Abstract
Objective
To investigate the views of health care professionals in a head and neck surgical department toward the implementation of advance care planning prior to surgery for older patients with head and neck cancer.
Method
Q methodology was used to explore and analyze participants’ views by combining quantitative and qualitative methods. Participants were asked to rank 35 Q statements generated via semi-structured interviews and a literature review and to explain the reasons for their ranking in subsequent interviews. The data was then analyzed and used to develop a factor series to illustrate participants’ views.
Results
This study surveyed 15 health care professionals, including eight doctors and seven nurses. The views of health care professionals toward preoperative implementation of advance care planning discussions were varied and could be categorized into three types: defending the autonomy of patients, patients’ knowledge and the Chinese traditional cultural context hinder the implementation of preoperative advance care planning, and lack of confidence in performing preoperative advance care planning.
Conclusions
Although the health care professionals in the head and neck surgical department in this study recognized the benefits of preoperative discussions regarding advance care planning, patients’ knowledge level, traditional Chinese values, inadequate capacity among health care professionals, and unsound legal policies have caused these professionals to have misgivings about preoperative counseling and discussing advance care planning with patients. Further studies should be conducted, and strategies to overcome barriers to discussions of preoperative advance care planning should be developed.
Keywords: Advance care planning, Aged, General surgery, Head and neck neoplasms, Hospice care
What is known?
-
•
The course of disease progression and treatment in head and neck cancer has a great impact on the patient’s ability to communicate, and there is limited research on advance care planning in the surgical field of head and neck cancer.
-
•
Advance care planning is a multi-party process involving the patient, family, and health care professionals in which health care professionals usually have an encouraging and guiding role. The views of these health care professionals are important for the implementation of preoperative advance care planning.
-
•
Q methodology helps to reveal underlying or hidden views, thereby uncovering a diversity of views.
What is new?
-
•
The views of health care professionals who perform preoperative advance care planning for older patients with head and neck cancer are discussed, laying the groundwork for future preoperative discussions of advance care planning in this population.
-
•
Health care professionals in the head and neck surgical department had commonalities with health care professionals in other specialties regarding the implementation of advance care planning, as well as unique characteristics related to their specialty.
1. Introduction
Head and neck cancer (HNC) is the seventh most common cancer in the world and mainly includes malignant oral, maxillofacial, pharyngeal, nasal, and neck tumors. HNC is characterized by a complex anatomical structure, deep lesion location, and high malignancy, and its incidence is slowly increasing worldwide [1,2]. HNC is prevalent in the middle-aged and older populations, with most cases diagnosed in people over the age of 50 years, and the risk of HNC increases with age [3]. Early or locally advanced stage HNC is primarily treated with surgery, which has a great impact on the patient’s respiratory, swallowing, and speech functions [4,5]. Additionally, older patients who undergo high-risk surgery face more serious comorbidities postoperatively, such as infections and bleeding from tumors because of advanced age, debility, and comorbidities with multiple chronic diseases [6]. When patients face a life-threatening situation after surgery or if their disease progresses toward a terminal state, their true wishes regarding treatment options are often easily ignored, forcing them to receive treatments and care that are inconsistent with their preferences, creating conflict in decision-making as well as emotional and financial burdens for patients’ families [7,8].
Advance care planning (ACP) is the process via which people who are in a good state of consciousness and who retain their decision-making capacity can discuss their preferred care plan if they enter an advanced or terminal stage of a serious illness with family members and health care professionals (HCPs) [9]. It has been suggested that patients with life-limiting illnesses should begin ACP as soon as the disease is diagnosed, especially because surgery usually occurs early in the diagnosis of the disease; this is a point in time that may lead to uncertain patient outcomes [10]. Preoperative counseling is an opportunity for patients and HCPs to discuss treatment goals and wishes, and patients can utilize this time for ACP discussions to clarify their treatment goals and values [11]. In this way, surgery can be an opportunity to initiate ACP discussions. There is a large body of literature validating the value and usefulness of ACP, but there is insufficient research on the effectiveness and application of ACP in the surgical field [12]. The implementation of ACP has been explored in cardiac surgery [13] and oncologic surgery [14], as well as in older patients scheduled for elective surgery [15], gastrointestinal surgery [16], and other populations. It has been confirmed that ACP achieves better results in terms of improving decision-making conflicts, increasing the rates of ACP discussions and of signing ACP-related documents, facilitating communication between patients and their families, and improving the level of patients’ knowledge regarding ACP. The authors have not found the literature on the implementation of ACP in patients undergoing surgery for HNC. However, Forner et al. [17] investigated the rate of preoperative ACP document signing in patients undergoing oral cancer surgery and found that the rate of preoperatively signing ACP documentation in this population was only 10.3%. On the one hand, this suggests the feasibility of applying ACP in patients undergoing HNC surgery; on the other hand, this also suggests that the views of stakeholders toward the implementation of ACP in patients undergoing HNC surgery need to be further investigated.
ACP is a multi-party process involving patients, families, and HCPs, and the wishes of each stakeholder are important. HCPs usually have an encouraging and guiding role in the ACP implementation process [18]. The level of knowledge and the attitudes of HCPs toward ACP affect the implementation of ACP in practical situations, and it is important for HCPs to be adequately prepared for the implementation of ACP [19]. Previous study has shown that when talking about ACP, most HCPs believe it is beneficial, yet surgical HCPs do not always have this view [20]. One study showed that the risks of any surgery cannot be accurately predicted, and it is recommended that ACP be routinely discussed prior to surgery [10]. However, some HCPs perceive a conflict between the curative purpose of surgery and the therapeutic limitations of ACP, and some HCPs refuse to operate on patients who have restrictive therapeutic measures [20]. There are no studies on the views of surgical HCPs specializing in HNC regarding the implementation of preoperative ACP in older patients with HNC, It is important to understand the views of HNC surgical HCPs regarding the implementation of preoperative ACP in older patients with HNC.
Q methodology is a psychological research method that combines quantitative and qualitative approaches to reveal subjective views such as attitudes, beliefs, and perceptions about a phenomenon via the categorizing and ranking of statements related to the research topic by study participants [21]. Within this approach, qualitative research is aimed at exploring the views of study participants, and quantitative research is aimed at analyzing the structure of participants’ views using statistical methods. Q methodology emphasizes “operational subjectivity,” where all operational categories are derived from participants’ own direct representations of their perceptions and are categorized and ordered autonomously by participants in relation to these representations, rather than relying exclusively on the researcher’s interpretive abilities [22]. As a result, Q methodology is less influenced by the researcher’s interviewing experience than traditional qualitative research methods. Additionally, quantitative methods such as factor analysis are used in data processing to support the interpreted views so that the results are verifiable, avoiding omissions of views and errors in interpretation [23]. Moreover, Q methodology requires participants to respond to each operational category by explicitly expressing their views about certain negative or unexpected views so as to overcome participant response bias in qualitative research to some extent [24]. With questionnaires or Likert rating scales, researchers must construct variables and select variables when developing the scale, stipulate the different meanings represented by different responses before the participants respond to a question, and use the general rules of the overall response to infer individual responses, often ignoring the specific responses of participants [25,26]. In contrast, Q methodology focuses on the expression of the true will of participants, is less restricted by scale entries, and emphasizes individuality, making this approach more likely to reveal potential or hidden views and yield a diversity of viewpoints [25,26]. Therefore, Q methodology was used in this study to gain a comprehensive understanding of the different views of HNC surgical HCPs regarding the implementation of preoperative ACP in older patients with HNC, to provide a basis for the future implementation of ACP in older surgical patients with HNC.
