INTRODUCTION
The experience of being diagnosed and treated for a blood cancer is complex, with many deeply personal and difficult turning points for an individual and his or her family. Blood cancer survivors, those diagnosed more recently, and their caregivers benefit from receiving step-by-step support in a personalized, individual-focused manner. They need this support across all aspects of their lives and for the duration of their cancer experience. People affected by a blood cancer require practical information and programs addressing day-to-day living, as well as psychosocial, familial, and mental health support from diagnosis through to long-term survivorship or palliative care.
Meeting these needs is best served through a partnership between healthcare professionals (HCPs) and the nonprofit sector supporting people affected by a blood cancer. The Leukemia & Lymphoma Society of Canada (LLSC) partners with healthcare professionals (HCPs) to help Canadians affected by a blood cancer.
In 2018, the LLSC decided to make the effort to better understand the experiences and preferences of people affected by a blood cancer. We wanted to hear directly about their perspectives by talking to:
-
Patients, survivors, and their caregivers on:
Their awareness of LLSC resources and services,
Their use of those resources and services, and
What they need at each step of their cancer experience.
-
Healthcare professionals in hematology-oncology, on:
Their awareness of LLSC resources and services,
Referral of their blood cancer patients and caregivers to LLSC resources and services, and
What they need from LLSC to help them support their blood cancer patients.
METHODS
Between June 2018 and January 2019, independent market research was undertaken by the healthcare division of Leger, a large, Canadian-owned market research and analytics company established in 1986. LLSC procured the services after assessing various Canadian firms. All interviews, in person and by telephone, were conducted by Leger staff. Questions for the interviews and for the survey were co-developed by LLSC and Leger. Analysis of the data, separately for HCPs and for patients/survivors/caregivers, was conducted by analysts at Leger.
Phase 1 – Qualitative pilot interviews were held on June 28, 2018 in Toronto, to test and adjust materials to ensure they met the project objectives. That pilot group included seven patients/survivors/caregivers and two HCPs.
Phase 2 – Qualitative interviews were held between August and November 2018, by telephone and in person, at facilities in Toronto, Montreal, Quebec City, Halifax, Calgary, and Vancouver. In all, 50 patients/survivors/caregivers, and 20 HCPs were interviewed to explore their experiences and perspectives in an in-depth manner.
Phase 3 – Quantitative surveys were distributed from September 2018 – January 2019. The (10–15 minute) online survey was distributed to 607 patients/caregivers/survivors, and 75 HCPs across Canada.
Participants affected by a blood cancer
Patients/survivors/caregivers were primarily recruited by LLSC through emails to individuals in their databases, as well as through ads sent via LLSC’s social media channels, such as Facebook. The Leger panel was used to recruit participants to supplement the number of participants and to assess differences between those unfamiliar with LLSC and those familiar with LLSC. Recruitment specifications for people affected by a blood cancer – for qualitative and quantitative research – were:
18 years or older.
Diagnosed with a blood cancer at any time; or has a family member ever diagnosed with a blood cancer.
Caregivers were required to be actively involved in the patient’s care, including participating in medical treatment decisions/discussions.
For the qualitative research (interviews)
19 survivors, 15 newly diagnosed patients, and 16 caregivers were interviewed in Toronto, Montreal, Halifax, Calgary, Vancouver, Quebec City, Prairies, and Ottawa (in descending order of numbers of interviewees). Two-thirds of interviewees were female. About half were ages 55 to 65; one-third were 25 to 55; and 20% were older than 65.
Participants in the qualitative interviews represented a range of blood cancers: non-Hodgkin lymphoma (NHL); chronic lymphocytic leukemia (CLL); multiple myeloma (MM); Hodgkin lymphoma (HL): chronic myeloid leukemia (CML); acute myeloid leukemia (AML); acute lymphoblastic leukemia (ALL); myelodysplastic syndromes (MDS); myeloproliferative neoplasms (MPN).
For the quantitative research (online survey)
487 patients and 120 caregivers across the country took the anonymous survey – the most lived in Quebec (179), Ontario (122), and Atlantic Canada (118). Participants in the quantitative (survey) phase represented the same range of blood cancers as with the qualitative interviews: NHL; CLL; MM; HL; CML; AML; ALL; MDS; and MPN.
