Abstract
Impacts of the COVID-19 pandemic in the United States have been exacerbated by preexisting inequities in resources and opportunities, leaving the most vulnerable to face a multitude of hardships. The goal of the current study was to characterize COVID-19 related stressful life events in specific life domains and to identify the sociodemographic characteristics of individuals who are more likely to experience such events. Participants (n=372, 57% female) in a follow-up study of the NICHD Study of Early Child Care and Youth Development (SECCYD) completed the Epidemic-Pandemic Impacts Inventory (June-August 2020) to assess COVID-19 related stressors. Sociodemographic factors (gender, race/ethnicity, socioeconomic status, and wealth) were examined simultaneously as predictors of the number of stressful life events in separate categories of work/finances, home life, social activity, health, and healthcare, adjusted for covariates (household size, community COVID-19 transmission risk). In negative binomial regression analyses, being female (vs. male) predicted a 31%, 64%, 13%, and 94% increase in the number of stressful life events in domains of work/finances, home life, social activity, and healthcare, respectively, while each one standard deviation increase in wealth predicted a 17%, 16%, and 21% reduction in the number of stressful life events in domains of work/finances, COVID-19 infection, and healthcare, respectively. Findings highlight the pronounced and far-reaching impacts of the COVID-19 pandemic on women as well as the unique role wealth may play in lessening such impacts. This new knowledge may be leveraged to develop intervention and policy-related strategies to remediate impacts of COVID-19 related stressors on those most vulnerable.
Keywords: COVID-19 pandemic, coronavirus disease pandemic, stressful life events, gender, socioeconomic status, wealth, SECCYD
Introduction
The consequences of the COVID-19 pandemic in the United States have been unprecedented in scope, negatively impacting diverse areas of employment, home life, social activity, health, and healthcare (Banerjee & Rai, 2020; Mattioli, Sciomer, Cocchi, Maffei, & Gallina, 2020; Patrick et al., 2020; Woolhandler & Himmelstein, 2020). Moreover, pre-existing inequities in resources and opportunities (e.g., unsafe working conditions; lack of access to healthcare) have exacerbated these impacts, leaving the most vulnerable to face a multitude of hardships. Among those groups most affected are women as well as individuals of racial/ethnic minority and socioeconomically disadvantaged backgrounds (Clouston, Natale, & Link, 2021; Connor et al., 2020; Krouse, 2020).
This unfortunate reality, although spurred by the COVID-19 pandemic, reflects a broader underlying dynamic, well-documented in the social determinants of health (SDH) literature. That is, SDH models suggest the social conditions of individuals may be causal factors accounting for disparities in health outcomes (e.g., Braveman & Gottlieb, 2014; Marmot & Allen, 2014; Phelan, Link, & Tehranifar, 2010). This framework likely extends to better understanding COVID-19 related outcomes as well. However, more work is needed to first examine disparities in specific COVID-19 related stressors, both with respect to the type and magnitude of stress experienced and to the specific sociodemographic characteristics of individuals who are more vulnerable to experiencing such stressors.
Women and the COVID-19 pandemic
Women in the United States have been disproportionately impacted by the COVID-19 pandemic. Since the pandemic began, 2.3 million women have fallen out of the U.S. workforce compared to 1.8 million men, including working mothers who left the workforce to accommodate the loss of childcare and the demands of remote schooling (Rothwell & Saad, 2021; “US Bureau of Labor Statistics. Labor Force Statistics from the Current Population Survey,” 2021, April 2). Women are especially vulnerable financially, as more women than men report not being able to afford necessities (e.g., housing, food) for more than a month if they lost their income (Lean In & SurveyMonkey, 2020) and single mothers have almost no financial reserve to draw from in the event of a crisis like job loss (Zaw, Bhattacharya, Price, Hamilton, & Darity Jr, 2017). In addition, women have incurred the increased burden of care for their families during the pandemic on top of existing household responsibilities commonly assumed by women (e.g., management of household activities and schedules) (Moreira da Silva, 2019; Power, 2020). Moreover, violence against women has increased during the pandemic (Peterman et al., 2020; Sánchez, Vale, Rodrigues, & Surita, 2020), possibly fueled by the social isolation experienced as a result of social distancing and quarantining measures, as well as by concomitant stressors such as increased financial stress (Morgan & Boxall, 2020).
Socioeconomic disadvantage and the COVID-19 pandemic
Individuals from socioeconomically disadvantaged backgrounds in the United States have also been disproportionately impacted by the COVID-19 pandemic. Workers who were part-time, hourly, or lower wage earners were more likely to experience reduced or total loss of employment during the pandemic and to report greater worry about this possibility (Kirzinger, 2020; Parker, 2020). Disparate impacts on workers are especially pronounced when examined across employment sectors. In the U.S. financial and information industries, in which wages are among the highest, there were few overall job losses followed by a quick and full recovery, while in the U.S. leisure and hospitality industries, in which wages are among the lowest, half of jobs were lost with a slow and limited recovery (Ghilarducci, 2021). Problems among socioeconomically disadvantaged groups during the pandemic extended to increased social problems with friends and family and increased symptoms of depression and anxiety, with such changes possibly driven or intensified by income insecurity (Rudenstine et al., 2021). Finally, closures of community health care centers and barriers facing lower-resourced hospital systems, particularly with respect to transitioning to telehealth services (i.e., lack of needed technology), disproportionately impacted services to lower income communities (Shin, Morris, Velasquez, Rosenbaum, & Somodevilla, 2020), likely only furthering underlying disparities in health—including rates of COVID-19 infection and death (Holmes Finch & Hernández Finch, 2020; Liao & De Maio, 2021).
Socioeconomic disadvantage is typically defined by income level and educational attainment. However, consideration of the accumulation of resources or ‘wealth’ is also important when examining impacts of a crisis such as the pandemic. Wealth provides a safety net that protects individuals from the immediate impacts of events such as job loss and may reduce psychological stress that potentiates problems in other areas (e.g., social relationships). For example, lower household savings was associated with an increase in risk for anxiety among lower income individuals during the pandemic (Rudenstine et al., 2021) and carrying debt more generally has been associated with feelings of hopelessness and frustration (Drentea & Reynolds, 2015). Various wealth indicators (e.g., home ownership, savings, and stocks), have also been associated with better physical health across a range of outcomes, including better self-rated health, fewer health conditions, and lower body mass index (Boen, Keister, & Aronson, 2020; Robert & House, 1996).
Building on the existing literature showing disparate impacts of the COVID-19 pandemic on individuals from vulnerable groups in the United States, the current study sought to examine a range of COVID-19 related stressors and the sociodemographic characteristics of individuals that may put them at risk of experiencing such stressors. The current study included a subset of 374 participants in a follow-up study of the landmark NICHD Study of Early Child Care and Youth Development (SECCYD) who subsequently completed a questionnaire pertaining to impacts of the COVID-19 pandemic. The goals of the current study were 1) to characterize stressful life events experienced as a result of the COVID-19 pandemic in five domains (i.e., work/finances, home life, social activity, health, and healthcare) and 2) to examine the extent to which sociodemographic factors (i.e., gender, race/ethnic minority status, SES, and wealth) account for disparities in these outcomes. Based on findings from prior studies of COVID-19 impacts, we hypothesized that women and individuals of racial/ethnic minority and lower SES backgrounds would experience a higher number of COVID-19 related stressful life events and that wealth, as a marker of financial reserve or stability, would predict these outcomes even independently of SES, indexed by education and income. Hypotheses were not specified, however, with respect to specific domains of stressful life events.
