Abstract
This study aimed to investigate the incidence and clinical characteristics of acute primary angle closure (APAC) during the Coronavirus Disease 2019 (COVID-19) pandemic in China. This was a retrospective study of patients diagnosed with APAC in a glaucoma clinic over a 5-year period. We compared the number of APAC cases during the COVID-19 outbreak (December 7, 2022 to January 7, 2023) with those during the same period in previous years and 2 months prior to the outbreak. We also collected data on the demographic and clinical features of APAC patients, such as age, sex, disease course, visual acuity, intraocular pressure (IOP), and lens opacity. We included 95 eyes of 88 patients with APAC were included. Of these, 65 were female and 23 were male. The mean age was 68.0 ± 8.1 years. The median disease course was 10.8 ± 9.5 days. There was a significant increase in the number of APAC cases during the COVID-19 outbreak compared with the same months over a 5-year period (44 vs 51, P < .001). A higher proportion of women developed APAC during the outbreak period than during the non-outbreak period (P < .001). Eyes with APAC in the outbreak period had a lower mean IOP than those in the preceding 6 months (40.5 ± 8.8 mm Hg vs 46.1 ± 10.1 mm Hg; P = .043). No significant differences were observed in disease duration, lens opacity, or bilateral or unilateral onset between the 2 groups. Our study suggests a potential correlation between APAC and COVID-19, marked by a significant surge in APAC cases concurrent with the COVID-19 outbreak. However, the underlying mechanisms and preventive strategies remain to be elucidated.
Keywords: acute primary angle closure, angiotensin-converting enzyme 2 receptor, COVID-19 outbreak, incidence, retrospective cohort study
1. Introduction
The novel coronavirus, responsible for the outbreak of Coronavirus Disease 2019 (COVID-19), has escalated into a global pandemic, impacting millions worldwide.[1,2] The initial cases were identified in Wuhan, China, in December 2019, and the virus has proliferated rapidly to other regions within China and globally.[3] Consequently, COVID-19 has emerged as a significant public health issue, affecting various body organs, including the eyes. Recent research indicates that COVID-19 may also present ocular risks such as conjunctivitis,[4,5] uveitis,[6] and retinopathy.[7,8] Specifically, the potential association between COVID-19 and acute primary angle closure (APAC) glaucoma is of significant concern due to the urgent nature of APAC and its potential to cause irreversible vision loss. Exploring the connection between COVID-19 and APAC presents unique challenges, such as the variability in COVID-19 symptomatology and the difficulty in conducting comprehensive eye examinations during pandemic conditions.
APAC is a variant of glaucoma, characterized by acute blockage of the trabecular meshwork by the peripheral iris, leading to an elevation in intraocular pressure (IOP) and subsequent damage to the optic nerve.[9,10] This condition predominantly affects individuals with a narrow anterior chamber angle and can be precipitated by pupillary dilation, such as in low-light conditions or following the administration of mydriatic agents. APAC can present with a range of symptoms, including ocular pain, redness, blurred vision, halos around lights, headache, nausea, and vomiting.[11] If not promptly managed, APAC can culminate in permanent vision loss. The potential association between COVID-19 and APAC has recently attracted considerable attention. Following the “Jing Shi Tiao” policy implementation on December 7, 2022, which eased COVID-19 restrictions, there was a subsequent outbreak of COVID-19 in December 2022. We also observed a significant surge in the number of APAC cases. However, the precise mechanism by which the virus precipitates APAC remains elusive. This observation underscores the need for further investigation into the potential impact of the pandemic on ocular health and its underlying mechanisms.
