Abstract
RFC1 disease, caused by biallelic repeat expansion in RFC1, is clinically heterogeneous in terms of age of onset, disease progression and phenotype. We investigated the role of the repeat size in influencing clinical variables in RFC1 disease. We also assessed the presence and role of meiotic and somatic instability of the repeat.
In this study, we identified 553 patients carrying biallelic RFC1 expansions and measured the repeat expansion size in 392 cases. Pearson’s coefficient was calculated to assess the correlation between the repeat size and age at disease onset. A Cox model with robust cluster standard errors was adopted to describe the effect of repeat size on age at disease onset, on age at onset of each individual symptoms, and on disease progression. A quasi-Poisson regression model was used to analyse the relationship between phenotype and repeat size. We performed multivariate linear regression to assess the association of the repeat size with the degree of cerebellar atrophy. Meiotic stability was assessed by Southern blotting on first-degree relatives of 27 probands. Finally, somatic instability was investigated by optical genome mapping on cerebellar and frontal cortex and unaffected peripheral tissue from four post-mortem cases.
A larger repeat size of both smaller and larger allele was associated with an earlier age at neurological onset [smaller allele hazard ratio (HR) = 2.06, P < 0.001; larger allele HR = 1.53, P < 0.001] and with a higher hazard of developing disabling symptoms, such as dysarthria or dysphagia (smaller allele HR = 3.40, P < 0.001; larger allele HR = 1.71, P = 0.002) or loss of independent walking (smaller allele HR = 2.78, P < 0.001; larger allele HR = 1.60; P < 0.001) earlier in disease course. Patients with more complex phenotypes carried larger expansions [smaller allele: complex neuropathy rate ratio (RR) = 1.30, P = 0.003; cerebellar ataxia, neuropathy and vestibular areflexia syndrome (CANVAS) RR = 1.34, P < 0.001; larger allele: complex neuropathy RR = 1.33, P = 0.008; CANVAS RR = 1.31, P = 0.009]. Furthermore, larger repeat expansions in the smaller allele were associated with more pronounced cerebellar vermis atrophy (lobules I–V β = −1.06, P < 0.001; lobules VI–VII β = −0.34, P = 0.005). The repeat did not show significant instability during vertical transmission and across different tissues and brain regions.
RFC1 repeat size, particularly of the smaller allele, is one of the determinants of variability in RFC1 disease and represents a key prognostic factor to predict disease onset, phenotype and severity. Assessing the repeat size is warranted as part of the diagnostic test for RFC1 expansion.
Keywords: CANVAS, RFC1, ataxia, neuropathy, repeat expansions, southern blotting
Currò et al. investigate whether the size of the repeat expansion in RFC1 functions as a disease modifier and find that larger expansions are associated with earlier onset and with more complex and severe disease. They show too that the repeat size is stable across generations and across different tissues and brain regions.
Introduction
Repeat expansion disorders are a group of diseases caused by abnormally long microsatellites, also called short tandem repeats, located either in coding or non-coding regions of the human genome.1-4 The recent developments in whole-genome sequencing methods have led to an increased identification and diagnosis of diseases caused by non-coding repeat expansion.5,6
Short tandem repeats are dynamic elements that are variably prone to further expand in offspring and across different tissues from the same individual, leading to genetic anticipation and, arguably, selective tissue involvement.7-13 Notably, repeat expansion disorders typically show a correlation between the repeat length and an earlier onset and more severe disease phenotype.10,14-22
Biallelic expansion of AAGGG pentanucleotides (TTCCC in the transcription sense) in the second intron of the replication factor complex subunit 1 (RFC1) was identified as the main cause of cerebellar ataxia, neuropathy and vestibular areflexia syndrome (CANVAS)23,24 and subsequent studies reported a high prevalence of biallelic AAGGG expansions in cases with sporadic or familial ataxia.23,25-29 To date, biallelic AAGGG expansions explain the vast majority of CANVAS cases, with only few cases recently reported to carry different, population-specific configurations (i.e. ACAGG or AAAGG10–25AAGGGexpAAAGG4–6 in East Asia and Oceania28,30,31) or mono-allelic AAGGG expansions in compound heterozygous state with truncating variants.32-35 A sensory neuropathy was recognized as the key feature in RFC1 disease spectrum and up to a third of cases diagnosed with idiopathic sensory neuropathy, with or without ataxia and vestibular impairment, carry biallelic RFC1 expansions.36,37 Clinical heterogeneity in RFC1 disease also involves the disease course and severity, as revealed by the wide range of age at onset and disability.29,36,38 However, determinants of the variability of RFC1 disease are still largely unknown.
In this multicentre study, we assessed the impact of the AAGGG repeat expansion size on the disease onset, phenotype and severity in a large cohort of patients carrying biallelic RFC1 expansions. To gain further insight into the intergenerational transmission and disease pathogenesis, we also investigated the stability of the AAGGG repeat in families and within different tissues of affected individuals.
Materials and methods
Patients
The study population consisted of a multicentre cohort of 2334 patients diagnosed with sensory neuropathy, adult-onset (>25 years old) cerebellar ataxia, complex neuropathy or CANVAS. Sensory neuropathy was diagnosed according to clinical and neurophysiological criteria.39,40 Complex neuropathy was defined by the presence of sensory neuropathy and evidence of either cerebellar or vestibular involvement on examination and/or investigations. Patients with combined involvement of sensory, vestibular and cerebellar systems were classified as CANVAS.41,42 Previous studies demonstrated that sensory involvement is the hallmark of RFC1 disorder.36,38 Accordingly, a phenotype category was not assigned to patients whose sensory examination or nerve conduction studies were not available. Furthermore, clinical phenotype was defined only when at least two of the three core systems (i.e. sensory, cerebellar and vestibular) were examined.
Clinical features
Clinical and demographic data of patients with positive genetic testing for biallelic RFC1 expansions were collected according to a standardized template, which was completed by all referring clinicians and which included: family history, age at onset of any neurological symptom, including sensory symptoms, dysarthria, dysphagia and oscillopsia, use of walking aids and detailed first and last available neurological examinations. To avoid a possible confounder effect of population-specific non-canonical configurations,28,30,31 we included only patients of Caucasian ancestry in our analyses. The presence of chronic cough was also recorded, but it was not considered to define the neurological onset of the condition. Assessment of sensory system was available in 381 cases (97%), of cerebellum in 385 (98%) and of vestibular system in 260 (66%). Based on the presence of symptoms and signs, patients were divided into three categories: sensory neuropathy, complex neuropathy, and CANVAS. Additional features, such as parkinsonism, cognitive impairment, symptomatic dysautonomia or pyramidal involvement were also recorded. Dysarthria and dysphagia and loss of independent walking were further analysed as markers of disease severity.
Brain MRI data acquisition
Structural T1 MRI of 59 brain MRIs acquired from 2004 to 2023 in a clinical setting at the National Hospital for Neurology and Neurosurgery (London, UK) were retrieved for volumetric analyses. Two-dimensional or 3D acquisitions were included depending on availability. Twenty-seven MRI were discarded as they did not pass quality check. Brain parcellations were computed using Geodesic Information Flows (GIF)43 (GIF is free and available as webservice in NiftyWeb44) and following the Desikan-Killiany-Tourville atlas.45 After parcellation, volumes were separately computed for cerebellar vermal lobules I–V, lobules VI–VII, lobules VII–X, and for the total intracranial volume in mm3.
PCR-based screening of RFC1 AAGGG repeat expansion
RFC1 genetic tests were performed as previously described.23,42 Samples with no amplifiable products on flanking PCR and positive repeat-primed PCR (RP-PCR) for the AAGGG repeat were considered likely positive for biallelic AAGGG RFC1 expansions, after the exclusion of the non-pathogenic AAAGG and AAAAG expansions on the other allele.
Southern blotting
Provided that enough good quality DNA was available, samples were analysed by Southern blotting, as previously described,23 to confirm the presence and to measure the size of the expanded alleles. The lowest size for AAGGG repeat expansions detected in this study was 6.5 kb (i.e. ∼250 repeat units).
Meiotic instability
DNA from affected or unaffected first-degree relatives of index cases from 27 families was tested by Southern blotting. RFC1 repeat size within families was compared to evaluate the stability of the AAGGG repeat during intergenerational transmission.
Somatic instability
Optical genome mapping (OGM; Bionano Genomics) was performed to assess the presence of post-zygotic instability in affected (vermis, cerebellar hemispheres) versus unaffected tissues (frontal cortex, muscle, fibroblasts) of patients carrying biallelic RFC1 expansions. OGM has shown a good correlation with Southern blotting in the identification and sizing of large repeat expansions, including RFC1,46 and a higher sensitivity in detecting the presence of somatic variation.47 Blood-derived DNA from a patient with C9orf72 GGGGCC expansion was also included as positive control for repeat instability.48 Samples were processed as previously described.47 Labelled ultra-high molecular weight (UHMW) gDNA was loaded on a Saphyr chip for linearization and imaging on the Saphyr instrument (Bionano Genomics). The repeat expansion size was estimated as the difference between the mean of the Gaussian distribution of molecules mapping to the expanded alleles and the reference intermarker distance. Repeat sizes in different tissues and their standard deviations were calculated and compared to detect somatic instability.
