Abstract
Background
Tuberculosis (TB) of CT junction is uncommon (5 % of all spinal TB), and difficult to approach surgically in view of its deep location with sternum in front and scapula in the back. We present 7 consecutively treated cases of cervico-thoraccic TB for outcome of treatment and discuss rationale of choosing surgical approach.
Methods
Present study includes 7 freshly diagnosed cases of CT junction TB. Plain radiographs, sagittal reconstruction of CT spine that included sternum on CT/MRI was performed in all cases. Disc space below the distal healthy vertebrae was identified and a line parallel to disc space was drawn. If this line passes above suprasternal notch, it was inferred that this VB can be accessed by anterior cervical approach. If disease focus was at or below suprasternal notch level, manubriotomy/sternotomy was added for better visualization of the lesion.
Results
All seven cases were female, with mean age of 20 years (9–45 years). The vertebral lesion involved 2VB (n = 3), 3VB (n = 2) and >3 VB (n = 2). The average Cervico-thoracic kyphosis was 15° (range 10–25°). All 7 cases were operated for anterior decompression, kyphotic deformity correction and instrumented stabilization. Anterior cervical approach and manubriotomy/sternotomy approach was performed in three cases each. In two pan-vertebral cases we performed 360° procedure. Six cases have shown first sign of neural recovery within 3 weeks of surgery and almost complete neural recovery at 3 months follow-up while one case showed partial recovery. ATT was stopped after 12 months once healed stage was demonstrated on contrast MRI in all.
Conclusions
CT junction TB usually presents with severe kyphotic deformity/neural deficit. These cases require anterior decompression/corpectomy, deformity correction, gap grafting and instrumented stabilization with anterior cervical plate. Lesion with pan-vertebral disease is stabilized 360°. These lesions can be decompressed by lower anterior cervical approach with/without manubriotomy. The Karikari method was useful in deciding the need for manubriotomy to decompress the lesion.
Keywords: Cervicothoracic spine TB, Surgical approaches, Spinal TB, Anterior cervical approach, Manubriotomy/sternotomy
1. Introduction
Cervico-thoracic (CT) junction of spine spans from Cervical(C)6 to Thorracic(T)3 vertebra and is inherently unstable, being a junction of lordotic mobile cervical and kyphotic, rigid thoracic spine.1,2 Tuberculosis (TB) of CT junction is uncommon (5 % of all spinal TB), and difficult to approach surgically in view of its deep location with sternum in front and scapula in the back.3 The complicated anatomical relationship by major vessels, thoracic-duct and important nerve makes it a challenging and difficult surgical exposure. The kyphotic deformity and progressive neural deficit may occur early in TB lesions. The vertebral body (VB) destruction and consequent kyphotic deformity is added to the normal thoracic kyphosis. The diameter of spinal canal in thoracic spine is small and spinal cord is close to the VB. The blood supply to spinal cord is relatively poor and thus disability rate is high.4 Hence anterior decompression, kyphotic deformity correction and instrumented stabilization is indicated and a challenge in tuberculosis affection at this region. The VB may be accessed by conventional supra-sternal anterior cervical approach or we may require manubriotomy/sternotomy/hemi sternotomy/resection of manubrio-clavicular complex besides anterior cervical approach.5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17 Addition of manubriotomy/sternotomy/hemi sternotomy/resection of manubrium-clavicular complex makes surgical exposure of cervicothoracic spine a complex procedure (see Table 1).
Table 1.
Summary of 7 operated cases of Cervicodorsal spine tuberculosis.
| Case No. | Age (yrs)/Sex | Vertebrae involved | Neurological gradea | Date of surgery | Relation of lesion with respect to Sternal notch | Surgical Approach used |
|---|---|---|---|---|---|---|
| 1 | 13/F | D1-D2 | Grade III | Jan 23, 2020 | – | Posterior instrumentation (pedicle screws & Sub laminar wiring) |
| Feb 24, 2020 | at the level of supra-sternal notch | Low anterior cervical approach + Sternotomy | ||||
| 2 | 9/F | C7-D2 | Grade IV | March 12, 2021 | below the level of supra-sternal notch | Low anterior-cervical approach + Manubriotomy |
| 3 | 20/F | C6-D1 | Grade IV | March 22, 2021 | above the level of supra-sternal notch | Low-anterior cervical approach |
| 4 | 45/F | C7-D2 | Grade IV | Sep 9, 2021 | below the level of supra-sternal notch | Low anterior cervical approach + Hemi- sternotomy |
| 5 | 23/F | C7-D1 | Grade-IV | Jan 2, 2023 | above the level of supra-sternal notch | Low anterior cervical approach |
| 6 | 10/F′ Reported after ALD done elsewhere | D2-D3 | Grade-IV | April 4, 2021 | Below the level of supra-sternal notch | Posterior stabilization followed by ALD from right side. |
| 7 | 23/F | C7,D1,D2 | Grade-IV | 2.1.20 | Extends below Supra-sternal notch | Low anterior cervical approach + Hemi-sternotomy |
ALD = Anterolateral decompression.
