Summary
Exposure to disasters and public health emergencies negatively affects mental health. Research documenting the psychosocial responses to these calamities in China increased dramatically after the 2008 Wenchuan earthquake. However, there is no comprehensive assessment of the available literature on China's mental health and psychosocial support (MHPSS) responses to these events. This scoping review systematically maps existing published research and grey literature sources regarding MHPSS to disasters and emergencies in China. We examined relevant literature in English and Chinese from six databases and official websites from Jan 1, 2000, to Aug 13, 2021, and included 77 full-text records in this review. The main types of interventions reported included a) stepped care intervention models, b) individual structured psychotherapy and pharmacotherapy, c) mental health education, d) psychological counselling, and e) government-based policy interventions. Most interventions were evaluated using quantitative methods that assessed the treatment of common mental disorders. The review found that rapid national mobilization, emphasis on resilience-strengthening interventions, and the widespread use of step-care models were essential components of reducing the adverse psychosocial effects of disasters. The review also identified remaining gaps, including a) a lack of integration of disaster-related services with the pre-existing health care system, b) inadequate supervision of MHPSS providers, and c) limited monitoring and evaluation of the services provided. These results show where additional research is needed in China to improve mental health services. It also provides a framework that other countries can adapt when developing and evaluating MHPSS policies and plans in response to disasters.
Keywords: Mental health, Disaster, Intervention, Policy, China
Introduction
Background
China is a developing country with the world's largest population and third-largest landmass. It is also one of the most disaster-prone countries. From 1908 to 2008, four of the ten worst global disasters occurred in China.1 Moreover, China's high population density makes nationwide public health emergencies such as epidemics of infectious diseases a significant threat to population health. For example, the 2003 severe acute respiratory syndrome (SARS) epidemic in China resulted in over 7000 cases and 600 deaths2; and the ongoing COVID-19 pandemic in China has already resulted in over 2,364,674 cases and 14,575 deaths.3
In addition to posing a direct threat to people's lives and property, exposure to disasters and public health emergencies is associated with adverse psychosocial consequences among survivors, front-line responders, and other community members. Psychosocial outcomes such as depression, anxiety, posttraumatic stress disorder (PTSD), and functional impairments have been reported in China both during and after different types of disasters (e.g., earthquakes, typhoons, floods, mudslides) and public health emergencies.4, 5, 6 One systematic review7 of publications spanning the ten years following the 2008 Wenchuan earthquake identified 45 peer-reviewed studies about the prevalence of PTSD among earthquake survivors; the reported prevalence of PTSD varied considerably (from 1·3% to 82·6%), partly due to differences in the target population and timing of the surveys. The psychosocial consequences of public health emergencies since the beginning of 21st century have previously been summarized in meta-analyses.8,9 According to a recent meta-analysis, the most prevalent mental health consequence of the COVID-19 pandemic in China is acute stress (39.4%), followed by depression (32·5%) and anxiety (29·6%).10 The deaths, property loss, and dramatic changes in living circumstances that typically accompany disasters and emergencies result in substantial psychosocial burdens on community members that can, in turn, dramatically increase the prevalence and severity of both acute and chronic mental disorders.11 Individual-, community-, and policy-level responses to the psychosocial consequences of disasters and emergencies are critically important.
In China, the development and implementation of mental health and psychosocial support (MHPSS) programs after large-scale disasters and emergencies are relatively new. There were few documented MHPSS interventions in response to disasters or emergencies in China prior to 200812; the only documented pre-2008 MHPSS program was the draft plan for psychological interventions included as part of the Chinese Ministry of Health's 2003 response to SARS.13 The need to include post-disaster psychological assistance as an integral part of the overall disaster response was first recognized by decision-makers and the public following the 2008 Wenchuan Earthquake in Sichuan Province, which resulted in an estimated 69,000 fatalities and nearly 400,000 injuries. Following this major disaster, there were many reports of interventions aimed at preventing or treating post-disaster mental disorders. Since then, China has been integrating MHPSS interventions into national and local plans for managing disasters and public health emergencies.
As summarized by the Chinese Ministry of Health,14 following the Wenchuan earthquake, 39,131 medical personnel in the afflicted areas were trained to administer MHPSS interventions. Mental health services were made available in 2721 local community health service centres (e.g., community hospitals, private clinics) and 1771 local medical institutions (e.g., governmental hospitals). A total of 142,113 individuals received basic psychological counselling, and 55,959 received psychological treatment provided by 1015 psychiatrists and psychiatric nurses from psychiatric hospitals and by 25,464 volunteers who came to Sichuan from all over the country.
The COVID-19 pandemic has been the largest emergency in China since the Sichuan earthquake. Lessons learned from the 2008 earthquake and the 2003 SARS outbreak have helped China improve its methods for addressing the mental health consequences of COVID-19. The State Council published national guidance on mental health interventions related to the pandemic within one month of the onset of the outbreak.15 In addition, 400 mental health professionals were recruited from eight provinces to provide professional MHPSS interventions to hospital workers and inpatients with COVID-19 in Wuhan, where the pandemic started and where the effects of the pandemic were most pronounced. Since the onset of the outbreak, more than 40 books and 100s of articles and videos about pandemic-related mental health education have been published in China, and more than 300 psychological support hotlines have been established.16 There have also been numerous scientific reports about new MHPSS interventions focused on the adverse psychosocial effects of the outbreak.
MHPSS interventions and related research have substantially developed in China during the past decade. Lessons learned from China's experiences with large-scale disasters, emergencies, and similar events can help inform the global framework for understanding and minimizing the mental health consequences of disasters and emergencies.17 However, the literature on disaster-related mental health interventions in China has not been summarized. Enough experience has now been accumulated to warrant systematic mapping of current knowledge about this important issue and, based on the findings, to identify areas that need further research.
Objectives
This scoping review maps existing research and policies regarding the MHPSS response to disasters and emergencies in China and identifies significant gaps in current knowledge about this issue. The review is primarily focused on two research questions: 1) What are the documented MHPSS intervention studies or policies for disasters and emergencies in China? 2) How have these interventions and policies been evaluated, and what is their reported efficacy?
Methods
Protocol registration
The study protocol was drafted based on the methods described in the checklist of the PRISMA extension for scoping reviews (PRISMA-ScR).18 The final protocol was registered prospectively with the Open Science Framework on August 13, 2021 (Identifier: DOI 10.17605/OSF.IO/NZWUR).
Selection criteria
For the purposes of this review, ‘disasters and emergencies’ include natural events, large-scale human-caused events, and widespread public health emergencies. ‘MHPSS responses to disasters and emergencies’ include any local or regional activity that aims to protect or promote psychosocial well-being and any intervention that aims to prevent or treat mental disorders. ‘Interventions’ include, but are not limited to, individual psychological therapy or pharmacologic treatment, formal governmental policies, and community-level mental health education.17
We developed inclusion and exclusion criteria for papers and documents based on the Population, Intervention, Comparator, and Outcome (PICO) framework: 1) Participants: Chinese citizens affected (or potentially affected) by disasters and emergencies in China; 2) Intervention: any MHPSS intervention in response to disasters or emergencies aimed at improving mental/psychological well-being; 3) Outcome: the efficacy of mental health and psychological interventions undertaken in response to disasters and emergencies in China; 4) Study design: randomised controlled trials, case-control studies, cohort studies, case series, case reports, and qualitative studies. We excluded the following types of papers: 1) literature reviews with no empirical data; 2) conference abstracts, dissertations, theses, or book chapters; 3) papers with inadequate information provided for data extraction (e.g., missing intervention details); 4) papers about interventions that do not target a mental health outcome; and 5) papers about interventions that do not occur after a specific disaster or emergency. If any specific intervention is reported in more than one study, only the study with the larger sample size or the longest follow-up was included.
Search strategy
The search strategy used to identify eligible papers and documents in English-language and Chinese-language databases and on Chinese governmental websites is shown in Supplementary Table 1. Three English-language databases (Web of Science, PubMed, and PsychINFO) and three Chinese-language databases (CNKI, Weipu, and Wanfang) were searched for peer-reviewed articles published between January 1, 2000, and August 13, 2021. For papers in Chinese, only articles published in high-quality journals were considered (i.e., ‘Chinese Core Journals’19). The reference lists of the included papers/reports were reviewed to identify other potentially eligible studies and reports not identified in the electronic searches.
The websites of the State Council Policy Document Database, the Chinese Center for Disease Control and Prevention, and the Chinese Psychological Society were searched for officially published national-level policy documents about governmental responses to disasters and emergencies released from 2000 to 2021. These documents were considered ‘grey literature’ sources.
The first round of screening to identify documents that require full-text review was based on titles and abstracts. The second-round review of the full text of potentially eligible papers identified peer-reviewed articles and government documents that met the inclusion and exclusion criteria. Both screening and full-text reviews were carried out by two independent researchers (GL and WS). Disagreements about inclusion were discussed until a consensus was reached.
Data extraction
The items in the final data-collection form used for peer-reviewed articles and government documents are shown in Supplementary Tables 2 and 3, respectively. Two independent research assistants conducted data charting for each article or document (XG, XS, and XF). Any disagreements were resolved by a senior reviewer (GL).
Quality assessment
The quality of evidence provided by each peer-reviewed study was assessed following the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) guidelines.20 Based on these criteria, the quality of evidence about the efficacy of the reported interventions was rated as ‘high’, ‘moderate’, ‘low’, or ‘very low’. Based on a structured assessment, the risk of bias of each included study was rated as ‘low’, ‘some concerns’, or ‘high’.
Synthesis of results
To answer the first research question, we tabulated the characteristics of all included studies. Intervention studies were described along three dimensions: type of disaster or emergency, target population, and type of intervention. To answer the second research question about the evaluation and effectiveness of reported interventions, we described the key outcomes of the identified MHPSS interventions. The grey literature (i.e., published government documents) was reviewed and tabulated separately.
Role of the funding source
The funding source for this review was not involved in the study design, data charting, manuscript drafting, or the decision to submit the manuscript for publication.
Findings
Characteristics of identified reports
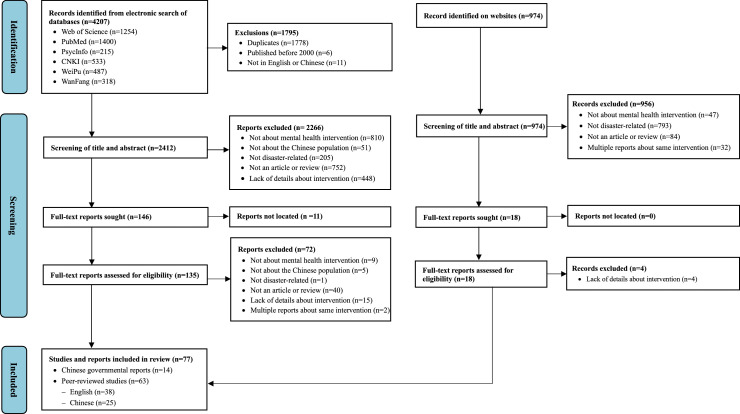
As shown in the PRISMA flowchart for the review (Figure 1), our search yielded 4207 study records and 974 grey literature records. The 77 full-text records that met inclusion and exclusion criteria included 38 English-language peer-reviewed studies, 25 Chinese-language peer-reviewed studies, and 14 Chinese governmental policy reports.
Figure 1.
PRISMA flowchart of documents identified for inclusion in scoping review about disaster-related psychological interventions in China.
The characteristics of the 63 included studies and 14 policy reports are summarized in Tables 1 and 2, respectively. The Chinese Psychological Society (CPS) classifies MHPSS interventions conducted in the first month after a disaster as short-term, those conducted between one to four months after a disaster as middle-term, and those conducted after four months as long-term.13 Among the 49 studies that reported the time between the disaster or emergency and implementation of the intervention, 8 interventions were short-term, 23 middle-term, and 17 long-term; one intervention was delivered across short-, middle-, and long-term periods.21 Except for two studies about interventions related to a 1999 earthquake in Taiwan,21,22 all studies and policies targeted events that occurred after the 2003 SARS epidemic; most of them focused on either the 2008 Wenchuan earthquake or the COVID-19 epidemic.
Table 1.
Characteristics of the 63 post-disaster and post-emergency intervention studies from China included in the review.
