postinoculation, was used to classify viruses into one of two groups: IFN resistant (R) or IFN sensitive (S). Those viruses which could not be reliably classified into either group with a significance greater than 0.05 are represented by I (intermediate).
—, vaccine strain derived from TRD virus (2).
Monolayers of the VEE virus permissive mouse fibroblast cell line (L929; American Type Culture Collection) grown in 96-well plates were treated with twofold dilutions of mouse IFN-α/β (mouse fibroblast IFN-α/β; Sigma) in quadruplicate or quintuplicate for a priming period of 24 h in M199 medium (GIBCO BRL) supplemented with penicillin-streptomycin (GIBCO BRL), sodium bicarbonate (0.15%), minimal essential medium nonessential amino acids (GIBCO BRL), amphotericin B (Fungizone [1 μg/ml; E.R. Squibb & Sons]), and 5% fetal bovine serum (FBS; HyClone). Use of established monolayers and long IFN treatment periods (24 h) increases the sensitivity of this assay (31). L929 cells of identical and limited passage number (from frozen aliquots), concentration, and culture conditions (including same lot of FBS) were used in each experimental set to avoid cell-associated variables such as cell age (12, 23), density, and lineage (7, 20, 32, 35), which have been shown to affect levels of endogenous IFN production (6). After IFN priming, cultures were washed, and 50 μl of virus per well (10,000 PFU/ml) was adsorbed for 60 min, followed by addition of 100 μl of supplemented M199 with 1%FBS and incubation at 37°C and 5% CO2. Unprimed virus-infected, primed uninfected, and unprimed uninfected cultures were included as internal controls on each plate infected with a given virus. A known IFN-resistant strain (TRD, P676, or VE/IC-109) and an IFN-sensitive strain (TC-83, 3880, or VE/IC-92) were included in each experimental set to gauge interexperimental variability. Cultures were observed individually every 24 h by light microscopy. The presence or absence of CPE was used in fraction-affected (FA) data analysis, and CPE scores (percent monolayer affected) of 1 to 4 (1, less than 10%; 2, 10 to 50%; 3, 50 to 95%; 4, 95 to 100%) were used to examine IFN dose responses of individual viruses and to calculate 50% inhibitory IFN concentrations, as reported previously (7, 21, 31).
To characterize the active factor(s) in this assay, monoclonal antibodies to IFN-α and to IFN-β were separately examined for their ability to negate the effects of IFN-α/β treatment. Since the IFN-α/β preparation was produced in L929 cells stimulated with poly(rI-rC), the predominant IFN-α/β IFN was expected to be IFN-β. However, viral infection of L929 cells also stimulates IFN-α production (13) and might have influenced our assay. Titration of anti-IFN-β (rat anti-mouse L929 IFN-β; YAMASA monoclonal antibody MCA[MIFN-BETA]MB-7; Seikagaku America) in L929 cells primed with 100 U of IFN-α/β per ml before infection with either TRD or TC-83 virus demonstrated a close correlation between higher doses of anti-IFN-β and higher CPE scores. When the anti-IFN-β dose equalled that of the priming IFN-α/β dose, the degree of CPE in treated cultures equalled that of untreated cultures infected with both TRD and TC-83 viruses (data not shown). Titrations of anti-IFN-α (rat anti-mouse L929 IFN-α; YAMASA monoclonal antibody MCA[MIFN-ALPHA]MA-4; Seikagaku America) had minimal to no effect, indicating that the predominant effector in this system was IFN-β. Treatment of unprimed, TC-83 virus-infected cultures with at least 87.5 U of anti-IFN-β antibody per ml increased the CPE, such that the character and degree of CPE induced by this IFN-sensitive virus resembled those of the IFN-resistant TRD virus in similarly infected cultures (data not shown). This demonstrated that without the inhibitory influence of IFN-β, the TC-83 virus-induced CPE in L929 cells was similar to that of TRD virus, much as is seen in BHK-21 cells, which do not produce IFN-α/β. This further implicates IFN-β as the key factor modulating the CPE phenotypes of TRD and TC-83 viruses in L929 cells and minimizes the possible effect of other cytokines that may have been present in the IFN-α/β preparation or produced during infection of the L929 cells.