Kumar and Tuli's grading of tubercular paraplegia.
Few studies are described There are no well-defined rationale/method to choose surgical approach one over other in tubercular spine of cervico-thoraccic Very few articles are available in English literature on cervicothoracic TB. We hereby present the outcome in 7 prospectively, consecutively treated cases of CT TB and discuss rationale of choosing a surgical approach.
2. Materials and methods
Present study includes 7 cases (Table 1) of CT junction TB, treated between 2020 and 2023. The consent was taken to use data from the patients. All cases were freshly diagnosed C6 to D3 tuberculosis of spine which were suspected, fully investigated and treated by surgery and Antitubercular treatment (ATT). All were histologically proven cases of tuberculosis of spine (TBS). The patients with lesion extending beyond C6-D3 level were excluded. The patients suffering from prolapse discs, metastasis, primary malignant or benign tumours of spine, spinal trauma were excluded.
The plain radiographs of CT spine (AP, lateral and swimmer's views) and Computed Tomography (CT)/Magnetic Resonance Imaging (MRI) were performed. Sagittal reconstruction of CT spine that included sternum on CT/MRI was performed in all cases. Disc space below the distal healthy vertebrae was identified and a line parallel to disc space was drawn. If this line passes above suprasternal notch, it was inferred that this VB can be accessed by low anterior cervical approach. If disease focus was at or below suprasternal notch level, manubriotomy/sternotomy was required for better visualization of the lesion.14,17 The help of cardiothoracic surgeon was taken when manubriotomy/sternotomy procedure was performed.
All cases were surgically treated by anterior decompression/corpectomy, iliac crest bone grafting and instrumented stabilization with anterior cervical plate(n = 6). While in one only tricortical graft was placed. Two cases required concomitant posterior instrumentation. All the patients were treated by 2 months of Intensive phase [Rifampicin, Isoniazid, Pyrazinamide, Ethambutol (RHZE)] followed by 10 months of Continuation phase [Rifampicin, Isoniazid, Ethambutol (RHE)].
3. Surgical approaches: a) low anterior cervical approach
The patients were placed under general anaesthesia with endotracheal tube on right side in supine position with neck extended. The left-sided approach was used to avoid possibility of injuring the recurrent laryngeal nerve. An oblique incision is made starting just below the thyroid cartilage, along anterior border of Sternocleidomastoid muscle (SCM) to sternal notch. The platysma was divided in line with skin incision. The Omohyoid was transacted. SCM was retracted along with carotid sheath laterally and oesophagus with trachea towards mid-line. The prevertebral fascia with abscess was exposed and structures posterior to sternum were dissected with a finger. A retractor was placed between brachiocephalic trunk and left common carotid artery to expose prevertebral fascia of CT spine. The fascia and abscess wall were carefully incised. The decompression was performed by removing caseous necrotic tissue/sequestra and intervertebral disc. The remaining body was curetted till bleeding bone was achieved. A tricortical autogenous bone graft was harvested from iliac crest and was placed in the gap created after corpectomy.18 Anterior cervical locking plate was then applied between proximal and distal healthy vertebrae. The wound was closed in layers over a corrugated drain.
Manubriotomy Approach: The cranial part of approach is same as that of low anterior cervical approach. The caudal part of incision continued down to midline over sternum (Fig. 1). The caudal incision was deepened to pre-sternal fascia. With the help of oscillating saw, the sternum was divided. A chest retractor was placed and slowly opened. The thymus was divided between its lobes to gain access to left innominate vein, which was freed along its length to superior vena cava (SVC). The upper portion of pericardial reflection over the ascending aorta was incised and the proximal innominate artery was dissected free. With the great vessels mobilized, the aorta could be rotated to the left and SVC extracted to the patient's right.19 Vessel loops were placed around innominate artery and the left innominate vein. The prevertebral fascia/abscess wall was then freed and incised. The abscess wall was found bulging due to underlying pus. Pus drainage, anterior decompression/corpectomy was performed. The gap bone grafting by tricortical bone graft and anterior cervical plating was performed in similar manner described in low cervical approach. The sternum was reapproximated using No. 5 titanium/SS wire. The wound was closed in layers.
