Abstract
Background
The most common and debilitating side effects of radiation therapy (RT) for prostate cancer (PC) are fatigue, sleep disturbance, anxiety, and depression. Previous research has reported palliative benefits from certain self-management approaches, such as mindfulness meditation.
Objective
To develop, pre-test, and evaluate the feasibility, acceptability and initial benefit of brief, audio-based mindfulness delivered during daily RT for PC compared to a relaxing music control.
Methods
Following intervention development, participants were randomized to either brief guided mindfulness audio recordings or a relaxing music control during daily RT. A pre-testing phase was first conducted to determine optimal program start time, length, and content most associated with retention. A final program (n = 26) was delivered daily, starting on day one of week 2 of RT and lasting 4 consecutive weeks. Feasibility was defined as ≥70% on enrollment rate, retention, and audio program adherence. Acceptability was measured with a 12-item post-study survey. A secondary focus compared between group changes on patient reported outcomes of fatigue, anxiety, depression, sleep disturbance, and related outcomes at baseline and follow up assessments. Descriptive statistics and general linear models were used.
Results
Overall, 76% (n = 38) of approached men enrolled. Pre-testing retention rates were <70% while the final program’s retention rate was 89%. The majority of acceptability criteria were met in both conditions, with relatively higher ratings in the mindfulness arm. Compared to music controls, mindfulness participants demonstrated significantly less uncertainty intolerance at 4-weeks (P = .046, d = .95); and significantly lower fatigue scores (P = .049, d = 1.3) and lower sleep disturbance scores (P = .035, d = 1.1) at the 3 months follow up.
Conclusion
The final intervention met feasibility and acceptability criteria. Pre-testing refinements played a key role for optimal program delivery and retention. Audio-based mindfulness delivered during RT for PC hold potential to help decrease RT-related physical and emotional side effects.
Keywords: mindfulness, meditation, prostatic neoplasms, radiation therapy
Introduction
Almost two-thirds of all new cancer patients in the United States receive radiation therapy (RT) at some point during their treatment, 1 from which short- and long-term side effects can negatively affect physical and psychosocial health. 1 Fatigue is one of the most common, debilitating, and distressing side effects of RT reported by cancer patients,2-4 which not only negatively affect quality of life, but may also be related to shorter recurrence free periods and overall survival. 5 Often related to fatigue are stress, anxiety, depression, and sleep disturbance – all of which are known to manifest before, during and following RT. 6
Prostate cancer (PC) is the most common non-cutaneous form and the second leading cause of cancer-related death among men in the United States. 7 Previous studies have reported the negative side effects of fatigue, sleep disturbance, anxiety and depression among men diagnosed with PC during and following RT.3,8-11 A growing body of evidence supports the benefits of mindfulness as an effective treatment to improve mood and decrease symptoms of sleep disturbance and fatigue in cancer patients.12-19 Mindfulness is defined as a quality of present moment awareness and attentional control characterized by curiosity, openness and acceptance 20 that can engender greater cognitive, affective, and physiological flexibility and self-regulation.21,22
Mindfulness has been described as regulating emotions through embodied “bottom-up” and “top-down” neural processes. 23 Bottom-up regulation decreases emotional reactivity through lower brain region activation without recruitment of higher brain regions in the prefrontal cortex. It is implicated in the modulation of sensory and interoceptive components. Top-down regulation decreases emotional reactivity through engagement of prefrontal brain regions by means of active reinterpretation and reappraisal of the meaning of emotional stimuli. 24 It is understood that mindfulness may enact similar top-down and bottom-up regulatory processes for physical symptoms such as fatigue 25 and sleep. 26 For example, mindfulness might assist bottom-up activation by aiding in the reorientation of attentional processes to be open, curious, and accepting of present moment experiences of fatigue or sleep disturbance without judgement of embellishment. In contrast, mindfulness may also facilitate top-down activation through reappraising physical sensations as simply being “different” sensory experiences instead of being automatically perceived as negative or deleterious.
Most mindfulness programs are delivered using face-to-face (in-person or online), group-based, time intensive formats lasting 18-24 hours over a 7-8-week period. 27 This format can present logistical and potential financial barriers for cancer patients with competing demands. Moreover, they may be less accessible to men undergoing cancer treatment, whose participation in supportive care is significantly lower than women with cancer. 28 Audio-based mindfulness programs may be a reasonable alternative, however only 2 studies using guided audios have been conducted with cancer patient groups.29,30 Further, no studies have implemented audio support during the cancer treatment encounter itself. Since most men receive RT for PC daily for up to 12 weeks, an opportunity exists to leverage the RT treatment experience for mindfulness training.
Due to the implementation unknowns of delivering mindfulness during RT, an implementation feasibility pre-testing approach was utilized first to test this clinical intervention until optimal retention benchmarks were achieved. This maximizes patient and medical team adoption, delivery, and sustainment. This flexible approach allows for certain compromises regarding traditional study power so long there is adequate face validity of the proposed interventions and strategies, has some basis of direct or indirect evidence, poses no more than minimal risk to patients, and is supported by clinical and organizational stakeholders.
The primary purpose of this study was to determine the implementation feasibility and acceptability of a brief audio mindfulness program delivered during RT for PC. A secondary focus was to examine early phase indicators of benefit of the audio program on self-reported physical and psychological outcomes. We hypothesized that the pre-tested mindfulness program would meet benchmarks of feasibility and acceptability and demonstrate preliminary patterns of improvement in patient reported outcomes compared to a time and attention matched control.
Methods
This study was approved by the participating institution (#STU00200537) and listed on ClinicalTrials.gov (NCT03852017). Methods undertaken were comprised of 3 separate phases: Phase I: Program Development; Phase II: Implementation Pre-Testing; and Phase III: Pilot Randomized Controlled Trial. Each phase is described below.
Phase I: Development of Mindfulness Program Content and Time/Attention Matched Control
Study members DV and CM (experienced mindfulness meditation teachers and researchers) worked with RT experts (JK and SS) to identify appropriate meditations that would be suitable for delivery during RT for PC. This included listening with mindful awareness, basic mindful breathing and bodily awareness meditations, mindful awareness of sounds and thoughts, and lovingkindness/compassion-focused meditations. Efforts were taken to frame instructor language to acknowledge the patient’s supine position and possible interruptions from treatment-related sounds or instructions, and to avoid words or phrases that might elicit a negative emotional reaction (e.g., instead of saying “body scan” it was referred to as “body awareness”). Scripts were written and guided audio recordings were created.
