ABSTRACT.
Biliary taeniasis is uncommon in clinical practice. We report two cases in our hospital. The first patient was diagnosed with acute biliary pancreatitis. Endoscopic retrograde cholangiopancreatography (ERCP) showed a white, flat, segmented 1-cm-wide tapeworm drilling into the duodenal papilla that was identified as Taenia saginata. After tapeworm removal, bile duct sweeping, and anthelmintic therapy, the patient recovered uneventfully. The second patient was diagnosed with acute cholangitis and multiple stones in the common bile duct and gallbladder. Emergency ERCP showed no tapeworm in the duodenum. During a subsequent ERCP 6 days later, a flat tapeworm, also T. saginata, was identified drilling into the duodenal papilla. We review five patients cases with acute acalculous cholecystitis or cholangitis caused by T. saginata or Taenia solium, and 1 patient with T. saginata drilling into the T-tube. Taeniasis should be taken into consideration when dealing with biliary and pancreatic disease.
INTRODUCTION
Human taeniasis is a regional parasitic disease caused by the infection of Taenia solium, Taenia saginata, or Taenia asiatica, and occurs primarily in areas where people ingest undercooked beef or pork routinely.1–3 The incidence of human taeniasis ranges from 0.4 to 29.7 cases per 100,000 person-years in different areas.4,5 Humans become infected by ingesting uncooked or undercooked infected meat. In the small intestine, the scolex of the cysticercus turns out and attaches to the intestinal wall, where the cysticercus develops into an adult tapeworm in 2–4 months and subsequently resides.6 Adult Taenia tapeworms are flat, segmented, white or yellowish, ∼10 mm wide, and 1–12 m in length.1,3 With the exception of the scolex, adult tapeworms have a short neck where growth and segment differentiation occur, and a strobila composed of thousands of sexually maturing, matured, and gravid proglottids.6 The proglottids occasionally migrate to the anus and are expelled with the feces.6
Most patients with taeniasis are asymptomatic, although some may encounter mild symptoms, including nausea, abdominal pain, loss of weight, and so on. Ascaris lumbricoides is well known to be motile and usually moves from the duodenum into the biliary and pancreatic ducts, resulting in biliary and pancreatic disease.7–9 As for human taeniasis, although acute appendicitis and bowel obstruction caused by Taenia have been reported,10,11 cases of pancreatic and biliary diseases caused by Taenia are rare. In this study, we summarize the clinical characteristics of biliary taeniasis through a report of a case series in our hospital, and provide a literature review.
CASE PRESENTATION
Case 1.
A 31-year-old female presented with severe and persistent abdominal pain for 2 days. Physical examination showed that the abdomen was soft, with obvious tenderness and rebound tenderness on the whole abdomen. The patient’s white blood cell count, percentage of neutrophils, and serum C-reactive protein (CRP) concentration were increased (Table 1). The serum procalcitonin concentration was normal. Blood gas analysis indicated that arterial potential of hydrogen, partial pressure of oxygen, partial pressure of carbon dioxide, base excess, and lactate were 7.424, 65 mmHg, 24.6 mmHg, –6.8 mmol/L, and 1.84 mmol/L, respectively. The serum amylase level was elevated (4,105.88 U/L; normal range, 35–135 U/L), as was the serum lipase level (250 U/L; normal range, 13–60 U/L). The tests of liver and renal function were all normal except for a slight increase in serum bilirubin concentrations (Table 1). Computed tomography (CT) of the chest showed ground-glass opacity and consolidation in the inferior lobe of both lungs, with a small amount of bilateral pleural effusion. Abdominal CT (Figure 1A) revealed an enlarged, swollen pancreas with peripheral multifocal exudation, and a small amount of fluid accumulation. Magnetic resonance cholangiopancreatography (MRCP) showed multiple small low-signal areas in the gallbladder, although no stricture, dilatation, or calculi was found in the bile duct system. This patient was diagnosed with moderately severe acute biliary pancreatitis, and conservative therapy commenced accordingly. However, the patient experienced continuing severe abdominal pain and distention without any relief; thus, an endoscopic retrograde cholangiopancreatography (ERCP) was performed during which a white, flat, segmented 1-cm-wide tapeworm drilling into the duodenal papilla was identified (Figure 1B). The endoscopist removed the tapeworm gently from the duodenal papilla using foreign-body forceps, after which selective bile duct cannulation was achieved with the aid of the double-guidewire technique. Radiography of the bile duct showed multiple flocculent low-density shadows in the superior common bile duct (Figure 1C). Last, endoscopic nose biliary drainage (ENBD) and endoscopic retrograde pancreatic drainage were carried out successfully (Figure 1D). The patient’s symptoms were relieved. Nine days later, a second ERCP was performed to sweep the bile duct; no residual tapeworm was found.
