Abstract
BACKGROUND
ART differs in effectiveness, side-effects, administration, and costs. To improve the decision-making process, we need to understand what factors patients consider to be most important.
OBJECTIVE AND RATIONALE
We conducted this systematic review to assess which aspects of ART treatment (effectiveness, safety, burden, costs, patient-centeredness, and genetic parenthood) are most important in the decision-making of patients with an unfulfilled wish to have a child.
SEARCH METHODS
We searched studies indexed in Embase, PubMed, PsycINFO, and CINAHL prior to November 2023. Discrete choice experiments (DCEs), surveys, interviews, and conjoint analyses (CAs) about ART were included. Studies were included if they described two or more of the following attributes: effectiveness, safety, burden, costs, patient-centeredness, and genetic parenthood.
Participants were men and women with an unfulfilled wish to have a child. From each DCE/CA study, we extracted the beta-coefficients and calculated the relative importance of treatment attributes or, in case of survey studies, extracted results. We assessed the risk of bias using the rating developed by the Grading of Recommendations Assessment, Development and Evaluation working group. Attributes were classified into effectiveness, safety, burden, costs, patient-centeredness, genetic parenthood, and others.
OUTCOMES
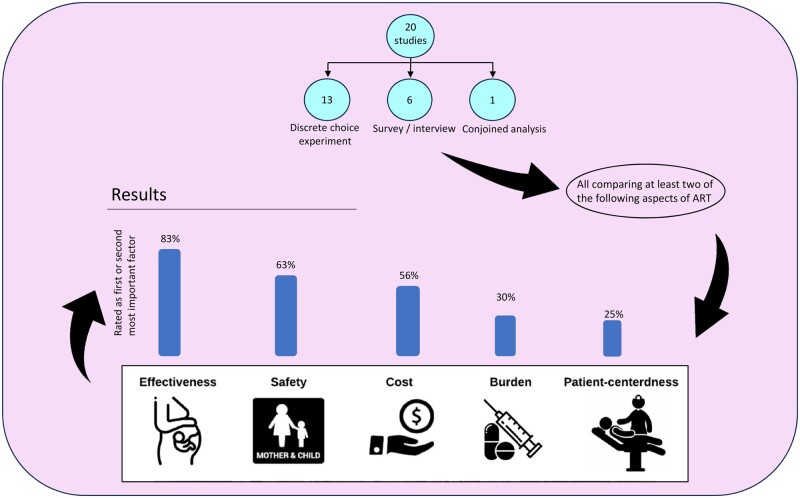
The search identified 938 studies of which 20 were included: 13 DCEs, three survey studies, three interview studies, and one conjoint analysis, with a total of 12 452 patients. Per study, 47–100% of the participants were women. Studies were assessed as having moderate to high risk of bias (critical: six studies, serious: four studies, moderate: nine studies, low: one study). The main limitation was the heterogeneity in the questionnaires and methodology utilized. Studies varied in the number and types of assessed attributes. Patients’ treatment decision-making was mostly driven by effectiveness, followed by safety, burden, costs, and patient-centeredness. Effectiveness was rated as the first or second most important factor in 10 of the 12 DCE studies (83%) and the relative importance of effectiveness varied between 17% and 63%, with a median of 34% (moderate certainty of evidence). Of eight studies evaluating safety, five studies valued safety as the first or second most important factor (63%), and the relative importance ranged from 8% to 35% (median 23%) (moderate certainty of evidence). Cost was rated as first or second most important in five of 10 studies, and the importance relative to the other attributes varied between 5% and 47% (median 23%) (moderate certainty of evidence). Burden was rated as first or second by three of 10 studies (30%) and the relative importance varied between 1% and 43% (median 13%) (low certainty of evidence). Patient-centeredness was second most important in one of five studies (20%) and had a relative importance between 7% and 24% (median 14%) (low certainty of evidence). Results suggest that patients are prepared to trade-off some effectiveness for more safety, or less burden and patient-centeredness. When safety was evaluated, the safety of the child was considered more important than the mother’s safety. Greater burden (cycle cancellations, number of injections, number of hospital visits, time) was more likely to be accepted by patients if they gained effectiveness, safety, or lower costs. Concerning patient-centeredness, information provision and physician attitude were considered most important, followed by involvement in decision-making, and treatment continuity by the same medical professional. Non-genetic parenthood did not have a clear impact on decision-making.
WIDER IMPLICATIONS
The findings of this review can be used in future preference studies and can help healthcare professionals in guiding patients’ decision-making and enable a more patient-centered approach.
Keywords: infertility, patient preference, child-wish, assisted reproduction, acceptability of healthcare, ART
Graphical Abstract
In patients seeking medical assistance for infertility, the most important attribute driving patients’ decision-making was effectiveness of treatment followed by safety and costs; burden and patient-centeredness were considered less important.
Introduction
Patients seeking medical assistance to fulfill their wish to have a child can utilize a wide range of ART. Technologies such as IVF, ICSI, frozen embryo transfer, or preimplantation genetic screening may result in reasonable chances for a pregnancy but differ in treatment duration, side-effects, and safety for mother and child—aspects that affect patient preferences. The availability of multiple reasonable treatment options makes treatment decisions highly preference-sensitive (van der Horst et al., 2023). Besides differences in treatment-related aspects, variability in costs may also affect decision-making, although in some countries fertility treatments are covered by health insurance with few out-of-pocket costs remaining for patients. Furthermore, using a patient-centered approach, for instance by providing more information and helping in shared decision-making, may affect how treatment options are perceived (Malin et al., 2001; Twisk et al., 2007). Technologies are rapidly advancing and new treatment options make decision-making even more complex, highlighting the need to know what factors are important to patients.
To elicit patient preferences in a quantitative way, discrete choice experiments (DCEs) and conjoint analyses (CAs) have been established as a way to quantify preferences. These are survey-based research methods used to understand how people make decisions when presented with multiple options. In a DCE, participants are typically presented with a series of hypothetical scenarios where they must choose between two scenarios. For example, a DCE might ask participants to choose between different treatment options based on attributes such as pregnancy chance, side-effects, number of hospital visits, and supervision by single or multiple providers. To ensure that the attributes are relevant, they are usually defined by expert focus groups and literature reviews (Botha et al., 2018). By analyzing participants’ choices, researchers can determine which attributes are considered most important when making decisions. Besides allowing us to determine trade-offs that patients are prepared to make, DCEs also allow us to objectively assess the relative importance patients place on the attributes of the scenarios (Reed Johnson et al., 2013). DCEs are commonly used in marketing research, health economics, and environmental economics to understand consumer preferences and predict behavior.
In a CA, treatment attributes and levels are used as well. While in a DCE patients choose between different choice sets, in a CA, patients are asked to rank hypothetical treatment scenarios from best to worst (Bridges et al., 2011; Louviere et al., 2010) in order to draw conclusions about ‘willingness to pay’ or trade-offs. Besides DCEs and conjoined designs, surveys and interviews are often used to evaluate patient preferences. Such studies have the advantage of being more flexible and with the potential to capture new ideas.
All these preference studies help to better understand how men and women value different aspects of their treatment. This allows clinicians to better respond to patient expectations, to enable patients’ decision-making, and to improve decision aids (Klitzman, 2018).
With this systematic review, we aimed to study what attributes patients with an unfulfilled wish to have a child consider to be most important when making treatment decisions about ART.
Methods
This systematic review followed the reporting guidelines of the PRISMA 2020 Statement (Page et al., 2021). The study protocol was registered in Prospero: CRD42022302551.
Eligibility criteria
Studies were considered eligible if preferences related to ART were evaluated in men and/or women with an unfulfilled wish to have a child. As technologies and preferences may change over time, only articles published since January 2000 were included. These had to be designed as a DCE, conjoint experiment, survey, or structured interview using quantitative techniques (i.e. varying the probability of pregnancy until preferences regarding ART techniques changed).