Next, members of the study team sought to identify an appropriate control condition that could match the time, attention, and delivery mode of the mindfulness audios. A second goal what that the control offered a sufficiently face valid health beneficial alternative for participants and yet remained adequately inert to still function as a control. Relaxing music audios were selected for this purpose and were created in consultation with the extant music therapy literature and a music therapist from the participating institution. While “relaxing” music is associated with highly subjective musical preferences and familiarity,31-33 universal elements often associated with cardiovascular and respiratory indicators of relaxation include slower tempo, melody, and rhythmic complexity. 34 To standardize what participants listened to we compiled a small library of selections from the genres of relaxing classical music, sounds of nature, and ambient/instrumental pieces (e.g., “spa music”) to offer a diverse yet standardized selection of recordings.
The audio delivery approach was originally planned to use earbuds and MP3 players. However, during a tour of the RT treatment room prior to starting, the investigators were instructed that RT patients were not permitted to have anything obstructing their ears given the need to hear instructions from a radiation therapist. During this tour it was noted that there was a circular rubber ring (e.g., dog toy) on the RT table, which therapists explained was for patients to hold with both hands up against their chest to prevent their arms from hanging off the table. With this in mind, we purchased several similar hypoallergenic rubber Frisbees and fastened MP3 players and Bluetooth speakers to each using self-locking cable zip ties. This way participants could use these to hold against their chest and be able to hear the audio content during their sessions without having their ears obstructed. See Figure 1 for an image of this configuration.
Figure 1.
Audio delivery device created for this study.
Phase II: Implementation Pre-testing
Setting and Participants
All participants were recruited from the Department of Radiation Oncology at Northwestern Memorial Hospital in Chicago. Working closely with medical team staff, a trained research assistant (RA) recruited participants directly from treatment clinics. Study participants were identified and referred by a designated physician, nurse, or clinician. The study RA obtained participants’ informed consent and HIPAA authorization according to IRB approved procedures. Study flyers were posted in clinic waiting rooms and on the cancer center website.
Eligible participants were diagnosed with clinically localized PC, were scheduled to receive at least 7 weeks of daily RT, were at least 18 years of age, able to speak and understand English, and cognitively intact and free of serious psychiatric illness (as determined by referring physician). Participants were ineligible if they reported using mindfulness meditation ≥ 3 times a week for the past 4 weeks.
Procedures
Following consent, participants were provided a brief audio equipment demonstration, given a 1-page handout to illustrate how to operate the equipment, and administered the baseline assessment. After this, a research team member randomized participants into mindfulness or music groups using a computer-based random assignment program with a 1:1 allocation ratio, then notified study participants and medical team staff of their group. Participants were instructed to pick up their audio equipment from the radiation technologist each day they came in for treatment. They were instructed to start the audio program just prior to their treatment and to turn it off after their treatment session ended. Instructions on how to operate the audio equipment were taped to the equipment. Participants were instructed to select their preferred audio recording on each given day, which was noted by the radiation technologist. Because the treatment length of RT for PC varied between 2-12 minutes depending on the week of treatment, audio recordings were purposefully created to last longer in duration than the longest RT session so that it would not end before their treatment had finished. Participants were told that when their treatment was done, their respective recording would not be finished, and it was OK to simply stop listening at that point and return the equipment to the radiation technologist.
Participants completed an assessment at baseline prior to randomization (T1), and again immediately following their intervention period (T2), as well as one (T3) and 3 months (T4) after completing the intervention. The assessment included several short questionnaires that asked about their quality of life and the symptoms they may have been experiencing. Participants received a $25 gift card after completing the 1-month assessment, and another $25 after completing the 3-month assessment. Because the primary purpose of Phase II was to pre-test different delivery timings and content, these data were not included in the final Phase III analysis of patient reported outcomes.
Measures and Metrics
Socio-demographic information collected at baseline included: birth date, relationship status, race/ethnicity, occupation, and educational history. Clinical data included: diagnosis date, height, weight, and clinical stage, most recent PSA, other previous or current cancer treatments, and co-morbid medical conditions. Other baseline-only measures included meditation history and expectancy/credibility using 4-items assessing one’s thoughts and feelings about the therapy being offered. 35
Implementation feasibility metrics included documenting the number of participants approached, enrolled, and retained throughout the study and tallying the total number possible listening opportunities during the audio program. Intervention acceptance was assessed using a brief questionnaire administered at the T2 assessment. Patient reported outcomes measures have all demonstrated adequate psychometric properties and were administered at all time points. Cronbach’s alpha (α) internal consistency estimates were calculated for each measure at baseline. Measures included: PROMIS 8-item short forms of Fatigue (α = .90), Anxiety (α = .91), Depression (α = .95), and Sleep Disturbance(α = .92) 36 ; the three-item Fear of Recurrence sub-scale of the Memorial Anxiety Scale (α = .73) 37 ; the 12-item Intolerance of Uncertainty Scale (α = .63), 38 and the 15-item Mindfulness Attention Awareness Scale (α = .86). 39 PROMIS raw scores were converted into T-scores (see https://www.healthmeasures.net/) where means = 50 and standard deviations = 10. PROMIS scores also offer clinical cut scores denoting within normal limits (mean scores <55), mild (mean scores between 55-59), moderate (mean scores between 60-79), and severe (mean scores >80). All other measures used raw summed scores with the following ranges: Fear of Recurrence = 0-12, Intolerance of Uncertainty = 0-48, Mindfulness = 15-90.
Analysis and Program Modification Decision Points
We used SPSS version 27 for all statistical analyses, which included calculation of frequency distributions, measures of central tendency, and variability for all variables of interest. The goal of implementation pre-testing programs was to identify optimal start time, program duration, and program content based on participant and medical team feedback. Feasibility was defined as ≥70%: enrollment rate (# enrolled/# approached), retention rate (# retained/# enrolled), and program adherence (total number of listening opportunities).
Phase III: Pilot Randomized Controlled Trial
All Phase III procedures, including setting, participant eligibility and recruitment, randomization, and measures and assessments were identical for the Phase III Pilot Randomized Controlled Trial. The following additional analyses were included: acceptability and analysis of patient reported outcomes. Acceptability was defined as ≥70% on post-intervention survey questions that indicated positive endorsement from “a little bit through “very much”.
An intention to treat analysis was conducted using general linear models to examine initial patterns of change between groups on self-reported outcomes over time. The primary focus of these analyses was to learn how group membership influenced self-reported fatigue, with a secondary focus on the final program’s influence on other physical and psychosocial outcomes. Age and number of audio sessions listened to were entered as covariates into analytic models given their potential influence on outcomes. Effect sizes were calculated for significant findings using the Morris (2008) d corr estimate, which is the difference between Hedge’s g of 2 different treatment groups in pre-post research designs. 40 Given the feasibility nature of this study, no power analysis was used for these analyses, which were intended to better understand initial patterns and relationships.