| Citation [language] Disaster type [year] Location of disaster Design [months interval] | Target population [scale] Number of participants Duration of intervention | Content of intervention | Primary outcome [assessment method] | Main findings |
|---|---|---|---|---|
| Chao, C. et al., 2009 [CN] Earthquake [1999] Taiwan QE [1 to 70 months]21 | Child [CL] N=537 6 years |
Stage 1 intervention: Mental health education plus group psychotherapy. Stage 2 intervention: group psychotherapy plus individual-level psychological counselling. Stage 3 intervention: screening for mental health problems plus psychological counselling. Stage 4 intervention: follow-up of mental health conditions plus psychological counselling. | PTSD, anxiety [SQ] | The school-based mental rehabilitation work was effective in improving children's long-term mental health after the earthquake. |
| Shen, Y. et al., 2002 [EN] Earthquake [1999] Taiwan RCT [unreported]22 |
Child [IL] N=30 [15 INT, 15 CON 4 weeks |
Intervention: short-term child-centered group play therapy. Control: no treatment. |
General mental health, adjustment, anxiety, and depression [SQ] | Children in the experimental group scored significantly lower on anxiety level and suicide risk after play therapy than children in the control group. |
| Zong, Y. et al., 2010 [CN] Earthquake [2008] Sichuan QE [1 year]68 |
Child [IL] N=210 [129 INT,81 CON] 30 days |
Intervention: Chinese calligraphic handwriting training. Control: no treatment. |
PTSD [SQ] | The PTSD symptom level of the experimental group decreased significantly during the intervention, but no significant changes in PTSD symptoms occurred in the control group. |
| Chen Y, et al. 2014 [EN] Earthquake [2008] Sichuan RCT [24 months]76 |
Adolescents [IL] N=32 [10 INT, 10 CON-A, 12 CON-B] 6 weeks |
Intervention: cognitive behavioural therapy (CBT). Control-A: general supportive intervention. Control-B: no treatment. |
Resilience, PTSD, depression [SQ] | Short-term CBT was more effective than both general supportive intervention and no treatment in enhancing psychological resilience and reducing PTSD and depression among adolescents who had lost parents in the earthquake. The general supportive intervention was only better than no treatment in improving psychological resilience. |
| Chen, L. et al., 2010 [CN] Earthquake [2008] Sichuan RCT [unreported]70 |
Adolescent [IL] N=120 [60 INT, 60 CON] 10 weeks |
Intervention: ballroom dance training (chia-cha). Control: no treatment. |
Anxiety [SQ] | Significant pre-post differences in anxiety levels were observed in the experimental group, but there was no change in the control group; sports, dance, and exercise reduced the anxiety level of middle school students in earthquake-stricken areas. |
| Ouyang, X. et al., 2009 [CN] Earthquake [2008] Sichuan QE [4 months]69 |
Adolescent [IL] N=150 3 months |
Physical exercise. | General mental health [SQ] | A three-month follow-up survey showed significant pre-post intervention reductions in obsessive-compulsive symptoms of boys. In contrast, significant pre-post intervention reductions in depression, anxiety, and phobia symptoms were observed for girls. |
| Qu, X. et al., 2013 [CN] Earthquake [2008] Sichuan QE [11 months]71 |
Adolescent [IL] N=11 [5 INT A, 6 INT B] 6 to 8 weeks |
Group and individual CBT. | PTSD, loneliness, anxiety, self-esteem [SQ] | For both groups, symptoms of PTSD and anxiety significantly decreased, and self-esteem increased significantly after the intervention compared with pre-treatment. There were no significant changes in symptoms between the end of treatment and the three-year follow-up. |
| Zhang, Y., 2019 [CN] Earthquake [2008] Sichuan RCT [unreported]72 |
Adolescent [IL] N=100 [50 INT, 50 CON] 4 months |
Intervention: physical exercise. Control: no treatment. |
General mental health [SQ] | The intervention showed high efficiency for general mental health, with a 90% satisfaction rate. |
| Han, P. et al., 2010 [CN] Earthquake [2008] Sichuan RCT [unreported]84 |
Adult [IL] N=100 [50 INT, 50 CON] 30 days |
Intervention: Chinese Qigong. Control: psychological counselling. |
General mental health, depression [SQ] | Both groups showed significant improvement in mental health conditions after the treatments; however, Chinese Qigong had a better effect than psychological counselling in psychological crisis intervention. |
| Jiang, R. et al., 2014 [EN] Earthquake [2008] Sichuan RCT [38 months]30 |
Adult [IL] N=49 [27 INT, 22 CON] 12 weeks |
Intervention: TAU plus Interpersonal psychotherapy. Control: TAU. |
PTSD, depression [CD] | A significantly greater reduction of PTSD and MDD diagnoses was found in the intervention group. Treatment gains were maintained at six months for the IPT group. |
| Meng, X. et al., 2011 [EN] Earthquake [2008] Sichuan RCT [5 months]79 |
Adult [IL] N=245 [123 INT, 122 CON] 8 weeks |
Intervention: Chinese herbal formula (Xiao-Tan-Jie-Yu-Fang). Control: placebo. |
General mental health [SQ] | The overall mental health of the Xiao-Tan-Jie-Yu-Fang intervention group improved significantly compared to the placebo group. More participants in the Xiao-Tan-Jie-Yu-Fang intervention reported ‘much improvement’ compared to the placebo group. |
| Ruan, X. et al., 2017 [EN] Earthquake [2008] Sichuan RCT [3 years]23 |
Adult [IL] N=239 [118 INT,121 CON] 15-30 minutes |
Intervention: general health education plus a structured brief intervention. Control: general health education. |
Alcohol use [SQ] | The intervention group had reduced alcohol use when compared with the control group. |
| Wang, Z. et al., 2013 [EN] Earthquake [2008] Sichuan RCT [3.5 years]31 |
Adult [IL] N=94 [49 INT, 45 CON] 4 weeks |
Intervention: web-based Intervention (Chinese My Trauma Recovery). Control: WL. |
PTSD [SQ] | Chinese My Trauma Recovery reduced PTSD symptoms significantly with a large effect size after one month of treatment, and the reduction was sustained at a 3-month follow-up. |
| Zang, Y. et al., 2014 [EN] Earthquake [2008] Sichuan RCT [30 months]77 |
Adult [IL] N=30 [10 INT A, 10 INT B, 10 CON] 3 months |
Intervention A: narrative exposure therapy (NET). Intervention B: revised narrative exposure therapy (NET-R). Control: WL. | PTSD, depression, anxiety, social support [SQ, SR] | Compared with controls, both NET and NET-R groups showed significant reductions in PTSD and related symptoms. Further reductions in PTSD symptoms were found at three months, indicating that NET-R is as effective as the original NET in treating post-earthquake traumatic symptoms. Perceived social support did not change as a result of the treatment. |
| Chen, L. et al., 2009 [CN] Earthquake [2008] Sichuan QE [14 to 19 days]62 |
Earthquake wounded (inpatient) [IL] N=60 unreported |
Less-severe symptom group intervention: mental health education. More-severe symptom group intervention: psychological counselling plus relaxation training plus group psychotherapy. | General mental health [SQ] | Significant reductions in pre-post SCL-90 and SRQ scores were observed within the psychological intervention group. |
| Hu, M. et al., 2010 [CN] Earthquake [2008] Sichuan CR [12 days]27 |
Earthquake wounded [IL] N=1 Unreported |
Cognitive therapy, emotional support, progressive muscle relaxation therapy. | Depression, anxiety [SQ, SR] | Cognitive therapy and relaxation techniques were effective in changing negative beliefs, and the treatment had significant effects in reducing depression and anxiety symptoms. |
| Tian, G. et al., 2010 [CN] Earthquake [2008] Sichuan QE [14 days]26 |
Earthquake wounded (inpatient) [IL] N=72 10-15 days |
Low-risk population: psychological counselling and mental health education. Moderate-risk population: cognitive therapy plus desensitization therapy. High-risk population: medications. | General mental health [SQ] | The intervention was effective; the SRQ of all the wounded and sick people returned to normal levels |
| Xi, S. et al., 2008 [CN] Earthquake [2008] Sichuan QE [unreported]129 |
Earthquake wounded (inpatient) [IL] N=34 unreported |
Psychological nursing, mental health education. | Depression, anxiety [SQ] | After the intervention, anxiety symptoms decreased significantly, but no significant changes in depression symptoms were found. |
| Xiang, M. et al., 2008 [CN] Earthquake [2008] Sichuan QE [within 2 weeks]29 |
Earthquake wounded (inpatient) [IL] N=238 2 weeks |
Psychological nursing, social support, mental health education. | General mental health, anxiety [SQ] | After the intervention, anxiety symptoms significantly decreased, though no significant improvements were observed in general mental health |
| Xue, Y. et al., 2009 [CN] Earthquake [2008] Sichuan QE [0.5 to 1.5 months]88 |
Earthquake wounded (inpatient) [IL] N=25 unreported |
Mental health education, psychological counselling. | Positive and negative emotions, stress [SQ] | After the intervention, the mental health status improved for male participants but not for female participants. |
| Yao, L. et al., 2008 [CN] Earthquake [2008] Sichuan QE [within a week]28 |
Earthquake wounded (inpatient) [IL] N=45 1 month |
Provide a safe and comfortable environment, daily nursing, psychological counselling, and social support. | Mental health [SQ] | The mental health of the wounded improved after the intervention. The pre-post intervention SRQ mean score was significantly lower. |
| Yu, H., 2019 [CN] Earthquake [2008] Sichuan QE [unreported]64 |
Earthquake wounded (inpatient), their caregivers [IL] N=80 3 months |
Art therapy, psychological counselling. | General mental health, depression, anxiety, stress [SQ, SR] | Art therapy showed better effectiveness in treating depression, anxiety, and general mental symptoms than psychological counselling. |
| Wang, H. et al., 2008 [CN] Earthquake [2008] Sichuan QE [unreported]78 |
Insomnia patients [IL] N=150 [50 INT A, 50 INT B, 50 INT C] Half a month |
Intervention A: Psychological counselling alone. Intervention B: medications alone. Intervention C: combination counselling and medication. | Sleeping time, mental status [SR] | Three treatments were compared. After treatment, the self-reported mental status of the first two groups had improved, and the time spent asleep had increased but remained short. When the two therapies were combined, the mental state improved significantly compared with either of the single treatments. |
| Leitch, L. et al., 2009 [EN] Earthquake [2008] Sichuan NE [2 months]34 |
Medical personnel, first responders [CL] N=367 18 months |
Biological-focused psychoeducation. | Intervention satisfaction [SQ] | A total of 97% of participants believed that biologically-oriented training would be ‘very to moderately relevant or useful’ for their work with the Chinese earthquake survivors. About 88% reported they would likely use the skills ‘very to moderately frequently’ during the two weeks following the training. Over 60% of the trainees reported they would likely use these skills for personal self-care. |
| Wu, S. et al., 2011 [EN] Earthquake [2008] Sichuan RCT [1 month]32 |
Rescuers [CL] N=1267 [417 INT A, 421 INT B, 429 CON] unreported |
Intervention A: critical incident stress debriefing (CISD) plus cohesion training. Intervention B: critical incident stress debriefing (CISD). Control: no treatment. | PTSD, anxiety, depression [SQ, INT] | Significantly lower scores of PTSD and positive efficacy in improving symptoms of re-experiencing, avoidance, and hyperarousal were found in the intervention group that received the debriefing intervention compared to the control group. |
| Niu, Y. et al., 2021 [EN] Earthquake [2010] Qinghai RCT [9 years]52 |
Adolescent [IL] N=56 [28 INT, 28 CON] unreported |
Intervention: culturally adapted resilience intervention. Control: TAU. |
Resilience, mental health, self-esteem, interpersonal skills [SQ] | Compared with the control group, the intervention group showed significant improvement in mental health and interpersonal skills, but no significant difference in resilience or self-esteem was found. |
| Li, X. et al., 2011 [CN] Earthquake [2010] Qinghai QE [3 days]51 |
Earthquake wounded (inpatient) [IL] N=90 47 days |
Tibetan culture-based counselling, group psychotherapy, medicine. | Acute stress disorder [SQ] | The acute stress disorder (ASD) rate dropped from 38.89% to 0% after the intervention. |
| Huang, X. et al., 2014 [CN] Earthquake [2013] Sichuan QE [within a week]53 |
Earthquake wounded (inpatient) [IL] N=107 4 weeks |
Psychological counselling. | General mental health, anxiety, depression [SQ] | After the intervention, mental health, anxiety, and depression scores were significantly lower. |
| Ke, Y. et al., 2017 [EN] Earthquake [2016] Taiwan QE [unavailable]55 |
Healthcare provider [IL] N=67 unreported |
Psychological support, muscle and mental relaxation. | PTSD [SR] | After the intervention, no healthcare providers reported PTSD in the follow-up questionnaire, indicating good resilience after the early intervention. |
| Guan, J. et al., 2018 [CN] Earthquake [2017] Sichuan QE [unreported]54 |
Earthquake wounded (inpatient) [IL] N=25 1 week |
Less-severe symptom group: general psychological nursing. Moderately severe symptom group: group psychotherapy. Serious symptom group: individual-level comprehensive psychotherapy. Severe symptom group: refer to psychiatrists. | Anxiety, depression [SQ] | After the intervention, anxiety and depression symptom levels were significantly lower. |
| Cheng S, et al. 2012 [EN] Typhoon [2009] Taiwan QE [2 months]59 |
Adult [IL] N=77 6 months |
Individual resilience strengthening and maintenance, resource linking and referral. | PTSD, depression, resilience [SQ] | After completing the individual resilience intervention program, participants had higher individual resilience scores than before participating in the program. |
| Jin, N. et al., 2003 [CN] SARS [2003] National QE [unreported]58 |
Adult [IL] N=138 14 days |
Mental health education, psychological counselling. | Anxiety [SQ] | After the intervention, the average anxiety score of isolated students decreased, which was not significantly different from the healthy population but lower than pre-intervention scores. |
| Cui, S. et al., 2004 [CN] SARS [2003] National QE [6 months]57 |
SARS patients (inpatient) [IL] N=48 unreported |
Cognitive therapy, emotional support, mental health education. | Sleeping time, emotional symptoms [SR] | Of the 17 individuals who reported sleeping difficulty, 10 improved after the intervention. Of the 18 individuals with emotional problems, 15 reported improved emotion after the intervention. |
| Wang, Z. et al., 2003 [CN] SARS [2003] National QE [5 months]56 |
SARS patients (inpatient) [CL] N=680 [483 INT,197 CON] unreported |
Hotline counselling, face-to-face counselling, and mental health education. | General mental health [SQ] | Most factors of the SCL-90 were significantly lower in the intervention group than in the control group after treatment. Patients’ response rates to different treatment sessions were compared. Active telephone consultation demonstrated the highest response rate (95.7%), and written materials rated the lowest (19.59%). The response rate of passively receiving telephone consultation was 46.7%. The response rate of face-to-face counselling provided by medical personnel or psychologists ranged from 81.4% to 87.1%. |
| Xie, X. et al., 2004 [CN] SARS [2003] National QE [unreported]25 |
Fever patients [CL] N=713 3 days |
Mental health education. | General mental health [SQ] | After treatment, all symptom factors were significantly improved for patients in the different subgroups. |
| Zheng, Y. et al., 2021 [EN] COVID-19 [2019] National RCT [3 months]48 |
Child [CL] N=896 [467 INT, 429 CON] 2 weeks |
Intervention: mental health education plus peer-to-peer live-streaming app (Recess and Exercise Advocacy Program). Control: mental health education. | Anxiety [SQ] | The 2-week decrease in self-reported anxiety scores was greater in the intervention versus the control group. |
| Chen, J, et al. 2021 [EN] COVID-19 [2019] National RCT [5 months]35 |
Adolescents [IL] N=69 [34 INT, 35 CON] 8 weeks |
Intervention: aerobics exercise combined with mindfulness meditation training. Control: treatment as usual (TAU). | Anxiety, positive and negative emotion, overall psychological well-being [SQ] | The decrease in anxiety symptoms was greater in the experimental group than in the control group, and the positive emotion score in the experimental group was higher than that of the control group. |
| Ding, X. et al., 2020 [EN] COVID-19 [2019] National RCT [2 months]74 |
Adolescents [IL] N=150 [75 INT, 75 CON] 8 weeks |
Intervention: aerobics exercise combined with mental health education. Control: TAU. | Anxiety, depression, sleep quality [SQ] | After the intervention, anxiety symptoms reduced more in the intervention group than those in the control group; depression symptoms and sleep quality improved in both groups, but the effect was larger among those receiving the intervention. |
|
Liu, X. et al., 2021 [EN] COVID-19 [2019] National RCT [4 months]37 |
Adolescents [IL] N=121 [61 INT, 60 CON] 8 weeks |
Intervention: TAU plus logotherapy-based mindfulness intervention. Control: TAU. |
Internet addiction [SQ, SR] |
After the intervention, five dimensions of internet addiction showed significant decreased in the experimental group compared to the control group. |
| Xu, W. et al., 2021 [EN] COVID-19 [2019] National RCT [3 months]43 |
Adolescent [IL] N=83 [39 INT, 44 CON] 8 weeks |
Intervention: acceptance and commitment therapy (ACT) plus aerobic exercise. Control: mental health education. | Psychological distress, well-being, psychological flexibility [SQ] | In the experimental group, significant differences in psychological distress, well-being, and psychological flexibility were found before and after the intervention; no significant differences were found in the control group. |
| Zhang, J. et al., 2021 [EN] COVID-19 [2019] National RCT [5 months]73 |
Adolescent [IL] N=153 [76 INT, 77 CON] 8 weeks |
Intervention: psychological counselling model plus physical exercise. Control: mental health education. |
Anxiety, depression, sleep quality, resilience [SQ] | After the intervention, the experimental group demonstrated greater improvement in anxiety, depression, resilience, and sleep quality scores compared to the control group. |
| Li, S. et al., 2021 [EN] COVID-19 [2019] National RCT [2 months]85 |
Adult [IL] N=187 [96 INT, 91 CON] 1 week |
Intervention: self-affirmation writing exercise. Control: unrelated writing exercise. |