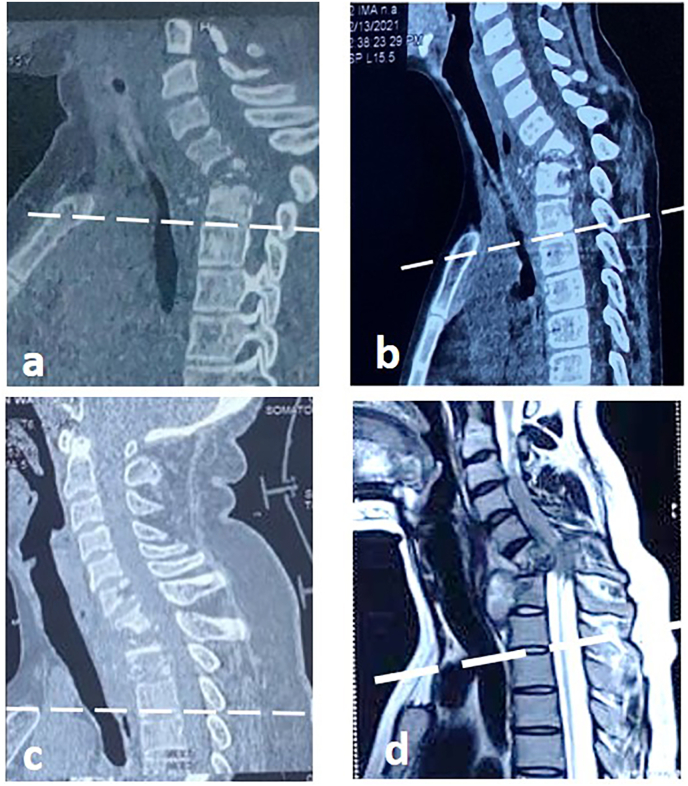
Fig. 1.
Case 2, 9 year girl presented with Grade IV paraplegia due to C7-D2 Tb spine. (a)Sagittal CT images showing the line drawn from D3-D4 using Karikari method passing below the suprasternal notch. Therefore, (b) patient underwent combination of manubriotomy and low anterior cervical approach. Debridement of the diseased vertebrae and autogenous iliac crest graft was placed in the defect and stabilized using Anterior cervical locking plate(c,d).
The tissue (pus, sequestra, granulation tissue) thus collected were sent for histopathology, AFB Smear, genotypic [Cartridge Based Nucleic Acid Amplification Test (CBNAAT), Line probe assay (LPA)] and phenotypic culture and Drug Sensitivity Testing (DST). The patients were given injection Ceftriaxone 1 gm IV twice a day for 5 days and ATT was started next day in postoperative period. They were given 2RHZE+10RHE. The ATT was modified based on TB culture report. The stitches were removed on 14th day. The patients were kept on fluid diet for 3–5 days. They were allowed solid food after 5 days. The patients were kept on Philadelphia collar (Cervico-thoracic orthosis) and a fitting ring below occiput throughout in view of complete paraplegia in all cases. Once neural recovery was achieved the patients were allowed to sit with suitable orthosis. The patients were called for follow-up at 6 weeks for two visits and then every three months for one year. On all visits patients were assessed clinically, neurologically and radiologically. ATT was stopped on demonstrating healed status on contrast MRI. Subsequently they were called for follow-up every 6 months till 2 years.
4. Results
Six out of seven cases were freshly diagnosed, investigated and treated while one patient reported to us with complications after being surgically intervened at other facility. Tuberculosis was ascertained on histology and no resistance was detected by genotypic/phenotypic DST in all.