Ethics
The study was approved by the ethics committee and by local institutional review boards. All patients gave informed consent prior to their inclusion in the study. The study complied with all relevant ethical regulations.
Statistical analysis
Data were expressed as means with standard deviations or medians with 25–75% interquartile ranges (IQRs) and min-max values depending on their distribution. Statistical significance threshold was set to P < 0.05 and correction for multiple comparisons was applied, as appropriate. We have accounted for the presence of clustered data (i.e. members of the same families) adopting cluster-adjusted robust standard errors in survival models and by adding a family random effect in linear regressions. To address the problem of collinearity due to the correlation between the repeat size of smaller and larger allele, all the analyses were performed adopting two separate models, one for each allele. First, we calculated Pearson’s correlation coefficients for repeat size of the smaller and larger allele and age at disease onset (cough excluded). We then ran a Cox regression to evaluate the effect of repeat size on age at disease onset (cough excluded) and at onset of main disease symptoms (i.e. unsteadiness, sensory symptoms, dysarthria and/or dysphagia, oscillopsia, chronic cough). Time from disease onset to dysarthria and/or dysphagia and to use of walking aids was considered as outcomes to predict the effect of repeat size on progression to disabling disease. A Fine-Gray competing risk model was adopted to adjust for competing risk (i.e. risk of the patient dying before experiencing the symptom). For each regression model, regression tables with hazard ratios (HR), 95% confidence intervals (CI) and P-value of a two-tailed Wald’s test on the coefficients for a 1000-unit change in repeat size were reported (Supplementary material). Predicted cumulative incidence functions (CIF) were plotted for all the symptoms of interest. A quasi-Poisson regression model was used to analyse the relationship between phenotype and number of repeat units. Coefficients were reported as rate ratios (RR). The model was adjusted for sex, age at last examination and disease duration, and was followed by Tukey adjusted pairwise comparisons between the three phenotypes. Multivariate linear regression was performed to assess the correlation between the repeat size and the degree of atrophy of cerebellar vermis, adjusted for age, disease duration and total intracranial volume. Meiotic stability of the repeat was assessed by a linear mixed-effects model. Pearson’s coefficient was calculated to test the correlation between age of neurological onset in members of the same family. All analyses were performed using STATA statistical software, version 14. Plots and graphs were created with GraphPad Prism version 9.4.1 for Windows, GraphPad Software, San Diego, California USA, www.graphpad.com.
Results
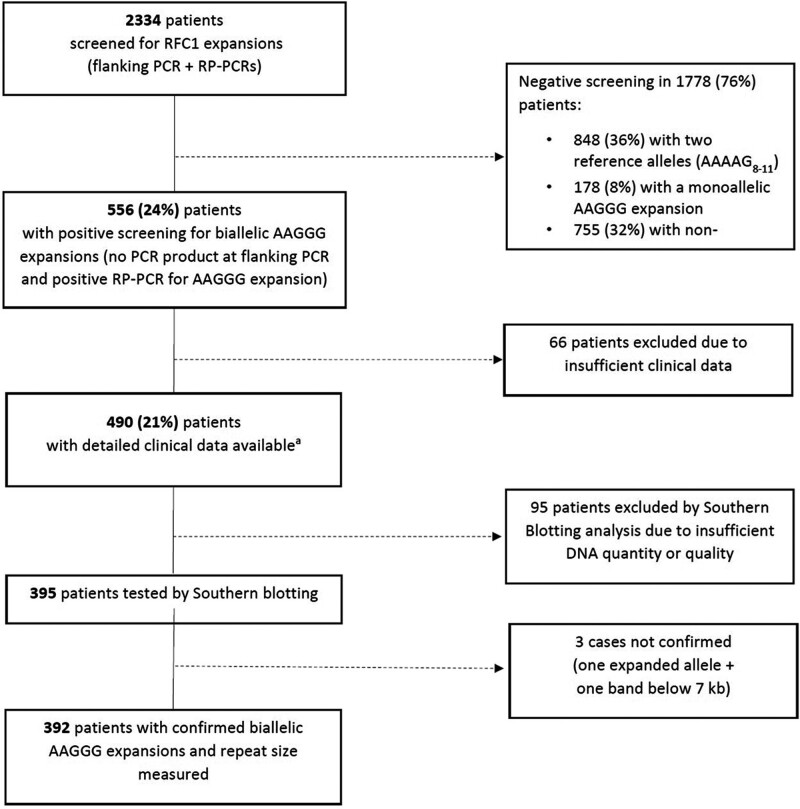
Genetic testing for RFC1 expansions
Of 2334 patients, 556 (24%) carried biallelic AAGGG expansions at PCR screening. A sufficient amount of good quality DNA to perform Southern blotting was available in 395 cases. We confirmed the biallelic expansions in 392 patients (99.3%). Sanger sequencing in the three unconfirmed samples showed intermediate expansions (<100 repeats) of non-pathogenic AAAAG, AAAGG or AAAGGG motifs, which were missed by the previous PCR-based screening (Fig. 1).
Figure 1.
Flow chart describing the results of the genetic screening for RFC1 expansions. RP-PCR = repeat-primed polymerase chain reaction.
aThree cases were subsequently excluded from the analysis because Southern blotting did not confirm the presence of biallelic expansions.
Clinical heterogeneity and disease course of RFC1 disease
Demographic and clinical data from the 392 patients confirmed at Southern blotting are summarized in Table 1. There was a similar number of males and females. Three hundred and forty-seven cases were sporadic (89%), 45 cases were familial from 19 families, including 14 families with two members, three with three members, and two families with four members affected. All cases were Caucasian and most of them (n = 363, 92%) from European descents, however multiple countries were represented, including Turkey (n = 18), Brazil (n = 1), Iran (n = 1), Iraq (n = 1), Algeria (n = 1) and Lebanon (n = 1). Country of origin was not specified for six patients. Median age at onset of neurological symptoms (cough excluded) was 54 years (IQR = 49–61), ranging from 25 to 80 years. Unsteadiness was the most common complaint at disease onset, followed by sensory symptoms (e.g. loss of feeling, tingling, pins and needles). Dysarthria and/or dysphagia, suggestive of cerebellar involvement, and oscillopsia, due to bilateral vestibular impairment, were less frequent in the initial stages of disease but were present in up to 51% and 27% of patients at the most recent evaluation, respectively. Chronic cough was investigated in 358 patients (91%) and reported by 267 of them (75%). Cough was the presenting symptom in half of the cases. Fifty-four per cent of patients required walking aids after a median disease duration of 10 years (IQR = 5–16) and 17% needed a wheelchair after 14 years (IQR = 11–21). Less common symptoms and signs included: symptomatic dysautonomia (n = 17), cognitive impairment (n = 7), parkinsonism (n = 2), upper motor neuron involvement other than brisk reflexes (e.g. spasticity, Babinski sign) (n = 1).
Table 1.
