Abstract
Introduction
Center-of-pressure (COP) synchronization and symmetry can inform adaptations in balance control following one-sided sensorimotor impairments (e.g., stroke). As established force plates are impossible to transport, we aimed to criterion validate a portable pressure plate for obtaining reliable COP synchronization and symmetry measures, next to conventional postural stability measures.
Methods
Twenty healthy adults participated. In a single session, three 40-s eyes-open and eyes-closed quiet stance trials were performed per plate-type, randomly ordered. Individual-limb COPs were measured to calculate between-limb synchronization (BLS) and dynamic control asymmetry (DCA). Net COP (i.e., limbs combined) area, amplitude, and velocity were used to describe anteroposterior (AP) and mediolateral (ML) postural stability. Criterion validity was evaluated using Spearman correlations (r) and Bland-Altman plots. Test-retest reliability was tested using intraclass correlation coefficients (ICC).
Results
Strong correlations (r > 0.75) and acceptable reliability (ICC > 0.80) were found regarding individual-limb COP velocity and DCA, net COP ML amplitude and AP and ML velocities. Bland-Altman plots yielded possible proportional bias; the pressure plate systematically underestimated COP scores by force plates and a larger error associated with a larger measurement.
Conclusions
Despite correlations between instruments and sufficient reliability for measuring postural stability and DCA, this technical note strongly suggests, due to a systematic deviation, using the same plate-type to accurately assess performance change within subjects longitudinally over time.
Keywords: Reliability and validity, postural balance, posturography, biomechanics, force plate, center of pressure
Background
Pathologies causing one-sided sensorimotor impairments (e.g., stroke) compromise balance control and increase the risk of falls. 1 However, balance recovery studies in this field remain scarce and often fail to distinguish behavioral restitution from compensations by relying on clinical scales, such as the Berg Balance Scale (BBS), 2 that have considerable ceiling effects 3 and do not show qualitative changes on the rated tasks.4,5 Likewise, most posturographic studies measuring, for example, the center-of-pressure (COP) area, velocity, or amplitude as a more precise postural stability measure are confounded by using only one force plate. This is insufficient to separate the limbs and inform adaptations in standing balance as reflected by, for example, the between-limb synchronization (BLS)6,7 and dynamic control asymmetry (DCA).8,9 These metrics are currently utilized in the stroke recovery literature to inform, respectively, how well both limbs work together to control balance and how much each limb contributes. Hence, these measures are complementary in providing greater insight into compensatory changes in balance performance following one-sided loss of sensorimotor function.
Measuring BLS and DCA requires posturographic systems with two floor-mounted force plates by established brands, which are currently considered the “gold standard” method.10,11 However, these force plates are expensive and impossible to transport, which makes clinical studies difficult to conduct over the first 3 to 6 months poststroke – the period of significant balance recovery 2 - while patients are being discharged from stroke services to their own homes or care facilities in the region. Acknowledging this limitation, pressure plates (or mats) have recently been proposed as a portable and more-affordable clinical tool to measure postural stability.12–14 Although not yet investigated, these instruments can record individual-limb COP movements using a single plate due to a larger number of embedded sensors. This advantage may further mitigate the need for extensive infrastructure to measure BLS and DCA, thus improving clinical feasibility of conducting serial measurements as part of trials.
As a “first step” toward its criterion validation, the current study involving healthy adults compared a portable pressure plate with gold standard force plates for measuring COP synchronization (i.e., BLS) and symmetry (i.e., DCA) while standing, next to conventional descriptors of postural stability. Acknowledging that repeatable measures are conditional for showing agreement between assessment methods, 15 we investigated the test-retest reliability of each plate type before comparing them. Our research questions were as follows:
(1) Are three immediate test-retest repetitions using a pressure plate or gold standard force plates sufficient to achieve reliable measures of postural stability, BLS, and DCA in healthy adults standing quietly?
(2) Are averaged pressure plate measures of postural stability, BLS, and DCA in agreement with those obtained using gold standard force plates in healthy adults standing quietly?
We expected to confirm the literature by showing a high test-retest reliability (i.e., intraclass correlation coefficients (ICC) ≥ 0.80) of AMTI (Advanced Mechanical Technology Inc., MA, USA) force plates for measuring postural stability,10,11 and hypothesized to find similar results with respect to BLS and DCA. Furthermore, we expected that a pressure plate’s reliability for measuring postural stability, BLS, and DCA would be comparable to force plates. Regarding our second question, we expected to find high positive correlations in these outcomes between instruments (i.e., a correlation coefficient ≥0.75), in line with three prior validation experiments using similar pressure-sensitive devices.12–14 Because correlations alone are insufficient to detect systematic biases, we additionally aimed to explore the level of agreement with a Bland-Altman analysis.15,16 Measurement bias with lower COP values by a pressure plate was priorly suggested,12,14 warranting further investigation.