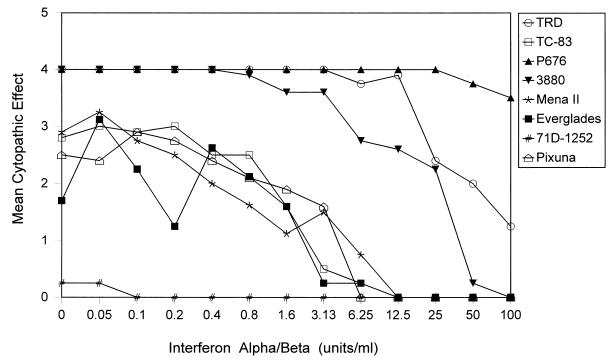
The dose responses of IFN-mediated CPE inhibition exhibited three general patterns (Fig. 1). Viruses TRD and P676 (both subtype 1 epizootic viruses) induced high scores for CPE at higher concentrations of IFN (resistant), while the vaccine virus, TC-83, was significantly inhibited at low IFN concentrations (sensitive). The 3880 virus was intermediate in sensitivity, inducing higher CPE scores than the IFN-sensitive TC-83 virus, but exhibiting inhibition at lower concentrations of IFN than the similarly cytopathic but IFN-resistant TRD and P676 viruses.
FIG. 1.
Dose-response curves of priming IFN concentration versus mean CPE (mean of four separate scores for each concentration of IFN used) for VEE virus infection in L929 cells. Sensitivities of various VEE viruses to increasing concentrations of IFN-α/β were compared at 5 days postinfection.
FA data (with FA represented by the percentage of equally treated cultures affected by CPE) at each given IFN priming dose were evaluated by multivariate statistical methods (25) to classify multiple viruses by multivariate statistical cluster analyses. Multiresponse permutation procedures (22) and cluster analyses (11) of FA data from 48 h and 5 days postinoculation indicated that the best ability to discriminate between “resistant” and “sensitive” viruses occurred on day 5 postinoculation and at priming concentrations of IFN-α/β between 20 and 200 U/ml. Therefore, FA data from day 5 postinfection at IFN concentrations of between 25 and 200 U/ml were used for classification by cluster analysis of individual viruses. The ability of this method to discriminate between different antigenic subtypes and varieties and between the same virus from different experimental sets was examined. All analysis was done at the 0.05 level of significance.
Multivariate statistical cluster analysis methods and 50% inhibitory IFN analysis methods demonstrated two distinct groups of naturally occurring VEE viruses: IFN resistant and IFN sensitive (Table 1), with some subtype 1 viruses exhibiting intermediate (Table 1) IFN sensitivity. Comparison of results from multiple experimental sets (minimum of three) for the TRD, TC-83, P676, and 3880 viruses demonstrated reproducibility of both the level of CPE and range of 50% inhibitory IFN values for individual viruses. In addition, discriminant functions between antigenic subtypes were evaluated (Table 2).
TABLE 2.
Discrimination of antigenic subtypes and varieties of VEE virus by cluster analysis of IFN phenotypes
| Antigenic group | Significancea | Groups compared | Overlap of clustersb |
|---|---|---|---|
| 1AB | a | 1AB and 1C | − |
| 1AB and 1D | − | ||
| 1AB and 1E | + | ||
| 1AB and Oc | + | ||
| 1C | a | 1C and 1D | − |
| 1C and 1E | + | ||
| 1C and O | + | ||
| 1D | a, b | 1D and 1E | − |
| 1D and O | + | ||
| 1E | a, c | 1E and O | + |
| O | c, d |
Groups with the same letter were not significantly different at the 0.05 level of significance. The level of significance was modified to take into consideration multiple comparisons in testing for significant differences.
