Abstract
Pancreatic ductal adenocarcinoma (PDAC) has a poor prognosis owing to its desmoplastic stroma. Therefore, therapeutic strategies targeting this tumor stroma should be developed. In this study, we describe the heterogeneity of cancer-associated fibroblasts (CAFs) and their diverse roles in the progression, immune evasion, and resistance to treatment of PDAC. We subclassified the spatial distribution and functional activity of CAFs to highlight their effects on prognosis and drug delivery. Extracellular matrix components such as collagen and hyaluronan are described for their roles in tumor behavior and treatment outcomes, implying their potential as therapeutic targets. We also discussed the roles of extracellular matrix (ECM) including matrix metalloproteinases and tissue inhibitors in PDAC progression. Finally, we explored the role of the adaptive and innate immune systems in shaping the PDAC microenvironment and potential therapeutic strategies, with a focus on immune cell subsets, cytokines, and immunosuppressive mechanisms. These insights provide a comprehensive understanding of PDAC and pave the way for the development of prognostic markers and therapeutic interventions.
Keywords: Pancreatic cancer, Stroma, Cancer-associated fibroblast, Extracellular matrix, Immune cells
INTRODUCTION
Pancreatic ductal adenocarcinoma (PDAC) is the most common form of pancreatic cancer and accounts for approximately 85% of all pancreatic cancers (Ryan et al., 2014). Arising from the pancreatic ductal cells, this aggressive malignancy is often characterized by a late-stage diagnosis and resistance to conventional therapies (Vincent et al., 2011). The molecular and cellular basis and clinical significance of PDAC have made it a subject of considerable research interest (Maitra and Hruban, 2008).
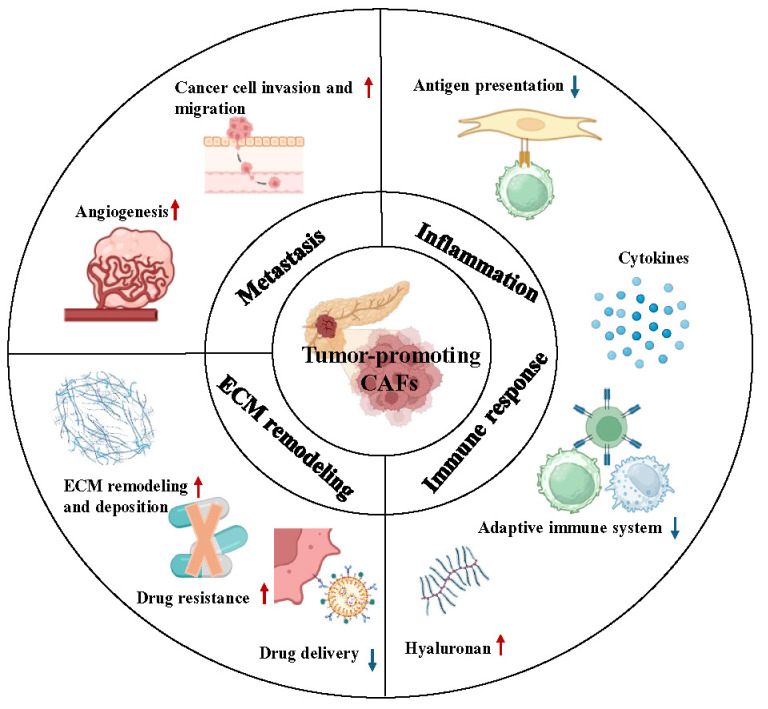
One of the distinguishing features of PDAC is a pronounced desmoplastic response characterized by an extensive fibrotic stroma that exceeds the tumor cell volume (Whatcott et al., 2015). This dense stromal component, which is composed primarily of cancer-associated fibroblasts (CAFs), immune cells, and a complex network of extracellular matrix (ECM), does not simply serve as a passive scaffold but actively participates in tumor progression and metastasis (Öhlund et al., 2014). The dynamic interaction between tumor cells and the surrounding stroma forms a self-reinforcing loop. On one hand, the stroma can protect tumor cells by blocking the access of therapeutic agents and immune cells (Provenzano et al., 2012). Conversely, signals from tumor cells can induce stromal cells to secrete growth factors and cytokines, thus further supporting tumor growth and survival (Feig et al., 2013). These complex tumor–stroma interactions have therapeutic implications because they affect drug delivery, modify the immune response, and influence the overall patient prognosis (Neesse et al., 2019) (Fig. 1).
Fig. 1.
The influence of cancer-associated fibroblasts (CAFs) on the principal hallmarks of PDAC. Through dynamic interactions with the tumor stroma microenvironment, CAFs assimilate physiological roles that fundamentally influence the principal hallmarks of PDAC.
Recent studies have sought to decipher the molecular profile of the stroma to reveal specific signatures that correlate with patient survival (Bailey et al., 2016). Identifying stromal biomarkers, such as specific collagen isoforms, matrix metalloproteinases (MMPs), and cytokine profiles, can provide deeper insights into disease aggressiveness and metastatic potential (Jiang et al., 2017). Furthermore, spatial interactions between tumor cells and stromal components, including the proximity and organization of fibroblasts and immune cells, have been found to be the key determinants of disease progression; these spatial patterns provide clues to the activity of the immune system against tumors and can predict resistance or sensitivity to specific therapeutic interventions (Biffi et al., 2019).
In this study, we explore the intricate tapestry of the stroma and how individual elements influence the prognosis of PDAC to elucidate potential pathways for the development of innovative therapeutic strategies and sophisticated prognostic assessments.
CANCER-ASSOCIATED FIBROBLASTS (CAFS)
Origin of cancer-associated fibroblasts (CAFs) in PDAC
CAFs are a major component of the characteristic desmoplastic response in PDAC and play a multifaceted role in tumor progression, immune evasion, treatment resistance, and metastasis. In general, the term “CAFs” refers to fibroblasts in the tumor microenvironment (TME) of solid cancers. These cells are characterized by their spindle-like morphology and functional activation, which distinguishes them from the dormant fibroblasts commonly found in healthy tissues (Zhang et al., 2022). Pancreatic stellate cells (PSCs) were considered to be the primary progenitors of CAFs in PDAC; however, recent studies have shown that PSC-derived CAFs represent only a fraction of the total CAF population (Helms et al., 2022). In addition, other cell types within the TME, including bone marrow–derived macrophages, endothelial cells, adipocytes, and perivascular cells, have been identified as potential sources of CAFs that are recruited and transformed at the tumor site (Huang et al., 2020; Sunami et al., 2020).
Activated factors of cancer-associated fibroblasts (CAFs) in PDAC
CAFs are activated fibroblasts characterized by the expression of specific markers such as alpha-smooth muscle actin (α-SMA), fibroblast activation protein (FAP), and platelet-derived growth factor receptors (PDGFRα/β) (Han et al., 2020). Once activated, CAFs secrete a variety of factors including growth factors, chemokines, and cytokines, which contribute to the creation of a pro-tumorigenic microenvironment. One of the primary mechanisms through which CAFs drive PDAC proliferation is through the modulation of ECM components (Joshi et al., 2021). CAFs remodel the ECM, increasing its stiffness and altering its composition, which in turn promotes cancer cell proliferation. This remodeling is facilitated by the secretion of matrix metalloproteinases (MMPs) and the deposition of fibrous proteins such as collagen and fibronectin, creating a physical scaffold that supports tumor growth (Belhabib et al., 2021). In addition, CAFs secrete several growth factors, including fibroblast growth factor (FGF), vascular endothelial growth factor (VEGF), and transforming growth factor-beta (TGF-β), which directly stimulate cancer cell proliferation and support angiogenesis (Feng et al., 2022). In particular, TGF-β signaling is a key pathway through which CAFs induce epithelial-to-mesenchymal transition (EMT) in cancer cells, a critical process for metastasis (Baulida, 2017). EMT facilitates the detachment of cancer cells from the primary tumor mass, enhancing their ability to migrate and become invasive, thereby promoting metastasis.