We excluded studies regarding fertility preservation in cancer, gonadotrophin application, and birth outcomes only. We also excluded studies that did not describe attributes related to at least two of the following: costs, safety, burden, effectiveness, genetic parenthood, and patient-centeredness.
Literature search
To identify eligible studies, we searched the databases Embase, PsycINFO, PubMed, and CINAHL from 1 January 2000 to 20 November 2023, without any language restriction. Additionally, we checked the reference lists of included studies. Our search strategy can be found in Supplementary Data File S1.
Study selection and critical appraisal
Two authors (M.v.W. and F.v.E.) independently screened the title and abstract of all identified publications. After initial screening, the full-text articles of studies identified as relevant were further evaluated by the same two authors. Disagreements were resolved by discussion until consensus was reached.
Two authors (M.v.W. and F.v.E.) assessed the risk of bias of each included study independently. Disagreements were resolved by consensus. Risk of bias assessments for preference studies were based on a rating developed by the Grading of Recommendations Assessment, Development and Evaluation (GRADE) working group (Zhang et al., 2019). The following criteria were assessed: participant selection, completeness of data, measurement instruments, and data analysis. These were rated as low, moderate, serious, or critical. Subsequently, we graded the evidence using the approach of the same GRADE working group (Zhang et al., 2019).
Data extraction and outcomes
Data were extracted from the studies, including:
Study characteristics: author, year of publication, country, preference elicitation method, response rate, type of assessed attributes, and number of attributes.
Patient characteristics: number of patients, gender, duration of child wish, education, and income.
Outcomes: study attributes were recorded. We aimed to combine the attributes, if possible, into the following attribute groups: effectiveness (chance to conceive, live birth rate, time to successful pregnancy), safety (ovarian hyperstimulation syndrome (OHSS), side effects, neonatal or maternal complications), burden (cycle cancellations, number of injections, hospital visits), patient-centeredness (patient involvement, continuity of physicians, information provision), cost, genetic parenthood, and others (e.g. moral acceptability, availability of experimental treatments).
For the DCE and CA designed studies, we present descriptive data of the relative importance of attributes and visually present the attributes that were chosen as most important or second most important. We also describe the trade-offs that patients were willing to make.
For the survey and interview studies, data representing the importance of examined attributes are described.
Data analysis
For DCE and CA designs, the effects of studied attributes were measured as beta-coefficients, and as relative measures of willingness to trade between attributes. We calculated the relative importance of attributes by first standardizing the beta-coefficients per study by taking the coefficient of the highest levels per attribute divided by the standard error. These standardized coefficients were subsequently translated to a scale ranging from 0 to 1, by dividing by the sum of all standardized coefficients. In case of multiple attributes per attribute group, we took the largest effect (largest beta) to calculate the relative importance.
From survey and interview studies, the effect of attributes was presented descriptively. This allowed us to extract the relative value of an attribute (versus the other studied attributes) as more important, equally important or less important.
As each study included a different combination and number of attributes, it was not possible to combine these estimates in a meta-analysis.
Results
Search results
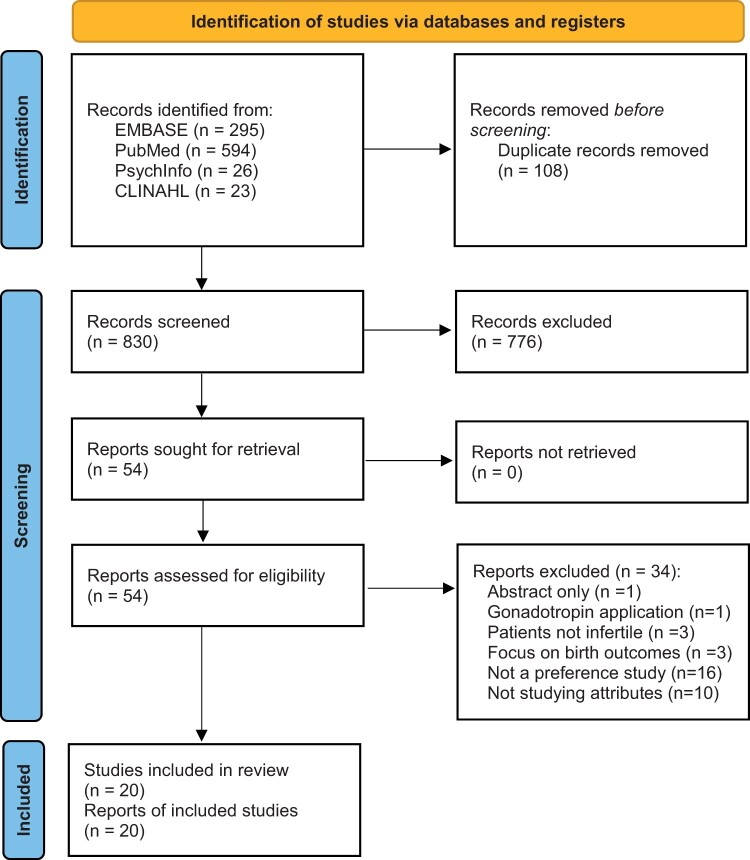
The electronic search generated 938 studies. After removing duplicates, the title and abstract of 830 studies were screened of which 54 were included for full-text review. Of these, 20 studies met inclusion criteria (Fig. 1).
Figure 1.
PRISMA flow diagram of the literature search for studies of factors driving treatment decision-making by patients seeking medical assistance for infertility.
Study characteristics
The characteristics of included studies are described in Table 1. Twelve studies had a DCE design (Musters et al., 2011; van Empel et al., 2011; Huppelschoten et al., 2014; van den Wijngaard et al., 2014, 2015; Weiss et al., 2017; Hendriks et al., 2019; Braam et al., 2020; Abdulrahim et al., 2021; Cornelisse et al., 2022; Skedgel et al., 2022; Keller et al., 2023), one study included both a DCE and a survey (Hendriks et al., 2016), one was designed as CAs study (Palumbo et al., 2011), and six were survey and/or interview studies (Bayram et al., 2005; Steures et al., 2005; van Weert et al., 2007; Sills et al., 2012; Duthie et al., 2017; Stormlund et al., 2019).
Table 1.
Characteristics of studies included in a systematic review of factors driving treatment decision-making by patients seeking medical assistance for infertility.