Results
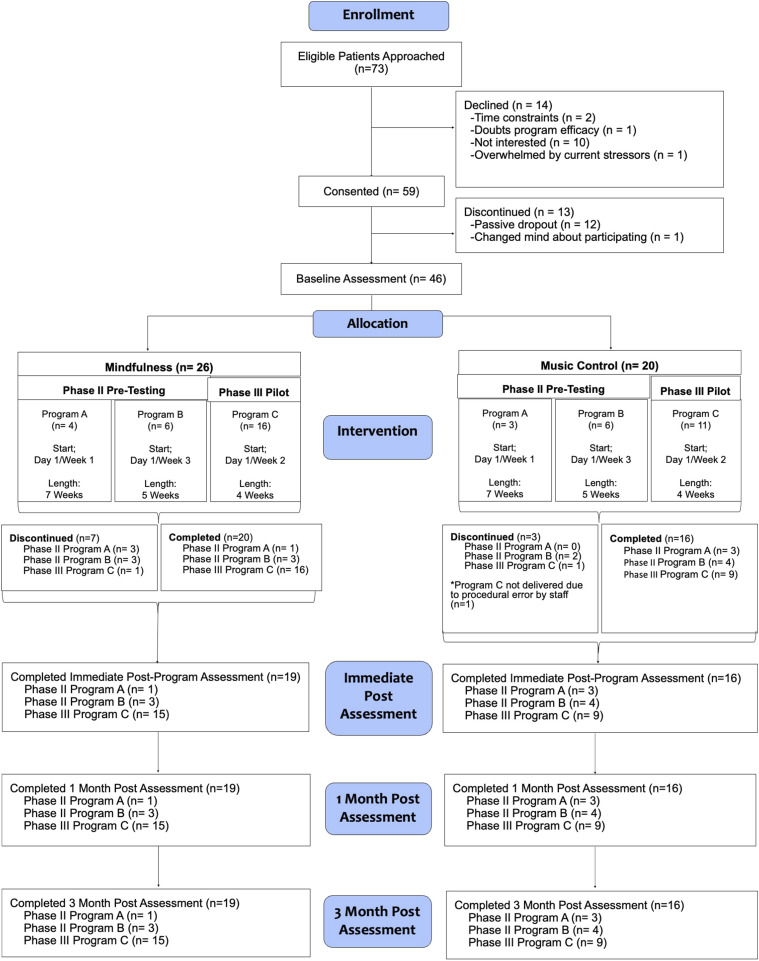
Please see Figure 2 for the study flow and assignment to the different groups and programs.
Figure 2.
CONSORT diagram.
Phase II: Pre-testing for Optimal Intervention Delivery Timing and Content
Two separate programs made up Phase II pre-testing (Programs A and B), each based on different start times and lengths. Program A began on day one of week one for 7 consecutive weeks, and Program B began on day one of week 3 for 5 consecutive weeks. Within each program, different cohorts tested slightly different content selections. Participant feedback was collected from those who dropped out.
In total, 19 participants were randomized to Programs A and B (seven in Program A; 12 in Program B). Program A was comprised of 4 mindfulness and 3 music group participants while Program B was comprised of 6 mindfulness and 6 music group participants. Between the 2 programs, 8 individuals dropped out (Group A = 3; Group B = 5), all within the first 3 days of their participation (57%-58% retention rate). Participants in the mindfulness group dropped out more often (n = 6) than music group participants (n = 2).
Program A Findings and Refinements
Program A’s enrollment rate was 70%. Audio adherence was 9.4% (mindfulness) and 66.4% (music), respectively. Cohort I of Program A began with 3 different mindfulness and 3 different music selections (see Table 1). For this Cohort, the sequence of when participants could listen to their respective recording was fixed so that everyone had to listen to the same recording each day for a week period before they were offered a new recording the following week. We learned quickly from music participants that only having 3 selections was suboptimal, and that other options were preferred. We received similar feedback from mindfulness participants regarding the lack of diversity in the selection of recordings. In response, for Cohort II of Program A, we expanded the music library to include several relaxing classical music selections, as well as several calming nature-based sounds (e.g., forest, river, etc.). We matched that with additional mindfulness selections and allowed all participants to freely choose which recordings they wanted. These changes were well received by music participants, and there were no additional complaints regarding the music options after that.
Table 1.
Audio Program Modifications and Frequency of Use.
| Program | Cohort | Audio Recording | # of Times Listened | Total | Average Audios Per Person |
|---|---|---|---|---|---|
| Phase II Program A: Day 1 of week 1 for 7 Weeks (n = 10) | Mindfulness cohort I (n = 3) | Listening awareness | 1 | 1.00 | .33 |
| Breathing awareness | 0 | ||||
| Bodily awareness | 0 | ||||
| Mindfulness cohort II (n = 3) | Compassion awareness I | 3 | 32.00 | 10.67 | |
| Compassion awareness II | 0 | ||||
| Bodily awareness I | 6 | ||||
| Bodily awareness II | 9 | ||||
| Breathing awareness I | 3 | ||||
| Breathing awareness II | 1 | ||||
| Breathing awareness III | 5 | ||||
| Listening awareness I | 5 | ||||
| Listening awareness II | 0 | ||||
| Open awareness I | 0 | ||||
| Open awareness II | 0 | ||||
| Music cohort I (n = 3) | Ambient/Instrumental I | 30 | 60.00 | 20.00 | |
| Ambient/Instrumental II | 20 | ||||
| Ambient/Instrumental III | 10 | ||||
| Music cohort II (n = 1) | Classical I (bach selections) | 5 | 33.00 | 33.00 | |
| Classical II (beethoven selections) | 4 | ||||
| Classical III (Handel, Hayden, & mascagni selections) | 5 | ||||
| Classical IV (mozart selections) | 1 | ||||
| Nature I (nature sounds without music) | 0 | ||||
| Nature II (forest sounds with gentle music) | 1 | ||||
| Nature III (ocean waves with gentle music) | 1 | ||||
| Nature IV (rainfall with gentle music) | 1 | ||||
| Ambient/Instrumental I | 6 | ||||
| Ambient/Instrumental II | 6 | ||||
| Ambient/Instrumental III | 3 | ||||
| Phase II Program B: Day 1 of week 3 for 5 Weeks (n = 11) | Mindfulness cohort I (n = 3) | Compassion awareness I | 4 | 14.00 | 4.67 |
| Compassion awareness II | 0 | ||||
| Bodily awareness I | 1 | ||||
| Bodily awareness II | 0 | ||||
| Breathing awareness I | 1 | ||||
| Breathing awareness II | 5 | ||||
| Breathing awareness III | 0 | ||||
| Listening awareness I | 1 | ||||
| Listening awareness II | 0 | ||||
| Open awareness I | 2 | ||||
| Open awareness II | 0 | ||||
| Mindfulness cohort II (n = 4) | Awareness of breath & body I | 12 | 61.00 | 15.25 | |
| Awareness of breath & body II | 9 | ||||
| Awareness of sounds & thoughts | 12 | ||||
| Body awareness | 12 | ||||
| Breathing space awareness | 9 | ||||
| Compassion awareness (befriending meditation) | 7 | ||||
| Music cohort I (n = 4) | Classical I (bach, beethoven, mozart selections) | 15 | 41.00 | 10.25 | |
| Classical II (handel, hayden, & mascagni selections) | 11 | ||||
| Nature I (forest sounds with and without music) | 4 | ||||
| Nature II (ocean and rainfall with gentle music) | 3 | ||||
| Ambient/Instrumental I | 5 | ||||
| Ambient/Instrumental II | 3 | ||||
| Phase III Program C: Day 1 of week 2 for 4 Weeks (n = 26) | Mindfulness (n = 16) | Awareness of breath & body I | 57 | 296.00 | 18.50 |