Table 1.
Laboratory values
| Items | WBC (× 109/L) | NEUT (%) | CRP (mg/L) | TBIL (µmol/L) | DBIL (µmol/L) | ALT (U/L) | AST (U/L) | ALP (U/L) | GGT (U/L) | TBA (µmol/L) |
|---|---|---|---|---|---|---|---|---|---|---|
| Normal range | 4.0–10.0 | 45–77 | ≤5.0 | 5.1–19.0 | 1.7–6.8 | <41 | <40 | 40–150 | 11–50 | <10 |
| Case 1 | 10.53 | 89.5 | 98.21 | 25.88 | 10.9 | 8.72 | 15.36 | 56.29 | 16.37 | 1.06 |
| Case 2 | 7.92 | 81.5 | 137.33 | 33.24 | 20.07 | 117.86 | 60.16 | 647.86 | 513.18 | 14.2 |
ALP = alkaline phosphatase; ALT = alanine transaminase; AST = aspartate aminotransferase; CRP = C-reactive protein; DBIL = direct bilirubin; GGT = glutamyl transpeptidase; NEUT = neutrophil; TBA = total bile acid; TBIL = total bilirubin; WBC = white blood cell count.
Figure 1.
(A) In case 1, computed tomography showed an enlarged, swollen pancreas with peripheral multifocal exudation and a small amount of fluid accumulation (white arrows). (B) During endoscopic retrograde cholangiopancreatography, a white, flat, segmented 1-cm wide tapeworm drilling into the duodenal papilla was identified. (C) After the tapeworm was dragged out, radiography with the iodine contrast medium showed multiple flocculent, low-density shadows in the superior common bile duct (red arrow). (D) Endoscopic nose biliary drainage and endoscopic retrograde pancreatic drainage was performed first.
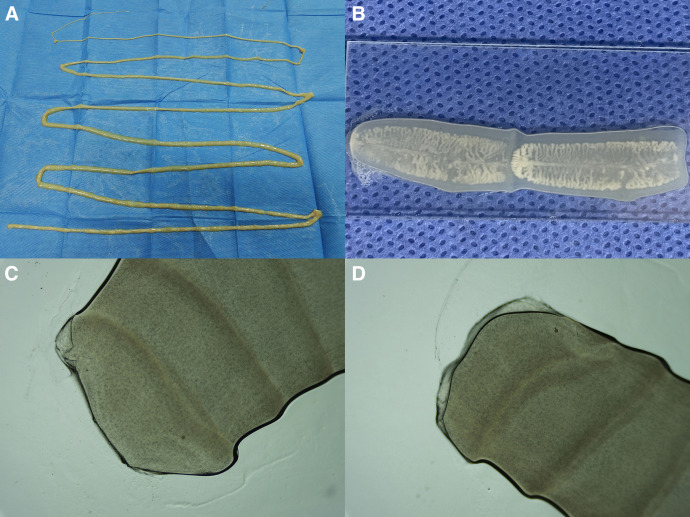
After the ERCP, the patient recalled seeing a white, flat segmented worm intermittently in her stool for the past 6 months. An episode of anthelmintic therapy was commenced by prescribing areca nuts (80 g/day), pumpkin seeds (125 g/day), and mirabilite (25 g/day) for the first 3 days, them albendazole (8 mg/kg/day) for the second 3 days. The tapeworm was identified microscopically as T. saginata (Figure 2). The patient felt well during the last follow-up 3 months later.