Demographic and clinical data of RFC1 positive patients
| Demographics | |||
|---|---|---|---|
| n males (%), females (%) | 195 (50%), 197 (50%) | ||
| Positive family history | 45 (11%) | ||
| Current age (IQR, min-max) | 70 years (64–77; 42–90) | ||
| Age at neurological onset (IQR; min-max) | 54 years (49–61; 25–80) | ||
| Deceased | 32 (8%) | ||
| Duration of follow-up | 10 years (6–17) | ||
| Symptoms | Disease onset (n/total) | Last follow–up (n/total) | Age at onset (median, IQRs, min-max) |
| Chronic cough | 178/358 (50%) | 267/358 (75%) | 40 years (30–50; 15–83) |
| Sensory symptoms | 138/383 (36%) | 276/383 (72%) | 55 years (50–62; 25–75) |
| Unsteadiness | 255/388 (66%) | 366/388 (94%) | 56 years (50–63; 30–80) |
| Oscillopsia | 19/352 (6%) | 94/352 (27%) | 62 years (55–70; 36–81) |
| Dysarthria/dysphagia | 21/381 (6%) | 196/381 (51%) | 64 years (57–70; 30–85) |
| Loss of independent walking | n/total (%) | Age at walking aid (median, IQRs, min–max) | Time to walking aid (median, IQRs, min–max) |
| Any walking aid | 203/379 (54%) | 67 years (61–72; 37–88) | 10 years (5–16; 0–43) |
| One stick | 181/377 (48%) | 66 years (61–71; 37–88) | 9 years (5–15; 0–43) |
| Two sticks | 86/354 (24%) | 70 years (65–75; 41–86) | 12 years (7–20; 0–45) |
| Wheelchair | 61/357 (17%) | 70 years (66–76; 46–85) | 14 years (11–21; 2–48) |
| Neurological examination | First examination (n = 392) | Most recent examination (n = 205) | |
| Age at examination (IQR, min-max) | 65 years (57–70; 32–86) | 69 years (62–75; 41–89) | |
| Disease duration (IQR, min-max) | 7 years (3–13; 0–49) | 12 years (8–20; 1–43) | |
| Interval between examinations (IQR, min–max) | — | 4 years (2–8; 1–26) | |
| Sensory impairment | 376/376 (100%) | 204/204 (100%) | |
| Pinprick | 215/304 (71%) | 144/164 (88%) | |
| Vibration | 295/333 (89%) | 173/179 (97%) | |
| Joint position | 116/267 (43%) | 88/149 (59%) | |
| Cerebellar signs | 270/374 (72%) | 170/202 (84%) | |
| Vestibular areflexia | 147/196 (75%) | 116/147 (79%) | |
| Clinical phenotype | First examination | Last follow–up | |
| Isolated neuropathy | 93 (24%) | 54 (14%) | |
| Complex neuropathy | 150 (38%) | 131 (33%) | |
| Sensory + cerebellar | 134 (34%) | 117 (30%) | |
| Sensory + vestibular | 16 (4%) | 14 (3%) | |
| CANVAS | 122 (31%) | 195 (50%) | |
| Not assigned due to incomplete clinical data | 28 (7%) | 12 (3%) | |
Data are presented as median (IQRs, min-max) or as percentages. Clinical phenotype was classified in three categories, as detailed in the ‘Materials and methods’ section, only when data from neurological examination and/or investigations included at least two of the three main systems involved in RFC1 disease. CANVAS = cerebellarataxia, neuropathy and vestibular areflexia syndrome; IQR = interquartile range.
Patients had a first neurological assessment at a median age of 65 years (IQR = 57–70), after a median disease duration of 7 years (IQR = 3–13). All cases had signs and/or symptoms of sensory neuropathy, when investigated. Ninety-three patients (24%) had an isolated sensory neuropathy, 150 (38%) a complex neuropathy with vestibular or cerebellar involvement and 122 (31%) CANVAS. No patient had isolated cerebellar or vestibular disease. A phenotype was not assigned in 28 cases (7%) due to incomplete clinical assessment. A second examination was available in 205 cases, after a median interval of 4 years (IQR = 2–8) from the first examination and of 12 years (IQR = 8–20) from disease onset. An additional 12% and 17% of patients developed signs of cerebellar and vestibular involvement, respectively. Overall, 195 patients (50%) had complete CANVAS, 131 (33%) had a complex neuropathy, while 54 (14%) still showed an isolated sensory neuropathy.
Thirty-two patients (8%) were deceased at the time of the study and in seven cases, death was related to the underlying neurological disease (i.e. four due to complications of prolonged immobility or falls, three due to aspiration pneumonia or cachexia in dysphagic patients). Other reported causes of death were neoplasms (n = 3), SARS-CoV2 infection (n = 2), myocardial infarction (n = 1), cerebral haemorrhage (n = 1), pulmonary fibrosis and respiratory failure (n = 2). Median age at death was 76 years (IQR = 74–78) for males and 76 years (IQR = 74–79) for females, which is slightly below the mean life expectancy in Europe according to World Health Organization (WHO) data (overall = 80.4; females = 83.2; males = 77.5).49
Repeat expansion size predicts onset and progression of RFC1 disease
The median number of AAGGG repeats was 1042 (IQR = 844–1306; range = 249–3885) and specifically 937 repeat units (IQR = 771–1129; range = 249–2411) for the smaller allele and 1195 repeat units (IQR = 927–1452; range = 294–3885) for the larger allele. Notably, we observed a significant correlation (r = 0.7, P < 0.001) between the size of the two alleles. In 143 patients (36%) the two expanded alleles appeared as a single band on Southern blotting. This suggests that they had the same or highly similar size, within the limits of detection resolution of this technique.
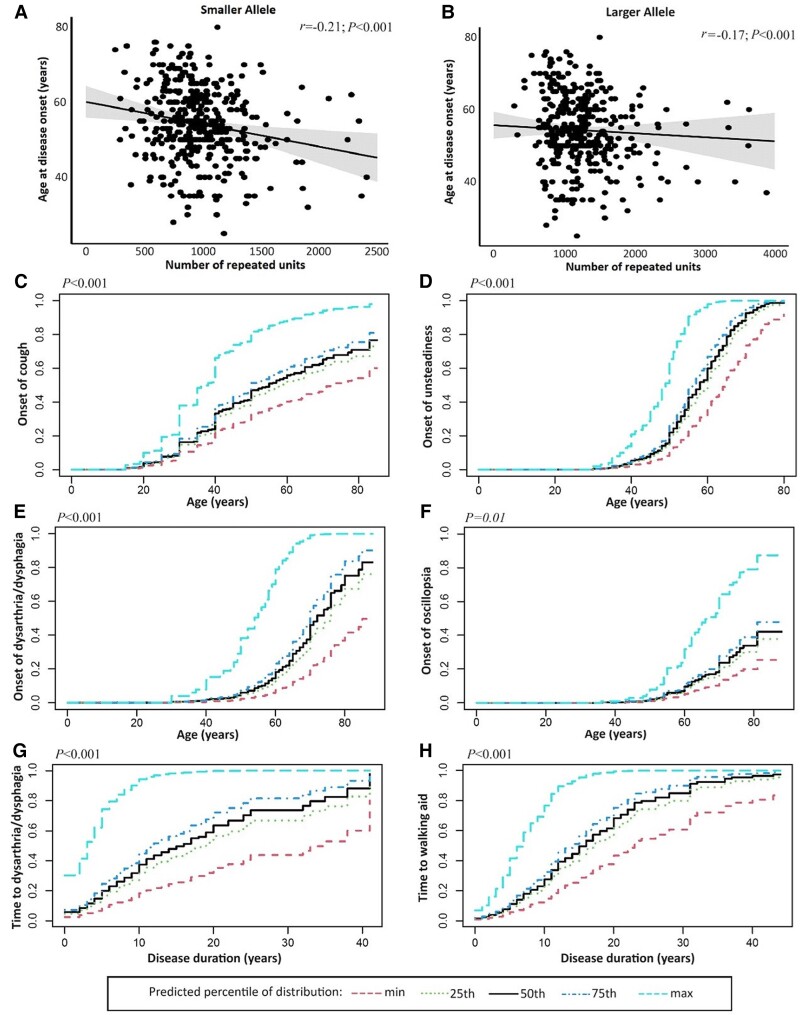
Detailed tables and figures for the statistical analyses are provided in the Supplementary material. We observed an inverse correlation between age at neurological onset and repeat size of the smaller allele (r = −0.21, r2 = 0.06, P < 0.001) and the larger allele (r = −0.17, r2 = 0.03, P < 0.001) (Fig. 2A and B). After adjusting for sex and clinical phenotype, the association with age at neurological onset was still more significant for the smaller allele (HR = 2.06, P < 0.001) than for the larger allele (HR = 1.53, P < 0.001) (Supplementary Table 1).
Figure 2.
Relationship between repeat size and main symptoms of RFC1 disease. (A and B) The scatter plots illustrate the strength and the direction of the correlation between the age at neurological onset of the disease (y-axis) and the repeat size of the smaller or the larger allele (x-axis). (C–F) The curves illustrate the predicted cumulative incidence function (CIF) for chronic cough, unsteadiness, dysarthria/dysphagia and oscillopsia plotted against age at onset. (G and H) Predicted CIF for dysarthria/dysphagia and need of walking aid plotted against disease duration. Curves are stratified for values of smaller allele repeat size equal to the minimum value, 25th, 50th,75th percentiles and maximum value of distribution.
A Fine-Gray model with robust cluster standard errors, adjusted for competing risk of death and corrected for gender, was adopted to analyse the effect of repeat size of smaller and larger allele on age at onset of main disease symptoms. Coefficients were calculated for 1000-repeat units increase.
