Abstract
Background
The International Classification of Diseases (ICD) is widely used by clinical coders worldwide for clinical coding morbidity data into administrative health databases. Accordingly, hospital data quality largely depends on the coders’ skills acquired during ICD training, which varies greatly across countries.
Objective
To characterise the current landscape of international ICD clinical coding training.
Method
An online questionnaire was created to survey the 194 World Health Organization (WHO) member countries. Questions focused on the training provided to clinical coding professionals. The survey was distributed to potential participants who met specific criteria, and to organisations specialised in the topic, such as WHO Collaborating Centres, to be forwarded to their representatives. Responses were analysed using descriptive statistics.
Results
Data from 47 respondents from 26 countries revealed disparities in all inquired topics. However, most participants reported clinical coders as the primary person assigning ICD codes. Although training was available in all countries, some did not mandate training qualifications, and those that did differed in type and duration of training, with college or university degree being most common. Clinical coding certificates most frequently entailed passing a certification exam. Most countries offered continuing training opportunities, and provided a range of support resources for clinical coders.
Conclusion
Variability in clinical coder training could affect data collection worldwide, thus potentially hindering international comparability of health data.
Implications
These findings could encourage countries to improve their resources and training programs available for clinical coders and will ultimately be valuable to the WHO for the standardisation of ICD training.
Keywords: international classification of diseases, clinical coding, health information management, education, data accuracy, data quality
Introduction
A clinical coding professional, clinical coding specialist or clinical coder (from now on referred to as ‘coder’) is the person responsible for accurately extracting clinical data from a health record and allocating a code for each condition (Walker, 2006). This process is known as ‘coding’, whereby morbidity data are coded into administrative health databases using the International Classification of Diseases (ICD). Developed by the World Health Organization Family of International Classifications (WHO-FIC), ICD is a reference standard used globally for morbidity and mortality statistics, disease monitoring, management and resource decisions, funding allocation, and public health surveillance (World Health Organization, 2021). Given the essential uses of ICD-coded administrative data, strong focus should be placed on improving the clinical coding process and the quality of coded data.
Various factors negatively affect hospital data quality (Doktorchik et al., 2020; Santos et al., 2008; So et al., 2010), particularly the education and resource supports available for coders. Coding morbidity data are a highly specialised task that requires a practical understanding of medical terminology and medical science, and an in-depth knowledge of the WHO guidelines for clinical coding (Bramley and Reid, 2007). Yet, sometimes the people assigning codes do not receive specific training. They also perform other duties beyond coding – such as quality assessment and clerical duties (McKenzie et al., 2004). Additionally, countries must upgrade coder training with every new version of ICD. Such a training upgrade occurred, when ICD-9 was transitioned to ICD-10 (Glenn, 2011; Harris et al., 2014; Rubenstein, 2014; Stanfill et al., 2014). As clinical coding quality depends mainly on the coders’ skills acquired during ICD training (Bramley and Reid, 2007), ICD implementation must emphasise education.
Although ICD is standardised internationally, ICD training is not. Previous literature explored the variations in training programs across countries to characterise the coder workforce and coder responsibilities (Bramley and Reid, 2007; McKenzie et al., 2004; Walker, 2006). Results revealed that the education that coders receive varies within and between countries. For example, formal training was not required for 10–18% of the coders in Australia, the United Kingdom and the United States (McKenzie et al., 2004). Moreover, training requirements can vary between coders working in the inpatient and outpatient settings. Although some studies focused exclusively on developed countries (Bramley and Reid, 2007; McKenzie et al., 2004), it should be noted that these articles were published between 2000 and 2010. Circumstances have changed due to the wider use of coded data. Consequently, updating these results would be instructive and enlightening for the standardisation of ICD training, which is ultimately necessary to enhance the quality of ICD-coded data.
Poor quality coded data could mislead statistical analyses, research findings and policy-making, whereas data quality is affected by multiple factors, including training, it is unknown whether differences in coders’ training might impact the quality of administrative health databases. With the overarching goal of eventually standardising ICD training globally, an online survey was created and distributed to determine the current landscape of international coder education.