All cases were female, with mean age of 20 years (9–45 years). All patients presented with neck pain (2–12 months) and stiffness of 2–3 months. The pain was dull aching, non-radiating, exaggerated by movements of neck and relieved by rest with night cries. None of the patients had difficulty in deglutition or torticollis. All patients reported with paraplegia (gradeIII/IV) at first attendance. Six patients reported first to us at first presentation while seventh was operated for left sided D2-D3 anterolateral decompression and reported to us after worsening of neural deficit. Mean Erythrocyte Sedimentation Rate (ESR) was 43 mm/h (28–61 mm/h). The average C- Reactive Protein (CRP) was 16.03 mg/dL (12–18.02 mg/dL). None of family members were treated by ATT before.
The plain radiographs showed diminished IV-disc spaces, destruction of para-discal margins of VB, kyphotic deformity and increased pre-vertebral soft tissue shadow in all. CT scan and MRI was performed in all 7 cases. C6, C7, D1 and D2 vertebral bodies were diseased in one, four, seven and 4 cases respectively. One of the cases had D3 disease also. Para-vertebral soft tissue shadow (representing abscess) was seen in all the seven cases. The vertebral lesion involved 2VB(n = 3), 3VB(n = 2) and >3 (n = 2). The average cervicothoracic kyphosis was 15°(range 10-25°).
CT scan sagittal reconstruction film including sternum3 showed TB lesion above suprasternal notch in three cases, hence were approached by low anterior cervical approach.6 In another three patients’ disease focus was at or below suprasternal notch level, hence manubriotomy/sternotomy was required for better visualization of the lesion16(Fig. 2). MRI showed contagious vertebral body involvement, relative preservation of disc height, prevertebral collection, septate paravertebral collection, epidural involvement suggestive of a TB lesion in all cases.
Fig. 2.
Sagittal CT/MRI films of patients of cervicothoracic Tb spine, which were used for deciding the surgical approach to diseased vertebral bodies by Karikari method. Patients a and b were accessed using anterior cervical approach with additional manubriotomy/sternotomy, however patients c and d were managed by only anterior cervical approach.
Two patients had pan-vertebral lesion. Hence in one case stage one posterior instrumentation followed by stage 2 anterior decompression and instrumented stabilization was performed. While second case had D2-D3 disease. He was operated elsewhere for left sided anterolateral decompression and developed grade IV paraplegia with flexor spasm. We first performed posterior instrumented stabilization by combing pedicle screw fixation and sublaminar wiring by Hartshill rectangle. The antero-lateral decompression and bone grafting from right side after removing second and third ribs was performed in the same sitting.
Six cases have shown first sign of neural recovery within 3 weeks of surgery and almost complete neural recovery at 3 months follow up. 7th case who reported after first surgery from somewhere had flexor spasm on presentation which gradually subsided. Although at 18 months patient was able to move their limbs albeit with severe spasticity. ATT was stopped 12 months of ATT in all once healed stage was demonstrated on contrast MRI.
5. Discussions
TB of CT junction though uncommon (<5 % of all spinal TB) but presents with kyphotic deformity and neural deficit very early in the course of disease. The diagnosis and treatment of TB is difficult in view of complex anatomy. The manubrium sternii is located in front of D2 and D3 vertebra with manubrio-sternal joint is at D4-D5. The complicated anatomical relationship of this segment of spine to major vessels, thoracic duct and important nerves make it more surgical challenging exposure and procedure.
CT junction is poorly visualized on plain radiographs in view of overlapping of shoulder, hence diagnosis of TB is usually delayed. On a lateral radiograph of CT junction, deviation of tracheal shadow more than 8–10 mm with anterior convexity is an indirect indicator of pre-vertebral collection due to disease in underlying bone.19,20 MRI in such instances have shown imaging findings suggestive of tuberculous lesion.20 We noticed this observation (Fig. 3) in all of our cases.
Fig. 3.
Demonstrating difficulty in diagnosing early Tb lesions in cervicothoracic spine due to overlapping lung shadow and thoracic cage. a and b showing Swimmer's view and lateral views of cervicothoracic spine with no gross evidence of osseous lesions, which are clearly evident on MRI scan (c). However, on vigilant evaluation of radiographs one can appreciate increased prevertebral shadow and anterior shifting of tracheal shadow in lateral xray (b).