Methods
Participants
Participants were drawn from the NICHD SECCYD, a prospective investigation of children and their families followed between birth and adolescence. Families (N=1364) were recruited in 1991 from 10 study sites across the United States. Details regarding the sample and inclusion criteria have been reported previously (NICHD Early Child Care Research Network, 2005). Currently, an SECCYD follow-up study—the Study of Health in Early and Adult Life (SHINE)—is underway to locate these children now in adulthood (late 20s to early 30s). SHINE entails an in-person study visit collecting extensive social, behavioral, and health data. Retained for analysis in the current study were participants in SHINE between January 2018 and March 2020 who subsequently completed a self-report questionnaire assessing impacts of the COVID-19 pandemic. The questionnaire was administered over a 3-month period between June and August 2020, beginning approximately 4 months after the first case of COVID-2019 was diagnosed in the U.S. (Holshue et al., 2020). The newly collected questionnaire data were then merged with the relevant SHINE data for analysis. Of the 430 eligible SHINE participants, 374 (87.0%) completed the questionnaire. This subset of participants is being examined in the current study ahead of the completion of the SHINE Study due to its timely focus on understanding impacts of the COVID-19 pandemic. Informed consent for the SECCYD follow-up study, SHINE, was obtained from the now adult children and the research was approved by the Human Subjects Division of the University of Washington.
Measures
Predictors: Sociodemographic factors
The sociodemographic factors of interest included self-identified gender (female=1, male=0), self-identified minority race/ethnic status (minority status=1, white, non-Hispanic=0), an SES composite of education and income, and a wealth composite of items reflecting accumulated wealth or financial stability. Items contributing to the SES and wealth composites were all assessed by self-report questionnaire at the time of the SECCYD follow-up study, SHINE. The SES composite included the participant’s individual-level educational attainment and total combined household income. Educational attainment was measured by self-report in categories: 1=less than high school; 2=high school or general education diploma; 3=some college or vocational degree; 4=college degree; 5=some graduate school or master’s degree; and 6=graduate degree greater than a master’s degree. Total combined household income was measured in categories ranging between <$5,000 and $300,000+. Household income included income from all sources (e.g., wages, veteran’s benefits, help from relatives) in the past 12 months, which was then divided by the number of dependents supported by the income. The indicated values were then standardized, summed, and re-standardized to produce a single composite of SES. The wealth composite included 7 items: 1) length of time able to live in current home and maintain current standard of living if lost all sources of household income (categories: ‘<1 month’, ‘1–2 months’, ‘3–6 months’, ‘7–12 months’, ‘>1 year’); 2) difficulty paying for basics like food and heating (rated on 5-point scale: ‘not at all difficult’ to ‘extremely difficult’); 3) endorsement of homeownership by self or other person living in the home (‘yes’/’no’); 4) rating of the condition of the home (categories: ‘very well kept/attractive for its type’, ‘moderately well kept’, ‘fair condition/needs repair’, ‘poor/badly deteriorated condition’; 5) number of bedrooms in home; 6) number of working motor vehicles owned; 7) took out-of-town vacation in the past year (‘yes’/’no’). All items were coded with higher values reflecting greater wealth. The indicated values were then standardized, summed, and re-standardized to produce a single composite of wealth.
Predictors: Covariates
The covariates included household size and community COVID-19 transmission risk assessed in the local areas of the participants. Household size was measured by self-report of the number of individuals living in the home, including the participant. Community COVID-19 transmission risk was measured using the data repository for the 2019 Novel Coronavirus Visual Dashboard operated by the Johns Hopkins University Center for Systems Science and Engineering https://github.com/CSSEGISandData/COVID-19. Data pertaining to county-level case incidence rates and case-fatality ratios were extracted based on the provided residential address and the date the COVID-19 impacts questionnaire was completed. The case incidence rate was defined as the cumulative confirmed cases divided by the county population x 100,000. The case-fatality ratio was defined as deaths divided by the cumulative confirmed cases. These two indicators were standardized, summed, and re-standardized to form a single composite of community COVID-19 transmission risk.
Outcomes: COVID-19 related stressful life events
Participants who already completed the SHINE study were invited to also complete the Epidemic-Pandemic Impacts Inventory (EPII) (Grasso, Briggs-Gowan, Ford, & Carter, 2020). The EPII was selected for administration following review of measures available through the NIH Repository of COVID-19 Research Tools on the US Department of Health and Human Services, NIH Public Health Emergency and Disaster Research Response (DR2) website: https://dr2.nlm.nih.gov/. The EPII assesses impacts of the COVID-19 pandemic in a variety of domains. Participants were asked: “Since the coronavirus disease pandemic began, what has changed for you and your family”? Participants responded to 92 specific statements or events by indicating ‘yes’ or ‘no’ regarding whether they were impacted by the event. In addition, in alignment with other life events questionnaires, a modification was made to the EPII in which all events endorsed ‘yes’ were rated using 5 ordinal categories reflecting the intensity of the impact: 0=no impact…2=moderate negative/positive impact…4=extreme negative/positive impact, according to the valence of the event. Because the EPII is newly developed, research supporting its scoring and psychometric properties is limited. Use of the EPII in the current study will contribute to the knowledge base regarding the further development and potential refinement of this questionnaire.
The current study focused only on a subset of the questions in the EPII. These items pertained to stressful life events in areas of work/finances, home life, social activity, health, and healthcare. Five EPII subscale scores were calculated representing the total number of events in these domains. Specifically, items that were endorsed ‘yes’ and rated 1+ on the impact rating scale (0=no impact… 2=moderate negative impact… 4=extreme negative impact) were summed to produce a 1) ‘Work/Financial Events’ subscale score (15 items); 2) ‘Home Disruption Events’ subscale score (17 items); 3) ‘Social Isolation Events’ subscale score (15 items); 4) ‘COVID-19 Infection Events’ subscale score (11 items); and 5) ‘Healthcare Barrier Events’ subscale score (7 items). Only items with impact ratings of 1+ (i.e., moderate negative impact or greater) were included in the subscales to ensure that the stressful life events that were experienced, in fact, had a meaningful impact on the participants’ lives.
Analytical Plan
Separate negative binomial regression models were fit to examine sociodemographic predictors of counts of COVID-19 related stressful life events in 5 domains (‘Work/Financial Events’, ‘Home Disruption Events’, ‘Social Isolation Events’, ‘COVID-19 Infection Events’, and ‘Healthcare Barrier Events’), adjusted for covariates (household size, community COVID-19 transmission risk). Analyses were performed examining three sociodemographic predictors simultaneously (gender, minority status, and the SES composite) and then repeated adding the wealth composite. This approach was taken to allow examination of the contribution of wealth uniquely. Results are reported from the final models, including incident rate ratios (IRR), 95% confidence intervals, and p-values. In addition, interactions were explored examining gender and minority status as potential moderators of effects of SES and wealth on counts of stressful life events as well as wealth as a moderator of SES effects on counts of stressful life events. For two participants missing values for the income variable, the SES composite was represented by educational attainment only. Prior to conducting the main analyses, variables in the analytic models were subjected to Little’s Test (Little, 1988), showing the data were missing completely at random (MCAR) (χ2=13, df=23, p=.952). Analyses were performed using Stata 13 software (College Station, TX).