While previous case reports and studies have explored the occurrence of APAC attacks during the COVID-19 pandemic, most of them were based on a small number of cases or focused on the clinical characteristics of APAC during lockdown.[12–15] However, the potential risk factors and clinical characteristics of APAC patients during a COVID-19 outbreak without lockdown remain unexplored. Our investigation assumes that the systemic inflammation and vascular abnormalities associated with COVID-19 may contribute to the pathophysiology of APAC, either by exacerbating preexisting conditions or by initiating new pathogenic processes in the eye. The objective of this retrospective analysis was to juxtapose the number of APAC cases during the COVID-19 outbreak with those during the corresponding period in previous years and to probe into the potential reasons for the surge in APAC cases during the COVID-19 outbreak. By shedding light on the relationship between COVID-19 and APAC, ophthalmologists and healthcare professionals can provide better care for patients with COVID-19 and prevent vision loss due to APAC.
2. Materials and methods
This retrospective study was approved by the Ethics Review Board of Peking University People Hospital, and the procedures were conducted in accordance with institutional guidelines and the Declaration of Helsinki. Informed consent was obtained from all patients after a comprehensive explanation of the procedures. Patients diagnosed with APAC were recruited from the glaucoma clinic of our hospital over a span of 5 years. For this study, we included patients with APAC during a nonconsecutive 7-month period, encompassing the following time frames: December 7, 2022, to January 7, 2023 (coinciding with the release of the “Jing Shi Tiao” policy on December 7, 2022, which relaxed COVID-19 restrictions); November 7, 2022, to December 7, 2022; October 7, 2022, to November 7, 2022; and the same period from December 7 to January 7 for the years 2018 to 2022. The patients were divided into 2 categories: the first included individuals who experienced acute attacks during the COVID-19 outbreak, while the second group comprised those with acute attacks during non-COVID-19 outbreak periods and served as the control group. All patients in the former group tested positive for the COVID-19 virus nucleic acid, whereas those in the latter group tested negative. This approach facilitated a comparison of the incidence of APAC during the COVID-19 outbreak with that of the same period in preceding years, as well as with the incidence during the 2 months prior to the outbreak.
Data for this study were systematically extracted from the hospital electronic health record system, following the hospital permission. The extraction process involved querying the electronic health record database for specific diagnostic codes related to APAC (e.g., ICD-10 code for APAC), along with patient demographics, symptom onset dates, diagnosis dates, and initial treatment details. Given that patients with APAC require either laser or filtration surgery, traceable records are available, enabling us to conduct a reliable and verifiable incidence study. The raw dataset underwent rigorous pre-processing to ensure data quality and consistency. This included the removal of duplicate records and normalization of data fields to a standard format. Patient identifiers were anonymized to maintain confidentiality. Furthermore, a manual review was conducted to validate the accuracy of APAC diagnoses by cross-referencing clinical notes and diagnostic test results. All steps in the processing workflow, from data extraction to statistical analysis, were documented in a reproducible manner, ensuring transparency and replicability of the study findings.
According to the International Society of Geography and Epidemiology of Ophthalmology classification system, the diagnosis of APAC was based on specific criteria. These included the absence of a history of glaucoma and the presence of at least 2 of the following symptoms: headache, ocular or periocular pain, nausea and vomiting, and blurred vision accompanied by light halos. Additionally, the patient had an IOP exceeding 30 mm Hg and a shallow anterior chamber, along with at least 3 of the following ophthalmologic signs: conjunctival hyperemia, corneal epithelial edema, keratic precipitates, glaucomatous fleck, iris atrophy, iris bombe, and mid-dilated pupil with or without glaucomatous optic neuropathy or visual field defect. For this study, we collected patient data encompassing a range of pertinent information, such as age, sex, disease course, best-corrected visual acuity (VA), IOP, medication history, degree of lens opacification based on the Lens Opacity Classification System III, and ultrasound biomicroscopy.
The data obtained in this study were analyzed using SPSS software (version 22.0; SPSS, Inc., Chicago, IL). Descriptive statistics, such as mean ± standard deviation, were computed for all variables. The Kolmogorov-Smirnov test was employed to evaluate the normality of the data distribution, revealing that certain quantitative parameters (age and best-corrected VA) adhered to a normal distribution. Therefore, parametric tests (Student t test) were used for normally distributed data, while nonparametric tests (Mann-Whitney test) were applied to data that did not conform to a normal distribution. Fisher exact test was used to assess the relationship between sex, bilateral onset, and occurrence of an acute attack during the outbreak. A P value <.05 was considered indicative of a statistically significant difference.