For the quantitative phase, a different, larger set of individuals were selected than for the qualitative phase. Individuals were pre-screened before they were sent the survey. Demographic questions were included as part of the screening process to be sure a wide representation of types of blood cancers, ages, genders, years since diagnosis, province/territory, and patient/survivor/caregiver. Patients were asked about 40 survey questions and caregivers about 45 questions – primarily the same questions.
Healthcare professionals participants
Leger primarily recruited healthcare professionals within Leger’s databases; LLSC recruited some HCPs through emails to its targeted HCP lists. Healthcare professionals worked in a range of settings from academia to community cancer centres.
For the qualitative interviews
Six hematologists, seven nurses, and seven oncology social workers were interviewed. Recruitment specifications were:
All the physicians were managing and treating hematological cancers.
All the nurses and social workers were involved in counselling and educating patients.
Nurses were either primary care oncology nurses or chemotherapy nurses.
For the quantitative (online surveys) research
Recruitment specifications were:
In active clinical practice for at least one year.
Working at least 26 hours a week.
Managing patients with at least one blood cancer type.
For the HCP survey (about 20 questions), participants included 50 physicians – specifically hematologist oncologists, hematologists, and medical oncologists – and 25 oncology nurses – chemotherapy nurses, as well as primary or pivotal nurses.
KEY FINDINGS AND ACTUALIZATIONS
From the start of the research project, LLSC made the commitment that “findings will guide benchmarking and assist in our development of materials/programs/services and create a positioning platform for the organization.” The following findings provide examples of how those objectives have been met (and continue to be met) since the research concluded.
Most of the findings come from the interviews and surveys of patients, survivors, and caregivers – identifying the reality of the blood cancer experience in Canada, as well as how they would like their experience to unfold. The number of research participants was substantially larger (seven-fold) compared to healthcare professionals, and healthcare professionals were asked a smaller set of questions. Where applicable, we have noted HCP perspectives, too, in these findings.
Finding: Need for personalized support
There was a clear message conveyed by people affected by a blood cancer: Treat me as an individual, not as a statistic or diagnosis. They wanted frequent, personalized connections and touch-points for support and services. In other words, they wanted to know they are “not alone.” Many patients/survivors/caregivers noted in interviews that, although they felt supported by their healthcare team and their families and friends, they did not always feel fully understood about their cancer experience, what they were going through and feeling emotionally. Almost a quarter of nurses interviewed in the research said they ranked the provision of emotional support to patients/families/survivors as “the most important service expected from LLSC.”
Peer support
Research participants resonated strongly with the concept of peer support, identifying their need to connect with someone who “gets it” (i.e., having or caring for someone who has a blood cancer). LLSC’s First Connection (FC) peer support program was very well received by research participants. Unfortunately, most people affected by a blood cancer said they had never heard of the program before the research. FC turned out to be the least known and least used program of LLSC.
“I would have liked it if they provided me with someone I could talk to who had gone through it [blood cancer experience]...It would have been nice to know about.”
Actualization: Personalized support expanded
The message about not having to go through the cancer experience alone is one that LLSC has been using over the past few years. The model of service at LLSC has, in recent years, been transformed, so that personalized support for people affected with a blood cancer is prioritized. The LLSC eschews automated, impersonal, or generic contact in any realm of need; they acknowledge that a real, live human is at the other end of every phone call and email to LLSC. People affected by a blood cancer interact with the same LLSC employee throughout their cancer experience; roles are designated by geographic region and unchanging.
The LLSC has also worked to broaden the reach of its existing support programs and worked to provide peer support in the most meaningful way (i.e., the right people at right time in the right way). This approach has been shown to have a positive impact on health outcomes (Allicock et al., 2014). The LLSC provides peer support in two programs.
One-on-one peer matching
Years before the market research was conducted, LLSC had been providing 1:1 peer matches for individuals living with a blood cancer. This occurred through its First Connection (FC) Program, where volunteer peers are trained, monitored, and supported by LLSC through the process of engaging with other patients and survivors.
To address the gap identified in the market research (e.g., low usage and low awareness of the program), LLSC provided more resources to the FC Program starting in 2020. Today, the FC program is thriving with more than 400 peer match requests a year, success the LLSC attributes to:
Coast-to-coast advertising for recruitment of volunteers with specific types of blood cancer to broaden the pool of prospective matches with like conditions.
Creation of a process for healthcare professionals’ referrals to the FC program.