CAFs also contribute to the immunosuppressive tumor microenvironment observed in PDAC by secreting cytokines such as interleukin-6 (IL-6) and interleukin-10 (IL-10), which can inhibit the function of immune cells and further facilitate tumor growth and metastasis (Morgan et al., 2023). CAFs significantly influence the pancreatic cancer progression through their role in ECM remodeling, secretion of growth factors and cytokines, and contribution to an immunosuppressive microenvironment (Wright et al., 2023). Understanding the intricate signaling networks between CAFs and cancer cells offers promising opportunities for the development of targeted therapies aimed at disrupting these interactions and thereby inhibiting PDAC progression and metastasis (Fig. 1).
Classification of cancer-associated fibroblasts (CAFs)
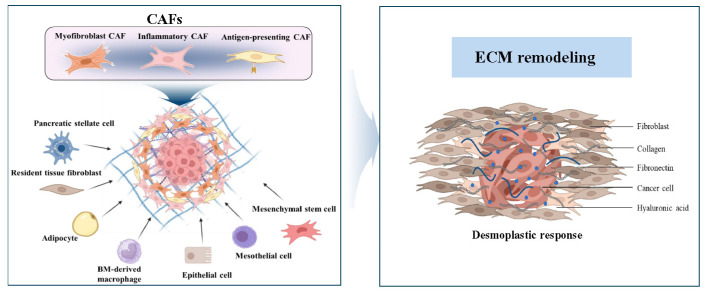
CAFs are heterogeneous and can be subclassified into multiple populations on the basis of their functions and markers. Recent advances in genetically engineered mouse models of PDAC and the application of single-cell ribonucleic acid sequencing have revealed the broad diversity of CAFs and demonstrated that CAFs in PDAC exert context-dependent functions that include both tumor-promoting and tumor-suppressive effects (Garcia et al., 2020; Boyd et al., 2022). The subtypes of CAFs commonly include myofibroblast CAFs (myCAFs), inflammatory CAFs (iCAFs), and antigen-presenting CAFs (apCAFs). In the current study, we focus on these three main types of CAFs (Fig. 2, Table 1).
Fig. 2.
Heterogeneity of cancer-associated fibroblast (CAFs) and ECM remodeling in PDAC. Pancreatic stellate cells (PSCs) and other resident tissue fibroblasts are the primary progenitors of CAFs in PDAC, and mesothelial cells, adipocytes and bone marrow-derived macrophages transform into CAFs. Epithelial and endothelial cells are also identified as potential sources of CAFs that are recruited and transformed in the tumor microenvironment. Based on the subtype of CAFs, they generally include myofibroblast CAFs, inflammatory CAFs and antigen-presenting CAFs. The ECM of PDAC is particularly dense and contributes to its desmoplastic response. It’s composed of collagen, proteoglycans, laminin, and fibronectin, etc.
Table 1.
The key markers of different subtypes of CAFs in PDAC
| CAF subtype | CAF markers | References |
|---|---|---|
| myCAF | α-SMAhigh | Murray et al., 2022 |
| PDGFR (CD147) | Rhim et al., 2014; Shin et al., 2014 | |
| TGF-β1 | Rhim et al., 2014; Shin et al., 2014 | |
| Col 1 | Özdemir et al., 2014 | |
| iCAF | FAP | McAndrews et al., 2022 |
| IL-6 | Elyada et al., 2019 | |
| LIF | Shi et al., 2019 | |
| CXCL1 | Öhlund et al., 2017; Biffi et al., 2019 | |
| apCAF | MHC Class II | Elyada et al., 2019 |
| CD74 | Elyada et al., 2019 |
Myofibroblast cancer-associated fibroblasts (myCAFs)
Öhlund et al. (2017) discovered that CAFs in PDAC exhibit myCAF or iCAF phenotypes. myCAFs are located in close proximity to tumor cells, express high levels of alpha-smooth muscle actin (α-SMA), and are stimulated by transforming growth factor. Interfering with the normal differentiation of PSCs into α-SMA+ myofibroblasts can result in a shift in activation to iCAFs, which can promote pancreatic tumor invasion (Murray et al., 2022). The selective depletion of α-SMA+ myofibroblasts in mice at the early and late stages of PDAC resulted in aggressive tumors with significantly reduced stiffness of the tumor tissue because of decreased collagen I (Col I) content and myCAF-induced ECM remodeling, thus leading to the decreased survival of the animals (Özdemir et al., 2014). Myofibroblast-depleted tumors were sensitive to anti-CTLA4 immunotherapy, thus opening a potential therapeutic avenue; however, the genetic ablation of sonic hedgehog signaling in mouse PDAC remarkably reduced α-SMA+ matrix content, increased vascularity, and resulted in aggressive tumors with increased metastatic potential (Rhim et al., 2014; Shin et al., 2014). Although this demonstrates the tumor-suppressive effects via the critical protective role of myofibroblasts and myCAF-secreting collagen/ECM in PDAC, the clinical application of non-selective matrix depletion strategies in PDAC requires caution.
Inflammatory cancer-associated fibroblasts (iCAFs)
iCAFs are located at a significant distance from malignant cells and express α-SMA at low levels but produce inflammatory cytokines, including interleukin (IL) 6 and CXCL1 (Öhlund et al., 2017; Biffi et al., 2019; Elyada et al., 2019). IL-6 plays a critical role in the formation of the tumor immune microenvironment and is an inflammatory cytokine secreted by iCAFs in response to paracrine signaling from the malignant epithelium, which promotes the invasion and colonization of pancreatic cancer cells (Nagathihalli et al., 2016; Öhlund et al., 2017). However, the removal of IL-6 from α-SMA+ CAFs improves the efficacy of gemcitabine and acts synergistically with immune checkpoint blockade (McAndrews et al., 2022). Leukemia inhibitory factor (LIF), which is another key paracrine mediator, is released by iCAFs and promotes tumor progression in mouse and human PDAC tissues (Shi et al., 2019). Targeting LIF with gene ablation or neutralizing antibodies can improve the efficacy of chemotherapy and prevent engraftment in pancreatic xenograft models (Wang et al., 2019). In addition, PDGFRα has been proposed as a surface marker of iCAF that inhibits myCAF differentiation (Djurec et al., 2018). Collectively, targeting iCAF offers a potential therapeutic avenue because it can reduce their tumor-promoting activity while promoting the tumor-suppressive properties of myCAFs.
Antigen-presenting cancer-associated fibroblasts (apCAFs)
Tubeson et al. identified a third CAF subtype in PDAC called apCAFs, which express the MHC-II gene and CD74 (Elyada et al., 2019). apCAFs induce T cell receptor binding to CD4+ T cells but lack costimulatory molecules for T cell proliferation (Elyada et al., 2019; Huang et al., 2022). Their abundance is negatively correlated with the CD8+/regulatory T cell (Treg) ratio in human PDAC, thus suggesting an immunosuppressive function. apCAFs are presumably derived from mesothelial cells and exhibit an overlapping gene expression signature (Huang et al., 2022). Targeting mesothelin may inhibit its conversion to apCAFs, reduce Tregs, and increase the number of cytotoxic T cells (Huang et al., 2022), thus making it a potential therapeutic strategy.
EXTRACELLULAR MATRIX (ECM) PROTEINS
The ECM of PDAC is particularly dense and contributes to its desmoplastic nature (Fig. 2). It is composed of collagen, proteoglycans, laminin, and fibronectin and provides structural integrity and biochemical cues for cell function (Table 2). The altered composition and cross-linking of the ECM can modulate tumor cell behavior, promote metastasis, and interfere with drug delivery (Provenzano et al., 2012). Particularly, the composition of the ECM and its interactions with cancer cells can affect the prognosis of patients with these malignancies.
Table 2.