| Author, year | Design | Setting | Number of patients | Percentage of women | Response rate | Mean age (years) | Duration childwish (months) | Income | Education | Types of attributes | Number of attributes |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Braam, 2020 | DCE | Netherlands | 91 | 100% | 79% | 30.2 | 8 | Low (3.3%), moderate (38,5%), high (47.3%), NR (11.0%) | Low (11%), moderate (44%), high (45.1%) | Three burden, safety, costs | 5 |
| Keller, 2023 | DCE | Australia | 376 | 100% | Unknown | Unclear | Unknown |
|
Not finished high school (8.2%), high school (11.4%), Certificate/trade/TAFE (36.2%), University (44.2%) | Pregnancy rate, burden, three patient-centeredness, availability of experimental treatment, cost | 7 |
| Hendriks, 2019 | DCE | Netherlands, Belgium | 173 | 54% | 32% | 37 | 52.8 | Higher than modal 127 (73%), equal or less than modal (13%), NR (13%) | University degree (62%), no university degree (38%) | Two safety, costs, pregnancy rate, genetic parenthood, curing infertility | 6 |
| van Empel, 2011 | DCE | Netherlands, Belgium | 925 | 52% | 67% | 34 | 33.6 | Unknown | Low-median (48%), high (52%) | Pregnancy rate, three patient-centeredness, burden | 5 |
| van den Wijngaard, 2015 | DCE | Netherlands | 93 | 100% | 77% | 33 | Unknown | Low (12%), moderate (30%), high (55%), NR (3%) | Not finished (2%), secondary (7%), vocational (36%), college/university (53%), NR 2 (2%) | Two burden, safety | 3 |
| Weiss, 2017 | DCE | Netherlands | 145 | 100% | Unknown | 30 | 12.6 | Below average (3.4%), average (22.1%), above average (69.7%), NR (4.9%) | Primary (0%), secondary (20%), tertiary (80%) | Three burden, cost, pregnancy rate, place of fertilization | 5 |
| Huppelschoten, 2014 | DCE | Netherlands | 550 | 51.20% | 55.20% | 35 | 28 | At or below modal income (21.5%), ≥1.5× modal income (78.5%) | Low–middle (51.2%), high (48.8%) | Three patients centered, pregnancy rate, costs | 5 |
| Musters, 2011 | DCE | Netherlands | 206 | 100% | 95% | Unclear: 52% ≥35 years old 48% <35 | 37.7 | Very low (13%), low (29%), moderate (23%), high (28%), NR (8%) | Low (9%), moderate (31%), high (59%), NR (1%) | Pregnancy rate, burden, costs | 3 |
| Abdulrahim, 2021 | DCE | UK | 208 | 50.5% | 58.80% | 37 | 38.1 | Up to £20 000 (7.2%), £20 000–40 000 (28.4%), £40 000–over 50 000 (61.5%), NR (2.9%) | Unknown | Pregnancy rate, safety, cost, chance of miscarriage | 4 |
| van den Wijngaard, 2014 | DCE | Netherlands | 172 | 100% | Unknown | Unknown | Unknown | Unknown | Unknown | Pregnancy rate, two burden, safety | 4 |
| Palumbo, 2011 | CA | Spain | 160 | 100% | Unclear | 35.8 | Unknown | Net income <1502 (50.0%), income of >1502 (40.8%), income between 1804 and 2404 (9.2%) | No school (0.6%), primary (13.8%), secondary (16.3%), college (14,4%), university (55.0%) | Costs, patient-centeredness, safety, pregnancy rate, burden | 5 |
| Sills, 2012 | Survey | USA, CA | 71 | Unclear | 100% | 34 | 28.8 | Unknown | College (33.8%), no college (66.2%) | Costs, burden | 2 |
| Duthie, 2017 | Survey | USA, WI | 118 | 50% | 19% | Unclear | Unknown |
|
No degree (27.1%), college degree (39.8%), advanced degree (30.5%), NR (2.5%) | Costs, two genetic parenthood, burden, two pregnancy rate | 6 |
| Skedgel, 2022 | DCE | USA, UK, Denmark, Nordic (Norway, Sweden, Finland), Spain, China | 7565 | China—57%, Nordic countries—58%, Spain-52%, UK—59%, USA—59% | Unknown | Unclear: between 31 and 45 years of age. | Unclear: majority over 12 months | China 52% and Nordic 35%, (£30–45k). Spain (51%) and UK (33%) (£15–30k). USA (24%) (£45k–60k) | Unknown | Pregnancy rate, safety, two burden, patient centeredness, and cost | 6 |
| Hendriks, 2016 | Survey | Netherlands | 988 | Unclear | 54% | 35.4 | 62.6 | Unknown | High (48.5%) | Burden, cost, curing infertility, conception at home, naturalness, moral acceptability, technological sophistication, safety for child, and pregnancy rate | 9 |
| Stormlund, 2019 | Survey | Denmark | 165 | 62.00% | 77.1% | 34.3 | 28.8 | Social class only women: 38% upper, 41% middle and 12% low men: 44% upper, 40% middle, 5% low | Unknown | Safety (OHSS), safety (of child), pregnancy rate, burden (time), and a natural process | 5 |
| Cornelisse, 2022 | DCE | Netherlands | 164 | 100% | 36.80% | 34 | Unknown | Unknown | High (75%), medium and low (25%) | Pregnancy rate, two burden (time to pregnancy and quality of life), and number of embryos | 4 |
| van Weert, 2007 | Interview | Netherlands | 146 | 50% | Unknown | 34.4 | 44.4 | Unknown | Unknown | Pregnancy rate, safety (OHSS), and risk of multiple pregnancies | 3 |
| Steures, 2005 | Interview | Netherlands | 80 | 50% | Unknown | 33 | 22 | Unknown | Unknown | Pregnancy rate, safety (OHSS), and risk of multiple pregnancies | 3 |
| Bayram, 2005 | Interview | Netherlands | 64 | 100% | 80% | Unknown | Unknown | Unknown | Unknown | Pregnancy rate, safety, and burden | 3 |
OHSS: ovarian hyperstimulation syndrome; DCE: discrete choice experiment; CA: conjoined analysis; NR: not reported.
Of the 20 studies, 11 had been conducted in the Netherlands (Bayram et al., 2005; Steures et al., 2005; van Weert et al., 2007; Musters et al., 2011; van Empel et al., 2011; Huppelschoten et al., 2014; van den Wijngaard et al., 2014, 2015; Weiss et al., 2017; Braam et al., 2020; Cornelisse et al., 2022), two studies were conducted in both the Netherlands and Belgium (Hendriks et al., 2016, 2019), two studies were carried out in the USA (Sills et al., 2012; Duthie et al., 2017), one in Australia (Keller et al., 2023), one in the UK (Abdulrahim et al., 2021), one in Denmark (Stormlund et al., 2019), and one in Spain (Palumbo et al., 2011). The largest study included multiple countries: the USA, the UK, Denmark, Norway, Sweden, Finland, Spain, and China (Skedgel et al., 2022).
The number of attributes ranged between two and nine and the average number of attributes used per study was five.
Patient characteristics
In total, 12 624 patients participated, ranging from 64 to 7565 patients per study. Two studies were unclear about the percentage of female respondents, while for the 18 other studies the majority was female (range 47–100%).
The mean age was 34.1 years (SD: 2.0) and ranged from 30 to 37 years in the 14 studies reporting on age. The time of unsuccessfully trying to have a child was on average 33.1 months (SD: 14.9; missing in eight studies). Response rate ranged from 19% to 100% (missing in seven studies). Twelve studies reported on participants’ income, nine studies included mainly participants with modal or higher than modal income, and in two studies (Palumbo et al., 2011; Duthie et al., 2017) at least 50% of the participants had a lower than modal income.
Except for two studies (Sills et al., 2012; Huppelschoten et al., 2014), the majority of participants reported having a high educational level (i.e. college or university degree), but in six studies the education level was unknown (Table 1).
