Abstract
Objective:
The purpose of this study was to implement a 2-phase approach to rapidly increase the number of annual wellness visits (AWVs) and build a sustainable model at 3 study units (Mayo Clinic in Rochester, Minnesota, and clinics in 2 regions of Mayo Clinic Health System), which collectively serve approximately 80 000 patients who qualify for an AWV annually.
Methods:
In the rapid improvement phase, beginning in July 2022, goals at the facilities were reoriented to prioritize AWVs, educate staff on existing AWV resources, and create low-effort workflows so that AWVs could be incorporated into existing patient appointments. Staff at all 3 study units worked independently and iterated quickly. In the second phase, all study units collaborated to design and implement a best-practice solution while they leveraged the engagement and lessons learned from the first phase and invested in additional system elements and change management to codify long-term success.
Results:
The number of AWVs completed monthly increased in each study unit. In the rapid improvement phase, the number of AWVs increased but then plateaued (or decreased at some study units). In April 2023, the final scheduled outreach automation and visit tools were implemented, and the number of AWVs was sustained or increased, while outreach and scheduling times were decreased. The number of completed AWVs increased from 1148 across all study units in the first 6 months of 2022 to 14 061 during the first 6 months of 2023.
Conclusions:
The lessons learned from this project can be applied to other health systems that want to provide more patients with AWVs while improving operational efficiency. The keys are to have a clear vision of a successful outcome, engage all stakeholders, and iterate quickly to find what works best for the organization.
Keywords: annual wellness visit, population health, preventive health care, primary care, team-based care
Introduction
Annual wellness visits (AWVs) are yearly appointments that are free to Medicare patients and focus on preventive care.1,2 These visits offer an opportunity for health care professionals to address key health concerns, screen for conditions such as depression and cognitive impairment, conduct health risk assessments, ensure safety evaluations, and administer age-appropriate cancer screenings. This multifaceted approach provides insights into a patient’s current health status and potential future health conditions. 3
AWVs are distinctly different from annual physical examinations. Many health care organizations encourage physicians and advanced practice professionals (hereafter, both groups are called clinicians) to complete AWVs with the expectation that chronic and acute concerns can also be addressed during the AWV. However, because those concerns often cannot be addressed during the allotted time, that expectation can be a factor leading to clinician burnout, patient dissatisfaction, and lower completion rates for AWVs.
A solution to this is a team-based approach in which a registered nurse (RN) completes the AWV, and a separate visit with a clinician is then used to address identified health concerns, close care gaps, and allow appropriate time for advanced care planning. Traditionally, nursing and pharmacy staff have not been fully used in this manner.4 -6
At our institution, opportunities had been identified to standardize sustainable workflows to gain efficiency, improve documentation compliance, and establish an efficient staffing plan, but previous efforts to provide resources, training, and education had not been fully implemented. AWV completion rates averaged 9% at 1 of its large campuses and its health system in the year before we began this project. Our goal was to implement a 2-phase approach to rapidly increase the number of AWVs and build a sustainable model that all the practices could use.
Methods
This project was initiated at Mayo Clinic in Rochester, Minnesota, and Mayo Clinic Health System, which includes health care facilities in southern Minnesota, western Wisconsin, and northern Iowa. Mayo Clinic in Rochester, Minnesota, is a tertiary not-for-profit academic medical center. The health system is the community practice—focused branch of Mayo Clinic. The strategy and commitment of the health system is to transform rural and community health care by serving 44 communities with 16 hospitals, 46 clinics, and a mobile health clinic. These practices serve approximately 580 000 patients, and 132 000 of them qualify for an AWV each year according to their enrollment in Medicare or Medicare Advantage insurance. Among those eligible patients, the average age is 73 years and the median hierarchical condition category risk adjustment factor is 0.89. The eligible population consisted of patients with the following race or ethnicity: Asian, 1.0%; Black or African American, 1.1%; and White, 96.7%. We considered Mayo Clinic in Rochester, Minnesota, and the clinics in 2 Mayo Clinic Health System geographic regions (Southeast Minnesota and Southwest Minnesota) as 3 study units.