Results
Descriptive Analyses
As shown in Table 1, the sample was 57% female and 29.1 (SD=0.2, range: 28.6–29.5) years of age on average. The racial/ethnic composition was 79.7% white, non-Hispanic (NH), 6.7% Hispanic, 8.8% black NH, 1.6% Asian NH, and 3.2% ‘other’ NH. The SES indicators revealed 62.8% held a college degree or higher and 24.1% had a household income $100,000/year or greater. The wealth indicators revealed 17.6% were able to maintain their current standard of living for more than a year if they lost all sources of income and 42.2% endorsed home ownership. Regarding community-level COVID-19 transmission risk, the mean case incidence rate was 633.3 (SD=609.7, range: 24.8–2630.5) per 100,000 persons and the mean case-fatality ratio was 4.2 (SD=2.7, range: 0–12.5).
Table 1.
Characteristics of the sample regarding sociodemographic factors and covariates (n = 374).
| n (%) | Mean (SD) | Range | |
|---|---|---|---|
| Age (years) | - | 29.1 (0.2) | 28.6 – 29.5 |
| Gender (% female) | 213 (57.0) | - | - |
| Race/ethnicity: | |||
| White, non-Hispanic (%) | 298 (79.7) | - | - |
| Non-white (%): | 76 (20.3) | - | - |
| Latino (%) | 25 (6.7) | - | - |
| Black, non-Hispanic (%) | 33 (8.8) | - | - |
| Asian, non-Hispanic (%) | 6 (1.6) | - | - |
| Other, non-Hispanic (%) | 12 (3.2) | - | - |
| SES: | |||
| Education, (college degree+, %) | 235 (62.8) | - | - |
| Household income ($100,000+/year, %) | 90 (24.1) | - | - |
| Wealth indicators: | |||
| Maintain current standard of living if lost all household income (‘>1 year’, %) | 66 (17.6) | - | - |
| Difficulty paying for basics (‘not at all’, %) | 465 (70.9) | - | - |
| Home ownership (‘yes’, %) | 158 (42.2) | - | - |
| Condition of home (‘very well kept’, %) | 194 (51.9) | - | - |
| Number of bedrooms (3+, %) | 195 (52.1) | - | - |
| Number of cars (2+, %) | 96 (25.7) | - | - |
| Take out-of-town vacation (‘yes’, %) | 332 (88.8) | - | - |
| Household size | - | 2.6 (1.4) | 1–10 |
| Community COVID-19 case incidence rate, county-level | - | 633.3 (609.7) | 24.8 – 2630.5 |
| Community COVID-19 case-fatality ratio, county-level | - | 4.2 (2.7) | 0 – 12.5 |
In Table 2, frequencies for all the individual items represented in the 5 domains of stressful life events (EPII subscales) are reported. For brevity, only examples from each domain are highlighted here: 14.2% were laid off from work or had to close their business (Work/Financial events); 61.5% experienced increases in mental health problems (Home disruption events); 76.7% experienced cancelations or restrictions on family celebrations (Social isolation events); 29.9% were quarantined due to possible COVID-19 exposure (COVID-19 infection events); and 22.5% received less routine or preventative care than usual (Healthcare barrier events).
Table 2.
Descriptive statistics for the five COVID-19 related stressful life events domains and the frequencies of the individual items in these domains.
| n (%) | Mean (SD) | Range | |
|---|---|---|---|
| COVID-19 related stressful life events: | |||
|
| |||
| Work/financial events: | - | 1.9 (1.6) | 0–7 |
|
| |||
| Laid off from job or had to close own business | 53 (14.2) | - | - |
| Reduced work hours or furloughed | 91 (24.3) | - | - |
| Had to lay-off or furlough employees or people supervised | 15 (4.0) | - | - |
| Had to continue to work even though in close contact with people who might be infected | 96 (25.7) | - | - |
| Spent a lot of time disinfecting at home due to close contact with people who might be infected at work | 87 (23.3) | - | - |
| Experienced increase in workload or work responsibilities | 125 (33.4) | - | - |
| Had hard time doing job well because of needing to take care of people in the home | 34 (9.1) | - | - |
| Had hard time making the transition to working from home | 65 (17.4) | - | - |
| Unable to go to school or training for weeks or had to withdraw | 30 (8.0) | - | - |
| Had to move or relocate | 16 (4.3) | - | - |
| Became homeless | 2 (0.5) | - | - |
| Unable to get enough food or healthy food | 13 (3.5) | - | - |
| Unable to access clean water | 0 (0.0) | - | - |
| Unable to pay important bills like rent or utilities | 32 (8.6) | - | - |
| Had difficulty getting places due to less access to public transportation or concerns about safety | 38 (10.2) | - | - |
|
| |||
| Home disruption events: | - | 2.1 (2.1) | 0–13 |
|
| |||
| Had child in home who could not go to school | 33 (8.8) | - | - |
| Childcare or babysitting unavailable when needed | 28 (7.5) | - | - |
| Difficulty taking care of children in the home | 25 (6.7) | - | - |
| More conflict with child or harsher in disciplining child or children | 19 (5.1) | - | - |
| Had to take over teaching or instructing a child | 28 (7.5) | - | - |
| Family or friends had to move into your home | 7 (1.9) | - | - |
| Had to spend a lot more time taking care of a family member | 23 (6.1) | - | - |
| Increase in verbal arguments or conflict with a partner or spouse | 61 (16.3) | - | - |
| Increase in physical conflict with a partner or spouse | 7 (1.9) | - | - |
| Increase in verbal arguments or conflict with other adult(s) in home | 27 (7.2) | - | - |
| Increase in physical conflict with other adult(s) in home | 1 (0.3) | - | - |
| Increase in physical conflict among children in home | 2 (0.5) | - | - |
| Increase in mental health problems or symptoms | 230 (61.5) | - | - |
| Increase in sleep problems or poor sleep quality | 145 (38.8) | - | - |
| Increase in use of alcohol or substances | 103 (27.5) | - | - |
| Increase in child behavioral or emotional problems | 32 (8.6) | - | - |
| Increase in child’s sleep difficulties or nightmares | 16 (4.3) | - | - |
|
| |||
| Social isolation events: | - | 4.6 (2.0) | 0–11 |
|
| |||
| Separated from family or close friends | 294 (78.6) | - | - |
| Did not have the ability or resources to talk to family or friends while separated | 16 (4.3) | - | - |
| Unable to visit loved one in a care facility (e.g., nursing home, group home) | 55 (14.7) | - | - |
| Family celebrations cancelled or restricted | 287 (76.7) | - | - |
| Planned travel or vacations cancelled | 246 (65.8) | - | - |
| Religious or spiritual activities cancelled or restricted | 84 (22.5) | - | - |
| Unable to be with a close family member in critical condition | 39 (10.4) | - | - |