2. Materials and methods
2.1. Inclusion and exclusion criteria
We recruited participants from April to July 2023 in the Head and Neck Surgery Department of Shanxi Provincial Cancer Hospital, which has a total of 83 HCPs, including 36 doctors and 47 nurses. Participants were eligible to participate in this study if they were willing to take part, were fluent in Chinese, had been practicing in the head and neck surgical department for two years or more, and had a bachelor’s degree or higher. Those undergoing a clinical internship or advanced training in the head and neck surgical department were not included in this study. In the first phase of the study, a qualitative method was used to determine Q statements. HCPs in the head and neck surgical department of different sexes and who have different educational backgrounds, work experience, and functions and who may therefore hold different views were selected according to the principle of maximum differentiation. The sample size was based on the information saturation criterion of no additional new emerging information. This phase resulted in interviews with 16 HCPs who met the inclusion and exclusion criteria and were broadly representative of the HCPs in the department. The second phase applied the quantitative study using the Q methodology to collect research data. The sample size was one-third to one-half the number of Q statements, and its upper limit was the number of Q statements [26]; 17 samples were included in this stage, with 15 valid samples.
2.2. Development of the Q-set
Q-set is a collection of Q statements. Q statements expressing participants’ views were generated via semi-structured interviews and a literature review; the form of Q statements was text. First, the first author conducted semi-structured interviews with 16 HCPs in the head and neck surgical department who met the above inclusion and exclusion criteria. Participants ranged in age from 26 to 47 years and included a total of seven surgeons and nine nurses, 10 of whom were female and six were male. After obtaining their informed consent, participants were invited to review their previous experiences with preoperative counseling and ACP discussions with older patients who had HNC and to express their views regarding the implementation of preoperative ACP in this population. The interviews consisted of a total of seven open-ended questions (Appendix A), and each interview lasted for no less than 10 min. The first author transcribed the recorded information into text within 24 h of each interview, continuously interviewing and transcribing until the information reached saturation. The information from interview texts was then distilled and summarized by two researchers into succinct statements to convey the themes of the study.
Referring to Shim et al.’s research [27], statements related to the research topic were refined and added through a literature review. The keywords used for the search were advance care planning, advance directive, living will, surgery, preoperative, perioperative, health care professionals, surgeons, and nurses. The databases searched included PubMed, Web of Science, CINAHL, Embase, China National Knowledge Infrastructure (CNKI), Chinese BioMedical Literature Service System (SinoMed), and Wanfang Data. Qualitative studies reflecting views regarding the research topics were included. Studies published in Chinese or English language were eligible for inclusion because the research team is proficient in both languages. Most papers published in widely used international databases are written in English, so by considering English papers, publications that met the standards to the maximum extent could be included. Databases, including Chinese publications, were searched to obtain evidence with a background of China. The retrieval period was from 1993 to 2023 because studies on ACP were first published in 1993 [28]. Studies from 1993 to May 2023 were included. The search and screening resulted in the identification of four articles (See the screening process in Appendix B). Two researchers independently read the articles and extracted statements regarding HCPs’ views on performing ACP before surgery; the collected statements were then summarized. By the above methods, 47 Q statements were developed. After a review by the research team, 35 statements were adopted as the Q-set.
2.3. Piloting
Five participants were recruited for a pilot study (including two surgeons and three nurses) to test the comprehensibility and applicability of the Q statements. According to the opinions of participants, two participants objected to the original statement “Will not take the initiative to discuss ACP with patients,” stating that “The statement is extreme and can lead to ambiguity. Considering many factors, some HCPs may be unwilling to discuss ACP with patients but are willing to actively participate in the discussion when requested or initiated by patients; it is suggested that additional derivations be added to avoid ambiguity”. The Q statements were revised in response to this comment to make them easier to understand. The remaining Q statements were considered to be clearly stated and free of omissions overall and were therefore not revised in any way. Finally, each Q statement was numbered, and they were then rearranged out of order for later use.
2.4. Participants selection
Participants were invited to rank the Q statements in the Q-set. Selection of the participants followed the inclusion and exclusion criteria mentioned above, without randomization, and was based on the principle of maximum differentiation. The small-sample population was explored in-depth according to the research topic. A self-administered questionnaire was used to collect participants’ general information, including age, sex, education level, professional title, and years of work experience.
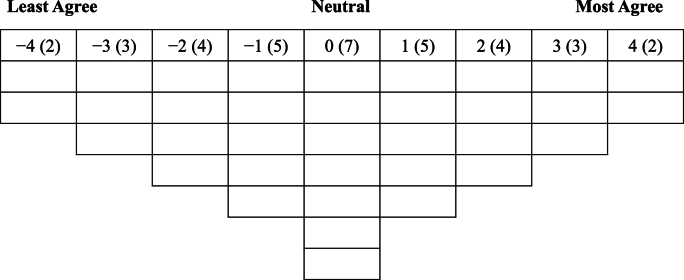
2.5. Q-sorting
A quasi-normally distributed table was developed for the collection of study data, which comprised nine piles and 35 cells (see Fig. 1). After explaining the purpose of the study to participants, they were instructed to read the Q statements and be sure that these were fully understood. The Q statements were broadly categorized as Agree, Unsure, and Disagree, and then further categorized according to the level of agreement until all Q statements were ranked in the table. The most agreed-upon entry counted as 4 points, and the least agreed-upon entry counted as −4 points. Upon completion of the Q-sorting, participants were asked to explain their reasons for the Q-sorting order, especially for the “most agreed” and “least agreed” Q statements. The researcher conducted in-depth interviews and recorded the reasons for the Q-sorting, after obtaining participants’ consent.
Fig. 1.
Q-sorting diagram. Note: Taking “−4 (2)” as an example, “2” indicates that there are two Q statements with a score of “−4”.
2.6. Q analysis
The data were analyzed using the Ken-Q Analysis 0.11.1 web version [29], which mainly includes three parts, as below. (i) Factor analysis: Principal component analysis was used to extract factors, and those with an eigenvalue >1 and cumulative variance contribution rate ≥50% were retained. These factors were rotated with maximum variance orthogonal rotation to explain the meaning of the factors. (ii) Calculation of factor loadings: according to the formula for calculating factor loadings in Q methodology, the factor loadings selected were ≥Number of factors/ (N is the number of Q statements) [30]. Ultimately, three factors were produced in this study, and the factor loadings were ≥0.51. The larger the absolute value of the factor loadings, the more statistically significant they were. Each factor reflected the views of at least two study participants. If participants were categorized into two or more factor categories at the same time, they were removed in subsequent data analysis. (iii) Calculation of factor scores: the standardized scores of each factor sort were calculated to derive the scores of each entry. The overall view of each factor was described based on the different factor scores of each entry on the factor, especially the extreme scores (±4 and ±3) and the distinguishing statements.
2.7. Ethical considerations
This study was conducted in accordance with the Declaration of Helsinki after being approved by the Research Ethics Committee of Shanxi Medical University and obtaining respondents’ written informed consent. The standard guidelines described by Zhou and Wang [21] and Watts [31] were followed because the reporting guidelines for the main research types do not include specific guidelines for studies involving Q methodology.