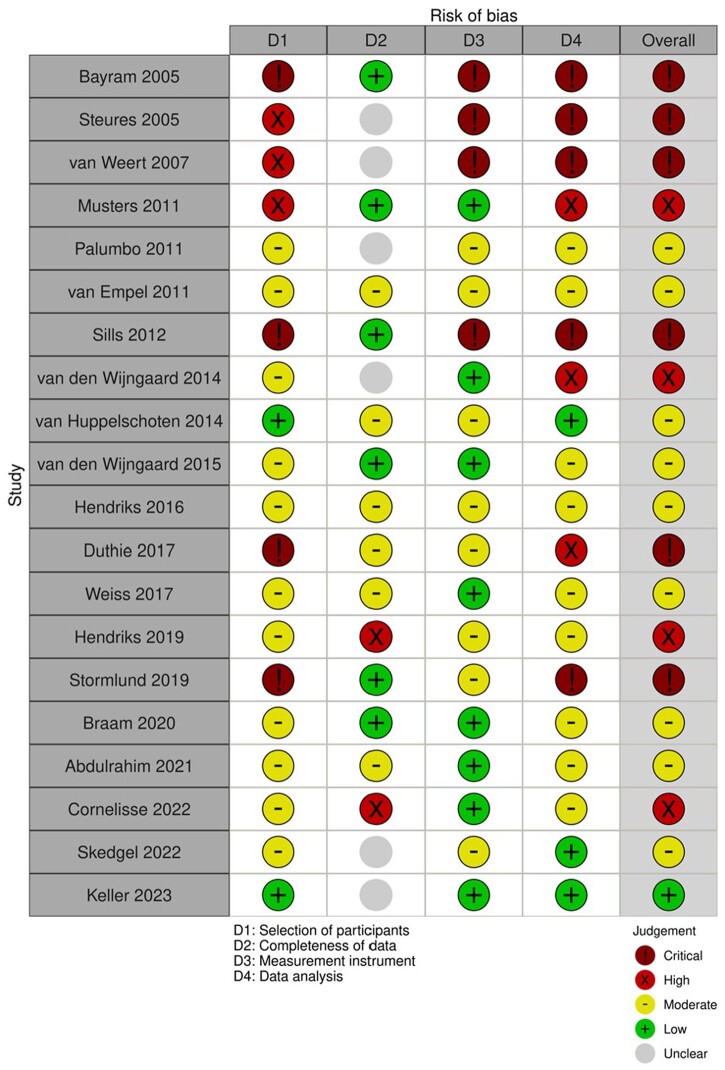
Risk of bias
The risk of bias rating is described in Fig. 2. All six survey/interview studies were rated as being at critical risk of bias owing to selection bias, use of unvalidated questionnaires, and not accounting for the lack of independence of the data in the analysis (multiple questions were answered by each participant) (Bayram et al., 2005; Steures et al., 2005; van Weert et al., 2007; Sills et al., 2012; Duthie et al., 2017; Stormlund et al., 2019). Of the 14 DCE/CA designs, nine had moderate risk of bias (Palumbo et al., 2011; van Empel et al., 2011; Huppelschoten et al., 2014; van den Wijngaard et al., 2015; Hendriks et al., 2016; Weiss et al., 2017; Braam et al., 2020; Abdulrahim et al., 2021; Skedgel et al., 2022) and four had high risk of bias, for example owing to low participation rates or suboptimal statistical analysis (Musters et al., 2011; van den Wijngaard et al., 2014; Hendriks et al., 2019; Cornelisse et al., 2022). The overall rating of a study was based on the lowest rating in any of the categories. One study was scored as having a low risk of bias (Keller et al., 2023) although completeness of data was unclear and selective missingness cannot be fully ruled-out; in this case, we considered the selection of participants, the instrument used and the data analysis to be the more important quality aspects.
Figure 2.
Risk of bias assessment.
Attribute representation
We identified 93 attributes in the 20 included studies. The most assessed attributes were burden (23), pregnancy rate (18), safety (14), costs (12), and patient-centeredness (11). Additional attributes were genetic parenthood, natural processes (i.e. having a natural menstrual cycle and not requiring hormones), place of fertilization (i.e. insemination at hospital or intercourse at home), curing infertility (the hypothetical situation that gametes could be produced from skin cells), and singleton versus multiple pregnancy. Other attributes, only included once, were moral acceptability, technological sophistication, availability of experimental treatment (i.e. add-on treatments that are not supported by scientific evidence), and number of embryos.
Effectiveness
Effectiveness was reported in 17 studies (Bayram et al., 2005; Steures et al. 2005; van Weert et al., 2007; Musters et al., 2011; Palumbo et al., 2011; van Empel et al., 2011; Huppelschoten et al., 2014; van den Wijngaard et al., 2014; Hendriks et al., 2016, 2019; Duthie et al., 2017; Weiss et al., 2017; Stormlund et al., 2019; Abdulrahim et al., 2021; Cornelisse et al., 2022; Skedgel et al., 2022; Keller et al., 2023). Effectiveness was operationalized by pregnancy rate or chance of pregnancy within a certain time after one treatment cycle and ranged between 2% and 50%. In one of the survey studies, patients seeking treatment to have a child were asked about ‘The importance of becoming a parent in the next year or 2’ and ‘Becoming a parent one way or another’ (Duthie et al., 2017). In view of the treatment-related context of these questions, we consider this the importance of effectiveness to patients.
Safety
Twelve studies reported about safety (Bayram et al., 2005; Steures et al., 2005; van Weert et al., 2007; Palumbo et al., 2011; van den Wijngaard et al., 2014, 2015; Hendriks et al., 2016, 2019; Stormlund et al., 2019; Braam et al., 2020; Abdulrahim et al., 2021; Skedgel et al., 2022). Safety was operationalized as the chance of developing OHSS (six studies, with OHSS ranging between 1% and 10%), neonatal or child health (three studies), or maternal health or complication (three studies).
Costs
Costs were reported in 12 studies (Musters et al., 2011; Palumbo et al., 2011; Sills et al., 2012; Huppelschoten et al., 2014; Hendriks et al., 2016, 2019; Duthie et al., 2017; Weiss et al., 2017; Braam et al., 2020; Abdulrahim et al., 2021; Skedgel et al., 2022; Keller et al., 2023), which differed greatly in all studies, ranging from 0 to 18 233 euros (Skedgel et al., 2022). In only one study, the costs were specified as covered by national health insurance (Hendriks et al., 2019). In four studies, it was specified that the costs were out of pocket for participants (Musters et al., 2011; Sills et al., 2012; Braam et al., 2020; Keller et al., 2023). In the rest of the studies, it was not specified but assumed to be out of pocket costs. In one study, cost was found to be statistically insignificant in China and highly important in the USA (Skedgel et al., 2022).
Burden
Burden was addressed 23 times in 15 studies, and some studies reported on burden multiple times with different operationalizations (Bayram et al., 2005; Musters et al., 2011; Palumbo et al., 2011; van Empel et al., 2011; Sills et al., 2012; Huppelschoten et al., 2014; van den Wijngaard et al., 2014, 2015; Duthie et al., 2017; Weiss et al., 2017; Stormlund et al., 2019; Braam et al., 2020; Cornelisse et al., 2022; Skedgel et al., 2022; Keller et al., 2023). In eight studies, burden was represented by hormonal stimulation, ranging from 2 to 20 injections. Five studies reported on side effects, such as headaches, hot flushes, and insomnia. Other operationalizations of burden were risk of cycle discontinuation (two studies), travel time to the hospital (one study), number of hospital visits (three studies), importance of adherence (one study), overall treatment duration (one study), and number of treatments to achieve a 30% pregnancy rate (one study).
Patient-centeredness
Patient-centeredness was addressed 11 times by five studies, as some studies had multiple operationalizations of patient-centeredness (Palumbo et al., 2011; van Empel et al., 2011; Huppelschoten et al., 2014; Skedgel et al., 2022; Keller et al., 2023). Four studies included the extent of patient involvement in the decision-making process (Palumbo et al., 2011; Huppelschoten et al., 2014; Skedgel et al., 2022; Keller et al., 2023). Three studies included providers’ information provision (e.g. customized versus general information), and the same studies included continuity of being treated by the same physician over time (van Empel et al., 2011; Huppelschoten et al., 2014; Keller et al., 2023). One study also looked at physicians’ attitudes (van Empel et al., 2011).
Genetic parenthood
Two studies examined genetic parenthood as a factor contributing to treatment decision-making (Duthie et al., 2017; Hendriks et al., 2019). The different situations that patients were asked to consider were absence of a genetic relation to a child in both parents, one of the parents would be a genetic parent, or both parents would be genetic parents.
