Distal triceps tendon rupture is an uncommon injury, constituting less than 1% of all upper extremity tendon injuries.1,7 Usually resulting from eccentric loading of a contracting triceps, these injuries often occur in weight lifters and athletes.6,10 Distal triceps tendon rupture occurs typically as an avulsion from the osseous tendon insertion but may also occur at the myotendinous junction or within the triceps muscle belly.10 Although no formal classification system exists, triceps tendon ruptures are described by degree of tear, location, and integrity of the lateral expansion.4
Diagnosis of acute triceps tendon rupture can be challenging and is not infrequently misdiagnosed.10 Misdiagnosis prolongs disability and adds significant complexity to management, as primary repair of the ruptured tendon is optimal when performed within three weeks of the injury.9 The purpose of this case study is to report a patient initially diagnosed and treated for olecranon bursitis that was subsequently discovered to have sustained a true full-thickness triceps tendon rupture.
Statement of informed consent
The patient whose case will be discussed was informed that data concerning the case would be submitted for publication and the patient agreed.
Case report
A 53-year-old male recreational bodybuilder and weight lifter presented to the orthopedic shoulder and elbow clinic for evaluation of a 5-week history of right elbow pain and swelling. The patient reported that he sustained an injury to the right elbow while doing triceps extension resistance training exercises in the gym. At the time of the injury, he felt a tearing sensation accompanied by immediate pain and swelling of the posterior aspect of his right elbow. Since the injury, he had also noticed weakness with extension of the elbow against resistance. At this time, he was seen by his primary care physician who, based on history and physical examination, diagnosed him with olecranon bursitis of the right elbow and performed an aspiration. The swelling recurred and pain persisted after the initial aspiration, and the patient was re-evaluated in the primary care clinic. Two more subsequent aspirations of the posterior elbow were performed several weeks apart. As a result of his persisting weakness, pain, and posterior elbow swelling, he presented to the orthopedic shoulder and elbow clinic for evaluation and treatment roughly 5 weeks after the original injury.
Past medical history was significant for anxiety. Past surgical history was significant for prior contralateral distal triceps repair and left knee arthroscopy. The patient reported that he did not take any prescription medications, although he did report prior use of anabolic steroids and drinks alcohol socially. On exam, he was a healthy-appearing 53-year-old male with muscular build. Evaluation of the right elbow demonstrated a 5 cm × 4 cm fluctuant collection around the posterior aspect of his elbow, with no spreading erythema or open wounds. There was full passive range of motion (ROM) from 0 to 140 degrees. He was able to extend the right elbow against gravity, but had marked weakness with extension against resistance. Flexion and extension arc was normal; he had full pronosupination, full strength with resisted elbow flexion, and no visible triceps retraction. Gross neurovascular assessment of the right hand was unremarkable.
Initial anteroposterior and lateral radiographs of the right elbow demonstrated chronic calcification of the triceps tendon posteriorly (Figs. 1 and 2). A T2-weighted magnetic resonance imaging (MRI) of the right elbow was then performed in order to further evaluate the injury, which was interpreted and reviewed by a fellowship-trained shoulder and elbow orthopedic surgeon. T2-weighted MRI of the right elbow demonstrated a full-thickness tear of the triceps tendon with approximately 5 centimeters of retraction off the distal insertion of the olecranon process with surrounding hyperintense T2 signal (Figure 3, Figure 4, Figure 5). No intra-articular effusion or loose bodies were present, and there was no significant radiocapitellar or ulnohumeral arthrosis. No other abnormalities were noted on the MRI.
Figure 1.
Preoperative radiograph. Anteroposterior view of the right elbow with evidence of swelling of the olecranon bursa and no evidence of radiocapitellar or ulnohumeral arthrosis.
Figure 2.
Preoperative radiograph. Lateral view of the right elbow in 90 degrees of flexion with evidence of chronic calcification of triceps tendon posteriorly (white arrow).
Figure 3.
