Abstract
Background
Therapeutic exercise has been considered a useful tool to rehabilitate shoulder pain, namely through its influence on scapular dynamics. Accordingly, the effectiveness of scapular therapeutic exercise needs to be explored. The present study aims to evaluate the effectiveness of scapular therapeutic exercises in shoulder pain and to identify the most effective exercise type (focal or multijoint) and ways of delivering them (as dose and progression).
Methods
Search was conducted at EMBASE, Cochrane Library, MEDLINE via PubMed, Web of Science, PEDro (Physiotherapy Evidence Database), and trial registration databases. The meta-analysis considered randomized controlled/crossover trials that compared the effect of scapular exercises against other types of intervention in the shoulder pain, shoulder function, scapular motion, and/or muscular activity. The risk of bias was assessed through the PEDro scale.
Results
From the 8318 records identified, 8 (high to low risk of bias– scoring from 4 to 8 on the PEDro scale) were included. The overall data, before sensitivity analysis, indicated that the scapular therapeutic exercises are: a) more effective than comparators in improving shoulder function (standardized mean difference [SMD] = 0.52 [95% Cl: 0.05, 0.99], P = .03, I2 = 76%); and b) as effective as comparators in reducing shoulder pain (SMD = 0.32 [95% Cl: −0.09, 0.73], P = .13, I2 = 70%). Subgroup analysis revealed that scapular exercises are more effective in improving shoulder function when the program duration is equal to or higher than 6 weeks (SMD = 0.43 [95% Cl: 0.09, 0.76] P = .01, I2 = 21%) and/or when the maximum number of exercise repetitions per session is lower than 30 (SMD = 0.79 [95% Cl: 0.15, 1.42], P = .01, I2 = 77%). Only 1 study considered scapular motion as an outcome measure, revealing therapeutic exercise effectiveness to improve scapular range of motion.
Conclusions
Intervention programs involving scapular therapeutic exercises are effective in improving shoulder function, presenting benefits when performed for 6 or more weeks and/or when used up to a maximum of 30 repetitions per exercise, per session.
Keywords: Scapular muscles, Pain, Function, Kinematics, Muscular activity, Rehabilitation
Shoulder pain is the third most common musculoskeletal disorder in primary healthcare,21,84 with a 66.7% lifetime prevalence.42 Independent from its structural origin,34,45,68,74 shoulder pain has been associated with adaptations in local and surrounding structures, namely in scapular positioning and motion8,34,40,45,46,50,52,68,74,78,84 and muscular function.15,27,29,41,45,50,60 This association is supported by the determinant role of the scapulothoracic joint in shoulder function.15,27,32,45,50,68 According to our knowledge, at least ten systematic reviews have thoroughly explored the effectiveness of therapeutic exercise interventions in patients with shoulder pain.1,7,9,17,23,50,63,70,72,18,83
From the mentioned reviews, only two (both published in 2020) have explored the effectiveness of specific scapular therapeutic exercises.50,63 Although these two reviews had reported exercise effectiveness in pain intensity, disability,50,63 and glenohumeral positioning sense,63 inconclusive findings have been reported for scapular position and motion.50 Moreover, some limitations have been highlighted as: 1) the isolated effects of scapular exercises could not always be assessed once other intervention techniques were combined with the scapular exercises in the experimental group and not in the control group; 2) while one of the reviews have only included patients with subacromial impingement syndrome,63 the other focused its interest in subjects with scapular dyskinesis, including and comparing both symptomatic or asymptomatic participants; and 3) both reviews only performed a qualitative analysis of the included studies. In turn, the other previous systematic reviews about global shoulder therapeutic exercises1,7,17,23,70,72,18,83 have demonstrated the following: 1) effectiveness,23,18 contradictory1,7,72 and inconclusive70 findings for shoulder pain; 2) effectiveness,17,23,72 contradictory1,7,18 and inconclusive findings70 for shoulder function; 3) effectiveness for shoulder range of motion23,72 and shoulder muscle strength1,9; 4) contradicting findings for quality of life,7 muscle length and posture outcomes18; and 5) inconclusive results about scapular position/motion.9 These conflicting results may be attributed to several factors, such as the inclusion of small sample-sized studies, high levels of observed heterogeneity, or the use of different comparators (between-groups vs. within-group comparisons). Given the mentioned facts, continued research about the effectiveness of therapeutic exercise in shoulder pain conditions, particularly the ones focusing on the scapular muscles, to reduce pain and/or restore shoulder function becomes relevant. The persistency20,51 of these conditions and their impact on daily life activities,38,42,53,56 psychological aspects,44 quality of life, and socioeconomic component20,44,73 highlight this need. Additionally, it is noteworthy that only two of the mentioned systematic reviews50,63 consider 3D scapular kinematics as an outcome measure and none considered the scapular muscular activity. The inclusion of such parameters seems relevant, considering: a) the importance of scapular positioning and muscular activity for scapulohumeral rhythm35,41,57,78; and b) the adaptations found in these parameters during shoulder pain.11,12,14,34,41,46,47,60,61,78,79 Moreover, to our knowledge, the previous systematic reviews did not consider in their analysis the type7,9,50,64 and the ways of delivering1,7,9,50,63,64 exercise which can contribute to the conflicting findings previously demonstrated.
The present review aims to evaluate the effectiveness of scapular therapeutic exercises, performed alone or in addition to a baseline intervention, in shoulder pain conditions, considering outcomes such as shoulder pain, shoulder function, and scapular motor control-related variables. Secondarily, it aims to identify the exercise characteristics that could be associated with the effectiveness of scapular therapeutic exercises in patients with shoulder pain. Specifically, the exercise type (focal or multijoint exercises) and ways of delivering (total duration of intervention, weekly frequency, maximum number of exercise repetitions, and progression) were considered for analysis.
Materials and methods
This systematic review follows the guidelines of PRISMA54,55 and was registered at PROSPERO (CRD42020215869).
Search strategy
A systematic search was performed in April 2023 in five main databases (EMBASE; Cochrane Library; MEDLINE via PubMed; Web of Science; PEDro), in the database of the World Health Organization (WHO ICTRP), and in the US National Institutes of Health (ClinicalTrials.gov). The search was limited to studies published after the year 2000. These criteria were used because most studies about scapula's role in the rehabilitation of shoulder pain82 and about scapular clinical tests (positioning and influence in shoulder pain29,31,62,77) had already been published during the XXI century. The search strategy developed and adapted to each specific thesaurus (Supplementary Appendix A) was based on the most common terms related to “shoulder pain” and “therapeutic exercise”.
Selection of studies
After removing the duplicates using Endnote software, all titles and abstracts were independently assessed by two reviewers. For this process, a pre-established template considering the eligibility criteria of the present review with meta-analysis was used and compared after each reviewer completed all decisions. Then, a full-text review of the potentially eligible studies was made independently by the two reviewers. At the end of this independent process, decisions were compared, and the disagreements were resolved by discussion or by a third independent reviewer.
Randomized controlled trials, controlled clinical trials, and interventional prepost-design studies, published in English, French, Portuguese, or Spanish, were eligible if, in accordance with the PICO (patient, intervention, comparison, outcome) strategy, they considered: a) adults (≥18 year old) with shoulder pain, nonspecific or associated with a diagnosis (as rotator cuff tendinopathy or tear, impingement syndrome, bursitis, instability, adhesive capsulitis, and periarthritis)59,18; b) any type of therapeutic exercises that has focused exclusively on the scapular musculature and that was performed in any type of context, with or without supervision and with or without resistance [body weight (self or manual resistance) and/or elastic or weights resistance]; c) comparators as no intervention or other types of control; d) outcomes as pain and/or function (through standardised and validated self-reported questionnaire), scapular motion (through 3D-kinematic), and/or muscular activity level or ratios (through electromyography). Studies in which it was not possible to isolate the effects of scapular exercises in the experimental group were excluded. Other exclusion criteria were considered, namely, studies including animal or cadaveric samples; shoulder pain resulting from infection, neoplasm, surgery, fractures, or dislocation and/or associated with spinal pathology or dysfunction; and pain originated in other related areas as cervical or thoracic regions.
Data extraction
A standardised data extraction form was developed, piloted, and used to collect data for analysis. Two reviewers extracted the following data: study identification, participants’ data, intervention description, outcomes of interest, assessment moments, and main results. Disagreements were resolved by mutual agreement or with a third reviewer. The template for intervention description and replication checklist was used to ensure the extraction of all the relevant details regarding included interventions (considering parameters such as exercise name; exercise aim/rationale; exercise provider; number of sessions, duration, intensity, and dose; tailoring or personalization or adaptation of the intervention to each participant; and modifications over the study). In the case of important missing data, the study’s authors were contacted by mail.