Method
Detailed descriptions of the population, sampling procedure, survey design and method of distribution are available elsewhere (Otero Varela et al., 2021). In summary, an online questionnaire created to survey the WHO member countries that use ICD was distributed via SurveyMonkey® (www.surveymonkey.com, Palo Alto, California, USA). Participants were self-selected through purposive and snowball sampling; senior members of WHO-FIC Collaborating Centres (World Health Organization, 2017) and other experts in ICD clinical coding were invited to complete the survey and forward it to their peers. Survey questions were derived from a comprehensive literature review and refined during four focus groups held with field experts. The survey was translated into Spanish to increase outreach. Finally, both versions were distributed electronically via email and in person through paper cards at WHO-FIC meetings (World Health Organization, 2017).
Survey questions
The survey consisted of closed questions where participants could answer from a set of options. However, some questions would lead to an open-ended question if selecting ‘No’ or ‘Other’ for further clarification. For instance, if the participant’s country did not have clinical coding training available for the person coding, the next question would allow the participant to explain why or elaborate on their specific situation. This also applied to questions regarding the minimum training requirement, the type and length of the training, and the ICD resources available. Survey respondents shared additional information about the certificates available in their country and their requirements, as well as the organisation that awards them using a free-text box (questions No 7–9).The survey is available in Box1.
Box 1. Survey Questions and Answers (English version)
1. In what country do you currently live? Specifically, what country’s data will you be describing?
2. Do you currently use ICD (As of 1 July 2017) for coding hospital morbidity data?
○ Yes ○ No ○ I don’t know
○ If No, then how do you collect hospital morbidity data?
3. Who assigns ICD codes (codes more than 80% of cases) to the hospital morbidity data? [multiple choice]
○ Coder ○ Physician / Resident
○ Nurse ○ Statistician
○ Anyone ○ Other (please specify)
4. Is ICD coding training available for the person coding?
○ Yes ○ No ○ I don’t know ○ If No, then why not?
5. Is there a minimum training requirement before a person can assign ICD codes?
○ Yes ○ No ○ I don’t know ○ If No, then why not?
6. Please select the type and how long the minimum training requirement is for coders: [table]
○ Type [rows]:
On-the-job / College or University / Course(s) nor part of college or university
○ Length [columns]:
Less than 1 month / 1 month to 1 year / 1–2 years / Greater than 2 years
○ If not applicable chosen, is there any other training? (Please also specify the type and length of the training)
7. What certification(s) are available to the person coding? (Certification is the process of providing someone with an official document proving that they are qualified for a particular job) [free-text]
○ Please enter ‘None’ if there are no certifications.
8. For each of the certifications identified in the previous question, please select the requirements of the professional coding certification(s). [free-text and multiple choice]
○ No requirements ○ Completion of on-the-job training or coding experience
○ College or University degree ○ Completion of course(s) not part of college or university
○ Passing a certification exam ○ Other requirements (please specify)
9. What organization awards a coding certificate? [free-text]
10. Are there continuing education opportunities available to the person coding? (Continuing education is ongoing education after initial formal training or certification)
○ Yes ○ No ○ I don’t know
11. What ICD resources are available for the person to use while coding? [multiple choice]
○ ICD coding books (hardcopy or electronic document format)
○ ICD electronic coding software (electronic code searching software)
○ Encoder software (a tool that automates the complex steps a coder takes when assigning a diagnostic or procedure code)
○ Online coding query (coding questions are submitted and answered through an online portal)
○ Coding standards or guidelines (documents containing standards for coding or guidelines on how to code ICD)
○ Coding phone support line
○ Coding online chat or discussion support
○ Other (please specify)
Data Analysis
Responses were collected automatically through SurveyMonkey®, exported into an Excel file, and de-identified once the participants’ eligibility criteria were verified. Survey answers were tabulated, grouped by country to better assess the differences between them, cross-checked and cleaned. Despite divergent replies from some respondents from the same country, all answers were reported for transparency. Categorical data from closed questions were analysed using descriptive statistics (i.e. percentages). Qualitative data from Spanish open-ended questions were first translated into English and then analysed by two research team members (LOV, PM), who reviewed and agreed upon the classification of information. Consultations with other research team members were undertaken when necessary. Differences between countries were explored and assessed, and results were presented in narrative form with semi-quantitative analysis.