Methods
Design
Ten female and 10 male adults with a perfect BBS score volunteered to participate. No back or lower limb injury, use of medication, or neurological condition were reported. All volunteers provided written informed consent according to the policy of the local ethics committee (Antwerp University Hospital, BE; protocol no. 19/18/233; date 24/06/2019).
In a single session, a 0.5 m Footscan (RS Scan, Materialize, BE) pressure plate (578 x 418 x 12 mm, sampling frequency 500 Hz) and two AMTI Type OR 6-7 force plates (500 x 400 mm, sampling frequency 1000 Hz) were used to quantify quiet standing balance during separate, randomly ordered measurements to avoid interference of the differently sized, rigid plates. As such, per instrument six 40-s trials were performed, alternatively with the eyes open or closed. The bare feet were positioned in a standardized way (8.4 cm heel-to-heel distance, 9° toe-out angle), and participants were instructed to stand as still as possible while keeping the eyes fixated at a 3-m distant target placed in front of them or with the eyes closed. This protocol aligns with typical clinical posturographic testing.8,9
To assess test-retest reliability per instrument, variation in three immediate test repetitions in the same participant and under the same condition (i.e., eyes-open or eyes-closed) was analyzed using ICCs. 17 Regarding criterion validity, defined following COSMIN 18 as the extent to which outcomes reflect results by the gold standard, averaged outcomes per condition and participant were compared between instruments.
Data processing
For each eligible trial, we calculated the net (i.e., both limbs combined) and individual-limb COP with anteroposterior (AP) and mediolateral (ML) coordinates from the last 30 s to avoid starting effects. The reference axes were rotated by 9° to coincide with the foot axis. We followed these steps, as described per instrument:
• Force plates: Raw tri-axial force data from four load sensors - one in each corner - were collected with Nexus (Vicon Motion Systems Ltd, UK). Then, a custom-made MATLAB (version R2018a) algorithm was used to compute the COP for each side using these equations:
Here, x, y, and z are the AP, ML, and vertical directions, respectively; F are the forces; M are the moments; and C is the offset from the geometric plate center.
Subsequently, the net COP was calculated as a weighted average using this equation:
• Pressure plate: Many embedded sensors (2.6 sensors/cm2) record the plantar distribution of vertical forces, or Fz. COP was then computed using the system’s own software (Footscan 9, RS Scan, Materialize, BE) as the point of application of the summed forces using all sensors bearing weight at the entire plate (i.e., net COP), or at either geometrical side to extract individual-limb COPs.
Finally, the COP signals from both instruments were low-pass filtered (2nd order Butterworth, 10 Hz) using the same MATLAB algorithm, and the same scripts were used to calculate outcome metrics.
Outcome metrics
Peak-to-peak sway amplitude in mm (nCOPamp-ap, nCOPamp-ml) and root mean square velocity in mm/s (nCOPvel-ap, nCOPvel-ml) were determined in the AP and ML directions as traditional descriptors of postural stability. 19 In addition, the net COP area (nCOParea) was calculated in mm2 as an ellipse that covered 85% of the entire signal using principal component analyses. 20
Amplitudes (iCOPamp-ap, iCOPamp-ml) and velocities (iCOPvel-ap, iCOPvel-ml) were also determined for each individual limb, next to BLS as a cross-correlation coefficient between COP movements at a zero time-lag6,7 and DCA as a symmetry index 8 following this equation:
The loaded and unloaded sides were determined by dividing the mean vertical force under each limb. We focused on the AP direction, and BLS and DCA were not calculated with ML COPs because frontal plane sway is mainly controlled by a loading-unloading mechanism that is not reflected by COP changes. 6
Statistical analysis
Regarding question 1, we computed the ICCs using a two-way mixed-effects model (ICC3,3) as a measure of agreement between the three test-retest measurements. 17 A multiple-measurement type was chosen because the actual application is based on averaging trials.10,11 Acceptable reliability was defined as an ICC3,3 > 0.80. Specifically, ICC3,3 ≥ 0.90 was interpreted as excellent and 0.80–0.90 as good reliability. 21
For question 2, averaged COP scores were plotted per participant to observe general trends between instruments. Spearman’s rank correlation coefficients (r) were calculated for each outcome and r ≥ 0.75 were interpreted as strong, 0.50–0.74 as moderate, and <0.50 as low or no relationship. 21 Mean differences were statistically analyzed using Wilcoxon singed rank tests because the averaged outcomes per instrument were not normally distributed. In conjunction, Bland-Altman plots (i.e., subject-specific mean scores by difference scores) were created, including the mean difference line with its standard error and the limits of agreement (LOA). 15 Narrower LOA encompassing zero reflect better agreement, whereas the distribution of difference scores was visually analyzed for bias. According to Ludbrook, 16 a significant difference by a constant amount is interpreted as fixed bias and a slope pattern as proportional bias. The significance level of all analyses was set two-tailed at 0.05.