3. Results
This study included 95 eyes from 88 patients with APAC. Of these, 65 were female and 23 were male. The mean age was 68.0 ± 8.1 years (range, 46–89 years). The median disease course was 10.8 ± 9.5 days (range, 1–30 days).
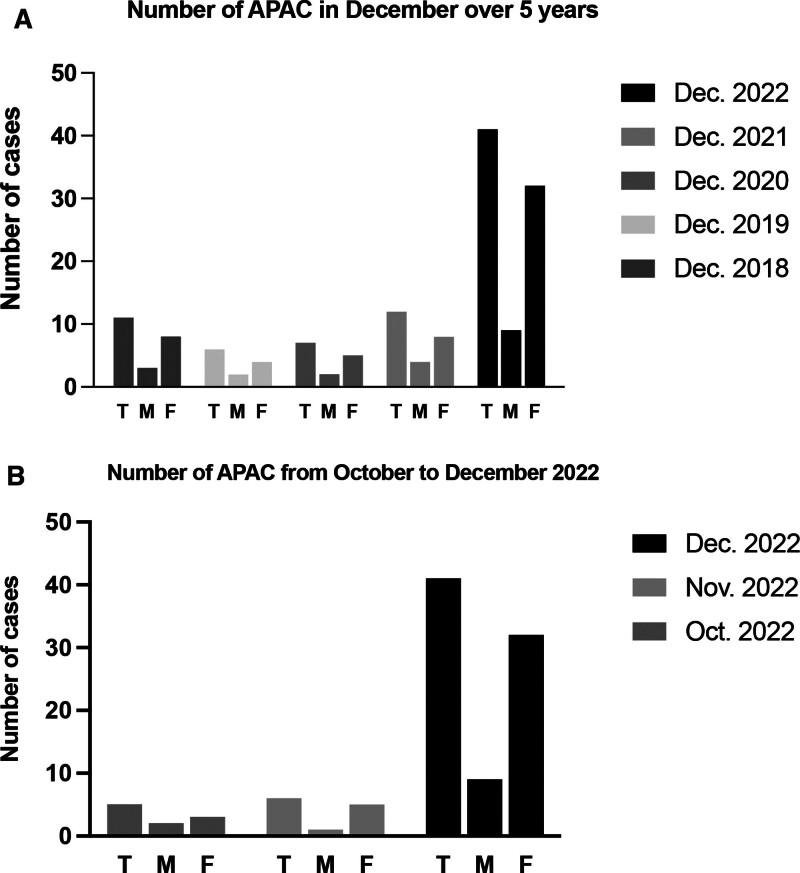
We observed a significant increase in the number of APAC cases during the COVID-19 outbreak compared with the same months over a 5-year period. Specifically, there were 44 cases of APAC during the outbreak period, compared to 51 cases during the other 6 months. Seven patients had bilateral attacks: 3 (7.3%) during the outbreak and 4 (8.5%) during the non-outbreak period. The number of acute attacks in each period is shown in Figure 1. Among the 44 eyes during the COVID-19 outbreak period, 6 patients had no clear association between COVID-19 infection and the onset of APAC, while the remaining 38 patients developed APAC after testing positive for the virus, with an average interval of 2 days. Additionally, 38 patients were administered antipyretic drugs, including ibuprofen and paracetamol. Three patients developed APAC after taking antipyretic agents and reducing fever, whereas the other 35 eyes developed APAC during the febrile phase.
Figure 1.
Comparison of the number of acute primary angle closure (APAC) cases during the COVID-19 outbreak and the same period in previous years over a 5-yr period, specifically during nonconsecutive 7 mo. (A) Number of APAC cases during the COVID-19 outbreak compared to the same period in previous years. (B) Number of APAC cases during the COVID-19 outbreak and 2 mo prior to the outbreak. T, total; M, male; F, female. COVID-19 = coronavirus disease 2019.