A negative value indicates overlap, while a positive value indicates a gap between groups. Thus, the discriminant function was powerful between the 1AB group and groups 1E and O, between the 1C group and groups 1E and O, and between group O and all other subtype 1 groups. The function was not reliable between the 1D group and 1C, 1E, or 1AB groups, and to some extent was also unreliable between the 1AB group and the 1C group.
O represents the subtype 2, 3, 4, and 6 viruses.
Both methods (multivariate statistical analysis of FA data and 50% inhibitory IFN values) clearly demonstrated that all non-subtype 1 enzootic viruses of antigenic subtypes 2, 3, 4, and 6 exhibited high sensitivity to IFN in primed L929 cell cultures. These viruses were classified by cluster analysis as IFN sensitive, with powerful discriminant abilities between these antigenic subtypes and all subtype 1 ABC viruses, except for the 1AB vaccine derivative, TC-83 virus.
As a group, VEE subtype 1 viruses (which include the 1D and 1E enzootic antigenic varieties as well as the 1 AB and 1C epizootic varieties) exhibited a wide range of sensitivity to IFN-α/β, so that discriminant functions between different antigenic varieties in this subtype were not significant. The most resistant viruses, which were resistant to priming with IFN at 200 U/ml, included the 1C viruses (P676, V178, and V198) and a 1D virus (V209A) (Table 1). The 1AB viruses TRD and Beck/Wyckoff and the 1C viruses B80371V and 125573 were also significantly resistant, showing little inhibition with priming with IFN-α/β at 100 U/ml. Most of the 1D viruses tested (3880, CoAn 9004, R16880, and IQT 1101), two 1C viruses (243884 and SH5), and a single 1AB virus (PTF-39) were at least twofold more sensitive to IFN (by 50% inhibitory IFN concentration) than the resistant 1AB virus, TRD, but still significantly more resistant than the sensitive TC-83 virus and possibly represent a group of intermediate IFN sensitivity. Two other 1D viruses, 24138 and DEI 5191, as well as another 1E virus, Mena II, were 8- to 64-fold more sensitive to IFN (50% inhibitory concentration) than the resistant TRD virus and were clearly IFN sensitive by cluster analysis.
Virus 93-42124, which was recently isolated during an equine epizootic in Mexico and has been classified antigenically as an enzootic 1E virus (30), demonstrated resistance with priming with IFN-α/β at 100 U/ml. Inclusion of this virus in cluster analyses by antigenic subtypes contributed to a loss of discriminant power between subtype 1E virus and other subtype 1 viruses. This suggests that demonstration of viral IFN resistance in vitro may be a valuable predictor of virulence or epizootic potential.
To identify the molecular determinants of VEE viral IFN resistance, we tested the IFN sensitivities of plaque-purified recombinant viruses between the IFN-resistant TRD strain and the sensitive TC-83 strain (Table 3). Infectious clone-derived VE/IC-92 virus is biologically equivalent to TC-83 virus, while the virulence phenotype of VE/IC-109 virus is nearly identical to that of TRD virus (15). Recombinant viruses that contained the TC-83 virus-specific 5′ noncoding (5′NC) region (VE/IC-102, -92, and TC-83) or the TC-83 virus-specific envelope glycoproteins (VE/IC-108) were inhibited by low doses of IFN. Only TRD and clone-derived VE/IC-109 viruses, which contained both the TRD virus 5′NC region and TRD virus glycoproteins, demonstrated IFN resistance. Multivariate statistical analysis of FA data from these experiments confirmed that both viral determinants were required for the full IFN resistance phenotype. These loci were previously associated with VEE virus neurovirulence in the TRD-TC-83 model (15).
TABLE 3.