A sample of 20 subjects was defined a priori, by offering 80% power to detect a correlation coefficient of a least r = 0.60 between both devices at a significance level of 0.05.
Results
One participant had a corrupted dataset, and 19 participants (10 female) with a mean (±SD) age of 35.4 ± 15.9 years were included in the analyzes. Their body mass and length were 77.3 ± 13.7 kg and 171.2 ± 7.0 cm, respectively.
Table 1 shows the reliability outcomes with ICC3,3 point-estimates and their confidence intervals. Regarding the force plates, ICC3,3 ≥ 0.80 were found for eyes-open and eyes-closed conditions regarding nCOParea, nCOPamp-ml, nCOPvel-ap, nCOPvel-ml, iCOPvel-ap, and DCA. A pressure plate yielded ICC3,3 ≥ 0.80 regarding the nCOPvel-ml, iCOPvel-ap, and DCA under both visual conditions. In addition, the pressure plate reached sufficient reliability for measuring nCOPamp-ml and nCOPvel-ap under the eyes-closed condition. In general, ICCs < 0.80 were found for measuring amplitudes (i.e., nCOPamp-ap, iCOPamp-ap) and BLS, irrespective of the instrument and visual condition.
Table 1.
Test-retest reliability of a pressure plate and laboratory-grade force plates for measuring postural stability and interlimb coordination in quiet standing balance control. ICC3,3 point-estimates with 95% confidence intervals are shown, reflecting variation between three immediate 30-s trial repetitions within a single measurement session.
| Eyes-open stance | Eyes-closed stance | |||
|---|---|---|---|---|
| ICC3,3 [force plates] | ICC3,3 [pressure plate] | ICC3,3 [force plates] | ICC3,3 [pressure plate] | |
| Net COP measures of postural stability (n = 19) | ||||
| nCOParea (mm2) | 0.84 (0.66; 0.94)* a | 0.04 (−1.24; 0.63) | 0.81 (0.59; 0.93)* | 0.70 (0.37; 0.88) |
| nCOPamp-ap (mm) | 0.53 (−0.43; 0.81) | 0.47 (−0.14; 0.78) | 0.70 (0.35; 0.88) | 0.62 (0.18; 0.84) |
| nCOPamp-ml (mm) c | 0.92 (0.84; 0.97)** a | 0.69 (0.30; 0.88) | 0.89 (0.76; 0.95)* | 0.83 (0.64; 0.93)* |
| nCOPvel-ap (mm/s) c | 0.89 (0.75; 0.95)* | 0.72 (0.39; 0.89) | 0.91 (0.81; 0.97)** | 0.86 (0.70; 0.94)* |
| nCOPvel-ml (mm/s)b,c | 0.95 (0.90; 0.98)** | 0.84 (0.65; 0.94)* | 0.94 (0.87; 0.98)** | 0.85 (0.67; 0.94)* |
| Individual-limb COP – dominant limb (n = 19) | ||||
| iCOPamp-ap (mm) | 0.73 (0.41; 0.89) | 0.59 (0.11; 0.83) | 0.85 (0.67; 0.94)* a | 0.57 (0.07; 0.82) |
| iCOPvel-ap (mm/s)b,c | 0.95 (0.89; 0.98)** | 0.80 (0.55; 0.92)* | 0.95 (0.89; 0.98)** | 0.89 (0.77; 0.96)* |
| Individual-limb COP – non-dominant limb (n = 19) | ||||
| iCOPamp-ap (mm) | 0.41 (−0.32; 0.77) | 0.48 (−0.11; 0.79) | 0.44 (−0.22; 0.77) | 0.62 (0.18; 0.84) |
| iCOPvel-ap (mm/s)b,c | 0.80 (0.56; 0.92)* | 0.81 (0.59; 0.93)* | 0.84 (0.65; 0.93)* | 0.84 (0.66; 0.93)* |
| Interlimb coordination measures (n = 19) | ||||
| BLS | 0.75 (0.43; 0.90) a | 0.47 (−0.14; 0.78) | 0.39 (−0.36; 0.75) | 0.23 (−0.49; 0.66) |
| DCA (%)b,c | 0.90 (0.78; 0.96)* | 0.91 (0.81; 0.96)** | 0.92 (0.83; 0.97)* | 0.93 (0.85; 0.97)* |
Results are shown per instrument and visual condition. ICC3,3 estimates highlighted in bold reflect a statistical significance finding with *, reflecting good reliability (ICC3,3 0.90-0.80), and **, reflecting excellent reliability (ICC3,3 > 0.90).
adiscrepancy between instruments of ICC3,3 > 0.20 favoring the marked value.
bICC3,3 ≥ 0.80 reflecting good reliability across instruments for the eyes open condition.
cICC3,3 ≥ 0.90 reflecting excellent reliability across instruments for the eyes closed condition.