Regarding clinical characteristics, a significantly higher proportion of women developed APAC during the COVID-19 outbreak than during the non-outbreak periods (P < .001). Furthermore, eyes with APAC in the outbreak period had a lower mean IOP than those in the preceding 6 months (40.5 ± 8.8 mm Hg vs 46.1 ± 10.1 mm Hg; P = .043). Additionally, patients in the outbreak period had better VA than those in the preceding 6 months, although the difference was not statistically significant (0.14 ± 0.18 vs 0.07 ± 0.12, P = .059). No significant differences were observed in sex, disease duration, lens opacity, or bilateral or unilateral onset (P > .05) between the 2 groups (Table 1).
Table 1.
Comparison of demographic and clinical characteristics between the 2 groups.
| Acute attacks during the COVID-19 outbreak | Acute attacks during the non-COVID-19 outbreak periods | P value | |
|---|---|---|---|
| Patients/Eyes | 41/44 | 47/51 | - |
| Gender (M/F) | 9/32 | 14/33 | <.001 |
| Age (yr) | 68.8 ± 7.1 | 67.4 ± 8.9 | .417 |
| Disease course (d) | 12.5 ± 9.2 | 9.4 ± 9.5 | .091 |
| Bilateral onset/total | 3/41 | 4/47 | 1.000 |
| BCVA (decimal) | 0.14 ± 0.07 | 0.07 ± 0.12 | .059 |
| IOP (mm Hg) | 40.5 ± 8.8 | 46.1 ± 10.1 | .043 |
| Degree of lens opacification (LOCSIII) | 2.5 ± 0.5 | 2.7 ± 0.8 | .478 |
BCVA = best-corrected visual acuity, COVID-19 = coronavirus disease 2019, F = female, IOP = intraocular pressure, LOCSIII = lens opacity classification system III, M = male.
4. Discussion
The current study observed a notable surge in the incidence of APAC concurrent with the COVID-19 outbreak. To mitigate the potential influence of seasonal variations on APAC incidence,[16] we collected data from the same month across a 5-year span. When compared to the corresponding period in the preceding years and 2 months prior to the COVID-19 outbreak, the incidence of APAC during the outbreak was significantly elevated. Interestingly, the initial IOP was lower and VA improved during the outbreak. These observations suggest a unique impact of the COVID-19 outbreak on APAC, warranting further exploration to elucidate its underlying mechanisms.
Zhou et al conducted a comparative analysis of APAC cases during the COVID-19 lockdown period and the corresponding period in the subsequent year.[14] Their study revealed that during the lockdown, patients experienced a prolonged duration from symptom onset to treatment initiation and presented with elevated IOP. In contrast, our investigation did not identify a significant variation in the disease course between the 2 cohorts. This divergence could be attributed to the fact that Zhou et al study was conducted during the lockdown, a period when patients might have postponed seeking medical care, whereas our study was devoid of the confounding influence of the lockdown. Our research encompassed non-COVID-19 outbreak periods, including the pre-epidemic and epidemic phases, without breakout. Furthermore, our study spanned a more extensive period of over 5 years, offering a more holistic view compared to the previous study, which was confined to a relatively short period. Interestingly, our study demonstrated that APAC cases during the outbreak period had a lower mean IOP, a finding that contradicts that of previous research. We postulated that the observed discrepancy in IOP could be associated with varying viral infections that influence aqueous humor secretion or the time interval from symptom onset to treatment initiation.
Our previous research has reported a higher prevalence of APAC in women than in men, with a female-to-male ratio of 70.7% to 29.3%.[16] In this study, we observed an increased incidence of APAC in women during the pandemic period (female-to-male ratio of 78.0% to 22.0%) compared to non-pandemic periods (female-to-male ratio of 70.2% to 29.8%). This trend could be attributed to the heightened susceptibility of women to stress and anxiety during the COVID-19 pandemic,[17] which may trigger sympathetic arousal, pupil dilation, and angle closure. This hypothesis requires further investigation to confirm these findings.