The repeat size of the smaller and larger allele resulted to be significant predictors of age at onset of unsteadiness (HR = 2.68, P < 0.001 for the smaller allele; HR = 1.64, P < 0.001 for the larger allele) and at onset of dysarthria and/or dysphagia (HR = 4.01, P < 0.001 for the smaller allele; HR = 1.93, P < 0.001 for the larger allele). The repeat size of the smaller allele also correlated with the onset of cough (HR = 1.95, P < 0.001), whereas the larger allele showed a borderline association with the onset of sensory symptoms (HR = 1.33, P = 0.009 with adjusted threshold of significance P = 0.01) (Fig. 2C–F and Supplementary Table 2). Patients carrying larger expansions had an increased risk to develop disabling symptoms earlier in disease course compared to individuals with smaller expansions (smaller allele: HR = 3.40, P < 0.001 for dysarthria/dysphagia and HR = 2.78, P < 0.001 for walking aids; larger allele: HR = 1.71, P = 0.002 for dysarthria/dysphagia and HR = 1.60, P < 0.001 for walking aids) (Fig. 2G and H). However, age at disease onset was an independent predictor of disease course, with a later disease onset being associated with a shorter time to the onset of these symptoms (Supplementary Table 3).
Median disease duration at onset of dysarthria/dysphagia and at need for walking aids was significantly shorter in patients with repeat size of the smaller allele above the 75th percentile (14.5 years for dysarthria/dysphagia, 15.1 years for walking aids) compared to patients with a repeat size below the 25th percentile (21.5 years for dysarthria/dysphagia, 19.2 years for walking aids; P < 0.001).
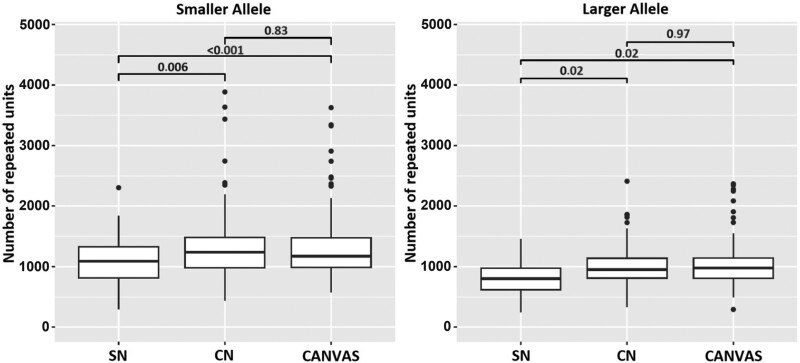
Repeat expansion size influences disease phenotype
After correcting for sex, age at last examination and age at disease onset, the mean size of both alleles was significantly higher in patients with complex neuropathy (smaller allele RR = 1.30, P = 0.003; larger allele RR = 1.33, P = 0.008) or CANVAS (smaller allele RR = 1.34, P < 0.001; larger allele RR = 1.31, P = 0.009) than in patients with isolated neuropathy (Supplementary Table 4). This difference was confirmed by pair-wise comparisons of repeat size between the three phenotypes (Fig. 3). Conversely, we did not observe a significant difference in repeat size between patients with complex neuropathy and CANVAS phenotype (P = 0.83 smaller allele; P = 0.97 larger allele).
Figure 3.
Relationship between phenotype and repeat length. The box plots compare the repeat size for the smaller (left) and larger (right) alleles in patients with different phenotypes at last examination. P-values were calculated adopting Tukey’s correction. CANVAS = cerebellar ataxia, neuropathy and vestibular areflexia syndrome; CN = complex neuropathy; SN = sensory neuropathy.
Repeat expansion size correlates with the degree of cerebellar atrophy
We next tested the association between the repeat length and the degree of cerebellar vermis atrophy in an internal cohort of 32 brain MRI performed at the National Hospital for Neurology and Neurosurgery, London (UK). After adjusting for age at MRI, disease duration and total intracranial volume, we observed a significant association (Bonferroni-adjusted significance level α = 0.017) between the repeat size of the smaller allele and the volume of cerebellar vermis lobules I–V (β = −1.06, P < 0.001) and lobules VI–VII (β = −0.34, P = 0.005). Conversely, the volume of lobules VIII-X did not correlate with the repeat size (β = −0.44, P = 0.07). No significant association was observed between the repeat size of the larger allele and cerebellar volume (Supplementary Table 5).
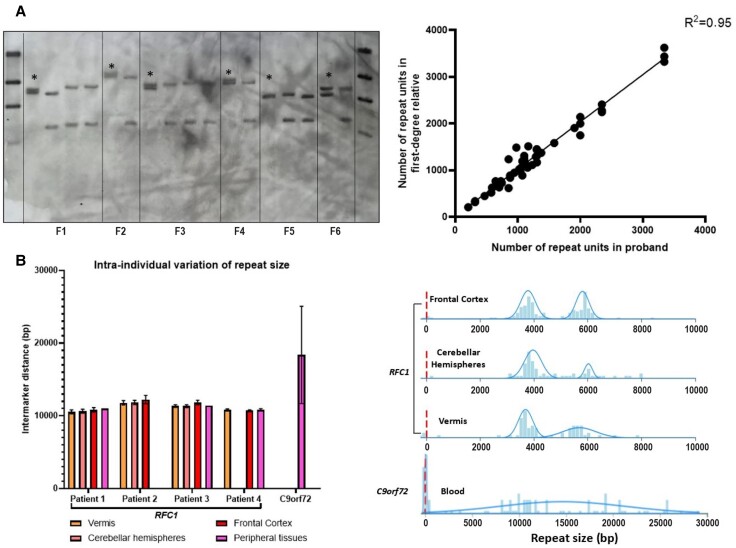
Stability of RFC1 repeat expansion across generations and tissues
We evaluated 69 subjects (including 27 probands, 22 siblings, 18 offspring and two parents) from 27 families, for a total of 64 meiotic events. AAGGG repeat expansion appeared stable across generations (r2 = 0.95), with a median intra-familial variation of 25 repeats (IQR = −17/+45, min max = −250/+510) and <10% compared to the proband’s allele in 80% of meiosis (Fig. 4A). This was paralleled by the observation of a significant correlation (r = 0.66, P < 0.001) between the age at onset of multiple affected members within the same family (n = 41 patients from 17 families). Expansion or contraction of the repeat across generations occurred with the same frequency. Next, we compared the RFC1 repeat size from different brain areas and peripheral tissues including blood, muscles and/or fibroblasts, as available, from four patients carrying biallelic RFC1 expansions. There was limited instability of the repeat across the tissues analysed, with a variation in size between −97 and +190 repeats (−5%/+7%) compared with the mean size (Fig. 4B). Furthermore, mean dispersion of the repeat length was ±1.7% for vermis, ±2% for cerebellar hemispheres and ±2.7% for frontal cortex, as opposed to a dispersion of ±36% in an individual carrying C9orf72 expansion. Overall, there was evidence of limited somatic instability across affected and unaffected bulk tissues.
Figure 4.
Limited meiotic and somatic instability of the AAGGG repeat expansion. (A) On the left, the picture illustrates a representative example of Southern blotting including probands (asterisks) and unaffected relatives from six families (Families F1–F6). On the right, the correlation plot shows the relationship of the repeat size within members of the same family. Each dot corresponds to a meiotic event. (B) Left: The bar chart shows the dispersion of the repeat size among different brain areas and peripheral tissues of four patients with RFC1 biallelic expansions and in one patient with C9orf72 expansion. Mean intermarker distance (expressed in base pairs, bp) and standard deviations (SDs) are shown. In Patient 1 and Patient 3, repeat size from peripheral tissue was measured by Southern blotting. Right: Distribution of DNA molecules measured by genome optical mapping (Bionano Genomics) in different tissues of a patient with a biallelic expansion in RFC1 and in blood-derived DNA of a patient with C9orf72 expansion. The size of DNA molecules mapping on RFC1 or C9orf72 locus is expressed in base pairs.
Discussion
In this study we leveraged a large international cohort of genetically confirmed patients carrying biallelic RFC1 expansions to assess the impact of the repeat expansion size on onset, clinical phenotype and progression of RFC1 disease.
Clinical data confirmed the existence of a spatial dissemination of the disease from an isolated sensory neuropathy with or without chronic cough to a complex neurodegenerative disease, mainly entailing clinically manifest cerebellar and vestibular involvement. Sensory neuropathy was present in all patients tested, confirming the central role of sensory involvement in RFC1 disease. We showed that the repeat size in patients with isolated sensory neuropathy is smaller compared to patients with multisystem involvement and similar disease duration. Therefore, the repeat expansion acts as a modifier of the disease phenotype, probably due to a higher susceptibility of sensory neurons to the AAGGG repeat expansion, even of small size, compared to other tissues.
We observed a significant influence of the repeat length on the age of neurological onset. The association could be better appreciated when looking at well-defined clinical symptoms, like the onset of dysarthria and dysphagia, which tend to appear later in the disease course. Indeed, early sensory symptoms, imbalance and chronic cough may be initially mild and progress very slowly over time, so that patients struggle to date back the exact onset of the disease and often tend to date the first symptoms to few years before seeking neurologic attention.