Quality assessment
The study’s methodological quality was assessed independently through the PEDro scale. The PEDro scale is a valid measure of the methodological quality of clinical trials,48 assessing study internal and external validity as well as the suitability of statistical information to allow the interpretation of the results. Scores from 0–5 were considered high risk of bias (ROB)10,66 and from 6–10, which satisfied at least 50% of the criteria,6 as low ROB.10,66
Statistical analysis
A meta-analysis, using Review Manager 5.4 (The Cochrane Collaboration, London, United Kingdom), was performed to compare scapular therapeutic exercises against other types of control and to compare studies interventions according to scapular therapeutic exercise type and ways of delivering. Groups’ mean, standard deviation, and final sample size were extracted from each study. The difference between groups was calculated considering the mean change in each group from the end of the intervention to the baseline, while the standard deviation (SD) change in each group was calculated using the formulae proposed by Higgins et al.24 When these values were not provided, the SD was calculated by multiplying the standard error (SE) by the square root of the sample size.24 Also, when one outcome was measured on a reverse scale (in which lower scores representing the worst condition), the mean values were multiplied by −1.24 To guarantee that all data from the scales assessing shoulder function used the same score range (0-100), the following formulas were applied:
where y and SDy are the rescaled mean and SD, respectively, the is the observed mean and max and min are the maximum and minimum numerical possible scores.
The following criteria were established for meta-analysis: 1) in the case of cross-over designs,49 only data obtained before the cross-over was considered; 2) considering shoulder pain assessment, only intensity reported in general (not associated with a specific condition) or during activity was considered. The effect size (<0.4, small effect; 0.4-0.7, moderate effect; >0.7, large effect, following Cohen’s16,24,67) was calculated by using the between-group standardized mean difference (SMD) once several studies assessed the same outcomes with different scales,24 with 95% confidence intervals. Calculations used the random-effects inverse variance model since some between-studies variation was expected.
The χ2 test and the I2 were used to assess statistical heterogeneity of effect estimates among studies (if <25%, low heterogeneity; if 25%-50% modest heterogeneity; and if >50%, large heterogeneity58). Subgroup analysis was performed when large heterogeneity was presented based on the comparator [other exercises (considering other muscles), or based on the selected exercise type and ways of delivering (total duration of intervention, weekly frequency, maximum number of exercise repetitions, and progression).
To evaluate the robustness of the findings and verify the influence of studies with high ROB, a leave-one-out method of sensitivity analysis was conducted.
Results
Study selection and characteristics
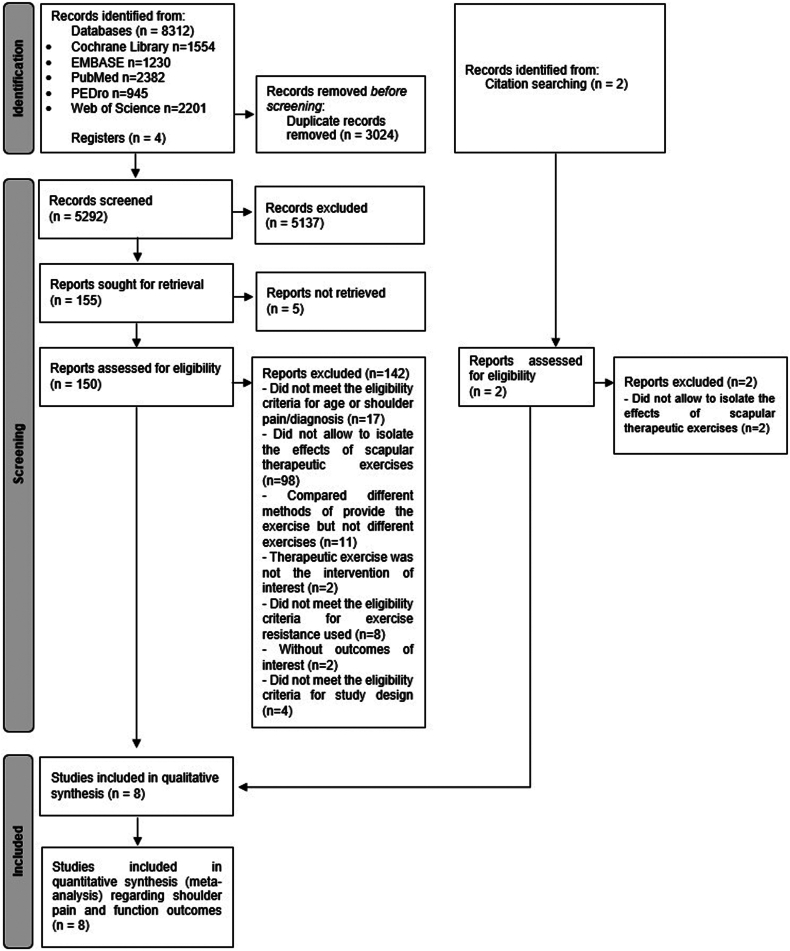
A total of 8314 records and 4 registers were found through the initial search. After removing 3024 duplicates and screening the title and abstract, 152 were analyzed by the full text. As depicted in Figure 1, eight studies met the eligibility criteria (7 randomized controlled trials3, 4, 5,13,25,69,80 and 1 randomized crossover trial49). Excluded studies (n = 144) are listed in Supplementary Appendix B. The concordance between the two independent reviewers was substantial (κ = 0.65).
Figure 1.
PRISMA 2020 flow diagram for literature search result.
The included studies3, 4, 5,13,25,49,69,80 considered a total of 346 participants of both genders, with shoulder pain conditions. Participants’ mean age ranged from 33.4 ± 9.380 to 58.6 ± 11.3.4 Intervention groups performed scapular therapeutic exercises, 23-749,80 times a week, through a total duration varied from a single-hour session4 to a 12-week program,80 (Table I).
Table I.
Overview of the included studies with respect to participants data, intervention, outcomes of interest and results.
| Author, year, study design, country | Participants: Diagnosis (location); n total∗ (by groups), age (mean ± SD) and gender | Comparison | Intervention: Exercises (position); sets/repetitions; progression; frequency (total length) – total number of sessions | Outcomes and assessment moments | Results |
|---|---|---|---|---|---|
| Akguller et al,3 2022, RCT, Turkey | Unilateral subacromial impingement syndrome for at least 3 mo (D or nD sides) N = 36 (16 EG, 16 CG); y: 47.56 ± 10.79 (EG), 47.37 ± 12.63 (CG); gender: 27F, 5M |
Standard exercise program: rotator cuff strengthening exercises (3 sets of 10 reps - with elastic band), scapula setting exercise, and posture exercises | Same as comparison, with additionally scapular PNF techniques: I. “Anterior elevation”-“posterior depression” and “anterior depression”-“posterior elevation” patterns of the scapula (side-lying - with rhythmic initiation and repeated stretch technique) 5-10 reps (20’’ rest between reps) Progressed by reps and added techniques 2 × week (6 weeks) – 12 sessions, applied by a physiotherapist |
Pain (VAS – at rest, at night and during activity); Shoulder function (DASH) Pre & Post |
Significant differences between groups on shoulder function, at 6 weeks (P = .026) No significant differences between groups on pain, at 6 weeks (P > .05) |
| Balci et al,4 2016, RCT, Turkey | Unilateral adhesive capsulitis of stage II and pain for at least 3 mo (D or nD sides) N = 53 (18 EG, 17 CG); y: 56.7 ± 7.7 (EG), 58.6 ± 11.3 (CG); gender: 25F, 10M |
Hot pack (20 min), conventional TENS (20 min, at a frequency of 100 Hz, a pulse duration of 60 μsn), US (3 min, at 1 MHz US head and 1.5 W/cm2 dosage) | EG - same as control group, with additionally scapular PNF: I. “anterior elevation”–“posterior depression” and “posterior elevation”–“anterior depression” scapula patterns (side-lying - rhythmic initiation and repeated contractions) 20 reps (20’’ rest between reps) - 1 h session, applied by a trained therapist |
Pain (VAS – during activity); Function (SST) Pre & Post |
No significant differences between groups on pain (P > .05) and shoulder function (P > .05) |
| Başkurt et al,5 2011, RCT, Turkey | Unilateral shoulder impingement of Neer stages I and II (ND) N = 40 (20 EG, 20 CG); y: 51.5 ± 8.4 (EG), 51.3 ± 11.6 (CG); gender: 27F, 13M |
Standardized flexibility (internal rotation and capsule stretching, forward flexion and abduction range of motion), strengthening (infraspinatus, deltoid, subscapularis and supraspinatus) and Codman exercises | Same as comparison, but with additionally scapular stabilization: I. Scapular clock exercise, II. Standing weight shift, III. Wall push up, IV. Wall slide exercises (upright) + V. scapular PNF exercises (side-lying) + VI. Double arm balancing and scapular depression (ND) 3 sets until 10 reps Progressed by reps and stronger elastic band (according to pain and fatigue) 3 × week (6 weeks) – 18 sessions, under physiotherapist supervision |
Pain (VAS – at rest and during activity); Physical symptoms and Function (WORC) Pre & Post |
No significant differences between groups on pain (P > .05) and shoulder function (P > .05), at 6 weeks |
| Çelik, 2010,13 RCT, Turkey | Primary or secondary adhesive capsulitis (D or nD sides) N = 29 (15 EG, 14 CG); y: ≈ 49.6 (EG), ≈ 54.8 (CG); gender: 22F, 7M |
Passive or active assistive manual stretching, PNF and phase I gliding exercises, Pulley exercises, TENS (20’, 5 weeks), Cold pack (15’), nonsteroidal anti-inflammatory drugs (5 weeks), home exercises (self-stick, posterior and inferior capsule stretching, flexion, scapular elevation, internal and external rotation - 20 reps, 2 × day, additionally) | Same as comparison, with additionally scapulothoracic strengthening and mobilization exercises: I. Scapular retraction with exercise band, II. Extension with exercise band, III. Scapular adduction and elevation, IV. Wall and table push-up, V. Scapular stabilization with ball and scapular abduction (upright) + VI. Floor push-up, VII. Extension and scapular adduction (prone) + VIII. Push-up (sitting) 2 sets of 15 reps Progressed by increased frequency and intensity (according to pain and muscle strength) 5 × week (6 weeks) – 30 sessions, led by physiotherapists at minimum pain level Note: Treatment planned accordingly the clinical phase of each patient |