The surge in APAC cases during the COVID-19 outbreak is likely attributable to the complex interplay between multiple factors. One potential contributor is the psychological stress induced by the COVID-19 outbreak,[18] which can trigger increased sympathetic activity, leading to pupil dilation and, subsequently, elevated IOP. This hypothesis is supported by a study conducted by Park et al, which found that university students exhibited higher IOP during examination periods compared to non-examination periods, underscoring the potential role of psychological stress in elevating IOP.[19] Further evidence comes from a study by Kong et al, which revealed that patients with PACG had higher anxiety and depression scores than those with primary open-angle glaucoma and normal controls. Notably, these scores were positively correlated with IOP.[20]
Beyond mydriatic eye drops, a range of medications typically employed for the management of cold and allergy symptoms have been implicated in pupil dilation, potentially precipitating acute APAC. These medications included antitussives, nasal decongestants, promethazine compound linctus, diphenhydramine compound linctus, identified syrup (comprising pseudoephedrine and triprolidine), chlorpheniramine, and a variety of antihistamines.[13,15] In our study, 38 eyes were administered antipyretic drugs, including ibuprofen and paracetamol, which may have played a role in triggering APAC. Additionally, recent literature indicates that COVID-19 vaccinations may precipitate APAC in certain individuals, although the underlying mechanisms remain elusive. Post-vaccination swelling of the ciliary body resulting in zonule laxity and subsequent phacodonesis has been proposed as a potential cause.[21]
Finally, we propose a novel hypothesis to elucidate the potential mechanisms linking COVID-19 to the onset of APAC. The receptors angiotensin-converting enzyme 2 (ACE2) and transmembrane protease serine 2 (TMPRSS2) are pivotal for COVID-19 infection, as they facilitate the entry of the virus into host cells.[22,23] ACE2 and TMPRSS2 have been identified in postmortem human eye specimens, notably in the superficial conjunctival and corneal epithelial surfaces, as well as in endothelial cells. Recent studies by Luhtala et al and Martin et al have demonstrated ACE2 activity in the ciliary and iris stroma.[24,25] It is possible that COVID-19 infection could affect the function of the ciliary body, leading to changes in iris thickness, ciliary body volume, and anterior rotation of the ciliary body, all of which could contribute to the development of APAC. However, more in-depth research is required to confirm this hypothesis.
This study had several limitations that should be considered. First, our analysis was confined to a significant uptick in APAC cases during the COVID-19 outbreak, with no data procured from other regions within China or internationally. It is crucial to acknowledge that our study was retrospective, potentially introducing inherent biases in the data collection and analysis. Detailed information on the presence of uveitis and trabeculitis, as well as the administration of high-dose systemic steroids, was not consistently recorded, which could play a significant role in the pathogenesis of glaucoma in the context of COVID-19 infection. Moreover, the study was unable to ascertain the relationship between ACE2, TMPRSS2 receptors, and APAC attacks given the absence of blood, intraocular fluid, or intraocular tissue samples for analysis. Further in vitro experiments and animal studies are required to validate the potential associations between these factors. Larger multicenter prospective trials are warranted for more robust evidence.
In conclusion, this study highlights a significant association between APAC and COVID-19, marked by a significant surge in APAC cases concurrent with the COVID-19 outbreak. Our findings underscore the critical importance of incorporating ocular health assessments into the standard care protocol for COVID-19 patients, particularly those with known risk factors for glaucoma. We advocate for healthcare systems to establish protocols that ensure the prompt referral of such at-risk individuals to ophthalmology services amidst pandemic conditions. While our research proposes potential mechanisms behind this association, further investigations are imperative to decipher the underlying mechanisms and validate the initial hypothesis. Future research should aim to elucidate the mechanism underlying the observed correlation between COVID-19 and APAC and devise effective preventive strategies to mitigate the risk of APAC in susceptible individuals. For instance, prospective cohort studies may be instrumental in investigating the relationship between COVID-19 and APAC. Moreover, delving into the potential roles of ACE2 receptors and TMPRSS2 in the pathogenesis of APAC may yield novel insights into the management of this condition.