Since this is a junction of mobile lordotic cervical spine and rigid kyphotic thoracic spine, the bio-mechanical stresses are enormous and disease focus ends in kyphosis. The retropulsed disease tissue in the spinal canal produces cord compression and consequent neural deficit. In CT junction STB, severe kyphotic deformity (disease focus kyphosis is added to normal thoracic kyphosis) and progressive neural deficit develops. In all of our cases the kyphotic deformity was present with severe grade of neural deficit. The anterior decompression, kyphosis correction and instrumented stabilization is indicated in all cases more than the other segment spinal TB. All 7 of our cases required surgery were operated for anterior decompression, kyphotic deformity correction and instrumented stabilization.
Decision to perform only anterior procedure or 360-degree procedure (1ststage posterior instrumentation followed by second stage anterior procedure) has to be taken first. In two of our cases, we performed 360-degree procedure where the lesion was pan-vertebral (lesion of both anterior and posterior column).
Various surgical approaches described for Cervico-thoracic junction are1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17,21, 22, 23, 24, 25:
-
A.
Posterior only approach: it is described and popular for thoracic and lumbar spine, where anterior VB is accessed through pedicles by posterior approach, however It is not considered a good approach at CT junction for anterior VB disease. However, it is indicated if lesion is confined only to posterior column.
-
B.
Combined anterior and posterior approach – It includes posterior fixation of vertebral column followed by anterior debridement and corpectomy and placement of bone graft with or without anterior fixation by anterior approach. Combined approach is indicated in long segment disease with 3 or more VB disease, or when both anterior and posterior column are affected by TB. It is also indicated in severe kyphotic deformity or when anterior approach may not allow placement of internal fixation. We used this in two of our case with pan-vertebral disease.
-
C.
Anterior only- This approach is indicated when damaged portion of vertebral body is in middle and anterior column of spine. Five of our cases were operated by anterior approach for anterior corpectomy, bone grafting and instrumented stabilization.
Optimal exposure of CT junction for anterior decompression and fixation needs a customized approach. For adequate exposure of vertebral body, the exposure should span the disease focus and should allow instrumented stabilization spanning proximal and distal healthy vertebrae. The various surgical approaches described are:
-
1.
Conventional supra-sternal anterior cervical approach
-
2.
Resection of the manubrio-clavicular complex
-
3.
Anterior cervical approach + Manubriotomy/Sternotomy/Hemi-sternotomy
The cervical plate is fixed over proximal/distal healthy vertebrae and tricortical bone graft is placed after corpectomy at diseased segment. Low anterior cervical approach14 can be used provided if we are able to expose one distal healthy VB. In case if full lesion and one distal healthy VB can't be exposed due to presence of manubrium sternum, we need to perform splitting of manubrium as happened in 3 of our cases. It is imperative for surgeon to know before contemplating surgery whether the surgical approach used will allow adequate exposure of disease focus to decompress and perform instrumented stabilization by conventional suprasternal anterior cervical approach or we need to split the manubrium sterni for adequate exposure.
Karikari6 took preoperative computed tomography (CT-Scan) to predict the lowest level that can be accessed with an anterior approach without the need for manubriotomy/sternotomy. On a sagittal reconstruction image of spine showing sternum was taken. Straight line passing through and parallel to the inferior disc space of distal healthy vertebral body was drawn. If the line passes above manubrium sternii than it could be inferred that the said lesion can be accessed anteriorly, decompressed and stabilized with anterior cervical plate by lower anterior cervical approach. By this we could take appropriate decision about surgical approach and 3 cases each were planned to be operated by lower cervical incision and in remaining three manubriotomy was required for adequate exposure of the lesion.
Mihir4 based on the association of the sternal notch with the most distal normal vertebra, divided the patients into 2 surgical groups. If a horizontal line is drawn over the manubrium sterni and it touches the distal normal vertebra it is a long neck and if it is at or above disease vertebra it is a short neck. He described the patients who had short necks a mandatory manubriotomy for optimal visualization and proper placement of the implant will be needed. The patients with long-necks can be operated with lower anterior cervical approach.
In three of our cases manubrium splitting was indicated as the lesion was found at or below the level of suprasternal notch. Anterior cervical platting could be performed in 6 cases by anterior lower cervical approach (n-3) and manubrium splitting approach in rest three. In one of global disease concomitant posterior stabilization was also performed. In seventh case of D2-3 disease which reported after surgical decompression by anterolateral decompression elsewhere and which has deteriorated neurologically. The spine was stabilized by posterior instrumentation and anterior gap grafting was performed after right sided anterolateral decompression.