Expansion of the FC Program to: a) parents of children with a blood cancer; b) blood cancer survivors; c) caregivers; d) those in palliative care; and e) young adults with a blood cancer.
“The [FC] program helped me hear other survivors’ stories and it also helped me regain the hope and faith that was lost earlier in my treatment.”
Support groups
The LLSC had been offering in-person support groups regionally for people affected by a blood cancer. When COVID happened, the LLSC pivoted to virtual support groups and, in the process, standardized and extended its efforts to serve more people. Today, more than 500 participants a year benefit from free virtual support groups that are conducted in various regions across the country. The groups are offered in English and French, with at least one general blood cancer group and one chronic blood cancer group in each language. An advanced cancer virtual support group has just been launched by LLSC. All the facilitation of the support groups is by allied HCPs such as psychologists and social workers.
Finding: Need for help with practical issues
People with a blood cancer and their caregivers told the market researchers they were looking for practical information on a wide range of issues. These issues included costs of medical travel, dealing with insurance companies, how to plan for short- and long-term disability/taking a leave from work, how to reintegrate back into the workforce after cancer, and how to plan for the future. Other practical topics of interest expressed by individuals affected by a blood cancer included how to manage chronic pain, when is it appropriate to return to exercising, what are the best and most nutritious foods, and how to stimulate appetite when taste buds are impacted by treatment.
Actualization: Practical services expanded
LLSC’s community services leads (bloodcancers.ca/connect-us) include seven trained staff working from coast to coast. These LLSC staff members interact directly with individuals affected by a blood cancer and are uniquely positioned to help answer their practical questions. Being in the same region as their constituents, LLSC staff can access healthcare professionals, allied HCPs, and various service providers in their specific region, and tap into LLSC’s larger national network of contacts.
Example of a fact sheet at bloodcancers.ca
Example of a LLSC podcast episode: Interview with a named blood cancer survivor
One of LLSC’s 50 short, animated videos on topics meaningful to individuals affected by a blood cancer.
In 2020, the LLSC launched its “One Kilometre at a Time” transportation subsidy program for people affected by a blood cancer who face financial constraints. The program is promoted to healthcare professionals to provide referrals for the subsidy. The program provides up to $300 for costs related to traveling for medical appointments and treatment. More than 1,600 individuals have received this financial support for their travel to date; 773 people in the last year alone accessed the program.
Practical information
LLSC meets the need for help with day-to-day practical issues by producing numerous short, easy-to-understand fact sheets and other multimedia resources on topics such as loss of appetite, pain management, self-care and mental health, having an active lifestyle, and dozens of other factsheets, videos and podcast episodes, side effects of treatments, wellness, and more. Our approach is to use images of diverse individuals to broaden the relatability of our material, as well as other visuals and bright colours to make it easier and more enjoyable to read. All LLSC’s information is vetted by healthcare professionals and available on bloodcancers. ca and cancersdusang.ca.
In 2021 and 2023, LLSC hosted four-day virtual conferences entitled, “Living Well with a Blood Cancer”, in English and French. During these conferences, health experts addressed the kinds of practical topics survivors, patients and caregivers wanted advice about, such as nutrition and sleep, sexuality, and managing how you look and feel. More than 2,500 people registered for the 2023 conference, which offered sessions on chronic pain, caregiver burnout, and spirituality among other topics.
Finding: Need for bite-sized, tailored information
The market research showed that people affected by a blood cancer (as well as HCPs) want to see blood cancer information designed to be as flexible as possible. By this, respondents meant smaller, more easily digestible pieces of content; pieces that were quick and easy to read (in plain language, with graphics); and available in multimedia formats. In the design of LLSC resources, factors taken into consideration include differing levels of (language and health) literacy, education, learning styles (i.e., watching, listening, or reading), and cognitive problems (such as brain fog related to chemotherapy).
Respondents said other blood cancer information they came across was generally impersonal, hard to digest, and rarely suitable for the exact spot in which they found themselves during their cancer experience. They often felt ‘overwhelmed’ – a word used throughout the research: information materials that were too long, too complex, too personally unrelatable, with too many steps in the cancer experience covered. People affected by a blood cancer said they preferred reading stories of real people talking about their specific challenges and triumphs in their blood cancer experiences.