Ethics
The first page of the online survey included a detailed consent document describing the study, the anonymity and confidentiality of responses, and whom to contact if participants wished to withdraw or had any questions. Participants clicked on an acceptance statement to proceed with the voluntary survey, thus providing informed consent. Ethics approval was obtained from the University of Calgary Conjoint Health Research Ethics Board (ethics identification number REB17-1692).
Results
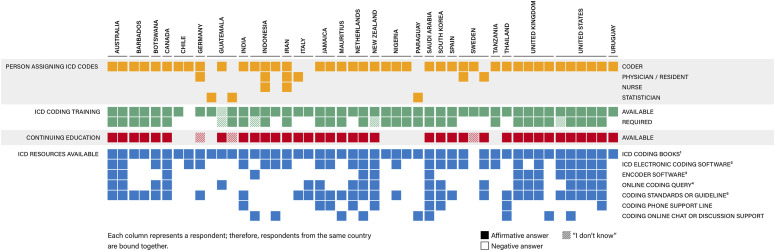
Overall, there were 47 survey respondents, some of whom were from the same country, making a total of 26 participating countries. As snowball sampling was used, the response rate was not calculated. However, the completion rate was 47/54 (87%), given that seven respondents started but did not complete the survey. All 26 participating countries that provided completed surveys used the ICD clinical coding system. Countries from all continents were represented. The geographical distribution was as follows: Europe (27.6%), North America (21.3%), Asia (17%), South America (14.9%), Africa (12.8%) and Oceania (6.4%). Respondents and specific countries are listed in Figure 1.
Figure 1.
Variations in clinical coding professionals, ICD training, and resources. 1 ICD clinical coding book (hardcopy or electronic document format); 2 ICD electronic clinical coding software (electronic code searching software); 3 Encoder software (a tool that automates the complex steps a coder takes when assigning a diagnostic or procedure code); 4 Online clinical coding query (clinical coding questions are submitted and answered through an online portal); 5 Clinical coding standards or guidelines (documents containing standards for clinical coding or guidelines on how to code ICD).
Who codes the data?
Survey results showed that 23 of the 26 countries (88%) responded to have a coder assigning ICD codes to hospital morbidity data (Figure 1). Conversely, the remaining countries identified other professionals assigning codes in most cases: Italy has physicians or residents coding; Paraguay and Guatemala use statisticians; Sweden has a 50–50 split between the coder and physician. Interestingly, some countries, for example, Indonesia, had physicians and nurses coding alongside the coder, as their national insurance scheme was transitioning.
ICD training available and required
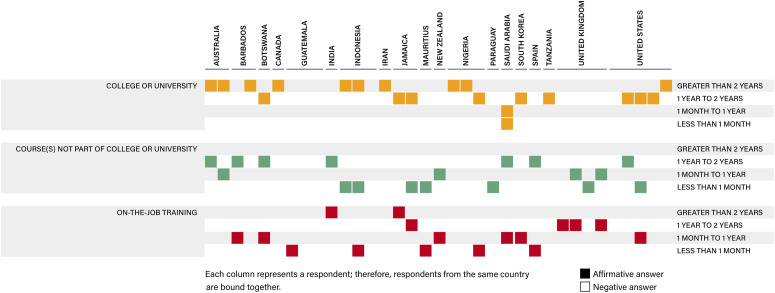
All 26 participating countries reported having training available for the professionals assigning codes. However, not all of them had requirements or regulations for training these individuals. Specifically, only 19 of the 26 countries (73%) had a minimum training requirement that the person coding must complete. As such, the type and length of the required training was examined in more detail (Figure 2). The most popular type of training reported by 63% of respondents was on-the-job training, which lasted between 1 month and 1 year. Courses not part of a college or university and being 1–2 years in duration provided 57% of training. Approximately half (52%) of the 26 countries required coders to complete a college or university program of greater than 2 years. Furthermore, 14 out of the 26 countries reported more than one-course type as required training.