Pain (VAS - in general); Shoulder Function (modified Constant score) Pre & Post plus follow-up |
Significant differences between groups on pain, at 6 weeks (P = .05) No significant differences between groups on pain, at 12 weeks (P > .05), and on shoulder function, at 6 and 12 weeks (P < .05) |
| Hotta et al,25 2020, RCT, Brazil | Subacromial pain syndrome, with history of shoulder pain for more than one week (D or nD sides) N = 60 (26 EG, 27 CG); y: 51 ± 8 (EG), 47 ± 10 (CG); gender: 42F, 18M |
Periscapular strength: side-lying external rotation with abduction at 0°; prone horizontal abduction with external rotation from 90° to 135°; scapular punch; knee push; full can; diagonal D1 | Same as comparison, with additionally scapular stabilization exercise: I. Towel slide, II. Scapular clock, III. Protraction/retraction in front of a mirror (upright) + IV. Scapular PNF (side-lying) + V. Modified inferior glide, VI. Scapular orientation exercise (sitting) 3 sets until 15 reps (1’ rest between reps) Progressed (weekly based) by reps (10, 12 or 15) and load from 60% of 1-RM to 80% of the new 1-RM. Knee push-up progress to push-up plus (feet flat on the floor and to feet on the supports) 50’, 3 × week (8 weeks) – 24 sessions, conducted by physical therapists |
Pain (NRS – during activity); Shoulder Functional Performance (SPADI) Pre & Post plus follow-up |
No significant differences between groups on pain and shoulder function, at 8 and 16 weeks (P > .05) |
| Mulligan et al,49 2016, Randomized Crossover trial, USA | Subacromial impingement syndrome (Neer stage I/II), with a primary pain complaint in shoulder and/or upper arm (D or nD sides) N = 50 (21 EG, 22 CG); y: 50.8 ± 11.1 (EG), 49.4 ± 10.6 (CG); gender: 26F, 14M |
Standardized physical therapy [education, postural advice, manual therapy of upper quarter, flexibility, range of motion exercises and, possibly, corticosteroid injection] and additional rotator cuff exercises [upright: external rotation (arm in rest position); 0-30° short arc military press (progressed to long arc scapular plane elevation); internal rotation; horizontal abduction]. | Standardized physical therapy (5 sessions) as comparison, but with additionally scapular stabilization exercise: I. Shoulder protraction punch (supine) + II. Wide grip rows at shoulder level, III. Shoulder extension/scapular depression and retraction from an overhead position, IV. Shoulder retraction with both shoulders in external rotation with the elbows at the side (upright) 3 sets of 20 repetitions Progressed by increasing theraband resistance (if exercise performed correctly and easy) 3 × day, 7 × week (4 weeks, home) – 28 sessions. Only standardized physical therapy was provided by a physical therapist |
Pain (NRS – during activity); Physical symptoms and Function (ASES) Pre & Post |
No significant differences between groups on pain and shoulder function, at 4 weeks (P > .5) |
| Shah et al,69 2014, RCT, India | Shoulder impingement syndrome (ND) N = 60 (30 EG, 30 CG); y: 46.9 (EG), 47.0 (CG); gender: 29F, 31M |
Strength [shoulder flexors, extensors, external rotators, adductors and horizontal adductors (side-lying)]; stretch (pectoralis major, levator scapulae and cross-chest); wand and pendulum exercises 3 sets of 8 reps |
Same as comparison, with additionally scapular stability exercise: I. Scapular clock, II. Towel sliding, III. Lawnmower, IV. Wall push up (upright) + V. Horizontal abduction, VI. Press up plus exercise (prone) + VII. Scapular PNF with alternative weight shifting (side-lying) 3 sets of 8 reps ND 1 × day, 6 × week (4 weeks) – 24 sessions, treated at physiotherapy |
Pain (VAS - in general); Shoulder Functional Performance (SPADI) Pre & Post |
Significant differences between groups on pain and shoulder function, at 6 weeks (P < .05) |
| Turgut et al,80 2017, RCT, Turkey | Subacromial impingement, with unilateral shoulder pain lasting more than 6 weeks, with type 1 or type 2 scapular dyskinesis (D or nD sides) N = 36 (15 EG, 15 CG); y: 33.4 ± 9.3 (EG), 39.5 ± 8.2(CG); gender: 14F, 16M |
Rotator cuff strengthening resisted shoulder internal or external rotation at 0° abduction, full can and self-stretching of posterior shoulder and pectoralis minor (upright); Stretching: levator scapulae and latissimus dorsi stretching (3 sets of 5 reps, sitting) | Same as comparison, with additionally scapular stabilization exercises: I. Wall slides with squat, II. Wall push-ups plus ipsilateral leg extension, III. Lawnmower with diagonal squat, IV. Resisted scapular retraction with contralateral 1-leg squat, V. Robbery with squat (upright) 3 sets until 20 reps (strengthening) Strength exercises progressed by reps (10, 15 or 20 given movement quality, presence of pain, and fatigue) and then by heavier resistance ban[3]d 7 × week (12 weeks), weekly monitored exercise program – 84 sessions |
Pain (VAS – at rest, at night and during activity); Shoulder Functional Performance (SPADI); 3D scapular and humeral kinematic (electromagnetic tracking system) Pre & Post |
Significant differences between groups on external rotation, posterior tilt, and upward rotation, at 12 weeks (P < .05) No significant differences between groups on pain and shoulder function, at 12 weeks (P > .05) |
ASES, American Shoulder and Elbow Surgeons shoulder score; CG, control group; D, dominant side; DASH, Disabilities of the Arm, Shoulder, and Hand Questionnaire; EG, experimental group; F, female; M, male; nDS, non-dominant side; ND, not defined; NRS, numeric rating scale; Pre&post, pre and postintervention; PNF, proprioceptive neuromuscular facilitation; RCT, randomized controlled trial; reps, repetitions; SPADI, shoulder pain and disability index; SST, simple shoulder test; US, ultrasound therapy; VAS, visual analog scale; WORC, western Ontario rotator cuff index; Y, years old; D1, diagonal pattern of flexion, horizontal adduction and external rotation; TENS, transcutaneous electrical nerve stimulation.
Total sample size (n), not considering dropouts.
Quality of studies
The ROB ranged from 4 to 8 (Table II). Specifically, six studies presented high ROB,4,5,13,49,69,80 and two presented low ROB.3,25 All studies specified the eligibility criteria, were randomized, and reported both between-group differences along with point estimates and variability. Regarding the internal validity, different sources of potential bias were found, with lack of blinding of therapists4,5,13,25,49,69,80 and assessors3, 4, 5,13,25,49,69,80 as the most frequent ones.
Table II.
PEDro scores resulting from the quality assessment of the included studies.
| Study | Eligibility criteria | Random allocation | Concealed allocation | Groups similar at baseline | Blind subject | Blind therapist | Blind assessor | Follow-up (<15% dropouts) | Intention-to-treat analysis | Between-group comparison | Point measures and variability | PEDro score | Risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Akguller et al3 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 8 | L |
| Balci et al4 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 4 | H |
| Başkurt et al5 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 | H |
| Çelik13 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 | H |
| Hotta et al25 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 8 | L |
| Mulligan et al49 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5 | H |
| Shah et al69 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 4 | H |
| Turgut et al80 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 | H |
H, high; L, low; PEDro, Physiotherapy Evidence Database.
Primary outcomes
Effectiveness of scapular therapeutic exercises on shoulder pain
Postintervention short-term assessment
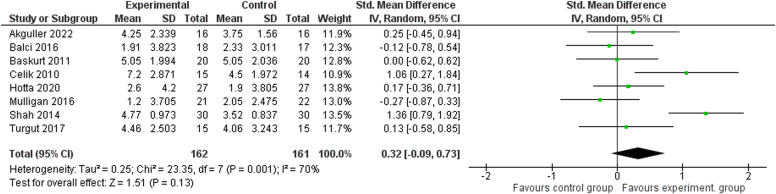
The shoulder pain intensity was assessed by all the included studies, which compared the addition of scapular therapeutic exercises with other exercises,3,5,25,49,69,80 with a multimodal intervention13 or with electrophysical modalities.4 The results of these two last studies,4,13 were analyzed narratively. According to the overall results, the addition of scapular therapeutic exercises intervention was not significantly more effective than those interventions applied to the control groups, but the heterogeneity was found to be large (SMD = 0.32 [95% Cl: −0.09, 0.73], P = .13, I2 = 70%, 323 patients total), Figure 2.
Figure 2.
Forest plot of the meta-analysis overall comparison of scapular therapeutic exercise against other types of control, regarding shoulder pain outcome at postintervention short-term assessment. SD, standard deviation; CI, confidence interval.