IFN sensitivity and CPE of recombinant TRD and TC-83 viruses in L929 cells
| Virus | Virus-specific genotypea
|
IFN resistanceb | |||||
|---|---|---|---|---|---|---|---|
| 5′NC | nsP1 | nsP2 | E2 | E1 | 3′NC | ||
| TRD | g | A | S | KH TVT | L | t | + |
| TC-83 | a | D | T | NY RDI | I | —c | − |
| VE/IC-109 | g | D | T | KH TVT | L | t | + |
| VE/IC-92 | a | D | T | NY RDI | I | t | − |
| VE/IC-102 | a | D | T | KH TVT | L | t | − |
| VE/IC-108 | g | D | T | NY RDI | I | t | − |
Virus-specific nucleotides in the 5′NC and 3′NC regions and amino acids in the nsP2 and nsP3 nonstructural proteins and E2 and E1 envelope glycoproteins of VEE TRD and TC-83 viruses are shown. The positions of mutations are as follows: 5′NC, 3; nsP2, 16; nsP3, 260; E2, -7, -85, -120, -192, and -296; and E1, -161 (15).
Results show viruses which were resistant (+) or sensitive (−) as demonstrated by the ability to achieve a CPE in L929 cells at an IFN-α/β priming concentration of 50 U/ml or greater. IFN phenotypes were confirmed by cluster analyses of FA data (from 25 to 200 U/ml on day 5 postinoculation) from plaque-purified recombinant viruses.
—, TC-83 virus has a single nucleotide deletion in the 3’NC region, relative to that of TRD virus.
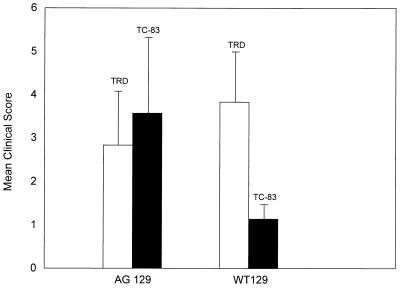
To gauge the in vivo importance of IFN-α/β to the virulence of viruses which differ in IFN-α/β sensitivity in vitro, 5.5-week-old mice lacking receptors for both IFN-α/β and IFN-γ (AG 129 mice, IFN-α/β and -γ R−/− [24]); with permission from M. Aguet, Swiss Institute for Experimental Cancer Research, Epalinges, Switzerland) and normal WT129 mice (IFN-α/β and -γ R+/+) were infected intracerebrally with 300 PFU of the IFN-resistant TRD virus or the IFN-sensitive TC-83 virus (Fig. 2). The mice were observed and scored for degree of clinical illness on day 3, when all but TC-83-infected WT129 mice and uninfected controls were severely ill and were euthanized. Clinical scores were assigned from 1 to 5 for increasing degree of clinical illness (1, minimal signs of lethargy and rough hair coat; 2, signs of depression, anorexia, hunched posture, and weakness; 3, physical evidence of neurologic dysfunction; 4, moribund behavior or complete paralysis; 5, mortality). All AG129 mice challenged with either TC-83 or TRD virus exhibited rapidly advancing clinical signs by day 3 postinfection and were euthanized. TRD-infected WT129 mice succumbed to infection at a similar rate. Only the WT129 mice with a functional IFN system survived TC-83 virus challenge with minimal clinical signs. The experiment was terminated at 10 days postinfection. Removal of the initial barrier of a functional IFN system in vivo negated the virulence differences typically demonstrated by these viruses. These results corroborate the importance of IFN-α/β in limiting the virulence of VEE virus in vivo.
FIG. 2.
Mean clinical scores (1 to 5 for increasing severity of clinical illness, as described in the text) ± standard deviation of IFN-α/β and -γ R−/− (AG129) mice and IFN-α/β and -γ R+/+ (WT129) mice infected intracerebrally with 300 PFU of IFN-resistant TRD virus (n = 6) or IFN-sensitive TC-83 virus (n = 7). All but TC-83 virus-infected WT129 mice and uninfected controls exhibited rapidly advancing clinical illness and were euthanized on days 2 to 3 postinfection. WT129/TC-83 mice survived until the experiment was terminated on day 10. Uninfected AG129 and WT129 mice showed no clinical symptoms (data not shown).