To improve AWV processes and completion rates, we formed a multidisciplinary project team with schedulers, RNs, clinicians, administrators, systems analysts, a project manager, and a health systems engineer. That team was led by a 3-person team (an RN, a clinician, and an administrator) that reported to the clinic’s Population Health Committee. We received support from our organization’s Practice Optimization and Acceleration group.
We used a 2-phase approach to rapidly increase AWV completion rates and build a sustainable model for the future. We considered Mayo Clinic in Rochester, Minnesota, and the clinics in 2 Mayo Clinic Health System geographic regions (Southeast Minnesota and Southwest Minnesota) as 3 study units with a total eligible patient population of 80 000.
Phase 1
In the first 3 months (July through September 2022), the rapid improvement phase, the focus was on reorienting clinic goals to make AWVs a top priority, increasing basic staff knowledge through peer-led training sessions about existing AWV resources, and creating low-effort workflows to incorporate AWVs into existing patient appointments. Initially, AWVs were scheduled as part of ongoing outreach to close care gaps and complete an annual visit for patients in our institution’s Accountable Care Organization. This work did not reach all AWV-eligible patients, and outreach attempts to patients who had not had an appointment in the previous 12 months were less likely to result in a scheduled visit.
The initial low-effort workflow was to focus on identifying patients who had upcoming appointments and were eligible for an AWV. With the use of scheduling and nursing resources, AWVs were added to these patients’ schedules before or after their existing appointments. The patients were responsive to extending their appointment times to include this added benefit.
Outcomes were monitored through weekly communication of completed and scheduled AWV counts. Workgroups met consistently to discuss patient and staff feedback and gathered suggested modifications for the phase 2 improvements.
Phase 2
Phase 2, the design and implementation of a long-term, best-practice solution phase, leveraged the engagement and lessons learned from phase 1. Participants at the study units collaborated to develop a standardized implementation model and to document guiding principles that outlined the attributes that defined a best-practice solution. These included putting the needs of the patient first, prioritizing patients who have complex medical needs, and striving for excellence through training and team-based models. Next, we defined the system elements necessary for a cohesive and comprehensive model. Workgroups were formed to design each element, and leaders in each study unit were responsible for implementation at their sites.
Six primary areas of focus were prioritized, and team members and leaders were assigned to workgroups (Figure 1). The 6 areas of focus were patient outreach and visit scheduling, visit workflow and education, communication, electronic health record (EHR) tools, metrics and data monitoring, and compliance and quality assurance. Workgroups met weekly to design, communicate, and implement new processes. A quality assurance workgroup met as needed to review eligibility reports and compliance in required documentation. To ensure alignment, project leaders held regular meetings and brought together representatives from all groups.
Figure 1.
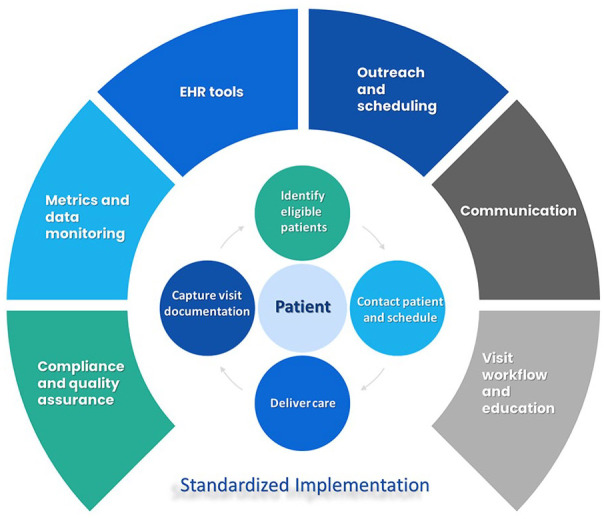
Standardized Implementation for Annual Wellness Visits. Each of the 6 outer segments represents a workgroup. The 4 inner circles revolving around the patient indicate responsibilities of the health care organization. EHR indicates electronic health record.