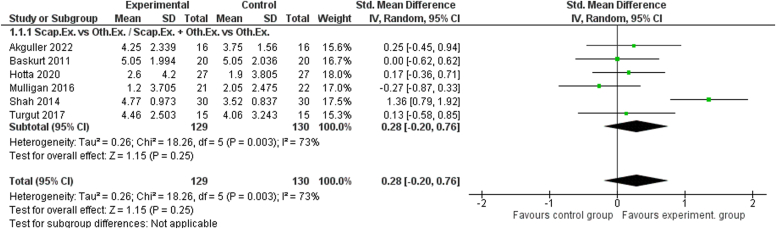
Subgroup analysis comparing scapular exercises with other exercise interventions was successfully conducted, and the combined data does not provide significant evidence for differences between both interventions regarding shoulder pain relief (SMD = 0.28 [95% Cl: −0.20, 0.76], P = .25, I2 = 73%, 259 patients total), Figure 3. The comparison of scapular exercise with electrophysical modalities4 and multimodal intervention13 were each assessed in 1 study which precluded meta-analysis interpretation. However, the first one4 does not show significant differences between groups while the second13 reported a statistically significant decrease in shoulder pain (assessed by the visual analog scales score) in the experimental group after 6 weeks of intervention (6 times/week in a total of 30 sessions).
Figure 3.
Forest plot of the meta-analysis considering subgroup comparison of scapular therapeutic exercise against other exercises, regarding shoulder pain outcome at postintervention short-term assessment. SD, standard deviation; CI, confidence interval.
Considering the mentioned heterogeneity between studies as well as the high ROB identified in some studies, a sensitivity analysis was made. Despite the exclusion of a study with high ROB69 from the subgroup of “other exercises” comparator leads to a reduction in heterogeneity (to I2 = 24% overall and 0% subgroup), the results from the pooled analysis have not been changed.
Follow-up assessment
Two studies assessed the effects of scapular therapeutic exercise, namely against other exercises intervention25 or a multimodal intervention,13 several weeks after the completion of scapular therapeutic exercises’ protocol. Both reported no differences between groups at a follow-up of 1213 or 1625 weeks after randomization.
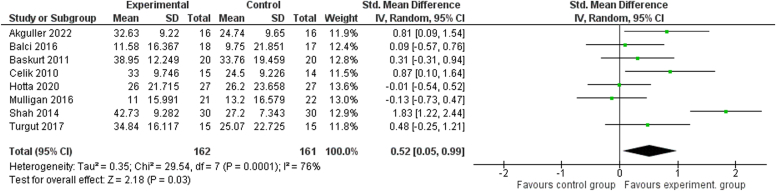
Effectiveness of scapular therapeutic exercises on shoulder function
Postintervention short-term assessment
As in shoulder pain outcome, the effect of scapular therapeutic exercises on shoulder function was assessed against other exercises,3,5,25,49,69,80 a multimodal intervention,13 or electrophysical modalities.4
Considering the overall results, adding scapular therapeutic exercises to the experimental group intervention was significantly more effective than the control group interventions (SMD = 0.52 [95%Cl: 0.05, 0.99], P = .03, I2 = 76%, 323 patients total) (Fig. 4). Despite the large heterogeneity, the results were associated with a moderate effect size.
Figure 4.
Forest plot of the meta-analysis overall comparison of scapular therapeutic exercise against other types of control, regarding shoulder function outcome at postintervention short-term assessment. SD, standard deviation; CI, confidence interval.
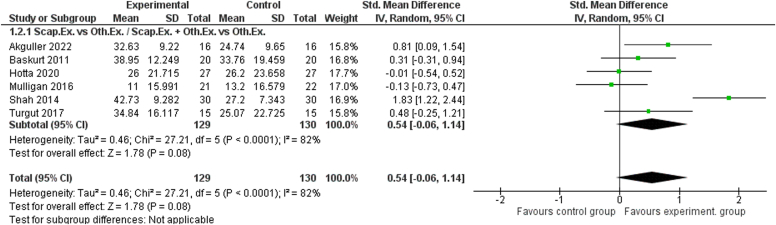
In turn, the subgroups analysis shows that the addition of scapular exercise was as effective as the other exercises intervention (SMD = 0.54 [95%Cl: −0.06, 1.14], P = .08, I2 = 82%, 259 patients total) Figure 5. Furthermore, the studies comparing scapular exercises with multimodal intervention13 or electrophysical modalities4 also reported no statistical significant differences between groups, regarding shoulder function.
Figure 5.
Forest plot of the meta-analysis considering subgroup comparison of scapular therapeutic exercise against other exercises, regarding shoulder function outcome at postintervention short-term assessment. SD, standard deviation; CI, confidence interval.
Considering the sensitivity analysis, although the maintenance of high heterogeneity, the exclusion of Celik13 or Turgut et al80 studies (high ROB), leads to different overall results (P ≥ .05, indicating no significant differences between groups).
Follow-up assessment
The comparison of scapular therapeutic exercise with a multimodal intervention13 or other exercises,25 at a time point after the completion of intervention protocols revealed no differences between groups at 1213 or 1625 weeks after randomization.
Secondary outcomes
Effectiveness of scapular therapeutic exercises on scapular motion (3D kinematics), muscular activity level, and/or muscular ratios (electromyographic data)
Turgut et al,80 a high ROB study, was the only one that assessed scapular 3D kinematics (at different humerothoracic elevation angles – 30°, 60°, 90°, and 120°). The study found significant differences between groups, indicating that the addition of multijoint scapular stabilization exercises (performed 7 times per week in a total of 84 sessions) was more effective than an intervention based on other exercises (stretching and rotator cuff strengthening) immediately after 12 weeks of intervention. Such results were expressed in the experimental group as a scapula more: a) externally rotated, an increase of 7.4-10.11°– considering all humerothoracic elevation angles; b) upwardly rotated, increased of 4.96° or 5.83° – considering humerothoracic 30° elevation and 60° lowering, respectively); and c) posteriorly tilted, an increase of 3.14-6.78° (at 12 weeks) – considering all humerothoracic elevation angles, except 120° elevation.
None of the 8 included studies3, 4, 5,13,25,49,69,80 reported data about muscular activity level or muscular ratios.
Exercise type and ways of delivering
Effectiveness of scapular therapeutic exercises considering their type and ways of delivering
The subgroup analysis, regarding exercise type and ways of delivery, was performed to identify the parameters that could be associated with higher exercise effectiveness. So, we tried to add knowledge by comparing exercise type (focal scapular exercises – when the exercise only involved movement and/or activation of the scapular structures; against multijoint exercises – exercises direct to scapula that included trunk or lower limb movements30,79 in addition to shoulder and scapular components) and ways of delivering, namely, considering exercise dose [total duration of the intervention (the duration of all the intervention protocol); weekly frequency; the maximum number of exercise repetitions (which includes the total number of repetitions done combining all the sets performed)] and progression (given the relevance of improving and/or modifying the exercises during the course of the intervention).
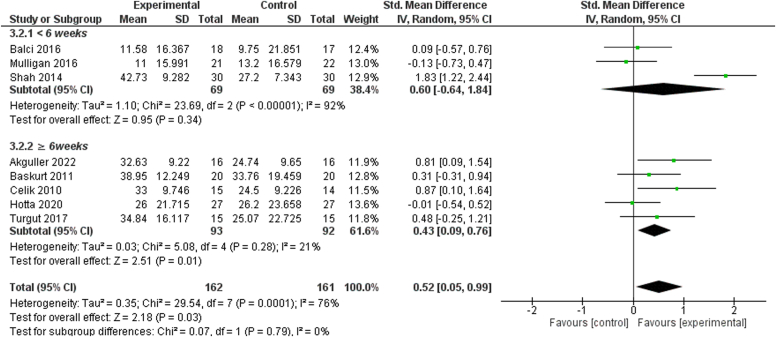
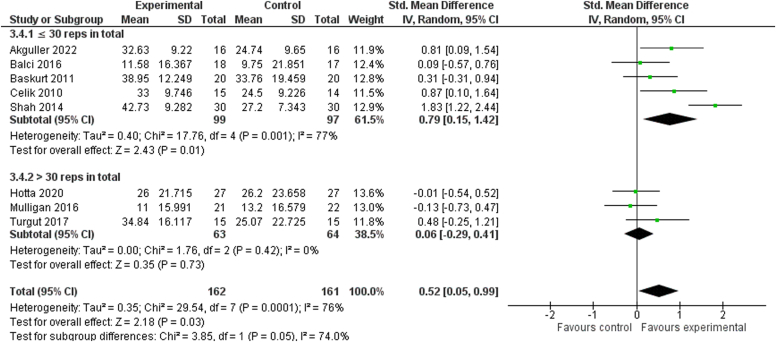
More specifically, statistical results pointed the addition of scapular therapeutic exercises, in comparison with control groups’ interventions, as more effective to improvement shoulder function when the following conditions were observed: a) the total duration of the intervention was at least of 6 weeks (SMD = 0.43 [95% Cl: 0.09, 0.76], P = .01, I2 = 21%, 185 patients total) – supported by a moderate effect size and a low heterogeneity, Figure 6; b) the maximum number of each exercise repetitions, per sessions, was not higher than 30 repetitions (SMD = 0.79 [95% Cl: 0.15, 1.42], P = .01, I2 = 77%, 196 patients total) – supported by a large effect size although the large heterogeneity, Figure 7. No other results were found considering exercise type or other ways of delivering (Supplementary Appendix C, Figures C1-C3).