Acknowledgments
The authors wish to thank the study participants for their contribution to the research as well as the current and past investigators and staff. The authors declare no conflict of interest.
Author contributions
Conceptualization: Huijuan Wu.
Data curation: Zhiqiao Liang, Huijuan Wu.
Formal analysis: Zhiqiao Liang, Huijuan Wu.
Funding acquisition: Huijuan Wu.
Investigation: Xianru Hou, Yong Liang, Yongzhen Bao, Huijuan Wu.
Methodology: Zhiqiao Liang, Kangyi Yang, Kun Lv, Yao Ma, Huijuan Wu.
Supervision: Xianru Hou, Yong Liang, Yongzhen Bao, Huijuan Wu.
Writing – original draft: Zhiqiao Liang.
Writing – review & editing: Huijuan Wu.
Abbreviations:
- ACE2
- angiotensin-converting enzyme 2
- APAC
- acute primary angle closure
- COVID-19
- coronavirus disease 2019
- IOP
- intraocular pressure
- TMPRSS2
- transmembrane protease serine 2
- VA
- visual acuity
This study was supported by the Program of Development and Cultivation of Innovative Medical Varieties and Industrial Support, Beijing Municipal Science and Technology Commission [Z191100007619045], and the National Natural Science Foundation of China [61634006], and the Central Guidance on Local Science and Technology Development Fund [2022ZY0026]. The sponsor or funding organization had no role in the design or conduct of this study.
Ethical approval for this study was obtained from the Ethics Review Board of our hospital, and the procedures were conducted in accordance with institutional guidelines and the Declaration of Helsinki. All participants provided written informed consent before their inclusion in the study. Confidence and anonymity were ensured throughout the study, and all data were collected and stored in accordance with IRB guidelines.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
How to cite this article: Liang Z, Yang K, Lv K, Ma Y, Hou X, Liang Y, Bao Y, Wu H. Increased incidence of acute primary angle closure during the COVID-19 outbreak in China: A retrospective analysis. Medicine 2024;103:18(e38030).
Contributor Information
Zhiqiao Liang, Email: drtytyty@126.com.
Kangyi Yang, Email: kangyi1225@163.com.
Kun Lv, Email: 1398311236@qq.com.
Yao Ma, Email: seu_mayao@163.com.
Xianru Hou, Email: drxxlxxl@126.com.
Yong Liang, Email: drtytyty@126.com.
Yongzhen Bao, Email: drlhylhy@126.com.
References
- [1].Atzrodt CL, Maknojia I, McCarthy RDP, et al. A guide to COVID-19: a global pandemic caused by the novel coronavirus SARS-CoV-2. FEBS J. 2020;287:3633–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Rudrapal M, Khairnar SJ, Borse LB, et al. Coronavirus Disease-2019 (COVID-19): an updated review. Drug Res (Stuttg). 2020;70:389–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Zhu H, Wei L, Niu P. The novel coronavirus outbreak in Wuhan, China. Glob Health Res Policy. 2020;5:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Binotti W, Hamrah P. COVID-19-related conjunctivitis review: clinical features and management. Ocul Immunol Inflamm. 2022;31:778–84. [DOI] [PubMed] [Google Scholar]
- [5].Güemes-Villahoz N, Burgos-Blasco B, García-Feijoó J, et al. Conjunctivitis in COVID-19 patients: frequency and clinical presentation. Graefes Arch Clin Exp Ophthalmol. 2020;258:2501–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Ferrand N, Accorinti M, Agarwal M, et al. COVID-19 vaccination and uveitis: epidemiology, clinical features and visual prognosis. Ocul Immunol Inflamm. 2022;30:1265–73. [DOI] [PubMed] [Google Scholar]
- [7].Teo KY, Invernizzi A, Staurenghi G, et al. COVID-19-related retinal micro-vasculopathy - a review of current evidence. Am J Ophthalmol. 2022;235:98–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Gascon P, Briantais A, Bertrand E, et al. Covid-19-associated retinopathy: a case report. Ocul Immunol Inflamm. 2020;28:1293–7. [DOI] [PubMed] [Google Scholar]