| Awareness of breath & body II | 47 | ||||
| Awareness of sounds & thoughts | 47 | ||||
| Body awareness | 49 | ||||
| Breathing space awareness | 45 | ||||
| Compassion awareness (befriending meditation) | 51 | ||||
| Music (n = 10) | Classical I (bach, beethoven, mozart selections) | 34 | 177.00 | 17.70 | |
| Classical II (handel, hayden, & mascagni selections) | 29 | ||||
| Nature I (forest sounds with and without music) | 30 | ||||
| Nature II (ocean and rainfall with gentle music) | 28 | ||||
| Ambient/Instrumental I | 31 | ||||
| Ambient/Instrumental II | 25 |
Several mindfulness participants who dropped out of Program A offered feedback that having a female narrator was undesirable (all selections were from a female instructor), and that a male’s voice would be preferred. One mindfulness participant who dropped out informed the attending physician that he found the content of the compassion selection to be “preachy” and that it was upsetting for him to be asked to focus on challenging people and situations from his past as he had enough to worry about. Two mindfulness participants who dropped out said they did not think it would be helpful. Finally, in consultation with the medical team, we learned that all patients were being placed on a 1-week treatment break during week 6 of RT, which interrupted the scheduled delivery of audio recordings. Medical team members also expressed concern that starting the study on the very first day of RT could add additional stress to their experience.
Program B Findings and Refinements
Program B’s enrollment rate was 77%. Audio adherence was 42.8% (mindfulness) and 41% (music), respectively. In response to Program A feedback, Program B started on day one of week 3 and was shortened to 5 weeks to ensure participants completed the audio program before the treatment break. Further, Cohort II of Program B only included a male narrator with consolidated mindfulness practices totaling 6 selections vs 11 (similar consolidations were made for music as well) to offer variety but not be overwhelming. The compassion meditation was modified so it only focused on sending thoughts of peace and goodwill to oneself, a loved one, a stranger, and all human beings, removing the instruction to direct these intentions to someone who is challenging or difficult. To try to address the perception that this program would not be helpful, the study PI (DV) recorded a brief audio welcome and orientation so that all participants could better understand the purpose and potential importance of this study. While Program B saw relative increases over Program A in the frequency of audio recording use, some mindfulness and music participants still dropped out due to disinterest. Finally, the medical team suggested shortening the program length to 4 weeks to make sure there was sufficient time to complete the program before the treatment break.
Phase III: Randomized Controlled Trial with Optimal Intervention
Phase II pre-testing feasibility metrics and participant and medical team feedback were used to create and implement the Phase III pilot study, which began on day one of week 2 of RT for 4 consecutive weeks.
Pilot study participants (n = 27) included 16 men assigned to the mindfulness arm and 11 men assigned to the music arm (see Table 2). There were no statistically significant differences on baseline self-reported outcomes measures between those who dropped out (n = 11) and remained in the study (n = 34). Further, there were no statistically significant differences on baseline sociodemographic, clinical, treatment (e.g., on hormone therapy), or self-reported outcomes measures except for self-reported hypertension (Mindfulness n = 6, Music n = 4) and arthritis (Mindfulness n = 1, Music n = 2). Given these minor differences would not be expected to disproportionately affect listening ability during RT, these were not included as additional covariates.
Table 2.
Baseline Characteristics Across Different Programs.
| All Participants (N = 46) | P | Phase II Program a (n = 7) | P | Phase II Program B (n = 12) | P | Phase III Program C (n = 27) | P | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mindfulness (N = 26) | Music (N = 20) | Mindfulness (n = 4) | Music (n = 3) | Mindfulness (n = 6) | Music (n = 6) | Mindfulness (n = 16) | Music (n = 11) | |||||
| Race | ||||||||||||
| White | 21 | 16 | 2.82 | 3 | 3 | n/a | 5 | 5 | 2.00 | 13 | 8 | 1.52 |
| Black | 2 | 4 | 0 | 0 | 0 | 1 | 2 | 3 | ||||
| Other | 3 | 0 | 2.45 | 1 | 0 | 3.94 | 1 | 0 | n/a | 1 | 0 | .71 |
| Ethnicity | ||||||||||||
| Hispanic | 2 | 0 | 1.61 | 0 | 0 | n/a | 2 | 0 | 2.40 | 0 | 0 | n/a |
| Non-Hispanic | 24 | 20 | 4 | 3 | 4 | 6 | 16 | 11 | ||||
| Relationship | ||||||||||||
| Married | 22 | 16 | .17 | 4 | 3 | n/a | 5 | 3 | 2.50 | 13 | 10 | .83 |
| Single | 2 | 2 | 0 | 0 | 0 | 1 | 2 | 1 | ||||
| Partner | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | ||||
| Widowed | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | ||||
| Income | ||||||||||||