Relative importance of attributes
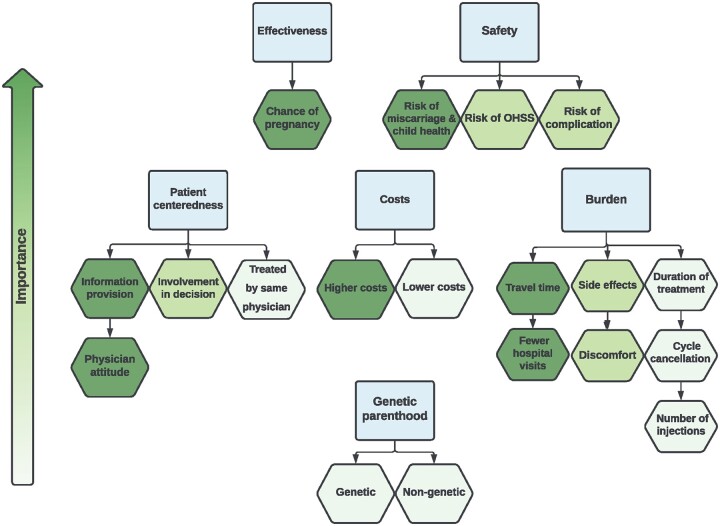
For 14 studies, the relative importance of the attributes effectiveness, safety, burden, costs, and patient-centeredness could be determined (Musters et al., 2011; Palumbo et al., 2011; van Empel et al., 2011; Huppelschoten et al., 2014; van den Wijngaard et al., 2014, 2015; Hendriks et al., 2016, 2019; Weiss et al., 2017; Braam et al., 2020; Abdulrahim et al., 2021; Cornelisse et al., 2022; Skedgel et al., 2022; Keller et al., 2023). The relative importance of these attributes is depicted in Fig. 3. The importance of effectiveness relative to other attributes varied between 17% and 63% (median 34%) and effectiveness was rated as first or second most important factor in 10 of 12 studies (83%). In eight studies evaluating safety, the relative importance ranged from 8% to 35% (median 23%), with five studies valuing safety as first or second most important driver (63%). Regarding costs, the importance relative to the other attributes varied between 5% and 47% (median 23%), with cost being first or second most important in five of 10 studies (50%). For burden, the relative importance varied in 10 studies between 1% and 43% (median 13%) and was first/second most important in three studies (30%). Patient-centeredness had a relative importance between 7% and 24% (median 12%) and was second most important in one of the included five studies (25%).
Figure 3.
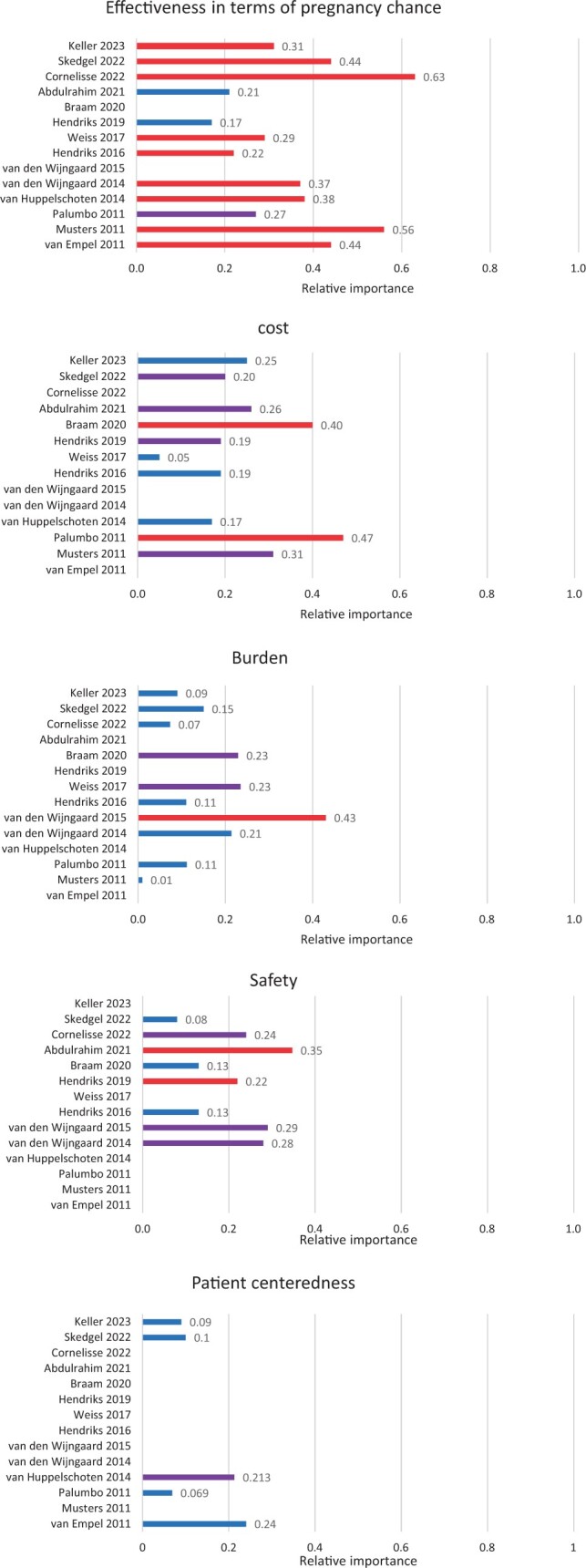
Relative importance of effectiveness, safety, cost, burden, and patient-centeredness in decision-making related to ART. Red = most important, purple = second most important, and blue = rest (third, fourth, fifth most important etc.).
Trade-offs
Twelve studies provided data on trade-offs that patients would be willing to make to gain something else.
Burden versus pregnancy rate
It was found that women could accept additional burden in exchange for higher pregnancy rates. For instance, women would choose injections over tablets for a 6.8% increase in pregnancy rates; as well as two hospital visits instead of none in exchange for an 8.9% increased pregnancy rate. (Weiss et al., 2017). Women were willing to accept a 5.2% decrease of pregnancy rate for 75 minutes less travel time (van Empel et al., 2011). Women were less willing to trade-off pregnancy rates for less burdening side-effects, importance of adherence, and duration of treatment. For less side effects, women were willing to accept a 0.8% decrease in pregnancy rate, for less importance of adherence this was 0.4%, and for a shorter duration of treatment, this was 0.3% (van den Wijngaard et al., 2014).
Safety
Participants were willing to accept a 1.3% reduction in the live birth rate in exchange for a 1% reduction in the risk of neonatal complications (Abdulrahim et al., 2021). Enduring more injections would be traded for a 6.2% decrease in risk of cycle cancellation or a 4.5% decrease in chance of OHSS (van den Wijngaard et al., 2015). Participants would also trade-off a 0.9% lower pregnancy rate for an OHSS risk reduction of 1.6% (van den Wijngaard et al., 2014). Women were willing to accept a 5.0% higher risk of cycle cancellation if the OHSS rate decreased by 2% (Braam et al., 2020). In addition, women accepted one extra IVF cycle for a reduction of 3.9% in OHSS risk (Braam et al., 2020).
Patient-centeredness
Patients would trade-off mean ongoing pregnancy rate for being treated with more patient-centeredness. One study found patients were willing to sacrifice 9.8% of pregnancy rate if being treated by a friendly, interested physician, or sacrifice 9.6% of pregnancy rate if getting clear and tailored information instead of contradictory information (van Empel et al., 2011). Continuity of physicians was worth a 4.0% decrease of pregnancy rate (van Empel et al., 2011).
Genetic parenthood
Although genetic parenthood did not influence decision-making statistically, one study stated that: ‘Patients would accept non-genetic parenthood over genetic parenthood in return for a pregnancy rate increase of 18%, a child health risk reduction of 3.6%, a cost reduction of €3500, an OHSS risk reduction of 4.6%, or a maternal cancer risk reduction of 2.7%’ (Hendriks et al., 2019).
Willingness to pay
More than half of the participants of one study would not pay extra for gains in comfort of drug administration or local tolerance of injections (Palumbo et al., 2011). In contrast, one study found patients were willing to pay more to avoid moderate side-effects €1303–€1786) and significant side effects (€2133–€2923), but the nature of these treatment-related side effects was not specified (Keller et al., 2023). Patients were also willing to pay €1000 for a decrease in OHSS rate of 5.4% (Braam et al., 2020).
In addition, patients were willing to pay a median of €463 for improved patient-centeredness (e.g. clearer information and more patient involvement; Huppelschoten et al., 2014), with higher income and age associated with greater willingness to pay. In the study of Skedgel et al. (2022), patients from Nordic countries and the USA would pay up to €3000 for ‘full’ shared decision-making.