- [9].Sun X, Dai Y, Chen Y, et al. Primary angle closure glaucoma: what we know and what we don’t know. Prog Retin Eye Res. 2017;57:26–45. [DOI] [PubMed] [Google Scholar]
- [10].You S, Liang Z, Yang K, et al. Novel discoveries of anterior segment parameters in fellow eyes of acute primary angle closure and chronic primary angle closure glaucoma. Invest Ophthalmol Vis Sci. 2021;62:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Razeghinejad MR, Myers JS. Contemporary approach to the diagnosis and management of primary angle-closure disease. Surv Ophthalmol. 2018;63:754–68. [DOI] [PubMed] [Google Scholar]
- [12].Özmen S, Özkan Aksoy N, Çakir B, et al. Acute angle-closure glaucoma concurrent with COVID-19 infection; case report. Eur J Ophthalmol. 2022;33:NP42–5. [DOI] [PubMed] [Google Scholar]
- [13].Barosco G, Morbio R, Chemello F, et al. Bilateral angle-closure during hospitalization for coronavirus disease-19 (COVID-19): a case report. Eur J Ophthalmol. 2022;32:NP75–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Zhou L, Wu S, Wang Y, et al. Clinical presentation of acute primary angle closure during the COVID-19 epidemic lockdown. Front Med (Lausanne). 2022;9:1078237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Au SCL. From acute angle-closure to COVID-19 during Omicron outbreak. Vis J Emerg Med. 2022;29:101514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Zhu J, Xu Y, Wang H, et al. The seasonality of acute attack of primary angle-closure glaucoma in Beijing, China. Sci Rep. 2018;8:4036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Sandanger I, Nygård JF, Sørensen T, et al. Is women’s mental health more susceptible than men’s to the influence of surrounding stress? Soc Psychiatry Psychiatr Epidemiol. 2004;39:177–84. [DOI] [PubMed] [Google Scholar]
- [18].Violant-Holz V, Gallego-Jiménez MG, González-González CS, et al. Psychological health and physical activity levels during the COVID-19 pandemic: a systematic review. Int J Environ Res Public Health. 2020;17:9419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Jiménez R, Vera J. Effect of examination stress on intraocular pressure in university students. Appl Ergon. 2018;67:252–8. [DOI] [PubMed] [Google Scholar]
- [20].Kong X, Yan M, Sun X, et al. Anxiety and depression are more prevalent in primary angle closure glaucoma than in primary open-angle glaucoma. J Glaucoma. 2015;24:e57–63. [DOI] [PubMed] [Google Scholar]
- [21].Ichhpujani P, Parmar UPS, Duggal S, et al. COVID-19 Vaccine-associated ocular adverse effects: an overview. Vaccines (Basel). 2022;10:1879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Collin J, Queen R, Zerti D, et al. Co-expression of SARS-CoV-2 entry genes in the superficial adult human conjunctival, limbal and corneal epithelium suggests an additional route of entry via the ocular surface. Ocul Surf. 2021;19:190–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Sungnak W, Huang N, Bécavin C, et al. SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat Med. 2020;26:681–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Luhtala S, Vaajanen A, Oksala O, et al. Activities of angiotensin-converting enzymes ACE1 and ACE2 and inhibition by bioactive peptides in porcine ocular tissues. J Ocul Pharmacol Ther. 2009;25:23–8. [DOI] [PubMed] [Google Scholar]
- [25].Martin G, Wolf J, Lapp T, et al. Viral S protein histochemistry reveals few potential SARS-CoV-2 entry sites in human ocular tissues. Sci Rep. 2021;11:19140. [DOI] [PMC free article] [PubMed] [Google Scholar]