The role of ECM proteins and their contribution to PDAC progression
| ECM Protein | Role in PDAC | Implications in PDAC | References |
|---|---|---|---|
| Collagen |
The principal structural component of the ECM. Facilitates cell-ECM interactions. |
Increased collagen deposition, especially Type I collagen, can drive invasive behavior in PDAC. Associated with the promotion of cell proliferation and immunosuppression. |
|
| Hyaluronan |
Another ECM molecule. Facilitates a physical barrier and a signaling molecule that influences the immune response. |
Accumulated HA leads to increased poor survival, and reduced T cell infiltration in the TME. Promotes infiltration and differentiation of tumor-associated macrophages. |
|
| Matrix Metalloproteinases (MMPs) |
Enzymes that degrade ECM components. Involved in tissue inhibitors. |
Their overexpression can drive PDAC progression by degrading ECM and altering ECM dynamics. MMPs are key drivers of both tumor growth and metastasis during PDAC. |
|
| Tissue Inhibitors of Metalloproteinases (TIMPs) |
Inhibit MMP activity. Regulate ECM turnover. |
Imbalance between TIMPs and MMPs can affect the integrity of the ECM in PDAC, influencing tumor behavior. | |
| Fibronectin | Facilitates cell adhesion to the EMT. |
Elevated in PDAC and has been associated with tumor progression. Promotes cell proliferation and adhesion. |
|
| Laminin |
Accumulate in the ECM. Facilitates cell migration and invasion. |
Alterations in laminin expression can affect PDAC cell adhesion and migration. |
Collagen
Collagen is a major component of ECM and plays an important role in PDAC progression The accumulation of collagen within the tumor environment is directly linked to increased tumor invasiveness. Furthermore, this enhanced deposition of collagen can impact treatment efficacy and contribute to drug resistance due to its barrier properties (Öhlund et al., 2013; Drifka et al., 2016). Several studies have highlighted that Col I remodeling may serve as a prognostic marker in patients with PDAC. PDAC cells produce a unique oncogenic Col I homotrimeric variant that differs from the heterotrimeric form found in normal cells and promotes cancer cell proliferation and immunosuppression (Chen et al., 2022). The Col I homotrimer influences the tumor immune microenvironment by altering the tumor-associated microbiome while repelling T cells and recruiting bone marrow–derived suppressor cells. In nutrient-limited environments, PDAC cells utilize amino acids, particularly proline, from the degradation of ECM proteins, such as Col I and IV, to support TCA cycle metabolism. The uptake of collagen triggers the extracellular signal-regulated kinase 1/2 signaling pathway, which contributes to the survival of cancer cells under nutritional stress conditions (Olivares et al., 2017). In terms of targeted therapy to ECM collagen, some researchers have utilized liposomes loaded with collagenase (called “collagosomes”) to degrade collagen in pancreatic tumor stroma. The targeted delivery of proteolytic enzymes can enhance tumor therapy with minimal damage to healthy tissue (Zinger et al., 2019). This ECM remodeling appears to disrupt signal transduction between cancer cells and CAFs, thus potentially inhibiting PDAC progression (Nakajima et al., 2022).
Hyaluronan (HA)
HA is another ECM molecule that is significantly upregulated in PDAC. High concentrations of HA can elevate tumor stromal pressure, which can interfere with drug delivery and affect treatment outcomes (Provenzano et al., 2012; Cheng et al., 2016; Kudo et al., 2017). In PDAC, stromal HA accumulation is an independent prognostic factor of poor survival and is associated with poor immune response, as indicated by reduced T cell infiltration in the TME (Tahkola et al., 2021). The role of HA is complex: it potentially acts as both a physical barrier and a signaling molecule that influences the immune response. An HA-rich environment can also promote tumor-associated macrophage infiltration and differentiation into a pro-tumor phenotype (Yang et al., 2023). Patients with high HA levels had significantly shorter survival. There were significant differences in HA levels between primary pancreatic tumors and metastatic sites, particularly in the liver. These variations in HA levels suggest that the treatment may need to be site-specific, thus raising concerns regarding the role of HA in different TMEs (Placencio-Hickok et al., 2022).
Matrix metalloproteinases (MMPs)
MMPs, which are enzymes that degrade the ECM, and its tissue inhibitors (TIMPs) have also been investigated for their roles in PDAC. This imbalance can alter ECM dynamics, thus potentially driving tumor progression and affecting patient prognosis (Slapak et al., 2020). MMPs, which are also known as matrix metallopeptidases, are calcium-dependent zinc-containing endopeptidases. MMPs are highly expressed in PDAC tissues compared with surrounding non-cancerous tissues (Zhai et al., 2016; Zhang et al., 2020). MMPs are key drivers of tumor growth, invasion and metastasis during pancreatic cancer progression (Kessenbrock et al., 2010). According to this notion, changes in MMP expression levels are often considered surrogate markers of pancreatic cancer progression and/or treatment response. Indeed, reduced MMP levels upon treatment (either pharmacological or genetic ablation) are considered proof of the antitumorigenic potential of this mediator (Slapak et al., 2020).
The tissue inhibitors of metalloproteinases (TIMPs)
An imbalance between TIMPs and MMPs can compromise the structural integrity of ECM in PDAC, thereby influencing tumor dynamics and behavior (Roy and Walsh, 2014; Schoeps et al., 2021; Tian et al., 2022). In particular, TIMP1 may be a biomarker for early intervention and a novel therapeutic target for the inhibition of liver metastasis in patients with PDAC. Precancerous or inflammatory lesions in the pancreas release TIMP1 into the blood to activate hepatic stellate cells in the liver, thus creating a “premetastatic niche” in which the liver is highly vulnerable to cancer cells. This metastatic niche can be prevented or reversed by targeting TIMP1 interactions or related signaling pathways (Grünwald et al., 2016). Furthermore, TIMP1 expression was found to be higher in gemcitabine-resistant PDAC cells. Its knockdown sensitizes cancer cells to gemcitabine by reducing cell proliferation and promoting apoptosis (Tan et al., 2021). Monocyte-like cells, particularly those secreting TIMP2, can significantly reduce the formation of invasive podia in PDAC cells, thereby reducing their invasiveness and metastatic potential. Furthermore, manipulating the TME to increase TIMP2-secreting monocytes may be a promising therapeutic strategy (Benzing et al., 2019).
Fibronectin
Fibronectin expression is significantly higher in the microenvironment of PDAC than in normal pancreatic tissue and is associated with aggressive tumor features such as larger size, advanced tumor stage, and worse disease outcomes (Xu et al., 2023). Although fibronectin is associated with EMT and has been proposed as a biomarker for EMT, its prognostic value in PDAC remains inconclusive. The role of fibronectin in tumor biology appears to be complex and context dependent, with different effects observed in different cancer types (Hu et al., 2019). Fibronectin fragments produced by pancreatic trypsin act to inhibit PDAC by disrupting the functional connections between β1 integrin, focal adhesion kinase, and fibroblast growth factor receptor. This inhibition reduces PDAC cell adhesion, proliferation, and tumor growth (Resovi et al., 2023). Additionally, near-infrared fluorescence (NIRF) and magnetic resonance (MR) imaging demonstrated higher FN levels in PDAC from obese mice. Obesity was associated with accelerated PDAC growth, increased metastasis, and reduced response to gemcitabine chemotherapy. The decreased efficacy of chemotherapy in obese PDAC mice was attributed to impaired drug delivery, potentially linked to elevated FN levels in the ECM (Xu et al., 2023).
Laminin
Laminins are a family of high-molecular-weight glycoproteins that primarily accumulate in the ECM of neuroretinal, skeletal, or epithelial cells. The expression levels of laminins, including laminin-5 gamma-2 (LAMC2), are increased in PDAC at both the messenger ribonucleic acid and protein levels (Kirtonia et al., 2022; Sari et al., 2023). High expression and levels of LAMC2 are associated with advanced pathological stages and poor survival outcomes. Its knockdown reduces the self-renewal, migration, invasion, tumorigenicity, and chemoresistance of PDAC cells. LAMC2-positive cells exhibit EMT properties and enhanced metastatic potential (Cave et al., 2022). Mechanistically, LAMC2 was found to interact with EGFR, activating downstream signaling pathways like EGFR-ERK1/2 and AKT/mTOR/P70S6K/P85S6K, thereby contributing to tumorigenesis and metastasis (Kirtonia et al., 2022). Its expression was also predictive of the response to gemcitabine-based therapy. The downregulation of LAMC2 increases gemcitabine sensitivity, induces apoptosis, and impairs the invasion and migration of PDAC cells. It also contributes to regulate EMT activation and adenosine triphosphate–binding cassette transporter expression (Okada et al., 2021). These studies suggest that laminins are potential therapeutic targets for controlling the invasive and metastatic aspects of PDAC (Huang and Chen, 2021).