Figure 2.
Type and length of required training.
Some countries did not require clinical coding skills before taking up the coding role, nor did they have national/regional standards for the coders’ training. Instead, training was locally organised or was dependent on the hospitals, such as in Sweden, Netherlands and Italy. As an example, the availability and attention paid to the training of coders in Sweden varied among the 21 regional health authorities. Although clinical coders had basic knowledge in health sciences, hospital work experience and private coding courses, physicians had no specific training for assigning codes. Similarly, although they had training available in Chile, the coder’s role was usually assigned to someone without specific training.
Certifications, requirements and awarding organisations
For this survey, certification was defined as the process of providing an official document proving that a person is qualified for a particular job. With this certification definition, 21 countries reported having clinical coding certificates available (see Table 1), along with the organisation that awards them. Of note, representatives from Spain and Australia pointed out the available graduate programs (Masters) in Health Information Management. It should also be emphasised that certifications were offered in some countries where ICD training was not required. For instance, although clinical coding training is not mandated in Uruguay, there is a university degree in Medical Registry, and in Thailand, Chile, Netherlands and Sweden, clinical coding courses are delivered by organisations specialised in the topic. The main requirement to obtain a coding certificate, as reported by survey respondents, was to ‘pass a certification exam’, usually taken after completing a high-level course in clinical coding, health information management, or health records technology. Other requirements included completing ‘a course not part of college or university’, followed by ‘a college or university degree’, and lastly, ‘an on-the-job training or coding experience’. Furthermore, most of these certificates were awarded by a post-secondary institution (university or college) and the country’s ministry of health, as well as national health information management professional associations (as reported by the respondents from Australia, Canada, Indonesia, Saudi Arabia, United Kingdom, United States and New Zealand) that are subdivisions/members of the International Federation of Health Information Management Associations (IFHIMA, 2017).
Table 1.
Coding certificates available and awarding organization.
| Country | Certification(s) available to the person coding | Organization that awards a coding certificate |
|---|---|---|
| Botswana (AF) | Diploma | — |
| Nigeria (AF) | Technician/Diploma Degree/Higher degree |
— |
| Tanzania (AF) | Certificates in Health Records Technology | - Allied Health training institute for Ministry of Health |
| Canada (NA) | College diploma/undergraduate degree Certification in Health Information Management (CHIM) |
- College or university - Canadian Health Information Management Association (CHIMA) |
| Jamaica (NA) | Associate of Science degree in Health Information Technology BSc. in Health Information Management |
- University |
| United States of America (NA) | Registered Health Information Technician Registered Health Information Administrator Certified Coding Specialist Certified Coding Specialist Physician Practice Certified Coding Associate (entry level) |
- American Health Information Management Association (AHIMA) |
| Chile* (SA) | Coding courses by RELACSIS | - Ministry of Health - Pan American Health Organization (PAHO) |
| Paraguay (SA) | Coding course from DIGIES (transl. General Direction of Strategic Health Information) Technical course from MSP-INS-MEC |
- Ministry of Public Health (MSP) - National Health Institute (INS) - Ministry of Education and Science (MEC) |
| Uruguay* (SA) | Degree in Medical Registry | - University (faculty of medicine) |
| Indonesia (AS) | Graduates of HIM or MR schools (3 years) Short courses from PORMIKI (less than 1 w) |
- Faculty or institution - The Municipality Health Department - Indonesian Professionals on Medical Record and Health Information Organization (PORMIKI) |
| Iran (AS) | University degree Clinical coding workshops |
- Medical universities - Ministry of Health |
| South Korea (AS) | National License of Health Information Management | - Ministry of Health and Welfare |
| Saudi Arabia (AS) | Certified Clinical Coder Certified Health Information Professional Certified Health Information Manager |
