Abstract
The odontogenic keratocyst (OKC) is a frequently developing odontogenic cyst that accounts for 10%–14% of all jaw cysts. Due to the high recurrence rate, aggressive therapeutic techniques such as jaw resection and marsupialization are indicated. Following a conservative marsupialization procedure in which Carnoy’s solution and an iodoform packing were used, the clinical, radiological, and histological evaluation of OKC in a 12-year-old female patient revealed no evidence of recurrence over the subsequent year of follow-up.
Keywords: Carnoy’s solution, case report, marsupialization, odontogenic keratocyst, thermoplastic splint
Introduction
Odontogenic cysts make up the vast majority of maxillofacial cystic lesions. Cysts have traditionally been classified as either developing, such as keratocysts and dentigerous cysts, or inflammatory, such as radicular cysts.[1,2,3]
The odontogenic keratocyst (OKC), first described by Philipsen in 1956, is also known as a keratocystic odontogenic tumor (KCOT) by the World Health Organization.[4,5] However, the WHO revised its classification of head and neck tumors in 2017. The pathology mentioned above could not be classified as a neoplastic lesion due to insufficient evidence; hence, KCOT was reclassified as an OKC and returned to the cyst category (OKC). The term “keratocystic odontogenic tumor” persists. In contrast to the first decade, it is often recorded in the second through fourth decades.[6]
Its multicentric development pattern allows it to invade cortical bone and neighboring soft tissue.[3] Treatment of KCOTs remains controversial due to their high recurrence rate.[7,8,9,10] The first surgical procedures in KCOT are occasionally decompression or marsupialization, and when the volume gets too small, enucleation is required.[11,12]
To avoid recurrence, aggressive treatment of this lesion is advised. If the patient is a child with unerupted permanent teeth in the OKC-affected area, the decision to proceed with intensive therapy may be difficult. Thus, children frequently get conservative therapies to minimize the complications linked to invasive procedures.[7] One such conservative method in children and teenagers is marsupialization alone or associated with additional measures (osteotomy, Carnoy’s solution, and cryotherapy).[2,8,9,10,13]
In this case report, we present a case of OKC in a young child who was treated with marsupialization, followed by Carnoy’s solution, iodoform dressing, and a thermoplastic splint.
Case Report
A 12-year-old pediatric patient reported to our department, Department of Pediatric and Preventive Dentistry, Institute of Dental Sciences Bareilly, Uttar Pradesh, for a cystic lesion located in the posterior right mandible with clinical and radiological features of a dentigerous cyst since 1 year.
There were no palpable pulsations or pus discharge seen on the extra oral examination, but there was facial asymmetry due to swelling detected on the mandibular right side of the face [Figure 1a]. Upon intraoral inspection, it was observed that the right mandibular region, extending from the permanent lateral incisor to the first molar, exhibited full obliteration buccally. However, the adjacent mucosa appeared to be in a healthy state. The swelling was painful, stable, and bone-like in texture [Figure 1b]. From the first right molar through the first left molar, all of the maxillary teeth were present and intact [Figure 2a]. The mandibular arch consisted of retained deciduous teeth: 71, 74, 81, 83, 84, and 85. This caused malpositioning of 41 and crowding in the mandibular anterior region. 44 and 45 were clinically absent [Figure 2b].
Figure 1.

(a) Preoperative view showing asymmetry of face due to swelling, (b) Intraoral swelling present on the right side of the lower vestibule
Figure 2.