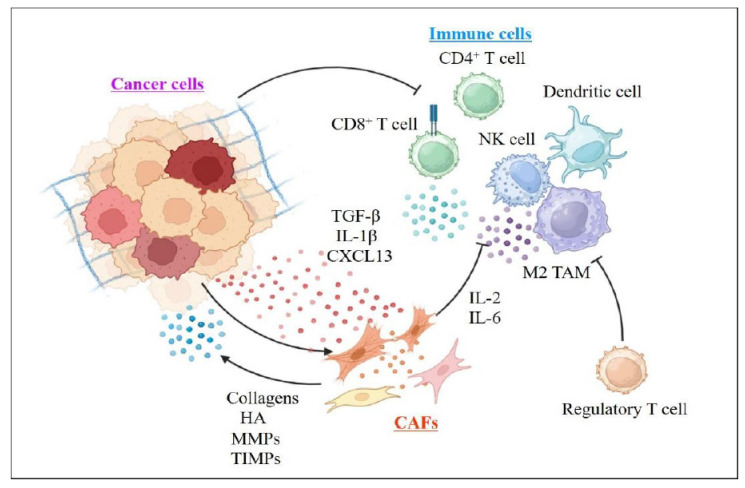
IMMUNE CELLS AND CYTOKINES
PDAC stroma is infiltrated by a variety of immune cells. Some immune cells, such as M2 macrophages and T regulatory cells, promote tumor progression and immune evasion, whereas others, such as cytotoxic T cells and NK cells, counteract tumor growth (Fig. 3). However, an immunosuppressive microenvironment often limits their activity (Beatty et al., 2021).
Fig. 3.
Cancer-associated fibroblasts (CAFs) interact with immune cells. CAFs secrete ECM components and contribute to the fibrotic tumor microenvironment. Cancer cytokines such as TGF-β, IL-1β and CXCL13 play a critical role in the activation of CAFs. Once activated, CAFs promote cancer cell growth by releasing factors that support tumor development. PDAC has dysfunctional T cells with decreased levels of CD3+, CD4+ and NK cells and increased levels of regulatory T cells. In addition to recruiting and regulating immunosuppressive cells, CAFs also interfere with the anti-tumor functions of CD8+ T cells.
INNATE IMMUNE SYSTEM
Macrophages
Macrophages are a major component of pancreatic TME, and an increase in macrophages is associated with poor patient survival (Poh and Ernst, 2021). Macrophages are broadly categorized into the M1 and M2 subtypes. M1 macrophages show increased expression of inducible nitric oxide synthase, whereas M2 macrophages express high levels of CD204, CD206, ARG1, and CD163 (Singh et al., 2014; Wang et al., 2015). These subtypes play distinct roles in tumor progression, with proinflammatory M1 macrophages inhibiting tumor growth, and M2 macrophages contributing to tumor progression by inhibiting T cell–mediated antitumor immune activity (Beatty et al., 2015). Tumor-associated macrophages (TAMs) release cytokines (e.g., TGF-β and PGE2) and chemokines (e.g., CCL7 and CCL2) that promote T cell exhaustion and contribute to the creation of a self-sustaining microenvironment conducive to tumor growth (Kalinski, 2012). TAMs inhibit antitumor responses by expressing inhibitory receptors such as PDL1/PDL2 and CD80/CD86, which bind to PD1 and CTLA4 on the surface of CD8 T cells, thus preventing the recruitment and activation of cytotoxic effector cells. TAMs also promote the accumulation of Tregs in tumors. Recent strategies to target TAMs in PDAC include macrophage depletion, macrophage recruitment inhibition, and macrophage reprogramming, and several agents are currently under clinical evaluation.
Natural killer (NK) cells
The proportion of NK cells is lower in tumor tissues than in blood, thus indicating that NK cell migration into the tumor is inhibited. Notably, NK cells from patients with PDAC show altered cytokine production, with decreased levels of interferon gamma, IL-6, and IL-2 but increased production of IL-10, thus suggesting a regulatory phenotype (Marcon et al., 2020). The mechanisms that inhibit the growth of pancreatic cancer mainly include the upregulation of multiple receptors and ligands and the promotion of the release of NK cell–associated cytokines. The secretion of cytokines, stimulation of immune drugs, and other methods to enhance the activity of NK cells are novel strategies for enhancing the tumor-killing effect of NK cells. In the future, additional NK cell–related immunotherapies will be applied for the treatment of pancreatic cancer (Peng et al., 2021).
Adaptive immune system
PDAC tumors are considered nonimmunogenic or cold, have a low mutational burden and low infiltration of CD8+ cytotoxic lymphocytes (T cells) localized along the invasive edge of the tumor border in the surrounding fibrotic tissue, and often exhibit an exhausted phenotype (Goulart et al., 2021). Patients with PDAC exhibit dysfunctional T cells with decreased levels of CD3, CD4, and NK cells and increased Treg cells (Xing et al., 2022). Tumor-infiltrating lymphocytes, particularly Tregs, and their interactions with dendritic cells (DCs) play an important role in tumorigenesis and response to antitumor immunotherapy. In PDAC, Tregs can inhibit the antitumor activity of CD8+ T cells, thereby undermining the effectiveness of immunotherapy. DCs recognize tumor cell antigens and present them to T cells to influence immune responses. A low number of tumor-infiltrating DCs in PDAC is associated with immune evasion. DCs can induce the differentiation of cytotoxic CD8+ T cells while potentially suppressing Treg formation or function. In addition, the TME with increased DC concentrations can promote T cell differentiation and suppress Tregs, thereby promoting antitumor immune responses (Pu et al., 2018a, 2018b). Recently, a new metric called the infiltrative immune response, which combines CD8+ T cell infiltration with the presence of FoxP3+ Tregs, was developed to provide better survival risk stratification (Yi et al., 2018).
Cytokines
Cytokines promote PDAC initiation, progression, metastasis, and the distant colonization of malignant cells via their receptors. These signaling mediators secreted by TAMs and CAFs, combined with oncogenic KRAS mutations, initiate ductal metaplasia in progenitors, thus resulting in the appearance of early preneoplastic lesions (Bhatia et al., 2022). The proinflammatory cytokine IL-1β has two roles. It cooperates with mutant KRAS to stimulate the proliferation of pancreatic epithelial cells and upregulates CXCL13 to attract B cells to the TME. The accumulation of B cells in the pancreas, particularly immunosuppressive subpopulations such as regulatory B cells and PD-L1+ B cells, plays an important role in promoting tumorigenesis by suppressing CD8+ T cell activity (Takahashi et al., 2021). One of the major factors that limit the efficacy of immune checkpoint inhibition in PDAC is the overexpression of TGF-β, which promotes immune tolerance. Although TGF-β pathway inhibitors have shown partial efficacy, their combination with PD-1/PD-L1 inhibitors has demonstrated potential to enhance antitumor immune responses (Principe et al., 2019). Studies have shown that TGF-β signaling can inhibit the activation and function of T-lymphocytes which is an important component of the antitumor immune response. TGF-β can inhibit T cell cytotoxicity by upregulating molecules such as Fas ligand and Granzyme B, which are essential for T cell–mediated tumor cell death. Additionally, TGF-β can induce anergy in T cells, thus making them less responsive to activation signals (Pu et al., 2018a, 2018b).
CONCLUSIONS
PDAC is a highly aggressive and challenging cancer with a poor prognosis. The characteristic complex TME and dense desmoplastic response of PDAC contribute to its tumorigenicity and tumor progression. CAFs are important components of the PDAC TME and contribute to tumor progression and dissemination. In this review, we discuss the functional heterogeneity of CAFs, the stromal ECM, and the immune responses. The functional status of CAFs as myofibroblasts or inflammatory cells may depend on their differentiation status or may simply be a dynamic process in response to environmental changes. The targeting of CAFs, ECM, and desmoplasticity is currently under consideration. Targeting CAFs and ECM-rich desmoplasia may still be attractive options for PDAC treatment; nevertheless, more research is needed to further characterize CAFs. Conclusively, a better understanding of the interaction between different types of CAFs and the stromal ECM may help guide new treatment paradigms and improve the prognosis of patients with PDAC.
Funding Statement
ACKNOWLEDGMENTS This study was supported by a research grant from Inha University.
Footnotes
CONFLICT OF INTEREST
The authors declare that they have no competing interests.