Figure 1 illustrates that a relatively higher COP score by the pressure plate corresponds to a higher force plate score, and vice versa. In line with this observation, Table 2 shows strong correlation coefficients of r ≥ 0.75 for both visual conditions regarding nCOPvel-ml, iCOPvel-ap, and DCA. In addition, nCOParea, nCOPamp-ml, nCOPvel-ap, and iCOPamp-ap were strongly correlated between instruments with r ≥ 0.75 with respect to the eyes-closed measurements.
Figure 1.
Mean COP scores per participant measured with either a pressure plate or gold standard force plates. Peak-to-peak amplitude (amp, shown in purple) and root mean square velocity (vel, shown in green) of the COP in anteroposterior and mediolateral directions, recorded at the limbs separately (ie, left-sided and right-sided) and combined (ie, net), are plotted per individual subject (N = 19). Thicker bars reflect pressure plate scores and thinner bars reflect force plates as the gold standard. These bars are overlapped per participant to visually compare outcomes obtained from both instrument types for measuring COP when quiet standing.
Table 2.
Criterion validity of a pressure plate for measuring postural stability and interlimb coordination in quiet standing control using two laboratory-grade force plates as the gold standard.
| Eyes-open stance | Eyes-closed stance | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pressure plate (SD) | Force plates (SD) | Mean difference (SE) | P | r | Pressure plate (SD) | Force plates (SD) | Mean difference (SE) | P | r | |||||||
| Net COP measures of postural stability (n = 19) | ||||||||||||||||
| nCOParea (mm2) | 27.55 | (16.55) | 104.63 | (71.01) | −77.08 | (14.48) | <.001 | 0.60* | 17.47 | (15.04) | 102.07 | (74.11) | −84.60 | (14.13) | <.001 | 0.80** |
| nCOPamp-ap (mm) | 10.44 | (4.17) | 19.91 | (5.19) | −9.47 | (1.04) | <.001 | 0.43 | 8.39 | (2.82) | 20.37 | (4.86) | −11.99 | (0.85) | <.001 | 0.61* |
| nCOPamp-ml (mm) | 4.47 | (1.73) | 10.31 | (4.20) | −5.84 | (0.70) | <.001 | 0.67* | 3.99 | (2.07) | 10.33 | (4.69) | −6.35 | (0.69) | <.001 | 0.82** |
| nCOPvel-ap (mm/s) | 2.61 | (0.79) | 8.40 | (2.28) | −5.79 | (0.39) | <.001 | 0.68* | 3.12 | (1.19) | 10.47 | (3.48) | −7.35 | (0.58) | <.001 | 0.80** |
| nCOPvel-ml (mm/s) | 1.41 | (0.55) | 4.88 | (1.77) | −3.47 | (0.30) | <.001 | 0.89** | 1.53 | (0.76) | 5.40 | (2.35) | −3.87 | (0.39) | <.001 | 0.87** |
| Individual-limb COP measures (n = 38) | ||||||||||||||||
| iCOPamp-ap (mm) | 11.24 | (4.81) | 21.72 | (6.22) | −10.48 | (0.79) | <.001 | 0.65* | 9.26 | (3.28) | 22.07 | (6.07) | −12.81 | (0.77) | <.001 | 0.57* |
| iCOPvel-ap (mm/s) | 2.88 | (1.19) | 9.18 | (3.00) | −6.30 | (0.34) | <.001 | 0.75** | 3.40 | (1.58) | 11.29 | (4.36) | −7.89 | (0.51) | <.001 | 0.78** |
| Interlimb coordination measures (n = 19) | ||||||||||||||||
| BLS | 0.82 | (0.14) | 0.81 | (0.17) | 0.01 | (0.03) | 0.77 | 0.65* | 0.76 | (0.14) | 0.81 | (0.09) | −0.05 | (0.02) | 0.06 | 0.61* |
| DCA (%) | −0.70 | (50.98) | 7.39 | (39.80) | −8.09 | (5.06) | 0.16 | 0.86** | 0.50 | (46.26) | 7.34 | (38.62) | −6.84 | (6.95) | 0.52 | 0.76** |
The mean values and their standard deviations (SDs) are shown per instrument. Mean differences are presented between devices with a standard error (SE). p values are the probability statistics that the mean values are the same (null hypothesis) assessed with Wilcoxon signed rank tests. Results highlighted in bold are statistically significant (p < .05). Lastly, r estimates show the strength of the Spearman correlation coefficients between instruments with *, reflecting a statistically significant correlation of moderate strength (r = 0.5-0.74); and **, reflecting a significant strong (r ≥ 0.75) correlation.