Figure 2.
Morphological identification of the tapeworm in case 1. The tapeworm was segmented, flat, and ∼2 m in length (A), the number of uterine branches in the gravid proglottids was ∼30 (B), and there were suckers and no rostellum or hook in the scolex (C, D). The tapeworm was identified as Taenia saginata.
Case 2.
A 73-year-old male presented with intermittent right upper quadrant pain and jaundice for 11 days. Physical examination indicated slightly yellow sclera, tenderness on the right upper abdomen, and a positive Murphy’s sign. Inflammatory indicators included an increase in the percentage of neutrophils and serum CRP concentration (Table 1). The serum liver enzymes and bilirubin concentrations were also elevated (Table 1). Abdominal CT indicated multiple high-density shadows in the gallbladder and inferior common bile duct, and the upper common bile duct was dilated. Magnetic resonance cholangiopancreatography showed multiple low-signal areas in the gallbladder, a low-signal area (1.9 × 1.4 cm) in the distal common bile duct, and secondary dilation in the superior common bile duct and hepatic bile duct. This patient was diagnosed with acute cholangitis, common bile duct stone, and multiple gallbladder stones.
Endoscopic retrograde cholangiopancreatography and ENBD was performed first, during which a low-density shadow in the common bile duct was noted; no tapeworm was seen in the duodenum or duodenal papilla (Figure 3A and B). A second ERCP was carried out 6 days later after relief of acute cholangitis. During this procedure a white, flat, segmented 1-cm-wide tapeworm was noted drilling into the duodenal papilla (Figure 3C). The tapeworm was removed gently from the duodenal papilla using foreign-body forceps, the stone was removed, and the bile duct was swept (Figure 3D). Final radiography revealed no low-density shadow. The patient admitted that a white, flat, segmented worm was seen intermittently in his stool for the past 6 months. An episode of anthelmintic therapy commenced similar to the first patient, and the tapeworm was also identified microscopically as T. saginata. The patient felt well during the last follow-up 3 years later.
Figure 3.
(A) In case 2, radiography with iodine contrast during emergency endoscopic retrograde cholangiopancreatography (ERCP) showed a low-density shadow (2.0 × 1.4 cm) in the common bile duct. (B) Endoscopic nose biliary drainage was carried out first. (C) A white, flat, segmented, 1-cm-wide tapeworm drilling into the duodenal papilla was noted during the second ERCP 6 days later. (D) The tapeworm was dragged gently out of the duodenal papilla, and the stone in the common bile duct was removed.
DISCUSSION
Human taeniasis is common in areas people habitually ingest raw or undercooked meat.1 In our study, both patients live in Tibet, where people commonly eat air-dried uncooked beef. Cattle and reindeer are the main moderate hosts for the cysticercus of T. saginata, and ingestion of uncooked beef might result in infection,1 which is consistent with our patients. Definite classification of Taenia species depends on morphological identification, immunohistological testing, and multiplex polymerase chain reaction using DNA.12,13 There are four suckers and no rostellum or hook in the scolex of T. saginata, and the number of uterine branches in the gravid proglottids reaches 18 to 32,1 which was used when identifying the Taenia species in our patients. Taenia saginata has been commonly considered harmless, but multiple cases of bowel obstruction, acute pancreatitis, acute cholangitis, acute cholecystitis, and gallbladder perforation resulting from T. saginata have been reported.11,13 Therefore, prevention and control of human taeniasis caused by T. saginata is important.