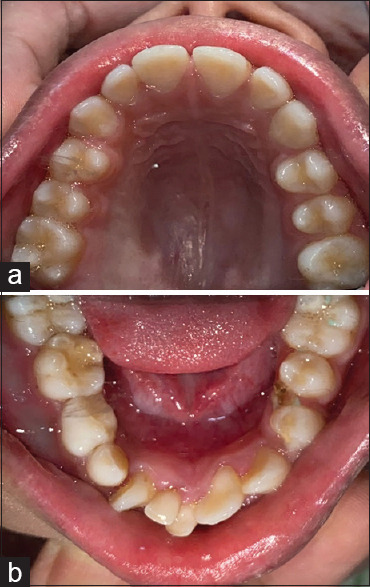
(a) Intra oral picture showing normal maxilla (b) Retained deciduous teeth in the mandibular anterior region
A panoramic radiographic examination of the patient’s right mandible revealed a single, well-defined radiolucency measuring about 3 by 3.5 centimeters and extending anteroposteriorly from the mesial aspect of 33 to the mesial side of 46. As the lesion grew, it pushed the permanent canine tooth bud downward and forward below the incisors and the premolar tooth bud downward and backward below the permanent molar. The roots of deciduous first and second molars have undergone resorption [Figure 3].
Figure 3.

Pre-operative orthopantomogram
Thereafter, to properly assess the lesion, a computed tomography (CT) scan was carried out. This revealed a huge expansile cystic lesion that covered the entire right half of the body and measured around 3.3 cm × 5.5 cm × 3 cm. On the right side of the mandible, the buccal and lingual cortical plates were enlarged [Figure 4]. A dentigerous cyst was provisionally diagnosed based on clinical and radiological evidence. OKC, dentigerous cyst, buccal bifurcation cyst, and unicystic ameloblastoma were all suspected diagnoses; thus, a histological analysis was performed.
Figure 4.
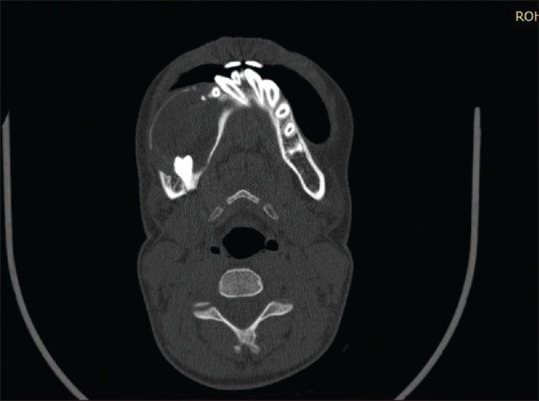
Computed tomography scan of face
Because of the lesion’s size, age, anatomical structures, affected teeth, and thin border of bone at the border of the mandible that had a high risk of fracture on surgical intervention, an incisional biopsy followed by marsupialization was planned. Both the parent’s and patient’s informed consent was taken before starting the procedure. The cyst was completely removed through a 2.5 cm × 1.5 cm window [Figure 5], and then Carnoy’s Solution was carefully applied. After being removed, the lesion was sent for histological analysis. Moreover, no paresthesia was observed following the application of carnoy solution (CS), and neither was there any harm done to the thin bone walls of the sinus or the periodontium of the nearby vital tooth.
Figure 5.
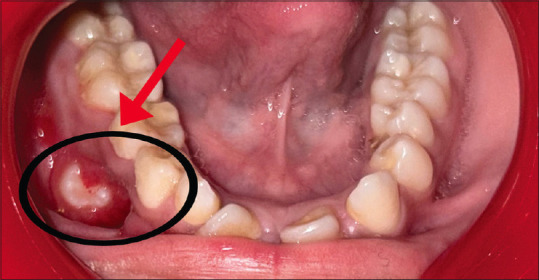
Red arrow indicates the window created and black circle indicates the size of the window generated as part of marsupialization.
A fluid with the color of red wine was collected by fine needle aspiration cytology using a 5 ml syringe. Cytopathological examination of the aspirate revealed features typical of a keratin-filled lesion, including an abundance of neutrophils, a dearth of nucleated epithelial cells, and an abundance of keratinocytes set against a hemorrhagic background [Figure 6]. Biopsy findings revealed parakeratinized stratified epithelial lining with prominent columnar basal cell layer, surface corrugation, and neutrophils, lymphocytes arranged against extravasated red blood cells, which confirmed the diagnosis of Odongenic Keratocyst [Figure 7].
Figure 6.