Anxiety [SQ] | Participants who affirmed their values showed lower anxiety responses than those in the control group in both post-treatment and follow-up assessments. |
| Liu, X. et al., 2021 [EN] COVID-19 [2019] National QE [2 months]89 |
Adult [IL] N=150 [90 INT, 60 CON] 8 weeks |
Intervention: strength-based online community intervention (SOCI). Control: TAU. |
Stress, well-being, resilience [SQ] | This research revealed that SOCI had significantly improved participants' resilience, spirituality, and positive growth over time but not post-traumatic stress or negative affect. |
| Lu, T. et al., 2021 [EN] COVID-19 [2019] National RCT [3 months]86 |
Adult [IL] N=63 [31 INT, 32 CON] 40 minutes |
Intervention: wise intervention. Control: unrelated reading and writing. |
Personal discrimination [SQ] | The wise intervention reduced perceived discrimination in the experimental group compared to the control group. |
| Song, J. et al., 2021 [EN] COVID-19 [2019] National QE [4 months]46 |
Adult [IL] N=129 [83 INT, 46 CON] 8 weeks |
Intervention: internet-based cognitive behavioural therapy (iCBT). Control: WL. |
Depression, intervention satisfaction [SQ, SR] | The MiCBT group showed significant improvement in depression compared with the wait-list group. The intervention was considered helpful (81.9%) and enjoyable (65.9%). |
| Sun, S. et al., 2021 [EN] COVID-19 [2019] National RCT [3 months]47 |
Adult [IL] N=114 [57 INT, 57 CON] 4 weeks |
Intervention: mindfulness-based mobile health. Control: social support-based mobile health. |
Anxiety, depression, and acceptability [SQ, SR] | Both mindfulness and social support, delivered via mHealth, showed promise in reducing distress among young adults in quarantine, with mindfulness being particularly effective in addressing anxiety and depression. Furthermore, mindfulness mHealth was more feasible and acceptable than social support mHealth. |
| Wu, C. et al., 2021 [EN] COVID-19 [2019] National QE [1 month]87 |
Adult [IL] N=638 [372 INT, 266 CON] 2 weeks |
Intervention: mental health education plus cognitive adjustment plus relaxation training. Control: no treatment. |
General mental health [SQ] | Most SCL-90 factors decreased significantly for participants in the intervention group. In contrast, SCL-90 factors changed little and showed no statistical significance in the control group. |
| Zhang, H. et al., 2021 [EN] COVID-19 [2019] National RCT [1 month]38 |
Adult [IL] N=57 [29 INT, 28 CON] 2 weeks |
Intervention: brief online mindfulness-based group intervention. Control: WL. |
Psychological distress [SQ] | The online mindfulness-based intervention was effective at reducing psychological distress for study participants in comparison to the control group. |
|
Zhang, W. et al., 2020 [EN] COVID-19 [2019] National CS [7 months]49 |
Adult (inpatient) [IL] N=3 unreported |
Virtual reality exposure therapy (VRET). |
Phobic symptoms, anxiety, avoidance behaviour, social functioning [SQ, SR] |
Anxiety symptoms showed a significant decrease between the pre-VRET intervention and after the final VRET intervention. No significant reduction in phobic symptoms, avoidance behaviour, or social functioning. |
| Ren, Y. et al., 2021 [EN] COVID-19 [2019] National RCT [unreported]42 |
Elderly [IL] N=121 [61 INT, 60 CON] 8 weeks |
Intervention: group reminiscence therapy plus physical exercise. Control: mental health education. |
Well-being, loneliness, and resilience [SQ] | After the intervention, significant improvements in loneliness, well-being, and resilience were observed in the experimental group compared to the control group. |
| Hu, C. et al., 2020 [EN] COVID-19 [2019] National CR [1 month]36 |
COVID-19 patient (inpatient) [IL] N=1 3 weeks |
Interpersonal psychotherapy. | Depression, anxiety [SQ] | IPT-based therapy reduced the patient's depression and anxiety symptoms. |
| Li, J. et al., 2020 [EN] COVID-19 [2019] National RCT [2 months]39 |
COVID-19 patient (inpatient) [IL] N=93 [47 INT, 46 CON] 4 weeks |
Intervention: TAU plus CBT. Control: TAU. |
Depression, anxiety, stress [SQ] | Significant decreases in depression, anxiety, stress, and total DASS-21 scores were found in both intervention and control groups, with participants in the intervention group having a greater reduction. After the intervention, more participants in the intervention group had no depression or anxiety symptoms compared to the control group. |
| Liu, Y. et al., 2021 [EN] COVID-19 [2019] National RCT [3 months]90 |
COVID-19 patient (inpatient) [IL] N=140 [70 INT, 70 CON] 1 month |
Intervention: group psychotherapy plus pulmonary rehabilitation exercises. Control: TAU. | Sleep quality, anxiety [SQ] | Group psychological intervention combined with pulmonary rehabilitation exercises significantly reduced anxiety symptoms and sleep disorders of COVID patients compared to controls. |
| Liu, Z. et al., 2021 [EN] COVID-19 [2019] National RCT [5 months]45 |
COVID-19 patient (inpatient) [IL] N=252 [126 INT,126 CON] 1 week |
Intervention: TAU plus computerized cognitive behavior therapy (cCBT). Control: TAU. |
Depression, anxiety [SQ] | The cCBT + TAU group displayed significantly decreased levels of depression and anxiety symptoms after the intervention compared to the TAU group. |
| Yang, D. et al., 2021 [CN] COVID-19 [2019] National QE [unreported]61 |
COVID-19 patient (inpatient) [IL] N=200 1 month |
Mental health education, individual-level comprehensive psychotherapy, group psychotherapy. | Depression, anxiety, general mental health [SQ] | After the intervention, depression, anxiety, and all SCL-90 dimensions except obsessive behaviour were significantly lower than before the intervention. |
| Cheng, W. et al., 2020 [EN] COVID-19 [2019] National QE [2 months]65 |
Medical personnel [IL] N=155 6 weeks |
Daily mood broadcast, online themed group chat, focused group discussion with health care professionals, and social support. | Daily Mood Index, individual impressions of gains and challenging issues [SQ] | The Daily Mood Index of the medical team significantly improved compared with its initial level and showed a gradual upward trend over time. |
| Li, Y. et al., 2021 [CN] COVID-19 [2019] National RCT [2 months]66 |
Medical personnel [IL] N=300 [150 INT,150 CON] unreported |
Intervention: Outward Bound training. Control: no treatment. |
General mental health, depression, anxiety, function [SQ] | General mental symptoms, depression, and anxiety symptoms significantly decreased in the intervention group, but no difference was found in the control group. Functional levels significantly improved for the intervention group but not for the control group. |
| Liu, Y. et al., 2021 [EN] COVID-19 [2019] National QE [2 months]40 |
Medical personnel [IL] N=140 2 weeks |
Diaphragmatic breathing relaxation training. | Sleep quality, anxiety, and depression [SQ] | Participants achieved significant improvement in overall sleep quality, different dimensions of sleep quality, and anxiety symptoms. No significant reductions were found in the use of sleeping medication or depression symptoms. |
|
Yang, C. et al., 2020 [EN] COVID-19 [2019] National QE [unreported]41 |
Medical personnel [IL] N=39 6 hours |
Short-term Balint group activity. |
Communication ability, self-efficacy [SQ, SR] |
After the intervention, 86.6% of nurses reported that their communication with patients had improved. Overall self-efficacy after the intervention was not significantly increased. |
| He, Z. et al, 2020 [EN] COVID-19 [2019] National NE [1 to 2 months]50 |
General population [IL] N unreported 1 to 2 months |
4-tier COVID-19 Psychological Resilience Model (Tier 1: mental health education, Tier 2: hotline counselling, Tier 3: online video psychotherapy & on-site psychological counselling, Tier 4: training and supervision of service providers). | N/A | A total of 45 episodes of live media programs on the COVID-19 outbreak-related psychological problems had over 10 million views during the broadcasts. Of the completed 4,236 hotline consultations, more than 50% of the clients had positive feedback. Online video interventions were shown to 223 subjects. Seventy one-on-one psychological interventions were conducted with 39 COVID-19 patients, and five training sessions were given to 98 front-line medical staff. |
| Huang, J et al., 2020 [EN] COVID-19 [2019] National CR [2 months]82 |
Pregnant woman (inpatient) [IL] N=1 2 weeks |
Dialectical behavioural therapy. | Depression, anxiety [SQ, INT] | The effectiveness of the intervention was supported by the reduction in depression and anxiety symptoms and the positive feedback about the alleviation of depression and anxiety symptoms reported by the patient. |
| Liu, G. et al., 2021 [EN] COVID-19 [2019] National QE [1 month]44 |
Mothers of autism child [IL] N=125 [65 INT, 60 CON] 12 weeks |
Intervention: WeChat-based parent training. Control: enhanced treatment as usual. |
Anxiety, depression, parenting stress, satisfaction [SQ, SR] | The intervention was significant in reducing anxiety, depression, and parenting stress. Of all participants in the intervention group, 90.4% reported extreme satisfaction with the WeChat-based training. |
| Zhang, Q. et al., 2021 [EN] COVID-19 [2019] National QE [2 months]24 |
Patients undergoing maintenance hemodialysis (inpatient) [IL] N=172 7 months |
General psychological nursing. | Depression, anxiety [SQ] | After the intervention, there were significant reductions in depression and anxiety symptoms. |
Language, language of publication: EN=English, CN=Chinese.
Year, year disaster occurred.
Design, design of intervention, RCT=randomised controlled trial, QE=quasi-experimental study, CS=case series, CR=case report, NE=no evaluation.
Months interval, months from occurrence of disaster to start of intervention.
Scale, type of intervention, IL=individual level, CL=community-level.
Number of participants, INT=number in intervention group, CON=number in control group.
Content of intervention, IPT=interpersonal psychotherapy, CBT=cognitive behavioural therapy, TAU=treatment as usual, WL=waitlist control.
Assessment method, SQ=structured questionnaire, SR=self-report, CD=clinical diagnosis, INT=interview.
Table 2.
Characteristics of the 14 national-level policy reports that consider post-disaster and post-emergency psychological services in China included in this review.
| Title | Type of disaster | Time of disaster | Geographic region | Content of intervention | Agency |
|---|---|---|---|---|---|
| Guidelines to further protect medical personnel during the COVID-19 pandemic100 | COVID-19 | 2019 | Nationwide | Improve the psychological intervention offered to first-line medical personnel, strengthen psychological assistance, and conduct psychological assessments. Monitor changes in mental health status via regular chats. | National work group for fighting the COVID-19 pandemic |
| The State Council's guidelines on the sanitary and anti-epidemic work in earthquake-stricken areas128 | Earthquake | 2008 | Sichuan | Conduct psychological assistance work based on existing medical and mental health service networks. Implement hierarchical interventions for different populations, especially for people most vulnerable to the disaster effects. | State Council of China |
| National Health Commission's guideline to further improve mental health work130 | Nonspecific | N/A | N/A | Make post-disaster mental health rescue contingency plans and control the morbidity of mental disorders after disasters. Conduct psychological interventions and assess the need for mental health services after disasters. Determine the target population for post-disaster psychological interventions and provide hotline counselling and out-patient psychiatric care. | National Health Commission of China |
| The State Council's rebuild plan for the Zhou Qu landslide98 | Landslide | 2010 | Gansu | Establish mental rehabilitation centres based on local medical institutions and organise professional therapists to conduct psychological interventions and treat psychological trauma. | State Council of China |
| The State Council's rebuild plan for the Yu Shu earthquake97 | Earthquake | 2010 | Qinghai | Establish mental rehabilitation centres based on local medical institutions and organise professional therapists who can speak Mandarin and Tibetan to conduct psychological interventions and treat psychological trauma. | State Council of China |
| The State Council's rebuild plan for the Lu Dian earthquake96 | Earthquake | 2013 | Yunnan | Establish mental rehabilitation centres based on local medical institutions and use comprehensive psychological intervention to treat psychological trauma. | State Council of China |
| The State Council's rebuild plan for the Lushan earthquake95 | Earthquake | 2013 | Sichuan | Use comprehensive psychological interventions to help build people's mental resilience in disaster-affected areas. | State Council of China |
| The State Council's rebuild plan for the Wenchuan earthquake94 | Earthquake | 2008 | Sichuan | Provide mental health education for primary and secondary schools, set up outpatient mental health care in local hospitals, host special news sessions via the media, organize professionals and volunteers to provide services in the communities, open hotline counselling services, train psychological workers, publish work manuals and textbooks for local volunteers, encourage internal collaborations in improving the mental health of the affected population. | State Council of China |
| The work plan to control the spread of H1N1 in communities99 | H1N1 epidemic | 2009 | Nationwide | Implement public psychological interventions to minimize the impact of the pandemic on the public's mental health. | National Health Commission of China |
| The emergency operation guide for natural disaster-related health work104 | All natural disasters | N/A | N/A | Conduct psychological intervention under the supervision of well-trained mental health professionals. Combine basic therapy techniques with mental health education to provide psychological rescue. Monitor the mental health condition of the affected populations. Establish social support networks among communities. Recommendations included short-term, group-based psychological counselling strategies with high flexibility. | China CDC |
| The technical guide for prevention and control of disease after an earthquake101 | All earthquakes | N/A | N/A | Provide psychological assistance to those exposed to corpses and chemical spills. Set up different onsite intervention plans for different situations. Follow-up assessments are needed post-interventions. Conduct mental health education in resettlement sites and schools. Provide training for teachers and medical personnel and enhance their ability to identify people with mental disorders and how to make referrals to psychiatrists or certificated psychotherapists. | China CDC |
| The information to set up psychological assistance hotlines during the COVID-19 pandemic103 | COVID-19 | 2019 | Nationwide | Build a hotline expert group to provide technical support; promote the hotline number via TV, websites, and other media; and expand the hotline service team. Develop a standard operating procedure for hotline services. Summarize and analyze the topics of the hotline counselling. | State Council of China |
| The 2010 post-earthquake psychological assistant program102 | Earthquake | 2008, 2010 | Sichuan, Qinghai | Provide mental health education for survivors and psychological counselling for high-risk individuals and civil servants who participated in the post-disaster reconstruction. Provide training to rural medical personnel to enhance their ability to provide mental health services. Provide psychological supervision for hospital mental health professionals from provincial and urban levels. | National Health Commission of China |
| The An Xin program to fight the COVID-19 pandemic105 | COVID-19 | 2019 | Nationwide | Provide online series of lectures on mental health for the public, volunteers, medical personnel, and students. Offer online psychological counselling, mental health assessments, and digital mental health interventions. Provide supervision for psychological workers. Build community workstations and service stations. Dispense psychological knowledge to the populace. | Chinese Psychological Society |
Among the 63 peer-reviewed studies, 57 interventions were delivered at the individual level and 6 at the community level. The shortest individual-level intervention was a one-time, 15- to 30-minute structured intervention to treat problematic alcohol use among earthquake survivors;23 the longest was a 7-month nursing support program for inpatients undergoing maintenance hemodialysis during the COVID-19 pandemic.24 The shortest community-level intervention was a three-day mental health education program for hospital outpatients with fever during the 2003 SARS epidemic25; the longest was a six-year, school-based mental health rehabilitation program after a 1999 earthquake in Taiwan.21
Disasters and emergencies considered in the MHPSS intervention studies
The 2008 Wenchuan earthquake
The 2008 Wenchuan earthquake marked a milestone in the development of clinical psychology in China. Some MHPSS work was conducted in response to public emergencies prior to the earthquake, but most of it remained undocumented or unpublished. Public awareness of the importance of mental health increased significantly after the disaster, resulting in a rapid increase in MHPSS-related organizations, policies, and research. In the current review, MHPSS interventions for this earthquake account for 60% (15/25) of all identified Chinese-language publications and 21% (8/38) of all identified English-language publications. The earliest individual-based MHPSS interventions were provided within two weeks after the earthquake to people hospitalized due to injuries;26, 27, 28, 29 all of these early interventions involved psychoeducation, emotional support, or brief psychological counselling provided to hospital inpatients by trained nurses. Some interventions included structured psychotherapies such as cognitive behavioural therapy (CBT) or mindfulness.26,27 One study provided stepped-care based on the assessed risk of adverse psychological outcomes:26 low-risk individuals received mental health education and psychological counselling, vulnerable individuals without severe stress symptoms (e.g., children) received cognitive behavioural therapy and desensitization therapy, and high-risk individuals with severe stress symptoms were prescribed psychotropic medications as adjunctive treatments to talk therapies.