3. Results
After the factor analysis for 17 samples, there were five factors with an eigenvalue >1. Considering the extent of the decline in the cumulative explanatory rate, three factors were selected with a cumulative variance contribution rate of 58%; two samples were not reflected in any of the factors, so these were deleted. The final valid sample was 15 samples. Scores for the 35 Q statements across all three factors are displayed in Table 1, and the sociodemographic characteristics of participants across the three factors are displayed in Table 2. The distinguishing statements across the three factors are shown in Table 3.
Table 1.
Q statements and factor scores across the three factors.
| No. | Q statement | Factor scores |
||
|---|---|---|---|---|
| Factor 1 | Factor 2 | Factor 3 | ||
| S1 | Never heard of ACP | −1 | 0 | −3∗∗ |
| S2 | Routinely provides preoperative education before surgery, but barely mentions ACP-related content. | 0 | 1 | 1 |
| S3 | Will not take the initiative to discuss ACP with patients, but is willing to cooperate if patients request it. | 1 | 0 | 2 |
| S4 | It is difficult to discuss ACP with patients because they do not know about their condition, and it may cause dissatisfaction among family members. | −1∗∗ | 4∗∗ | 2∗∗ |
| S5 | Most patients’ decisions about treatment are made by family members at present. | 1 | −1∗∗ | 2 |
| S6 | Discussing ACP preoperatively may increase patients’ anxiety about the surgery. | −1∗∗ | 3 | 2 |
| S7 | ACP may be considered unfavorable by patients and their families, and discussing it with them before surgery may be rejected. | −1∗∗ | 3 | 1 |
| S8 | Surgery offers hope for a cure, and discussing ACP before surgery is like a death sentence for patients, which may lead to a loss of confidence in the treatment. | −4∗∗ | 0 | 0 |
| S9 | Discussing ACP before surgery may influence patients’ decision to undergo surgery. | −1 | 1∗∗ | −2 |
| S10 | Discussing ACP with patients before surgery is energy-consuming and may lead to emotional and work-related burdens on health care professionals. | −3 | 0∗∗ | −3 |
| S11 | Preoperative discussion of ACP is beneficial in facilitating communication between patients and their families, which can reduce the burden of decision-making on families and alleviate decision-making conflicts among family members. | 2∗∗ | 0∗∗ | −2∗∗ |
| S12 | Implementation of ACP in advance can alleviate anxiety among family members during emergencies. | 0∗∗ | 2∗∗ | −4∗∗ |
| S13 | Preoperative discussion of ACP improves patients’ prognostic awareness and increases their understanding of the disease and surgery. | 3 | 2 | −2∗∗ |
| S14 | Implementation of ACP in advance can ease the financial burden on families. | 1∗∗ | −1 | −1 |
| S15 | Patients have the power to choose the treatment they want to receive, and discussing ACP before surgery helps patients receive therapy and care in line with their goals and helps to safeguard their autonomy. | 4∗∗ | 1 | 0 |
| S16 | Having ACP discussions in advance ensures quality of life and dignity for patients at the end of life. | 3∗∗ | −1 | 0 |
| S17 | Health care professionals and families should respect patients’ wishes and choices about the end of life. | 4 | 3 | 3 |
| S18 | Implementation of ACP in advance can facilitate patient-centered medical care. | 2∗∗ | 0 | −1 |
| S19 | The higher the surgical risk, the greater the need to discuss ACP. | 1∗ | 4 | 3 |
| S20 | Surgery is a point in time with uncertain risk, an opportunity for patients to ponder death, and can serve as a trigger for discussion of ACP. | 1 | 2 | −4∗∗ |
| S21 | Even elective surgery in young people can have a poor outcome. | 0 | 2∗ | 0 |
| S22 | Discussing ACP before surgery is not necessary, and patients may be advised not to have surgery if the risk of surgery is very high. | −3∗∗ | −2 | −1 |
| S23 | The decision to have a preoperative ACP discussion should depend on the surgeon’s judgment of the risks and adverse outcomes of surgery. | 0 | −1 | −1 |
| S24 | It is important to know patients’ wishes for end of life in advance. | 3∗∗ | 1 | 0 |
| S25 | The choice of whether to implement preoperative ACP can be made in consultation with the family and based on patients’ psychological profile. | 2∗∗ | 0∗∗ | −2∗∗ |
| S26 | The timing of an ACP discussion should be decided by patients and families. | −2 | −3 | 4∗∗ |
| S27 | Time is limited before surgery and there is insufficient time to discuss ACP with patients. | −3 | −3 | −3 |
| S28 | Surgeons are good at discussing surgical risks with patients and surgery is an ideal time to introduce ACP. | 0 | 1 | −1 |
| S29 | The goal of surgery is to cure and prolong life, which contradicts what ACP is about. | −4 | −4 | 0∗∗ |
| S30 | Head and neck cancers are relatively mild compared to other cancers, and it is unusual to talk to them about such serious topics. | −2 | −3 | 4∗∗ |
| S31 | Not having the confidence to discuss such topics successfully with patients. | −2 | −2 | 1∗∗ |
| S32 | If not communicated properly, ACP can lead to medical disputes. | 0 | −1 | 3∗∗ |
| S33 | ACP is best discussed when there is little time left to live; it is too early to discuss ACP before surgery. | −2∗∗ | −4∗∗ | 1∗∗ |
| S34 | Implementation of ACP in advance can reduce the waste of medical resources and ease financial pressure on the state. | 2∗∗ | −2∗ | 0∗ |
| S35 | The conditions for discussing ACP-related topics are lacking at this time. | 0 | −2 | 1∗ |
Note: ACP = advance care planning. ∗Distinguishing statement significant at P < 0.05; ∗∗ Distinguishing statement significant at P < 0.01. Bold indicates a consensus statement.
Table 2.
Sociodemographic characteristics of participants across the three factors.
| Variables | n | Factor 1 (n = 7) | Factor 2 (n = 6) | Factor 3 (n = 2) | |
|---|---|---|---|---|---|
| Age, years | 20–30 | 4 | 3 | 1 | 0 |
| 31–40 | 8 | 2 | 4 | 2 | |
| ≥41 | 3 | 2 | 1 | 0 | |
| Sex | Male | 7 | 3 | 4 | 0 |
| Female | 8 | 4 | 2 | 2 | |
| Occupation | Doctor | 8 | 3 | 5 | 0 |
| Nurse | 7 | 4 | 1 | 2 | |
| Professional title | Junior | 5 | 3 | 1 | 1 |
| Intermediate | 6 | 1 | 4 | 1 | |
| Senior | 4 | 3 | 1 | 0 | |
| Level of education | Bachelor | 6 | 3 | 1 | 2 |
| Master | 7 | 3 | 4 | 0 | |
| PhD | 2 | 1 | 1 | 0 | |
| Years of work experience | 2–10 | 8 | 3 | 4 | 1 |
| 11–20 | 6 | 3 | 2 | 1 | |
| ≥21 | 1 | 1 | 0 | 0 | |
Table 3.
