Abstract
Background
Rotator cuff tendinopathy (RCT) is a widespread musculoskeletal disorder and a primary cause of shoulder pain and limited function. The resulting pain and limited functionality have a detrimental impact on the overall quality of life. The purpose of this study was to perform a systematic review of the effects of extracorporeal shock wave therapy (ESWT) for RCT.
Methods
The literature search was conducted on the following databases from inception to February 20, 2024: PubMed, Web of Science, the Cochrane Library, Scopus, MEDLINE, EMBASE, EBSCO, and China National Knowledge Infrastructure (CNKI) were checked to identify the potential studies exploring the effect of ESWT for the treatment of Rotator cuff tendinopathy (Calcification or non-calcification), control group for sham, other treatments (including placebo), without restriction of date, language. Two researchers independently screened literature, extracted data, evaluated the risk of bias in the included studies, and performed meta-analysis using RevMan 5.3 software.
Results
A total of 16 RCTs with 1093 patients were included. The results showed that compared with the control group, ESWT for pain score Visual Analogue Scale/Score (VAS) (SMD = -1.95, 95% CI -2.47, -1.41, P < 0.00001), function score Constant-Murley score (CMS) (SMD = 1.30, 95% CI 0.67, 1.92, P < 0.00001), University of California Los Angeles score (UCLA) (SMD = 2.69, 95% CI 1.64, 3.74, P < 0.00001), American Shoulder and Elbow Surgeons form (ASES) (SMD = 1.29, 95% CI 0.93, 1.65, P < 0.00001), Range of motion (ROM) External rotation (SMD = 1.00, 95% CI 0.29, 1.72, P = 0.02), Total effective rate (TER) (OR = 3.64, 95% CI 1.85, 7.14, P = 0.0002), the differences in the above results were statistically significant. But ROM-Abduction (SMD = 0.72, 95% CI -0.22, 1.66, P = 0.13), the difference was not statistically significant.
Conclusion
Currently limited evidence suggests that, compared with the control group, ESWT can provide better pain relief, functional recovery, and maintenance of function in patients with RCT.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12891-024-07445-7.
Keywords: Extracorporeal shock wave therapy, Rotator cuff tendinopathy, Shoulder, Rehabilitation, ESWT, Meta-analysis
Introduction
Rotator cuff tendinopathy (RCT) is a common shoulder condition and one of the primary causes of shoulder pain and functional impairment [1]. The incidence of RCT in individuals aged 60 and above is approximately 20% to 50%, manifesting primarily as pain, limitations in daily activities, and reduced shoulder joint function [2, 3]. The etiology of RCT is multifactorial, and its pathogenesis is not fully understood. Common factors such as aging, overuse, mechanical shock, smoking, and family inheritance, and studies of familial susceptibility have shown that genetics also play a role in the pathogenesis of rotator cuff disease [4]. Injury and degeneration are two common mechanisms of RCT. Most chronic shoulder pain is caused by repeated impingement of the rotator cuff at the acromion. The early manifestations are local edema of the rotator cuff Hemorrhage, which then develops into tendinitis with localized fibrosis [5, 6]. If the influencing factors persist for a long time, it will eventually lead to a tear of the rotator cuff [7]. Therefore, effective treatment of RCT is crucial for restoring shoulder function, alleviating pain, and enhancing patient's quality of life. The treatment of RCT is mainly divided into surgical treatment and non-surgical treatment [8]. Available evidence suggests that both physical therapy and surgery can significantly improve patient-reported outcomes in symptomatic patients with small-to-moderate full-thickness RCT [6]. At present, great progress has been made in the non-surgical treatment of RCT. Non-surgical treatment mainly includes (1) physical therapy; (2) subacromial closed injection; (3) non-steroidal anti-inflammatory drugs; and (4) Traditional Chinese medicine preparations and acupuncture [9]. However, none of the treatments is simple, effective and non-invasive.