Figure 6.
Forest plot of the meta-analysis considering subgroup comparison about intervention total duration, namely, comparing the execution of the scapular therapeutic exercises less than 6 weeks (<6 weeks) against 6 or more (≥6 weeks) weeks, regarding shoulder function outcome at postintervention short-term assessment. SD, standard deviation; CI, confidence interval.
Figure 7.
Forest plot of the meta-analysis considering subgroup comparison about maximum number of exercise repetitions (considering all sets performed), namely, comparing the execution of each scapular therapeutic exercise 30 or less repetitions in total (≤30 reps in total) against more than 30 repetitions in total (>30 reps in total), regarding shoulder function outcome at postintervention short-term assessment. SD, standard deviation; CI, confidence interval.
The sensitivity analysis, considering shoulder function outcome, revealed that when the study of Celik13 was excluded from the subgroups’ analysis regarding intervention total duration and maximum number of exercise repetition factors, the heterogeneity level was maintained, but the results pointed to similarity between groups (P > .05).
Considering shoulder pain outcome, the results agreed with the overall data, not allowing any recommendations regarding other exercise parameters (Supplementary Appendix C, Figures C4-C8). Despite the mentioned, the sensitivity analysis revealed that the exclusion of the study from Mulligan et al49 leads to significant results favoring the scapular therapeutic exercises group if the exercises were performed more than 3 times a week (P = .02), but maintaining the large heterogeneity (I2 = 72%). For the remaining factors, the results were consistent and robust enough to be maintained.
Discussion
Scapular adaptations, regardless its direction, the outcome40,65,74,78 and the high scapular kinematics’ variability,63 have been reported in shoulder pain conditions.4,41,74,78 Thus, several studies have included scapular exercises in their intervention protocols with the aim to restore scapular motor control and, consequently, to decrease shoulder symptomatology and improve shoulder function.50,63 With this in mind, the present meta-analysis aimed to investigate the effectiveness of scapular therapeutic exercises against other types of interventions. In terms of shoulder function, the obtained results provide evidence on the effectiveness of adding scapular therapeutic exercises. Also, the present meta-analysis aimed to identify the most effective exercise type and ways of delivering it. When considering shoulder function, it appears that performing scapular therapeutic exercises for a total duration of 6 weeks or more, along with a maximum number of each exercise repetitions (across all sets performed) not exceeding 30, yields greater benefits.
Effectiveness of scapular therapeutic exercises on primary outcomes (pain and shoulder function)
Based on 8 studies, the addition of scapular therapeutic exercises to shoulder pain rehabilitation shows an overall superior effectiveness in improving shoulder function when compared to control interventions at short term. These results, despite being based on a set of heterogeneous studies (with high to low ROB and including different comparators), were represented by a moderate effect size. Thus, it seems that the addition of scapular therapeutic exercises is beneficial for the shoulder function of patients with shoulder pain. This could possibly be related to the influence of scapular therapeutic exercise in scapula’s positioning, synchronous movement during shoulder motion5,25 and adequate motor control,49 and muscular length tension.5 The mentioned results agree with the ones from two previous systematic reviews, considering exercise effectiveness in patients with subacromial impingement syndrome.50,63 Despite all the mentioned facts, it should be noted that, according to the sensitivity analysis, 2 studies of high ROB13,80 seems to be influencing the results to a large extent, requiring their interpretation with caution. Moreover, it should be highlighted that the results of the present study could be influenced by the performance of a higher exercise volume. This is because, with the exception of the Mulligan et al49 study, scapular exercises were performed in addition to a common intervention performed by both groups.
In turn, considering shoulder pain outcome, the studies included in the present review indicate that adding scapular therapeutic exercises to shoulder pain rehabilitation is as effective as the control intervention, both at postintervention and at follow-up (12 or 16 weeks after randomization). Previous systematic reviews1,23 and meta-analysis70 reported similar findings when compared therapeutic exercise to several interventions. Despite the mentioned, it should be noted that the effectiveness of adding scapular therapeutic exercises to a multimodal intervention was verified, from a single study of high ROB,13 given the higher reduction of shoulder pain. Such results seem relevant once the difference between groups considering the pre to postintervention mean change (2.7) was higher than visual analog scales minimal clinically important differences (MCIDs = 1.4cm) to assess a shoulder pain condition.76 Thus, the presented results highlight the need for more studies regarding the effectiveness of scapular therapeutic exercise, particularly about shoulder pain outcome, which is a usual alteration seen in subjects with shoulder pain.8,36
Secondary outcomes – scapular motor control-related variables
Despite their relevance, electromyographic data regarding scapular muscular activity level and/or ratio were not found and scapular motion assessment with 3D kinematics was only identified in one study.80 Evidence from this single study,80 indicates that the addition of daily multijoint scapular stabilization exercises to a rotator cuff strengthening protocol, increase scapular external rotation (at all humerothoracic elevation angles), posterior tilt (at all humerothoracic elevation angles, except at 120° elevation), and upward rotation (at humerothoracic 30° elevation and 60° lowering) of subjects with unilateral SIS, at postintervention (12 weeks). However, not all the differences found between groups were higher than the measurement error of electromagnetic track system.22 More specifically, considering the standard measurement error, the clinically significant postintervention changes were found for: a) external rotation, at all humerothoracic levels assessed; b) upward rotation, at 30° elevation; and c) posterior tilt, at all humerothoracic elevation angles excepting 120° elevation and 90 lowering°.
The three previous systematic reviews that included studies assessing the effectiveness of therapeutic exercises for shoulder pain (not only focused on scapula) through 3D scapular kinematics,50,63,75 only found the same single study considered in the present review63 or reported no significant75 or conflicting50 findings.
The relevance of considering outcomes related to scapular structures and function, was already highlighted by previous systematic reviews64 and meta-analysis,65 which reported that more benefits could possibly be obtained if the participants’ inclusion criteria also considered scapular presentation and its relation with pain. This seems relevant once previous studies reported a variable presence of scapular dyskinesis50,80 and scapular kinematics’ alterations63 in patients with shoulder conditions, as well as a high variability considering the type of scapular kinematics’ alteration.63 In the case of the present review, only one study80 defined scapular dyskinesis types and scapular assistance or reposition tests as a criteria for eligibility.
Effectiveness of scapular therapeutic exercises considering their type and ways of delivering
The identification of the most effective exercise type and ways of delivering (dose and progression characteristics), adds knowledge about the total duration of the intervention and the maximum number of exercise repetitions, regarding shoulder function outcome. More specifically, while the use of scapular therapeutic exercises is as effective as the comparators for shoulder pain; when the protocol total duration is equal or higher than 6 weeks and/or the maximum number of each exercise repetitions are not higher than 30, the addition of scapular exercises seems to be beneficial.
The findings regarding the total duration of the intervention seem to be consistent with the knowledge regarding the adaptations induced by exercise. According to previous studies, fast changes exist considering the selection and establishment of a plan to execute a task28 or considering the increase in muscle mass (by neuromuscular and connective tissue adaptations and/or oedema).43 However, motor skill learning28,81 and other changes in musculoskeletal tissues43 require time and continued practice. More specifically, neural and muscular incremental gains associated with exercise are expected to occur until, approximately, the sixth and eighth weeks of intervention, respectively.26 Then, these gains seem to slow down or reach a plateau, and hypertrophy becomes the major gain.26 Based on the mentioned adaptations cause by exercise, it is thought that the performance of scapular therapeutic exercise during at least 6 weeks seems to benefit from most functional, neural, and muscular effects of exercises, increasing patients’ shoulder function. Moreover, the performance of regular exercise (without knowledge of the exact duration needed) could help relieve chronic pain, namely by modulating some receptors involved in the hyperalgesia processes or using the endogenous inhibitory systems.37 However, in the present study, the scapular exercise performance did not add benefits to the comparators in the reduction of shoulder pain. A previous narrative review regarding the effects of exercise in chronic pain71 and a systematic review with meta-analysis regarding the effectiveness of specific exercises for patients with SIS,70 also did not find the most appropriate dose or minimal dose needed for exercise to effective in chronic pain. In turn, consensus for physiotherapy regarding conditions of shoulder pain33,39 recommends and expects improvements with at least 12 weeks of intervention.
Considering the total number of repetitions per exercise, in previous studies it was found recommendations based on the type of exercise purpose (as resistance, flexibility, and neuromotor control)19 and not on patient pain condition or recommendations to adapt at the exercise dose according to each patient symptom response and requirements.33,39 In our study, up to 30 repetitions seemed to be a suitable dose to obtain beneficial effects for shoulder function. Possibly, the lower benefits obtained with higher repetitions could be related to a reduction in participants’ adherence to the intervention protocol, once adherence39 has been highlighted as an important factor in enhancing exercise effects. Also, the lack of time was negatively related to adherence when considering the number of exercises performed.33 However, adherence was not considered in the present review, and, therefore, future studies are required to confirm this hypothesis.
The mentioned results regarding shoulder function outcomes should be interpreted with caution once the exclusion of a study of high ROB13 seems to influence them, and should take into account the influence of the higher exercise volume performed.
Beyond the mentioned suggestion, the fact that the present meta-analysis does not support other recommendations indicates the necessity of more studies and highlights the importance of adjusting the chosen parameters to exercise goals and to each patient.33 Moreover, the lack of recommendations about the scapular exercise type (focal scapular exercises vs. multijoint), seems to agree with a previous systematic review50 which found that independently from the type of exercise performed, significant effects could be achieved, namely, changes in scapular position and movement and/or pain and disability reduction.