Distinguishing statements across the three factors.
| No. | Factor scores |
||
|---|---|---|---|
| Factor 1 | Factor 2 | Factor 3 | |
| Factor 1 | |||
| S8 | −4∗∗ | 0 | 0 |
| S22 | −3∗∗ | −2 | −1 |
| S33 | −2∗∗ | −4∗∗ | 1∗∗ |
| S7 | −1∗∗ | 3 | 1 |
| S6 | −1∗∗ | 3 | 2 |
| S4 | −1∗∗ | 4∗∗ | 2∗∗ |
| S12 | 0∗∗ | 2∗∗ | −4∗∗ |
| S19 | 1∗ | 4 | 3 |
| S14 | 1∗∗ | −1 | −1 |
| S25 | 2∗∗ | 0∗∗ | −2∗∗ |
| S18 | 2∗∗ | 0 | −1 |
| S11 | 2∗∗ | 0∗∗ | −2∗∗ |
| S34 | 2∗∗ | −2∗ | 0∗ |
| S24 | 3∗∗ | 1 | 0 |
| S16 | 3∗∗ | −1 | 0 |
| S15 | 4∗∗ | 1 | 0 |
| Factor 2 | |||
| S33 | −2∗∗ | −4∗∗ | 1∗∗ |
| S34 | 2∗∗ | −2∗ | 0∗ |
| S5 | 1 | −1∗∗ | 2 |
| S10 | −3 | 0∗∗ | −3 |
| S25 | 2∗∗ | 0∗∗ | −2∗∗ |
| S11 | 2∗∗ | 0∗∗ | −2∗∗ |
| S9 | −1 | 1∗∗ | −2 |
| S21 | 0 | 2∗ | 0 |
| S12 | 0∗∗ | 2∗∗ | −4∗∗ |
| S4 | −1∗∗ | 4∗∗ | 2∗∗ |
| Factor 3 | |||
| S20 | 1 | 2 | −4∗∗ |
| S12 | 0∗∗ | 2∗∗ | −4∗∗ |
| S1 | −1 | 0 | −3∗∗ |
| S13 | 3 | 2 | −2∗∗ |
| S11 | 2∗∗ | 0∗∗ | −2∗∗ |
| S25 | 2∗∗ | 0∗∗ | −2∗∗ |
| S34 | 2∗∗ | −2∗ | 0∗ |
| S29 | −4 | −4 | 0∗∗ |
| S33 | −2∗∗ | −4∗∗ | 1∗∗ |
| S31 | −2 | −2 | 1∗∗ |
| S35 | 0 | −2 | 1∗ |
| S4 | −1∗∗ | 4∗∗ | 2∗∗ |
| S32 | 0 | −1 | 3∗∗ |
| S30 | −2 | −3 | 4∗∗ |
| S26 | −2 | −3 | 4∗∗ |
Note: ∗Distinguishing statement significant at P < 0.05; ∗∗Distinguish statement significant at P < 0.01.
3.1. Factor 1. Defending the autonomy of patients
Factor 1 reflected the views of seven participants and accounted for 36% of the total variance, with an eigenvalue of 6.15. The five Q statements that most closely aligned with the views of participants were: “Health care professionals and families should respect patients’ wishes and choices about end of life” (S17: 4, 1.610; where “4” indicates the factor score of Q statement No. 17, and “1.610” represents its standardized score), “Patients have the power to choose the treatment they want to receive, and discussing ACP before surgery helps patients receive therapy and care in line with their goals and helps to safeguard their autonomy” (S15: 4, 1.494), “Having ACP discussions in advance ensures quality of life and dignity for patients at the end of life” (S16: 3, 1.380), “It is important to know patients’ wishes for end of life in advance” (S24: 3, 1.371), and “Preoperative discussion of ACP improves patients’ prognostic awareness and increases their understanding of the disease and surgery” (S13: 3, 1.258). The five Q statements that were most inconsistent with participants’ views were: “The goal of surgery is to cure and prolong life, which contradicts what ACP is about” (S29: −4, −1.808), “Surgery offers hope for a cure, and discussing ACP before surgery is like a death sentence for patients, which may lead to a loss of confidence in the treatment” (S8: −4, −1.698), “Discussing ACP before surgery is not necessary, and patients may be advised not to have surgery if the risk of surgery is very high” (S22: −3, −1.569), “Time is limited before surgery and there is insufficient time to discuss ACP with patients” (S27: −3, −1.317), and “Discussing ACP with patients before surgery is energy-consuming and may lead to emotional and work-related burdens on health care professionals” (S10: −3, −1.292). The main concern of this group of participants was the preoperative discussion of the benefits of ACP for the patient. They felt that discussing ACP preoperatively would preserve the patient’s rights, as stated by Participant No. 8:
“There are many possibilities that may be faced during treatment. Time has to be found to discuss things that relate to a patient’s life, and it is important to get informed consent and cooperation for a patient's treatment and discussing ACP before surgery. Doing all these things can help patients prepare, and engaging them in their own decision-making also improves the quality of their life and reduces over-medication. I believe it is an initiative to promote patient-centered care, a patient’s right to self-determination, and effectively protect informed consent.” (Doctor, age 28 years)
3.2. Factor 2. Patient’s knowledge and the Chinese cultural context hinder preoperative implementation of ACP
Factor 2 reflected the views of six participants and accounted for 11% of the total variance, with an eigenvalue of 1.86. The five Q statements that most closely aligned with the views of participants were: “It is difficult to discuss ACP with patients because they do not know about their condition, and it may cause dissatisfaction among family members” (S4: 4, 2.033), “The higher the surgical risk, the greater the need to discuss ACP prior to surgery” (S19: 4, 1.733), “Health care professionals and families should respect patients’ wishes and choices about end of life” (S17: 3, 1.314), “Discussing ACP preoperatively may increase the patient’s anxiety about the surgery.” (S6: 3, 1.289), and “ACP may be considered unfavorable by patients and their families, and discussing it with them before surgery may be rejected” (S7: 3, 1.201). The five Q statements that were most inconsistent with participants’ views were as follows. “ACP is best discussed when there is little time left to live; it is too early to discuss ACP before surgery” (S33: −4, −2.082), “The goal of surgery is to cure and prolong life, which contradicts what ACP is about” (S29: −4, −1.658), “Time is limited before surgery and there is insufficient time to discuss ACP with patients” (S27: −3, −1.568), “Head and neck cancers are relatively mild compared to other cancers, and it is unusual to talk to them about such serious topics” (S30: −3, −1.245), and “The timing of an ACP discussion should be decided by patients and families” (S26: −3, −1.155). The main consideration for this group of participants was the negative influence of traditional Chinese thoughts and attitudes regarding people’s acceptance of preoperative discussions of ACP. It is hard for many people to understand these concepts in China, as expressed by Participant No. 3:
“Some patients do not know about their own condition. When admitted to the hospital, the family of these patients instructs us not to let the patient find out that they have cancer. For this type of patient, there is no way to discuss ACP. If you talk to patients directly, the family will be upset, and it is likely to cause conflicts between doctors and patients. And then some people feel that the topic is unlucky. People come to the hospital for treatment, but if health care professionals talk to them about death, they will think this is a curse. In particular, some older patients who are very ill are very mindful of hearing this.” (Doctor, age 33 years)
3.3. Factor 3. Lack of confidence in performing preoperative ACP
Factor 3 reflected the views of two participants and accounted for 11% of the total variance, with an eigenvalue of 1.81. The five Q statements that most closely aligned with the views of participants were: “The timing of an ACP discussion should be decided by patients and families” (S26: 4, 2.214), “Head and neck cancers are relatively mild compared to other cancers, and it is unusual to talk to them about such serious topics” (S30: 4, 1.503), “The higher the surgical risk, the greater the need to discuss ACP prior to surgery” (S19: 3, 1.264), “If not communicated properly, ACP can lead to medical disputes” (S32: 3, 1.186), “Health care professionals and families should respect patients’ wishes and choices about end of life” (S17: 3, 1.027). The five Q statements that were most inconsistent with participants’ views were: “Surgery is a point in time with uncertain risk, an opportunity for patients to ponder death, and can serve as a trigger for discussion of ACP” (S20: −4, −1.897), “Implementation of ACP in advance can alleviate anxiety among family members during emergencies”(12: −4, −1.66), “Time is limited before surgery and there is insufficient time to discuss ACP with patients” (S27: −3, −1.581), “Never heard of ACP” (S1: −3, −1.503), “Discussing ACP with patients before surgery is energy-consuming and may lead to emotional and work-related burdens on health care professionals” (S10: −3, −1.423). Participants had low confidence in successfully conducting preoperative ACP conversations, and they typically did not initiate such conversations with patients, as stated by Participant No. 9:
“It should be left up to the patient and their family to decide when to discuss ACP. If a healthcare provider initiates the conversation, the patient and their family may mistakenly assume that the treatment is hopeless, leading to increased anxiety and fear about the surgery, which can be detrimental to their care. In reality, it is impossible to determine the critical moment in terms of end-of-life care accurately. Some people have survived because they received resuscitation. If they choose to give up, it will be really hopeless.” (Nurse, age 35 years)
4. Discussion
In this study, Q methodology was used to explore the views of head and neck surgical HCPs toward preoperative ACP discussions with older patients who have HNC, which generated three main viewpoints.