Most importantly, we have demonstrated a direct impact of the repeat size on the disease severity and progression. Patients carrying larger expansions had a less favourable prognosis, with over 3-fold increased hazard of developing dysarthria or dysphagia and over 2-fold increased hazard of losing independent walking per 1000-units increase in repeat size. An older age at disease onset was associated with a faster progression. This has been observed in other neurodegenerative disorders, including sporadic and familial (C9orf72) ALS/ALS-FTD (frontotemporal dementia).50-53 It has been postulated that the faster progression observed in late-onset ALS cases might reflect the reduced neuronal reserve at baseline in older patients.51 This hypothesis may also apply to RFC1 disease. Alternatively, the shorter interval between disease onset and reaching disability milestones in cases with late onset may simply reflect a delayed diagnosis in individuals where early neurological symptoms, including sensory symptoms or mild unsteadiness, were overlooked or absent.
Importantly, we also showed that the repeat size of the smaller allele correlates with the degree of cerebellar vermis atrophy. The correlation is significant for lobules I–V and lobules VI–VII, in keeping with the selective atrophy of these lobules reported in previous neuroimaging and neuropathological studies.54,55
However, the degree of correlation might be influenced by the small sample size and by possible partial volume artefacts in 2D acquisitions. Prospective studies with larger cohorts and homogenous volumetric acquisitions are warranted to confirm these findings.
Importantly, the repeat size explained only up to 6% of the variability in age of neurological disease onset, suggesting that additional environmental or genetic modifiers at the repeat locus or in distant genes may be at play. In particular, the study was not designed to address the role of repeat interruptions, as Southern blotting only provides information about the repeat size.
The study also demonstrated that the pathogenic AAGGG repeat has limited germline and somatic instability. Unlike most short tandem repeats, including the CAG repeat in Huntington’s disease and other polyglutamine diseases, CTG in myotonic dystrophy type 1, CGG in fragile X syndrome-FXTAS, and CCGGGG in C9orf72, in which a significant instability of the expanded repeat was demonstrated,8,48,56-59 the RFC1 AAGGG repeat appears stable across generations, with a repeat size variation, including contraction and further expansion, mostly unchanged or limited to 10% of repeat size.
In this regard, it is interesting to note that the size of the two alleles was not independent in the population tested and one-third of cases had biallelic expansions of identical or highly similar size. We hypothesize that this observation could be caused by a geographic distribution of expanded alleles of a similar size, which is maintained over time and across generations, and we speculate that the stability of the RFC1 repeat observed in single families may extend to broader areas and regions, inhabited by distantly related individuals.
To gain insight into the mechanisms underlying the tissue-specific involvement of RFC1 disease, we tested whether the AAGGG repeat may undergo a further somatic expansion in the affected cerebellum. Although a variation of the repeat size at single cell level cannot be excluded, the data obtained from bulk tissue do not support the existence of significant instability of the repeat size as a determinant of the selective involvement of specific regions and neuronal populations in RFC1 disease.
Finally, the relative stronger effect of the size of the smaller allele may suggest the existence of an underlying loss-of-function mechanism in RFC1 disease, with progressive decrease of the residual RFC1 function sustained by the allele carrying the smaller of the two expansions. This hypothesis is also supported by the recent identification of truncating variants in RFC1 in compound heterozygous state with an expansion on the second allele, leading to typical, if not more severe, CANVAS phenotype.32,33 These observations are particularly relevant to the understanding of the disease-causing mechanism of RFC1 disease as, despite the recessive mode of inheritance, the expression of RFC1 transcript and protein seems unchanged.23 Notably, truncating variants in the coding region and a prominent effect of the smaller allele have both been previously observed in Friedreich’s ataxia, a recessive disorder caused by biallelic GAA expansion in FXN, and for which, as opposed to RFC1 disease, a reduced expression and loss-of-function of the repeat containing gene has been clearly shown.60
The main limits of this work are related to its retrospective nature. In particular, the milder influence of the repeat size on some clinical features might be partly explained by the difficulty of patients in dating back the onset of their earliest symptoms, as well as by a lack of homogeneity in the clinical examinations and investigations performed in different centres. Prospective studies in RFC1 disease are needed to more accurately trace the disease progression and fully capture the effect of repeat expansion disease.
In conclusion, the study contributed to better define the genotype-phenotype spectrum of RFC1 disease and highlighted the key role of the repeat size as disease modifier. Larger expansions, in particular of the smaller allele, are associated with an earlier onset, a more complex phenotype and a more aggressive disease progression. Estimating the size of the repeat expansion by Southern blotting or alternative methods, which became only recently available (e.g. optical genome mapping) is important not only to confirm the presence of biallelic expansions, but also to identify patients with higher risk to develop more complex and disabling phenotypes after a shorter disease duration and to better inform them and their families on prognosis. This may also impact the future design of trials as it will be key that patients in placebo/active drug groups will have a comparable distribution of repeat sizes.
Supplementary Material
Acknowledgements
We thank the patients and relatives who participated in this study.
Appendix 1
RFC1 repeat expansion study group
Inés Albájar, Catherine Ashton, Nick Beauchamp, Sarah J Beecroft, Emilia Bellone, Josè Berciano, Petya Bogdanova-Mihaylova, Barbara Borroni, Bernard Brais, Enrico Bugiardini, Catarina Campos, Aisling Carr, Liam Carroll, Francesca Castellani, Tiziana Cavallaro, Patrick F. Chinnery, Silvia Colnaghi, Giuseppe Cosentino, Joana Damasio, Soma Das, Grazia Devigili, Daniela Di Bella, David Dick, Alexandra Durr, Amar El-Saddig, Jennifer Faber, Moreno Ferrarini, Massimiliano Filosto, Geraint Fuller, Salvatore Gallone, Chiara Gemelli, Marina Grandis, John Hardy, Channa Hewamadduma, Rita Horvath, Vincent Huin, Daniele Imperiale, Pablo Iruzubieta, Diego Kaski, Andrew King, Thomas Klockgether, Müge Koç, Kishore R. Kumar, Thierry Kuntzer, Nigel Laing, Matilde Laurà, Timothy Lavin, Peter Nigel Leigh, Lea Leonardis, Michael P. Lunn, Stefania Magri, Francesca Magrinelli, Maria João Malaquias, Michelangelo Mancuso, Hadi Manji, Sara Massucco, John McConville, Renato P. Munhoz, Sara Nagy, Alain Ndayisaba, Andrea Hilary Nemeth, Luiz Eduardo Novis, Johanna Palmio, Elena Pegoraro, David Pellerin, Benedetta Perrone, Chiara Pisciotta, James Polke, Malcolm Proudfoot, Laura Orsi, Aleksandar Radunovic, Nilo Riva, Aiko Robert, Riccardo Ronco, Elena Rossini, Alex M Rossor, Irmak Şahbaz, Qais Sa’di, Ettore Salsano, Alessandro Salvalaggio, Lucio Santoro, Elisa Sarto, Andrew Schaefer, Angelo Schenone, Carolin Scriba, Joseph Shaw, Gabriella Silvestri, James Stevens, Michael Strupp, Charlotte J. Sumner, Agnieszka Szymura, Matteo Tagliapietra, Cristina Tassorelli, Alessandra Tessa, Marie Theaudin, Pedro Tomaselli, Stefano Tozza, Arianna Tucci, Enza Maria Valente, Maurizio Versino, Richard A. Walsh, Nick W. Wood, Way Yan Yau, Stephan Zuchner.
Contributor Information
Riccardo Currò, Department of Neuromuscular Diseases, UCL Queen Square Institute of Neurology, London, WC1N 3BG, UK; Department of Brain and Behavioral Sciences, University of Pavia, 27100 Pavia, Italy.
Natalia Dominik, Department of Neuromuscular Diseases, UCL Queen Square Institute of Neurology, London, WC1N 3BG, UK.
Stefano Facchini, Department of Neuromuscular Diseases, UCL Queen Square Institute of Neurology, London, WC1N 3BG, UK; Department of Brain and Behavioral Sciences, University of Pavia, 27100 Pavia, Italy.
Elisa Vegezzi, IRCCS Mondino Foundation, 27100 Pavia, Italy.
Roisin Sullivan, Department of Neuromuscular Diseases, UCL Queen Square Institute of Neurology, London, WC1N 3BG, UK.
Valentina Galassi Deforie, Department of Neuromuscular Diseases, UCL Queen Square Institute of Neurology, London, WC1N 3BG, UK.
Gorka Fernández-Eulate, Nord/Est/Ile-de-France Neuromuscular Reference Center, Institute of Myology, Pitié-Salpêtrière Hospital, APHP, 75013 Paris, France.
Andreas Traschütz, Research Division ‘Translational Genomics of Neurodegenerative Diseases’, Hertie-Institute for Clinical Brain Research and Center of Neurology, University of Tübingen, 72076 Tübingen, Germany; German Center for Neurodegenerative Diseases (DZNE), University of Tübingen, 72076 Tübingen, Germany.