Willingness to pay for higher pregnancy rate
The willingness to pay for improved pregnancy rates was evaluated by six studies and all found that patients were prepared to pay for more effectiveness. In one study, patients would pay €107 for 1% higher pregnancy rates (Huppelschoten et al., 2014), which is consistent with another study where 36% of participants were willing to pay €101–€300 for a 1–2% increase (Weiss et al., 2017). This is in the same range as €1000 in exchange for 5–14% increased pregnancy rates (Musters et al., 2011) or an additional €500 in exchange for an 8.9% increase in pregnancy rate (Palumbo et al., 2011). An Australian study (Keller et al., 2023) found patients were willing to pay €232–€317 for 1% increase in pregnancy rate, which is considerably more than in the European countries. Overall, the willingness to pay was dependent on patients’ income. Likewise, patients were willing to pay more for an increased likelihood of a live birth than for an improvement in any other attribute (Skedgel et al., 2022). Thereby, it was noted that ‘Nordic countries, Spain and the UK were willing to pay between €3000 and €3500 for a 15% absolute improvement in effectiveness, whilst respondents from the USA were willing to pay more than €6000’ (Skedgel et al., 2022).
Based on the relative importance of attributes and trade-offs, a schematic diagram was developed (Fig. 4).
Figure 4.
Visual representation of relative importance of attributes. Darker color represents higher priority of attributes.
Results of survey and interview studies
In five preference studies, effectiveness was seen as most important, but the child’s health was also regarded as very important in these studies (Bayram et al., 2005; Steures et al., 2005; van Weert et al., 2007; Duthie et al., 2017; Stormlund et al., 2019). Stormlund et al. (2019) found that women were even willing to accept risks to their own health in order to achieve a pregnancy. However, Hendriks et al. (2016) found that the safety of the child was slightly more important than pregnancy rates. In the study of Sills et al. (2012), effectiveness was not studied, but cost and burden were of equal importance. When costs were low (i.e. €90) most patients would pay extra for fewer injections, but not when costs increased.
Besides effectiveness, burden also played an important role in the study of Bayram et al. (2005), with some patients never opting for the offered treatment because they did not want to undergo surgery or inject hormones. In addition, genetic parenthood and costs were seen as a moderate priority (Duthie et al., 2017). As a hypothetical option, curing infertility was the third most important factor in one study (Hendriks et al., 2019). Costs, burden, natural process, and technological sophistication were of about equal importance in the same study.
Conceiving at home and moral acceptability of ART were found to be less important than the attributes mentioned earlier (Hendriks et al., 2016). A longer waiting time for embryo transfer and a more natural process without hormones were also less important in the decision-making process (Stormlund et al., 2019). Avoiding side effects was not as important to women as effectiveness or genetic parenthood in one study (Duthie et al., 2017). Risk of twin pregnancies was not important (Steures et al., 2005; van Weert et al., 2007).
Discussion
With this systematic review, we aimed to determine which attributes are valued most by ART patients with an unfulfilled wish to have a child. We identified 93 attributes in 20 studies that were classified as effectiveness, safety, burden, cost, patient-centeredness, genetic parenthood, and others. The most assessed attributes were burden, effectiveness (pregnancy rate), safety, costs, and patient-centeredness. The relative importance of attributes was established in 14 studies. We found that effectiveness was rated as the first or second most important factor in 83%, safety in 63%, cost in 50%, burden in 30%, and patient-centeredness in 25% of studies. This was in line with the six survey and structured interview studies that also found attributes related to effectiveness, safety, cost, and burden having most impact on decision-making.
A strength of this study is that we calculated the relative importance of the different attributes, thus enabling us to make more objective statements on the order of importance of the attributes. Although the studies included in this review were conducted in many different countries, patient preferences were very similar. This overlap in findings suggests that patient preference studies regarding ART treatments may be generalizable across different populations.
Although we limited our review to particular attributes of ART, by design, the included studies differed in assessed attributes and methodology. Effectiveness was included in almost every study, while genetic parenthood and other attributes, such as curing infertility, place of fertilization, chance of miscarriage, and importance of adherence, were only included in one or two studies; owing to the lack of representation in the studies, we were unable to assess their influence and therefore do not know whether these aspects are of importance to patients.
A large proportion of the included studies was performed in Europe, particularly in the Netherlands, and, although comparable choices were made across studies and suggest generalizability, we did find some notable differences between countries both within and between the studies. Within the largest study (Skedgel et al., 2022) among patients from the USA, China, and Europe, it was found that patient-centeredness and costs were not considered important in China, while particularly costs were almost as important as effectiveness in the USA. The authors suggest that this was related to differences in the health and reimbursement system. Similar to the USA, the Australian study (Keller et al., 2023) observed that patients were prepared to pay more for treatment success than in Europe, possibly due to less of the costs being reimbursed, resulting in significant out-of-pocket costs.
It is advisable to ascertain patients’ preferences before recommending certain treatments. Preference measurement approaches, particularly DCEs, have been shown to be effective instruments to understand decision-making in patients, as well as in providers and administrators (Salloum et al., 2017). Furthermore, although the choices that are made in the studies may differ from those made in real life (Hendriks et al., 2019), a previous study found that DCEs have moderate accuracy when predicting health-related choices (Quaife et al., 2018). In preference research, the non-random selection of participants and selection bias owing to non-response jeopardized the external validity. Such non-response tends not to be random, and most studies include, for example, highly educated patients earning (more than) modal income. Strategies need to be implemented to ensure that the participants included are representative of the target population.
Findings in context
Pregnancy rate was often only slightly more important than safety and never more important than child health risks. Two studies did not value effectiveness (pregnancy rate) as the most important attribute (Hendriks et al., 2019; Abdulrahim et al., 2021). In both of these studies, half of study participants were male partners, and both included neonatal complication as a safety attribute, which other DCEs did not include. In both studies, preventing neonatal complication was considered most important, particularly by the (male) partner.
In our review, burden was found to be less important when having to choose between different attributes, which is consistent with the study by Dancet et al., (2011) that found ‘physical burden’ to be one of the least important aspects. Likewise, a review indicated that physical burden of treatment was of minimal importance during first-order treatments, while psychological burden was a frequently named reason for patients to drop-out of the fertility program (Gameiro et al., 2012). This may imply that women are willing to endure quite some burden to have a child before starting ART, but that the reality of going through such treatments can be harder than expected (Cousineau and Domar, 2007; Copp et al., 2020). Unfortunately, psychological burden was not included as an attribute in the studies included in our review and may be considered in future preference studies. Much is still unknown about how psychological constructs relate to preference formation or differences in preferences between participants in general (Russo et al., 2019). However, in a recent study of patients experiencing unsuccessful IVF/ICSI cycles, 93.3% expressed a desire for psychosocial care, particularly when faced with a poor prognosis. Participants emphasized the need for personalized information on treatment options, outcomes, and comprehensive psychosocial support, as well as addressing coping strategies to process loss and sustain hope toward the future (Sousa-Leite et al., 2023).
Our findings on patient-centeredness are largely consistent with the literature. In line with a previous review, we found information provision to be an important aspect of patient-centeredness, together with time for discussions, personalized care, and friendly and interested providers (Dancet et al., 2010). Another study looked particularly at the role of the doctor and partner in decision-making in women with an unfulfilled wish to have a child. In this study, patient involvement in the decision-making process was valued as important by 92% of the patients (Chan et al., 2019). Patient involvement remains an attribute that needs further investigation.