REFERENCES
- Bailey P., Chang D. K., Nones K., Johns A. L., Patch A. M., Gingras M. C., Miller D. K., Christ A. N., Bruxner T. J., Quinn M. C., Nourse C., Murtaugh L. C., Harliwong I., Idrisoglu S., Manning S., Nourbakhsh E., Wani S., Fink L., Holmes O., Chin V., Anderson M. J., Kazakoff S., Leonard C., Newell F., Waddell N., Wood S., Xu Q., Wilson P. J., Cloonan N., Kassahn K. S., Taylor D., Quek, Robertson A., Pantano L., Mincarelli L., Sanchez L. N., Evers L., Wu J., Pinese M., Cowley M. J., Jones M. D., Colvin E. K., Nagrial A. M., Humphrey E. S., Chantrill L. A., Mawson A., Humphris J., Chou A., Pajic M., Scarlett C. J., Pinho A. V., Giry-Laterriere M., Rooman I., Samra J. S., Kench J. G., Lovell J. A., Merrett N. D., Toon C. W., Epari K., Nguyen N. Q., Barbour A., Zeps N., Moran-Jones K., Jamieson N. B., Graham J. S., Duthie F., Oien K., Hair J., Grützmann R., Maitra A., Iacobuzio-Donahue C. A., Wolfgang C. L., Morgan R. A., Lawlor R. T., Corbo V., Bassi C., Rusev B., Capelli P., Salvia R., Tortora G., Mukhopadhyay D., Petersen G. M., Australian Pancreatic Cancer Genome Initiative, Munzy D. M., Fisher W. E., Karim S. A., Eshleman J. R., Hruban R. H., Pilarsky C., Morton J. P., Sansom O. J., Scarpa A., Musgrove E. A., Bailey U. M., Hofmann O., Sutherland R. L., Wheeler D. A., Gill A. J., Gibbs R. A., Pearson J. V., Waddell N., Biankin A. V., Grimmond S. M. Genomic analyses identify molecular subtypes of pancreatic cancer. Nature. 2016;531:47–52. doi: 10.1038/nature16965. [DOI] [PubMed] [Google Scholar]
- Baulida J. Epithelial-to-mesenchymal transition transcription factors in cancer-associated fibroblasts. Mol. Oncol. 2017;11:847–859. doi: 10.1002/1878-0261.12080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beatty G. L., Winograd R., Evans R. A., Long K. B., Luque S. L., Lee J. W., Clendenin C., Gladney W. L., Knoblock D. M., Guirnalda P. D., Vonderheide R. H. Exclusion of T cells from pancreatic carcinomas in mice is regulated by Ly6Clow F4/80+ extratumoral macrophages. Gastroenterology. 2015;149:201–210. doi: 10.1053/j.gastro.2015.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beatty G. L., Werba G., Lyssiotis C. A., Simeone D. M. The biological underpinnings of therapeutic resistance in pancreatic cancer. Genes Dev. 2021;35:940–962. doi: 10.1101/gad.348523.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belhabib I., Zaghdoudi S., Lac C., Bousquet C., Jean C. Extracellular matrices and cancer-associated fibroblasts: targets for cancer diagnosis and therapy? Cancers (Basel) 2021;13:3466. doi: 10.3390/cancers13143466.ddbd7a53bfed48a29a5fb4641379790b [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benzing C., Lam H., Tsang C. M., Rimmer A., Arroyo-Berdugo Y., Calle Y., Wells C. M. TIMP-2 secreted by monocyte-like cells is a potent suppressor of invadopodia formation in pancreatic cancer cells. BMC Cancer. 2019;19:1214. doi: 10.1186/s12885-019-6429-z.f560872f34c64405b7258d44b284a3e7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatia R., Bhyravbhatla N., Kisling A., Li X., Batra S. K., Kumar S. Cytokines chattering in pancreatic ductal adenocarcinoma tumor microenvironment. Semin. Cancer Biol. 2022;86:499–510. doi: 10.1016/j.semcancer.2022.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biffi G., Oni T. E., Spielman B., Hao Y., Elyada E., Park Y., Preall J., Tuveson D. A. IL1-induced JAK/STAT signaling is antagonized by TGFβ to shape CAF heterogeneity in pancreatic ductal adenocarcinoma. Cancer Discov. 2019;9:282–301. doi: 10.1158/2159-8290.CD-18-0710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd L. N. C., Andini K. D., Peters G. J., Kazemier G., Giovannetti E. Heterogeneity and plasticity of cancer-associated fibroblasts in the pancreatic tumor microenvironment. Semin. Cancer Biol. 2022;82:184–196. doi: 10.1016/j.semcancer.2021.03.006. [DOI] [PubMed] [Google Scholar]
- Cave D. D., Buonaiuto S., Sainz B., Jr., Fantuz M., Mangini M., Carrer A., Di Domenico A., Iavazzo T. T., Andolfi G., Cortina C., Sevillano M., Heeschen C., Colonna V., Corona M., Cucciardi A., Di Guida M., Batlle E., De Luca A., Lonardo E. LAMC2 marks a tumor-initiating cell population with an aggressive signature in pancreatic cancer. J. Exp. Clin. Cancer Res. 2022;41:315. doi: 10.1186/s13046-022-02516-w.7a66930b577747c385f65ad7170426ec [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Yang S., Tavormina J., Tampe D., Zeisberg M., Wang H., Mahadevan K. K., Wu C. J., Sugimoto H., Chang C. C., Jenq R. R., McAndrews K. M., Kalluri R. Oncogenic collagen I homotrimers from cancer cells bind to α3β1 integrin and impact tumor microbiome and immunity to promote pancreatic cancer. Cancer Cell. 2022;40:818–834. doi: 10.1016/j.ccell.2022.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng F., Gong Q., Yu H., Stephanopoulos G. High-titer biosynthesis of hyaluronic acid by recombinant Corynebacterium glutamicum. Biotechnol. J. 2016;11:574–584. doi: 10.1002/biot.201500404. [DOI] [PubMed] [Google Scholar]
- Djurec M., Graña O., Lee A., Troulé K., Espinet E., Cabras L., Navas C., Blasco M. T., Martín-Díaz L., Burdiel M., Li J., Liu Z., Vallespinós M., Sanchez-Bueno F., Sprick M. R., Trumpp A., Sainz B., Jr., Al-Shahrour F., Rabadan R., Guerra C., Barbacid M. Saa3 is a key mediator of the protumorigenic properties of cancer-associated fibroblasts in pancreatic tumors. Proc. Natl. Acad. Sci. U. S. A. 2018;115:E1147–E1156. doi: 10.1073/pnas.1717802115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drifka C. R., Loeffler A. G., Mathewson K., Keikhosravi A., Eickhoff J. C., Liu Y., Weber S. M., Kao W. J., Eliceiri K. W. Highly aligned stromal collagen is a negative prognostic factor following pancreatic ductal adenocarcinoma resection. Oncotarget. 2016;7:76197–76213. doi: 10.18632/oncotarget.12772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elyada E., Bolisetty M., Laise P., Flynn W. F., Courtois E. T., Burkhart R. A., Teinor J. A., Belleau P., Biffi G., Lucito M. S., Sivajothi S., Armstrong T. D., Engle D. D., Yu K. H., Hao Y., Wolfgang C. L., Park Y., Preall J., Jaffee E. M., Califano A., Robson P., Tuveson D. A. Cross-species single-cell analysis of pancreatic ductal adenocarcinoma reveals antigen-presenting cancer-associated fibroblasts. Cancer Discov. 2019;9:1102–1123. doi: 10.1158/2159-8290.CD-19-0094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feig C., Jones J. O., Kraman M., Wells R. J., Deonarine A., Chan D. S., Connell C. M., Roberts E. W., Zhao Q., Caballero O. L., Teichmann S. A., Janowitz, Jodrell D. I., Tuveson D. A., Fearon D. T. Targeting CXCL12 from FAP-expressing carcinoma-associated fibroblasts synergizes with anti-PD-L1 immunotherapy in pancreatic cancer. Proc. Natl. Acad. Sci. U. S. A. 2013;110:20212–20217. doi: 10.1073/pnas.1320318110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng B., Wu J., Shen B., Jiang F., Feng J. Cancer-associated fibroblasts and resistance to anticancer therapies: status, mechanisms, and countermeasures. Cancer Cell Int. 2022;22:166. doi: 10.1186/s12935-022-02599-7.f7d0149fcab7426b89a50fba5ead5c12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia P. E., Scales M. K., Allen B. L., Pasca, di Magliano M. Pancreatic fibroblast heterogeneity: from development to cancer. Cells. 2020;9:2464. doi: 10.3390/cells9112464.7ea95e2bf5de4af2aac3fc14fc1752a7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goulart M. R., Stasinos K., Fincham R. E. A., Delvecchio F. R., Kocher H. M. T cells in pancreatic cancer stroma. World J. Gastroenterol. 2021;27:7956–7968. doi: 10.3748/wjg.v27.i46.7956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grünwald B., Harant V., Schaten S., Frühschütz M., Spallek R., Höchst B., Stutzer K., Berchtold S., Erkan M., Prokopchuk O., Martignoni M., Esposito I., Heikenwalder M., Gupta A., Siveke J., Saftig P., Knolle P., Wohlleber D., Krüger A. Pancreatic premalignant lesions secrete tissue inhibitor of metalloproteinases-1, which activates hepatic stellate cells via CD63 signaling to create a premetastatic niche in the liver. Gastroenterology. 2016;151:1011–1024. doi: 10.1053/j.gastro.2016.07.043. [DOI] [PubMed] [Google Scholar]