Identifying and prioritizing patients who were eligible for AWVs required a process that was revised many times. Finally, a health maintenance topic in the EHR was created to efficiently identify eligible patients. Importantly, the patient’s primary care clinician can also view this information, along with other preventive services, and advocate for the patient to receive an AWV.
Using the health maintenance information, we added AWVs to automated, scheduled outreach workflows that notify patients quarterly of the recommended preventive services that are due. Additionally, we developed parameters that allow patients to self-schedule their AWV before an annual appointment. These automations are a key element of a sustainable system that will support targeted manual outreach efforts with low-effort, broad outreach.
Before we could automate the self-scheduling process for patients’ AWVs, we needed to define our best-practice model for the visit, including who should complete the visit and how it should be completed. We evaluated calendar access and resource costs and determined that RNs would be the best care team members to complete the majority of AWVs, allowing them to practice to the full extent of their education and training (ie, “top-of-license”). Additionally, RN-led visits let clinicians focus on patients’ problems and make the best use of the close relationships of care teams in our institution’s care team model.
We found, though, that an RN-only AWV was often unsatisfactory for patients when they had expected a physical examination and were frustrated by not being able to have their problems addressed during the same appointment. Additionally, an RN visit could not be used to determine the patient’s chronic condition score, which must be completed by a clinician. Therefore, we proposed a dual-visit model, which would pair the RN AWV with a clinician’s physical examination to meet patient and institutional expectations. Ideally, the RN AWV would occur immediately before the visit with the clinician so that the clinician could address the patient’s concerns without extending the visit into a full preventive health screening or requiring the patient to return another day.
We standardized the duration of the RN-only AWV to 30 min to create a consistent AWV patient experience. This duration is supported by processes that streamline nursing documentation, billing, and reordering for the next year (called an EHR Express Lane). Additionally, RNs have the authority to refer patients to our institution’s online patient education classes for further education outside the visit time. We also worked with the desk staff to ensure that patients receive an electronic tablet upon check-in to complete the Health Risk Assessment before the visit if they have not already done so.
Results
Phase 1
During the first 3 months, the study units worked separately and saw substantial growth in the number of AWVs, ranging from 2 to 8 times more AWVs than in the previous quarter. However, a decrease in AWVs in the fourth quarter showed that more work was needed to sustain these improvements long-term.
With the increased focus on AWVs came a better understanding of improvements necessary for AWVs to be done consistently well and efficiently. Inconsistent documentation resulted in nonbillable appointments. Additionally, clinics needed standardized communication methods and scripts so that patients received clear, consistent information, and better tools were needed to accurately identify patients eligible for AWVs.
Phase 2
All study units substantially increased the number of AWVs completed monthly (Figure 2). An initial surge of resources and enthusiasm in summer 2022 yielded a rapid increase but then a decrease. In January 2023, enthusiasm and resources were renewed again, and another increase occurred. In April 2023, the final scheduled outreach automation and visit tools were implemented and resulted in sustained or increased volumes with large decreases in manual outreach and scheduling times. At all study units, 1148 AWVs were completed, encompassing approximately 1% of the eligible population, in the first half of 2022. In the first half of 2023, a total of 14 061 AWVs were completed, reaching 17% of the eligible population.
Figure 2.
Phased implementation of annual wellness visits (AWVs). The number of completed AWVs is shown for 3 study units.
Abbreviations: ROCH, Mayo Clinic in Rochester, Minnesota; SEMN, Mayo Clinic Health System—Southeast Minnesota region; SWMN, Mayo Clinic Health System—Southwest Minnesota region.
The median potential hierarchical condition category risk adjustment factor for patients with a completed AWV was 0.93. The race or ethnicity of patients receiving AWVs as a percentage of the total group was as follows: Asian, 0.6%; Black or African American, 0.5%; and White, 98.2%. In Rochester, Minnesota, an unmet transportation need was a factor for 1.7% of patients receiving an AWV and for 2.6% of the eligible population; a medium or high financial resource strain was a factor for 5.4% of patients receiving an AWV and for 8.0% of the eligible population.