Strengths and limitations
The present review did not limit the search to a specific shoulder pain condition, as in the previous ones.7,9,23,63,64,65,70,83 Therefore, the conclusions are based on more studies. This decision was made since scapular changes have been reported in several shoulder conditions,41,74,78 and because recommendations regarding physiotherapy intervention highlight the relevance of making choices considering physical assessment findings instead of structural pathologies.33 Also, considering data from the studies included in the present review with meta-analysis, for both adhesive capsulitis and SIS conditions, similar scapular exercises were used for both conditions such as, for example, scapular proprioceptive neuromuscular facilitation, push-ups or scapular retraction.
In turn, some limitations were identified. First, the low quality found in some of the included studies may have limited the results of the present review with meta-analysis. Then, despite the intention of including several musculoskeletal shoulder pain conditions, the present review only found about 2 conditions,with a higher number of reports about SIS. Also, it was not possible to differentiate the results considering the chronicity of the shoulder symptoms. This is because only 4 studies3,4,25,80 defined a minimum time of pain duration as an inclusion criteria, and from them, 2 studies may have included patients with both acute or chronic conditions, once the least time of shoulder pain considered was of 125 or 680 weeks, without a limited maximum range. Considering the overall results found, the ones from the present review with meta-analysis were obtained by gathering studies that used different comparators. However, despite their differences, all control interventions were composed of procedures that a physiotherapist could use. As highlighted in the manuscript, with the exception of a crossover study, the results of the included studies may possibly be influenced by the differences in exercise volume between groups. Moreover, considering the conclusions about secondary outcomes, these were insufficient or not possible, given the lack of studies reporting them. Future studies should include these outcomes and/or other scapular-related clinical variables, namely observation or manual testing for scapular position like the ones applied in some of the included studies,2,4,5,69 not only to monitor the participants but also as an inclusion criteria.
Conclusion
The present meta-analysis revealed that the addition of scapular therapeutic exercise interventions is more effective than comparators to improve shoulder function at postintervention. It also found the benefits of adding scapular exercises to the control interventions when the protocol has a total duration of 6 or more weeks and/or when a maximum of 30 repetitions of each exercise are done.
Considering shoulder pain, the use of scapular therapeutic exercises was as effective as the comparators.
Regarding secondary outcomes, no data were found considering muscular activity level or ratios. The only study assessing scapular 3D kinematics, revealed clinically significant results such as increased scapular external rotation, posterior tilt, and, at 30° elevation, upward rotation.
Disclaimers:
Funding: This work was supported by the under Grant SFRH/BD/140874/2018 and through R&D Units funding (UIDB/05210/2020), Fundação para a Ciência e Tecnologia (FCT), Portugal. Vera Afreixo is supported in part by the Fundação para a Ciência e a Tecnologia (FCT), through CIDMA - Center for Research & Development in Mathematics and Applications, within project UIDB/04106/2020 and UIDP/ 04106/2020.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was not required for this systematic review/meta-analysis.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.xrrt.2023.12.006.
Supplementary Data
References
- 1.Abdulla S.Y., Southerst D., Côté P., Shearer H.M., Sutton D., Randhawa K., et al. Is exercise effective for the management of subacromial impingement syndrome and other soft tissue injuries of the shoulder? A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Man Ther. 2015;20:646–656. doi: 10.1016/j.math.2015.03.013. [DOI] [PubMed] [Google Scholar]
- 2.Akbaş E., Güneri S., Serkan T., Erdem E.U., Yüksel İ. The effects of additional proprioceptive neuromuscular facilitation over conventional therapy in patients with adhesive capsulitis. Turk J Physiother Rehabil. 2015;26:1–8. doi: 10.7603/s40680-015-0012-6. [DOI] [Google Scholar]
- 3.Akgüller T., Akbaba Y.A., Taşkıran H. The effect of scapular proprioceptive neuromuscular facilitation techniques on pain and functionality in patients with subacromial impingement syndrome: a randomized controlled trial. Phys Med. 2022;33:149–161. doi: 10.1055/a-1869-9195. [DOI] [Google Scholar]
- 4.Balcı N.C., Yuruk Z.O., Zeybek A., Gulsen M., Tekindal M.A. Acute effect of scapular proprioceptive neuromuscular facilitation (PNF) techniques and classic exercises in adhesive capsulitis: a randomized controlled trial. J Phys Ther Sci. 2016;28:1219–1227. doi: 10.1589/jpts.28.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Başkurt Z., Başkurt F., Gelecek N., Özkan M.H. The effectiveness of scapular stabilization exercise in the patients with subacromial impingement syndrome. J Back Musculoskelet Rehabil. 2011;24:173–179. doi: 10.3233/bmr-2011-0291. [DOI] [PubMed] [Google Scholar]
- 6.Brandt C., Sole G., Krause M.W., Nel M. An evidence-based review on the validity of the Kaltenborn rule as applied to the glenohumeral joint. Man Ther. 2007;12:3–11. doi: 10.1016/j.math.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 7.Braun C., Hanchard N.C. Manual therapy and exercise for impingementrelated shoulder pain. Phys Ther Rev. 2010;15:62–83. doi: 10.1179/174328810X12786297204675. [DOI] [Google Scholar]
- 8.Brudvig T.J., Kulkarni H., Shah S. The effect of therapeutic exercise and mobilization on patients with shoulder dysfunction : a systematic review with meta-analysis. J Orthop Sports Phys Ther. 2011;41:734–748. doi: 10.2519/jospt.2011.3440. [DOI] [PubMed] [Google Scholar]
- 9.Bury J., West M., Chamorro-Moriana G., Littlewood C. Effectiveness of scapula-focused approaches in patients with rotator cuff related shoulder pain: A systematic review and meta-analysis. Man Ther. 2016;25:35–42. doi: 10.1016/j.math.2016.05.337. [DOI] [PubMed] [Google Scholar]
- 10.Cashin A.G., McAuley J.H. Clinimetrics: Physiotherapy Evidence Database (PEDro) Scale. J Physiother. 2020;66:1–59. doi: 10.1016/j.jphys.2019.08.005. [DOI] [PubMed] [Google Scholar]
- 11.Castelein B., Cagnie B., Cools A. Scapular muscle dysfunction associated with subacromial pain syndrome. J Hand Ther. 2017;30:136–146. doi: 10.1016/j.jht.2017.03.006. [DOI] [PubMed] [Google Scholar]
- 12.Castelein B., Cagnie B., Parlevliet T., Cools A. Superficial and deep scapulothoracic muscle electromyographic activity during elevation exercises in the scapular plane. J Orthop Sports Phys Ther. 2016;46:184–193. doi: 10.2519/jospt.2016.5927. [DOI] [PubMed] [Google Scholar]
- 13.Celik D. Comparison of the outcomes of two different exercise programs on frozen shoulder. Acta Orthop Traumatol Turc. 2010;44:285–292. doi: 10.3944/aott.2010.2367. [DOI] [PubMed] [Google Scholar]
- 14.Cole A.K., McGrath M.L., Harrington S.E., Padua D.A., Rucinski T.J., Prentice W.E. Scapular bracing and alteration of posture and muscle activity in overhead athletes with poor posture. J Athl Train. 2013;48:12–24. doi: 10.4085/1062-6050-48.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cools A.M., Dewitte V., Lanszweert F., Notebaert D., Roets A., Soetens B., et al. Rehabilitation of scapular muscle balance: which exercises to prescribe? Am J Sports Med. 2007;35:1744–1751. doi: 10.1177/0363546507303560. [DOI] [PubMed] [Google Scholar]
- 16.Cortés-Pérez I., Sánchez-Alcalá M., Nieto-Escámez F.A., Castellote-Caballero Y., Obrero-Gaitán E., Osuna-Pérez M.C. Virtual reality-based therapy improves fatigue, impact, and quality of life in patients with multiple sclerosis. a systematic review with a meta-analysis. Sensors (Basel) 2021;21:7389. doi: 10.3390/s21217389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Desmeules F., Boudreault J., Dionne C.E., Frémont P., Lowry V., MacDermid J.C., et al. Efficacy of exercise therapy in workers with rotator cuff tendinopathy: a systematic review. J Occup Health. 2016;58:389–403. doi: 10.1539/joh.15-0103-RA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van den Dolder P.A., Ferreira P.H., Refshauge K.M. Effectiveness of soft tissue massage and exercise for the treatment of non-specific shoulder pain: a systematic review with meta-analysis. Br J Sports Med. 2014;48:1216–1226. doi: 10.1136/bjsports-2011-090553. [DOI] [PubMed] [Google Scholar]