Participants’ views categorized in factor 1 were mainly concerned with the benefits of preoperative discussion of ACP with patients. They advocated for patients’ right to informed consent and that treatment decision-making should be respected, and felt that preoperative discussion of ACP could help them to understand the patients’ wishes, which would be conducive to protecting patients’ rights and interests. Participants who held this view supported ACP discussions with patients before HNC surgery, which may be explained by the fact that of all cancer surgeries, HNC surgery has the greatest impact on the patient’s language function, and communication-related problems are more common in the postoperative period [32]. When patients experience serious adverse postoperative complications such as bleeding and infection, they may not be able to directly express their wishes for treatment, resulting in them being forced to undergo treatments that are inconsistent with their values [33]. Presurgical ACP discussions can be effective in helping patients to fully express their wishes and in promoting understanding of the patient’s treatment wishes among HCPs and family members. In addition to this, these participants thought that discussing ACP prior to surgery improves the patient’s quality of life, reduces the financial burden on family members, and mitigates decision-making conflicts between the patient and family members. Song et al.’s study of preoperative ACP interventions in patients undergoing cardiac surgery also confirmed these effects [13]. In contrast to this view, a study in 2018 showed that surgeons generally disapprove of ACP in the perioperative period because they believe it limits treatment [20]. However, ACP focuses on the final outcome and quality of life among patients in the terminal phase and is not a limitation to treatment. Surgery usually occurs during the early stages of the disease, and its severe morbidity and mortality are risks that patients must be aware of. Furthermore, discussions about end-of-life treatment choices can naturally arise during the informed consent process, such that consideration of surgical risks can be coupled with consideration of the patient’s end-of-life preferences [34]. These preferences may reflect the patient's expectations about the disease and the procedure and guide HCPs’ diagnostic and therapeutic activities rather than limiting treatment [35]. Therefore, HCPs should design ACP specifically for the surgical setting to clarify the patient’s goals for treatment in the perioperative period, thereby providing greater flexibility in treatment, enabling patient-centered care, and safeguarding patients’ autonomy [36].
Participants categorized within factor 2 believed that patients’ knowledge and the Chinese cultural context presented barriers to discussing ACP prior to surgery. Participants in this group perceived that discussing ACP with patients who have no knowledge of their condition is difficult and might cause patients to be suspicious of their condition, increase anxiety and fear about surgery, and even affect surgical decision-making. Family members have a strong voice in Asian cultures, and when faced with treatment decisions, HCPs prioritize the wishes of family members over those of the patient [37]. Especially against the background of Confucianism as the predominant culture in China, people prioritize filial piety, and when a patient is diagnosed with a serious illness, family members tend to conceal the condition from the patient to avoid creating a psychological burden and compromising treatment [38]. Death is a very sensitive topic, and when a patient's disease progresses to the point where treatment is hopeless, most family members tend to make life-prolonging treatment decisions on behalf of the patient and avoid discussing death directly with the patient, believing that talking about death with the patient will not be conducive to their recovery [39]. HCPs are strongly influenced by the mission to save lives, and most usually prioritize life-prolonging treatments in emergency situations [40]. Participants in this group were concerned that the conventional values of filial piety and the concept of death may hinder the implementation of preoperative discussions about ACP, and that discussing ACP with patients may cause conflicts between the health care system and the patient side, leading to medical disputes. It has been found that patients’ knowledge about ACP is key to its widespread implementation [41], and family-centered ACP has significant advantages in China [42]. Therefore, future research should focus on Chinese culture and the health care system, and HCPs should attach greater importance to communication between patients and their families, provide family-centered end-of-life education, emphasize the role of the family, actively disseminate knowledge related to the treatment and prognosis of diseases for patients and their families, and elucidate the effect of preoperative ACP on the family’s role in counteracting the perioperative risks of adverse effects of surgical patients and in promoting the long-lasting benefits of late-stage health care. Family members should also be encouraged to provide high-quality hospice care services for patients in the terminal phase as a way to maintain filial piety and gradually weaken the influence of traditional Chinese concepts regarding ACP.
Participants categorized within Factor 3 had low confidence in performing preoperative ACP at this time, which was consistent with Lee et al.’s findings [43]. Surgical risk and disease prognosis are influenced by multiple factors and are often difficult to predict accurately [44]; HCPs find it difficult to recognize the appropriate time to initiate an ACP discussion and therefore do not take the initiative to start a discussion about ACP preoperatively. Some HCPs believe that discussing ACP preoperatively is a form of abandoning treatment for the patient, and they are concerned that discussing ACP with the patient prematurely will deprive them of hope in the surgical treatment and may even negatively affect the doctor–patient relationship [45]. However, because patients and their families lack sufficient disease-related information, they often rely on HCPs when making decisions. Some patients are overly optimistic about surgery and believe that HCPs will convey information to them at the appropriate time, so they usually do not take the initiative to express their preference for treatment to HCPs; in these cases, the evasive attitudes of HCPs toward preoperative ACP can easily lead to patients and their families not knowing what to do in an emergency [11]. In addition, this study found that nurses generally did not feel that they should take on the responsibility of discussing ACP prior to surgery and that it was more appropriate for a physician to discuss such topics; this result is supported by another study [46]. Some participants also felt that HNC surgery was a lower-risk procedure and had a better prognosis than other cancer surgeries, eliminating the need for premature ACP discussions. The possible reasons for these results are that ACP is currently under-popularized in China, and some staff within the health care system have limited knowledge of ACP, and their communication skills must be urgently improved [47]. Chen et al. [48] conducted a survey on 1,036 nurses in 30 provinces in China, and the results showed that only 25.9% thought they understood the actual connotation of ACP, only 0.6% answered all the questions correctly in the ACP knowledge questionnaire, and the participation rate of nurses in ACP-related behaviors was less than 30%. These results further confirm the lack of knowledge and practice of ACP among Chinese HCPs. Therefore, it is crucial to carry out ACP education and skills training for HCPs as soon as possible to promote the practice of ACP. At the same time, HCPs with different specialties should be prompted to adopt different roles in preoperative ACP according to their own work nature and strengths [19]. In addition, limited legal and policy support has contributed to the lack of confidence in preoperative ACP discussions among HCPs. Currently, ACP in China remains in the academic realm, and although a pilot law on living wills was passed in Shenzhen in 2023, the law has not yet been implemented nationwide and does not mention protection of the right of HCPs to perform ACP. The above may have contributed to the legal concerns of HCPs about preoperative ACP implementation [49]. Therefore, improvement of the legal system and the provision of financial support may mobilize HCPs to implement preoperative ACP. A living will with legal effect not only safeguards the patient’s autonomy but also guarantees that HCPs will carry out their diagnostic and therapeutic activities in accordance with the law and eliminates misgivings among HCPs about medical disputes arising from the implementation of ACP [19].