Extracorporeal shock wave therapy (ESWT) has been widely used as a treatment method for musculoskeletal tendon disorders [10]. Biological effects of ESWT have been reported to include tissue regeneration, wound healing, angiogenesis, bone remodeling, and anti-inflammation [11]. Its mechanism is similar to the cascade process triggered by mechanotransduction: mechanical energy causes changes in the cytoskeleton, causing a response in the nucleus (such as the release of mRNA), thereby affecting various cellular structures such as mitochondria, endoplasmic reticulum, and intracellular vesicles, enzymes Nootropic responses lead to improvements in the healing process [12]. Through ESWT coagulation, the adhesive tissue can be loosened to promote the rapid recovery of skeletal muscle injury and internal inflammation, so the analgesic effect of ESWT is more obvious. In recent years, shock waves have achieved remarkable results in the treatment of RCT, with the characteristics of non-invasiveness and high safety. ESWT is widely used in the field of rehabilitation, especially for improving chronic pain and tendinosis. It has a good therapeutic effect [13]. Indeed, ESWT emerges as a viable option for the treatment of RCT.
At present, the efficacy of ESWT in the treatment of RCT is still controversial. Some studies have indicated that extracorporeal shock waves have a significant effect in reducing pain, improving function and promoting tissue repair in patients with RCT [14, 15], while other studies have reached the opposite conclusion [16, 17]. Danilo et al.'s meta-analysis [18] found that, in short-term follow-up, ESWT showed a slight improvement in shoulder pain compared to sham ESWT. ESWT was not superior to sham ESWT in improving functionality, and it was also not superior to other treatments in improving both shoulder pain and function. There is still controversy regarding the effectiveness of ESWT, as there are few systematic reviews on the impact of extracorporeal shock waves on shoulder pain and function in patients with RCT, and the latest published studies are yet to be included. This study aims to systematically review and meta-analyze the effect of ESWT on shoulder pain and functional recovery in patients with RCT. The effectiveness of clinical efficacy and its scientific basis, hoping to provide a reference for future research in this field based on the research results.
Methods
Study protocol
This systematic review was performed following Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2020 guidelines (PRISMA 2020) [19] (see Supplementary Material 1) and has been registered at PROSPERO (Identification number: CRD42023441407).
Eligibility criteria
The inclusion criteria for this study encompassed all Randomized Controlled Trials (RCTs) that assessed the efficacy of ESWT in the treatment of RCT.
(1) Adult patients (18 years of age and older) with RCT will be included, consistent with clinical or radiographic findings, regardless of race, nationality, or course of disease. (2) RCTs comparing the effect of ESWT and other treatments (including placebo) for RCT. The experimental group was treated with ESWT and the control group was treated with a placebo ESWT or other treatments. (3) Outcome indicator: The main outcome indicator is the Visual Analogue Scale/Score (VAS), Secondary outcome indicators are the Constant-Murley score (CMS), University of California Los Angeles score (UCLA), Range of motion (ROM), American Shoulder and Elbow Surgeons form (ASES) and Total effective rate (TER). (4) Without restriction of date and language.
Exclusion criteria
(1) Non-randomized control trials; (2) Animal experiments; (3) Incomparability between the intervention and control groups; (4) Letters, reviews, case reports, conference abstracts and comments. (5) if individuals who had a history of trauma or other conditions (partial or full rotator cuff tears, osteoarthritis, and adhesive capsulitis), systemic inflammation, or associated neurological diseases.
Search strategy
The literature search was conducted on the following databases from inception to February 20, 2024: PubMed, Web of Science, the Cochrane Library, Scopus, MEDLINE, EMBASE, EBSCO, and China National Knowledge Infrastructure (CNKI) were checked to identify the potential studies exploring the effect of ESWT for the treatment of RCT. The search strategy uses the combination of subject words and free words, Boolean operators (AND or OR), and the search strategies of different databases are slightly different. Search terms included “Rotator cuff tendinopathy”, “Cuff Tendinopathy, Rotator”, “Rotator Cuff Tendinitis”, “Extracorporeal shock wave therapy”, “ESWT”, “Physical therapy modalities”, “Physical therapy”, “Randomized controlled trial,” “Controlled clinical trial,” “Randomized,” and “Trial.” Take Pubmed as an example, the specific retrieval strategy is displayed in Supplementary Material 2. Besides, the reference lists of eligible studies and relevant reviews were searched in case of possible missing articles.