Another subset of studies focuses on the long-term psychosocial outcomes of the earthquake. Clinical trials assessing the efficacy of treatments of mental health problems among earthquake survivors three years after the disaster include studies about in-person interpersonal psychotherapy,30 a web-based intervention,31 and a structured brief intervention for substance abuse.23 However, interventions targeting more chronic psychosocial consequences of disasters – such as the delayed onset of mental disorders – are lacking.
Community-level interventions include the ‘512 Psychological Intervention Model’ administered one month after the earthquake to 1267 military personnel who participated in the initial rescue operation.32 Based on Mitchell's critical incident stress debriefing (CISD) model,33 the intervention contained five sessions: introduction, facts and thoughts, reaction and symptoms, stress management, and training to increase community cohesion. Another community-level intervention evaluated the administration of a neuroscience-focused psychoeducation program for medical personnel and first responders.34
The COVID-19 pandemic
The outbreak of COVID-19 in late 2019 was a regional medical emergency in Wuhan (the capital city of Hubei Province) that subsequently expanded to become a nationwide public health emergency. The governmental response to the adverse psychosocial effects of the pandemic was more systematic and better organized than its response to the 2008 Sichuan earthquake. Among the 63 included studies, 8% (2/25) of the Chinese-language papers and 68% (26/38) of the English-language papers were about the COVID-19 pandemic.
One-half of the reported interventions (14/28) were conducted within two months after the onset of the outbreak, soon after the release of the government's national guidance on the identification and management of mental health problems during the epidemic.16 Compared to the interventions employed after the 2008 earthquake, more study participants were treated with structured, time-limited interventions, including cognitive behaviour therapy (CBT), interpersonal therapy, and mindfulness training.35, 36, 37, 38, 39, 40, 41 To improve both the physical and psychosocial functioning of targeted communities, aerobic exercise was combined with psychotherapy,35 reminiscence therapy,42 and acceptance and commitment therapy.43 Several interventions based on IT technologies (e.g., virtual reality exposure therapy, mobile internet CBT, and online mindfulness-based group intervention) were developed and tested.38, 44, 45, 46, 47, 48, 49 One large-scale community intervention,50 the ‘COVID-19 Psychological Resilience Model’, broadcast media programs about COVID-19-related psychological problems to 10 million viewers, completed 4236 hotline consultations, conducted 233 online video assessments, and provided one-on-one psychological treatment to 39 individuals with COVID-19-related mental disorders.
Other disasters and emergencies
Only 8 of the 25 identified intervention studies published in Chinese and 4 of the 38 intervention studies published in English were not about the 2008 Sichuan earthquake or the COVID-19 epidemic. Seven of these 12 studies were about post-earthquake interventions: two interventions for children following the 1999 Taiwan earthquake;21,22 two interventions conducted after the 2010 Yushu earthquake in Qinghai Province;51,52 and one intervention reported after the 2013 Lushan earthquake in Sichuan Province,53 the 2017 Jiuzhai earthquake in Sichuan Province,54 and the 2016 earthquake in Taiwan.55 The remaining five studies included four education and counselling-based interventions provided to SARS patients and quarantined students during the 2003 SARS epidemic25,56, 57, 58 and one individual resilience-focused intervention after the 2009 Typhoon Morkot in Taiwan.59 To date, no study has reported MHPSS interventions after man-made disasters in China.
Target populations in the MHPSS intervention studies
Direct survivors
Direct survivors are individuals who directly experience a threat to their life during disasters or emergencies. They are more likely to experience mental health problems than indirectly affected individuals and, if they do experience a mental health problem, it is likely to be more severe and more persistent.60 About 29% (18/63) of the identified interventions focused on direct survivors, including people injured in earthquakes or infected during the SARS or COVID-19 epidemics and half of these interventions (9/18) were initiated soon after the index event.
Interventions for direct survivors were all conducted by medical personnel in general hospital settings; most of these interventions integrate mental health education, social support, and individual or group counselling into daily nursing care.28,53,54,56,57,61 Some interventions also provide structured therapies including cognitive therapy or CBT.27,39,45,57 Considering the need to triage services in the immediate aftermath of the index event – when local medical systems are overwhelmed by the high demand for mental health services – the national government's State Council recommended using hierarchical models to provide stepped care to direct survivors. Two studies of earthquake victims have reported using hierarchical stepped-care MHPSS interventions: after baseline assessments by experts that classified the wounded into low- and high-risk groups based on the severity of their psychological symptoms, different levels of services were provided.54,62
Indirect survivors
Indirect survivors do not personally experience the disaster but are involved in rescue operations, medical care, or the disposal of dead bodies. Psychosocial responses such as compassion fatigue, burnout, and vicarious traumatic stress symptoms have been documented among medical personnel during the COVID-19 pandemic.63 Eight studies reported interventions for indirect survivors. Four studies involved indirect survivors of earthquakes: two interventions provided psychoeducation and stress management skills to a combined total of 1634 rescuers, medical personnel, and first responders;32,34 one study treated insomnia and grief among caregivers of the wounded;64 and one study provided psychological support and muscle relaxation training to healthcare providers with posttraumatic psychiatric disorders.55 The other four interventions for indirect survivors focused on medical personnel during the COVID-19 pandemic, including diaphragmatic breathing relaxation training,40 short-term Balint groups,41 general psychological support,65 and psychological crisis support.66
Less-exposed survivors
Adverse mental health consequences of disasters and emergencies can also arise in community members, particularly children and adolescents,67 who experienced the disaster or emergency but did not experience serious life-threatening events. An example of survivors with less direct exposure to a disaster who do not directly experience injury include individuals who live in a community at risk of coronavirus infection but did not get infected. Among the 34 reported interventions for the less-exposed survivors, 15 (44%) were focused on children and adolescents. Interventions for children – often conducted in schools by local departments of education21,22,68, 69, 70, 71, 72 – usually combine physical exercise (including playground activities and dancing)69,70,72,73 with counselling, health education, and structured therapies.22,35,43,74 Although older adults are considered particularly vulnerable after disasters, only one of the identified interventions focused on this group;42 it combined group reminiscence therapy with physical exercise to decrease loneliness and improve well-being and resilience among older people after the outbreak of COVID-19.
Types of interventions used in MHPSS intervention studies
Stepped-care intervention models
Stepped-care intervention models systematically provide different levels of services to different cohorts of survivors to ensure that all individuals in a community receive the level of support and treatment they need. Preliminary evidence from large-scale randomized trials shows that stepped care might have higher cost-effectiveness than the uniform application of a single intervention or usual treatment.75 Stepped-care MHPSS intervention models are a relatively new health care innovation in China; six stepped-care interventions for the psychosocial consequences of disasters and emergencies were identified in this review.21,26,50,54,62,65
A recent example is the four-tier ‘COVID-19 Psychological Resilience Model’.50 Tier 1 provided basic mental health education via live media groups; Tier 2 was a 24-hour hotline counselling service that responded to community members’ concerns about the epidemic and provided referrals for psychological emergencies; Tier 3 provided online video psychotherapy and on-site psychological counselling to high-risk individuals; and Tier 4 organized COVID-19-specific training and supervision for mental health service providers. This innovative fourth tier provided training to mental health providers and, more importantly, feedback to program managers who used providers’ feedback to make ongoing updates to the content of the intervention.
Structured psychotherapy and pharmacotherapy
Structured psychotherapy and pharmacotherapy have become an increasingly important component of the overall management of disaster-related psychosocial problems in China. Among the 63 disaster-related MHPSS interventions identified for this review, 22 (35%) interventions used structured psychotherapy, pharmacotherapy, or a combination of both. Five studies used psychosocial interventions based on individual or group CBT administered face-to-face or via the internet.39,45,46,71,76 Different versions of mindfulness training were used in four separate studies to treat stress-related disorders.35,37,38,47 Other frequently mentioned psychotherapies include interpersonal therapy,30,36 cognitive therapy,26,27 and exposure therapy.49,77 Psychopharmacological interventions (including treatment with alprazolam, paroxetine, diazepam and Chinese herbal formulae) were used in four studies.26,51,78,79
Mental health education, psychological counselling, and other supportive interventions
General mental health education, psychological counselling, and emotional support were the most reported interventions. These interventions are primarily administered in general hospitals or schools – locations that lack the psychological and psychiatric professionals needed to provide more well-guided interventions. These minimal-level, community-based interventions are quite helpful in the short term immediately after a disaster or emergency.80 Considering the poor mental health literacy and stigma associated with mental illnesses in China,81 mental health education remains a valuable part of a comprehensive MHPSS response to help people identify their mental health needs and inform them about the different types of available treatment.
Methods used to assess the outcome of MHPSS intervention studies
The main findings of the 63 intervention studies are detailed in Table 1. The efficacy of the interventions was primarily assessed by administering questionnaires to participants; only two studies evaluated interventions based on clinical interviews,32,82 and only one study evaluated the intervention based on the prevalence of a clinical diagnosis.30 Some studies also evaluated the process of the intervention, describing training conditions, acceptability, and participant satisfaction.34,44,46,47,72
Study design
According to the Oxford Centre for Evidence-Based Medicine criteria for classifying study designs,83 the current review included 27 randomised controlled trials (RCT), 30 quasi-experimental studies, 4 case studies (1 case series and 3 case reports), and 2 studies without rigorous quantitative evaluations.
Most of the 27 RCT studies compared before versus after outcomes between an active treatment group and a ‘treatment as usual’ (or ‘no treatment’) group.22,30,32,35,37,39,45,52,66,68,70,72,73 In some trials, ‘enhanced treatment as usual’ (e.g., enhanced by adding a mental health education component) was used as a control condition.23,42,43,73,84 Some studies used wait-listed control groups who received the experimental intervention after the main trial was over.31,38,77 Three studies used a three-arm design32,76,77; for example, a study testing a culturally adapted version of narrative exposure therapy (NET) among earthquake survivors randomly assigned participants to an original NET group, a culturally adapted NET group, or a wait-list control group.77 Some studies gave the control group a mock intervention similar to the experimental intervention.47.85.86 For example, in a trial about the effect of self-affirmation on anxiety, intervention-group participants performed self-affirmation writing exercises while control-group participants did unrelated writing exercises.85 Similarly, in a study aimed at reducing perceived discrimination among people living in Wuhan during the COVID-19 epidemic,86 intervention-group participants received a focused reading- and writing-based intervention while control-group participants did unrelated reading and writing.
The 30 studies that used quasi-experimental designs included 9 non-randomised controlled trials and 21 single-group, pre-post studies. The nine non-randomized controlled trials assessed the efficacy of hotline and face-to-face counselling,56 mental health education plus relaxation training,87 WeChat-based parent training,37 a strength-based online community intervention,44 Chinese calligraphic handwriting training,68 mobile-administered internet CBT,46 art therapy,64 face-to-face CBT,71 and a combination of counselling plus medication intervention for insomnia.78 Most of the pre-post studies assessed the efficacy of psychological counselling, mental health education, or psychological nursing interventions that are not well-structured or guided.24,25,29,51,61,88 Single-group, pre-post designs were also used to assess comprehensive, multi-component interventions; for example, an intervention for 155 medical personnel conducted during the COVID-19 pandemic that included daily mood broadcasts, online themed group chats, and social support-focused group discussions.65
The 4 case studies assessed the efficacy of emotional support plus progressive muscle relaxation therapy,27 interpersonal psychotherapy,36 dialectical behaviour therapy,82 and virtual reality exposure therapy.49
Target outcomes
Our review finds that anxiety, depression, and stress-related disorders are commonly observed following disasters and are frequently the focus of post-disaster MHPSS interventions. Several studies concurrently assessed more than one of these disorders. Among the 63 studies, 29 assessed anxiety (four exclusively studied anxiety48,51,70,85), 24 assessed depression (none exclusively studied depression), and 12 (19%) assessed stress-related disorders (four exclusively studied stress-related disorders31,51,55,68). The severity of anxiety was typically assessed using validated scales such as the Self-rating Anxiety Scale (SAS), the Hamilton Anxiety Scale (HAMA), and the Generalized Anxiety scale-7 (GAD-7). All 29 studies reported a significant decrease in anxiety symptoms after the intervention. The severity of depressive symptoms was usually assessed using the Self-rating Depression Scale (SDS), the Patient Health Questionnaire (PHQ-9), or the Hamilton Rating Scale for Depression (HAMD-17). Among the 24 studies that assessed depression, 21 (88%) reported significant improvement after the intervention. The 12 studies that evaluated stress-related interventions included ten about post-traumatic stress disorder (PTSD), one about acute stress disorder,51 and one about parenting stress.44
General mental health and well-being are also commonly assessed outcomes of disaster-related intervention and prevention programs included in this review. These studies account for 17 (27%) of the 63 identified interventions. In nine of these studies general mental health is assessed using the self-report Symptom Checklist-90-Revised (SCL-90-R), which considers nine mental health domains including anxiety, depression, somatization, and psychotic symptoms. Improvements in different SCL-90-R domains have been reported following the use of different types of interventions.61,69,87 Four COVID-19 interventions reported improvement in ‘well-being’ (their primary outcome) based on the results of self-report scales, including the Psychological Well-Being Scale and the Spirituality Index of Well-Being scale.35,42,43,89
Six of the 63 intervention studies reported the efficacy of interventions for treating sleep problems.40,57,73,74,78,90 A non-randomised trial that compared psychotherapy alone, medication alone, and combined psychotherapy and medication to treat insomnia after the earthquake found some improvement in sleep time with both psychotherapy and medication but greater improvement when the two treatments were combined.78
Psychological resilience, defined as the process of adapting well in the face of adversity, trauma, tragedy, threats, or other significant sources of stress,91 has recently been a target of a growing number of MHPSS interventions. Six of the 63 interventions considered evaluated the efficacy of interventions designed to promote resilience.42,52,59,73,76,89 A short-term CBT group intervention was more effective than a general supportive intervention in enhancing the psychological resilience of adolescent earthquake survivors.76 However, another resilience-focused intervention that combined group reminiscence therapy and physical exercise for adolescents found no significant effects on resilience.52
Our review also found that some individuals exposed to disasters or emergencies develop problematic coping behaviours, negatively affecting physical and mental health. One 30-minute intervention focused on reducing inappropriate alcohol use after the Wenchuan earthquake23 proved effective in reducing alcohol use for at least three months. Another study reported the efficacy of a logotherapy-based mindfulness intervention on internet addiction among adolescents during the COVID-19 pandemic.37
Quality of evidence provided in reports of MHPSS interventions
The results of using the GRADE criteria to assess the quality of evidence about the effectiveness of the 63 interventions are shown in Supplementary Table 4: 9 studies were classified as high quality, 13 as moderate quality, 27 as low quality, and 12 as very low quality (2 studies did not assess the effectiveness of the intervention). Among the 27 RCTs, 9 were classified as high quality, but the remaining 18 had a serious or very serious risk of bias (detailed below). Among the 34 non-RCT studies, 6 were classified as moderate quality, but the remaining 28 had a serious risk of bias and (for the studies classified as very low quality) serious or very serious indirectness (i.e., the sample or intervention was not directly relevant to the target group or intervention of interest).