- Saudi Health Information Management Association (SHIMA) |
| Thailand* (AS) | Advance Level Clinical Coders | - Thai Health Coding Centre, Ministry of Public Health |
| Germany* (EU) | Health Information Manager Clinical Coder |
— |
| Netherlands* (EU) | Basic course Refresher course |
- 3 organizations: Kiwa Training, de Zorginfostraat, de Amstelacademie |
| Spain (EU) | High-level Technician in Health documentation and Administration Certified coding short courses Master in Health Information Management |
- Ministry of Education - Ministry of Health - University |
| Sweden* (EU) | Exam after 3-month course Advanced skills test |
- Coders' association (not officially recognised) |
| United Kingdom (EU) | National Clinical Coding Standards Course Certificate National Clinical Coding Qualification Clinical Coding Auditor Programme Clinical Coding Trainer Programme |
- National Health Service (NHS) Digital - Institute of Health Records and Information Management (IHRIM) |
| Australia (OC) | Statement of Attainment in Medical Records Coding Bachelor/Masters Health Information Management Certificate IV in Clinical Classification Refresher Clinical Coding |
- Technical and Further Education (TAFE) institution - Health Information Management Association of Australia (HIMAA) |
| New Zealand (OC) | Clinical Coding course (Introductory/Intermediate/Advanced) Clinical Coder Certification |
- Health Information Management Association of Australia (HIMAA) |
AF: Africa; NA: North America; SA: South America; AS: Asia; EU: Europe; OC: Oceania. * These countries have certifications available even though ICD training was not required.
Continuing training opportunities and clinical coding resources
When asked whether continuing or ongoing training opportunities were available, 36 out of 47 respondents (76.6%) answered positively, corresponding to 21 of the 26 participating countries (see Figure 1). Eight respondents (17%) specified that their country did not have ongoing education after initial formal training or certification, while three reported not knowing if their country offered continuing training was offered in their country. Some countries did not require ICD training but provided continuing education opportunities for the people coding (i.e. Indonesia, Italy, Netherlands, Sweden, Thailand and Uruguay).
Countries had varying degrees of available resources and coding supports. All 26 countries reported having ICD coding books on hand (either hardcopy or electronic), with the most updated ICD codes listed. The second most common resources used in 19 countries (73.08%) were as follows: (i) clinical coding standards or guidelines and (ii) an electronic ICD code searching software. The former is a document that guides the person coding to assign ICD codes. Conversely, the latter is a software program that enables a more efficient search of ICD codes, thus improving the productivity of the professional coder. A less popular (n = 8 countries, 30.77%) tool was the encoder software, which automates and assists the coder with the complex steps required to assign diagnostic codes. Other types of support (n = 8) included having a phone support line, an online coding query, or an online chat. These communication supports were noted to be particularly helpful when there was a considerable physical distance between the workplaces of those coding. No countries used or had all of the resources as mentioned earlier in place. Saudi Arabia reported the greatest variety of resources, followed by New Zealand, the United States and the United Kingdom. In addition to the resources suggested, respondents in Spain reported that another coding support resource was in-person consultations with a physician.
Discussion
Variability in training provided to clinical coding specialists for the use of ICD can lead to disparities in hospital morbidity data collection worldwide, thus potentially hindering comparability of international health data (Jetté et al., 2010; Otero Varela et al., 2021; Santos et al., 2008). An online questionnaire surveyed 47 participants from 26 countries to explore the differences in clinical coding training globally. Outcomes of this study showed disparities across countries in all of the topics investigated: who the coder was; whether training was available and/or mandatory; the type and length of the required training; whether certifications were available; as well as ongoing training and clinical coding resources for the person assigning codes. These results could help those looking to improve or implement a comprehensive program for ICD coders and may encourage WHO member countries to pay attention to this overlooked but relevant issue.