Preoperative magnetic resonance imaging. Sagittal T2-weighted MRI of the right elbow with evidence of full-thickness tear of the triceps tendon with approximately 5 cm of retraction off the distal insertion of the olecranon process and surrounding hyperintense T2 signal.
Figure 4.
Preoperative magnetic resonance imaging. Axial T2-weighted MRI of the right elbow with evidence of full-thickness tear of the triceps tendon with surrounding hyperintense T2 signal.
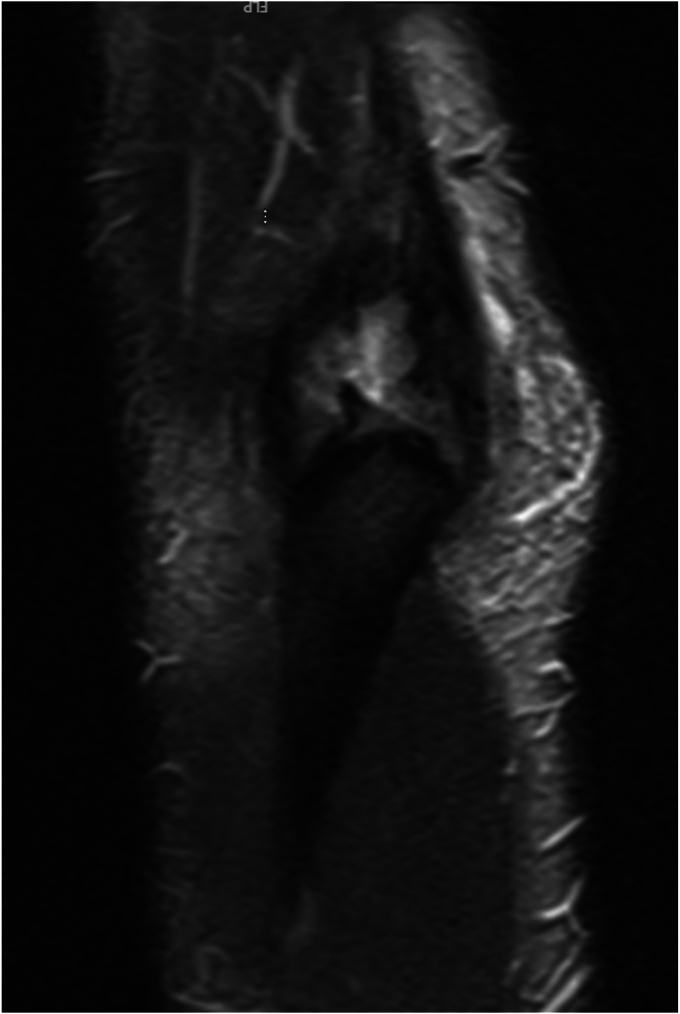
Figure 5.
Preoperative magnetic resonance imaging. Coronal T2-weighted MRI of the right elbow with evidence of full-thickness tear of the triceps tendon.
It was determined that the patient’s injury would be best managed by surgical repair of the right triceps tendon repair. A longitudinal direct posterior incision was made that curved slightly laterally around the tip of the olecranon. Medial and lateral epicondyles were marked, “M” medially over the medial epicondyle and an “L” over the lateral epicondyle. Next, the skin was incised longitudinally with a scalpel. Full-thickness flaps were developed. A large bursal sac was encountered and excavated away from the skin. The sac was removed completely and a total bursectomy was performed. Next, attention was turned to the triceps. The dissection was developed sharply down to the triceps fascia and the extensor carpi ulnaris - flexor carpi ulnaris interval overlying the ulna. The distal triceps tendon rupture was identified. Full-thickness skin and subcutaneous flaps were made. At this point in time, the tension edge was débrided to healthy tissue with a curette and scalpel. The site was copiously irrigated. The tendon insertion site was débrided and prepared. A 5.0-mm drill was utilized to make two diagonal bone tunnels from the insertion bed through the dorsal cortex of the olecranon. Two #5 Kevlar core (Fiberwire; Arthrex Naples, FL, USA) sutures were placed up through the triceps tendon in a running locking fashion. A suture retriever was utilized to shuttle the tails. The proximal portion of the tendon was then reduced. The tails were taken back up through the triceps tendon and tied. Those tails were then taken through a 5.5-mm biocomposite anchor (Arthrex Swivelock; Arthrex, Naples, FL, USA). A 5.0-mm drill was utilized to make a cortical drill hole midline more distal on the ulna. The hole was tapped. The anchor was placed and suture tails tensioned. Secure fixation of the construct was obtained. The patient was then examined and the elbow had full extension, flexion, and pronosupination without mechanical block. Hemostasis was obtained. The wound was copiously irrigated. Deep and superficial closures were performed. Final x-rays were obtained (Fig. 6). Sterile dressing was applied. A posterior mold splint was applied for soft tissue rest at 50 degrees of flexion. All counts were reported as correct and the patient was extubated and taken to the recovery without complication (Fig. 7).