In this study, it was found that HCPs in the head and neck surgical department had commonalities with the HCPs in other specialties regarding the implementation of ACP, as well as their own characteristics related to their specialty. This is consistent with the findings of previous studies that most HCPs generally recognize the benefits of ACP, which they believe is important to promote patients’ acceptance of goal-aligned care and protect patients’ rights [50]. In addition, new details regarding the views of HCPs in the head and neck surgical department on the implementation of preoperative ACP in older patients undergoing surgery for HNC were identified. Participants’ recognition of the benefits of preoperative ACP was also based on limitations on the ability of patients with HNC to communicate throughout the course of the disease and the course of treatment, which may result in the inability of patients to adequately access information related to HNC, particularly in relation to end-of-life care [51]. Communicating with patients about their life priorities before and after surgery is important to enable shared decision-making and provide care that respects patients’ values and preferences. However, some HCPs in this study also believed that preoperative counseling for HNC should emphasize cure and that survival and cure should be the first priority for patients receiving treatment [51]. With the relatively low risk of surgery for HNC, it is premature to discuss ACP at this point in time. Such discussions should be held in the event of a critical condition or at the end stage of the disease. The reason for this divergence may lie in the different areas of focus among participants, with the former focusing on safeguarding patients’ informed consent and autonomy and the latter focusing on healing and paying less attention to patients’ psychological, social, and other needs. With the shift in the biomedical paradigm, patient-centered care is increasingly valued, and while emphasizing the curative effects of surgery, it is important to focus on the psychosocial needs of patients, recognizing their concerns and the impact of the consequences of surgery on their daily lives, to provide comprehensive care for patients.
Previous study has shown that the main barrier to ACP implementation is primarily a lack of time [52]. In contrast to other studies, no participants in the three groups believed that there was insufficient time to discuss ACP with patients before surgery. On the contrary, they believed that it was important to make time to discuss matters that were closely related to patients’ lives and treatments, and that despite busy clinical schedules, the necessary discussions would be held, and that the participants in this study would be willing to discuss matters related to ACP with patients if patients take the initiative to communicate with them about it, reflecting the importance that HCPs place on patient autonomy. The participants included in this study were staff members of the Head and Neck Surgery Department, where elective surgery is the mainstay and there is more adequate time for preoperative discussion, which may account for this result.
This study has several limitations. First, only the views of head and neck surgical HCPs were discussed; the views of patients, family members, and other stakeholders on the implementation of preoperative ACP are also important. Second, the study participants were not selected through random sampling and were all from the same hospital, so the study results may not be universally representative, and generalization of the results is somewhat limited. Lastly, to obtain Q statements that are as comprehensive as possible, semi-structured interviews and a literature review were used to generate a Q-set. However, it cannot be guaranteed that the Q statements are sufficiently comprehensive due to the limited number of relevant studies retrieved using the existing strategy. Based on this, future studies should be conducted among all stakeholders in HNC surgery to clarify their views on the implementation of preoperative ACP discussions, and quantitative methods should be used to investigate the extent of the distribution of different perspectives in a multicenter, large-sample setting to better guide future clinical practice. Attempts also should be made to explore interventions to enhance preoperative communication between head and neck surgical HCPs and older patients so as to facilitate preoperative ACP discussions between HCPs and patients and to fully respect patients’ treatment goals and wishes.
5. Conclusion
Q methodology was used in this study to explore the views of head and neck surgical HCPs on the implementation of ACP discussions prior to surgery. The study results yielded three themes: defending the autonomy of patients, patient’s knowledge and the Chinese cultural context hinder preoperative implementation of ACP, and the lack of confidence in performing preoperative ACP. These themes reflected the expectations and concerns of head and neck surgical HCPs on the current implementation of preoperative ACP discussions in China. Some HCPs recognized the benefits of preoperative ACP discussions for patients, but some HCPs were concerned about the negative impact of traditional values, inadequate capacity among HCPs, and unsound laws, making preoperative counseling and ACP discussions with patients undergoing HNC surgery complex. Future studies should be conducted to develop strategies to overcome barriers to preoperative ACP discussions.
CRediT authorship contribution statement
Huixian Yang: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Data Curation, Writing - Original Draft, Writing - Review & Editing. Ruirui Duan: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Writing – review & editing. Yongxia Ding: Conceptualization, Methodology, Validation, Formal analysis, Data Curation, Writing - review & editing, Supervision, Project administration, Funding acquisition. Jing Xu: Conceptualization, Methodology, Validation, Formal analysis, Writing - review & editing. Yanzhi Tian: Conceptualization, Methodology, Validation, Formal analysis, Writing - review & editing.
Funding
This study was funded by Fund Program for the Scientific Activities of Selected Returned Overseas Professionals in Shanxi Province (grant number: 20230024). The funding organizations did not have any role in the study’s design, implementation, or analysis.
Declaration of competing interest
The authors have declared no conflict of interest.
Data availability statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Acknowledgments
We thank LetPub (www.letpub.com) for its linguistic assistance during the preparation of this manuscript.
Footnotes
Peer review under responsibility of Chinese Nursing Association.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2024.03.011.