Studies report different views on the importance of genetic parenthood. Two studies reported the importance of genetic parenthood for patients (Hendriks et al., 2017; Duthie et al., 2017), while another study reported that genetic parenthood did not influence decision-making (Hendriks et al., 2019). This could be partially explained by differences in study participants, where those who have tried to have a child for longer (Hendriks et al., 2019) may be more willing to accept non-genetic parenthood than patients who are in the earlier stages of infertility treatment (Duthie et al., 2017). Most couples in a study conducted in Iran had a preference for biological children rather than children conceived with donor gametes or adopted children, despite repeated treatment failure, low success rate, and high costs of infertility treatment (Behjati Ardakani et al., 2022). Cultural differences or sexual orientation may further explain the different levels of importance placed on genetic parenthood.
Implications for practice
The findings from this review can be used to inform patient-centered care guidelines. One of the key aspects of clinical practice guidelines is to provide information about the benefits and harms of specific interventions or treatments, to help healthcare providers and patients to make informed decisions that consider individual patients’ needs and preferences (Huppelschoten et al., 2013). Acknowledging the importance of information about all aspects of different treatment options can help to promote transparency in medical decision-making (Gärtner et al. 2019).
Implications for further research
To date, mental and psychological factors (e.g. burden) of fertility treatments remain understudied and could enrich research and contribute to better patient experiences and care in the future. Qualitative studies will be needed to find understudied attributes that are potentially relevant to patients. To study the importance of attributes and trade-offs, the preferred methodology is the DCE as this likely provides the most objective information. New DCEs may consider assessing an opt-out option as this is more representative of reality, rather than forcing patients to make a choice between treatment options when they might be in doubt.
The identification of driving factors in treatment decision-making for ART may stimulate further research. It would be of value to study whether the importance of driving factors shifts over time or over treatment trajectories. It is also unknown whether these factors influence risk of drop-out.
Conclusion
We found effectiveness of treatment, followed by safety, costs, and burden as the most important attributes determining patient preferences for ART. Patient-centeredness should also be considered in clinical practice and research, although its impact on decision-making is still unclear. Patients were prepared to trade-off some effectiveness for more safety, less burden, more patient-centeredness and were prepared to pay for more effectiveness.
The results of this review can be used in future preference studies, while they can also help healthcare professionals in guiding patients’ decision-making and enable a more patient-centered approach.
Supplementary Material
Contributor Information
Felicia von Estorff, Department of Obstetrics and Gynaecology, Centre for Reproductive Medicine, Amsterdam UMC, University of Amsterdam, Amsterdam, The Netherlands.
Monique H Mochtar, Department of Obstetrics and Gynaecology, Centre for Reproductive Medicine, Amsterdam UMC, University of Amsterdam, Amsterdam, The Netherlands; Amsterdam Reproduction and Development Research Institute, Amsterdam, The Netherlands.
Vicky Lehmann, Amsterdam Reproduction and Development Research Institute, Amsterdam, The Netherlands; Department of Medical Psychology, Amsterdam UMC, University of Amsterdam, Amsterdam, The Netherlands.
Madelon van Wely, Department of Obstetrics and Gynaecology, Centre for Reproductive Medicine, Amsterdam UMC, University of Amsterdam, Amsterdam, The Netherlands; Amsterdam Reproduction and Development Research Institute, Amsterdam, The Netherlands.
Supplementary data
Supplementary data are available at Human Reproduction Update online.
Data availability
The data underlying this article are available in the article and in its Supplementary Material.
Authors’ roles
F.v.E. and M.v.W. conceptualized and registered the study with V.L. and M.H.M. as advisors. F.v.E. and M.v.W. selected the studies and extracted the data and discussed the data with V.L. and M.H.M. All authors contributed to the writing of the article and approved the final version. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding
The present work was not externally funded but facilitated by the AmsterdamUMC.
Conflict of interest
The authors have no conflict of interest to declare.
References
- Abdulrahim B, Scotland G, Bhattacharya S, Maheshwari A.. Assessing couples’ preferences for fresh or frozen embryo transfer: a discrete choice experiment. Hum Reprod 2021;36:2891–2903. [DOI] [PubMed] [Google Scholar]
- Bayram N, van Wely M, van der Veen F, Bossuyt PM, Nieuwkerk P.. Treatment preferences and trade-offs for ovulation induction in clomiphene citrate-resistant patients with polycystic ovary syndrome. Fertil Steril 2005;84:420–425. [DOI] [PubMed] [Google Scholar]
- Behjati Ardakani Z, Navabakhsh M, Ranjbar F, Akhondi MM, Mohseni Tabrizi A.. Step-by-step decision-making process in third party assisted reproduction: a qualitative study. Hum Fertil (Camb) 2022;25:487–498. [DOI] [PubMed] [Google Scholar]
- Botha W, Donnolley N, Shanahan M, Chambers GM.. Assessment of the societal and individual preferences for fertility treatment in Australia: study protocol for stated preference discrete choice experiments. BMJ Open 2018;8:e020509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braam SC, de Bruin JP, Mol BWJ, van Wely M.. The perspective of women with an increased risk of OHSS regarding the safety and burden of IVF: a discrete choice experiment. Hum Reprod Open 2020;2020:hoz034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bridges JFP, Hauber AB, Marshall D, Lloyd A, Prosser LA, Regier DA, Johnson FR, Mauskopf J.. Conjoint analysis applications in health—a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health 2011;14:403–413. [DOI] [PubMed] [Google Scholar]
- Chan CHY, Lau BHP, Tam MYJ, Ng EHY.. Preferred problem solving and decision-making role in fertility treatment among women following an unsuccessful in vitro fertilization cycle. BMC Womens Health 2019;19:153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copp T, Kvesic D, Lieberman D, Bateson D, McCaffery KJ.. ‘Your hopes can run away with your realistic expectations’: a qualitative study of women and men’s decision-making when undergoing multiple cycles of IVF. Hum Reprod Open 2020;2020:hoaa059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornelisse S, Vos MS, Groenewoud H, Mastenbroek S, Ramos L, Braat DDM. et al. Women's preferences concerning IVF treatment: a discrete choice experiment with particular focus on embryo transfer policy. Hum Reprod Open 2022;3:hoac030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cousineau TM, Domar AD.. Psychological impact of infertility. Best Pract Res Clin Obstet Gynaecol 2007;21:293–308. [DOI] [PubMed] [Google Scholar]
- Dancet EA, Nelen WL, Sermeus W, De Leeuw L, Kremer JA, D'Hooghe TM.. The patients' perspective on fertility care: a systematic review. Hum Reprod Update 2010;16:467–487. [DOI] [PubMed] [Google Scholar]
- Dancet EA, Van Empel IW, Rober P, Nelen WL, Kremer JA, D'Hooghe TM.. Patient-centred infertility care: a qualitative study to listen to the patient's voice. Hum Reprod 2011;26:827–833. [DOI] [PubMed] [Google Scholar]