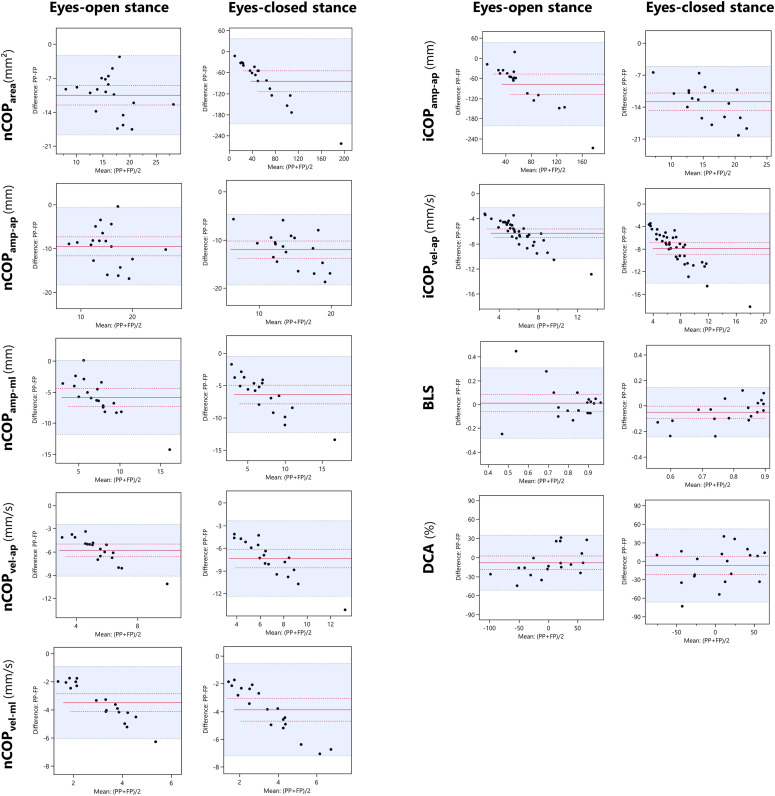
A second observation from Figure 1 is that the pressure plate COP scores are consistently lower than those of the force plates. In the same vein, mean differences between instruments were highly significant with respect to each COP metric investigated (p < .001, Table 2). Bland-Altman plots further show that most difference scores were positioned within the LOA with broad ranges that were situated below zero, except for nCOParea (Figure 2). In addition, an inclined distribution slope is shown for nCOParea, nCOPamp-ml, nCOPvel-ap, nCOPvel-ml, iCOPvel-ap, and iCOPvel-ml, such that an increasingly larger difference was observed relative to the mean score, indicating proportional bias.
Figure 2.
Bland-Altman plots with subject-specific differences and mean scores between a pressure plate and two force plates as the gold standard. The Y-axis shows the subject-specific difference scores between the two measurement instruments, and the X-axis represents the mean scores per subject. Solid red lines represent the mean difference score of the entire group of healthy participants (N = 19), dotted red lines represent the standard error of the mean score, and blue dotted lines and the blue-colored area in-between represent the upper and lower ends of the limits of agreement. On the left, the net COP metrics reflecting postural stability are displayed. On the right, individual-limb COP and interlimb coordination metrics are displayed. A downwards shift of the mean scores deviating from the zero score, as can be observed in most of the shown figures, reflect a systematic difference with lower pressure plate value compared with force plates that increases relative to the magnitude of the measure (ie, proportional bias). PP, pressure plate; FP, force plates.
Mean differences in BLS and DCA were, however, non-significant (p > .05, Table 2) and Bland-Altman plots show difference scores that are evenly distributed within the LOA, ranging above and below zero.
Discussion
In the current study, a reliability analysis (question 1) and head-to-head comparison were performed between a pressure plate and gold standard force plates to criterion validate the former (question 2) for measuring COP while quiet standing. We advanced prior validation experiments12–14 by addressing the capability of a single pressure plate to capture individual-limb COP movements to address postural stability, as reflected by the total amount of COP sway, and interlimb coordination in terms of BLS and DCA. We found acceptable test-retest reliability for measuring velocity-based COP metrics with the pressure plate, including DCA, with strong correlations relative to force plates. COP amplitudes and BLS were found less reliable. Despite strong associations between instruments, we identified a systematic deviation. The pressure plate systematically underestimated force plate outcomes of COP with proportional bias. Seemingly, both instruments acted in a similar, but not identical way. These findings are discussed with implications for clinical use.
Similar to prior validation studies,12–14 we found strong associations between a pressure plate and established force plates for measuring postural stability. In our analyzes, this association was strongest for velocity-based measures of COP (Table 2), and we have shown for the first time a similar correlation strength with respect to DCA, i.e., a symmetry index of individual-limb COP velocities.