In accordance with previous literature, this study revealed variations between people assigning ICD codes and the training they received, resulting in a different definition of who the coder was (Walker, 2006). For instance, this role was sometimes filled by a clinical coding specialist and sometimes by a mix of professionals. In addition, given the disagreements in the requirements and regulations for clinical coding training internationally, an individual who assigns ICD codes in Barbados or Canada must undertake college-level education for a period greater than 2 years, in contrast with Chile or Sweden, where there is currently no required training. To our knowledge, it is not possible to determine which training is best or more successful, as there is no metric for training quality. Future research could address this issue and explore how coded data are impacted by alternative training approaches or even differences in training curricula. However, for consistent data, the American Health Information Management Association has highlighted the importance of following the same coding rules and conventions when assigning codes (Bielby, 2013). Therefore, standardisation in the training of clinical coding professionals would be beneficial for better comparison of hospital morbidity data.
At the same time, this also raises the issue of the extent to which standardisation is possible worldwide. First, most studies have uniformly reported that incomplete medical chart documentation was the main barrier to high-quality coded data for coders (Lucyk et al., 2017; McKenzie et al., 2004; Santos et al., 2008; Tang et al., 2017). Although documentation may be a universal barrier to high-quality clinical coding, other challenges vary depending on resources available and infrastructure (coding guidelines). As an example, not all countries reported having coding guidelines or standards (respondents from nine countries answered ‘no’). Results also showed that 19 of the 26 participating countries had electronic ICD code searching software. However, less than half of those (n = 8) had deployed an encoder software. This may relate to the readiness of countries to transition to electronic health record systems fully, and to subsequently generate health information from them (Oderkirk, 2017). Nonetheless, with the implementation of ICD-11, these concerns about resources and access to support will be lessened in the future, as the ICD-11 Reference Guide acts as a clinical coding guideline. In addition, the Coding Tool is a free code searching tool (World Health Organization, 2019).
Regardless of whether training is standardised or not, education in ICD clinical coding and feedback has proved to be successful in improving the quality of abstracting information from the medical record, especially in the countries where training was not required, such as Italy (Lorenzoni et al., 1999, 2000). This success illustrates the relevance of ongoing training, which is also beneficial considering the learning curve that coders go through when they are adjusting to a new ICD version (Martin-Vegue, 2017), or even to a national clinical modification (e.g. Australia ICD-10-AM, USA ICD-10-CM, Canada ICD-10-CA, Germany ICD-10-GM or Korea ICD-10-KM) (Hirsch et al., 2016; Jetté et al., 2010). Moreover, to improve the training that coders receive, some authors have suggested: firstly, to include the role of a coder educator (i.e. someone with comprehensive knowledge in clinical coding and a demonstrated ability to educate), for discussing clinical coding issues and enhance clinical coding skills (Bramley and Reid, 2007; Logan et al., 2003; McKenzie et al., 2004), and secondly, to take into account coders’ needs when creating a training curriculum. In respect to the latter, some areas need to be strengthened, such as specific clinical and coding topics, and technical skills (Bramley and Reid, 2007; McKenzie et al., 2004). Together with our results, these suggestions could be an incentive for countries to implement training for coders at a national level, and could be valuable for the WHO-FIC Education & Implementation Committee (EIC) when working on the development of international credentials for morbidity coders. Indeed, the WHO is launching an academy with courses designed to build and streamline clinical coding competency among the coding workforce, which might advance international training standards (World Health Organization, 2020). In addition, the EIC is working towards enhancing clinical coding quality by introducing a core curriculum for training morbidity coders (Baker et al., 2021). However, the training and language variations between countries, such as those found in our study, make these international efforts particularly challenging.
Limitations
This study had limitations mentioned elsewhere (Otero Varela et al., 2021), such as the low response rate and the non-response bias. Purposive and snowball sampling were used to reach a broad audience that resulted in all continents being represented, thus gaining a deeper understanding of coders’ training worldwide. Grouping responses geographically posed another difficulty, as answers sometimes varied among respondents from the same country. Responses from all participants were disclosed for transparency to mitigate this issue. Additionally, participants’ responses were inconsistent in a few cases (e.g. proclaiming there was no required training in a given country but later selecting the type and length of the required training). Some of these inconsistencies could be explained by the lack of standards both at international and national levels or could even be due to respondents misinterpreting the question regarding who requires the training (i.e. the government vs an employer). Thus, the reported information was revised by team members prior to its classification, and the differences between and within respondents’ reported data were appraised and thoroughly considered. Lastly, study results were limited to those reported by respondents, meaning that there might have been respondents from some countries who did not mention that certain resources were available or specific training programs (e.g. graduate education) in the free-text boxes, even if they had them.