Salvatore Rossi, Dipartimento di Scienze dell'Invecchiamento, Neurologiche, Ortopediche e della Testa-Collo, UOC Neurologia, Fondazione Policlinico Universitario A. Gemelli IRCCS, 00168 Rome, Italy; Facoltà di Medicina e Chirurgia, Dipartimento di Neuroscienze, Università Cattolica del Sacro Cuore, 00168 Rome, Italy.
Matteo Garibaldi, Neuromuscular and Rare Disease Center, Department of Neuroscience, Mental Health and Sensory Organs (NESMOS), Sant'Andrea Hospital, Sapienza University of Rome, 00189 Rome, Italy.
Mariusz Kwarciany, Department of Adult Neurology, Medical University of Gdańsk, 80-952 Gdańsk, Poland.
Franco Taroni, Unit of Medical Genetics and Neurogenetics, Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan 20133, Italy.
Alfredo Brusco, Department of Medical Sciences, University of Torino, 10124 Turin, Italy.
Jean-Marc Good, Division of Genetic Medicine, Lausanne University Hospital (CHUV), 1011 Lausanne, Switzerland.
Francesca Cavalcanti, Institute for Biomedical Research and Innovation (IRIB), Italian National Research Council (CNR), 87050 Mangone, Italy.
Simon Hammans, Wessex Neurological Centre, Southampton General Hospital, Southampton, SO16 6YD, UK.
Gianina Ravenscroft, Neurogenetic Diseases Group, Centre for Medical Research, QEII Medical Centre, University of Western Australia, Nedland, WA 6009, Australia.
Richard H Roxburgh, Neurology Department, Auckland City Hospital, New Zealand and the Centre for Brain Research, University of Auckland, Auckland 1142, New Zealand.
Ricardo Parolin Schnekenberg, Department of Neuromuscular Diseases, UCL Queen Square Institute of Neurology, London, WC1N 3BG, UK.
Bianca Rugginini, Department of Brain and Behavioral Sciences, University of Pavia, 27100 Pavia, Italy.
Elena Abati, Department of Neuromuscular Diseases, UCL Queen Square Institute of Neurology, London, WC1N 3BG, UK; Department of Pathophysiology and Transplantation, University of Milan, 20122 Milan, Italy.
Arianna Manini, Department of Neuromuscular Diseases, UCL Queen Square Institute of Neurology, London, WC1N 3BG, UK; Department of Pathophysiology and Transplantation, University of Milan, 20122 Milan, Italy.
Ilaria Quartesan, Department of Brain and Behavioral Sciences, University of Pavia, 27100 Pavia, Italy.
Arianna Ghia, Department of Brain and Behavioral Sciences, University of Pavia, 27100 Pavia, Italy.
Adolfo Lòpez de Munaìn, Neurology Department, Donostia University Hospital, University of the Basque Country-Osakidetza-CIBERNED-Biodonostia, 20014 Donostia-San Sebastián, Spain.
Fiore Manganelli, Department of Neuroscience and Reproductive and Odontostomatological Sciences, University of Naples Federico II, 80131 Naples, Italy.
Marina Kennerson, Sydney Medical School, Faculty of Medicine and Health, University of Sydney, Sydney, NSW 2050, Australia.
Filippo Maria Santorelli, IRCCS Stella Maris Foundation, Molecular Medicine for Neurodegenerative and Neuromuscular Disease Unit, 56128 Pisa, Italy.
Jon Infante, University Hospital Marquès de Valdecilla-IDIVAL, University of Cantabria, 39008 Santander, Spain.
Wilson Marques, Department of Neurology, School of Medicine of Ribeirão Preto, University of São Paulo, 2650 Ribeirão Preto, Brazil.
Manu Jokela, Neuromuscular Research Center, Department of Neurology, Tampere University and University Hospital, 33520 Tampere, Finland; Neurocenter, Department of Neurology, Clinical Neurosciences, Turku University Hospital and University of Turku, 20014 Turku, Finland.
Sinéad M Murphy, Department of Neurology, Tallaght University Hospital, D24 NR0A Dublin, Ireland; Academic Unit of Neurology, Trinity College Dublin, D02 R590 Dublin, Ireland.
Paola Mandich, Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (DINOGMI), University of Genoa, 16132 Genoa, Italy; IRCCS Ospedale Policlinico San Martino-UOC Genetica Medica, 16132 Genova, Italy.
Gian Maria Fabrizi, Department of Neurosciences, Biomedicine, and Movement Sciences, University of Verona, 37134 Verona, Italy.
Chiara Briani, Department of Neurosciences, ERN Neuromuscular Unit, University of Padova, 35100 Padova, Italy.
David Gosal, Manchester Centre for Clinical Neurosciences, Salford Royal Hospital, Northern Care Alliance NHS Foundation Trust, Greater Manchester, M6 8HD, UK.
Davide Pareyson, Unit of Medical Genetics and Neurogenetics, Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan 20133, Italy.
Alberto Ferrari, IRCCS Mondino Foundation, 27100 Pavia, Italy.
Ferran Prados, Centre for Medical Image Computing (CMIC), Department of Medical Physics and Biomedical Engineering, University College London, London, WC1V 6LJ, UK; NMR Research Unit, Institute of Neurology, University College London (UCL), London, WC1N 3BG, UK; e-Health Centre, Universitat Oberta de Catalunya, 08018 Barcelona, Spain.
Tarek Yousry, Neuroradiological Academic Unit, Queen Square Institute of Neurology, University College London, London, WC1N 3BG, UK.
Vikram Khurana, Division of Movement Disorders and Ann Romney Center for Neurologic Diseases, Department of Neurology, Brigham and Women's Hospital and Harvard Medical School, Boston, MA 02115, USA.
Sheng-Han Kuo, Department of Neurology, College of Physicians and Surgeons, Columbia University, New York, NY 10032, USA.
James Miller, Department of Neurology, Royal Victoria Hospitals, The Newcastle upon Tyne Hospitals NHS Foundation Trust, Newcastle, NE1 4LP, UK.
Claire Troakes, London Neurodegenerative Diseases Brain Bank, Department of Basic and Clinical Neuroscience, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, SE21 8EA, UK.
Zane Jaunmuktane, Department of Clinical and Movement Neurosciences, Queen Square Institute of Neurology, University College London, London, WC1N 3BG, UK.
Paola Giunti, Department of Neuromuscular Diseases, UCL Queen Square Institute of Neurology, London, WC1N 3BG, UK.
Annette Hartmann, Division of General Psychiatry, Medical University of Vienna, 1090 Vienna, Austria.
Nazli Basak, Koç University, School of Medicine, Suna and İnan Kıraç Foundation, Neurodegeneration Research Laboratory (NDAL), Research Center for Translational Medicine, 34010 Istanbul, Turkey.
Matthis Synofzik, Research Division ‘Translational Genomics of Neurodegenerative Diseases’, Hertie-Institute for Clinical Brain Research and Center of Neurology, University of Tübingen, 72076 Tübingen, Germany; German Center for Neurodegenerative Diseases (DZNE), University of Tübingen, 72076 Tübingen, Germany.
Tanya Stojkovic, Nord/Est/Ile-de-France Neuromuscular Reference Center, Institute of Myology, Pitié-Salpêtrière Hospital, APHP, 75013 Paris, France.
Marios Hadjivassiliou, Academic Department of Neurosciences, Sheffield Teaching Hospitals NHS Trust and University of Sheffield, Sheffield, S10 2JF, UK.
Mary M Reilly, Department of Neuromuscular Diseases, UCL Queen Square Institute of Neurology, London, WC1N 3BG, UK.
Henry Houlden, Department of Neuromuscular Diseases, UCL Queen Square Institute of Neurology, London, WC1N 3BG, UK.
Andrea Cortese, Department of Neuromuscular Diseases, UCL Queen Square Institute of Neurology, London, WC1N 3BG, UK; Department of Brain and Behavioral Sciences, University of Pavia, 27100 Pavia, Italy.