Risk of bias for each individual study was evaluated as suggested by the GRADE guideline92 (see Supplementary Table 5 and 6). For RCT studies, the most common source of risk of bias comes from unspecified randomisation and blinding procedures, and the lack of adherence to intention-to-treat (ITT) analysis principles. Only 8 of the 27 RCT studies reported adequate randomisation of participants. Due to the nature of psychotherapy, double-blind design is usually unfeasible, only two studies used a double-blind design while seven studies used a single-blind design or blinded the outcome assessments. Less than half of the RCTs followed the ITT principle for analysis. For non-RCT trials, the major concern is lack of follow-up assessments after the posttests. For MHPSS interventions, follow-up studies are critical to determine the long-time effect of the treatment in preventing relapses of psychiatric symptoms. Only 2 of the 34 studies reported follow-up assessments. Another issue is the absence of control or comparison groups: 26 of the 34 studies do not have comparison conditions. Other sources of bias include limited sample size, unvalidated outcome measures, and inappropriate data analysis.
Governmental policies
National-level policies to address the psychosocial consequences of disasters and emergencies have been developed, implemented, and updated as experience with providing such services has increased. The first such policy was the general guidelines about post-disaster MHPSS provided by the National Health Commission in 200493; these guidelines recommended 1) developing post-disaster mental health rescue contingency plans, 2) assessing mental health needs, 3) identifying target populations, and 4) providing MHPSS services to reduce the prevalence and severity of mental disorders. These initial guidelines provided few details about how to conduct the recommended assessments and interventions. After the 2008 Wenchuan earthquake, more details about the recommended MHPSS interventions were included in governmental plans for rebuilding after disasters (e.g., after the mudslide in Gansu and earthquakes in Qinghai, Yunnan, and Sichuan province)94, 95, 96, 97, 98 and in governmental methods of managing public health emergencies (e.g., during the H1N1 epidemic and COVID-19 pandemic).99,100 Most government-initiated interventions included 1) establishing mental rehabilitation centres based at local medical institutions,96, 97, 98 2) organization of professional therapists to conduct MHPSS interventions,94,97,98 and 3) the treatment of psychological trauma.96, 97, 98,100
Over time the recommendations became more specific, including 1) providing psychological assessment, treatment and follow-up services to frontline workers101; 2) providing training for teachers and medical personnel to enhance their ability to identify mental disorders and to make appropriate referrals to psychiatrists or certified psychotherapists101; 3) providing non-professional psychological services supervised by mental health professionals102; and 4) establishing peer-support networks among affected communities.103 To support this effort, the Chinese CDC developed technical guidelines for providing disaster-related MHPSS and promulgated these guidelines to mental health workers and mental health institutions.101,104
MHPSS usually constitute a minor part of crisis intervention policies, but two policies specifically targeted mental health outcomes.102,105 The 2010 psychological assistance program for earthquake survivors promulgated by the National Health Commission102 advocated the provision of mental health education and psychological counselling supervised by hospital-based mental health professionals and recommended formal assessment of the program's efficacy. Another government-supported program, the ‘An Xin’ (‘Stay Relieved’ in English) program administered by the Chinese Psychological Society during the COVID-19 epidemic,105 included 1) online lectures with over 400,000 participants; 2) free provision of online mental health assessment, counselling, and other supportive interventions to over 50,000 people; and 3) community-based service stations to deliver standard face-to-face mental health services.
None of the government policies identified included specific measures to evaluate the efficacy of the proposed intervention(s) or the fidelity of the implementation of the policy.
Discussion
This scoping review provides the first systematic summary of China's mental health and psychosocial (MHPSS) responses after large-scale adverse events, including natural disasters and public health emergencies. The review is based on 63 research reports about MHPSS interventions conducted in China and 14 related policy documents published by government agencies in mainland China.
Most disaster-related MHPSS interventions in China reported in the scientific literature were developed and documented following the 2008 Wenchuan earthquake. All disaster-related MHPSS interventions focused on natural disasters, predominantly earthquakes; there were no documented MHPSS interventions that addressed the consequences of human-made disasters such as fires or explosions. The first documented MHPSS intervention related to a public health emergency occurred during the nationwide 2003 SARS epidemic; several recent reports have focused on MHPSS interventions related to the ongoing COVID-19 pandemic that started in late 2019. Reported interventions include general support, psychotherapies, and pharmacological treatments focusing on different target groups. The outcome assessed in most of the studies was an improvement in overall mental health or in the severity of anxiety, depressive symptoms, or stress-related symptoms, and few interventions in China have been developed to address substance use disorders in disaster-exposed populations. Both quantitative and qualitative methodologies were used to assess the efficacy of the interventions; in almost all cases, the interventions were deemed effective. However, based on the WHO GRADE criteria, the quality of the evidence supporting the efficacy of these interventions was considered high in only 9 of the 63 studies; the remaining studies had a substantial risk of bias that undermined confidence in the validity of their results.
Given the projected rapid increase in the frequency, scope, and severity of disasters and public health crises, it is essential that China work with all other countries to improve the methods for developing, implementing, and evaluating post-crisis MHPSS interventions. This review highlights several important issues that need to be considered as we work towards that goal.
The need for long-term interventions and regular follow-up
After experiencing catastrophic events, individuals demonstrate different patterns of psychological responses.91 While most individuals show resilience and experience few or no symptoms, some individuals experience aggravated psychiatric symptoms at different time points after the event: including relapse or exacerbation of pre-existing mental disorders, development of new-onset subthreshold symptoms, and the onset of new, full-criteria psychiatric disorders. Psychological distress experienced in the acute phase after an event usually fades over time without requiring treatment, but in some cases, such symptoms persist and intensify to the point of meeting the criteria of a psychiatric disorder, resulting in chronic distress and substantial functional impairment. Short-term MHPSS interventions undertaken soon after the index event are considered a cost-effective way to prevent chronic symptoms.60 However, individuals who do not display any distress in the short term but subsequently display delayed symptoms long after the event are often neglected. A comprehensive meta-analysis reported that the mean prevalence of delayed-onset mental disorders after traumatic events ranged from 6.4% to 17.6%, and the prevalence for delayed-onset general distress was 5.6%.106 Currently, no method exists to reliably identify which individuals exposed to catastrophic events will experience delayed-onset psychological problems. Moreover, it does not appear that short-term interventions given soon after the crisis can prevent the onset of delayed psychosocial impairment.107
The Chinese Psychological Society recommends that MHPSS services continue for at least 20 years after major disasters,13 but this recommendation has not, as yet, been adopted – partly because post-disaster MHPSS research has only recently emerged in China. The longest follow-up intervention identified was a 9-year intervention among adolescent survivors of the 2010 Yushu earthquake that provided nine 90-minute sessions on strategies to improve academic achievement, self-confidence, coping, interpersonal competence, and earthquake preparedness.52 Another relatively long follow-up intervention was a 6-year, school-based intervention following an earthquake in Taiwan that established a specific centre in the school which provided regular mental health assessments, group therapy, and counselling on request.21 All other post-crisis psychosocial interventions identified were conducted within 3.5 years after the crisis. More long-term follow-up studies are needed to identify the best methods for recognizing individuals with different symptom trajectories after the crisis, including individuals who are likely to experience relapses of pre-existing mental disorders, new-onset subthreshold or full-criteria mental disorders, and chronic or delayed-onset psychological symptoms. Different psychological and pharmacological intervention plans can then be developed to address the varying needs of these different post-disaster cohorts. Until China produces its own culture-specific research in this area, it can deal with the immediate need for relevant policies and projects by adapting long-term post-disaster MHPSS interventions developed in Western countries, such as the psychotherapy program provided to first responders at the 2001 World Trade Center attack in New York City that has continued for 20 years.108
An intervention can only be considered effective when its long-term efficacy is demonstrated following treatment; simply assessing the outcome at the end of the treatment is not sufficient. Follow-up surveys after the posttest of the intervention are critical in the evaluation of intervention efficacy and implementation. Only 10 of the 63 included interventions (16%) in our review included post-intervention follow-up assessments. The longest follow-up assessment was three years after the intervention;71 all other follow-up assessments were conducted between two weeks and three months post-intervention.21,30, 31, 32,44,47,55,77,85 Future studies of post-disaster MHPSS interventions should include sufficiently large samples that are followed up at appropriate time frames to provide robust evidence of the long-term efficacy of the interventions. Interventions that have positive post-test effects that fade during follow-up should either be extended in duration or expanded to include periodic booster sessions and then reassessed.
Cultural-specific interventions and outcomes
Cultural differences should be accounted for when providing psychosocial interventions, especially when adapting interventions developed in Western cultures. A network meta-analysis comparing the efficacy of different treatment modalities for common mental health problems reported in 235 clinical trials conducted in China109 found that indigenous therapies (e.g., Naikan therapy,110 sand play, and Morita therapy111) and humanistic–experiential therapies (e.g., art therapies) which are closer to the Chinese understanding of psychopathology are more effective than cognitive–psychoeducational therapies such as CBT adapted from the West. One study during the COVID-19 pandemic reported that mental health services using Western models were less acceptable to target participants16; feedback from first-line mental health workers indicated that many patients in shelter hospitals during COVID-19 were unwilling to receive mental health assessments or evidence-based mental health interventions, but they were willing to engage in generic group activities such as square dancing or other aerobic exercises. This problem can potentially be addressed by culturally adapting Western interventions or by developing cultural-specific interventions, which may enhance acceptability and effectiveness.112 But there have been few well-documented reports of cultural adaptations for psychosocial interventions after disasters or emergencies in China. The only study identified in this review involved comparing a culturally-adapted version of narrative exposure therapy (NET) for earthquake survivors to the directly translated original version of NET77; the briefer, adapted version was better at reducing PTSD-related symptoms than the original version.
Few Chinese culture-specific MHPSS interventions have been employed in post-disaster situations. One study reported that Chinese calligraphic handwriting therapy was effective in managing students’ posttraumatic stress reactions after an earthquake.68 A randomised control study found that Qigong – an exercise based on the principles of traditional Chinese medicine – was more effective than psychological counselling in reducing depression symptoms.84 A traditional Chinese medicine herbal formula was more effective than a placebo in the treatment of posttraumatic symptoms in survivors of the Wenchuan earthquake.79 More work is needed to develop and assess culture-specific interventions in China and to adapt these methods when they are provided to ethnic minority communities within China – such as the inclusion of religious support provided by Tibetan lamas in the intervention provided to manage acute stress reactions among Tibetan survivors of the 2010 Yushu earthquake.51
Sociocultural factors should also be considered when determining the appropriate target outcome(s) of interventions. All identified interventions targeted psychological disorders or constructs based on Western psychological theories that were assessed using instruments developed and validated in Western populations. Relying on these constructs and evaluation methods raises two fundamental problems: 1) Are these psychosocial constructs validated in the Chinese cultural context?113 For example, psychological resilience was the primary outcome in several post-disaster interventions identified in China. However, the conceptualization and assessment of resilience are heavily influenced by Western cultural norms,114 so its use as an outcome measure in non-Western cultures should be carefully reconsidered; if necessary, an alternative, culture-specific definition and assessment of the construct should be developed. 2) Are there any Chinese cultural-specific post-crisis mental health conditions that are unrecognized and untreated?115 Psychological factors are closely associated with various physical symptoms and disorders in traditional Chinese medicine, so many Chinese individuals manifest psychological distress as physical – not psychological – problems.116 There are, as yet, no studies related to the assessment and treatment of these types of somaticized symptoms in victims of disasters and public health emergencies.
Digital mental health interventions
Digital mental health interventions involve using digital technology in mental health care delivery, such as telemental health, smartphone app-based or web-based psychological interventions.117 Traditional telemental health services (e.g., psychological support hotlines) are widely available in urban China, but use of novel types of digital mental health services in China has only recently become popular during the COVID-19 pandemic, primarily due to the greater difficulty of accessing and providing face-to-face services. Before 2019, only one post-disaster digital mental health intervention was reported: a web-based intervention for individuals exposed to the Wenchuan earthquake.32 In contrast, six digital mental health interventions that focus on the psychological effects of COVID-19 have already been reported. These include CBT, mindfulness training, and peer-to-peer live-streaming interventions delivered via mobile phones, computers, or web platforms.38,44, 45, 46, 47, 48,118 In combination, these reports show the feasibility and effectiveness of digital MHPSS interventions in reducing distress, depression, and anxiety experienced by different cohorts of community members after a major crisis.