Appendices. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Sung H., Ferlay J., Siegel R.L., Laversanne M., Soerjomataram I., Jemal A., et al. Global cancer statistics 2020:GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Ca - Cancer J Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Xia C.F., Dong X.S., Li H., Cao M.M., Sun D.Q., He S.Y., et al. Cancer statistics in China and United States, 2022:Profiles, trends, and determinants. Chin Med J. 2022;135(5):584–590. doi: 10.1097/CM9.0000000000002108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gormley M., Creaney G., Schache A., Ingarfield K., Conway D.I. Reviewing the epidemiology of head and neck cancer: definitions, trends and risk factors. Br Dent J. 2022;233(9):780–786. doi: 10.1038/s41415-022-5166-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ellis M.A., Sterba K.R., Day T.A., Marsh C.H., Maurer S., Hill E.G., et al. Body image disturbance in surgically treated head and neck cancer patients: a patient-centered approach. Otolaryngol Head Neck Surg. 2019;161(2):278–287. doi: 10.1177/0194599819837621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen S.C., Yu P.J., Hong M.Y., Chen M.H., Chu P.Y., Chen Y.J., et al. Communication dysfunction, body image, and symptom severity in postoperative head and neck cancer patients: factors associated with the amount of speaking after treatment. Support Care Cancer. 2015;23(8):2375–2382. doi: 10.1007/s00520-014-2587-3. [DOI] [PubMed] [Google Scholar]
- 6.Noor A., Gibb C., Boase S., Hodge J.C., Krishnan S., Foreman A. Frailty in geriatric head and neck cancer: a contemporary review. Laryngoscope. 2018;128(12):E416–E424. doi: 10.1002/lary.27339. [DOI] [PubMed] [Google Scholar]
- 7.Mott F.E., Adams K.C. Advance care planning and end-of-life issues in head and neck cancer. J Palliat Care. 2019;34(1):18–20. doi: 10.1177/0825859718788768. [DOI] [PubMed] [Google Scholar]
- 8.Kalbfell E.L., Buffington A., Kata A.N., Brasel K.J., Mosenthal A.C., Cooper Z., et al. Expressions of conflict following postoperative complications in older adults having major surgery. Am J Surg. 2021;222(4):670–676. doi: 10.1016/j.amjsurg.2021.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rietjens J.A.C., Sudore R.L., Connolly M., van Delden J.J., Drickamer M.A., Droger M., et al. Definition and recommendations for advance care planning: an international consensus supported by the European Association for Palliative Care. Lancet Oncol. 2017;18(9):e543–e551. doi: 10.1016/S1470-2045(17)30582-X. [DOI] [PubMed] [Google Scholar]
- 10.Schuster A.L., Aslakson R.A., Bridges J.F. Creating an advance-care-planning decision aid for high-risk surgery: a qualitative study. BMC Palliat Care. 2014;13:32. doi: 10.1186/1472-684X-13-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Demyan L., Wu G., Moumin D.N., Blumenthaler A.N., Deutsch G.B., Nealon W., et al. Advance care planning in patients undergoing surgery to resect pancreatic adenocarcinoma: underlying tension between balancing hope and realism. Surgery. 2022;171(2):459–466. doi: 10.1016/j.surg.2021.08.033. [DOI] [PubMed] [Google Scholar]
- 12.Goswami P. Impact of advance care planning and end-of-life conversations on patients with cancer: an integrative review of literature. J Nurs Scholarsh. 2023;55(1):272–290. doi: 10.1111/jnu.12804. [DOI] [PubMed] [Google Scholar]
- 13.Song M.K., Kirchhoff K.T., Douglas J., Ward S., Hammes B. A randomized, controlled trial to improve advance care planning among patients undergoing cardiac surgery. Med Care. 2005;43(10):1049–1053. doi: 10.1097/01.mlr.0000178192.10283.b4. [DOI] [PubMed] [Google Scholar]
- 14.Aslakson R.A., Isenberg S.R., Crossnohere N.L., Conca-Cheng A.M., Moore M., Bhamidipati A., et al. Integrating advance care planning videos into surgical oncologic care: a randomized clinical trial. J Palliat Med. 2019;22(7):764–772. doi: 10.1089/jpm.2018.0209. [DOI] [PubMed] [Google Scholar]
- 15.Kata A.N., Sudore R., Finlayson E., Broering J.M., Ngo S., Tang V.L. Increasing advance care planning using a surgical optimization program for older adults. J Am Geriatr Soc. 2018;66(10):2017–2021. doi: 10.1111/jgs.15554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yamamoto K., Kaido T., Yokoi T., Shimada G., Taketa T., Nakayama K. Implementation of advance care planning decision aids for patients undergoing high-risk surgery: a field-testing study. BMC Palliat Care. 2022;21(1):179. doi: 10.1186/s12904-022-01068-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Forner D., Lee D.J., Grewal R., MacDonald J., Noel C.W., Taylor S.M., et al. Advance care planning in adults with oral cancer: multi-institutional cross-sectional study. Laryngoscope Investig Otolaryngol. 2021;6(5):1020–1023. doi: 10.1002/lio2.647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johnson S., Butow P., Kerridge I., Tattersall M. Advance care planning for cancer patients: a systematic review of perceptions and experiences of patients, families, and healthcare providers. Psycho Oncol. 2016;25(4):362–386. doi: 10.1002/pon.3926. [DOI] [PubMed] [Google Scholar]
- 19.Zhu N.X., Yang L., Wang X.L., Tuo J.M., Chen L.L., Deng R.L., et al. Experiences and perspectives of healthcare professionals implementing advance care planning for people suffering from life-limiting illness: a systematic review and meta-synthesis of qualitative studies. BMC Palliat Care. 2023;22(1):55. doi: 10.1186/s12904-023-01176-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blackwood D.H., Vindrola-Padros C., Mythen M.G., Walker D. Advance-care-planning and end-of-life discussions in the perioperative period: a review of healthcare professionals' knowledge, attitudes, and training. Br J Anaesth. 2018;121(5):1138–1147. doi: 10.1016/j.bja.2018.05.075. [DOI] [PubMed] [Google Scholar]
- 21.Zhou F.H., Wang J.Y. Q methodology:A bridge between qualitative and quantitative research. Wuhan University Journal (Philosophy & Social Sciences) 2006;59(3):401–406. [in Chinese] [Google Scholar]
- 22.Churruca K., Ludlow K., Wu W., Gibbons K., Nguyen H.M., Ellis L.A., et al. A scoping review of Q-methodology in healthcare research. BMC Med Res Methodol. 2021;21(1):125. doi: 10.1186/s12874-021-01309-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gu M., Gong C., Kang X.F., Sun J.Y., Zhang B.P., Liu B., et al. Preference of interventions on medication compliance disorders among the heart transplant recipients:A Q methodology research. Military Nursing. 2021;38(3):1–5. doi: 10.3969/j.issn.1008-9993.2021.03.001. [in Chinese] [DOI] [Google Scholar]
- 24.Zabala A., Sandbrook C., Mukherjee N. When and how to use Q methodology to understand perspectives in conservat-ion research. Conserv Biol. 2018;32(5):1185–1194. doi: 10.1111/cobi.13123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ho G.W.K. Examining perceptions and attitudes. West J Nurs Res. 2017;39(5):674–689. doi: 10.1177/0193945916661302. [DOI] [PubMed] [Google Scholar]
- 26.Ramlo S.E. Using Q methodology in health sciences education to study subjectivity. Adv Health Sci Educ. 2023;28(5):1711–1722. doi: 10.1007/s10459-023-10214-1. [DOI] [PubMed] [Google Scholar]