Conclusion
Results of this study have demonstrated that although most countries had coders assigning ICD codes and training available, there was considerable variation in whether or not education was required, the type and length of training provided, and the resources available. These results have highlighted the differences in ICD coding training within and between countries and could encourage countries to improve or establish a comprehensive education program and provide supports for coders. Furthermore, given the use of the ICD classification system for international comparisons of health data, the results of the current study will be particularly valuable in highlighting the need for standardisation of clinical coder training for better quality global data.
Acknowledgements
The authors would like to acknowledge the contributions of study collaborators (Maria Santana and Daniel Cid) for their assistance with the translation of the survey into Spanish. Additionally, we would like to thank the international organizations that helped forward the online questionnaire to their representatives to reach a wider audience. These organizations are: World Health Organization Family of International Classifications (WHO-FIC) Collaborating Centres, Pan American Health Organization (PAHO), the International Federation of Health Information Management Association (IFHIMA) and RELACSIS (Red Latinoamericana y del Caribe para el fortalecimiento de los Sistemas de Salud, transl. the Latin American and Caribbean Network for the enhancement of Health Systems).
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The authors received partial financial support, provided by the Libin Cardiovascular Institute of Alberta, and the European Union’s Horizon 2020 Research and Innovation Programme under the Marie Sklodowska-Curie grant agreement No. 753816.
ORCID iDs
Lucia Otero Varela https://orcid.org/0000-0002-4406-6314
Chelsea Doktorchik https://orcid.org/0000-0003-3051-6780
Danielle Southern https://orcid.org/0000-0002-0006-0033
Søren Knudsen https://orcid.org/0000-0002-8306-1102
References
- Baker S, Guevel C, Pretty F, et al. (2021) Education and Implementation Committee Annual Report 2020-2021. WHO – Family of International Classifications network annual meeting 2021. World Health Organization, 7. Available at: https://cdn.who.int/media/docs/default-source/classification/who-fic-network/meetings/who-fic-network-virtual-annual-meeting-2021/who-fic_booklet_poster_2021.pdf?sfvrsn=bba58ef9_5. [Google Scholar]
- Bielby JA. (2013) Coding with integrity. Journal of AHIMA 84(7): 28–33. [PubMed] [Google Scholar]
- Bramley M, Reid B. (2007) Evaluation standards for clinical coder training programs. Health Information Management Journal 36(3): 21–30. [PubMed] [Google Scholar]
- Doktorchik C, Lu M, Quan H, et al. (2020) A qualitative evaluation of clinically coded data quality from health information manager perspectives. Health Information Management Journal 49(1): 19–27. [DOI] [PubMed] [Google Scholar]
- Glenn RM. (2011) Competencies and Training required by Acute Care Coders in Preparation for the Conversion to the ICD-10-CM and ICD-10-PCS Coding Classification systems. PhD Dissertation. Capella University. [Google Scholar]
- Harris ST, Zeng X, Ross T, et al. (2014) International classification of diseases, 10th revision training. The Health Care Manager 33(1): 91–93. [DOI] [PubMed] [Google Scholar]
- Hirsch JA, Nicola G, McGinty G, et al. (2016) ICD-10: history and context. AJNR American Journal of Neuroradiology 37(4): 596–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IFHIMA (2017) International Federation of Health Information Management Association. National member country listing. Available at: https://ifhima.files.wordpress.com/2017/10/national-member-country-listing-2016-2019-as-of-11-october-2017.pdf (accessed 27 Dec 2021).