To conclude, CT junction TB usually presents with severe kyphotic deformity/neural deficit. These cases require anterior decompression/corpectomy, deformity correction, gap grafting and instrumented stabilization with anterior cervical plate. Lesion with pan-vertebral disease is stabilized 360°. These lesions can be decompressed by lower anterior cervical approach with/without manubriotomy. The need for manubriotomy can be decided by Karikari method beforehand and is useful.
Contributor Information
Anil K. Jain, Email: dranilkjainprof@gmail.com, profakjain@gmail.com.
Ish K. Dhammi, Email: drikdhammi@gmail.com.
Rajesh Arora, Email: rajeshmamc@gmail.com.
Amartya Gain, Email: amartyagain@gmail.com.
References
- 1.Jain A.K., Kumar S., Tuli S.M. Tuberculosis of spine (C1 to D4) Spinal Cord. 1999 May;37(5):362–369. doi: 10.1038/sj.sc.3100833. PMID: 10369174. [DOI] [PubMed] [Google Scholar]
- 2.Lam F.C., Groff M.W. An anterior approach to spinal pathology of the upper thoracic spine through a partial manubriotomy. J Neurosurg Spine. 2011 Nov;15(5):467–471. doi: 10.3171/2011.6.SPINE11189. Epub 2011 Jul 22. PMID: 21780863. [DOI] [PubMed] [Google Scholar]
- 3.Morgan H., Abood C. Disc herniation at T1-2. Report of four cases and literature review. J Neurosurg. 1998;88:148–150. doi: 10.3171/jns.1998.88.1.0148. [DOI] [PubMed] [Google Scholar]
- 4.Dommissee G.F. The blood supply of the spinal cord. Acritical vascular zone in spinal surgery. Bone Joint Surg.(Br) 1974;56(2):225–235. [PubMed] [Google Scholar]
- 5.Ramani P.S., Sharma A., Jituri S., Muzumdar D.P. Anterior instrumentation for cervical spine tuberculosis: an analysis of surgical experience with 61 cases. Neurol India. 2005 Mar;53(1):83–89. doi: 10.4103/0028-3886.15067. discussion 89. PMID: 15805662. [DOI] [PubMed] [Google Scholar]
- 6.Mihir B., Vinod L., Umesh M., Chaudhary K. Anterior instrumentation of the cervicothoracic vertebrae: approach based on clinical and radiologic criteria. Spine (Phila Pa1976) 2006;31(9):E244–E249. doi: 10.1097/01.brs.0000214883.11874.80. Apr20. PMID: 16641764. [DOI] [PubMed] [Google Scholar]
- 7.Karikari I.O., Powers C.J., Isaacs R.E. Simple method for determining the need for sternotomy/manubriotomy with the anterior approach to the cervicothoracic junction. Neurosurgery. 2009 Dec;65(6 Suppl):E165–E166. doi: 10.1227/01.NEU.0000347472.07670.EB. discussion E166. PMID: 19935010. [DOI] [PubMed] [Google Scholar]
- 8.Cauchoix J., Binet J.P. Anterior surgical approaches to the spine. Ann R Coll Surg Engl. 1957;21:237–243. [PMC free article] [PubMed] [Google Scholar]
- 9.Fang H.S., Ong G.B., Hodgson A.R. Anterior spinal fusion: the operative approaches. Clin Orthop Relat Res. 1964;35:16–33. [PubMed] [Google Scholar]
- 10.Kurz L.T., Pursel S.E., Herkowitz H.N. Modified anterior approach to the cervicothoracic junction. Spine (Phila Pa 1976) 1991;16(10 Suppl):S542–S547. doi: 10.1097/00007632-199110001-00018. [DOI] [PubMed] [Google Scholar]
- 11.Lakshmanan P., Lyons K., Davies P.R., Howes J.P., Ahuja S. Radiographic assessment of sternal notch level and its significance in approaching the upper thoracic spine. Am J Orthoped. 2009;38:E71–E74. [PubMed] [Google Scholar]
- 12.Sharan A.D., Przybylski G.J., Tartaglino L. Approaching the upper thoracic vertebrae without sternotomy or thoracotomy: a radiographic analysis with clinical application. Spine (Phila Pa 1976) 2000;25:910–916. doi: 10.1097/00007632-200004150-00003. [DOI] [PubMed] [Google Scholar]
- 13.Zaveri G.R., Mehta S.S., Deshpande R. Trans-sternal approach to the cervico thoracic junction: our experience of eight cases with minimum 24-month follow-up. Coluna/Columna. 2008;7:65–70. [Google Scholar]