Most patients with taeniasis are asymptomatic or have nonspecific complaints such as nausea, abdominal pain, and so on. To our knowledge, biliary taeniasis is rare in clinical practice. We searched PubMed with “((Taenia[Title/Abstract]) AND ((cholecystitis[Title/Abstract]) OR (cholangitis[Title/Abstract]) OR (common bile duct[Title/Abstract]) OR (pancreatic duct[Title/Abstract]) OR (duodenal papilla[Title/Abstract]) OR (atypical localization[Title/Abstract]))) AND (English[Language])” on September 9, 2023. Ten articles were identified, four of which we excluded (three had irrelevant content and one did not contain the complete text). Thus, a total of six articles, all case reports, were eligible for literature review (Table 214–19). Of these reports, there were four cases of acute acalculous cholecystitis resulting from T. saginata or T. solium, one case of acute cholangitis caused by T. saginata, and one case of T. saginata drilling into the T-tube after cholecystectomy with a T-tube drain.14–19 We describe two patients with biliary taeniasis who presented to our institution. One had acute biliary pancreatitis caused by T. saginata; the other had T. saginata drilling into the duodenal papilla. Diagnosis of taeniasis should be taken into consideration when dealing with biliary and pancreatic diseases, especially in endemic areas.
Table 2.
Reported cases of biliary taeniasis
| No. | Year | Location | Age (year) | Sex | Habit | Taenia Species | Auxiliary Examination | Disease | Operation | Anthelmintic Therapy | Prognosis | Authors |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 1960 | Belfast, Northern Ireland, UK | 69 | Female | NA | Taenia saginata | NA | Acute pancreatitis, gallbladder stone, common bile stone, paralytic ileus | Cholecystectomy with T-tube drain | NA | NA | Logan14 |
| 2 | 1999 | Erzurum, Turkey | 35 | Female | NA | T. saginata | Muddy appearance in the gallbladder by ultrasonography | Acute acalculous cholecystitis | Cholecystectomy | NA | NA | Ozbek et al.15 |
| 3 | 2008 | Srinagar, Kashmir | 26 | Female | NA | T. saginata | Multiple echogenic, non-shadowing linear strips by ultrasonography | Acute acalculous cholecystitis | Cholecystectomy, exploration of the common bile duct | Mebendazole | NA | Malik et al.16 |
| 4 | 2012 | Srinagar, Kashmir | 32 | Male | Beef eater | T. saginata | NA | Acute acalculous cholecystitis with gallbladder perforation | Closure of perforation and cholecystostomy in emergency, interval cholecystectomy | Praziquantel | Cure | Hakeem et al.17 |
| 5 | 2012 | Istanbul, Turkey | 58 | Female | Raw-meat eater | T. saginata | Sludge in the gallbladder, dilation of the common bile duct by ultrasonography, MRCP, plaque-like structure creeping out of the sphincter of Oddi by endoscopy | Acute cholangitis | ERCP | Niclosamide | Cure | Uygur-Bayramicli et al.18 |
| 6 | 2019 | Seoul, Korea | 70 | Male | Did not eat uncooked food | Taenia solium | Hypointense linear structures within the intrahepatic and extrahepatic bile ducts by MRCP | Acute acalculous cholecystitis | Percutaneous transhepatic gallbladder drainage in emergency and laparoscopic cholecystectomy | Praziquantel | Cure | Yu et al.19 |
| 7 | 2023 | Tibet, China | 31 | Female | Uncooked air-dried beef eater | T. saginata | A white, flat, segmented 1-cm-wide tapeworm drilling into the duodenal papilla by endoscopy | Acute biliary pancreatitis | ERCP | Areca nuts, pumpkin seeds, mirabilite, albendazole | Cure | Our study |
| 8 | 2023 | Tibet, China | 73 | Male | Uncooked air-dried beef eater | T. saginata | A white, flat, segmented 1-cm-wide tapeworm drilling into the duodenal papilla by endoscopy | Acute cholangitis, common bile duct stone, gallbladder stone | ERCP | Aareca nuts, pumpkin seeds, mirabilite, albendazole | Cure | Our study |
ERCP = endoscopic retrograde cholangiopancreatography; MRCP = magnetic resonance cholangiopancreatography; NA = not applicable.