COP velocities are known to be particularly consistent, requiring two to three trials to reach reliable outcomes.10,11 This reliability is thought to result from a sensitivity to high-frequency changes in the COP signal that are more consistent and reflect stabilizing responses to body sway. 19 In agreement, we found AMTI force plates to yield good-to-excellent reliability for measuring nCOPvel-ml, nCOPvel-ap, iCOPvel-ap, and DCA, whereas displacement-based measures including COP amplitudes and BLS were less reliable, despite averaging three 30-s trials (Table 1). A low reliability of force plates for measuring BLS agrees with a previous study in stroke patients. 22 In comparison, the pressure plate exhibited a similar reliability in the same measures during the eyes-closed condition, whereas eyes-open measurements often yielded ICCs < 0.8, or insufficient reliability (Table 2). This may suggest that a pressure plate’s measurement precision is lower relative to a force platform, but improves when sway is provoked by closing the eyes, which typically causes larger and more regular COP movements. 23
Notwithstanding strong correlations and acceptable test-retest reliability, we identified a systematic deviation. COP scores by the pressure plate were significantly smaller than those by force plates (Table 2), and this deviation shows increment proportionally to the magnitude of the measure (Figure 2). To gain more insight into this deviation, we have added a limited power spectral analysis in a single subject for each instrument (see attachment A). The energy content of the COP signal measured with the pressure plate is lower compared the force platform. Furthermore, the attached figures suggest that the pressure plate particularly misses out on the higher-frequency COP components.
Proportional bias in summary outcomes of COP was earlier suggested,12,14 pointing toward an underlying cause inherent to the use of different soft- and hardware. Although speculative, this may include the sensor type because, relative to force plates, horizontal forces are not recorded by a pressure plate. Furthermore, averaging forces over many embedded sensors could result in a smoothing effect, causing a lower COP velocity and amplitude. Alternatively, the different sampling frequencies (pressure plate 500 Hz vs force plates 1000 Hz) may have caused bias, acknowledging that COP measures are sensitive to sampling frequencies, 24 although both instruments exceed the recommended 100 Hz. 11
Interestingly, Bland-Altman plots show agreement between instruments for measuring DCA, yet with fairly large LOA (eyes-open [52.5; −66.2], eyes-closed [35.2; −51.3]; Figure 2). The systematic deviation appears to be controlled for by using two instrument-dependent COP measures to calculate this symmetry index. This underpins our finding of systematic rather than random deviation from force plates when measuring COP with a pressure plate. However, whether both plate-types exhibit agreement in the case of asymmetric balance due to, for example, post-stroke hemiplegia7,8 cannot be addressed here.
Implications
First, strong correlations between instruments indicate that the pressure plate can serve as an alternative; however, because of systematic bias, it cannot replace force plates. Therefore, we strongly recommend that researchers and clinicians use the same instrumentation between testing sessions to evaluate performance changes in standing postural control within subjects. Second, the pressure plate yielded similar reliability to gold standard force plates when visual input was suppressed. This finding may suggest that a pressure plate’s utility to measure COP is limited to challenging test conditions, or when assessing quiet standing balance in clinical populations who exhibit greater spontaneous sway. However, this requires confirmation of our findings in these populations. Third, velocity-based measures are particularly reliable and therefore advised for describing (change in) balance performance, irrespective of the choice of plate-type. Finally, general similarities between instruments suggest that existing recommendations for standardizing force plate measurements are applicable to pressure plates. This includes that at least 90 s of COP data should be collected over several test repetitions within a session.10,11 In line with prior reliability studies,10,11,19 averaging three 30-s trials was found sufficient to achieve reliable outcomes in our study. This is important for clinical use because pathological populations are often unable to adhere to longer assessment durations. Our own protocol, as part of a recently completed stroke recovery study, 25 is attached in supplement (see attachment B).
Limitations
We included a small sample of mostly younger adults. Replication in larger samples, including healthy age-matched subjects, is needed to confirm our findings and provide normative values in higher-age categories as a reference for clinical trials. Moreover, generalization of our findings to people with asymmetric balance remains unknown. Second, we did not record COP data simultaneously by “stacking” plates to avoid interference. However, simultaneous recordings are recommended for future studies to allow more-accurate comparisons by eliminating within-subject variability. Third, our analyses should be viewed within the context of specific devices, and outcome metrics and balance conditions that were chosen to align with established clinical testing protocols. This includes, for example, cropping the first 10 s of each recording and calculating summary measures of the resultant 30 s of data. Alternatively, future studies may investigate epoch-based metrics, as recently argued. 26 Finally, we tested intrasession test-retest reliability. However, assessing test-retest reliability between sessions is required to further develop standardized testing protocols for tracking changes in balance performance due to ongoing sensorimotor recovery or an intervention, as outlined above (see implications).
Conclusion
The current results suggest that the pressure plate is a reliable assessment tool, yielding strong correlations with gold standard force plates for measuring postural stability and individual limb contributions to balance control, as reflected by DCA. However, there are some concerns with its criterion validity as we found a systematic deviation causing lower COP scores compared with outcomes by force plates. This strongly suggests using of the same instrumentation to accurately assess performance changes in a consistent way within a specific subject. If this limitation is considered when designing data collection protocols, a pressure plate may hold promise as a clinical tool to make serial measurements as part of longitudinal studies in populations with impaired balance and an increased risk of falls feasible. Therefore, further validation experiments investigating measurement properties of pressure plates for assessing balance, next to pressure insoles to measure COP movements during various upright activities 27 and portable force plates that are emerging, 28 are encouraged in pathological populations.