| Unable to attend in-person funeral or religious services for a family member or friend who died | 34 (9.1) | - | - |
| Unable to participate in social clubs, sports teams, or usual volunteer activities | 164 (43.9) | - | - |
| Unable to do enjoyable activities or hobbies | 274 (73.3) | - | - |
| Limited physical closeness with child or loved one due to concerns of infection | 91 (24.3) | - | - |
| Moved out or lived away from family due to a high-risk job (e.g., health care worker, first responder) | 6 (1.6) | - | - |
| Close family member not in the home was quarantined | 33 (8.8) | - | - |
| Family member was unable to return home due to quarantine or travel restrictions | 13 (3.5) | - | - |
| Entire household was quarantined for a week or longer | 71 (19.0) | - | - |
|
| |||
| COVID-19 infection events: | - | 0.5 (0.8) | 0–4 |
|
| |||
| Isolated or quarantined due to possible exposure to this disease | 112 (29.9) | - | - |
| Isolated or quarantined due to symptoms of this disease | 24 (6.4) | - | - |
| Isolated due to existing health conditions that increase risk of infection or disease | 24 (6.4) | - | - |
| Currently have symptoms of this disease but have not been tested | 1 (0.3) | - | - |
| Tested and currently have this disease | 0 (0.0) | - | - |
| Had symptoms of this disease but never tested | 25 (6.7) | - | - |
| Tested positive for this disease but no longer have it | 4 (1.1) | - | - |
| Got medical treatment due to severe symptoms of this disease | 3 (0.8) | - | - |
| Hospital stay due to this disease | 0 (0.0) | - | - |
| Someone died of this disease while in our home | 0 (0.0) | - | - |
| Death of close friend or family member from this disease | 10 (2.7) | - | - |
|
| |||
| Healthcare barrier events: | - | 0.5 (0.8) | 0–5 |
|
| |||
| Unable to get needed medications (e.g., prescriptions or over-the-counter) | 8 (2.1) | - | - |
| Unable to access mental health treatment or therapy | 31 (8.3) | - | - |
| Not satisfied with changes in mental health treatment or therapy | 27 (7.2) | - | - |
| Important medical procedures cancelled (e.g., surgery) | 10 (2.7) | - | - |
| Unable to access medical care for a serious condition (e.g., dialysis, chemotherapy) | 1 (0.3) | - | - |
| Got less medical care than usual (e.g., routine or preventive care appointments) | 84 (22.5) | - | - |
| Elderly or disabled family member not in the home unable to get the help they need | 13 (3.5) | - | - |
Unadjusted Analyses
In Table 3, correlations between the sociodemographic factors, covariates, and five domains of stressful life events (EPII subscales) are reported. Associations between the sociodemographic factors and the stressful life events showed being female (vs. male) was significantly associated with a higher number of events in four domains: ‘Work/Financial Events’, ‘Home Disruption Events’, ‘Social Isolation Events’, and ‘Healthcare Barrier Events’ (all ps<.05). Minority status (vs. white, non-Hispanic) was significantly associated with a higher number of events in one domain: ‘Work/Financial Events’ (p<.05). Higher SES was significantly associated with a lower number of events in the ‘Work/Financial Events’ and ‘Home Disruption Events’ domains (all ps<.001) but a higher number of events in the ‘Social Isolation Events’ domain (p<.001). Greater wealth was significantly associated with a lower number of events in three domains: ‘Work/Financial Events’, ‘COVID-19 Infection Events’, and ‘Healthcare Barrier Events’ (all ps<.05).
Table 3.
Bivariate correlations between the sociodemographic factors, covariates, and the five COVID-19 related stressful life events domains.
| Variables: | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Gender | - | −.017 | −.041 | −.037 | .076 | −.087 | .161** | .246*** | .120* | −.079 | .180*** |
| 2. Minority status | - | −.200*** | −.044 | .061** | −.009 | .128* |
.060 | −.033 | −.002 | −.036 | |
| 3. SES composite | - | .209*** | −.424*** | .201*** | −.204*** | −.254*** | .215*** | .022 | −.039 | ||
| 4. Wealth composite | - | .130* | .014 | −.244*** | −.093 | .038 | −.108* | −.130* | |||
| 5. Household size | - | −.026 | .146** | .316*** | −.039 | −.007 | .048 | ||||
| 6. Community COVID-19 risk | - | −.015 | .028 | .126* | .170** | −.033 | |||||
| 7. Work/financial events | - | .364*** | .297*** | .170** | .266*** | ||||||
| 8. Home disruption events | - | .156** | .100 | .228*** | |||||||
| 9. Social isolation events | - | .307*** | .233*** | ||||||||
| 10. COVID-19 infection events | - | .182*** | |||||||||
| 11. Healthcare barrier events | - |
Gender: female=1, male=0; Minority race/ethnic status: minority status=1, white, non-Hispanic=0; SES and Wealth composites: higher values reflect higher SES and wealth
p<.05;
p<.01;
p<.001
Adjusted Analyses
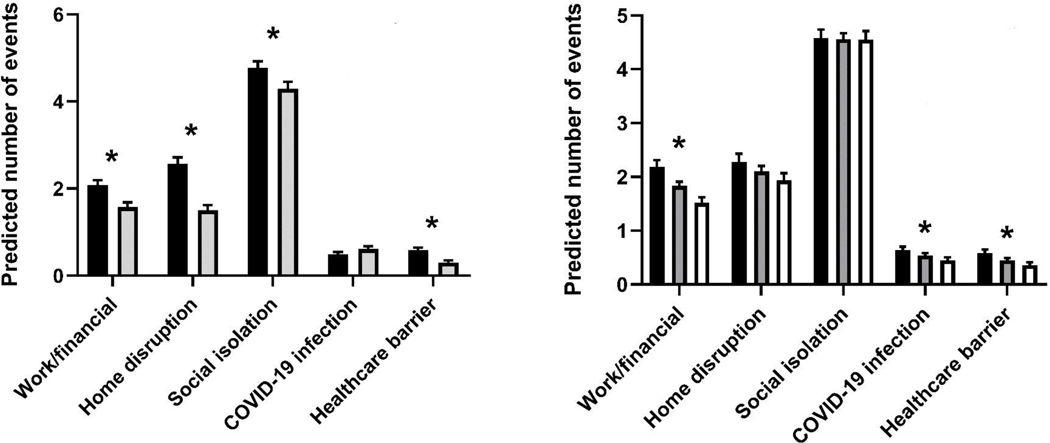
In Table 4, results of negative binomial regression analyses are reported, predicting counts of stressful life events in five domains (EPII subscales) by the indicated sociodemographic factors, adjusted for covariates. In the final models in which the sociodemographic predictors, including the wealth composite, were examined simultaneously, a higher number of ‘Work/Financial Events’ was predicted by female gender (IRR=1.293, 95% CI=1.091–1.531, p=.003) and lower wealth (IRR=0.833, 95% CI=0.767–0.905, p=.000). A higher number of ‘Home Disruption Events’ was predicted by greater household size (IRR=1.174, 95% CI=1.092–1.261, p=.000), higher community COVID-19 transmission risk (IRR=1.103, 95% CI=1.006–1.210, p=.037), female gender (IRR=1.631, 95% CI=1.351–1.970, p=.000), and lower SES (IRR=0.870, 95% CI=0.780–0.969, p=.012). A higher number of ‘Social Isolation Events’ was predicted by female gender (IRR=1.125, 95% CI=1.021–1.240, p=.018) and higher SES (IRR=1.103, 95% CI=1.042–1.166, p=.001). A higher number of ‘COVID-19 Infection Events’ was predicted by higher community COVID-19 transmission risk (IRR=1.243, 95% CI=1.081–1.430, p=.002) and lower wealth (IRR=0.839, 95% CI=0.721–0.976, p=.023). Finally, a higher number of ‘Healthcare Barrier Events’ was predicted by female gender (IRR=1.921, 95% CI=1.315–2.808, p=.001) and lower wealth (IRR=0.787, 95% CI=0.656–0.945, p=.010). Figure 1 depicts adjusted associations between gender and levels of wealth in relation to counts of events in the five stressful life events domains.