To avoid feeling overwhelmed, the individuals said their challenges were best managed one step at a time. Therefore, any information they deemed useful should be designed for and provided at their specific step. In contrast to that approach, in reality, most people affected by a blood cancer said they received information primarily at the time of their diagnosis – an emotionally challenging time to absorb new, often complicated information. Furthermore, the information given to them at diagnosis included details about the later cancer stages, which they were not ready to discover.
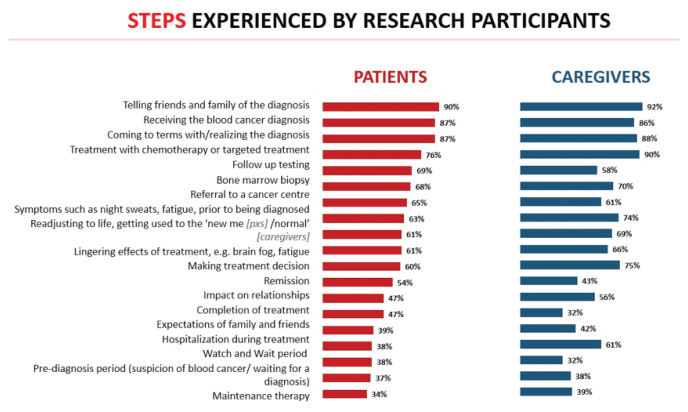
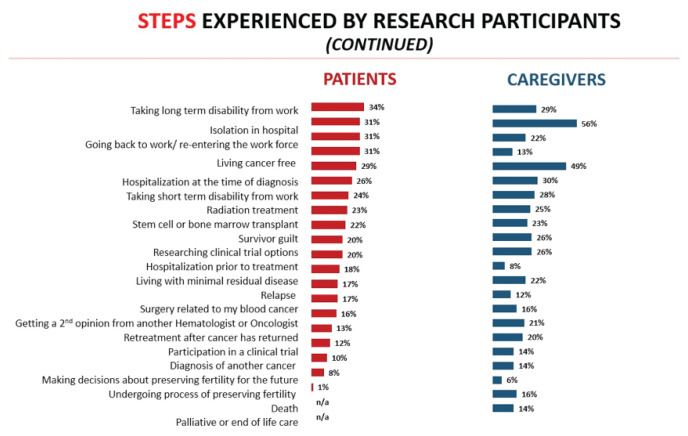
Patients/survivors/caregivers identified 40 steps in their blood cancer experience (Diagrams 1 and 2). In stark contrast, the clinical perspective from HCP participants was four steps: pre-diagnosis; diagnosis; treatment; remission or palliative care.
Diagram 1.
Diagram 2.
Diagram 3.
Actualization: Information designed to be flexible
After learning from the results of the market research, the LLSC engaged in a pervasive overhaul in all aspects of the information provided by the organization. We extended the types of multimedia used, personalizing, shortening, and brightening content with images representing all demographics and ages, trying to tailor the amount and format of information to each unique audience. The LLSC changed some of its wording, and created a lexicon based on feedback from individuals during the research. For example, we replaced the word ‘journey’ with ‘experience,’ and ‘fighting/battling cancer’ with ‘living with.’
Website redesign
Having a personalized approach was intrinsic in the complete redesign and rewrite of bloodcancers.ca and cancersdusang. ca, starting around 2021. The websites were organized around individuals: “I have a blood cancer” (including pediatrics, teens, and young adults)/”I care for someone with a blood cancer”/”I am a blood cancer survivor”/”I am a professional in the blood cancer community”/” I lost someone to a blood cancer.”
“It [bloodcancers.ca] is a very well-organized website; it is very easy to look up issues or download materials; it is very user friendly.”
Multimedia resources
Considering the various challenges facing individuals with a blood cancer, as well as preferred learning styles, the LLSC changed direction from primarily text content, to include:
Videos (webcasts, conference session recordings and more) placed on: LLSC’s YouTube channel; the relevant disease- or user-specific LLSC website pages, as well as within each websites’ Resource Library searchable by topic (disease type; diagnosis and test; treatment and side effects; mental health and wellness; work, school, and finance)
From 2021 to 2023, LLSC created 50 short, animated videos covering cancer survivorship issues such as fear of recurrence, and basic overviews of specific types of blood cancer.
Podcasts: The LLSC launched “The Blood Cancer Experience” podcast, with episodes from conversations with actual (named) blood cancer survivors and caregivers (several of those were hosted by a survivor of childhood blood cancer) as well as interviews with blood cancer experts on their work in discovery of cures and better treatment.