Single proglottids of Taenia expelling from the anus actively and spontaneously has occurred frequently in patients infected with T. asiatica or T. saginata, and in groups and passively in patients infected with T. solium.1 This demonstrates the motile characteristic of Taenia similar to Ascaris lumbricoides. Based on our patients, we guess that Taenia has a habit of drilling, especially T. saginata. In the human body, Taenia mainly attach to the wall of the small intestine with its scolex and then resides in the intestine.1 The similar alkalescent microenvironment of the biliary tract and the small intestine might explain why Taenia drilled into the biliary tract. Further studies exploring the pathogenesis are still needed.
Signs, including echogenic non-shadowing linear strips or a muddy appearance in the gallbladder by ultrasonography, and hypointense linear structures within the intrahepatic and extrahepatic bile ducts by MRCP, are helpful in diagnosing biliary taeniasis.15,16,18,19 However, there were no specific manifestations on CT, MRCP, and bile duct radiography in our patients, which may be because the flat, long vermicular structure of Taenia is difficult to identify. A white, flat, segmented 1-cm-wide tapeworm drilling into the duodenal papilla was seen using endoscopy, similar to the case presented by Uygur-Bayramicli et al.18 Therefore, ERCP might be applicable for the diagnosis of biliary taeniasis, especially in endemic areas.
As for the treatment of biliary taeniasis, anthelmintic therapy for T. solium, T. saginata, or T. asiatica is similar.13,20 The standard treatment options for taeniasis are praziquantel, niclosamide, and albendazole.21 The combination of pumpkin seed extract and areca—namely, ‘Qu Tao Tang’ (cestode-expelling decoction)—is a widely used traditional treatment in China.21 Surgical operations, including cholecystostomy, cholecystectomy, and common bile duct exploration were used most often to relieve inflammation and extract the tapeworm from the bile duct system.15–17,19 Taenia was extracted successfully from the bile duct system by ERCP in our patients and in the case reported by Uygur-Bayramicli et al.18 As endoscopic therapy is minimally invasive, we recommend ERCP as the first option to relieve the biliary obstruction and remove the tapeworm. If difficult, cholecystectomy and bile duct exploration are alternatives.
CONCLUSION
A diagnosis of biliary taeniasis should be kept in mind during the management of biliary and pancreatic diseases, especially in endemic areas.
REFERENCES
- 1. Ito A, Nakao M, Wandra T, 2003. Human taeniasis and cysticercosis in Asia. Lancet 362: 1918–1920. [DOI] [PubMed] [Google Scholar]
- 2. Braae UC, Thomas LF, Robertson LJ, Dermauw V, Dorny P, Willingham AL, Saratsis A, Devleesschauwer B, 2018. Epidemiology of Taenia saginata taeniasis/cysticercosis: A systematic review of the distribution in the Americas. Parasit Vectors 11: 518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Flisser A, Viniegra AE, Aguilar-Vega L, Garza-Rodriguez A, Maravilla P, Avila G, 2004. Portrait of human tapeworms. J Parasitol 90: 914–916. [DOI] [PubMed] [Google Scholar]
- 4. Krol-Pakulska E, Pakulski C, Szmid J, 2000. Evaluation of taeniasis prevalence in the area supervised by the Provincial Sanitary-Epidemiological Unit in Szczecin between 1994 and 1998. Med Sci Monit 6: 746–750. [PubMed] [Google Scholar]