- Duthie EA, Cooper A, Davis JB, Sandlow J, Schoyer KD, Strawn E, Flynn KE.. Priorities for family building among patients and partners seeking treatment for infertility. Reprod Health 2017;14:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gameiro S, Boivin J, Peronace L, Verhaak CM.. Why do patients discontinue fertility treatment? A systematic review of reasons and predictors of discontinuation in fertility treatment. Hum Reprod Update 2012;18:652–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gärtner FR, Portielje JE, Langendam M, Hairwassers D, Agoritsas T, Gijsen B, Liefers GJ, Pieterse AH, Stiggelbout AM.. Role of patient preferences in clinical practice guidelines: a multiple methods study using guidelines from oncology as a case. BMJ Open 2019;9:e032483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendriks S, Hessel M, Mochtar MH, Meissner A, van der Veen F, Repping S, Dancet EAF.. Couples with non-obstructive azoospermia are interested in future treatments with artificial gametes. Hum Reprod 2016;31:1738–1748. [DOI] [PubMed] [Google Scholar]
- Hendriks S, Peeraer K, Bos H, Repping S, Dancet EAF.. The importance of genetic parenthood for infertile men and women. Hum Reprod 2017;32:2076–2087. [DOI] [PubMed] [Google Scholar]
- Hendriks S, van Wely M, D'Hooghe TM, Meissner A, Mol F, Peeraer K, Repping S, Dancet EAF.. The relative importance of genetic parenthood. Reprod Biomed Online 2019;39:103–110. [DOI] [PubMed] [Google Scholar]
- Huppelschoten AG, van Dongen AJCM, Philipse ICP, Hamilton CJCM, Verhaak CM, Nelen WLDM, Kremer JAM.. Predicting dropout in fertility care: a longitudinal study on patient-centredness. Hum Reprod 2013;28:2177–2186. [DOI] [PubMed] [Google Scholar]
- Huppelschoten AG, Verkerk EW, Appleby J, Groenewoud H, Adang EMM, Nelen WLDM, Kremer JAM.. The monetary value of patient-centred care: results from a discrete choice experiment in Dutch fertility care. Hum Reprod 2014;29:1712–1720. [DOI] [PubMed] [Google Scholar]
- Keller E, Botha W, Chambers GM.. What features of fertility treatment do patients value? Price elasticity and willingness-to-pay values from a discrete choice experiment. Appl Health Econ Health Policy 2023;21:91–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klitzman R. Impediments to communication and relationships between infertility care providers and patients. BMC Womens Health 2018;18:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Louviere JJ, Flynn TN, Carson RT.. Discrete choice experiments are not conjoint analysis. J Choice Model 2010;3:57–72. [Google Scholar]
- Malin M, Hemmink E, Räikkönen O, Sihvo S, Perälä ML.. What do women want? Women's experiences of infertility treatment. Soc Sci Med 2001;53:123–133. [DOI] [PubMed] [Google Scholar]
- Musters AM, de Bekker-Grob EW, Mochtar MH, van der Veen F, van Mello NM.. Women's perspectives regarding subcutaneous injections, costs and live birth rates in IVF. Hum Reprod 2011;26:2425–2431. [DOI] [PubMed] [Google Scholar]
- Page MJ, , McKenzieJE, , BossuytPM, , BoutronI, , HoffmannTC, , MulrowCD, , ShamseerL, , TetzlaffJM, , AklEA, , Brennan SE. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palumbo A, De La Fuente P, Rodríguez M, Sánchez F, Martínez-Salazar J, Muñoz M, Marqueta J, Hernández J, Espallardo O, Polanco C. et al. Willingness to pay and conjoint analysis to determine women's preferences for ovarian stimulating hormones in the treatment of infertility in Spain. Hum Reprod 2011;26:1790–1798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quaife M, Terris-Prestholt F, Di Tanna GL, Vickerman P.. How well do discrete choice experiments predict health choices? A systematic review and meta-analysis of external validity. Eur J Health Econ 2018;19:1053–1066. [DOI] [PubMed] [Google Scholar]
- Reed Johnson F, Lancsar E, Marshall D, Kilambi V, Mühlbacher A, Regier DA, Bresnahan BW, Kanninen B, Bridges JFP.. Constructing experimental designs for discrete-choice experiments: report of the ISPOR Conjoint Analysis Experimental Design Good Research Practices Task Force. Value Health 2013;16:3–13. [DOI] [PubMed] [Google Scholar]
- Russo S, Jongerius C, Faccio F, Pizzoli SFM, Pinto CA, Veldwijk J, Janssens R, Simons G, Falahee M, de Bekker-Grob E. et al. Understanding patients' preferences: a systematic review of psychological instruments used in patients' preference and decision studies. Value Health 2019;22:491–501. [DOI] [PubMed] [Google Scholar]
- Salloum RG, Shenkman EA, Louviere JJ, Chambers DA.. Application of discrete choice experiments to enhance stakeholder engagement as a strategy for advancing implementation: a systematic review. Implement Sci 2017;12:140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sills ES, Collins GS, Salem SA, Jones CA, Peck AC, Salem RD.. Balancing selected medication costs with total number of daily injections: a preference analysis of GnRH-agonist and antagonist protocols by IVF patients. Reprod Biol Endocrinol 2012;10:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skedgel C, Ralphs E, Finn E, Markert M, Samuelsen C, Whitty JA.. How do people with experience of infertility value different aspects of assistive reproductive therapy? Results from a multi-country discrete choice experiment. Patient 2022;15:459–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sousa-Leite M, Costa R, Figueiredo B, Gameiro S.. Discussing the possibility of fertility treatment being unsuccessful as part of routine care offered at clinics: patients' experiences, willingness, and preferences. Hum Reprod 2023;38:1332–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steures P, Berkhout JC, Hompes PGA, van der Steeg JW, Bossuyt PMM, van der Veen F, Habbema JDF, Eijkemans MJC, Mol BWJ.. Patients' preferences in deciding between intrauterine insemination and expectant management. Hum Reprod 2005;20:752–755. [DOI] [PubMed] [Google Scholar]
- Stormlund S, Schmidt L, Bogstad J, Løssl K, Prætorius L, Zedeler A, Pinborg A.. Patients’ attitudes and preferences towards a freeze-all strategy in ART treatment. Hum Reprod 2019;34:679–688. [DOI] [PubMed] [Google Scholar]
- Twisk M, van der Veen F, Repping S, Heineman MJ, Korevaar JC, Bossuyt PM.. Preferences of subfertile women regarding elective single embryo transfer: additional in vitro fertilization cycles are acceptable, lower pregnancy rates are not. Fertil Steril 2007;88:1006–1009. [DOI] [PubMed] [Google Scholar]
- van den Wijngaard L, Rodijk ICM, van der Veen F, Gooskens-van Erven MHW, Koks CAM, Verhoeve HR, Mol BWJ, van Wely M, Mochtar MH.. Patient preference for a long-acting recombinant FSH product in ovarian hyperstimulation in IVF: a discrete choice experiment. Hum Reprod 2015;30:331–337. [DOI] [PubMed] [Google Scholar]
- van den Wijngaard L, van Wely M, Dancet EAF, van Mello NM, Koks CAM, van der Veen F, Mol BWJ, Mochtar MH.. Patients' preferences for gonadotrophin-releasing hormone analogs in in vitro fertilization. Gynecol Obstet Invest 2014;78:16–21. [DOI] [PubMed] [Google Scholar]
- van der Horst DEM, Garvelink MM, Bos WJW, Stiggelbout AM, Pieterse AH.. For which decisions is shared decision making considered appropriate?—a systematic review. Patient Educ Couns 2023;106:3–16. [DOI] [PubMed] [Google Scholar]
- van Empel IWH, Dancet EAF, Koolman XHE, Nelen WLDM, Stolk EA, Sermeus W, D'Hooghe TM, Kremer JAM.. Physicians underestimate the importance of patient-centredness to patients: a discrete choice experiment in fertility care. Hum Reprod 2011;26:584–593. [DOI] [PubMed] [Google Scholar]
- van Weert J-M, van den Broek J, van der Steeg JW, van der Veen F, Flierman PA, Mol BWJ, Steures P.. Patients' preferences for intrauterine insemination or in-vitro fertilization. Reprod Biomed Online 2007;15:422–427. [DOI] [PubMed] [Google Scholar]
- Weiss NS, Schreurs AMF, van der Veen F, Hompes PGA, Lambalk CB, Mol BW, van Wely M.. Women's perspectives on ovulation induction with or without IUI as treatment for normogonadotrophic anovulation: a discrete choice experiment. Hum Reprod Open 2017;2017:hox021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Alonso-Coello P, Guyatt GH, Yepes-Nuñez JJ, Akl EA, Hazlewood G, Pardo-Hernandez H, Etxeandia-Ikobaltzeta I, Qaseem A, Williams JW. et al. GRADE Guidelines: 19 Assessing the certainty of evidence in the importance of outcomes or values and preferences-Risk of bias and indirectness. J Clin Epidemiol 2019;111:94–104. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in the article and in its Supplementary Material.