Table 4.
Negative binomial regression, predicting counts of COVID-19 stressful life events domains by the indicated sociodemographic factors, adjusted for covariates.
| IRR | 95% CI | sig | IRR | 95% CI | sig | |
|---|---|---|---|---|---|---|
| Outcomes: COVID-19 related stressful life events | ||||||
|
| ||||||
| 1. Work/financial events | ||||||
|
| ||||||
| Covariates: | ||||||
| Household size | 1.030 | 0.965, 1.099 | .380 | 1.065 | 0.999, 1.135 | .054 |
| Community COVID-19 risk | 1.029 | 0.943, 1.122 | .526 | 1.019 | 0.937, 1.109 | .658 |
| Sociodemographic predictors: | ||||||
| Female gender=1 (vs. male=0) | 1.312 | 1.101, 1.562 | .002 | 1.293 | 1.091, 1.531 | .003 |
| Minority status=1 (vs. white, non-Hispanic=0) | 1.176 | 0.960, 1.442 | .118 | 1.187 | 0.976, 1.443 | .086 |
| SES composite (education/income) | 0.869 | 0.789, 0.958 | .005 | 0.931 | 0.845, 1.027 | .153 |
| Wealth | - | - | - | 0.833 | 0.767, 0.905 | .000 |
|
| ||||||
| 2. Home disruption events | ||||||
|
| ||||||
| Covariates: | ||||||
| Household size | 1.157 | 1.079, 1.240 | .000 | 1.174 | 1.092, 1.261 | .000 |
| Community COVID-19 risk | 1.108 | 1.011, 1.216 | .029 | 1.103 | 1.006, 1.210 | .037 |
| Sociodemographic predictors: | ||||||
| Female gender=1 (vs. male=0) | 1.639 | 1.356, 1.980 | .000 | 1.631 | 1.351, 1.970 | .000 |
| Minority status=1 (vs. white, non-Hispanic=0) | 1.015 | 0.813, 1.267 | .893 | 1.016 | 0.815, 1.268 | .886 |
| SES composite (education/income) | 0.845 | 0.761, 0.938 | .002 | 0.870 | 0.780, 0.969 | .012 |
| Wealth | - | - | - | 0.922 | 0.840, 1.011 | .085 |
|
| ||||||
| 3. Social isolation events | ||||||
|
| ||||||
| Covariates: | ||||||
| Household size | 1.015 | 0.976, 1.056 | .444 | 1.016 | 0.976, 1.058 | .436 |
| Community COVID-19 risk | 1.040 | 0.992, 1.091 | .104 | 1.040 | 0.992, 1.091 | .106 |
| Sociodemographic predictors: | ||||||
| Female gender=1 (vs. male=0) | 1.126 | 1.021, 1.241 | .017 | 1.125 | 1.021, 1.240 | .018 |
| Minority status=1 (vs. white, non-Hispanic=0) | 1.007 | 0.891, 1.138 | .909 | 1.007 | 0.891, 1.138 | .913 |
| SES composite (education/income) | 1.101 | 1.043, 1.163 | .000 | 1.103 | 1.042, 1.166 | .001 |
| Wealth | - | - | - | 0.996 | 0.947, 1.048 | .881 |
|
| ||||||
| 4. COVID-19 infection events | ||||||
|
| ||||||
| Covariates: | ||||||
| Household size | 0.996 | 0.883, 1.125 | .952 | 1.032 | 0.915, 1.165 | .607 |
| Community COVID-19 risk | 1.252 | 1.087, 1.442 | .002 | 1.243 | 1.081, 1.430 | .002 |
| Sociodemographic predictors: | ||||||
| Female gender=1 (vs. male=0) | 0.828 | 0.615, 1.113 | .211 | 0.816 | 0.608, 1.095 | .175 |
| Minority status=1 (vs. white, non-Hispanic=0) | 0.987 | 0.680, 1.434 | .946 | 0.972 | 0.672, 1.405 | .880 |
| SES composite (education/income) | 0.976 | 0.825, 1.155 | .781 | 1.038 | 0.874, 1.232 | .671 |
| Wealth | - | - | - | 0.839 | 0.721, 0.976 | .023 |
|
| ||||||
| 5. Healthcare barrier events | ||||||
|
| ||||||
| Covariates: | ||||||
| Household size | 1.031 | 0.896, 1.187 | .669 | 1.073 | 0.932, 1.236 | .328 |
| Community COVID-19 risk | 0.976 | 0.813, 1.173 | .798 | 0.960 | 0.799, 1.153 | .663 |
| Sociodemographic predictors: | ||||||
| Female gender=1 (vs. male=0) | 1.944 | 1.328, 2.846 | .001 | 1.921 | 1.315, 2.808 | .001 |
| Minority status=1 (vs. white, non-Hispanic=0) | 0.855 | 0.535, 1.367 | .513 | 0.864 | 0.544, 1.373 | .536 |
| SES composite (education/income) | 0.951 | 0.774, 1.168 | .632 | 1.029 | 0.834, 1.269 | .789 |
| Wealth | - | - | - | 0.787 | 0.656, 0.945 | .010 |
Figure 1.
Gender and levels of wealth depicted in relation to counts of events in the five COVID-19 related stressful life events domains with adjustment for the other sociodemographic factors and covariates.