- 27.Shim M.J., Lee S.Y. South Korean early cancer patients' perceptions of difficulties in fighting their disease: a Q methodological approach. Int J Environ Res Publ Health. 2022;19(19) doi: 10.3390/ijerph191912510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Curd P.R. Advance care planning reconsidered: toward an operational definition of outpatient advance care planning. J Palliat Med. 1999;2(2):157–159. doi: 10.1089/jpm.1999.2.157. [DOI] [PubMed] [Google Scholar]
- 29.Banasick S. Ken-Q Analysis (Version 2.0.1)[Computer software]. 10.5281/zenodo.8310377. [Accessed 29 January 2024]. [DOI]
- 30.Xu J., Liang Y. Cognition of clinical tutors by undergraduate nursing students based on Q-methodology. Chin J Pract Nurs. 2017;33(32):2536–2541. doi: 10.3760/cma.j.issn.1672-7088.2017.32.015. [in Chinese] [DOI] [Google Scholar]
- 31.Watts S. SAGE Publications Ltd; London: 2012. Factor interpretation. Doing Q methodological research: theory, method & interpretation. [Google Scholar]
- 32.Mayland C.R., Ho Q.M., Doughty H.C., Rogers S.N., Peddinti P., Chada P., et al. The palliative care needs and experiences of people with advanced head and neck cancer: a scoping review. Palliat Med. 2021;35(1):27–44. doi: 10.1177/0269216320963892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van Rooij J.A.F., Roubos J., Vrancken Peeters N.J.M.C., Rijken B.F.M., Corten E.M.L., Mureau M.A.M. Long-term patient-reported outcomes after reconstructive surgery for head and neck cancer: a systematic review. Head Neck. 2023;45(9):2469–2477. doi: 10.1002/hed.27450. [DOI] [PubMed] [Google Scholar]
- 34.Bradley C.T., Brasel K.J., Schwarze M.L. Physician attitudes regarding advance directives for high-risk surgical patients: a qualitative analysis. Surgery. 2010;148(2):209–216. doi: 10.1016/j.surg.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 35.Wang Y.X., Zhang Y.K., Hong Y., Zeng P., Hu Z.T., Xu X.L., et al. Advance directives and end-of-life care: knowledge and preferences of patients with brain Tumours from Anhui, China. BMC Cancer. 2021;21(1):25. doi: 10.1186/s12885-020-07775-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Berlin A., Kunac A., Mosenthal A.C. Perioperative goal-setting consultations by surgical colleagues: a new model for supporting patients, families, and surgeons in shared decision making. Ann Palliat Med. 2017;6(2):178–182. doi: 10.21037/apm.2016.11.07. [DOI] [PubMed] [Google Scholar]
- 37.Martina D., Lin C.P., Kristanti M.S., Bramer W.M., Mori M., Korfage I.J., et al. Advance care planning in Asia: a systematic narrative review of healthcare professionals' knowledge, attitude, and experience. J Am Med Dir Assoc. 2021;22(2):349.e1–349.e28. doi: 10.1016/j.jamda.2020.12.018. [DOI] [PubMed] [Google Scholar]
- 38.Cheng H.W.B., Shek P.S.K., Man C.W., Chan O.M., Chan C.H., Lai K.M., et al. Dealing with death taboo: discussion of do-not-resuscitate directives with Chinese patients with noncancer life-limiting illnesses. Am J Hosp Palliat Care. 2019;36(9):760–766. doi: 10.1177/1049909119828116. [DOI] [PubMed] [Google Scholar]
- 39.Sun W., Zhang Q.N., Lee S., Luo Z.L. When social work client self-determination principle meets Confucius culture: a living will decision-making case study in China. Omega. 2022 doi: 10.1177/00302228221117864. [DOI] [PubMed] [Google Scholar]
- 40.Zhang J.X., Cao Y.J., Su M.Z., Cheng J., Yao N.L. The experiences of clinical nurses coping with patient death in the context of rising hospital deaths in China: a qualitative study. BMC Palliat Care. 2022;21(1):163. doi: 10.1186/s12904-022-01054-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liao J., Wu B., Ni P., Mao J. Advance directive preferences among terminally ill older patients and its facilitators and barriers in China: a scoping review. J Am Med Dir Assoc. 2019;20(11):1356. doi: 10.1016/j.jamda.2019.05.013. 61.e2. [DOI] [PubMed] [Google Scholar]
- 42.Liu X.B., Chen H., Zhang L.L., Zhang Q.W., Feng T., Liu D.L. Advance care planning engagement among family members of community-dwelling elderly patients with chronic diseases in China: a mixed-methods study. J Hospice Palliat Nurs. 2022;24(2):E26–E34. doi: 10.1097/NJH.0000000000000829. [DOI] [PubMed] [Google Scholar]
- 43.Lee M.C., Auth R., Hinderer K.A., Alexander C.S. Challenges to advance care planning among multidisciplinary health professionals in China. Int J Palliat Nurs. 2017;23(11):552–557. doi: 10.12968/ijpn.2017.23.11.552. [DOI] [PubMed] [Google Scholar]
- 44.Gillies M.A., Sander M., Shaw A., Wijeysundera D.N., Myburgh J., Aldecoa C., et al. Current research priorities in perioperative intensive care medicine. Intensive Care Med. 2017;43(9):1173–1186. doi: 10.1007/s00134-017-4848-3. [DOI] [PubMed] [Google Scholar]
- 45.Dixon J., Knapp M. Whose job? The staffing of advance care planning support in twelve international healthcare organizations: a qualitative interview study. BMC Palliat Care. 2018;17(1):78. doi: 10.1186/s12904-018-0333-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cheng Q.Q., Liu X.Y., Li X.Y., Qing L.M., Lin Q., Wen S.W., et al. Discrepancies among knowledge, practice, and attitudes towards advance care planning among Chinese clinical nurses: a national cross-sectional study. Appl Nurs Res. 2021;58 doi: 10.1016/j.apnr.2021.151409. [DOI] [PubMed] [Google Scholar]
- 47.Cai S.Y., Wang X.J., Wang R.X., Zhou Y.C., Zhou X., Peng X.X. Clinicians' practices and attitudes regarding advance care planning in mainland China: a multicenter cross-sectional survey. Palliat Support Care. 2023;21(3):477–482. doi: 10.1017/S1478951522000177. [DOI] [PubMed] [Google Scholar]
- 48.Chen Y.Y., Cheng Q.Q., Wang Y., Liu X.Y., Li X.Y., Mao T., et al. Knowledge-attitude-practice and counter-measures of advance care planning among nurses. Chinese Nursing Management. 2019;19(3):334–340. doi: 10.3969/j.issn.1672-1756.2019.03.004. [DOI] [Google Scholar]
- 49.Yao D.D., Dong H.J. Application and suggestion for improvement of living will system:Based on article 78 of the medical regulations of shenzhen special economic zone. J Harbin Inst Technol. 2023;25(2):64–71. doi: 10.16822/j.cnki.hitskb.2023.02.007. [DOI] [Google Scholar]
- 50.Fulmer T., Escobedo M., Berman A., Koren M.J., Hernández S., Hult A. Physicians' views on advance care planning and end-of-life care conversations. J Am Geriatr Soc. 2018;66(6):1201–1205. doi: 10.1111/jgs.15374. [DOI] [PubMed] [Google Scholar]
- 51.Roscoe L.A., Tullis J.A., Reich R.R., McCaffrey J.C. Beyond good intentions and patient perceptions: competing definitions of effective communication in head and neck cancer care at the end of life. Health Commun. 2013;28(2):183–192. doi: 10.1080/10410236.2012.666957. [DOI] [PubMed] [Google Scholar]
- 52.Blackwood D.H., Walker D., Mythen M.G., Taylor R.M., Vindrola-Padros C. Barriers to advance care planning with patients as perceived by nurses and other healthcare professionals: a systematic review. J Clin Nurs. 2019;28(23–24):4276–4297. doi: 10.1111/jocn.15049. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.