| <$50k | 1 | 2 | 9.82 | 0 | 0 | 2.24 | 0 | 1 | 6.29 | 1 | 1 | 4.92 |
| $50k - $100K | 7 | 2 | 1 | 1 | 2 | 0 | 4 | 1 | ||||
| $101-$150k | 6 | 2 | 1 | 0 | 2 | 1 | 3 | 1 | ||||
| $151-$200k | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | ||||
| $201-$250k | 2 | 1 | 0 | 0 | 0 | 0 | 2 | 1 | ||||
| > $250k | 4 | 5 | 0 | 0 | 1 | 1 | 3 | 4 | ||||
| Declined | 5 | 7 | 1 | 2 | 1 | 3 | 3 | 2 | ||||
| Employment | ||||||||||||
| Self-employed | 7 | 3 | 1.50 | 3 | 0 | 7.00 | 1 | 1 | 4.68 | 3 | 2 | 1.00 |
| Employed FT | 9 | 6 | 1 | 0 | 4 | 2 | 4 | 4 | ||||
| Employed PT | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | ||||
| Disabled | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | ||||
| Retired | 8 | 9 | 0 | 2 | 0 | 2 | 8 | 5 | ||||
| Education | ||||||||||||
| Some HS | 0 | 1 | 4.56 | 0 | 0 | 4.28 | 0 | 1 | 4.00 | 0 | 0 | 4.52 |
| HS or GED | 3 | 0 | 0 | 0 | 0 | 0 | 3 | 0 | ||||
| Some college | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | ||||
| College | 6 | 7 | 0 | 1 | 2 | 2 | 4 | 4 | ||||
| Some graduate | 3 | 3 | 1 | 2 | 2 | 0 | 0 | 1 | ||||
| Graduate school | 13 | 8 | 3 | 0 | 2 | 2 | 8 | 6 | ||||
| Comorbidities | ||||||||||||
| Arthritis | 12 | 6 | 1.24 | 2 | 2 | .19 | 4 | 0 | 6.00 | 6 | 4 | .00 |
| Hypertension | 9 | 6 | .11 | 1 | 1 | .06 | 2 | 1 | .44 | 6 | 4 | .00 |
| Diabetes | 3 | 2 | .03 | 0 | 0 | n/a | 1 | 1 | .06 | 2 | 1 | .08 |
| Heart disease | 7 | 4 | .30 | 1 | 1 | .06 | 2 | 1 | .44 | 4 | 2 | .18 |
| Depression | 2 | 2 | .08 | 0 | 0 | n/a | 0 | 0 | n/a | 2 | 2 | .17 |
| Anxiety | 2 | 0 | 1.61 | 0 | 0 | n/a | 0 | 0 | n/a | 2 | 0 | 1.49 |
| Insomnia | 0 | 0 | n/a | 0 | 0 | n/a | 0 | 0 | n/a | 0 | 0 | n/a |
| Clinical stage | ||||||||||||
| 1 | 3 | 4 | 1.34 | 0 | 0 | .19 | 1 | 0 | 4.00 | 2 | 4 | 3.10 |
| 2 | 4 | 3 | 3 | 0 | 2 | 1 | 2 | 2 | ||||
| 3 | 3 | 2 | 0 | 1 | 0 | 1 | 1 | 0 | ||||
| 4 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | ||||
| Don’t know | 15 | 11 | 2 | 2 | 2 | 4 | 11 | 5 | ||||
Evaluation of Feasibility and Acceptability
Phase III feasibility metrics achieved >70% in all areas: enrollment rate = 83%, retention = 89%, audio program adherence = 92.5% and 88.5% (mindfulness and music programs, respectively). One mindfulness participant completed the entire program but passively withdrew just prior to the follow up assessments; one music participant dropped out before the program began and another dropped out after the first week. Both groups found the programs to be easy to participate in; get, set up and use the equipment; and hear the audios clearly. Phase III’s mindfulness arm participants reported enjoying participation relatively more than music controls (93% vs 67%, respectively), including looking forward to listening (93% vs 78%, respectively), finding listening helpful (93% vs 89%, respectively), having enough variety (87% vs 78%, respectively), and being affected positively by participation (93% vs 78%, respectively). Both groups reported being willing to recommend this program to someone else at similar rates (87%-89%). Neither group met acceptability criteria of >70% for being interested in staying on the study for a longer duration if permitted (67%).
Patterns of Change in PROs
Most of self-reported outcomes measures (anxiety, depression, fear of recurrence, mindfulness) showed no significant differences between groups over time (see Table 3). However, immediately following the 4-week program, mindfulness participants reported significantly lower uncertainty intolerance compared to music controls (P = .046; F(3, 20) = 4.540; M = 6.73 ± 4.76 [mindfulness]; M = 11.11 ± 7.25 [music]), ES = .95. At the 1-month follow up, these differences became non-significant, however trends remained (P = .502; F (3, 20) = .467; M = 7.13 ± 6.3 [mindfulness]; M = 8.89 ± 7.82 [music]). At the 3-month follow up, mindfulness participants reported significantly lower fatigue (P = .049, F(3, 13) = 4.733; M = 50.05 ± 5.17 [mindfulness]; M = 54.53 ± 4.66 [music]), ES = 1.3, and sleep disturbance (P = .035, F(3, 13) = 5.33; M = 46.93 ± 7.91 [mindfulness]; M = 55.46 ± 5.82 [music]), ES = 1.1, compared with music participants. Effect sizes were large for all 3 outcomes. For PROMIS measures, the mindfulness group demonstrated ≥ 2-point decrease in scores over time (2.65-point decrease in fatigue; 4.5-point decrease in sleep disturbance), suggesting a clinically meaningful improvement. 41 Control group PROMIS Fatigue and Sleep scores worsened by 7.46 and 6.15 points, respectively, moving scores from normal limits to the mild impairment range (Table 4).
Table 3.
Final Phase III Acceptability Ratings.
| Mindfulness (n = 15) (%) | Music (n = 9) (%) | |
|---|---|---|
| Enjoyed participating | 93 | 67 |
| Easy to participate | 100 | 100 |
| Looked forward to listening | 93 | 78 |
| Listening was helpful | 93 | 89 |
| Enough variety | 87 | 78 |
| Easy to get equipment | 93 | 100 |
| Easy to set up & use | 100 | 100 |
| Able to hear clearly | 100 | 100 |
| Participation affected Me positively | 93 | 78 |
| Would like to continue on study longer | 67 | 67 |
| Would recommend to someone | 87 | 89 |
Table 4.