Although the mechanisms were not specifically investigated in this study, at least two viral determinants (glycoproteins and 5′NC region) were required to express the full IFN resistance phenotype of TRD virus relative to that of its attenuated vaccine derivative, strain TC-83. Other studies have also suggested that distinct combinations of mutations are required to generate alphaviruses with virulence phenotypes (18, 26, 36). The fact that several viruses of the 1C-1D group exhibited intermediate sensitivity to IFN and also exhibited ambiguous antigenic classification (125573, V209A, and SH5) (29, 38) supports the hypothesis that IFN resistance may be a multideterminant phenotype and suggests that viruses of the 1C and 1D subtypes represent a biological gradient with respect to IFN resistance and behave as a quasispecies. Those viruses which exhibit an intermediate IFN resistance phenotype may possess only part of the determinants required for the full resistance phenotype. Recent gene-sequencing studies support the theory that epizootic 1C viruses evolve from enzootic 1D viruses (17, 27, 28, 38). Interestingly, the 3880 virus, which exhibited an intermediate sensitivity to IFN and is antigenically classified as a 1D enzootic virus, was not historically associated with an epizootic, yet was isolated from a fatal human infection and is also virulent for mice. This suggests that viruses with intermediate IFN resistance may cause fatal infections in individuals but lack the potential to disseminate in epizootics. When cluster analysis was performed with only FA data from IFN concentrations between 50 and 100 U of IFN per ml (rather than between 25 and 200 U/ml) to classify the VE/IC-102 recombinant virus (which possesses the TRD-specific envelope glycoproteins but not the 5′NC region), this virus clustered with the IFN-sensitive viruses VE/IC-108 and VE/IC-92 at 48 h postinoculation, but clustered with the IFN-resistant virus VE/IC-109 at 5 days postinoculation (data not shown). The need for the increased discriminatory power for comparison of FA data from four IFN concentrations (between 25 and 200 U/ml) rather than two to reliably classify VE/IC-102 illustrates the marginal quality of the IFN phenotype of this virus. This virus produces an attenuated disease relative to that produced by VE/IC-109 virus in mice, whereas mice infected peripherally with the IFN-sensitive VE/IC-108 or VE/IC-92 virus do not exhibit significant clinical signs (15). Early classification as sensitive and late classification as resistant were also exhibited by V209A virus (not shown). The behavior of VE/IC-102 in our assay also suggested that the 5′NC region has less influence over the IFN resistance phenotype with each viral generation. If the E2 glycoprotein, which contains the major virus neutralization determinants and is continually exposed to a high degree of immunological pressure, is also a major determinant for IFN resistance, then immunologic selection of new VEE viruses with altered E2 glycoproteins could result in emergence of new IFN-resistant epizootic strains of VEE virus.
Genetic evidence suggests that VEE epizootics may result from repeated emergence of epizootic subtype IC viruses from enzootic subtype ID viruses which are maintained in ever-abundant rodent populations. The emergence of these epizootics is often associated with flooding in typically arid regions (34), suggesting that the appearance of abundant VEE virus-infected vectors in a region not typically exposed, and thus immunologically naive, provides the necessary recipe for an epizootic. The lack of an immunologic barrier leaves naive hosts dependent on IFN-α/β as a barrier to viral infection. The acutely fatal outcomes (before IFN-γ and other immunologic factors can exert influence) of TC-83 viral infections in mice which lack a functional IFN system demonstrate the importance of this system in defense against viruses which are sensitive to IFN-α/β. Evolution of viral resistance to IFN-α/β removes this barrier to infection in naive hosts and provides the potential for emergence of an epizootic in which adequate numbers of nonimmune hosts and vectors occur. Without these coincident factors, IFN-resistant viruses might die out within the rodent population. However, due to the significant selective pressure of IFN-α/β on viruses that are dependent on high viremias for efficient transmission by mosquitoes and the constant immunologic pressure for antigenic variability in an IFN resistance determinant in the envelope glycoproteins, IFN-resistant viruses would eventually reemerge, again poised for dissemination from the rodent reservoir to human and equine hosts should environmental conditions become permissive. Use of an in vitro IFN sensitivity assay with continuous VEE virus surveillance (virus isolation from sentinel animals and mosquito vectors) might predict the presence of emerging viral IFN resistance (intermediate IFN sensitivity and the potential for individual fatal outcomes) and/or potential emergence of epizootic viruses with the full IFN resistance phenotype and permit early intervention to limit the impact of these viruses.