Supplemental Material
Supplemental Material for Is a portable pressure plate an alternative to force plates for measuring postural stability and interlimb coordination of quiet standing balance control? by Jonas Schröder, Ann Hallemans, Wim Saeys, Laetitia Yperzeele, Gert Kwakkel and Steven Truijen in Journal of Rehabilitation and Assistive Technologies Engineering
Acknowledgments
The authors would like to thank Charlotte Johnson for writing assistance, and the following M.Sc. students for aiding data collection and subject recruitment: Heleen Leurs, Carolien Van de Perck, Silke Van Goubergen, Gabriela Wimberska, Denice Kliebisch, and Sofia Lopez-Cotarelo Flemons.
Appendix.
Abbreviations
- AMTI
Advanced Mechanical Technology Inc.
- AP
Anteroposterior
- BBS
Berg Balance Scale
- BLS
Between-limb synchronization
- COP
Center-of-pressure
- COPamp
Peak-to-peak sway amplitude of the center-of-pressure in mm
- COParea
Sway area of the center-of-pressure calculated as an ellipse covering 85% of the signal in mm2
- COPvel
Root mean squared sway velocity of the center-of-pressure in mm/s
- COSMIN
Consensus-based Standards for the selection of health Measurement INstruments
- DCA
Dynamic control asymmetry
- ICC
Intraclass correlation coefficient
- ICC3,3
Two-way mixed-effects, multiple-measurements type intraclass correlation coefficient
- iCOP
Individual-limb center-of-pressure trajectory
- LOA
Limits of agreements
- ML
Mediolateral
- nCOP
Net center-of-pressure trajectory
Author Contributor: JS collected, analyzed, and interpreted the data, and was a major contributor in writing the manuscript. AH contributed substantially to the data processing and writing the manuscript. WS, LY and GK contributed by revising the manuscript. ST contributed to the conception of this study and revised the manuscript. All authors have read and approved the final manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The authors would like to acknowledge funding by the Research Foundation Flanders (FWO), Belgium who provided JS a doctoral (PhD) grant for strategic basic research (application number 1S64819N) to conduct this research.
Guarantor: JS
Supplemental Material: Supplemental material for this article is available online.
ORCID iD
Jonas Schröder https://orcid.org/0000-0003-0290-9923
References
- 1.Batchelor FA, Mackintosh SF, Said CM, et al. Falls after stroke. Int J Stroke 2012; 7: 482–490. DOI: 10.1111/j.1747-4949.2012.00796.x. [DOI] [PubMed] [Google Scholar]
- 2.Buvarp D, Rafsten L, Abzhandadze T, et al. A cohort study on longitudinal changes in postural balance during the first year after stroke. BMC Neurol 2022; 22: 324–2022. DOI: 10.1186/s12883-022-02851-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blum L, Korner-Bitensky N. Usefulness of the Berg balance scale in stroke rehabilitation: a systematic review. Phys Ther 2008; 88: 559–566. DOI: 10.2522/ptj.20070205. [DOI] [PubMed] [Google Scholar]
- 4.Garland SJ, Ivanova TD, Mochizuki G. Recovery of standing balance and health-related quality of life after mild or moderately severe stroke. Arch Phys Med Rehabil 2007; 88: 218–227. DOI: 10.1016/j.apmr.2006.11.023. [DOI] [PubMed] [Google Scholar]
- 5.Patterson KK, Inness E, McIlroy WE, et al. A retrospective analysis of post-stroke Berg balance scale scores: how should normal and at-risk scores be interpreted? Physiother Can 2017; 69: 142–149. DOI: 10.3138/ptc.2015-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Winter DA, Prince F, Frank JS, et al. Unified theory regarding A/P and M/L balance in quiet stance. J Neurophysiol 1996; 75: 2334–2343. DOI: 10.1152/jn.1996.75.6.2334. [DOI] [PubMed] [Google Scholar]
- 7.Mansfield A, Mochizuki G, Inness EL, et al. Clinical correlates of between-limb synchronization of standing balance control and falls during inpatient stroke rehabilitation. Neurorehabil Neural Repair 2012; 26: 627–635. DOI: 10.1177/1545968311429688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roelofs JMB, van Heugten K, de Kam D, et al. Relationships between affected-Leg Motor impairment, postural asymmetry, and impaired body sway control after Unilateral Supratentorial stroke. Neurorehabil Neural Repair 2018; 32: 953–960. DOI: 10.1177/1545968318804405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Haart M, Geurts AC, Huidekoper SC, et al. Recovery of standing balance in postacute stroke patients: a rehabilitation cohort study. Arch Phys Med Rehabil 2004; 85: 886–895. DOI: 10.1016/j.apmr.2003.05.012. [DOI] [PubMed] [Google Scholar]