- 5. Rodriguez-Morales AJ, Yepes-Echeverri MC, Acevedo-Mendoza WF, Marin-Rincon HA, Culquichicon C, Parra-Valencia E, Cardona-Ospina JA, Flisser A, 2018. Mapping the residual incidence of taeniasis and cysticercosis in Colombia, 2009–2013, using geographical information systems: Implications for public health and travel medicine. Travel Med Infect Dis 22: 51–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Schantz PM, 1996. Tapeworms (cestodiasis). Gastroenterol Clin North Am 25: 637–653. [DOI] [PubMed] [Google Scholar]
- 7. Khuroo MS, Rather AA, Khuroo NS, Khuroo MS, 2016. Hepatobiliary and pancreatic ascariasis. World J Gastroenterol 22: 7507–7517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Khuroo MS, Zargar SA, 1985. Biliary ascariasis: A common cause of biliary and pancreatic disease in an endemic area. Gastroenterology 88: 418–423. [PubMed] [Google Scholar]
- 9. Khuroo MS, Zargar SA, Mahajan R, 1990. Hepatobiliary and pancreatic ascariasis in India. Lancet 335: 1503–1506. [DOI] [PubMed] [Google Scholar]
- 10. Chakrabarti I, Gangopadhyay M, Bandopadhyay A, Das NK, 2014. A rare case of gangrenous appendicitis by eggs of Taenia species. J Parasit Dis 38: 135–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Karanikas ID, Sakellaridis TE, Alexiou CP, Siaperas PA, Fotopoulos AC, Antsaklis GI, 2007. Taenia saginata: A rare cause of bowel obstruction. Trans R Soc Trop Med Hyg 101: 527–528. [DOI] [PubMed] [Google Scholar]
- 12. Yamasaki H, Allan JC, Sato MO, Nakao M, Sako Y, Nakaya K, Qiu D, Mamuti W, Craig PS, Ito A, 2004. DNA differential diagnosis of taeniasis and cysticercosis by multiplex PCR. J Clin Microbiol 42: 548–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Qian MB, Xiao N, Li SZ, Abela-Ridder B, Carabin H, Fahrion AS, Engels D, Zhou XN, 2020. Control of taeniasis and cysticercosis in China. Adv Parasitol 110: 289–317. [DOI] [PubMed] [Google Scholar]
- 14. Logan CJ, 1960. Bizarre presentation of Taenia saginata in a T-tube draining the common bile duct. Ulster Med J 29: 142–143. [PMC free article] [PubMed] [Google Scholar]
- 15. Ozbek A, Guzel C, Babacan M, Ozbek E, 1999. An infestation due to a Taenia saginata with an atypical localization. Am J Gastroenterol 94: 1712–1713. [DOI] [PubMed] [Google Scholar]
- 16. Malik AA, Wani RA, Bari S, 2008. Acute acalculous cholecystitis due to Taenia saginata . Ann Saudi Med 28: 388–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hakeem SY, Rashid A, Khuroo S, Bali RS, 2012. Taenia saginata: A rare cause of gall bladder perforation. Case Rep Surg 2012: 572484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Uygur-Bayramicli O, Ak O, Dabak R, Demirhan G, Ozer S, 2012. Taenia saginata: A rare cause of acute cholangitis: A case report. Acta Clin Belg 67: 436–437. [DOI] [PubMed] [Google Scholar]
- 19. Yu HJ, Ahn CS, Lim S, Kim JG, Kim MS, Chae SW, Yeom JS, Joo EJ, Sohn WM, Kwon MJ, 2019. Biliary taeniasis with cholecystitis: An unusual case of Taenia solium infection with a literature review. Am J Trop Med Hyg 100: 135–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ito A, Urbani C, Jiamin Q, Vuitton DA, Dongchuan Q, Heath DD, Craig PS, Zheng F, Schantz PM, 2003. Control of echinococcosis and cysticercosis: A public health challenge to international cooperation in China. Acta Trop 86: 3–17. [DOI] [PubMed] [Google Scholar]
- 21. Zhang H, Liu C, Zheng Q, 2019. Development and application of anthelminthic drugs in China. Acta Trop 200: 105181. [DOI] [PubMed] [Google Scholar]