Figure 6.
Intraoperative radiograph. Lateral view of right elbow in 60 degrees of flexion after repair of the triceps tendon. No evidence of loose bodies or calcifications is present.
Figure 7.
Step-by-step images of the procedure. (a) Patient in lateral position, elbow at 90 degrees of flexion, and longitudinal direct posterior incision that curves slightly laterally around the tip of the olecranon. (b) Development of full-thickness skin flaps and excavation of olecranon bursa. (c) Identification and reduction of ruptured distal triceps tendon. (d) Two #5 Kevlar core (Fiberwire; Arthrex Naples, FL, USA) sutures were placed up through the triceps tendon in a running locking fashion. (e) A 5.0-mm drill was utilized to make two diagonal bone tunnels from the insertion bed through the dorsal cortex of the olecranon. A suture retriever was utilized to shuttle the tails of suture through the bone tunnel. (f) The suture tails were then taken through a 5.5-mm biocomposite anchor (Arthrex Swivelock; Arthrex, Naples, FL, USA). (g) A 5.0-mm drill was utilized to make a cortical drill hole midline more distal on the ulna. The hole was tapped. The anchor was placed and suture tails tensioned. (h) Secure fixation of the construct was obtained.
The patient underwent 2 weeks of immobilization in a posterior mold splint. At two weeks postop, the posterior mold splint and 3-0 nylon sutures were removed, and the patient was transferred to a fitted hinged elbow brace locked at 120 degrees of extension for four weeks. Formal occupational therapy was begun at 3 weeks postop. The patient was monitored for signs and symptoms of infection or increased pain. At 6 weeks postop, the patient achieved 5-135 degrees of ROM through flexion and extension, the hinged elbow brace was unlocked, and formal occupational therapy was continued. At 12 weeks postop, the patient achieved 0-140 degrees of ROM through flexion and extension, and the hinged elbow brace was discontinued. The patient was discharged from occupational therapy, continued a light home exercise program, and had no formal restrictions to movement or weight bearing. At 16 weeks, he returned to weightlifting without restriction. At one year postop, he had full strength and ROM compared to the contralateral side, was able to perform all activities of daily living without issues, and had a Mayo Elbow Performance Score of 100.
Discussion
Diagnosis of acute triceps tendon rupture may be difficult and at times misdiagnosed if there is not a high index of suspicion. In addition, focused examinations of patients presenting with acute traumatic elbow injuries are often limited due to pain and swelling. Particularly, elbow extension against gravity, a test specific for function of the triceps tendon, is often forgone. Furthermore, radiographic findings such as the Dunn-Kusnezov sign—tiny avulsed flecks visible on lateral elbow radiograph—can be missed in fast-paced emergency room settings.2 Imaging tools such as MRI or ultrasound can be useful for differentiating full-thickness and partial-thickness tears as well as surgical planning.3 However, even in cases where MRI has been performed, it has been documented that MRI can overestimate the severity of distal triceps tendon ruptures.5
Consequences of full-thickness triceps tendon rupture misdiagnosis include prolonged disability, increased complexity of management, and increased risk of suboptimal outcomes.8,9 In this unique case, olecranon bursitis was the only diagnosis made initially, which resulted in a 5-week delay in definitive surgical management. With careful history, it was discovered that this avid weightlifter meets the demographic of patients with a high index of suspicion of tendon rupture. Focused physical examination demonstrated that in addition to a large fluctuant collection about the olecranon, the patient had significant weakness of right elbow extension against resistance. When exam findings raise suspicion of full-thickness triceps tendon rupture, advanced imaging is advisable to confirm the diagnosis.