The primary patient outcome we focused on during this pilot was the completion rate of the initial or subsequent AWV. Anecdotal patient experiences were repeatedly sought and collected to provide guidance during the implementation process. Comments submitted from patients who visited the family medicine practice at Mayo Clinic’s campus in Rochester, Minnesota, or at a Mayo Clinic Health System site in southwestern Minnesota were reviewed with the use of keyword searches for “wellness visit,” “annual visit,” and “Medicare.” Comments indicated that patients want and expect an AWV, they want to be able to schedule the visit easily, and they prefer to have the RN AWV before (rather than after) the clinician visit. Patients also indicated that they want clear communication from staff, including the persons scheduling the appointments, so they understand what an AWV entails and whether an RN or a clinician will be conducting that visit. 7
Patient participation in AWVs may affect many short- and long-term outcomes, such as receipt of vaccination, completion of age-appropriate screening tests, adoption of lifestyle behavior changes or implementation of risk-reduction strategies, hospitalization rates, and use of acute care service. Research to measure these outcomes is ongoing and beyond the scope of this article, but the importance of the research is undeniable.8 -10
Discussion
This project’s methods used a 2-phase strategy that combined rapid improvement efforts with the development of a long-term, best-practice solution. This entailed the collaboration of various health care professionals to streamline workflows, enhance documentation, and establish sustainable models for AWV delivery. The integration of automated outreach, patient identification tools, and standardized scripting further facilitated patient engagement and participation in AWVs.
Improvements were observed during the initial stages, as various study units recorded substantial increases in AWVs completed by RNs. The involvement of engaged champions and operational leadership triads bolstered accountability and quality control. The implementation of a dual-visit model, combining RN-led AWVs with clinician appointments, catered to patient expectations and delivered a more holistic health care experience.
Patient outcomes and satisfaction were central to the project’s objectives, and ongoing research is focusing on the broader effect of AWVs on health behaviors, use of health care services, and patients’ overall well-being. Patient feedback highlighted the importance of clear communication, convenient scheduling, and the seamless integration of RN-led AWVs into the patient’s health care.
Challenges
Completing AWVs to the quality required by our institution and the Centers for Medicare & Medicaid Services is not negotiable. Early on, we discovered that AWVs were missing required documentation, but the practice was not receiving regular feedback. Additionally, denied AWVs were sometimes being billed to the patient in contrast to the advertised no-charge feature of the service. We brought coding operations, revenue compliance, and practice representatives together to understand documentation requirements and rewrite our documentation template to meet requirements and include elements to identify errors. In addition, we built the billing logic into the EHR Express Lane to decrease the number of incorrectly billed visits and created a process to waive patient fees due to reimbursement denials. After making these corrections, we established ongoing data reports to monitor the number of nonbillable visits and reimbursement denials to allow quick responses if the numbers increased.
Engaged champions and accountability are necessary to maintain quality. We identified an operational leadership triad supported by a network of local “AWV champions” to support the ongoing monitoring of AWV volumes and quality and carry on the institutional knowledge. The leadership triad (a physician, an RN, and an operations proponent) is responsible for maintaining institutional AWV goals, keeping the process standardized across the study units, and identifying and implementing future improvements. The AWV champions support them as site-based experts and resources who can identify opportunities and help implement process improvements.
Lessons Learned
Our project team learned several valuable lessons through this process. Early and sustained stakeholder engagement, representing both role and geography, is necessary to arrive at optimal solutions that are acceptable to all parties. Clear delineation at the onset of standardized and required process elements (rather than nonstandardized or variable process elements) decreases confusion and disagreements among stakeholders. Local leadership support is critical to achieving meaningful, sustained implementation. Early implementation of a monitoring and feedback process can keep the implementation on track and allow for nearly real-time corrections and adjustment of the processes or tools. The patient experience should be considered throughout the design process, and patients should be engaged to identify communication gaps and other specific problems.