There are two key reasons digital platforms should be considered an essential vehicle for delivering MHPSS interventions after crises. First, the level of psychological services needed in locations affected by disasters such as an earthquake far exceeds the capacity of available mental health professionals, a situation that is more acute in countries like China, where most locations have few mental health providers (2·19 registered psychiatrists and 5·51 psychiatric nurses for per 100,000 population).119 Second, service providers who deliver needed interventions are often overwhelmed by the number of survivors who need help, leading to suboptimal service delivery and clinician burnout.120 China's current solution to this problem is to send out-of-province psychological rescue teams to affected areas to provide on-site treatments, but these rescue teams are challenging to coordinate and can usually only stay for a relatively short period. Once internet access is available in the affected area (which generally happens quickly), professionals from around the country can be recruited easily. Digital services are a much more efficient method for providing the quantity and quality of psychological support services needed. Second, the stigma associated with mental disorders is another barrier to providing psychosocial services after a crisis, particularly in locations where community members have limited knowledge about mental health issues. As is true in other countries, stigma is associated with delayed treatment-seeking and poor treatment adherence in China.121 A study among Chinese students who experienced a mental disorder following exposure to a natural disaster reported a low intention of seeking help mainly because of stigma.122 The provision of digital mental health services – which can be completely confidential and does not involve a loss of face (i.e., feeling embarrassed or humiliated due to perceived loss of others’ respect) associated with visiting a psychiatric clinic or talking face-to-face with a clinician – can help reduce the barriers to care-seeking.
The rapid development of digital mental health interventions in China is an encouraging trend. Still, more work is needed to assess the efficacy and effectiveness of these interventions and to integrate them with the traditional face-to-face services that are still required to manage moderate to severe mental disorders.
Implementation science
Over time the proportion of crisis-related interventions that use randomised controlled trials to assess the efficacy of interventions has increased. Overall, this represents an increase in the confidence that potential users can have in the reported results, but it is essential to understand that efficacy (results in a tightly controlled study) does not necessarily ensure that the intervention works in the real world.123 Implementation science is the scientific study of methods to promote the integration of research findings and other evidence-based practices into routine practice124; it aims to provide information on the extent to which an intervention has been scaled up from a laboratory finding (or specific RCTs) to benefit people in the real world and to develop strategies for improving the quality and effectiveness of health services. The importance of using implementation science to scale-up psychological treatments is well-recognized;125 however, very few studies have reported on the process of implementing post-crisis psychosocial interventions in China. Only five of the 63 identified interventions considered the acceptability of the intervention to participants or their satisfaction with the provided services.34,44,46,47,72 Only one of the 63 studies conducted a formal, structured assessment of the implementation of the intervention;34 this study used the Training Relevance, Use, and Satisfaction Scale and the Training Evaluation Form to assess the Implementation of a psychoeducation program for medical personnel and first responders of the Wenchuan earthquake. The lack of systematic assessment of the implementation of post-disaster MHPSS interventions in China seriously undermines the potential value of such studies. Because of the absence of detailed data about the implementation of these interventions, the likely effectiveness of the employed strategies when used in other locations, with different population cohorts, or at other times is unknown.
Remaining gaps
The earliest reported MHPSS intervention in China was for the 1999 earthquake in Taiwan and the 2003 SARS epidemic. There has been substantial improvement in the coordination and comprehensiveness of such efforts over the subsequent two decades, but critical gaps remain. The first and potentially most crucial step would be to integrate MHPSS responses into the current national and local emergency response system coordinated by the Ministry of Emergency Management. A wide range of unqualified agencies in China provide psychiatric and psychosocial services, so failure to effectively coordinate these services during a crisis can lead to major problems. For example, many psychological rescue workers who provided services during the 2008 Wenchuan earthquake reported that they had felt ill-equipped to provide assistance due to the lack of relevant training and expertise. Moreover, they reported that inappropriate interventions were often delivered to those who did not need treatment, causing secondary trauma.12 If the Ministry of Emergency Management managed all MHPSS interventions during a major crisis, it could coordinate, provide training, and organize human resources effectively, ensuring that everyone who responds to the emergency is clear about their role and able to fulfil it. The ministry would also then be able to ensure that the provision of baseline assessments, interventions, and follow-up treatments and assessments becomes an integral part of the comprehensive emergency response to the crisis.
Another missing component in the current psychosocial crisis intervention model in China is the supervision of mental health providers. The need for supervision was mentioned in passing in 2 of the 14 government policy documents identified,102,105 but only one of the 63 interventions considered in this review mentioned the supervision of or support for service providers.50 During and after emergencies and disasters, mental health care providers and first responders may experience secondary trauma, which can undermine their ability to provide services and, thus, indirectly influence the wellbeing of the survivors.126 All MHPSS interventions in crisis settings must include structured supervision, psychosocial support, and periodic evaluation of the frontline service providers; this is essential to prevent burnout and other psychological problems among service providers and, thus, ensure they can provide high-quality services.
There are also several gaps in the scientific rigour of crisis intervention studies in China that need to be addressed. Among the 63 identified interventions, 57 (90%) were either RCTs or quasi-randomised studies, but only 9 of these case-control studies provided definitive answers about the efficacy of the assessed intervention. Too often the quality of the evidence was marred by failure to control different types of biases or other methodological issues. Most MHPSS interventions in emergency settings lack a comprehensive monitoring and evaluation framework that addresses different stages of the intervention. The primary outcomes for clinical trials are often not clearly defined, and the assessment of results is usually based on self-report scales. Samples identified in some studies are either too small or too unrepresentative to arrive at definitive conclusions about the efficacy of the intervention. The timing and method of assessing the outcome are often unsuited to the stated goal of the study. Randomization and blinding methods are not mentioned clearly in RCT studies. These methodological issues threaten the validity of study results, leaving other researchers and policy makers wondering whether the interventions worked as reported and whether they should be scaled up, thereby slowing the development of effective evidenced-based MHPSS crisis interventions. Increased attention to these methodological issues is needed to improve the scientific quality of crisis-related intervention research in China. Another threat to the validity of these disaster studies is the failure to distinguish pre-existing and new-onset symptoms after disaster exposure. Most studies in this review assumed that reported mental disorder symptoms were direct consequences of the disaster or emergency. However, as shown in one included study, the effectiveness of an intervention on pre-existing and new-onset symptoms can be different.81 More clarification regarding participant inclusion criteria or retrospective assessment of pre-disaster symptoms by interview or review of medical records is critical to address treatment effectiveness in future post-disaster intervention studies.
The overall capacity of mental health services in China is increasing rapidly. However, the persistent regional imbalance in the quality and coverage of these services is a serious problem that affects all components of the mental health care system, including the acute and long-term provision of disaster-related intervention services. High-quality, comprehensive services are available in major urban areas, while mental health services in many rural communities – particularly those in the western part of the country – are limited and of low quality. The equitable distribution of mental health resources is an essential precursor to developing an effective national strategy for reducing the adverse psychosocial effects of disasters and public health emergencies. During the COVID-19 pandemic, China's policy makers were determined to build a full-spectrum mental health service network based on the current mental health system as an important component of the overall response to crises. However, it remains unclear how best to coordinate the efforts between the Ministry of Emergency Management and the Ministry of Health. Clearly, building sustainable and collaborative partnerships between these departments is critical. Identifying champions (i.e., key persons responsible for coordinating post-disaster service projects) in the mental health system could be a particularly effective strategy to increase the commitment of the Ministry of Health and facilitate regular communication with the Ministry of Emergency Management.
Lessons learned from China
Despite the identified gaps, several take-home messages based on China's experiences in managing disasters may be of value to other countries, particularly other low- and middle-income countries that experience frequent natural or man-made disasters or public health emergencies. In addition, international collaboration and sharing of best practices and methods could help develop international guidelines or frameworks for MHPSS responses to disasters (e.g., the Sendai framework127) and speed up the maturation of the underlying science.
One of the most impressive components of China's response to disasters and emergencies is the rapid national mobilization of the workforce needed to provide psychiatric and psychosocial services to affected communities. For example, after the 2008 earthquake in Sichuan Province, the central government immediately paired high-resource provinces and municipalities with specific earthquake-affected counties in Sichuan. It made the high-resource provinces responsible for providing the matched county in Sichuan with material supplies, emergency medical services, and psychiatric/psychosocial services; psychiatric teams were on the ground in Sichuan within days of the disaster.128 Based on the experience of the 2008 earthquake, the national emergency response network was streamlined and strengthened. When COVID-19 broke out in Hubei Province in early 2020, it was relatively easy to rapidly deploy mental health professionals trained in crisis response techniques from provinces around the country to provide MHPSS interventions at paired hospitals in different cities throughout Hubei Province. China's method of training crisis intervention professionals in all locations around the country, immediately pairing communities after a major disaster or crisis occurs, and assigning trained professionals from the unaffected communities for short-term (3-6 month) secondments to the paired-affected communities has proven an effective strategy for rapidly mobilizing the mental health professionals needed at the time of disasters and large-scale public health emergencies.
Many crisis-related intervention programs in China are not only aimed at reducing symptoms of mental disorders but also focus on building survivors’ resilience to psychological trauma. Several of the interventions identified in this review included improving resilience as one of the key outcome measures assessed: an online strength-oriented group intervention,89 a culturally adapted resilience intervention,52 an intervention that established social support networks among communities,104 and a resource-linking intervention that established referral networks.59 Resilience-oriented interventions can prevent chronic symptoms, functional impairments, and the development of adverse psychosocial responses to subsequent crises in individuals living in disaster-prone locations. Based on the experience in China, we recommend that the assessment of adverse psychosocial consequences of disasters should include a cultural-sensitive evaluation of participants’ resilience.
Finally, China's efforts to effectively dispense limited personnel resources during a crisis by using multi-level, stepped-care intervention models merit consideration in other jurisdictions with limited mental health personnel. Within one month of the first reported COVID-19 case in China, the central government released a four-level mental health support plan for managing the psychosocial effects of the pandemic. Four different populations with varying levels of mental health needs were defined in the model: hospitalized patients and frontline healthcare workers; quarantined patients; individuals related to identified patients; and the general public. Detailed population-specific intervention strategies were provided in the plan: 1) rescue teams comprising psychiatrists, psychologists, and liaison officers provided psychological crisis intervention and consultation-liaison psychiatry services for COVID-19 inpatients and frontline healthcare workers; 2) telephone- or online-based services assessed the psychological status of quarantined patients and provided psychosocial support if needed; 3) teams of assistant psychologists provided 24/7 hotline or online consulting services for patients’ relatives; and 4) social welfare services and mental health experts provided mental health education and psychosocial support to the general public. Other post-crisis interventions identified in this review provided small-scale stepped-care mental health services to specific populations, including medical personnel, children, and adolescents. Such models require that all potential participants be categorized into different risk groups prior to providing services. This method of triaging the target population is a relatively easy way to improve the efficiency (and, presumably, cost-effectiveness) of psychosocial interventions during major crises.
Limitations
Some potential sources of information about psychosocial responses to disasters in China were not included in the current report. 1) Policy reports from provincial- or city-level governments from the areas affected by disasters or emergencies should provide information on the implementation of community-level psychosocial interventions, but few relevant official documents were retrievable, so we limited our search for relevant policy documents to national-level departments. 2) Some mental health and psychosocial support services provided after disasters are provided by non-government organizations, such as the Hong Kong Red Cross (which provides psychological first aid to survivors of air crashes and other disasters) and the Chinese National Alliance of Psychological Assistance (which provides services to survivors of disasters). However, there is little detailed information about these services available, so they were not included in this review. 3) The COVID-19 pandemic is an ongoing public health crisis that started in late 2019. All of the 28 COVID-19-related MHPSS interventions included in this review were published before August 13, 2021; more recent publications are not included.
Conclusions
This scoping review examines how MHPSS systems in China evolved over the last 20 years in response to the psychosocial burden caused by major crises such as disasters and public health emergencies. Before the 2008 Wenchuan earthquake, China's experience in post-crisis psychosocial support was limited. The Wenchuan earthquake dramatically highlighted the urgent need for better coordinated, more comprehensive, evidence-based MHPSS interventions. The central government subsequently provided the resources and leadership needed to streamline the provision of mental health and psychosocial services after disasters. Since then, many interventions have been developed to prevent or decrease the severity of psychological problems caused by disasters. Innovative interventions have targeted a broader range of psychosocial outcomes. Randomised controlled trials are being used to assess the efficacy of these interventions rigorously, but methodological limitations remain, and there are few implementation science studies that evaluate their effectiveness. This accumulating experience has helped prepare China to address the psychosocial challenges posed by the COVID-19 pandemic: trained mental health crisis teams around the country can closely monitor the psychosocial consequences of the pandemic using internet-based surveillance and provide stepped-care interventions to patients, front-line health care providers, and the general public. Despite remaining gaps in the quality, comprehensiveness, equity, and long-term follow-up of disaster-related psychosocial services, China has exhibited its determination and its willingness to mobilize the resources needed to improve public mental health after large-scale disasters and emergencies.
Contributors
GL, WS, MRP, and BJH conceived and conceptualized the study design. GL conducted searches. GL and WS carried out the study selection. XG, XS, and XF conducted data charting under the guidance of GL and WS. GL dealt with the disagreements in data charting. GL carried out the quality assessment. GL wrote the first draft which was reviewed by WS, DL, CL, MRP, and BJH. All study authors approved the final paper.
Funding
Funding support is provided by the Center for Global Health Equity, NYU Shanghai.
Declaration of interests
Dr Wei Shi and Dr Chunbo Li report a grant from the Fundamental Research Funds for the Central Universities. The authors declare no conflicts of interest.
Acknowledgements
This project was completed as part of the preparatory work for the Lancet Commission of Mental Health in China, co-chaired by Professors Shuiyuan Xiao, M.D. and Michael R. Phillips, M.D. We are grateful to the coordinator of the scoping reviews for the Commission, Marlys Bueber M.N., for her editorial contributions to this work.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanwpc.2022.100580.
Appendix. Supplementary materials
References
- 1.Udomratn P. Mental health and the psychosocial consequences of natural disasters in Asia. Int Rev Psychiatry. 2008;20(5):441–444. doi: 10.1080/09540260802397487. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Summary of Probable SARS Cases with Onset of Illness from 1 November 2002 to 31 July 2003. Accessed 18 May 2022. https://www.who.int/publications/m/item/summary-of-probable-sars-cases-with-onset-of-illness-from-1-november-2002-to-31-july-2003.
- 3.Center for Systems Science and Engineering at Johns Hopkins University. COVID-19 Dashboard. Accessed 18 May 2022. https://www.arcgis.com/apps/dashboards/bda7594740fd40299423467b48e9ecf6.