- Jetté N, Quan H, Hemmelgarn B, et al. (2010) The development, evolution, and modifications of ICD-10: challenges to the international comparability of morbidity data. Medical Care 48: 1105–1110. [DOI] [PubMed] [Google Scholar]
- Logan E, O’Neill M, Martin C. (2003) Coder educator: the way forward. Health Information Management 31(2): 9–12. [DOI] [PubMed] [Google Scholar]
- Lorenzoni L, Da Cas R, Aparo U. (1999) The quality of abstracting medical information from the medical record: the impact of training programmes. International Journal for Quality in Health Care 11(3): 209–213. [DOI] [PubMed] [Google Scholar]
- Lorenzoni L, Cas RD, Aparo UL. (2000) Continuous training as a key to increase the accuracy of administrative data. Journal of Evaluation in Clinical Practice 6(4): 371–377. [DOI] [PubMed] [Google Scholar]
- Lucyk K, Tang K, Quan H. (2017) Barriers to data quality resulting from the process of coding health information to administrative data: a qualitative study. BMC Health Services Research 17(1): 766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martín-Vegue AJ. (2017) [International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM): only shadows in its implementation]. Revista de Calidad Asistencial: Organo de la Sociedad Espanola de Calidad Asistencial 32(1): 6–9. [DOI] [PubMed] [Google Scholar]
- McKenzie K, Walker SM, Dixon-Lee C, et al. (2004) Clinical coding internationally: a comparison of the coding workforce in Australia, America, Canada and England. The 14th International Federation of Health Records Organizations (IFHRO) Congress and the 76th AHIMA National Convention Proceedings. American Health Information Management Association, pp. 52–64. [Google Scholar]
- Oderkirk J. (2017). Readiness of Electronic Health Record Systems to Contribute to National Health Information and Research. OECD Library Health Working Papers 99. 10.1787/9e296bf3-en [DOI]
- Otero Varela L, Doktorchik C, Wiebe N, et al. (2021) Exploring the differences in ICD and hospital morbidity data collection features across countries: an international survey. BMC Health Services Research 21(1): 308–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubenstein J. (2014) ICD-10: are you ready? Current Urology Reports 15(11): 449. [DOI] [PubMed] [Google Scholar]
- Santos S, Murphy G, Baxter K, et al. (2008) Organisational factors affecting the quality of hospital clinical coding. Health Information Management Journal 37(1): 25–37. [DOI] [PubMed] [Google Scholar]
- So L, Beck CA, Brien S, et al. (2010) Chart documentation quality and its relationship to the validity of administrative data discharge records. Health Informatics Journal 16(2): 101–113. [DOI] [PubMed] [Google Scholar]
- Stanfill MH, Hsieh KL, Beal K, et al. (2014) Preparing for ICD-10-CM/PCS implementation: impact on productivity and quality. Perspectives in Health Information Management 11(Summer):1f. [PMC free article] [PubMed] [Google Scholar]
- Tang KL, Lucyk K, Quan H. (2017) Coder perspectives on physician-related barriers to producing high-quality administrative data: a qualitative study. CMAJ Open 5(3): E617–E622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker S. (2006) Capturing health information: a perspectives paper. Health Information Management Journal 35(3): 13–22. [DOI] [PubMed] [Google Scholar]
- World Health Organization (2017). Collaborating Centres for the WHO Family of International Classifications (WHO-FIC). Available at: http://www.who.int/classifications/network/collaborating/en/ (accessed 27 Dec 2021).
- World Health Organization (2019). ICD-11 Reference Guide. Available at: https://icd.who.int/icd11refguide/en/index.html (accessed 27 Dec 2021).
- World Health Organization (2020). 11 Training Tool and WHO Academy Course. Available at: https://score.tools.who.int/tools/count-births-deaths-and-causes-of-death/tool/icd-11-training-tool-and-who-academy-course-142/ (accessed Dec 27, 2021).
- World Health Organization (2021). International Statistical Classification of Diseases and Related Health Problems (ICD). Available at: https://www.who.int/standards/classifications/classification-of-diseases (accessed 27 Dec 2021).