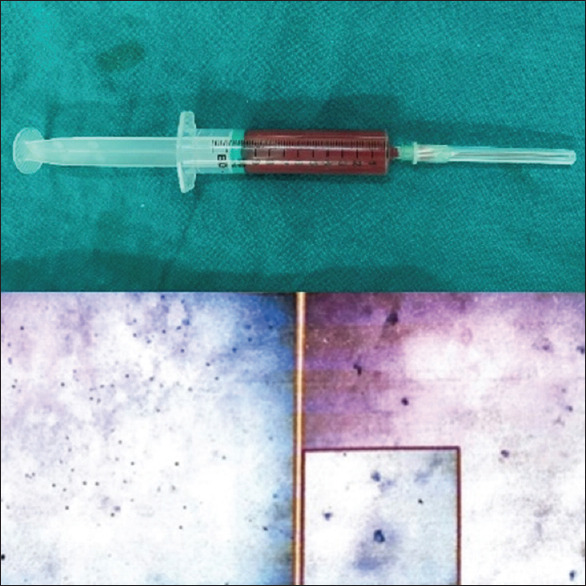
Final needle aspiration cytology (FNAC) aspirate showing a high concentration of neutrophils, a low number of nucleated epithelial cells, and a high concentration of keratinocytes against a hemorrhagic backdrop
Figure 7.

Biopsy of the patient showing the presence of a parakaratinizd stratified epithelial lining with a large columnar basal cell layer, surface corrugation, and neutrophils, lymphocytes organised against extravasated red blood cells
After receiving conservative treatment, the patient was evaluated every 3rd day and was instructed to maintain oral hygiene. Every 3rd day, the iodoform dressing was replaced. The cavity was irrigated with betadine. Interrupted sutures were applied after inserting an iodoform gauze tail that made contact with the cavity wall. This process took place for 4 months. Between these intervals, the use of CS as adjuvant therapy was carried out.
The importance of good dental hygiene was stressed once more, and the patient was instructed to replace the iodoform dressing daily for the next 5 months. A thermoplastic splint was also placed over the opening to prevent bacteria from entering the cavity [Figure 8].
Figure 8.

Thermoplastic splint
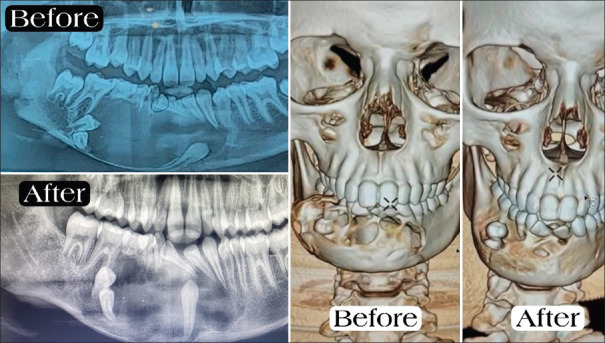
An orthopantomogram (OPG) and CT scan were performed after 4 months, and the results showed increased bone density. The impacted teeth’s position shifted, indicating upright movement. The cystic lesion shrank and was 2 × 4.2 × 1.8 in size. The maximum preoperative thickness of the inferior and posterior cortex of the mandible was 1.6 mm and 1.7 mm, respectively. Postoperative thickness was 6.0 mm and 4.0 mm (thickness measured in right hemimandible) [Figure 9].
Figure 9.
Orthopantomogram and computed tomography scan after 4 months
After obtaining an OPG showing movement and eruptive capacity of teeth 43, 44, and 45, extraction of retained deciduous teeth 83, 84, and 85 was planned under local anesthesia (LA). The patient was recalled every 1 month for evaluation.
Outcome and follow-up: After a year, an OPG was performed, which indicated the typical eruptive force of 44 and 45 in the usual place, with no evidence of recurrence and the patient being asymptomatic [Figure 10]. The patient continues to be examined when undergoing orthodontic treatment for lower anterior crowding and unerupted 43, 44, and 45.
Figure 10.