- 4.Guo JC, Tian ZL, Wang XD, et al. Post-traumatic stress disorder after typhoon disaster and its correlation with platelet 5-HT concentrations. Asian Pac J Trop Med. 2016;9(9):913–915. doi: 10.1016/j.apjtm.2016.07.011. [DOI] [PubMed] [Google Scholar]
- 5.Chen H, Chen Y, Au M, et al. The presence of post-traumatic stress disorder symptoms in earthquake survivors one month after a mudslide in southwest China. Nurs Health Sci. 2014;16(1):39–45. doi: 10.1111/nhs.12127. [DOI] [PubMed] [Google Scholar]
- 6.Feng S, Tan H, Benjamin A, et al. Social support and posttraumatic stress disorder among flood victims in Hunan, China. Ann Epidemiol. 2007;17(10):827–833. doi: 10.1016/j.annepidem.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 7.Liang Y, Cheng J, Ruzek JI, Liu Z. Posttraumatic stress disorder following the 2008 Wenchuan earthquake: a 10-year systematic review among highly exposed populations in China. J Affect Disord. 2019;243:327–339. doi: 10.1016/j.jad.2018.09.047. [DOI] [PubMed] [Google Scholar]
- 8.Rogers JP, Chesney E, Oliver D, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020;7(7):611–627. doi: 10.1016/S2215-0366(20)30203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhou Y, Sun Z, Wang Y, et al. The prevalence of PTSS under the influence of public health emergencies in last two decades: a systematic review and meta-analysis. Clin Psychol Rev. 2021;83 doi: 10.1016/j.cpr.2020.101938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bareeqa SB, Ahmed SI, Samar SS, et al. Prevalence of depression, anxiety and stress in China during COVID-19 pandemic: a systematic review with meta-analysis. Int J Psychiatry Med. 2021;56(4):210–227. doi: 10.1177/0091217420978005. [DOI] [PubMed] [Google Scholar]
- 11.Bonanno GA, Brewin CR, Kaniasty K, Greca AM La. Weighing the costs of disaster: consequences, risks, and resilience in individuals, families, and communities. Psychol Sci Public Interest. 2010;11:1–49. doi: 10.1177/1529100610387086. [DOI] [PubMed] [Google Scholar]
- 12.Higgins LT, Xiang G, Song Z. The development of psychological intervention after disaster in China. Asia Pac J Counsel Psychother. 2010;1(1):77–86. [Google Scholar]
- 13.Chinese Psychological Society. http://www.cpsbeijing.org/. Accessed 1 February 2022.
- 14.Xian-peng M, Jun Y, Xue-li S, et al. Investigation and analysis on psychological assistance status among health system after Wenchuan earthquake. Chin J Health Educ. 2012;28(11):916–919. (in Chinese) [Google Scholar]
- 15.Joint Prevention and Control Mechanism of the State Council . 2020. Guidelines of Psychological Crisis Intervention for Coronavirus Disease.http://www.nhc.gov.cn/jkj/s3577/202001/6adc08b966594253b2b791be5c3b9467.shtml Accessed 27 January 2020. [Google Scholar]
- 16.Ju YM, Zhang Y, Wang XP, Li WH, Ng RMK, Li LJ. China's mental health support in response to COVID-19: progression, challenges and reflection. Global Health. 2020;16(1):102. doi: 10.1186/s12992-020-00634-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The Inter-Agency Standing Committee . 2022. IASC Strategic Priorities 2022-2023. Published.https://interagencystandingcommittee.org/inter-agency-standing-committee/iasc-strategic-priorities-2022-2023-0 Accessed 1 February 2022. [Google Scholar]
- 18.Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 19.Peking University . 9th ed. Peking University Press; 2020. Catalogue of Chinese Core Periodicals in Library of Peking University. [Google Scholar]
- 20.Brozek JL, Akl EA, Alonso-Coello P, et al. Grading quality of evidence and strength of recommendations in clinical practice guidelines. Part 1 of 3. An overview of the GRADE approach and grading quality of evidence about interventions. Allergy. 2009;64(5):669–677. doi: 10.1111/j.1398-9995.2009.01973.x. [DOI] [PubMed] [Google Scholar]
- 21.Chao CC, Wu YY, Shiau RJ, Lee LW, Jiang HJ, Chang MY. School-based mental rehabilitation work after Taiwan 921 earthquake. J Psychol Chin Soc. 2009;10(2):107–130. (in Chinese) [Google Scholar]
- 22.Shen YJ. Short-term group play therapy with Chinese earthquake victims: effects on anxiety, depression and adjustment. Int J Play Ther. 2002;11(1):43–63. [Google Scholar]
- 23.Ruan XL, Wang WW, Ali R, et al. Feasibility of studying a brief intervention to help Chinese villagers with problem alcohol use after an earthquake. Alcohol Alcohol. 2017;52(4):472–476. doi: 10.1093/alcalc/agx014. [DOI] [PubMed] [Google Scholar]
- 24.Zhang QL, Wang S, Zhang Y, Meng F. The effect of refined nursing intervention on patients undergoing maintenance hemodialysis in the hemodialysis center during the COVID-19 epidemic. BMC Nurs. 2021;20(1):66. doi: 10.1186/s12912-021-00584-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xie X, Su Y, Yao C. Comprehensive psychological intervention on fever patients in the epidemic period of severe acute respiratory syndrome. Clin Focus. 2004;19(4):196–198. (in Chinese) [Google Scholar]
- 26.Tian G, Chen Z, Gan J. Exploration of pattern of psychological intervention on victims of earthquake in general hospital. Med Soc. 2010;23(5):84–86. (in Chinese) [Google Scholar]
- 27.Hu M, Chen J. A case report of psychological crisis intervention for a wounded and bereaved earthquake victim. Chin Gen Pract. 2010;13(S1):47–48. (in Chinese) [Google Scholar]
- 28.Yao L, Wu W, Zhang Y. Access on psychological health status of 45 earthquake wounded persons and nursing care. Chin J Nurs. 2008;43(12):1067–1069. (in Chinese) [Google Scholar]
- 29.Xiang M, Wang G, Huang M, Qing Y, Tian R. Stress reaction of inpatients injured in the earthquake and its therapeutic intervention. Chin J Phys Med Rehabil. 2008;30(11):769–772. (in Chinese) [Google Scholar]
- 30.Jiang RF, Tong HQ, Delucchi KL, Neylan TC, Shi Q, Meffert SM. Interpersonal psychotherapy versus treatment as usual for PTSD and depression among Sichuan earthquake survivors: a randomized clinical trial. Confl Health. 2014;8:14. doi: 10.1186/1752-1505-8-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang Z, Wang J, Maercker A. Chinese my trauma recovery, a web-based intervention for traumatized persons in two parallel samples: randomized controlled trial. J Med Internet Res. 2013;15(9):e213. doi: 10.2196/jmir.2690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu SJ, Zhu X, Zhang YL, et al. A new psychological intervention: “512 Psychological Intervention Model” used for military rescuers in Wenchuan Earthquake in China. Soc Psychiatry Psychiatr Epidemiol. 2012;47(7):1111–1119. doi: 10.1007/s00127-011-0416-2. [DOI] [PubMed] [Google Scholar]
- 33.Mitchell JT. When disaster strikes: the critical incident stress debriefing process. J Emerg Nurs. 1983;8(1):36–39. [PubMed] [Google Scholar]
- 34.Leitch L, Miller-Karas E. A case for using biologically-based mental health intervention in post-earthquake china: evaluation of training in the trauma resiliency model. Int J Emerg Ment Health. 2009;11(4):221–233. [PubMed] [Google Scholar]
- 35.Chen J, Sang G, Zhang Y, Jiang A. Intervention effect of the integration model on negative emotions of adolescents during the outbreak of corona virus disease 2019. Psychiatr Danub. 2021;33(1):86–94. doi: 10.24869/psyd.2021.86. [DOI] [PubMed] [Google Scholar]
- 36.Hu CC, Huang JW, Wei N, et al. Interpersonal psychotherapy-based psychological intervention for patient suffering from COVID-19: a case report. World J Clin Cases. 2020;8(23):6064–6070. doi: 10.12998/wjcc.v8.i23.6064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu X, Jiang JG, Zhang YL. Effects of logotherapy-based mindfulness intervention on internet addiction among adolescents during the COVID-19 pandemic. Iran J Public Health. 2021;50(4):789–797. doi: 10.18502/ijph.v50i4.6005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang H, Zhang AA, Liu CB, Xiao J, Wang KP. A brief online mindfulness-based group intervention for psychological distress among Chinese residents during COVID-19: a pilot randomized controlled trial. Mindfulness. 2021;12(6):1502–1512. doi: 10.1007/s12671-021-01618-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li JZ, Li XC, Jiang J, et al. The effect of cognitive behavioral therapy on depression, anxiety, and stress in patients with COVID-19: a randomized controlled trial. Front Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.580827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu Y, Jiang TT, Shi TY, et al. The effectiveness of diaphragmatic breathing relaxation training for improving sleep quality among nursing staff during the COVID-19 outbreak: a before and after study. Sleep Med. 2021;78:8–14. doi: 10.1016/j.sleep.2020.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yang C, Zhou B, Wang J, Pan S. The effect of a short-term Balint group on the communication ability and self-efficacy of pre-examination and triage nurses during COVID-19. J Clin Nurs. 2021;30:93–100. doi: 10.1111/jocn.15489. [DOI] [PubMed] [Google Scholar]
- 42.Ren YJ, Tang R, Sun H, Li X. Intervention effect of group reminiscence therapy in combination with physical exercise in improving spiritual well-being of the elderly. Iran J Public Health. 2021;50(3):531–539. doi: 10.18502/ijph.v50i3.5594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Xu W, Shen W, Wang S. Intervention of adolescent’ mental health during the outbreak of COVID-19 using aerobic exercise combined with acceptance and commitment therapy. Child Youth Serv Rev. 2021;124 doi: 10.1016/j.childyouth.2021.105960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liu G, Wang S, Liao J, et al. The efficacy of WeChat-based parenting training on the psychological well-being of mothers with children with autism during the COVID-19 pandemic: quasi-experimental study. JMIR Ment Health. 2021;8(2):e23917. doi: 10.2196/23917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liu Z, Qiao D, Xu Y, et al. The efficacy of computerized cognitive behavioral therapy for depressive and anxiety symptoms in patients with COVID-19: randomized controlled trial. J Med Internet Res. 2021;23(5):e26883. doi: 10.2196/26883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Song JQ, Jiang RH, Chen N, et al. Self-help cognitive behavioral therapy application for COVID-19-related mental health problems: a longitudinal trial. Asian J Psychiatr. 2021;60 doi: 10.1016/j.ajp.2021.102656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sun S, Lin D, Goldberg S, et al. A mindfulness-based mobile health (mHealth) intervention among psychologically distressed university students in quarantine during the COVID-19 pandemic: a randomized controlled trial. J Couns Psychol. 2022;69(3):157–171. doi: 10.1037/cou0000568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zheng YF, Wang W, Zhong YX, et al. A peer-to-peer live-streaming intervention for children during COVID-19 homeschooling to promote physical activity and reduce anxiety and eye strain: cluster randomized controlled trial. J Med Internet Res. 2021;23(4):e24316. doi: 10.2196/24316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang WL, Paudel R, Shi R, et al. Virtual reality exposure therapy (VRET) for anxiety due to fear of COVID-19 infection: a case series. Neuropsychiatr Dis Treat. 2020;16:2669–2675. doi: 10.2147/NDT.S276203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.He ZL, Chen JJ, Pan KL, et al. The development of the “COVID-19 Psychological Resilience Model” and its efficacy during the COVID-19 pandemic in China. Int J Biol Sci. 2020;16(15):2828–2834. doi: 10.7150/ijbs.50127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Li X, Li T, Wu X, Tao Q, Huang X, Zhu S. Effectiveness of Tibet culture-based intervention to acute stress response of earthquake wounded in Yushu earthquake. Chin Ment Health J. 2011;25(07):492–493. (in Chinese) [Google Scholar]
- 52.Niu Y, Jiang XL, Ashong Z, et al. Developing a resilience intervention approach for adolescents living with natural hazards risks: a pilot randomized controlled trial. Int J Disaster Risk Reduct. 2021;58 [Google Scholar]
- 53.Huang X, Liu K, Huang X, et al. The effect of Equilibrium Psychological Intervention in wounded patients in Lushan earthquake. J Sichuan Normal Univ. 2014;45(03):533–535. (in Chinese) [PubMed] [Google Scholar]
- 54.Guan J, Wen X, Li J, Wang Y, Zhu S, Lei H. The practice of hierarchical psychological nursing for post-earthquake victims. Chin J Nurs. 2018;18(07):894–897. (in Chinese) [Google Scholar]
- 55.Ke YT, Chen HC, Lin CH, et al. posttraumatic psychiatric disorders and resilience in healthcare providers following a disastrous earthquake: an interventional study in Taiwan. Biomed Res Int. 2017;2017 doi: 10.1155/2017/2981624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wang Z, Zhu Z, Zhu H, et al. Psychological crisis intervention model in Xiaotangshan Hospital of PLA. Chin Ment Health J. 2003;17:587–590. (in Chinese) [Google Scholar]
- 57.Cui S, Deng B, Zhu Y, Zhou L. Analysis and intervention of mental health problems in 48 SARS patients. Chin J Nurs. 2004;39(08):43–45. (in Chinese) [Google Scholar]
- 58.Jin N, Zuo Y, Zhang X, Tang H, Ma X. Intervention of anxiety in 138 quarantined high school students during SARS. Chin Ment Health J. 2003;17(9):597. (in Chinese) [Google Scholar]
- 59.Cheng SF, Cheng CW, Hsieh WC, Chi MC, Lin SJ, Liao YT. Effects of individual resilience intervention on indigenous people who experienced Typhoon Morkot in Taiwan. Kaohsiung J Med Sci. 2012;28(2):105–110. doi: 10.1016/j.kjms.2011.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zatzick D, Jurkovich G, Rivara FP., et al. A randomized stepped care intervention trial targeting posttraumatic stress disorder for surgically hospitalized injury survivors. Ann Surg. 2013;257(3):390–399. doi: 10.1097/SLA.0b013e31826bc313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yang D, Xhen L, Gu J, Chen L, Ji H, Chen X. Psychological status and psychological intervention of COVID-19 patients in Fangcang shelter hospital. China J Health Psychol. 2021;29(04):560–564. (in Chinese) [Google Scholar]
- 62.Chen L, Yin G, Zhang L, Ping H. Psychological intervention to Sichuan earthquake survivors who were sent to Hangzhou for treatment. Med Soc. 2009;22(4):50–52. (in Chinese) [Google Scholar]
- 63.Chen Q, Liang M, Li Y, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):e15–e16. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Yu H. Study on intervention methods of psychological crisis of survivors after Wenchuan earthquake. J Catastrophol. 2019;34(04):176–180. (in Chinese) [Google Scholar]