Phase III Means, Standard Deviations, and Confidence Intervals of PROs Over Time.
| Measure | Baseline | 4-Weeks | 1-Month | 3-Months | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mind (n = 16) | Music (n = 11) | CI | P | Mind (n = 15) | Music (n = 9) | CI | P | Mind (N = 15) | Music (N = 9) | CI | P | Mind (N = 15) | Music (N = 9) | CI | P | |
| PROMIS anxiety | 48.22 (9.09) | 47.89 (6.32) | −6.20 to 6.86 | .92 | 45.460 (9.628) | 46.044 (9.102) | 45.68 to 41.78 | .60 | 45.353 (9.591) | 44.811 (7.637) | 41.46 to 48.84 | .63 | 47.293 (10.345) | 47.033 (7.671) | 43.23 to 51.10 | .77 |
| PROMIS depression | 46.38 (6.51) | 45.48 (6.81) | −5.23 to 7.02 | .76 | 44.782 (8.302) | 45.986 (7.580) | 41.36 to 49.14 | .48 | 43.640 (7.582) | 48.757 (3.390) | 42.36 to 49.13 | .09 | 45.940 (7.312) | 47.871 (6.325) | 43.25 to 50.22 | .55 |
| PROMIS sleep disturbance | 51.43 (10.56) | 49.31 (6.30) | −6.20 to 10.44 | .60 | 50.155 (7.970) | 52.286 (6.140) | 47.40 to 54.56 | .29 | 47.770 (9.771) | 51.829 (7.759) | 44.83 to 54.11 | .36 | 46.930 (7.915) | 55.457 (5.819) | 46.24 to 54.64 | .04 |
| PROMIS fatigue | 52.70 (8.61) | 47.07 (6.12) | −1.44 to 12.71 | .11 | 52.036 (11.069) | 48.386 (10.892) | 45.23 to 56.00 | .22 | 48.460 (7.883) | 51.643 (5.616) | 46.21 to 53.44 | .33 | 50.050 (5.175) | 54.529 (4.657) | 49.17 to 54.63 | .05 |
| Uncertainty intolerance | 11.19 (3.62) | 11.0 (5.10) | −3.26 to 3.63 | .91 | 6.733 (4.758) | 11.111 (7.253) | 5.82 to 10.94 | .05 | 7.133 (6.300) | 8.889 (7.817) | 4.92 to 10.66 | .50 | 9.533 (6.323) | 9.222 (6.399) | 6.79 to 12.04 | .89 |
| MAX PC fear of recurrence | 3.00 (2.34) | 3.64 (1.86) | −2.38 to 1.11 | .46 | 1.5333 (1.885) | 3.222 (2.167) | 1.27 to 3.062 | .06 | 1.333 (1.839) | 1.778 (2.108) | .693 to 2.31 | .77 | 2.933 (2.374) | 1.889 (1.965) | 1.59 to 3.49 | .20 |
| Mindful attention and awareness | 68.88 (12.10) | 69.91 (10.41) | −10.27 to 8.21 | .82 | 72.600 (11.438) | 71.556 (13.712) | 67.12 to 77.30 | .90 | 74.200 (13.919) | 74.556 (11.370) | 68.94 to 79.72 | .81 | 73.267 (9.728) | 74.333 (11.023) | 69.44 to 77.89 | .92 |
Note: Bolded P-values of .05, when extended to the thousandth decimal level were .046 (uncertainty intolerance) and .049 (fatigue).
Discussion
This study examined the implementation feasibility and acceptability and initial patterns of PRO change of daily delivery of brief mindfulness and music audio programs to men during RT for PC. Using an implementation pre-testing approach, we identified optimal program delivery timing and content, which began on day one of week 2 of RT for 4 consecutive weeks. Pre-testing different starting times and program lengths suggested it is possible that starting a program like this on the first day of RT may be overwhelming for men, while waiting until the third week might be longer than necessary for men to feel adjusted.
Pre-testing audio program modifications included increasing the diversity of audio selections, giving participants the power to select ones they preferred, adjusting content and word choice for specific meditations given the context, and replacing the mindfulness audios narrated by a female instructor with a male instructor. The request to have a male mindfulness narrator was surprising, as previous mindfulness intervention studies in PC conducted by this team have all primarily utilized female mindfulness instructors without issue. It is possible that since these were all multi-week, in-person, face-to-face interventions outside of the treatment environment that male participants may have been more able to create a personal and trusting relationship with the instructor compared with only hearing a female voice (without the benefit of a relationship) during a private, vulnerable, and stressful treatment experience. Furthermore, listeners may respond more favorably to audio-only recordings that mimic an “inner voice.”
Among the self-reported outcome measures that were administered, uncertainty intolerance, fatigue, and sleep disturbance demonstrated significant differences between groups at 4 weeks (uncertainty intolerance) and 3 months post (fatigue, sleep disturbance), all in favor of the mindfulness condition compared with the music control. Mindfulness practice has demonstrated improvements in these areas in other cancer patient samples,19,42,43 however, to our knowledge, this is the first study to demonstrate improvements from brief, daily audio exposure during the delivery of RT. It is possible that fatigue and sleep disturbance only demonstrated improvements at 3 months due to RT being completed, however it is unclear why this change only occurred in the mindfulness condition and not the music control. The relatively small number of participants in each group is a possible reason.
To our knowledge, this is the first study to deliver a brief mindfulness intervention during actual RT itself, compared to “during treatment” intervention studies that offer supportive therapies or resources outside of the treatment setting. Our pilot findings suggest this may be a suitable time and place upon which to intervene for several reasons. First, men receiving RT for PC must come daily for multiple weeks. They are in many ways, a “captive audience.” While the treatment timeframe is relatively brief, being able to seamlessly “piggyback” a supportive, symptom reduction intervention onto an existing medical treatment is novel and frees up resources, both for busy hospitals, and for patients, who don’t have to attend yet another program in addition to their treatment. In effect, it becomes an efficiently bundled, “one stop shopping” approach that eliminates unnecessary burden during a highly stressful time.
Another benefit of a piggybacked program like this lies in its ease of delivery and passive/receptive nature, both of which may be a draw for older men affected by cancer, who are notorious for not engaging in supportive oncology programming at the same rates as their women counterparts.44-46 While this was not explicitly queried in this study, there may be a preference by some men to receive support individually, and in ways that do not require verbal expression amongst others.
A final advantage of this approach lies in its relative low touch (and thereby low budget) nature, making a program like this accessible and achievable for a wide variety of RT care settings, especially those with less psychosocial support professionals or resources.
This study is not without limitations. Most notably, this study utilized a small, mostly Caucasian sample from a single treatment center. As a result, it may not be possible to generalize these findings to other, more diverse patient groups and settings. This also places limitations on interpreting findings of self-reported outcomes. Even though the diverse selections of intervention content (e.g., different types of mindfulness recordings and different forms of relaxing music, including sounds of nature) was deemed feasible and acceptable by Phase III participants, it is unclear what aspects of these audios may have contributed the most to observed beneficial effects. While initial patterns of change were encouraging for uncertainty intolerance, fatigue, and sleep disturbance, most outcomes tested were non-significant. These preliminary results should be interpreted cautiously given this was not powered as an efficacy trial. Future studies will benefit from larger, more geographically and culturally diverse patient samples.
Overall, the final program tested was feasible and acceptable with some promising preliminary trends that warrant follow up with larger, more geographically and racially diverse populations. Given participant uptake, retention, and overall adherence of the final program, use of guided audio recordings during RT may offer a low-touch support option for a population that otherwise may be less inclined to seek out and utilize supportive care services.