- 14.Kaya R.A., Turkmeno lu O.N., Koc O.N., et al. A perspective for the selection of surgical approaches in patients with upper thoracic and cervicothoracic junction instabilities. Surg Neurol. 2006;65:454–463. doi: 10.1016/j.surneu.2005.08.017. [DOI] [PubMed] [Google Scholar]
- 15.Teng H., Hsiang J., Wu C., et al. Surgery in the cervicothoracic junction with an anterior low suprasternal approach alone or combined with manubriotomy and sternotomy: an approach selection method based on the cervicothoracic angle. J Neurosurg Spine. 2009 Jun;10(6):531–542. doi: 10.3171/2009.2.SPINE08372. PMID: 19558285. [DOI] [PubMed] [Google Scholar]
- 16.Falavigna A., Righesso O., Teles A.R. Anterior approach to the cervicothoracic junction: proposed indication for manubriotomy based on preoperative computed tomography findings. J Neurosurg Spine. 2011 Jul;15(1):38–47. doi: 10.3171/2011.3.SPINE10342. Epub 2011 Apr 15. PMID: 21495813. [DOI] [PubMed] [Google Scholar]
- 17.Yin H., Wang K., Gao Y., et al. Surgical approach and management outcomes for junction tuberculous spondylitis: a retrospective study of 77 patients. J Orthop Surg Res. 2018 Dec 6;13(1):312. doi: 10.1186/s13018-018-1021-9. PMID: 30522509; PMCID: PMC6282286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee J., Paeng S.H., Lee W.H., Kim S.T., Lee K.S. Cervicothoracic junction approach using modified anterior approach: J-type manubriotomy and low cervical incision. Korean J Nutr. 2019 Apr 22;15(1):43–49. doi: 10.13004/kjnt.2019.15.e8. PMID: 31098349; PMCID: PMC6495574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jain A.K., Arora A., Kumar S., Sethi A., Avtar R. Measurement of pre-vertebral soft tissue space in an Indian Population - Indian. J Orthop. 1994;28(2):27–31. [Google Scholar]
- 20.Jain A.K., Sreenivasan R., Saini N.S., Kumar S., Jain S., Dhammi I.K. Magnetic Resonance evaluation of tubercular lesion in spine. Int Orthop. 2012 Feb;36(2):261–269. doi: 10.1007/s00264-011-1380-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhu Z., Hao D., Wang B., et al. Selection of surgical treatment approaches for cervicothoracic spinal tuberculosis: a 10-year case review. PLoS One. 2018 Feb 8;13(2) doi: 10.1371/journal.pone.0192581. PMID: 29420648; PMCID: PMC5805302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cohen Z.R., Fourney D.R., Gokaslan Z.L., Walsh G.L., Rhines L.D. Anterior stabilization of the upper thoracic spine via an "interaortocaval subinnominate window": case report and description of operative technique. J Spinal Disord Tech. 2004 Dec;17(6):543–548. doi: 10.1097/01.bsd.0000117541.10843.c9. PMID: 15570130. [DOI] [PubMed] [Google Scholar]
- 23.Babici D., Johansen P.M., Echeverry N., Mantripragada K., Miller T., Snelling B. Low anterior cervical approach without sternotomy or clavicle resection for upper thoracic vertebra corpectomy. Cureus. 2021 Nov 7;13(11) doi: 10.7759/cureus.19329. PMID: 34909292; PMCID: PMC8653864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Park J.H., Im S.B., Jeong J.H., Hwang S.C., Shin D.S., Kim B.T. The transmanubrial approach for cervicothoracic junction lesions : feasibility, limitations, and advantages. J Korean Neurosurg Soc. 2015 Sep;58(3):236–241. doi: 10.3340/jkns.2015.58.3.236. Epub 2015 Sep 30. PMID: 26539267; PMCID: PMC4630355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wu W.J., Tang Y., Lyu J.T., et al. Clinical efficacy of three surgical approaches for the treatment of cervicothoracic tuberculosis: a multicenter retrospective study. Orthop Surg. 2020 Dec;12(6):1579–1588. doi: 10.1111/os.12527. Epub 2019 Sep 30. PMID: 31568641; PMCID: PMC7767672. [DOI] [PMC free article] [PubMed] [Google Scholar]