- 10.Lafond D, Corriveau H, Hebert R, et al. Intrasession reliability of center of pressure measures of postural steadiness in healthy elderly people. Arch Phys Med Rehabil 2004; 85: 896–901. DOI: 10.1016/j.apmr.2003.08.089. [DOI] [PubMed] [Google Scholar]
- 11.Ruhe A, Fejer R, Walker B. The test-retest reliability of centre of pressure measures in bipedal static task conditions--a systematic review of the literature. Gait Posture 2010; 32: 436–445. DOI: 10.1016/j.gaitpost.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 12.Pena Junior PM, de Sa Ferreira A, Telles G, et al. Concurrent validation of the centre of pressure displacement analyzed by baropodometry in patients with chronic non-specific low back pain during functional tasks. J Bodyw Mov Ther 2021; 28: 489–495. DOI: 10.1016/j.jbmt.2021.06.020. [DOI] [PubMed] [Google Scholar]
- 13.Bickley C, Linton J, Sullivan E, et al. Comparison of simultaneous static standing balance data on a pressure mat and force plate in typical children and in children with cerebral palsy. Gait Posture 2019; 67: 91–98. DOI: 10.1016/j.gaitpost.2018.08.012. [DOI] [PubMed] [Google Scholar]
- 14.Goetschius J, Feger MA, Hertel J, et al. Validating center-of-pressure balance measurements using the MatScan® pressure mat. J Sport Rehabil 2018; 27. DOI: 10.1123/jsr.2017-0152. [DOI] [PubMed] [Google Scholar]
- 15.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 1: 307–310. [PubMed] [Google Scholar]
- 16.Ludbrook J. Comparing methods of measurements. Clin Exp Pharmacol Physiol 1997; 24: 193–203. DOI: 10.1111/j.1440-1681.1997.tb01807.x. [DOI] [PubMed] [Google Scholar]
- 17.Koo TK, Li MY. A Guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 2016; 15: 155–163. DOI: 10.1016/j.jcm.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mokkink LB, Terwee CB, Patrick DL, et al. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol 2010; 63: 737–745. DOI: 10.1016/j.jclinepi.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 19.Geurts AC, Nienhuis B, Mulder TW. Intrasubject variability of selected force-platform parameters in the quantification of postural control. Arch Phys Med Rehabil 1993; 74: 1144–1150. [PubMed] [Google Scholar]
- 20.Oliveira LF, Simpson DM, Nadal J. Calculation of area of stabilometric signals using principal component analysis. Physiol Meas 1996; 17: 305–312. DOI: 10.1088/0967-3334/17/4/008. [DOI] [PubMed] [Google Scholar]
- 21.Portney LG. Foundations of clinical research: applications to evidence-based practice. Fourth edition ed. F. A. Davis, 2020. [Google Scholar]
- 22.Martello SK, Boumer TC, Almeida JC, et al. Reliability and minimal detectable change of between-limb synchronization, weight-bearing symmetry, and amplitude of postural sway in individuals with stroke. Res Biomed Eng 2017; 33: 113–120. DOI: 10.1590/2446-4740.06816. [DOI] [Google Scholar]
- 23.Donker SF, Roerdink M, Greven AJ, et al. Regularity of center-of-pressure trajectories depends on the amount of attention invested in postural control. Exp Brain Res 2007; 181: 1–11. DOI: 10.1007/s00221-007-0905-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schmid M, Conforto S, Camomilla V, et al. The sensitivity of posturographic parameters to acquisition settings. Med Eng Phys 2002; 24: 623–631. DOI: 10.1016/s1350-4533(02)00046-2. [DOI] [PubMed] [Google Scholar]
- 25.Schroder J, Saeys W, Yperzeele L, et al. Time course and mechanisms underlying standing balance recovery early after stroke: design of a prospective cohort study with repeated measurements. Front Neurol 2022; 13: 781416. DOI: 10.3389/fneur.2022.781416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reed CA, Chaudhari AMW, Worthen-Chaudhari LC, et al. A new perspective on transient characteristics of quiet stance postural control. PLoS One 2020; 15: e0237246. DOI: 10.1371/journal.pone.0237246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cudejko T, Button K, Al-Amri M. Wireless pressure insoles for measuring ground reaction forces and trajectories of the centre of pressure during functional activities. Sci Rep 2023; 13: 14946. DOI: 10.1038/s41598-023-41622-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Walsh M, Church C, Hoffmeister A, et al. Validation of a portable force plate for evaluating postural sway. Percept Mot Skills 2021; 128: 191–199. DOI: 10.1177/0031512520945092. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Is a portable pressure plate an alternative to force plates for measuring postural stability and interlimb coordination of quiet standing balance control? by Jonas Schröder, Ann Hallemans, Wim Saeys, Laetitia Yperzeele, Gert Kwakkel and Steven Truijen in Journal of Rehabilitation and Assistive Technologies Engineering