Conclusion
Although atraumatic aseptic olecranon bursitis is an extremely common cause of focal posterior elbow swelling, providers should continue to consider comprehensive differential diagnoses. It is important to identify patients that have specific risk factors for triceps tears and thus have a high index of suspicion for this injury. It is imperative to obtain a detailed history and comprehensive musculoskeletal examination to ensure accurate and timely diagnosis. Confirmatory imaging may aid in diagnosis prior to recommending or performing invasive treatments, such as aspiration. When abnormal findings are suggestive of severe soft tissue injury, prompt advanced imaging is warranted to guide management.
Disclaimers:
Funding: No funding was disclosed by the authors.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Patient consent: Obtained.
Footnotes
Institutional review board approval was not required for this case report.
References
- 1.Anzel S.H., Covey K.W., Weiner A.D., Lipscomb P.R. Disruption of muscles and tendons; an analysis of 1, 014 cases. Surgery. 1959;45:406–414. [PubMed] [Google Scholar]
- 2.Dunn J.C., Kusnezov N., Fares A., Rubin S., Orr J., Friedman D., et al. Triceps tendon ruptures: a systematic review. Hand (N Y) 2017;12:431–438. doi: 10.1177/1558944716677338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Homen D., Domingo-Johnson E.L., Helm J.M., Schalow M., Zumwalt M. Triceps tendon rupture - a novel repair of an uncommon injury. J Orthop Case Rep. 2020;10:35–39. doi: 10.13107/jocr.2020.v10.i02.1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Keener J.D., Sethi P.M. Distal triceps tendon injuries. Hand Clin. 2015;31:641–650. doi: 10.1016/j.hcl.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 5.Kholinne E., Al-Ramadhan H., Bahkley A.M., Alalwan M.Q., Jeon I.H. MRI overestimates the full-thickness tear of distal triceps tendon rupture. J Orthop Surg. 2018;26 doi: 10.1177/2309499018778364. [DOI] [PubMed] [Google Scholar]
- 6.Lee J.H., Ahn K.B., Kwon K.R., Kim K.C., Rhyou I.H. Differences in rupture patterns and associated lesions related to traumatic distal triceps tendon rupture between outstretched hand and direct injuries. Clin Orthop Relat Res. 2021;479:781–789. doi: 10.1097/CORR.0000000000001550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Neumann H., Schulz A.-P., Breer S., Faschingbauer M., Kienast B. Traumatic rupture of the distal triceps tendon (a series of 7 cases) Open Orthop J. 2015;9:536–541. doi: 10.2174/1874325001509010536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van Riet R.P., Morrey B.F., Ho E., O’Driscoll S.W. Surgical treatment of distal triceps ruptures. J Bone Joint Surg Am. 2003;85:1961–1967. doi: 10.2106/00004623-200310000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Sharma S.C., Singh R., Goel T., Singh H. Missed diagnosis of triceps tendon rupture: a case report and review of literature. J Orthop Surg. 2005;13:307–309. doi: 10.1177/230949900501300317. [DOI] [PubMed] [Google Scholar]
- 10.Yeh P.C., Dodds S.D., Smart L.R., Mazzocca A.D., Sethi P.M. Distal triceps rupture. J Am Acad Orthop Surg. 2010;18:31–40. doi: 10.5435/00124635-201001000-00005. [DOI] [PubMed] [Google Scholar]