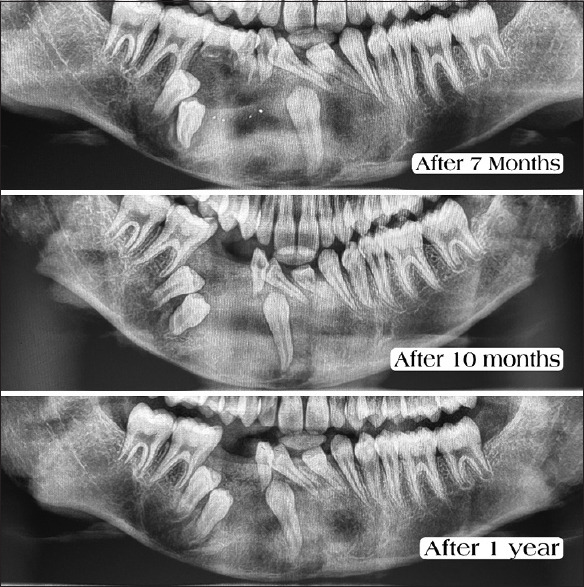
Post-operative orthopantomogram after 7 months, 10 months and 1 year
Discussion
Common odontogenic cysts (OKCs) develop in the mandible three times more frequently than in the maxilla. Common locations include the spaces between the canine and premolar, the mandibular retromolar and ramus, and the maxillary second permanent molar.[14]
Odontogenic myxoma, traumatic cyst, dentigerous cyst, and giant cell granuloma (typically in the anterior region of the jaw) are all possible differential diagnoses. In OKC, the cyst is connected to the tooth at a point apical to the cementoenamel junction.[15]
As seen on radiographs, OKCs in children and teenagers displace the teeth throughout the length of the jaw. Histopathologically, OKCs have a connective tissue capsule coated with para-keratinized stratified squamous epithelium (5–8 layers thick). Hyperchromatic nuclei are organized in a palisade pattern in the columnar epithelial cells of the basal layer. At the junction of the epithelium and connective tissue, no epithelial projections are present. The consistency of the luminal material is like that of a caseous, cheesy, thick, milk-white mass. Straw-colored fluid, thick pus-like substance, and similar words have been used to describe it.[16] In this case, classical histologic features of OKC were present.
Management of the OKC is controversial. Both conservative and aggressive treatments are common. One form of conservative treatment is simple marsupialization, which may or may not be accompanied by curettage using spoon curettes. Large cysts that include numerous teeth and anatomic components that have yet to emerge are reportedly best treated by marsupialization (Partsch I procedure).[17] By shrinking the lesion, more invasive surgery can be avoided, and healthy tissue can be protected.[7]
Surgeons have different opinions on whether the cyst must be enucleated or left intact if removed. Limitations in surgical access, the skill and experience of the surgeon, the risk of perforating the OKC’s cortical lining, and the need to safeguard neighboring vital structures all increase the difficulty of removing the OKC in its entirety. Minimizing postoperative complications while eliminating the risk of recurrence should be the primary therapeutic goal. There is disagreement on how long this lesion should be left untreated. Marx and Stern state that insufficient cyst clearance and the development of new primary cysts are the two most common reasons for recurrence.[17]
To reduce the probability of reoccurrence, it has been proposed to perform marsupialization together with excision of the soft tissue that covers the OKC. Before performing cyst marsupialization, some studies have advocated the utilization of Carnoy’s solution (comprised of absolute alcohol, chloroform, glacial acetic acid, and ferric chloride) for tanning purposes. Accordingly, this approach was implemented in the present case. After the surgical procedure, it is common practice to excise the underlying mucosa along with the lesion.[18]
Even though it has some benefits, it also has some drawbacks, such as a longer healing time, pain for the patient, the need for twice-daily irrigation, and the need to change the surgical splint once a week to keep the cystic hole open.[19] Different tools, like tubes, gauzes, obturators, and acrylic stents, can treat cystic windows. However, due to problems like retention failure, increased porosity, the irritating effect of residual monomer, and the trouble of processing, thermoformed devices are becoming more popular.[17] In this case, a thermoform splint was used. It is made of acetal resin and polyoxymethylene. It stays in the right place because there is negative pressure inside the mouth. This obturator has many benefits, such as being easy to take out to clean the hollow, nontoxic, nonallergic, flexible, and resistant to wear and breakage, which makes it a good choice for a surgical stent.[20]
Ziccardi et al. used a marsupialization stent and a space maintainer to keep space for teeth that have not erupted yet.[21] In this case, a space maintainer or orthodontic traction was not needed because the thermoform splint kept the space between existing teeth and allowed the teeth that were out of place to emerge in the right position.