RFC1 repeat expansion study group:
Inés Albájar, Catherine Ashton, Nick Beauchamp, Sarah J Beecroft, Emilia Bellone, Josè Berciano, Petya Bogdanova-Mihaylova, Barbara Borroni, Bernard Brais, Enrico Bugiardini, Catarina Campos, Aisling Carr, Liam Carroll, Francesca Castellani, Tiziana Cavallaro, Patrick F Chinnery, Silvia Colnaghi, Giuseppe Cosentino, Joana Damasio, Soma Das, Grazia Devigili, Daniela Di Bella, David Dick, Alexandra Durr, Amar El-Saddig, Jennifer Faber, Moreno Ferrarini, Massimiliano Filosto, Geraint Fuller, Salvatore Gallone, Chiara Gemelli, Marina Grandis, John Hardy, Channa Hewamadduma, Rita Horvath, Vincent Huin, Daniele Imperiale, Pablo Iruzubieta, Diego Kaski, Andrew King, Thomas Klockgether, Müge Koç, Kishore R Kumar, Thierry Kuntzer, Nigel Laing, Matilde Laurà, Timothy Lavin, Peter Nigel Leigh, Lea Leonardis, Michael P Lunn, Stefania Magri, Francesca Magrinelli, Maria João Malaquias, Michelangelo Mancuso, Hadi Manji, Sara Massucco, John McConville, Renato P Munhoz, Sara Nagy, Alain Ndayisaba, Andrea Hilary Nemeth, Luiz Eduardo Novis, Johanna Palmio, Elena Pegoraro, David Pellerin, Benedetta Perrone, Chiara Pisciotta, James Polke, Malcolm Proudfoot, Laura Orsi, Aleksandar Radunovic, Nilo Riva, Aiko Robert, Riccardo Ronco, Elena Rossini, Alex M Rossor, Irmak Şahbaz, Qais Sa’di, Ettore Salsano, Alessandro Salvalaggio, Lucio Santoro, Elisa Sarto, Andrew Schaefer, Angelo Schenone, Carolin Scriba, Joseph Shaw, Gabriella Silvestri, James Stevens, Michael Strupp, Charlotte J Sumner, Agnieszka Szymura, Matteo Tagliapietra, Cristina Tassorelli, Alessandra Tessa, Marie Theaudin, Pedro Tomaselli, Stefano Tozza, Arianna Tucci, Enza Maria Valente, Maurizio Versino, Richard A Walsh, Nick W Wood, Way Yan Yau, and Stephan Zuchner
Data availability
With publication, de-identified data collected for the study, including individual participant data and a data dictionary defining each field in the set, can be made available to interested parties on reasonable request, and if in line with privacy regulations. Data can be requested at least 18 months after publication of this manuscript by sending an e-mail to the corresponding author.
Funding
This work was supported by Medical Research Council (MR/T001712/1), Fondazione Cariplo (grant n. 2019-1836), the Inherited Neuropathy Consortium, and Fondazione Regionale per la Ricerca Biomedica (Regione Lombardia, project ID 1751723), PRIN (F53D23002330006 - 20229MMHXP) and National Ataxia Foundation to A.C. R.C. was supported by the European Academy of Neurology (EAN) Research Fellowship 2021. H.H. and M.M.R. thank the MRC, the Wellcome Trust, the MDA, MD UK, Ataxia UK, The MSA Trust, the Rosetrees Trust and the NIHR UCLH BRC for grant support. F.T. thanks the Fondazione Regionale per la Ricerca Biomedica (CP 20/2018 (Care4NeuroRare) and the Italian Ministry of Health (RC) for grant support. D.P. thanks the Italian Ministry of Health (RRC) for grant support. F.M.S. thanks Ricerca Corrente 2022 Ministero della Salute 5X1000 for grant support. M.S. thanks the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) and the European Joint Programme on Rare Diseases for grant support. P.F.C. thanks the Medical Research Council Mitochondrial Biology Unit, the Medical Research Council (MRC) International Centre for Genomic Medicine in Neuromuscular Disease, the Leverhulme Trust (RPG-2018-408), the Medical Research Council, the Alzheimer's Society Project, and the NIHR Cambridge Biomedical Research for grant support. V.K. thanks the Silva Family Ataxia Foundation and the National Ataxia Foundation.
Competing interests
The authors report no competing interests.
Supplementary material
Supplementary material is available at Brain online.
References
- 1. Richard G-F, Kerrest A, Dujon B. Comparative genomics and molecular dynamics of DNA repeats in eukaryotes. Microbiol Mol Biol Rev. 2008;72:686–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Paulson H. Repeat expansion diseases. Handb Clin Neurol. 2018;147:105–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Orr HT, Zoghbi HY. Trinucleotide repeat disorders. Annu Rev Neurosci. 2007;30:575–621. [DOI] [PubMed] [Google Scholar]
- 4. Hannan AJ. Tandem repeats mediating genetic plasticity in health and disease. Nat Rev Genet. 2018;19:286–298. [DOI] [PubMed] [Google Scholar]
- 5. Ibañez K, Polke J, Hagelstrom RT, et al. Whole genome sequencing for the diagnosis of neurological repeat expansion disorders in the UK: A retrospective diagnostic accuracy and prospective clinical validation study. Lancet Neurol. 2022;21:234–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Depienne C, Mandel JL. 30 years of repeat expansion disorders: What have we learned and what are the remaining challenges? Am J Hum Genet. 2021;108:764–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rodriguez CM, Todd PK. New pathologic mechanisms in nucleotide repeat expansion disorders. Neurobiol Dis. 2019;130:104515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Matsuura T, Fang P, Lin X, et al. Somatic and germline instability of the ATTCT repeat in spinocerebellar ataxia type 10. Am J Hum Genet. 2004;74:1216–1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Khristich AN, Mirkin SM. On the wrong DNA track: Molecular mechanisms of repeat-mediated genome instability. J Biol Chem. 2020;295:4134–4170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Long A, Napierala JS, Polak U, et al. Somatic instability of the expanded GAA repeats in Friedreich’s ataxia. PLoS One. 2017;12:e0189990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Morales F, Couto JM, Higham CF, et al. Somatic instability of the expanded CTG triplet repeat in myotonic dystrophy type 1 is a heritable quantitative trait and modifier of disease severity. Hum Mol Genet. 2012;21:3558–3567. [DOI] [PubMed] [Google Scholar]
- 12. Swami M, Hendricks AE, Gillis T, et al. Somatic expansion of the Huntington’s disease CAG repeat in the brain is associated with an earlier age of disease onset. Hum Mol Genet. 2009;18:3039–3047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Nordin A, Akimoto C, Wuolikainen A, et al. Extensive size variability of the GGGGCC expansion in C9orf72 in both neuronal and non-neuronal tissues in 18 patients with ALS or FTD. Hum Mol Genet. 2015;24:3133–3142. [DOI] [PubMed] [Google Scholar]
- 14. Filla A, De Michele G, Cavalcanti F, et al. The relationship between trinucleotide (GAA) repeat length and clinical features in Friedreich ataxia. Am J Hum Genet. 1996;59:554–560. [PMC free article] [PubMed] [Google Scholar]
- 15. Dürr A, Cossee M, Agid Y, et al. Clinical and genetic abnormalities in patients with Friedreich’s ataxia. N Engl J Med. 1996;335:1169–1175. [DOI] [PubMed] [Google Scholar]
- 16. Figueroa KP, Coon H, Santos N, Velazquez L, Mederos LA, Pulst SM. Genetic analysis of age at onset variation in spinocerebellar ataxia type 2. Neurol Genet. 2017;3:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Johansson J, Forsgren L, Sandgren O, Brice A, Holmgren G, Holmberg M. Expanded CAG repeats in Swedish spinocerebellar ataxia type 7 (SCA7) patients: Effect of CAG repeat length on the clinical manifestation. Hum Mol Genet. 1998;7:171–176. [DOI] [PubMed] [Google Scholar]
- 18. Jodice C, Malaspina P, Persichetti F, et al. Effect of trinucleotide repeat length and parental sex on phenotypic variation in spinocerebellar ataxia I. Am J Hum Genet. 1994;54:959–965. [PMC free article] [PubMed] [Google Scholar]
- 19. Orr HT, Chung M-y, Banfi S, et al. Expansion of an unstable trinucleotide CAG repeat in spinocerebellar ataxia type 1. Nat Genet. 1993;4:221–226. [DOI] [PubMed] [Google Scholar]
- 20. Komure O, Sano A, Nishino N, et al. DNA analysis in hereditary dentatorubral-pallidoluysian atrophy: Correlation between CAG repeat length and phenotypic variation and the molecular basis of anticipation. Neurology. 1995;45:143–149. [DOI] [PubMed] [Google Scholar]
- 21. Brook JD, McCurrach ME, Harley HG, et al. Molecular basis of myotonic dystrophy: Expansion of a trinucleotide (CTG) repeat at the 3′ end of a transcript encoding a protein kinase family member. Cell. 1992;68:799–808. [DOI] [PubMed] [Google Scholar]
- 22. Richard P, Trollet C, Stojkovic T, et al. Correlation between PABPN1 genotype and disease severity in oculopharyngeal muscular dystrophy. Neurology. 2017;88:359–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cortese A, Simone R, Sullivan R, et al. Biallelic expansion of an intronic repeat in RFC1 is a common cause of late-onset ataxia. Nat Genet. 2019;51:649–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rafehi H, Szmulewicz DJ, Bennett MF, et al. Bioinformatics-based identification of expanded repeats: A non-reference intronic pentamer expansion in RFC1 causes CANVAS. Am J Hum Genet. 2019;105:151–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Fan Y, Zhang S, Yang J, et al. No biallelic intronic AAGGG repeat expansion in RFC1 was found in patients with late-onset ataxia and MSA. Park Relat Disord. 2020;73:1–2. [DOI] [PubMed] [Google Scholar]