In sum, this pattern of results shows female gender was a consistent, independent predictor of a higher number of stressful life events in four of the five domains. That is, being female (vs. male) was associated with a 31%, 64%, 13%, and 94% increase in the number of stressful life events in the ‘Work/Financial Events’, ‘Home Disruption Events’, ‘Social Isolation Events’, and ‘Healthcare Barrier Events’ domains, respectively. In addition, higher SES and higher wealth predicted a lower number of stressful life events in the ‘Home Disruption Events’ and ‘Work/Financial Events’ domains, respectively. Specifically, each one standard deviation increase in SES was associated with a 13% reduction in the number of stressful life events in the ‘Home Disruption Events’ domain and each one standard deviation increase in wealth was associated with a 17% reduction in the number of stressful life events in the ‘Work/Financial Events’ domain. In addition, higher wealth, but not SES, was uniquely related to a lower number of ‘COVID-19 Infection Events’ and ‘Healthcare Barrier Events’. Specifically, each one standard deviation increase in wealth was associated with a 16% reduction in the number of stressful life events in the ‘COVID-19 Infection Events’ domain and a 21% reduction in the number of stressful life events in the ‘Healthcare Barrier Events’ domain. Unexpectedly, higher SES was related to a higher number of ‘Social Isolation Events’; each one standard deviation increase in SES was associated with a 24% increase in the ‘Social Isolation Events’ domain.
In exploratory analyses, interactions by gender were all non-significant (ps>.05). Interactions by minority status showed minority status moderated associations between SES and ‘Work/Financial Events’ (p=.037) as well as associations between SES and ‘Social Isolation Events’ (p=.040). That is, lower SES predicted a higher number of ‘Work/Financial Events’ in the race/ethnic minority participants (p=.001), while there was no association between SES and ‘Work/Financial Events’ in the white, non-Hispanic participants (p=.355). In addition, higher SES predicted a higher number of ‘Social Isolation Events’ in the white, non-Hispanic participants (p=.000), while there was no association between SES and ‘Social Isolation Events’ in the race/ethnic minority participants (p=.757). Finally, analyses of wealth as a moderator of SES effects were all non-significant (ps>.05).
Discussion
Impacts of the COVID-19 pandemic in the United States have exacerbated pre-existing inequities in multiple life domains, especially among women and individuals of racial/ethnic minority and socioeconomically disadvantaged backgrounds (e.g., (Clouston et al., 2021; Connor et al., 2020; Krouse, 2020)). Associations between the social conditions of individuals and disparities in health outcomes are well-documented in the SDH literature (e.g., Braveman & Gottlieb, 2014; Marmot & Allen, 2014; Phelan et al., 2010); however, more work is needed to extend these models to consider COVID-19 specific outcomes. Building on these literatures, the goals of the current study were to examine COVID-19 related stressful life events in specific life domains (i.e., work/finances, home life, social activity, health, and healthcare) and to identify the sociodemographic characteristics of individuals who are at risk of experiencing these events.
In adjusted, multivariable analyses, women compared to men experienced a 31%, 64%, 13%, and 94% increase in the number of stressful life events in domains of work/finances, home life, social activity, and healthcare, respectively. These findings are consistent with prior studies showing women have fallen out of the U.S. workforce disproportionately and that women face unique demands (e.g., household management) and risks (e.g., domestic violence) in the home environment (Moreira da Silva, 2019; Peterman et al., 2020; Power, 2020; Sánchez et al., 2020). Beyond areas of work and home life, these findings also show that women experienced a greater number of stressful life events related to social isolation and difficulty accessing healthcare. Understanding social isolation in women is especially important as evidence suggests it is a risk factor for domestic violence (Morgan & Boxall, 2020). As well, understanding healthcare barriers in women, including access to mental health services, is necessary to ensure that women are receiving the care needed to mitigate impacts of the disproportionate burdens they face.
Also, in adjusted, multivariable analyses, SES and wealth significantly predicted the number of stressful life events experienced but with varying patterns of association across the life domains. With respect to SES, each one standard deviation increase in SES was associated with a 13% reduction in the number of stressful life events in the domain of home life. In addition, there were two significant interactions involving SES. One showed lower SES was related to a higher number of work/finance related events in the racial/ethnic minority group, but not in the white, non-Hispanic group; another showed higher SES was related to a higher number of social isolation events in the white, non-Hispanic group, but not in the racial/ethnic minority group. In sum, the association between SES and stressful life events in the domain of home life suggests that lower SES may potentiate stress experienced in the home environment. This is consistent with prior studies suggesting financial stress contributes to relationship problems and domestic violence (Morgan & Boxall, 2020). In addition, effects of SES on work/finance related events, observed only in the racial/ethnic minority group, may reflect that individuals in this group were more likely to experience job loss during the pandemic (Gemelas, Davison, Keltner, & Ing, 2021); and effects of SES on social isolation events, observed only in the white, non-Hispanic group, may reflect the unique experiences of more privileged individuals during the pandemic such as working from home or experiencing a reduction in travel.
With respect to wealth, each one standard deviation increase in wealth was associated with a 17%, 16%, and 21% reduction in the number of stressful life events in domains of work/finances, COVID-19 infection, and healthcare, respectively. Individuals with greater wealth, even independently of their income and education, were protected from experiencing stressful life events related to work/finances as well as COVID-19 infection and difficulties accessing healthcare during the pandemic. These findings suggest that SES, typically indexed by income level and educational attainment, may not be sufficient in characterizing socioeconomic disadvantage and that the inclusion of wealth, representing the accumulation of resources and greater financial stability, may contribute to a fuller picture of understanding risk associated with material disadvantage. Interestingly, the correlation between SES and wealth in the current sample was significant, albeit small in size (r = .21). The current findings are consistent with prior studies showing greater wealth has been associated with a variety of positive emotional and physical health outcomes (Boen et al., 2020; Carter, Blakely, & Collings, 2009; Robert & House, 1996), although few studies have examined both SES and wealth.
Strengths and Limitations
The current study has several notable strengths. Its focus is timely in characterizing the broader impacts of the COVID-19 pandemic in the United States and the individuals most vulnerable to these impacts. This is an important objective motivated by the need to develop strategies to remediate the many short- and long-term consequences of the COVID-19 pandemic, especially among individuals from disadvantaged backgrounds. In addition, the current study reflects a unique opportunity to integrate new measures into an existing, on-going study with the benefits of using pre-collected sociodemographic data to predict the examined COVID-19 impacts. The added measures included the assessment of COVID-19 related stressful life events as well as data derived from the coronavirus data repository (operated by Johns Hopkins University) used to index community-level COVID-19 transmission risk. This index was included as a covariate in all analyses to account for variability in COVID-19 infections across the geographically diverse sample. Finally, the current study was uniquely positioned to disentangle effects of SES from wealth by using the multiple markers of wealth available in the current study in analyses that examined these factors simultaneously.
Weaknesses of the current study were its relatively small size and the lack of racial/ethnic diversity in the sample. Most of the sample was white, non-Hispanic (79.7%), precluding opportunities to examine specific race/ethnic groups or intersections between the groups. For example, research examining individuals’ identification with multiple disadvantaged groups (e.g., female gender and African American) termed ‘intersectionality’ suggests there may be a combined effect of group membership that enhances risk (Crenshaw, 1991). This concept is especially relevant when considering impacts of the COVID-19 pandemic. In addition, the assessment tool used to measure the COVID-19 related stressful life events (EPII) was recently developed and lacked psychometric information about its reliability and validity. However, it was selected from the NIH Repository of COVID-19 Research Tools and, given the time-sensitive nature of this study, was deemed the most appropriate choice among available assessment tools on this topic. The assessment of wealth was also limited. Wealth was indexed by a composite of relevant indicators (e.g., home ownership). However, there were gaps in its measurement as a more comprehensive assessment of assets and debts was not conducted. Moreover, other relevant constructs that could have informed the study findings were not considered, such as measures of occupational status, social support, coping strategies, and resiliency.