Conclusions
The study described the development, pre-testing, and implementation of audio-based mindfulness and music programs during RT for PC. Optimal program timing and content were identified, with initial improvements in uncertainty intolerance, fatigue, and sleep disturbance over time for mindfulness participants. Brief, audio-based mindfulness may be effective in decreasing RT-related physical and emotional side effects at 4 weeks and several months later.
Footnotes
Author’s Note: The corresponding author has full control of all primary data.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by a grant from the Fagen Family Foundation through the Department of Radiation Oncology at Northwestern University Feinberg School of Medicine. All authors certify they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethical Statement
Ethical Approval
All procedures performed in this study were in accordance with the ethical standards of the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Scientific Research Committee of the Robert H. Lurie Comprehensive Cancer Center and Institutional Research Board at Northwestern University Feinberg School of Medicine.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
ORCID iD
David Victorson https://orcid.org/0000-0002-3530-8633
Data Availability Statement
The dataset generated and/or analyzed are available from the corresponding author on request.*
References
- 1.Berkey FJ. Managing the adverse effects of radiation therapy. Am Fam Physician. 2010;82(4):381-8, 394. [PubMed] [Google Scholar]
- 2.Jereczek-Fossa BA, Santoro L, Alterio D, et al. Fatigue during head-and-neck radiotherapy: prospective study on 117 consecutive patients. Int J Radiat Oncol Biol Phys. 2007;68(2):403-415. doi: 10.1016/j.ijrobp.2007.01.024 [DOI] [PubMed] [Google Scholar]
- 3.Feng LR, Espina A, Saligan LN. Association of fatigue intensification with cognitive impairment during radiation therapy for prostate cancer. Oncology. 2018;94(6):363-372. doi: 10.1159/000487081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jereczek-Fossa BA, Marsiglia HR, Orecchia R. Radiotherapy-related fatigue. Crit Rev Oncol Hematol. 2002;41(3):317-325. [DOI] [PubMed] [Google Scholar]
- 5.Groenvold M, Petersen MA, Idler E, Bjorner JB, Fayers PM, Mouridsen HT. Psychological distress and fatigue predicted recurrence and survival in primary breast cancer patients. Breast Cancer Res Treat. 2007;105(2):209-219. doi: 10.1007/s10549-006-9447-x [DOI] [PubMed] [Google Scholar]
- 6.Kawase E, Karasawa K, Shimotsu S, et al. Estimation of anxiety and depression in patients with early stage breast cancer before and after radiation therapy. Breast Cancer. 2012;19(2):147-152. doi: 10.1007/s12282-010-0220-y [DOI] [PubMed] [Google Scholar]
- 7.Carr E. Rising prostate cancer incidence rates: what can we do about it? Clin J Oncol Nurs. 2023;27(2):109-110. doi: 10.1188/23.CJON.109-110 [DOI] [PubMed] [Google Scholar]
- 8.Garrett K, Dhruva A, Koetters T, et al. Differences in sleep disturbance and fatigue between patients with breast and prostate cancer at the initiation of radiation therapy. J Pain Symptom Manage. 2011;42(2):239-250. doi: 10.1016/j.jpainsymman.2010.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Knapp K, Cooper B, Koetters T, et al. Trajectories and predictors of symptom occurrence, severity, and distress in prostate cancer patients undergoing radiation therapy. J Pain Symptom Manage. 2012;44(4):486-507. doi: 10.1016/j.jpainsymman.2011.10.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miaskowski C, Paul SM, Cooper BA, et al. Predictors of the trajectories of self-reported sleep disturbance in men with prostate cancer during and following radiation therapy. Sleep. 2011;34(2):171-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mohamed NE, Bovbjerg DH, Montgomery GH, Hall SJ, Diefenbach MA. Pretreatment depressive symptoms and treatment modality predict post-treatment disease-specific quality of life among patients with localized prostate cancer. Urol Oncol. 2012;30(6):804-812. doi: 10.1016/j.urolonc.2011.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lengacher CA, Johnson-Mallard V, Barta M, et al. Feasibility of a mindfulness-based stress reduction program for early-stage breast cancer survivors. J Holist Nurs. 2011;29(2):107-117. doi: 10.1177/0898010110385938 [DOI] [PubMed] [Google Scholar]
- 13.Lengacher CA, Johnson-Mallard V, Post-White J, et al. Randomized controlled trial of mindfulness-based stress reduction (MBSR) for survivors of breast cancer. Psycho Oncol. 2009;18(12):1261-1272. doi: 10.1002/pon.1529 [DOI] [PubMed] [Google Scholar]
- 14.Gross CR, Kreitzer MJ, Reilly-Spong M, et al. Mindfulness-based stress reduction versus pharmacotherapy for chronic primary insomnia: a randomized controlled clinical trial. Explore (NY). 2011;7(2):76-87. doi: 10.1016/j.explore.2010.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li J, Li C, Puts M, et al. Effectiveness of mindfulness-based interventions on anxiety, depression, and fatigue in people with lung cancer: a systematic review and meta-analysis. Int J Nurs Stud. 2023;140:104447. doi: 10.1016/j.ijnurstu.2023.104447 [DOI] [PubMed] [Google Scholar]
- 16.McCloy K, Hughes C, Dunwoody L, Marley J, Gracey J. Effects of mindfulness-based interventions on fatigue and psychological wellbeing in women with cancer: a systematic review and meta-analysis of randomised control trials. Psycho Oncol. 2022;31(11):1821-1834. doi: 10.1002/pon.6046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johns SA, Tarver WL, Secinti E, et al. Effects of mindfulness-based interventions on fatigue in cancer survivors: a systematic review and meta-analysis of randomized controlled trials. Crit Rev Oncol Hematol. 2021;160:103290. doi: 10.1016/j.critrevonc.2021.103290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xie C, Dong B, Wang L, et al. Mindfulness-based stress reduction can alleviate cancer- related fatigue: a meta-analysis. J Psychosom Res. 2020;130:109916. doi: 10.1016/j.jpsychores.2019.109916 [DOI] [PubMed] [Google Scholar]
- 19.Johns SA, Brown LF, Beck-Coon K, Monahan PO, Tong Y, Kroenke K. Randomized controlled pilot study of mindfulness-based stress reduction for persistently fatigued cancer survivors. Psycho Oncol. 2015;24(8):885-893. doi: 10.1002/pon.3648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. New York, NY: Random House Publishing Group; 1990. [Google Scholar]