- 26. Aboud Syriani D, Wong D, Andani S, et al. Prevalence of RFC1-mediated spinocerebellar ataxia in a North American ataxia cohort. Neurol Genet. 2020;6:e440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Akçimen F, Ross JP, Bourassa CV, et al. Investigation of the RFC1 repeat expansion in a Canadian and a Brazilian ataxia cohort: Identification of novel conformations. Front Genet. 2019;10:1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Tsuchiya M, Nan H, Koh K, et al. RFC1 repeat expansion in Japanese patients with late-onset cerebellar ataxia. J Hum Genet. 2020;65:1143–1147. [DOI] [PubMed] [Google Scholar]
- 29. Traschütz A, Cortese A, Reich S, et al. Natural history, phenotypic Spectrum, and discriminative features of multisystemic RFC1 disease. Neurology. 2021;96:e1369-e1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Beecroft SJ, Cortese A, Sullivan R, et al. A Māori specific RFC1 pathogenic repeat configuration in CANVAS, likely due to a founder allele. Brain. 2020;143:2673–2680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Scriba CK, Beecroft SJ, Clayton JS, et al. A novel RFC1 repeat motif (ACAGG) in two Asia-Pacific CANVAS families. Brain. 2020;143:2904–2910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ronco R, Perini C, Currò R, et al. Truncating variants in RFC1 in cerebellar ataxia, neuropathy, and vestibular areflexia syndrome. Neurology. 2023;100:e543-554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Benkirane M, Da Cunha D, Marelli C, et al. RFC1 nonsense and frameshift variants cause CANVAS: Clues for an unsolved pathophysiology. Brain. 2022;145:3770–3775. [DOI] [PubMed] [Google Scholar]
- 34. King KA, Wegner DJ, Bucelli RC, et al. Whole-Genome and long-read sequencing identify a novel mechanism in RFC1 resulting in CANVAS syndrome. Neurol Genet. 2022;8:e200036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Arteche-López A, Avila-Fernandez A, Damian A, et al. New Cerebellar Ataxia, Neuropathy, Vestibular Areflexia Syndrome cases are caused by the presence of a nonsense variant in compound heterozygosity with the pathogenic repeat expansion in the RFC1 gene. Clin Genet. 2023;103:236–241. [DOI] [PubMed] [Google Scholar]
- 36. Currò R, Salvalaggio A, Tozza S, et al. RFC1 expansions are a common cause of idiopathic sensory neuropathy. Brain. 2021;144:1542–1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Tagliapietra M, Cardellini D, Ferrarini M, et al. RFC1 AAGGG repeat expansion masquerading as Chronic Idiopathic Axonal Polyneuropathy. J Neurol. 2021;268:4280–4290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Cortese A, Tozza S, Yau WY, et al. Cerebellar ataxia, neuropathy, vestibular areflexia syndrome due to RFC1 repeat expansion. Brain. 2020;143:480–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. England JD, Gronseth GS, Franklin G, et al. Distal symmetric polyneuropathy: A definition for clinical research—Report of the American Academy of Neurology, the American Association of Electrodiagnostic Medicine, and the American Academy of Physical Medicine and Rehabilitation. Neurology. 2005;64:199–207. [DOI] [PubMed] [Google Scholar]
- 40. Freeman R, Gewandter JS, Faber CG, et al. Idiopathic distal sensory polyneuropathy: ACTTION diagnostic criteria. Neurology. 2020;95:1005–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Szmulewicz DJ, Roberts L, McLean CA, MacDougall HG, Michael Halmagyi G, Storey E. Proposed diagnostic criteria for cerebellar ataxia with neuropathy and vestibular areflexia syndrome (CANVAS). Neurol Clin Pract. 2016;6:61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Cortese A, Curro’ R, Vegezzi E, Yau WY, Houlden H, Reilly MM. Cerebellar ataxia, neuropathy and vestibular areflexia syndrome (CANVAS): Genetic and clinical aspects. Pract Neurol. 2022;22:14–18. [DOI] [PubMed] [Google Scholar]
- 43. Cardoso MJ, Modat M, Wolz R, et al. Geodesic information flows: Spatially-variant graphs and their application to segmentation and fusion. IEEE Trans Med Imaging. 2015;34:1976–1988. [DOI] [PubMed] [Google Scholar]
- 44. Prados F, Cardoso MJ, Burgos N, Wheeler-Kingshott CAMG, Ourselin S. NiftyWeb: web based platform for image processing on the cloud. In: 24th Scientific Meeting and Exhibition of the International Society for Magnetic Resonance in Medicine. Singapore. 2016.
- 45. Klein A, Tourville J. 101 labeled brain images and a consistent human cortical labeling protocol. Front Neurosci. 2012;6:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ghorbani F, de Boer-Bergsma J, Verschuuren-Bemelmans CC, et al. Prevalence of intronic repeat expansions in RFC1 in Dutch patients with CANVAS and adult-onset ataxia. J Neurol. 2022;269:6086–6093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Dai Y, Li P, Wang Z, et al. Single-molecule optical mapping enables quantitative measurement of D4Z4 repeats in facioscapulohumeral muscular dystrophy (FSHD). J Med Genet. 2020;57:109–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. van Blitterswijk M, DeJesus-Hernandez M, Niemantsverdriet E, et al. Association between repeat sizes and clinical and pathological characteristics in carriers of C9ORF72 repeat expansions (Xpansize-72): A cross-sectional cohort study. Lancet Neurol. 2013;12:978–988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Eurostat . Mortality and life expectancy statistics. Accessed 25 April 2022. Data extracted from Eurostat Web site: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Mortality_and_life_expectancy_statistics#Life_expectancy_at_birth
- 50. Chiò A, Logroscino G, Hardiman O, et al. Prognostic factors in ALS: A critical review. Amyotroph Lateral Scler. 2009;10(5–6):310–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kjældgaard AL, Pilely K, Olsen KS, et al. Prediction of survival in amyotrophic lateral sclerosis: A nationwide, Danish cohort study. BMC Neurol. 2021;21:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Westeneng HJ, Debray TPA, Visser AE, et al. Prognosis for patients with amyotrophic lateral sclerosis: Development and validation of a personalised prediction model. Lancet Neurol. 2018;17:423–433. [DOI] [PubMed] [Google Scholar]
- 53. Glasmacher SA, Wong C, Pearson IE, Pal S. Survival and prognostic factors in C9orf72 repeat expansion carriers: A systematic review and meta-analysis. JAMA Neurol. 2020;77:367–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Szmulewicz DJ, McLean CA, Rodriguez ML, et al. Dorsal root ganglionopathy is responsible for the sensory impairment in CANVAS. Neurology. 2014;82:1410–1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Szmulewicz DJ, Waterston JA, Macdougall HG, et al. Cerebellar ataxia, neuropathy, vestibular areflexia syndrome (CANVAS): A review of the clinical features and video-oculographic diagnosis. Ann N Y Acad Sci. 2011;1233:139–147. [DOI] [PubMed] [Google Scholar]
- 56. Ranen NG, Stine OC, Abbott MH, et al. Anticipation and instability of IT-15 (CAG)(N) repeats in parent-offspring pairs with Huntington disease. Am J Hum Genet. 1995;57:593–602. [PMC free article] [PubMed] [Google Scholar]
- 57. Duyao M, Ambrose C, Myers R, et al. Trinucleotide repeat length instability and age of onset in Huntington’s disease. Nat Genet. 1993;4:387–392. [DOI] [PubMed] [Google Scholar]
- 58. Fu YH, Pizzuti A, Fenwick RG, et al. An unstable triplet repeat in a gene related to myotonic muscular dystrophy. Science. 1992;255:1256–1258. [DOI] [PubMed] [Google Scholar]
- 59. Nolin SL, Glicksman A, Tortora N, et al. Expansions and contractions of the FMR1 CGG repeat in 5,508 transmissions of normal, intermediate, and premutation alleles. Am J Med Genet Part A. 2019;179:1148–1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Campuzano V, Montermini L, Moltò MD, et al. Friedreich’s ataxia: Autosomal recessive disease caused by an intronic GAA triplet repeat expansion. Science. 1996;271:1423–1427. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
With publication, de-identified data collected for the study, including individual participant data and a data dictionary defining each field in the set, can be made available to interested parties on reasonable request, and if in line with privacy regulations. Data can be requested at least 18 months after publication of this manuscript by sending an e-mail to the corresponding author.