- Han C., Liu T., Yin R. Biomarkers for cancer-associated fibroblasts. Biomark. Res. 2020;8:64. doi: 10.1186/s40364-020-00245-w.77dbba9141c64c1cb51df5c93aeac649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helms E. J., Berry M. W., Chaw R. C., DuFort C. C., Sun D., Onate M. K., Oon, Bhattacharyya S., Sanford-Crane H., Horton W., Finan J. M., Sattler A., Makar R., Dawson D. W., Xia Z., Hingorani S. R., Sherman M. H. Mesenchymal lineage heterogeneity underlies nonredundant functions of pancreatic cancer-associated fibroblasts. Cancer Discov. 2022;12:484–501. doi: 10.1158/2159-8290.CD-21-0601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu D., Ansari D., Zhou Q., Sasor A., Said Hilmersson K., Andersson R. Stromal fibronectin expression in patients with resected pancreatic ductal adenocarcinoma. World J. Surg. Oncol. 2019;17:29. doi: 10.1186/s12957-019-1574-z.e740cbdb891f4aad9065595f0a27069e [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Chen J. Laminin-332 mediates proliferation, apoptosis, invasion, migration and epithelial-to-mesenchymal transition in pancreatic ductal adenocarcinoma. Mol. Med. Rep. 2021;23:11. doi: 10.3892/mmr.2020.11649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang H., Wang Z., Zhang Y., Pradhan R. N., Ganguly D., Chandra R., Murimwa G., Wright S., Gu X., Maddipati R., Müller S., Turley S. J., Brekken R. A. Mesothelial cell-derived antigen-presenting cancer-associated fibroblasts induce expansion of regulatory T cells in pancreatic cancer. Cancer Cell. 2022;40:656–673.e7. doi: 10.1016/j.ccell.2022.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang X., He C., Hua X., Kan A., Mao Y., Sun S., Duan F., Wang J., Huang P., Li S. Oxidative stress induces monocyte-to-myofibroblast transdifferentiation through p38 in pancreatic ductal adenocarcinoma. Clin. Transl. Med. 2020;10:e41. doi: 10.1002/ctm2.41.544ac0c7e2154209b1a3423d47f0b7a0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang H., Hegde S., Knolhoff B. L., Zhu Y., Herndon J. M., Meyer M. A., Nywening T. M., Hawkins W. G., Shapiro I. M., Weaver D. T., Pachter J. A., Wang-Gillam A., DeNardo D. G. Targeting focal adhesion kinase renders pancreatic cancers responsive to checkpoint immunotherapy. Nat. Med. 2017;23:851–860. doi: 10.1038/nm.4123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joshi R. S., Kanugula S. S., Sudhir S., Pereira M. P., Jain S., Aghi M. K. The role of cancer-associated fibroblasts in tumor progression. Cancers (Basel) 2021;13:1399. doi: 10.3390/cancers13061399.6acec43623de42d5bbf1749435326d81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalinski P. Regulation of immune responses by prostaglandin E2. J. Immunol. 2012;188:21–28. doi: 10.4049/jimmunol.1101029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessenbrock K., Plaks V., Werb Z. Matrix metalloproteinases: regulators of the tumor microenvironment. Cell. 2010;141:52–67. doi: 10.1016/j.cell.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirtonia A., Pandey A. K., Ramachandran B., Mishra D. P., Dawson D. W., Sethi G., Ganesan T. S., Koeffler H. P., Garg M. Overexpression of laminin-5 gamma-2 promotes tumorigenesis of pancreatic ductal adenocarcinoma through EGFR/ERK1/2/AKT/mTOR cascade. Cell. Mol. Life Sci. 2022;79:362. doi: 10.1007/s00018-022-04392-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kudo D., Suto A., Hakamada K. The development of a novel therapeutic strategy to target hyaluronan in the extracellular matrix of pancreatic ductal adenocarcinoma. Int. J. Mol. Sci. 2017;18:600. doi: 10.3390/ijms18030600.f88f1934dbee4d25b897b1b6003b358a [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maitra A., Hruban R. H. Pancreatic cancer. Annu. Rev. Pathol. 2008;3:157–188. doi: 10.1146/annurev.pathmechdis.3.121806.154305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcon F., Zuo J., Pearce H., Nicol S., Margielewska-Davies S., Farhat M., Mahon B., Middleton G., Brown R., Roberts K. J., Moss P. NK cells in pancreatic cancer demonstrate impaired cytotoxicity and a regulatory IL-10 phenotype. Oncoimmunology. 2020;9:1845424. doi: 10.1080/2162402X.2020.1845424.9cab5ad3fc4d48768fc0086ab29de4c8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAndrews K. M., Chen Y., Darpolor J. K., Zheng X., Yang S., Carstens J. L., Li B., Wang H., Miyake T., Correa, de Sampaio P., Kirtley M. L., Natale M., Wu C. C., Sugimoto H., LeBleu V. S., Kalluri R. Identification of functional heterogeneity of carcinoma-associated fibroblasts with distinct IL6-mediated therapy resistance in pancreatic cancer. Cancer Discov. 2022;12:1580–1597. doi: 10.1158/2159-8290.CD-20-1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan A., Griffin M., Kameni L., Wan D. C., Longaker M. T., Norton J. A. Medical biology of cancer-associated fibroblasts in pancreatic cancer. Biology (Basel) 2023;12:1044. doi: 10.3390/biology12081044.8c8aafbc1f2847a9bb0cd02917da7074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray E. R., Menezes S., Henry J. C., Williams J. L., Alba-Castellón L., Baskaran P., Quétier I., Desai A., Marshall J. J. T., Rosewell I., Tatari M., Rajeeve V., Khan F., Wang J., Kotantaki P., Tyler E. J., Singh N., Reader C. S., Carter E. P., Hodivala-Dilke K., Grose R. P., Kocher H. M., Gavara N., Pearce O., Cutillas P., Marshall J. F., Cameron A. J. M. Disruption of pancreatic stellate cell myofibroblast phenotype promotes pancreatic tumor invasion. Cell Rep. 2022;38:110227. doi: 10.1016/j.celrep.2021.110227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagathihalli N. S., Castellanos J. A., VanSaun M. N., Dai X., Ambrose M., Guo Q., Xiong Y., Merchant N. B. Pancreatic stellate cell secreted IL-6 stimulates STAT3 dependent invasiveness of pancreatic intraepithelial neoplasia and cancer cells. Oncotarget. 2016;7:65982–65992. doi: 10.18632/oncotarget.11786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakajima K., Ino Y., Naito C., Nara S., Shimasaki M., Ishimoto U., Iwasaki T., Doi N., Esaki M., Kishi Y., Shimada K., Hiraoka N. Neoadjuvant therapy alters the collagen architecture of pancreatic cancer tissue via Ephrin-A5. Br. J. Cancer. 2022;126:628–639. doi: 10.1038/s41416-021-01639-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neesse A., Bauer C. A., Öhlund D., Lauth M., Buchholz M., Michl P., Tuveson D. A., Gress T. M. Stromal biology and therapy in pancreatic cancer: ready for clinical translation? Gut. 2019;68:159–171. doi: 10.1136/gutjnl-2018-316451. [DOI] [PubMed] [Google Scholar]