Acknowledgments
This work was supported in part by the American Society for Microbiology/National Center for Infectious Diseases (Centers for Disease Control and Prevention) postdoctoral research associates program.
We also thank Scott Weaver of Galveston, Tex., for the gift of viruses SH5, CoAn 9004, 243884, and R16880 and Rebecca Rico-Hesse, San Antonio, Tex., for the gift of viruses 93-42124 and 125573.
REFERENCES
- 1.Bakich, E. A. Personal communication.
- 2.Berge T O, Banks I S, Tiggertt W D. Attenuation of Venezuelan equine encephalomyelitis virus by in vitro cultivation in guinea-pig heart cells. Am J Hyg. 1961;73:209–218. [Google Scholar]
- 3.Calisher C H, Kinney R M, De Souza Lopes I, Trent D W, Monath T P, Francy D B. Identification of a new Venezuelan equine encephalitis virus from Brazil. Am J Trop Med Hyg. 1982;31:1260–1272. doi: 10.4269/ajtmh.1982.31.1260. [DOI] [PubMed] [Google Scholar]
- 4.Calisher C H, Monath T P, Mitchell C J, Sabattini M S, Cropp C B, Kershchner J, Hunt A R, Lazuick J S. Arbovirus investigations in Argentina, 1977–1986. III. Identification and characterization of viruses isolated, including new subtypes of western and Venezuelan equine encephalitis viruses and four new bunyaviruses (Las Malayos, Resistencia, Barranqueras, and Antequera) Am J Trop Med Hyg. 1988;34:956–965. [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Venezuelan equine encephalitis—Colombia, 1995. Morbid Mortal Weekly Rep. 1995;44:721–724. [PMC free article] [PubMed] [Google Scholar]
- 6.Demaeyer E, Demaeyer-Guignard J. Interferons and other regulatory cytokines. New York, N.Y: John Wiley & Sons, Inc.; 1988. pp. 42–58. [Google Scholar]
- 7.Fleishman W R, Simon E H. Effect of interferon on virus production from isolated single cells. J Gen Virol. 1973;20:127–137. doi: 10.1099/0022-1317-20-2-127. [DOI] [PubMed] [Google Scholar]
- 8.France J K, Wyrick B C, Trent D W. Biochemical and antigenic comparisons of the envelope glycoproteins of Venezuelan equine encephalomyelitis virus strains. J Gen Virol. 1979;44:725–740. doi: 10.1099/0022-1317-44-3-725. [DOI] [PubMed] [Google Scholar]
- 9.Groot H. Venezuelan encephalitis. Science publication no. 243. Washington, D.C: Pan American Health Organization; 1972. The health and economic impact of Venezuelan equine encephalitis (VEE) pp. 7–16. [Google Scholar]
- 10.Jahrling P B, Navarro E, Scherer W F. Interferon induction and sensitivity as correlates to virulence of Venezuelan encephalitis viruses for hamsters. Virology. 1976;5:23–35. doi: 10.1007/BF01317831. [DOI] [PubMed] [Google Scholar]
- 11.Johnson R A, Wichern D H. Applied multivariate statistical analysis. Englewood Cliffs, N.J: Prentice-Hall, Inc.; 1982. [Google Scholar]
- 12.Jordan G W. Interferon sensitivity of Venezuelan equine encephalomyelitis virus. Infect Immun. 1973;7:911–917. doi: 10.1128/iai.7.6.911-917.1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kelly K A, Pitha P M. Differential effect of poly rI.rC and Newcastle disease virus on the expression of interferon and cellular genes in mouse cells. Virology. 1985;147:382–393. doi: 10.1016/0042-6822(85)90140-0. [DOI] [PubMed] [Google Scholar]