Finally, a deeper criticism of the study’s conceptual and analytical approach concerns the relatively superficial examination of the main sociodemographic variables of interest and the lack of mediational testing that may have informed causal associations between the variables. In this context, findings from the current study are primarily descriptive, serving as a starting place for additional research. In one theoretical model of the fundamental causes of health disparities, for example, Link and Phelan (1995) highlight common mechanisms through which advantaged individuals avoid risks and engage in protective behaviors. This approach could be leveraged to study pathways between social conditions, behavioral strategies, and COVID-19 related impacts.
Implications and Future Directions
Findings from the current study show the toll of the COVID-19 pandemic on women in the United States has been pronounced and far-reaching, with women experiencing increases in stressful life events across broad areas of work/finances, home life, social activity, and access to healthcare. The identification of these specific areas of impact is a necessary step in developing intervention strategies to target their remediation. Building on this, additional work is needed to further delineate the significance of specific stressors, their inter-relation, and whether there are common underlying factors that drive the occurrence of stressful life events in multiple areas. Importantly, significant effects of female gender on the number of stressful life events were found to be independent of race/ethnicity, SES, and wealth, suggesting socioeconomic factors do not underpin gender effects and more needs to be learned about the unique experiences of women that put them at risk.
One area of future investigation regards the unique experiences of women in their roles in the care economy. More work is needed to better understand and quantify the unpaid work of women in relation to the capacity of women to respond to a crisis. That is, women whose capacity is already reduced due to the demands of unpaid and largely unrecognized care work may be poorly equipped to negotiate a crisis like the pandemic (Power, 2020), even across the socioeconomic spectrum. To date, U.S. governmental interventions have focused on affordable childcare, the provision of unemployment benefits for women voluntarily leaving the workforce due to care responsibilities, and adjustments to the child tax credit (Alon, Doepke, Olmstead-Rumsey, & Tertilt, 2020; Goldin & Michelmore, 2020). Building the capacity of women long-term, however, will require permanent, integrated solutions that address the multiple areas of impact in women’s lives beyond financial strains, including improved mental health services and social supports to offset these stressful impacts (Almeida, Shrestha, Stojanac, & Miller, 2020).
Findings from the current study also point to the unique and potentially protective role of wealth, with greater wealth related independently to a lower number of stressful life events across domains of work/finances, COVID-19 infection, and access to healthcare. Although prior studies show links between wealth and positive outcomes in areas of psychological well-being and physical health (Boen et al., 2020; Carter et al., 2009; Robert & House, 1996), more work is needed to characterize the role that wealth plays, apart from SES (as indexed by income and education), that may shield individuals from impacts in these areas. As a first step, future studies should consistently include the assessment of both SES and wealth indicators. Other areas of focus may include whether the protection that greater wealth affords is partly operating through psychological mechanisms such as reduced perceived stress or greater perceived family or social support, as the accumulation of wealth is often intergenerational. Additionally, this new knowledge may be leveraged to consider how wealth related benefits and wealth-building itself may be targeted as an intervention strategy.
Conclusions
In conclusion, findings from the current U.S. based study highlight the vulnerability of women, compared to men, who experienced a higher number of COVID-19 related stressful life events across multiple life domains as well as the potentially protective role of wealth in reducing stressful life events in these areas. Future research should focus on better understanding the unique experiences of women that put them at risk independently of socioeconomic factors, as well as the ways greater wealth affords protection possibly through psychological mechanisms that reduce perceived stressed or increase feelings of support. Delineating sociodemographic factors associated with risk will help inform intervention and policy-related strategies to remediate impacts of COVID-19 related stressful life events within and across life domains.
What is known about this topic?
Pre-existing inequities in resources and opportunities have exacerbated negative impacts of the COVID-19 pandemic, leaving the most vulnerable to face numerous hardships.
Specific COVID-19 related stressors are poorly understood as are the sociodemographic characteristics of individuals who are more vulnerable to experiencing such stress.
What this paper adds?
Women experienced a higher number of COVID-19 related stressful life events across areas of work/finances, home life, social activity, and access to healthcare.
Greater wealth was related to experiencing a lower number of stressful life events across areas of work/finances, COVID-19 infection, and access to healthcare.
Delineating sociodemographic factors associated with risk will inform intervention strategies to remediate impacts of COVID-19 related stressful life events.
Funding Sources:
This study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (U10HD025447, R01HD091132) and the National Heart, Lung, and Blood Institute (R01HL130103) at the National Institutes of Health.
Footnotes
Conflicts of Interest: Alexis S. Thomas, BA1; Madalyn Osbourne, BA1; Bradley M. Appelhans, PhD2; Glenn I. Roisman, PhD3; Cathryn Booth-LaForce, PhD1; and Maria E. Bleil, PhD1 declare that they have no conflicts of interest.