- Öhlund D., Elyada E., Tuveson D. Fibroblast heterogeneity in the cancer wound. J. Exp. Med. 2014;211:1503–1523. doi: 10.1084/jem.20140692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Öhlund D., Franklin O., Lundberg E., Lundin C., Sund M. Type IV collagen stimulates pancreatic cancer cell proliferation, migration, and inhibits apoptosis through an autocrine loop. BMC Cancer. 2013;13:154. doi: 10.1186/1471-2407-13-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Öhlund D., Handly-Santana A., Biffi G., Elyada E., Almeida A. S., Ponz-Sarvise M., Corbo V., Oni T. E., Hearn S. A., Lee E. J., Chio I. I., Hwang C. I., Tiriac H., Baker L. A., Engle D. D., Feig C., Kultti A., Egeblad M., Fearon D. T., Crawford J. M., Clevers H., Park Y., Tuveson D. A. Distinct populations of inflammatory fibroblasts and myofibroblasts in pancreatic cancer. J. Exp. Med. 2017;214:579–596. doi: 10.1084/jem.20162024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okada Y., Takahashi N., Takayama T., Goel A. LAMC2 promotes cancer progression and gemcitabine resistance through modulation of EMT and ATP-binding cassette transporters in pancreatic ductal adenocarcinoma. Carcinogenesis. 2021;42:546–556. doi: 10.1093/carcin/bgab011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olivares O., Mayers J. R., Gouirand V., Torrence M. E., Gicquel T., Borge L., Lac S., Roques J., Lavaut M. N., Berthezène P., Rubis M., Secq V., Garcia S., Moutardier V., Lombardo D., Iovanna J. L., Tomasini R., Guillaumond F., Vander Heiden M. G., Vasseur S. Collagen-derived proline promotes pancreatic ductal adenocarcinoma cell survival under nutrient limited conditions. Nat. Commun. 2017;8:16031. doi: 10.1038/ncomms16031.6a73d2e74efe45e79489251d11428d7b [DOI] [PMC free article] [PubMed] [Google Scholar]
- Özdemir B. C., Pentcheva-Hoang T., Carstens J. L., Zheng X., Wu C. C., Simpson T. R., Laklai H., Sugimoto H., Kahlert C., Novitskiy S. V., De Jesus-Acosta A., Sharma P., Heidari P., Mahmood U., Chin L., Moses H. L., Weaver V. M., Maitra A., Allison J. P., LeBleu V. S., Kalluri R. Depletion of carcinoma-associated fibroblasts and fibrosis induces immunosuppression and accelerates pancreas cancer with reduced survival. Cancer Cell. 2014;25:719–734. doi: 10.1016/j.ccr.2014.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng X., Chen L., Jiao Y., Wang Y., Hao Z., Zhan X. Application of natural killer cells in pancreatic cancer. Oncol. Lett. 2021;22:647. doi: 10.3892/ol.2021.12908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Placencio-Hickok V. R., Lauzon M., Moshayedi N., Guan M., Kim S., Nissen N., Lo S., Pandol S., Larson B. K., Gong J., Hendifar A. E., Osipov A. Hyaluronan heterogeneity in pancreatic ductal adenocarcinoma: primary tumors compared to sites of metastasis. Pancreatology. 2022;22:92–97. doi: 10.1016/j.pan.2021.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poh A. R., Ernst M. Tumor-associated macrophages in pancreatic ductal adenocarcinoma: therapeutic opportunities and clinical challenges. Cancers. 2021;13:2860. doi: 10.3390/cancers13122860.a832968140b24553814ac3561f513a10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Principe D. R., Park A., Dorman M. J., Kumar S., Viswakarma N., Rubin J., Torres C., McKinney R., Munshi H. G., Grippo P. J., Rana A. TGFβ blockade augments PD-1 inhibition to promote T-cell-mediated regression of pancreatic cancer. Mol. Cancer Ther. 2019;18:613–620. doi: 10.1158/1535-7163.MCT-18-0850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Provenzano P. P., Cuevas C., Chang A. E., Goel V. K., Von Hoff D. D., Hingorani S. R. Enzymatic targeting of the stroma ablates physical barriers to treatment of pancreatic ductal adenocarcinoma. Cancer Cell. 2012;21:418–429. doi: 10.1016/j.ccr.2012.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pu N., Zhao G., Gao S., Cui Y., Xu Y., Lv Y., Nuerxiati A., Wu W. Neutralizing TGF-β promotes anti-tumor immunity of dendritic cells against pancreatic cancer by regulating T lymphocytes. Cent. Eur. J. Immunol. 2018a;43:123–131. doi: 10.5114/ceji.2018.77381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pu N., Zhao G., Yin H., Li J. A., Nuerxiati A., Wang D., Xu X., Kuang T., Jin D., Lou W., Wu W. CD25 and TGF-β blockade based on predictive integrated immune ratio inhibits tumor growth in pancreatic cancer. J. Transl. Med. 2018b;16:294. doi: 10.1186/s12967-018-1673-6.43c054cfd17349709f2029e712fcd4be [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resovi A., Persichitti P., Brunelli L., Minoli L., Borsotti P., Garattini G., Tironi M., Dugnani E., Redegalli M., De Simone G., Pastorelli R., Bani M. R., Piemonti L., Mosher D. F., Giavazzi R., Taraboletti G., Belotti D. Fibronectin fragments generated by pancreatic trypsin act as endogenous inhibitors of pancreatic tumor growth. J. Exp. Clin. Cancer Res. 2023;42:201. doi: 10.1186/s13046-023-02778-y.4bc68fabcf3a4866bfd7e59ee7c138f6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhim A. D., Oberstein P. E., Thomas D. H., Mirek E. T., Palermo C. F., Sastra S. A., Dekleva E. N., Saunders T., Becerra C. P., Tattersall I. W., Westphalen C. B., Kitajewski J., Fernandez-Barrena M. G., Fernandez-Zapico M. E., Iacobuzio-Donahue C., Olive K. P., Stanger B. Z. Stromal elements act to restrain, rather than support, pancreatic ductal adenocarcinoma. Cancer Cell. 2014;25:735–747. doi: 10.1016/j.ccr.2014.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy D. M., Walsh L. A. Candidate prognostic markers in breast cancer: focus on extracellular proteases and their inhibitors. Breast Cancer (Dove Med. Press) 2014;6:81–91. doi: 10.2147/BCTT.S46020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan D. P., Hong T. S., Bardeesy N. Pancreatic adenocarcinoma. N. Engl. J. Med. 2014;371:1039–1049. doi: 10.1056/NEJMra1404198. [DOI] [PubMed] [Google Scholar]