- 14.King R W, Simon E H. The virion of mengovirus contains anti-interferon activity. J Interferon Res. 1993;13:1–7. doi: 10.1089/jir.1993.13.1. [DOI] [PubMed] [Google Scholar]
- 15.Kinney R M, Chang G-J, Tsuchiya K R, Sneider J M, Roehrig J T, Woodward T M, Trent D W. Attenuation of Venezuelan equine encephalitis virus strain TC-83 is encoded by the 5′-noncoding region and the E2 envelope glycoprotein. J Virol. 1993;67:1269–1277. doi: 10.1128/jvi.67.3.1269-1277.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kinney R M, Trent D W, France J K. Comparative immunological and biochemical analyses of viruses in the Venezuelan equine encephalitis complex. J Gen Virol. 1983;64:135–147. doi: 10.1099/0022-1317-64-1-135. [DOI] [PubMed] [Google Scholar]
- 17.Kinney R M, Tsuchiya K R, Sneider J M, Trent D W. Genetic evidence that epizootic Venezuelan equine encephalitis (VEE) viruses may have evolved from enzootic VEE subtype 1-D virus. Virology. 1992;191:579–580. doi: 10.1016/0042-6822(92)90232-e. [DOI] [PubMed] [Google Scholar]
- 18.Kuhn R J, Griffin D E, Owen K E, Niesters H G M, Strauss J H. Chimeric Sindbis-Ross River viruses to study interactions between alphavirus nonstructural and structural regions. J Virol. 1996;70:7900–7909. doi: 10.1128/jvi.70.11.7900-7909.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.LeBlanc P A, Scherer W F, Sussdorf D H. Infections of congenitally athymic (nude) and normal mice with avirulent and virulent strains of Venezuelan encephalitis virus. Infect Immun. 1978;21:779–785. doi: 10.1128/iai.21.3.779-785.1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lockart R Z, Jr, Horn B. Interaction of an interferon with L cells. J Bacteriol. 1963;85:996–1002. doi: 10.1128/jb.85.5.996-1002.1963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meager A. Quantification of interferons by anti-viral assays and their standardization. In: Clemens M J, Morris A G, Gearing A J H, editors. Lymphokines and interferons: a practical approach. Oxford, United Kingdom: IRL Press; 1987. pp. 129–147. [Google Scholar]
- 22.Mielke P W., Jr Non-metric statistical analysis: some metric alternatives. Stat Plan Inference. 1986;13:377–387. [Google Scholar]
- 23.Monahan P S, Grossberg S E. Age-related cellular resistance of the chicken embryo to viral infections. II. Inducible resistance produced by influenza virus and E. coli. J Infect Dis. 1970;121:624–633. doi: 10.1093/infdis/121.6.624. [DOI] [PubMed] [Google Scholar]
- 24.Muller U, Steinhoff U, Reis L F, Hemii S, Pavlovic J, Zinkernagel R M, Auguet M. Functional role of type I and type II interferons in antiviral defense. Science. 1994;264:1918–1921. doi: 10.1126/science.8009221. [DOI] [PubMed] [Google Scholar]
- 25.Pedhazur E J. Multiple regression in behavioral research: explanation and prediction. 2nd ed. Austin, Tex: Holt, Rinehart and Winston, Inc.; 1982. Multiple regression, discriminant analysis, and multivariate analysis of variance; pp. 685–719. [Google Scholar]
- 26.Powers A M, Oberste M S, Brault A C, Rico-Hesse R, Schmura S M, Smith J F, Kang W, Sweeney W P, Weaver S C. Repeated emergence of epidemic/epizootic Venezuelan equine encephalitis from a single genotype of enzootic subtype 1D virus. J Virol. 1997;71:6697–6705. doi: 10.1128/jvi.71.9.6697-6705.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ricco-Hesse R, Roehrig J T, Dickerman R W. Monoclonal antibodies define antigenic variation in the 1D variety of Venezuelan equine encephalitis virus. Am J Trop Med Hyg. 1988;38:157–194. doi: 10.4269/ajtmh.1988.38.187. [DOI] [PubMed] [Google Scholar]