Conclusion
This project’s evolution underscores the pivotal role of AWVs in reshaping health care delivery, emphasizing proactive care, and contributing to healthier populations. The collaborative efforts of health care teams, supported by innovative tools and standardized processes, have laid the groundwork for a sustainable and patient-centered approach to preventive care, ultimately paving the way for a healthier future for patients. The RN-led AWV is an innovative solution that provides preventive care to patients without increasing the workload of clinicians, promotes collaboration, and allows RNs to practice to the full extent of their education and training.
Acknowledgments
Randall J. Fritz, DVM, Mayo Clinic, substantively edited the manuscript. The Scientific Publications staff at Mayo Clinic provided proofreading, administrative, and clerical support. The authors have authorized Scientific Publications to submit the manuscript on their behalf and the authors have approved all statements and declarations.
Footnotes
Author Contributions: Each author has reviewed and agreed to the content and submission of the manuscript in its current form.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Rachael C. Passmore  https://orcid.org/0009-0005-2905-0217
https://orcid.org/0009-0005-2905-0217
Taylor L. Rader  https://orcid.org/0009-0005-5485-5121
https://orcid.org/0009-0005-5485-5121
References
- 1. Colburn JL, Nothelle S. The medicare annual wellness visit. Clin Geriatr Med. 2018;34(1):1-10. doi: 10.1016/j.cger.2017.09.001 [DOI] [PubMed] [Google Scholar]
- 2. Centers for Medicare & Medicaid Services. Medicare benefit policy manual: chapter 13 - Rural Health Clinic (RHC) and Federally Qualified Health Center (FQHC) services. 2023. Accessed November 13, 2023. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/bp102c13.pdf
- 3. Patient Protection and Affordable Care Act, Pub. L. No. 111-148, (2010). [Google Scholar]
- 4. Woodall T, Landis SE, Galvin SL, Plaut T, Roth McClurg MT. Provision of annual wellness visits with comprehensive medication management by a clinical pharmacist practitioner. Am J Health Syst Pharm. 2017;74(4):218-223. doi: 10.2146/ajhp150938 [DOI] [PubMed] [Google Scholar]
- 5. Bogrett H, Carriel M. The case for utilizing RNs in medicare annual wellness visits. J Nurs Adm. 2018;48(2):75-78. doi: 10.1097/NNA.0000000000000577 [DOI] [PubMed] [Google Scholar]
- 6. Farford BA, Baggett CL, Paredes Molina CS, Ball CT, Dover CM. Impact of an RN-led medicare annual wellness visit on preventive services in a family medicine practice. J Appl Gerontol. 2021;40(8):865-871. doi: 10.1177/0733464820947928 [DOI] [PubMed] [Google Scholar]
- 7. Solinsky P, Rochester-Eyeguokan C, Brandt N, Pincus KJ. A Multicenter focus group analysis of medicare beneficiaries perception of annual wellness visits. J Healthc Qual. 2021;43(3):e33-e42. doi: 10.1097/JHQ.0000000000000273 [DOI] [PubMed] [Google Scholar]
- 8. Simpson VL, Kovich M. Outcomes of primary care-based Medicare annual wellness visits with older adults: a scoping review. Geriatr Nurs. 2019;40(6):590-596. doi: 10.1016/j.gerinurse.2019.06.001 [DOI] [PubMed] [Google Scholar]
- 9. Watkins S, Astroth KS, Kim M, Dyck MJ. Effects of Medicare wellness visits on health promotion outcomes. J Am Assoc Nurse Pract. 2023;35(2):104-111. doi: 10.1097/JXX.0000000000000795 [DOI] [PubMed] [Google Scholar]
- 10. Beckman AL, Becerra AZ, Marcus A, et al. Medicare Annual Wellness Visit association with healthcare quality and costs. Am J Manag Care. 2019;25(3):e76-e82. [PubMed] [Google Scholar]