- Sari B., Gulbey O., Hamill K. J. Laminin 332 expression levels predict clinical outcomes and chemotherapy response in patients with pancreatic adenocarcinoma. Front. Cell Dev. Biol. 2023;11:1242706. doi: 10.3389/fcell.2023.1242706.7456a6f6c89f4d6d80486307a35ced1d [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoeps B., Eckfeld C., Flüter L., Keppler S., Mishra R., Knolle P., Bayerl F., Böttcher J., Hermann C. D., Häußler D., Krüger A. Identification of invariant chain CD74 as a functional receptor of tissue inhibitor of metalloproteinases-1 (TIMP-1) J. Biol. Chem. 2021;297:101072. doi: 10.1016/j.jbc.2021.101072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi Y., Gao W., Lytle N. K., Huang P., Yuan X., Dann A. M., Ridinger-Saison M., DelGiorno K. E., Antal C. E., Liang G., Atkins A. R., Erikson G., Sun H., Meisenhelder J., Terenziani E., Woo G., Fang L., Santisakultarm T. P., Manor U., Xu R., Becerra C. R., Borazanci E., Von Hoff D. D., Grandgenett P. M., Hollingsworth M. A., Leblanc M., Umetsu S. E., Collisson E. A., Scadeng M., Lowy A. M., Donahue T. R., Reya T., Downes M., Evans R. M., Wahl G. M., Pawson T., Tian R., Hunter T. Targeting LIF-mediated paracrine interaction for pancreatic cancer therapy and monitoring. Nature. 2019;569:131–135. doi: 10.1038/s41586-019-1130-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin K., Lim A., Zhao C., Sahoo D., Pan Y., Spiekerkoetter E., Liao J. C., Beachy P. A. Hedgehog signaling restrains bladder cancer progression by eliciting stromal production of urothelial differentiation factors. Cancer Cell. 2014;26:521–533. doi: 10.1016/j.ccell.2014.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh A., Talekar M., Raikar A., Amiji M. Macrophage-targeted delivery systems for nucleic acid therapy of inflammatory diseases. J. Control. Release. 2014;190:515–530. doi: 10.1016/j.jconrel.2014.04.021. [DOI] [PubMed] [Google Scholar]
- Slapak E. J., Duitman J., Tekin C., Bijlsma M. F., Spek C. Matrix metalloproteases in pancreatic ductal adenocarcinoma: key drivers of disease progression? Biology. 2020;9:80. doi: 10.3390/biology9040080.854e41da336842e683ff4162e4fd55ac [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sunami Y., Häußler J., Kleeff J. Cellular heterogeneity of pancreatic stellate cells, mesenchymal stem cells, and cancer-associated fibroblasts in pancreatic cancer. Cancers (Basel) 2020;12:3770. doi: 10.3390/cancers12123770.703dad5366bf4b368c549f6109640bd9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tahkola K., Ahtiainen M., Mecklin J. P., Kellokumpu I., Laukkarinen J., Tammi M., Tammi R., Väyrynen J. P., Böhm J. Stromal hyaluronan accumulation is associated with low immune response and poor prognosis in pancreatic cancer. Sci. Rep. 2021;11:12216. doi: 10.1038/s41598-021-91796-x.b4f44af321ba49f18edf717a8c6c488d [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi R., Macchini M., Sunagawa M., Jiang Z., Tanaka T., Valenti G., Renz B. W., White R. A., Hayakawa Y., Westphalen C. B., Tailor Y., Iuga A. C., Gonda T. A., Genkinger J., Olive K. P., Wang T. C. Interleukin-1β-induced pancreatitis promotes pancreatic ductal adenocarcinoma via B lymphocyte-mediated immune suppression. Gut. 2021;70:330–341. doi: 10.1136/gutjnl-2019-319912. [DOI] [PubMed] [Google Scholar]
- Tan Y., Li X., Tian Z., Chen S., Zou J., Lian G., Chen S., Huang K., Chen Y. TIMP1 down-regulation enhances gemcitabine sensitivity and reverses chemoresistance in pancreatic cancer. Biochem. Pharmacol. 2021;189:114085. doi: 10.1016/j.bcp.2020.114085. [DOI] [PubMed] [Google Scholar]
- Tian F., Ma L., Zhao R., Ji L., Wang X., Sun W., Jiang Y. Correlation between matrix metalloproteinases with coronary artery lesion caused by kawasakidisease. Front. Pediatr. 2022;10:802217. doi: 10.3389/fped.2022.802217.dc48dff1e72c4792b2e09a149d6a25b9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent A., Herman J., Schulick R., Hruban R. H., Goggins M. Pancreatic cancer. Lancet. 2011;378:607–620. doi: 10.1016/S0140-6736(10)62307-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Cao Z., Zhang X. M., Nakamura M., Sun M., Hartman J., Harris R. A., Sun Y., Cao Y. Novel mechanism of macrophage-mediated metastasis revealed in a zebrafish model of tumor development. Cancer Res. 2015;75:306–315. doi: 10.1158/0008-5472.CAN-14-2819. [DOI] [PubMed] [Google Scholar]
- Wang M. T., Fer N., Galeas J., Collisson E. A., Kim S. E., Sharib J., McCormick F. Blockade of leukemia inhibitory factor as a therapeutic approach to KRAS driven pancreatic cancer. Nat. Commun. 2019;10:3055. doi: 10.1038/s41467-019-11044-9.1264485d73e0466695383206f5054dba [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whatcott C. J., Diep C. H., Jiang P., Watanabe A., LoBello J., Sima C., Hostetter G., Shepard H. M., Von Hoff D. D., Han H. Desmoplasia in primary tumors and metastatic lesions of pancreatic cancer. Clin. Cancer Res. 2015;21:3561–3568. doi: 10.1158/1078-0432.CCR-14-1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright K., Ly T., Kriet M., Czirok A., Thomas S. M. Cancer-associated fibroblasts: master tumor microenvironment modifiers. Cancers (Basel) 2023;15:1899. doi: 10.3390/cancers15061899.98409293ef5e4ca7bdbd241c7efc045b [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xing Y., Zhang X., Qin F., Yang J., Ai L., Wang Q., Zhai Y. The clinical significance of circulating tumor cells and T lymphocyte subtypes in pancreatic cancer patients. Bioengineered. 2022;13:2130–2138. doi: 10.1080/21655979.2021.2023800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu T., Xu X., Liu D., Chang D., Li S., Sun Y., Xie J., Ju S. Visual investigation of tumor-promoting fibronectin potentiated by obesity in pancreatic ductal adenocarcinoma using an MR/NIRF dual-modality dendrimer nanoprobe. Adv. Healthc. Mater. 2023;12:e2300787. doi: 10.1002/adhm.202300787. [DOI] [PubMed] [Google Scholar]
- Yang Y., Chen Z., Chu X., Yan Q., He J., Guo Y., Zhao Z., Zhang Y., Hu D., Ding H., Zhao X., Pan Y., Dong H., Wang L., Pan J. Targeting LAYN inhibits colorectal cancer metastasis and tumor-associated macrophage infiltration induced by hyaluronan oligosaccharides. Matrix Biol. 2023;117:15–30. doi: 10.1016/j.matbio.2023.02.005. [DOI] [PubMed] [Google Scholar]
- Yi G., Guo S., Liu W., Wang H., Liu R., Tsun A., Jin G., Li B. Identification and functional analysis of heterogeneous FOXP3+ Treg cell subpopulations in human pancreatic ductal adenocarcinoma. Sci. Bull. (Beijing) 2018;63:972–981. doi: 10.1016/j.scib.2018.05.028. [DOI] [PubMed] [Google Scholar]
- Zhai L. L., Wu Y., Cai C. Y., Huang Q., Tang Z. G. High-level expression and prognostic significance of matrix metalloprotease-19 and matrix metalloprotease-20 in human pancreatic ductal adenocarcinoma. Pancreas. 2016;45:1067–1072. doi: 10.1097/MPA.0000000000000569. [DOI] [PubMed] [Google Scholar]
- Zhang X., Lu J., Zhou L., You L., Liang Z., Guo J., Zhao Y. Matrix metalloproteinase 11 as a novel tumor promoter and diagnostic and prognostic biomarker for pancreatic ductal adenocarcinoma. Pancreas. 2020;49:812–821. doi: 10.1097/MPA.0000000000001583. [DOI] [PubMed] [Google Scholar]
- Zhang Z., Zhang H., Shi L., Wang D., Tang D. Heterogeneous cancer-associated fibroblasts: a new perspective for understanding immunosuppression in pancreatic cancer. Immunology. 2022;167:1–14. doi: 10.1111/imm.13496. [DOI] [PubMed] [Google Scholar]
- Zinger A., Koren L., Adir O., Poley M., Alyan M., Yaari Z., Noor N., Krinsky N., Simon A., Gibori H., Krayem M., Mumblat Y., Kasten S., Ofir S., Fridman E., Milman N., Lübtow M. M., Liba L., Shklover J., Shainsky-Roitman J., Binenbaum Y., Hershkovitz D., Gil Z., Dvir T., Luxenhofer R., Satchi-Fainaro R., Schroeder A. Collagenase nanoparticles enhance the penetration of drugs into pancreatic tumors. ACS Nano. 2019;13:11008–11021. doi: 10.1021/acsnano.9b02395. [DOI] [PMC free article] [PubMed] [Google Scholar]