Factsheets: Newly created, short, plain language, colourful and with faces of people from diverse populations.
Real stories: Dozens of real-world patient stories added to websites, often with individuals’ photos, talking about their personal experiences with specific blood cancers.
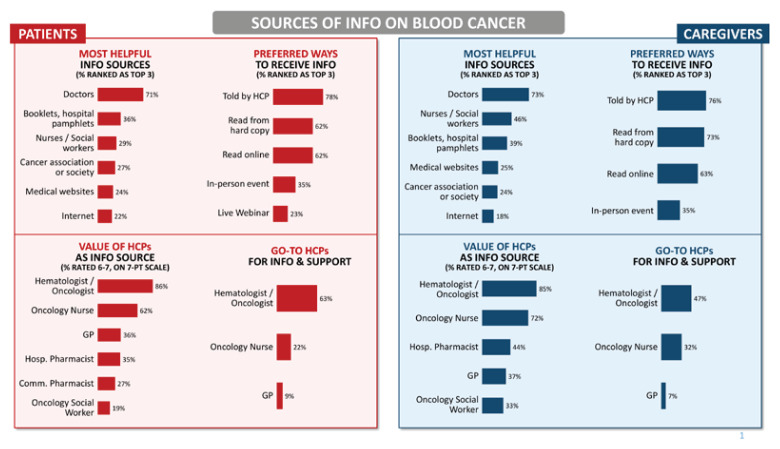
Finding: HCPs are trusted sources of information
All patients/survivors/caregivers said they look to their oncology HCPs as key sources of information. It is worth noting that many patients and caregivers turn to their family physician for support and answers, as well. About half of individuals affected by a blood cancer said that if they were referred to the LLSC by their nurse or physician, they would act.
However, a referral gap was identified. Four of five oncology nurses, and three of five hematologist-oncologists said they recommend LLSC and other cancer associations if asked by patients and caregivers. That type of request to HCPs is unlikely, as individuals affected by blood cancer are often overwhelmed and/or do not know to ask. Therefore, the research implied that to make the most of the high level of trust invested in HCPs by patients/survivors/caregivers, the LLSC would need to boost its profile to HCPs through its member organizations, presentations, and other partnership efforts.
Other sources of information
Family and friends, Google searches, and social media ads placed by LLSC were ranked fairly highly, as “helpful sources of information,” albeit with some real disadvantages. Google-generated blood cancer information was described by some people as not necessarily credible, and even scary. Many individuals mentioned that while they appreciated medical websites, such as the Mayo Clinic, they found such sites overwhelming in the volume, detail, and impersonal nature of the information.
Actualization: Deeper connections and partnerships with HCPs
Given the vital role played by nurses and other HCPs, as trusted sources of information, the LLSC decided to deepen its relationships with relevant HCP organizations. For example, managers and directors of the LLSC have given presentations and had information booths at organizations such as the Canadian Association of Nurses in Oncology (CANO). In 2023, LLSC was honoured to co-host the first ever Pediatric Oncology Day at the annual CANO/ACIO conference.
LLSC’s community service leads give regular presentations at cancer centres across Canada about LLSC support, services, and programs. Every meeting with HCPs counts: Stronger connections with LLSC can translate into more referral to services and support for people affected by a blood cancer. As one nurse participant said:
“LLSC has awesome tools and materials with useful information, and great training for nurses. All of their tools most definitely increased my awareness about the challenges faced by blood cancer patients.”
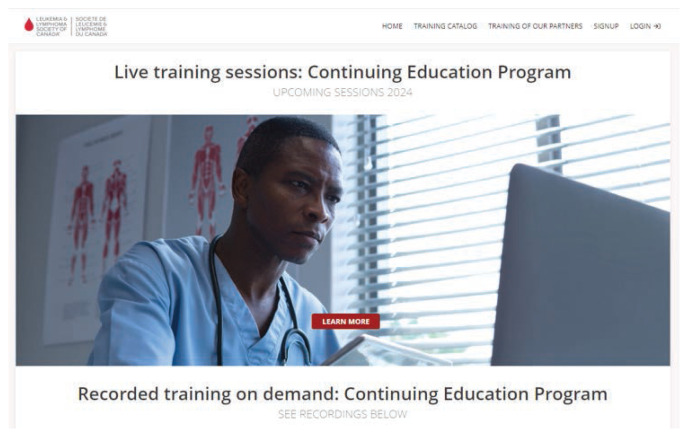
LLSC has built a continuing education platform (hcpen-llscanada.talentlms. com/) with dozens of recorded (on-demand) training, with videos and downloadable materials, as well as live training webcasts on a wide range of subjects from caring for survivors to the latest blood cancer treatments.