- 21.Bishop SR, Lau M, Shapiro S, et al. Mindfulness: a proposed operational definition. Clin Psychol Sci Pract. 2004;11(3):230-241. doi: 10.1093/clipsy.bph077 [DOI] [Google Scholar]
- 22.Hülsheger UR, Alberts HJ, Feinholdt A, Lang JW. Benefits of mindfulness at work: the role of mindfulness in emotion regulation, emotional exhaustion, and job satisfaction. J Appl Psychol. 2013;98(2):310-325. doi: 10.1037/a0031313 [DOI] [PubMed] [Google Scholar]
- 23.Guendelman S, Medeiros S, Rampes H. Mindfulness and emotion regulation: insights from neurobiological, psychological, and clinical studies. Front Psychol. 2017;8:220. doi: 10.3389/fpsyg.2017.00220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chiesa A, Serretti A, Jakobsen JC. Mindfulness: top-down or bottom-up emotion regulation strategy? Clin Psychol Rev. 2013;33(1):82-96. doi: 10.1016/j.cpr.2012.10.006 [DOI] [PubMed] [Google Scholar]
- 25.Fan J, Li W, Lin M, Li X, Deng X. Effects of mindfulness and fatigue on emotional processing: an event-related potentials study. Front Behav Neurosci. 2023:17:1175067. doi: 10.3389/fnbeh.2023.1175067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lau WKW, Leung MK, Wing YK, Lee TMC. Potential Mechanisms of mindfulness in improving sleep and distress. Mindfulness (NY). 2018;9(2):547-555. doi: 10.1007/s12671-017-0796-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Victorson D, Kentor M, Maletich C, et al. A systematic review and meta-analysis of mindfulness-based randomized controlled trials relevant to lifestyle medicine. Am J Lifestyle Med. 2015;9(3):185-211. [Google Scholar]
- 28.Kumar P, Casarett D, Corcoran A, et al. Utilization of supportive and palliative care services among oncology outpatients at one academic cancer center: determinants of use and barriers to access. J Palliat Med. 2012;15(8):923-930. doi: 10.1089/jpm.2011.0217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Atreya CE, Kubo A, Borno HT, et al. Being present: a single-arm feasibility study of audio-based mindfulness meditation for colorectal cancer patients and caregivers. PLoS One. 2018;13(7):e0199423. doi: 10.1371/journal.pone.0199423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Altschuler A, Rosenbaum E, Gordon P, Canales S, Avins AL. Audio recordings of mindfulness-based stress reduction training to improve cancer patients’ mood and quality of life—a pilot feasibility study. Support Care Cancer. 2012;20(6):1291-1297. doi: 10.1007/s00520-011-1216-7 [DOI] [PubMed] [Google Scholar]
- 31.Thaut MH, Davis WB. The influence of subject-selected versus experimenter-chosen music on affect, anxiety, and relaxation. J Music Ther. 1993;30(4):210-223. doi: 10.1093/jmt/30.4.210 [DOI] [Google Scholar]
- 32.Tan XL, Yowler CJ, Super DM, Fratianne RB. The interplay of preference, familiarity and psychophysical properties in defining relaxation music. J Music Ther. 2012;49(2):150-179. doi: 10.1093/jmt/49.2.150 [DOI] [PubMed] [Google Scholar]
- 33.Strauser JM. The effects of music versus silence on measures of state anxiety, perceived relaxation, and physiological responses of patients receiving chiropractic interventions. J Music Ther. 1997;34(2):88-105. doi: 10.1093/jmt/34.2.88 [DOI] [Google Scholar]
- 34.Bernardi L, Porta C, Sleight P. Cardiovascular, cerebrovascular, and respiratory changes induced by different types of music in musicians and non-musicians: the importance of silence. Heart. 2006;92(4):445-452. doi: 10.1136/hrt.2005.064600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry. 2000;31(2):73-86. Not in File. [DOI] [PubMed] [Google Scholar]
- 36.Cella D, Yount S, Rothrock N, et al. The patient-reported outcomes measurement information system (PROMIS): progress of an NIH Roadmap cooperative group during its first two years. Med Care. 2007;45(5 Suppl 1):S3-S11. doi: 10.1097/01.mlr.0000258615.42478.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Roth AJ, Rosenfeld B, Kornblith AB, et al. The memorial anxiety scale for prostate cancer: validation of a new scale to measure anxiety in men with with prostate cancer. Cancer. 2003;97(11):2910-2918. doi: 10.1002/cncr.11386 [DOI] [PubMed] [Google Scholar]
- 38.Carleton RN, Norton MA, Asmundson GJ. Fearing the unknown: a short version of the intolerance of uncertainty scale. J Anxiety Disord. 2007;21(1):105-117. Not in File. [DOI] [PubMed] [Google Scholar]
- 39.Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84(4):822-848. [DOI] [PubMed] [Google Scholar]
- 40.Morris SB. Estimating effect sizes from pretest-posttest-control group designs. Organ Res Methods. 2008;11(2):364-386. doi: 10.1177/1094428106291059 [DOI] [Google Scholar]
- 41.Katz P, Pedro S, Alemao E, et al. Estimates of responsiveness, minimally important differences, and patient acceptable symptom state in five patient-reported outcomes measurement information system short forms in systemic lupus erythematosus. ACR Open Rheumatol. 2020;2(1):53-60. doi: 10.1002/acr2.11100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Victorson D, Hankin V, Burns J, et al. Feasibility, acceptability and preliminary psychological benefits of mindfulness meditation training in a sample of men diagnosed with prostate cancer on active surveillance: results from a randomized controlled pilot trial. Psycho Oncol. 2016;26:1155. doi: 10.1002/pon.4135 [DOI] [PubMed] [Google Scholar]
- 43.Lengacher CA, Reich RR, Paterson CL, et al. The effects of mindfulness-based stress reduction on objective and subjective sleep parameters in women with breast cancer: a randomized controlled trial. Psycho Oncol. 2015;24(4):424-432. doi: 10.1002/pon.3603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wenger LM, Oliffe JL. Men managing cancer: a gender analysis. Sociol Health Illn. 2014;36(1):108-122. doi: 10.1111/1467-9566.12045 [DOI] [PubMed] [Google Scholar]
- 45.Johnson JL, Oliffe JL, Kelly MT, Galdas P, Ogrodniczuk JS. Men’s discourses of help-seeking in the context of depression. Sociol Health Illn. 2012;34(3):345-361. doi: 10.1111/j.1467-9566.2011.01372.x [DOI] [PubMed] [Google Scholar]
- 46.Martopullo C, Oberoi D, Levin G, et al. “In the same boat”-a mixed-methods exploration of reasons why male gastrointestinal cancer patients joined a professionally led men-only cancer support group. J Cancer Surviv. 2020;14(3):261-272. doi: 10.1007/s11764-019-00838-x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset generated and/or analyzed are available from the corresponding author on request.*