Data availability statement:
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- Almeida M, Shrestha AD, Stojanac D, & Miller LJ (2020). The impact of the COVID-19 pandemic on women’s mental health. Archives of Women’s Mental Health, 23(6), 741–748. doi: 10.1007/s00737-020-01092-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alon TM, Doepke M, Olmstead-Rumsey J, & Tertilt M. (2020). The impact of COVID-19 on gender equality (0898–2937). Retrieved from https://www.nber.org/system/files/working_papers/w26947/w26947.pdf
- Banerjee D, & Rai M. (2020). Social isolation in Covid-19: The impact of loneliness. International Journal of Social Psychiatry, 66(6), 525–527. doi: 10.1177/0020764020922269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boen C, Keister L, & Aronson B. (2020). Beyond net worth: Racial differences in wealth portfolios and black–white health inequality across the life course. Journal of Health and Social Behavior, 61(2), 153–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman P, & Gottlieb L. (2014). The social determinants of health: it’s time to consider the causes of the causes. Public health reports, 129(1_suppl2), 19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter KN, Blakely T, & Collings S. (2009). What is the association between wealth and mental health? Journal of Epidemiology & Community Health, 63, 221–226. [DOI] [PubMed] [Google Scholar]
- Clouston SAP, Natale G, & Link BG (2021). Socioeconomic inequalities in the spread of coronavirus-19 in the United States: A examination of the emergence of social inequalities. Social Science & Medicine, 268, 113554. doi: 10.1016/j.socscimed.2020.113554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor J, Madhavan S, Mokashi M, Amanuel H, Johnson NR, Pace LE, & Bartz D. (2020). Health risks and outcomes that disproportionately affect women during the Covid-19 pandemic: A review. Soc Sci Med, 266, 113364. doi: 10.1016/j.socscimed.2020.113364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crenshaw K. (1991). Mapping the Margins: Intersectionality, Identity Politics, and Violence against Women of Color. Stanford Law Review, 43(6), 1241–1299. doi: 10.2307/1229039 [DOI] [Google Scholar]
- Drentea P, & Reynolds JR (2015). Where Does Debt Fit in the Stress Process Model? Society and Mental Health, 5(1), 16–32. doi: 10.1177/2156869314554486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gemelas J, Davison J, Keltner C, & Ing S. (2021). Inequities in Employment by Race, Ethnicity, and Sector During COVID-19. J Racial Ethn Health Disparities. doi: 10.1007/s40615-021-00963-3 [DOI] [PMC free article] [PubMed]
- Ghilarducci T. (2021). Economists Weigh In On Covid-19 And Inequality. Retrieved from https://www.forbes.com/sites/teresaghilarducci/2021/03/04/economists-weigh-in-on-covid-19-and-inequality/?sh=3f66fc1241e0
- Goldin J, & Michelmore K. (2020). Who Benefits From the Child Tax Credit? National Bureau of Economic Research Working Paper Series, No. 27940. doi: 10.3386/w27940 [DOI]
- Grasso DJ, Briggs-Gowan MJ, Ford JD, & Carter AS (2020). The Epidemic – Pandemic Impacts Inventory (EPII). [DOI] [PMC free article] [PubMed]
- Holmes Finch W, & Hernández Finch ME (2020). Poverty and Covid-19: Rates of Incidence and Deaths in the United States During the First 10 Weeks of the Pandemic. Frontiers in Sociology, 5(47). doi: 10.3389/fsoc.2020.00047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, . . . Washington State -nCo, V. C. I. T. (2020). First Case of 2019 Novel Coronavirus in the United States. The New England journal of medicine, 382(10), 929–936. doi: 10.1056/NEJMoa2001191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirzinger A, Kearney A, Hamel L, & Brodie M. (2020). KFF Health Tracking Poll - Early April 2020: The Impact Of Coronavirus On Life In America. Retrieved from https://www.kff.org/coronavirus-covid-19/report/kff-health-tracking-poll-early-april-2020/
- Krouse HJ (2020). COVID-19 and the Widening Gap in Health Inequity. Otolaryngol Head Neck Surg, 163(1), 65–66. doi: 10.1177/0194599820926463 [DOI] [PubMed] [Google Scholar]
- Lean In, & SurveyMonkey. (2020). The coronavirus is a financial crisis for women. Retrieved from https://leanin.org/article/the-coronavirus-is-a-financial-crisis-for-women
- Liao TF, & De Maio F. (2021). Association of Social and Economic Inequality With Coronavirus Disease 2019 Incidence and Mortality Across US Counties. JAMA Network Open, 4(1), e2034578-e2034578. doi: 10.1001/jamanetworkopen.2020.34578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, & Phelan J. (1995). Social Conditions As Fundamental Causes of Disease. Journal of Health and Social Behavior, 80–94. doi: 10.2307/2626958 [DOI] [PubMed]
- Little RJA (1988). A Test of Missing Completely at Random for Multivariate Data with Missing Values. Journal of the American Statistical Association, 83(404), 1198–1202. doi: 10.1080/01621459.1988.10478722 [DOI] [Google Scholar]
- Marmot M, & Allen JJ (2014). Social Determinants of Health Equity. American Journal of Public Health, 104(S4), S517–S519. doi: 10.2105/ajph.2014.302200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattioli AV, Sciomer S, Cocchi C, Maffei S, & Gallina S. (2020). Quarantine during COVID-19 outbreak: Changes in diet and physical activity increase the risk of cardiovascular disease. Nutr Metab Cardiovasc Dis, 30(9), 1409–1417. doi: 10.1016/j.numecd.2020.05.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreira da Silva J. (2019). Why you should care about unpaid care work. Retrieved from https://oecd-development-matters.org/2019/03/18/why-you-should-care-about-unpaid-care-work/
- Morgan A, & Boxall H. (2020). Social isolation, time spent at home, financial stress and domestic violence during the COVID-19 pandemic. Trends & Issues in Crime & Criminal Justice(609). [Google Scholar]
- NICHD Early Child Care Research Network. (2005). Child care and child development: Results from the NICHD study of early child care and youth development. New York, NY, US: The Guilford Press. [Google Scholar]
- Parker K, Minkin R, & Bennett J. (2020). Economic Fallout From COVID-19 Continues To Hit Lower-Income Americans the Hardest. Retrieved from https://www.pewresearch.org/social-trends/2020/09/24/economic-fallout-from-covid-19-continues-to-hit-lower-income-americans-the-hardest/
- Patrick SW, Henkhaus LE, Zickafoose JS, Lovell K, Halvorson A, Loch S, . . . Davis MM. (2020). Well-being of Parents and Children During the COVID-19 Pandemic: A National Survey. Pediatrics, 146(4), e2020016824. doi: 10.1542/peds.2020-016824 [DOI] [PubMed] [Google Scholar]
- Peterman A, Potts A, O’Donnell M, Thompson K, Shah N, & Oertelt-Prigione S. (2020). Pandemics and violence against women and children. Center for Global Development Working Paper 528. Retrieved from Washington, DC: www.cgdev.org/sites/default/files/pandemics-and-vawg-april2.pdf [Google Scholar]
- Phelan JC, Link BG, & Tehranifar P. (2010). Social Conditions as Fundamental Causes of Health Inequalities: Theory, Evidence, and Policy Implications. Journal of Health and Social Behavior, 51(1_suppl), S28–S40. doi: 10.1177/0022146510383498 [DOI] [PubMed] [Google Scholar]
- Power K. (2020). The COVID-19 pandemic has increased the care burden of women and families. Sustainability: Science, Practice and Policy, 16(1), 67–73. [Google Scholar]
- Robert S, & House JS (1996). SES differentials in health by age and alternative indicators of SES. Journal of aging and health, 8(3), 359–388. [DOI] [PubMed] [Google Scholar]
- Rothwell J, & Saad L. (2021). How Have U.S. Working Women Fared During the Pandemic?. Retrieved from https://news.gallup.com/poll/330533/working-women-fared-during-pandemic.aspx
- Rudenstine S, McNeal K, Schulder T, Ettman CK, Hernandez M, Gvozdieva K, & Galea S. (2021). Depression and anxiety during the covid‐19 pandemic in an urban, low‐income public university sample. Journal of Traumatic Stress, 34(1), 12–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sánchez OR, Vale DB, Rodrigues L, & Surita FG (2020). Violence against women during the COVID‐19 pandemic: An integrative review. International Journal of Gynecology & Obstetrics, 151, 180–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin P, Morris R, Velasquez M, Rosenbaum S, & Somodevilla A. (2020). Keeping community health centers strong during the coronavirus pandemic is essential to public health. Health Affairs Blog.
- US Bureau of Labor Statistics. Labor Force Statistics from the Current Population Survey. (2021, April 2). Retrieved from https://www.bls.gov/web/empsit/cpseea03.htm#cps_eande_m03.f.1
- Woolhandler S, & Himmelstein DU (2020). Intersecting U.S. Epidemics: COVID-19 and Lack of Health Insurance. Ann Intern Med, 173(1), 63–64. doi: 10.7326/m20-1491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaw K, Bhattacharya J, Price A, Hamilton D, & Darity W Jr (2017). Women, race and wealth. Research Brief Series, 1. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.