Finding: Need for help with healthcare system issues
Another high-level need identified in the market research was help with navigating the healthcare system. People affected by a blood cancer identified they wanted: 1) continuity/coordination of their care between cancer centres/hospitals and various HCPs/specialists, and 2) a way to transition from oncology treatment team more easily after cancer to the ‘new normal’ of life with a chronic blood cancer or in remission. As one patient said:
“You get these letters from the hospital telling you to go to such and such a place for your procedure. Who do you call to find out if there’s going to be some support, to find out why you are having this test?”
Respondents emphasized that they are often trying to coordinate their care while exhausted from treatment and dealing with ‘brain fog’. Some report having to repeat their cancer story repeatedly – an experience they find distressing.
The market research also showed that one of the unmet needs for people touched by a blood cancer was their desire to become an “empowered patient” – feeling they have the right to speak up, ask questions, and take notes – within an environment of medical authority.
The LLSC’s Continuing Education Program platform: hcpen-llscanada.talentlms.com
Actualization: Advocacy and navigational help
Since each LLSC community support employee has a specific geographic catchment area of service in which they work, this allows them to become very familiar with the unique processes and steps involved in cancer care and treatment in their own region. LLSC believes that individuals can and should participate in decisions about their own cancer care. LLSC enables this through their regional employees by:
Educating people about their rights within the healthcare system
Providing educational tools to help them better understand their treatment options
Helping individuals prepare for a medical consult (what questions to ask) and/or explore a clinical trial
Providing personalized support to help empower people to participate in decisions related to their care.
Formally introduced in recent years at LLSC, advocacy work by staff is a burgeoning area. The advocacy team has the mandate to:
Coach individuals affected by a blood cancer on how to self-advocate for their own care or for their loved one.
Reach out, using LLSC’s credibility, on behalf of individuals to help solve their problems.
Work strategically, often with other cancer organizations, to influence decision makers (government, payors) to effect systemic and policy changes in the best interests of all Canadians affected by a blood cancer.
CONCLUSION
This article was written to illustrate how a market research project provides a foundation for understanding the needs and experiences of individuals an organization wishes to serve. The LLSC has been able to design and offer support and services, which they believe align with the perspectives of individuals who are affected by a blood cancer.
The research showed the vital role that nurses and other healthcare professionals play in the lives of individuals touched by a blood cancer. However, there was a low awareness on the part of the HCPs, at the time of the research, about LLSC services and support programs. Encouragingly, most HCPs expressed interest in knowing more about the LLSC.
The LLSC is committed to the model of optimally serving people affected by a blood cancer through partnerships, and to enabling full-circle sharing of information, support, and services across Canada. The best partners for this purpose are nurses, other healthcare professionals, social workers, psychologists and others. These partnerships require seamless coordination centred on:
A proactive approach by HCPs with their patients - as early as possible after diagnosis, and then ongoing throughout the cancer experience – offering LLSC information and service referrals (bloodcancers.ca/partnering-with-us)
A continuous effort by LLSC to raise awareness about its resources and services with HCPs, as well as with individuals affected by a blood cancer.
A communication channel between HCPs and LLSC for identifying needs and gaps and potential solutions.
Together, we are working towards the day every person in Canada affected by a blood cancer learns about and uses the resources and programs of LLSC – and when they do, finds their individual and familial experiences validated and helped.
Footnotes
Editor Note: This manuscript was developed based on a symposium presentation given at the Annual CANO/ACIO Conference held in Niagara Falls in the Fall of 2023.
REFERENCE
- Allicock M, Carr C, Johnson LS, Smith R, Lawrence M, Kaye L, Gellin M, Manning M. Implementing a one-on-one peer support program for cancer survivors using a motivational interviewing approach: Results and lessons learned. Journal of Cancer Education: The Official Journal of the American Association for Cancer Education. 2014;29(1):91–98. doi: 10.1007/s13187-013-0552-3. [DOI] [PMC free article] [PubMed] [Google Scholar]