In children with unerupted teeth, aggressive interventions endanger the eruption process and the growth of the affected jaw; therefore, a conservative approach should be preferred.[22] As a result, conservative treatment should be recommended over aggressive treatment in young patients.
Conclusion
This study suggests that several patient parameters, including age, general health, and lesion features, should be taken into account when deciding on the best course of treatment. Treatment by marsupialization was conducted in this case, and there was no recurrence at the 1-year follow-up despite the patient’s young age and the subsequent expansion of the mandible and facial contour. Although marsupialization is an unorthodox approach to treating OKC, it has proven to be highly beneficial in children whose lesions are close to the tooth buds and other critical tissues in the jaws. At least annually and for 6 years after the surgical intervention, patients with a diagnosis of OKC should be evaluated in outpatient clinics with follow-up orthopantomography and contrast enhanced CT.
Patient’s perspective
The patient and her family were pleased with the therapy they received because the patient’s major issue was the swelling, which caused her pain and difficulties eating. The patient also desires additional orthodontic treatment for the unerupted teeth for esthetic reasons.
Informed consent: The authors declare that they have all the necessary consent forms from the patient. On the form, the patient has given their permission for the pictures and other clinical details to be published in the journal. The patients know that their names and initials won’t be released and that every effort will be made to keep them anonymous, but this can’t be guaranteed.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.High AS, Robinson PA, Klein CE. Discrimination of parakeratinised odontogenic keratocysts from other odontogenic and non-odontogenic cyst types by expression of a 38kd cell-surface glycoprotein. J Oral Pathol Med. 1993;22:363–7. doi: 10.1111/j.1600-0714.1993.tb01090.x. [DOI] [PubMed] [Google Scholar]
- 2.Stoelinga PJ. Long-term follow-up on keratocysts treated according to a defined protocol. Int J Oral Maxillofac Surg. 2001;30:14–25. doi: 10.1054/ijom.2000.0027. [DOI] [PubMed] [Google Scholar]
- 3.Myoung H, Hong SP, Hong SD, Lee JI, Lim CY, Choung PH, et al. Odontogenic keratocyst: Review of 256 cases for recurrence and clinicopathologic parameters. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:328–33. doi: 10.1067/moe.2001.113109. [DOI] [PubMed] [Google Scholar]
- 4.Kaczmarzyk T, Stypułkowska J, Tomaszewska R. Update of the WHO classification of odontogenic and maxillofacial bone tumors. J Stomatol. 2017;70:484–506. [Google Scholar]
- 5.Soluk-Tekkeşin M, Wright JM. The World Health Organization 37 classification of odontogenic lesions: A summary of the changes 38 of the 2017 (4th) edition. Turk Patoloji Derg. 2018;34:1–18. doi: 10.5146/tjpath.2017.01410. [doi: 10.5146/tjpath. 2017.01410] [DOI] [PubMed] [Google Scholar]
- 6.Telles DC, Castro WH, Gomez RS, Souto GR, Mesquita RA. Morphometric evaluation of keratocystic odontogenic tumor before and after marsupialization. Braz Oral Res. 2013;27:496–502. doi: 10.1590/S1806-83242013000600009. [DOI] [PubMed] [Google Scholar]