- 19.Garber C.E., Blissmer B., Deschenes M.R., Franklin B.A., Lamonte M.J., Lee I.-M., et al. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 20.Gava V., Ribeiro L.P., Barreto R.P.G., Camargo P.R. Effectiveness of physical therapy given by telerehabilitation on pain and disability of individuals with shoulder pain: A systematic review. Clin Rehabil. 2022;36:715–725. doi: 10.1177/02692155221083496. [DOI] [PubMed] [Google Scholar]
- 21.Gordon C.M., Andrasik F., Schleip R., Birbaumer N., Rea M. Myofascial triggerpoint release (MTR) for treating chronic shoulder pain: A novel approach. J Bodyw Mov Ther. 2016;20:614–622. doi: 10.1016/j.jbmt.2016.01.009. [DOI] [PubMed] [Google Scholar]
- 22.Haik M.N., Alburquerque-Sendín F., Camargo P.R. Reliability and minimal detectable change of 3-dimensional scapular orientation in individuals with and without shoulder impingement. J Orthop Sports Phys Ther. 2014;44:341–349. doi: 10.2519/jospt.2014.4705. [DOI] [PubMed] [Google Scholar]
- 23.Haik M.N., Alburquerque-Sendín F., Moreira R.F., Pires E.D., Camargo P.R. Effectiveness of physical therapy treatment of clearly defined subacromial pain: a systematic review of randomised controlled trials. Br J Sports Med. 2016;50:1124–1134. doi: 10.1136/bjsports-2015-095771. [DOI] [PubMed] [Google Scholar]
- 24.Higgins J.P., Thomas J., Chandler J., Cumpston M., Li T., Page M.J., et al. 2021. Cochrane handbook for systematic reviews of interventions version 6.3. Cochrane. www.training.cochrane.org/handbook. [Google Scholar]
- 25.Hotta G.H., Gomes de Assis Couto A., Cools A.M., McQuade K.J., Siriani de Oliveira A. Effects of adding scapular stabilization exercises to a periscapular strengthening exercise program in patients with subacromial pain syndrome: A randomized controlled trial. Musculoskelet Sci Pract. 2020;49 doi: 10.1016/j.msksp.2020.102171. [DOI] [PubMed] [Google Scholar]
- 26.Jull G., Moore A., Falla D., Lewis J., McCarthy C., Sterling M. Elsevier Health Sciences; Oxford, United Kingdom: 2015. Grieve's modern musculoskeletal physiotherapy. [Google Scholar]
- 27.Kara D., Harput G., Duzgun I. Trapezius muscle activation levels and ratios during scapular retraction exercises: A comparative study between patients with subacromial impingement syndrome and healthy controls. Clin Biomech. 2019;67:119–126. doi: 10.1016/j.clinbiomech.2019.05.020. [DOI] [PubMed] [Google Scholar]
- 28.Karni A., Meyer G., Rey-Hipolito C., Jezzard P., Adams M.M., Turner R., et al. The acquisition of skilled motor performance: fast and slow experience-driven changes in primary motor cortex. Proc Natl Acad Sci U S A. 1998;95:861–868. doi: 10.1073/pnas.95.3.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kibler W.B., Ludewig P.M., McClure P.W., Michener L.A., Bak K., Sciascia A.D. Clinical implications of scapular dyskinesis in shoulder injury: the 2013 consensus statement from the ‘scapular summit’. Br J Sports Med. 2013;47:877. doi: 10.1136/bjsports-2013-092425. [DOI] [PubMed] [Google Scholar]
- 30.Kibler W.B., Sciascia A.D., Uhl T.L., Tambay N., Cunningham T. Electromyographic analysis of specific exercises for scapular control in early phases of shoulder rehabilitation. Am J Sports Med. 2008;36:1789–1798. doi: 10.1177/0363546508316281. [DOI] [PubMed] [Google Scholar]
- 31.Kibler W.B., Uhl T.L., Maddux J.W., Brooks P.V., Zeller B., McMullen J. Qualitative clinical evaluation of scapular dysfunction: a reliability study. J Shoulder Elbow Surg. 2002;11:550–556. doi: 10.1067/mse.2002.126766. [DOI] [PubMed] [Google Scholar]
- 32.Kinsella R., Pizzari T. Electromyographic activity of the shoulder muscles during rehabilitation exercises in subjects with and without subacromial pain syndrome: a systematic review. Shoulder Elbow. 2017;9:112–126. doi: 10.1177/1758573216660038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Klintberg I.H., Cools A.M., Holmgren T.M., Holzhausen A.C., Johansson K., Maenhout A.G., et al. Consensus for physiotherapy for shoulder pain. Int Orthop. 2015;39:715–720. doi: 10.1007/s00264-014-2639-9. [DOI] [PubMed] [Google Scholar]
- 34.Lefèvre-Colau M.M., Nguyen C., Palazzo C., Srour F., Paris G., Vuillemin V., et al. Kinematic patterns in normal and degenerative shoulders. Part II: Review of 3-D scapular kinematic patterns in patients with shoulder pain, and clinical implications. Ann Phys Rehabil Med. 2018;61:46–53. doi: 10.1016/j.rehab.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 35.Lempereur M., Brochard S., Leboeuf F., Remy-Neris O. Validity and reliability of 3D marker based scapular motion analysis: a systematic review. J Biomech. 2014;47:2219–2230. doi: 10.1016/j.jbiomech.2014.04.028. [DOI] [PubMed] [Google Scholar]
- 36.Lentz T.A., Barabas J.A., Day T., Bishop M.D., George S.Z. The relationship of pain intensity, physical impairment, and pain-related fear to function in patients with shoulder pathology. J Orthop Sports Phys Ther. 2009;39:270–277. doi: 10.2519/jospt.2009.2879. [DOI] [PubMed] [Google Scholar]
- 37.Lima L.V., Abner T.S.S., Sluka K.A. Does exercise increase or decrease pain? Central mechanisms underlying these two phenomena. J Physiol. 2017;595:4141–4150. doi: 10.1113/jp273355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lin J.-J., Hanten W.P., Olson S.L., Roddey T.S., Soto-quijano D.A., Lim H.K., et al. Functional activity characteristics of individuals with shoulder dysfunctions. J Electromyogr Kinesiol. 2005;15:576–586. doi: 10.1016/j.jelekin.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 39.Littlewood C., Bateman M., Connor C., Gibson J., Horsley I., Jaggi A., et al. Physiotherapists’ recommendations for examination and treatment of rotator cuff related shoulder pain: a consensus exercise. Physiother Pract Res. 2019;40:87–94. doi: 10.3233/PPR-190129. [DOI] [Google Scholar]
- 40.Ludewig P.M., Cook T.M. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000;80:276–291. [PubMed] [Google Scholar]
- 41.Ludewig P.M., Reynolds J.F. The association of scapular kinematics and glenohumeral joint pathologies. J Orthop Sports Phys Ther. 2009;39:90–104. doi: 10.2519/jospt.2009.2808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Luime J.J., Koes B.W., Hendriksen I.J., Burdorf A., Verhagen A.P., Miedema H.S., et al. Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand J Rheumatol. 2004;33:73–81. doi: 10.1080/03009740310004667. [DOI] [PubMed] [Google Scholar]
- 43.Maestroni L., Read P., Bishop C., Papadopoulos K., Suchomel T.J., Comfort P., et al. The benefits of strength training on musculoskeletal system health: practical applications for interdisciplinary care. Sports Med. 2020;50:1431–1450. doi: 10.1007/s40279-020-01309-5. [DOI] [PubMed] [Google Scholar]
- 44.Maxwell C., Robinson K., McCreesh K. Understanding shoulder pain: a qualitative evidence synthesis exploring the patient experience. Phys Ther. 2021;101 doi: 10.1093/ptj/pzaa229. [DOI] [PubMed] [Google Scholar]
- 45.Moeller C.R., Bliven K.C., Valier A.R. Scapular muscle-activation ratios in patients with shoulder injuries during functional shoulder exercises. J Athl Train. 2014;49:345–355. doi: 10.4085/1062-6050-49.3.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Moezy A., Sepehrifar S., Solaymani Dodaran M. The effects of scapular stabilization based exercise therapy on pain, posture, flexibility and shoulder mobility in patients with shoulder impingement syndrome: a controlled randomized clinical trial. Med J Islam Repub Iran. 2014;28:87. [PMC free article] [PubMed] [Google Scholar]
- 47.Morais N.V., Pascoal A.G. Scapular positioning assessment: is side-to-side comparison clinically acceptable? Man Ther. 2013;18:46–53. doi: 10.1016/j.math.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 48.de Morton N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother. 2009;55:129–133. doi: 10.1016/s0004-9514(09)70043-1. [DOI] [PubMed] [Google Scholar]
- 49.Mulligan E.P., Huang M., Dickson T., Khazzam M. The effect of axioscapular and rotator cuff exercise training sequence in patients with subacromial impingement syndrome: a randomized crossover trial. Int J Sports Phys Ther. 2016;11:94–107. [PMC free article] [PubMed] [Google Scholar]
- 50.Nodehi Moghadam A., Rahnama L., Noorizadeh Dehkordi S., Abdollahi S. Exercise therapy may affect scapular position and motion in individuals with scapular dyskinesis: a systematic review of clinical trials. J Shoulder Elbow Surg. 2020;29:e29–e36. doi: 10.1016/j.jse.2019.05.037. [DOI] [PubMed] [Google Scholar]
- 51.Noten S., Struyf F., Lluch E., D'Hoore M., Van Looveren E., Meeus M. Central pain processing in patients with shoulder pain: a review of the literature. Pain Pract. 2017;17:267–280. doi: 10.1111/papr.12502. [DOI] [PubMed] [Google Scholar]