- 28.Ricco-Hesse R, Roehrig J T, Trent D W, Dickerman R W. Genetic variations of Venezuelan equine encephalitis virus strains of the 1D variety in Colombia. Am J Trop Med Hyg. 1988;38:195–204. doi: 10.4269/ajtmh.1988.38.195. [DOI] [PubMed] [Google Scholar]
- 29.Ricco-Hesse R, Weaver S C, De Siger J, Medina G, Salas R A. Emergence of a new epidemic/epizootic Venezuelan equine encephalitis virus in South America. Proc Natl Acad Sci USA. 1995;92:5278–5281. doi: 10.1073/pnas.92.12.5278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roehrig J T, Bolin R A. Monoclonal antibodies capable of distinguishing epizootic from enzootic varieties of subtype 1 Venezuelan equine encephalitis viruses in a rapid indirect immunofluorescence assay. J Clin Microbiol. 1997;35:1887–1890. doi: 10.1128/jcm.35.7.1887-1890.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rubinstein S, Familletti P C, Pestka S. Convenient assay for interferons. J Virol. 1981;37:755–758. doi: 10.1128/jvi.37.2.755-758.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Simon E H, Isono N, Bradley C. The role of interferon induction in the interferon sensitivity of the Mengovirus mutant is-1. J Gen Virol. 1984;65:247–250. doi: 10.1099/0022-1317-65-1-247. [DOI] [PubMed] [Google Scholar]
- 33.Simon E H, Kung S, Koh T T, Brandman P. Interferon-sensitive mutants of Mengovirus. I. Isolation and biological characterization. Virology. 1976;69:727–736. doi: 10.1016/0042-6822(76)90501-8. [DOI] [PubMed] [Google Scholar]
- 34.Sudia W D, Newhouse V F. Epidemic Venezuelan equine encephalitis in North America: a summary of virus-vector-host relationships. Am J Epidemiol. 1975;101:1–13. doi: 10.1093/oxfordjournals.aje.a112066. [DOI] [PubMed] [Google Scholar]
- 35.Tze-Ta C, Simon E H, Fleischmann W R, Jun Z. The mechanism of interferon action in single cells: accumulation of intracellular virus. J Gen Virol. 1973;20:139–149. doi: 10.1099/0022-1317-20-2-139. [DOI] [PubMed] [Google Scholar]
- 36.Vrati S, Tucker P C, Griffin D E, Hardwick J M. Ross River virus with a deletion in the E2 gene: properties of the virion virus-specific macromolecular synthesis, and attenuation of virulence in mice. Virology. 1994;151:222–232. doi: 10.1016/0042-6822(86)90044-9. [DOI] [PubMed] [Google Scholar]
- 37.Walton T E, Johnson K M. Epizootiology of Venezuelan equine encephalomyelitis in the Americas. J Am Vet Med Assoc. 1972;161:1509–1515. [PubMed] [Google Scholar]
- 38.Weaver S C, Bellew L A, Ricco-Hesse R. Phylogenetic analysis of alphaviruses in the Venezuelan equine encephalitis complex and identification of the source of epizootic viruses. Virology. 1992;191:282–290. doi: 10.1016/0042-6822(92)90190-z. [DOI] [PubMed] [Google Scholar]
- 39.Young N, Johnson K M. Antigenic variants of Venezuelan equine encephalitis virus: their geographic distribution and epidemiological significance. Am J Epidemiol. 1969;89:286–307. doi: 10.1093/oxfordjournals.aje.a120942. [DOI] [PubMed] [Google Scholar]