- 7.Kim J, Nam E, Yoon S. Conservative managemen (marsupialization) of unicystic ameloblastoma: Literature review and a case report. Maxillofac Plast Reconstr Surg. 2017;39:38. doi: 10.1186/s40902-017-0134-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Güler N, Sençift K, Demirkol O. Conservative management of keratocystic odontogenic tumors of jaws. ScientificWorldJournal 2012. 2012 doi: 10.1100/2012/680397. 680397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaczmarzyk T, Mojsa I, Stypulkowska J. A systematic review of the recurrence rate for keratocystic odontogenic tumour in relation to treatment modalities. Int J Oral Maxillofac Surg. 2012;41:756–67. doi: 10.1016/j.ijom.2012.02.008. [DOI] [PubMed] [Google Scholar]
- 10.Johnson NR, Batstone MD, Savage NW. Management and recurrence of keratocystic odontogenic tumor: A systematic review. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:e271–6. doi: 10.1016/j.oooo.2011.12.028. [DOI] [PubMed] [Google Scholar]
- 11.Patil K, Mahima VG, Gupta B. Gorlin syndrome: A case report. J Indian Soc Pedod Prev Dent. 2005;23:198–203. doi: 10.4103/0970-4388.19010. [DOI] [PubMed] [Google Scholar]
- 12.Shear M. The aggressive nature of the odontogenic keratocyst: Is it a benign cystic neoplasm? Part 1. Clinical and early experimental evidence of aggressive behaviour. Oral Oncol. 2002;38:219–26. doi: 10.1016/s1368-8375(01)00065-3. [DOI] [PubMed] [Google Scholar]
- 13.Morgan TA, Burton CC, Qian F. A retrospective review of treatment of the odontogenic keratocyst. J Oral Maxillofac Surg. 2005;63:635–9. doi: 10.1016/j.joms.2004.07.026. [DOI] [PubMed] [Google Scholar]
- 14.Khalam AS, Zacariah RK. Under diagnosis of an odontogenic keratocyst-a controversial lesion. IOSR J Dent Med Sci. 2012;2:37–40. [Google Scholar]
- 15.Garg S, Sunil MK, Trivedi A, Singla N. Odontogenic keratocyst of the angle and ramus of the mandible-a case report. J Dent Spec. 2015;3:195–8. [Google Scholar]
- 16.Rajkumar GC, Hemalatha M, Shashikala R, Sonal P. Massive keratocystic odontogenic tumor of mandible: A case report and review of literature. Indian J Dent Res. 2011;22:181. doi: 10.4103/0970-9290.80000. [DOI] [PubMed] [Google Scholar]
- 17.Briki S, Elleuch W, Karray F, Abdelmoula M, Tanoubi I. Cysts and tumors of the jaws treated by marsupialization: A description of 4 clinical cases. J Clin Exp Dent. 2019;11:e565–9. doi: 10.4317/jced.55563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Webb DJ, Brockbank J. Treatment of the odontogenic keratocyst by combined enucleation and cryosurgery. Int J Oral Surg. 1984;13:506–10. doi: 10.1016/s0300-9785(84)80021-6. [DOI] [PubMed] [Google Scholar]
- 19.Bataineh AB, al Qudah M. Treatment of mandibular odontogenic keratocysts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:42–7. doi: 10.1016/s1079-2104(98)90148-2. [DOI] [PubMed] [Google Scholar]
- 20.Checherita L, Beldiman MA, Stamatin O, Foia L, Forna NC. Aspects on structure of materials used for different types of occlusal splints. Rev Chim. 2013;64:864–7. [Google Scholar]
- 21.Wiemer SJ, Pruitt CA, Rallis DJ, Viozzi CF. Use of a modified removable partial denture as a marsupialization stent in a pediatric patient. J Oral Maxillofac Surg. 2013;71:1382–6. doi: 10.1016/j.joms.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 22.Hyun HK, Hong SD, Kim JW. Recurrent keratocystic odontogenic tumor in the mandible: A case report and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:e7–10. doi: 10.1016/j.tripleo.2009.04.030. [DOI] [PubMed] [Google Scholar]