- 52.Ogston J.B., Ludewig P.M. Differences in 3-dimensional shoulder kinematics between persons with multidirectional instability and asymptomatic controls. Am J Sports Med. 2007;35:1361–1370. doi: 10.1177/0363546507300820. [DOI] [PubMed] [Google Scholar]
- 53.Page M.J., Green S., McBain B., Surace S.J., Deitch J., Lyttle N., et al. Manual therapy and exercise for rotator cuff disease. Cochrane Database Syst Rev. 2016;2016:Cd012224. doi: 10.1002/14651858.Cd012224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Page M.J., Moher D., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160. doi: 10.1136/bmj.n160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Page M.J., O'Connor D.A., Malek M., Haas R., Beaton D., Huang H., et al. Patients' experience of shoulder disorders: a systematic review of qualitative studies for the OMERACT Shoulder Core Domain Set. Rheumatology (Oxford) 2019;58:1410–1421. doi: 10.1093/rheumatology/kez046. [DOI] [PubMed] [Google Scholar]
- 57.Paine R., Voight M.L. The role of the scapula. Int J Sports Phys Ther. 2013;8:617–629. [PMC free article] [PubMed] [Google Scholar]
- 58.Patsopoulos N.A., Evangelou E., Ioannidis J.P. Sensitivity of between-study heterogeneity in meta-analysis: proposed metrics and empirical evaluation. Int J Epidemiol. 2008;37:1148–1157. doi: 10.1093/ije/dyn065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Peek A.L., Miller C., Heneghan N.R. Thoracic manual therapy in the management of non-specific shoulder pain: a systematic review. J Man Manip Ther. 2015;23:176–187. doi: 10.1179/2042618615y.0000000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Phadke V., Camargo P., Ludewig P. Scapular and rotator cuff muscle activity during arm elevation: A review of normal function and alterations with shoulder impingement. Rev Bras Fisioter. 2009;13:1–9. doi: 10.1590/s1413-35552009005000012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pizzari T., Wickham J., Balster S., Ganderton C., Watson L. Modifying a shrug exercise can facilitate the upward rotator muscles of the scapula. Clin Biomech. 2014;29:201–205. doi: 10.1016/j.clinbiomech.2013.11.011. [DOI] [PubMed] [Google Scholar]
- 62.Rabin A., Irrgang J.J., Fitzgerald G.K., Eubanks A. The intertester reliability of the Scapular Assistance Test. J Orthop Sports Phys Ther. 2006;36:653–660. doi: 10.2519/jospt.2006.2234. [DOI] [PubMed] [Google Scholar]
- 63.Ravichandran H., Janakiraman B., Gelaw A.Y., Fisseha B., Sundaram S., Sharma H.R. Effect of scapular stabilization exercise program in patients with subacromial impingement syndrome: a systematic review. J Exerc Rehabil. 2020;16:216–226. doi: 10.12965/jer.2040256.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Reijneveld E.A., Noten S., Michener L.A., Cools A., Struyf F. Clinical outcomes of a scapular-focused treatment in patients with subacromial pain syndrome: a systematic review. Br J Sports Med. 2017;51:436–441. doi: 10.1136/bjsports-2015-095460. [DOI] [PubMed] [Google Scholar]
- 65.Saito H., Harrold M.E., Cavalheri V., McKenna L. Scapular focused interventions to improve shoulder pain and function in adults with subacromial pain: A systematic review and meta-analysis. Physiother Theory Pract. 2018;34:653–670. doi: 10.1080/09593985.2018.1423656. [DOI] [PubMed] [Google Scholar]
- 66.Salazar A.P., Pinto C., Ruschel Mossi J.V., Figueiro B., Lukrafka J.L., Pagnussat A.S. Effectiveness of static stretching positioning on post-stroke upper-limb spasticity and mobility: Systematic review with meta-analysis. Ann Phys Rehabil Med. 2019;62:274–282. doi: 10.1016/j.rehab.2018.11.004. [DOI] [PubMed] [Google Scholar]
- 67.Sanz-París A., Matía-Martín P., Martín-Palmero Á., Gómez-Candela C., Camprubi Robles M. Diabetes-specific formulas high in monounsaturated fatty acids and metabolic outcomes in patients with diabetes or hyperglycaemia. A systematic review and meta-analysis. Clin Nutr. 2020;39:3273–3282. doi: 10.1016/j.clnu.2020.02.036. [DOI] [PubMed] [Google Scholar]
- 68.Schory A., Bidinger E., Wolf J., Murray L. A systematic review of the exercises that produce optimal muscle ratios of the scapular stabilizers in normal shoulders. Int J Sports Phys Ther. 2016;11:321–336. [PMC free article] [PubMed] [Google Scholar]
- 69.Shah M., Sutaria J., Khant A. Effectiveness of scapular stability exercises in the patient with the shoulder impingement syndrome. Indian J Phys Ther. 2014;2:79–84. [Google Scholar]
- 70.Shire A.R., Stæhr T.A.B., Overby J.B., Bastholm Dahl M., Sandell Jacobsen J., Høyrup Christiansen D. Specific or general exercise strategy for subacromial impingement syndrome-does it matter? A systematic literature review and meta analysis. BMC Musculoskelet Disord. 2017;18:158. doi: 10.1186/s12891-017-1518-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Sluka K.A., Frey-Law L., Hoeger Bement M. Exercise-induced pain and analgesia? Underlying mechanisms and clinical translation. Pain. 2018;159 Suppl 1:S91–S97. doi: 10.1097/j.pain.0000000000001235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Steuri R., Sattelmayer M., Elsig S., Kolly C., Tal A., Taeymans J., et al. Effectiveness of conservative interventions including exercise, manual therapy and medical management in adults with shoulder impingement: a systematic review and meta-analysis of RCTs. Br J Sports Med. 2017;51:1340–1347. doi: 10.1136/bjsports-2016-096515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Struyf F., Lluch E., Falla D., Meeus M., Noten S., Nijs J. Influence of shoulder pain on muscle function: implications for the assessment and therapy of shoulder disorders. Eur J Appl Physiol. 2015;115:225–234. doi: 10.1007/s00421-014-3059-7. [DOI] [PubMed] [Google Scholar]
- 74.Struyf F., Nijs J., Baeyens J.P., Mottram S., Meeusen R. Scapular positioning and movement in unimpaired shoulders, shoulder impingement syndrome, and glenohumeral instability. Scand J Med Sci Sports. 2011;21:352–358. doi: 10.1111/j.1600-0838.2010.01274.x. [DOI] [PubMed] [Google Scholar]
- 75.Takeno K., Glaviano N.R., Norte G.E., Ingersoll C.D. Therapeutic interventions for scapular kinematics and disability in patients with subacromial impingement: a systematic review. J Athl Train. 2019;54:283–295. doi: 10.4085/1062-6050-309-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tashjian R.Z., Deloach J., Porucznik C.A., Powell A.P. Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J Shoulder Elbow Surg. 2009;18:927–932. doi: 10.1016/j.jse.2009.03.021. [DOI] [PubMed] [Google Scholar]
- 77.Tate A.R., McClure P.W., Kareha S., Irwin D. Effect of the Scapula Reposition Test on shoulder impingement symptoms and elevation strength in overhead athletes. J Orthop Sports Phys Ther. 2008;38:4–11. doi: 10.2519/jospt.2008.2616. [DOI] [PubMed] [Google Scholar]
- 78.Timmons M.K., Thigpen C.A., Seitz A.L., Karduna A.R., Arnold B.L., Michener L.A. Scapular kinematics and subacromial-impingement syndrome: a meta-analysis. J Sport Rehabil. 2012;21:354–370. doi: 10.1123/jsr.21.4.354. [DOI] [PubMed] [Google Scholar]
- 79.Tsuruike M., Ellenbecker T.S. Serratus anterior and lower trapezius muscle activities during multi-joint isotonic scapular exercises and isometric contractions. J Athl Train. 2015;50:199–210. doi: 10.4085/1062-6050-49.3.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Turgut E., Duzgun I., Baltaci G. Effects of scapular stabilization exercise training on scapular kinematics, disability, and pain in subacromial impingement: a randomized controlled trial. Arch Phys Med Rehabil. 2017;98:1915–1923.e3. doi: 10.1016/j.apmr.2017.05.023. [DOI] [PubMed] [Google Scholar]
- 81.Vila-Chã C., Falla D., Farina D. Motor unit behavior during submaximal contractions following six weeks of either endurance or strength training. J Appl Phys. 2010;109:1455–1466. doi: 10.1152/japplphysiol.01213.2009. [DOI] [PubMed] [Google Scholar]
- 82.Voight M.L., Thomson B.C. The role of the scapula in the rehabilitation of shoulder injuries. J Athl Train. 2000;35:364–372. [PMC free article] [PubMed] [Google Scholar]
- 83.Warby S.A., Pizzari T., Ford J.J., Hahne A.J., Watson L. The effect of exercise-based management for multidirectional instability of the glenohumeral joint: a systematic review. J Shoulder Elbow Surg. 2014;23:128–142. doi: 10.1016/j.jse.2013.08.006. [DOI] [PubMed] [Google Scholar]
- 84.Worsley P., Warner M., Mottram S., Gadola S., Veeger H.E., Hermens H., et al. Motor control retraining exercises for shoulder impingement: effects on function, muscle activation, and biomechanics in young adults. J Shoulder Elbow Surg. 2013;22:e11–e19. doi: 10.1016/j.jse.2012.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.