- 65.Cheng W, Zhang F, Liu Z, et al. A psychological health support scheme for medical teams in COVID-19 outbreak and its effectiveness. Gen Psychiatr. 2020;33(5) doi: 10.1136/gpsych-2020-100288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Li Y, Li J, Wang Z, Wang F. Analysis of Psychological crisis intervention effect of medical workers during pneumonia epidemic. J Catastrophol. 2021;36(2):166–170. (in Chinese) [Google Scholar]
- 67.Dyregrov A, Yule W, Olff M. Children and natural disasters. Eur J Psychotraumatol. 2018;9(2):9–11. doi: 10.1080/20008198.2018.1500823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zong Y, Zhu Z, Wang X, et al. Chinese calligraphic handwriting intervention to posttraumatic stress of 210 primary school students after earthquake. Chin J Behav Med Brain Sci. 2010;19(03):267–268. (in Chinese) [Google Scholar]
- 69.Ouyang X, Lei H, Tu S, Chen X. Physical exercise intervention of teenage mental health after major disasters. Chin J Special Educ. 2009;108(6):91–96. (in Chinese) [Google Scholar]
- 70.Chen L, Zhang H. Sports dance intervention of student's anxiety in earthquake-stricken areas. J Sichuan Normal Univ. 2010;33(5):715–718. (in Chinese) [Google Scholar]
- 71.Qu X, Liu Y, Liao J, Wang X. Survey of cognitive-behavioral therapy for orphans with post-traumatic stress disorder following Wenchuan earthquake. Chin Ment Health J. 2013;27(07):502–507. (in Chinese) [Google Scholar]
- 72.Zhang Y. Study on the recovery and psychological reconstruction of stress disorder in adolescents in disaster environment. J Catastrophol. 2019;34(03):150–154. (in Chinese) [Google Scholar]
- 73.Zhang J, Zhou Z, Zhang W. Intervention effect of research-based psychological counseling on adolescents’ mental health during the COVID-19 epidemic. Psychiatr Danub. 2021;33(2):209–216. doi: 10.24869/psyd.2021.209. [DOI] [PubMed] [Google Scholar]
- 74.Ding XS, Yao JW. Peer education intervention on adolescents' anxiety, depression, and sleep disorder during the COVID-19 pandemic. Psychiatr Danub. 2020;32(3-4):527–535. doi: 10.24869/psyd.2020.527. [DOI] [PubMed] [Google Scholar]
- 75.Yan C, Rittenbach K, Souri S, Silverstone PH. Cost-effectiveness analysis of a randomized study of depression treatment options in primary care suggests stepped-care treatment may have economic benefits. BMC Psychiatry. 2019;19(1):240. doi: 10.1186/s12888-019-2223-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chen Y, Shen WW, Gao K, Lam CS, Chang WNC, Deng H. Effectiveness RCT of a CBT intervention for youths who lost parents in the Sichuan, China, earthquake. Psychiatr Serv. 2014;65(2):259–262. doi: 10.1176/appi.ps.201200470. [DOI] [PubMed] [Google Scholar]
- 77.Zang Y, Hunt N, Cox T. Adapting narrative exposure therapy for Chinese earthquake survivors: a pilot randomised controlled feasibility study. BMC Psychiatry. 2014;14:262. doi: 10.1186/s12888-014-0262-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wang H, Mi W, Wang Z, et al. Therapeutic effects of psychological intervention with medication on 150 patients of severe insomnia in post-earthquake. Acad J PLA Postgrad Med Sch. 2008;29(4):251–253. (in Chinese) [Google Scholar]
- 79.Meng XZ, Wu F, Wei PK, et al. A Chinese herbal formula to improve general psychological status in posttraumatic stress disorder: a randomized placebo-controlled trial on Sichuan earthquake survivors. Evid Based Complement Alternat Med. 2012;2012 doi: 10.1155/2012/691258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jacobs GA, Gray BL, Erickson SE, Gonzalez ED, Quevillon RP. Disaster mental health and community-based psychological first aid: concepts and education/training. J Clin Psychol. 2016;72(12):1307–1317. doi: 10.1002/jclp.22316. [DOI] [PubMed] [Google Scholar]
- 81.Liang D, Mays VM, Hwang WC. Integrated mental health services in China: challenges and planning for the future. Health Policy Plan. 2018;33(1):107–122. doi: 10.1093/heapol/czx137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Huang JW, Zhou XY, Lu SJ, et al. Dialectical behavior therapy-based psychological intervention for woman in late pregnancy and early postpartum suffering from COVID-19: a case report. J Zhejiang Univ Sci B. 2020;21(5):394–399. doi: 10.1631/jzus.B2010012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Howick J, Chalmers I, Glasziou P, et al. Explanation of the 2011 Oxford Centre for Evidence-Based Medicine (OCEBM) Levels of Evidence (Background Document). Oxford Centre for Evidence-Based Medicine. https://www.cebm.ox.ac.uk/resources/levels-of-evidence/explanation-of-the-2011-ocebm-levels-of-evidence/
- 84.Han P, Cao Z, Wang R, Xu Z. Effectiveness of “HuanHenYinDao” therapy in psychological crisis intervention after the disaster. Lishizhen Med Mater Med Res. 2010;21(3):702–703. (in Chinese) [Google Scholar]
- 85.Li S, Xu Q, Zhou A. Follow-up to a randomized controlled trial of the effect of self-affirmation on anxiety during the COVID-19 pandemic. Psychol Health Med. 2022;27:361–366. doi: 10.1080/13548506.2021.1917770. [DOI] [PubMed] [Google Scholar]
- 86.Lu T, Guo ZH, Li H, et al. Effects of wise intervention on perceived discrimination among college students returning home from Wuhan during the COVID-19 outbreak. Front Psychol. 2021;12 doi: 10.3389/fpsyg.2021.689251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wu C, Zhou T, Wu LP, et al. Analysis of psychological status and effect of psychological intervention in quarantined population during the epidemic of SARS-CoV-2. Medicine. 2021;100(19):e25951. doi: 10.1097/MD.0000000000025951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Xue Y, Lu L, Liang Z, Zhong P, Liu M. A study of sex difference in reaction to the psychological intervention after earthquake. Chin J Rehabil Med. 2009;24(12):1128–1130. (in Chinese) [Google Scholar]
- 89.Liu X, Ng SM, Xing YY, et al. A strength-based online community intervention (SOCI) for promoting resilience among adults in Hubei province, China, during COVID-19 lockdown. Asia Pac J Soc Work Dev. 2021;31(4):253–270. [Google Scholar]
- 90.Liu Y, Yang YQ, Liu Y, et al. Effects of group psychological intervention combined with pulmonary rehabilitation exercises on anxiety and sleep disorders in patients with mild coronavirus disease 2019 (covid-19) infections in a fangcang hospital. Psychol Health Med. 2022;27(2):333–342. doi: 10.1080/13548506.2021.1916956. [DOI] [PubMed] [Google Scholar]
- 91.Bonanno GA. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am Psychol. 2004;59(1):20–28. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- 92.Guyatt G, et al. GRADE guidelines: 4. Rating the quality of evidence–study limitations (risk of bias) J Clin Epidemiol. 2011;64(4):407–415. doi: 10.1016/j.jclinepi.2010.07.017. [DOI] [PubMed] [Google Scholar]
- 93.Qian MY. Comparison of psychological intervention after disaster at home and abroad. Psychology and Health. 2005;4:4–6. (in Chinese) [Google Scholar]
- 94.The State Council of China. The State Council's Rebuild Plan for the Wenchuan Earthquake. http://www.gov.cn/zhengce/content/2008-09/24/content_6121.htm. Accessed 24 September 2008.
- 95.The State Council of China. The State Council's Rebuild Plan for the Lushan Earthquake. http://www.gov.cn/zhengce/content/2013-07/15/content_6528.htm. Accessed 15 July 2013.
- 96.The State Council of China. The State Council's Rebuild Plan for the Ludian Earthquake. http://www.gov.cn/zhengce/content/2014-11/23/content_9234.htm. Accessed 23 November 2014.
- 97.The State Council of China. The State Council's Rebuild Plan for the Yushu Earthquake. http://www.gov.cn/zhengce/content/2010-06/13/content_5598.htm. Accessed 13 June 2010.
- 98.The State Council of China. The State Council's Rebuild Plan for the Zhouqu Mud-Rock Flow. http://www.gov.cn/zhengce/content/2010-11/10/content_6563.htm. Accessed 10 November 2010.
- 99.National Health Commission. The Work Plan to Control the Spread of H1N1 in Communities. https://www.chinacdc.cn/tzgg/200906/t20090617_40375.html. Accessed 17 June 2009.
- 100.The Central Work Group of Fighting COVID-19 Pandemic. Guidelines to Further Protect Medical Personnel during the COVID-19 Pandemic. http://www.gov.cn/zhengce/content/2020-02/23/content_5482345.htm. Accessed 23 February 2020.
- 101.China CDC. The Technical Guide for Prevention and Control of Disease after Erathquake. https://www.chinacdc.cn/dfdt/201205/t20120509_60635.html. Accessed 9 May 2012.
- 102.National Health Commission. The 2010 Postearthquake Psychological Assisstant Program. https://www.chinacdc.cn/jkzt/tfggwssj/gl/201712/P020171228500001593909.pdf. Accessed 28 December 2011.
- 103.The State Council of China. The Information to Setup Psychological Assisstant Hotlines during the COVID-19 Pendemic. https://www.chinacdc.cn/jkzt/crb/zl/szkb_11803/jszl_11813/202002/t20200203_212165.html. Accessed 3 February 2020.
- 104.China CDC. The Emergency Operation Guide for Natural Disaster-Related Health Work. https://www.chinacdc.cn/jkzt/tfggwssj/gl/201708/t20170810_149326.html. Accessed 10 August 2017.
- 105.Chinese Psychological Society. The “AnXin” Program to Fight with COVID-19 Pandemic. https://www.cpsbeijing.org/news/index.htm. Accessed 1 March 2020.
- 106.Galatzer-Levy IR, Huang SH, Bonanno GA. Trajectories of resilience and dysfunction following potential trauma: a review and statistical evaluation. Clin Psychol Rev. 2018;63:41–55. doi: 10.1016/j.cpr.2018.05.008. [DOI] [PubMed] [Google Scholar]
- 107.Mayou RA, Ehlers A., Hobbs M. Psychological debriefing for road traffic accident victims. Three-year follow-up of a randomised controlled trial. Br J Psychiatry. 2000;176:589–593. doi: 10.1192/bjp.176.6.589. [DOI] [PubMed] [Google Scholar]
- 108.Masterson-Duva M, Haugen P, Werth A, et al. Adapting meaning-centered psychotherapy for World Trade Center responders. Palliat Support Care. 2020;18(6):636–643. doi: 10.1017/S1478951520000061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Xu H, Tracey TJG. Cultural congruence with psychotherapy efficacy: a network meta-analytic examination in China. J Couns Psychol. 2016;63(3):359–365. doi: 10.1037/cou0000145. [DOI] [PubMed] [Google Scholar]
- 110.Reynolds DK. Naikan therapy–an experiential view. Int J Soc Psychiatry. 1977;23(4):252–263. doi: 10.1177/002076407702300404. [DOI] [PubMed] [Google Scholar]
- 111.Kitanishi K, Mori A. Morita therapy: 1919 to 1995. Psychiatry Clin Neurosci. 1995;49(5-6):245–254. doi: 10.1111/j.1440-1819.1995.tb01896.x. [DOI] [PubMed] [Google Scholar]
- 112.Benish SG, Quintana S, Wampold BE. Culturally adapted psychotherapy and the legitimacy of myth: a direct-comparison meta-analysis. J Couns Psychol. 2011;58(3):279–289. doi: 10.1037/a0023626. [DOI] [PubMed] [Google Scholar]
- 113.Hall BJ. The Oxford Handbook of Traumatic Stress Disorders. 2nd ed. Oxford University Press; 2020. Assessment of PTSD in non-western cultures. [Google Scholar]
- 114.Xie Q, Wong DFK. Culturally sensitive conceptualization of resilience: a multidimensional model of Chinese resilience. Transcult Psychiatry. 2021;58(3):323–334. doi: 10.1177/1363461520951306. [DOI] [PubMed] [Google Scholar]
- 115.Gureje O, Lewis-Fernandez R, Hall BJ, Reed GM. Systematic inclusion of culture-related information in ICD-11. World Psychiatry. 2019;18(3):357–358. doi: 10.1002/wps.20676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Wang X, Gao L, Shinfuku N, Zhang H, Zhao C, Shen Y. Longitudinal study of earthquake-related PTSD in a randomly selected community sample in north China. Am J Psychiatry. 2000;157(8):1260–1266. doi: 10.1176/appi.ajp.157.8.1260. [DOI] [PubMed] [Google Scholar]
- 117.Ling R, Sit HF, Balaji S, et al. Crowdsourcing to design a marketing package to promote a WHO digital mental health intervention among Chinese young adults. Internet Interv. 2021;25 doi: 10.1016/j.invent.2021.100397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Sit HF, Hong IW, Burchert S, et al. A feasibility study of the WHO Digital Mental Health Intervention Step-by-Step to address depression among Chinese young adults. Front Psychiatry. 2022;12 doi: 10.3389/fpsyt.2021.812667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Que J, Lu L, Shi L. Development and challenges of mental health in China. Gen Psychiatr. 2019;32(1) doi: 10.1136/gpsych-2019-100053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.O'Connor K, Muller Neff D, Pitman S. Burnout in mental health professionals: a systematic review and meta-analysis of prevalence and determinants. Eur Psychiatry. 2018;53:74–99. doi: 10.1016/j.eurpsy.2018.06.003. [DOI] [PubMed] [Google Scholar]
- 121.Lee S, Chiu MYL, Tsang A, Chui H, Kleinman A. Stigmatizing experience and structural discrimination associated with the treatment of schizophrenia in Hong Kong. Soc Sci Med. 2006;62(7):1685–1696. doi: 10.1016/j.socscimed.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 122.Shi W, Hall BJ. Help-seeking preferences among Chinese college students exposed to a natural disaster: a person-centered approach. Eur J Psychotraumatol. 2020;11(1) doi: 10.1080/20008198.2020.1761621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Bauer MS, Kirchner JA. Implementation science: what is it and why should I care? Psychiatry Res. 2020;283 doi: 10.1016/j.psychres.2019.04.025. [DOI] [PubMed] [Google Scholar]
- 124.Eccles MP, Mittman BS. Welcome to implementation science. Implement Sci. 2006;1:1. [Google Scholar]
- 125.Singla DR, Hollon SD. The importance of implementation science in scaling up psychological treatments. Behav Res Ther. 2020;130 doi: 10.1016/j.brat.2020.103614. [DOI] [PubMed] [Google Scholar]
- 126.Kessler RC, Mclaughlin KA, Koenen KC, Petukhova M, Hill ED.The importance of secondary trauma exposure for post-disaster mental disorder. http://www.economist.com/blogs/dailychart/2011/03/. Accessed March 2011. [DOI] [PMC free article] [PubMed]
- 127.United Nations Office for Disaster Risk Reduction. Sendai framework for disaster risk reduction 2015–2030. https://www.undrr.org/publication/sendai-framework-disaster-risk-reduction-2015-2030. Accessed 18 March 2015.
- 128.The State Council of China. The State Council‘s Guidelines on the Sanitary and Anti-Epidemic Work in Earthquake-Striken Areas.http://www.gov.cn/zhengce/content/2008-06/25/content_5677.htm. Accessed 25 June 2008.
- 129.Xi S, Lu G, Ma J, Lu L, Shao X, Wang L. Effectiveness of psychological intervention on anxiety and depression in persons wounded in earthquake. Chin J Nurs. 2008;12:1064–1066. (in Chinese) [Google Scholar]
- 130.National Health Commission. National Health Commission's Guideline to Further Improve Mental Health Work. http://www.gov.cn/zhengce/content/2008-03/28/content_6282.htm. Accessed 28 March 2008.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.