Selection process
Two experienced researchers (XLX and QFS) independently screened and evaluated the title and abstract of each study according to the established criteria, excluded unqualified literature, and then read the remaining full text and screened based on the previous content. Full text, determining criteria for eligible research. In case of disagreement, decisions were made by discussion with the corresponding author (GQC).
Data collection process
Two researchers (XWY and FH) independently conducted data extraction. They used a pre-designed data collection form to record information including first author details, publication date, publication year, country of origin, study design, sample size, basic patient characteristics, intervention details for treatment and control groups, and primary and secondary outcomes. In cases where the above-mentioned data were incomplete, attempts were made to contact the article authors for additional information. When data were not reported, authors were emailed three times with one week in between attempts to clarify the information. In trials in which SD was not reported, the study will be excluded directly. Any disagreements during data extraction were resolved through discussions with a third researcher (GQC).
Study risk of bias assessment
Two researchers (XLX and QFS), independently evaluated the methodological quality of each reviewed study using the Cochrane Risk of Bias tools 2.0 (ROB 2.0) to assess the risk of bias in randomized trials. Any discrepancies between their assessments were resolved through discussion, or consultation with a third researcher (GQC) was sought if a consensus could not be reached. The methodological quality of the studies was assessed across several domains, including the randomization process, adherence to intended interventions, handling of missing outcome data, measurement of outcomes, and selection of reported results. Each of these domains was categorized as Low risk, High risk, or Some concerns according to the ROB 2.0 criteria.
Statistical analysis
Review Manager software (RevMan 5.3) was used for data analysis. Continuous variables were diagnosed with the Standardized mean difference (SMD) and 95% Confidence interval (CI), and the Odds Ratio (OR) was used for pooled analysis of dichotomous variables. SMD were classified as small (< 0.40), medium (between 0.41 and 0.70), and large (> 0.70). Statistical heterogeneity between studies will be assessed using P and I2 values, with P < 0.1 and I2 > 50% showing high heterogeneity, using a random effects model. When heterogeneity is not significant, a fixed effects model was used. If heterogeneity is high, subgroup analysis or meta-regression was performed to explore sources of heterogeneity. Funnel plots were applied for the assessment of publication bias. The extracted data was input into the computer, reviewed, and independently analyzed by two researchers. The meta-analysis is set at P < 0.05 for the significance level.
Results
Study selection
A total of 927 studies were retrieved by retrieving each data, 638 of which were excluded according to the title and abstract. After removing duplicate results, the full text of 30 articles was checked. Following this, 13 articles were excluded for not meeting our inclusion criteria and 17 articles were eligible for inclusion in the meta-analysis. The publication years of the included studies were from 2006 to 2023, the sample size is between 20—160. The screening process and results of the literature are shown in Fig. 1.
Fig. 1.
Flow diagram of the study selection process
Study characteristics
A total of 1131 patients with RCT were included in the 17 included studies [20–36]. The research characteristics of each included study, encompassing the sample size in both the experimental and control groups, participant age, disease duration, type and dosage of extracorporeal shock wave therapy, intervention duration, as well as outcome evaluation indicators are presented in Table 1.
Table 1.
Characters of included studies in the meta-analysis
| Author Year (Ref.) | Sample size (T/C) |
Age, years (T/C) |
Duration of symptoms (T/C) |
Type of intervention (T/C) |
Types and Brands of ESWT | Dose of EWST | Duration of intervention | Main Outcomes | |
|---|---|---|---|---|---|---|---|---|---|
| Shao 2023 | 19/19 | 51.4 ± 8.2/55.7 ± 9.2 | 6.4 ± 3.5/5.2 ± 4.2m | ESWT + Routine rehabilitation training | Routine rehabilitation training | Radial shock wave, Swiss Dolor-Clast, EMS | Each point received 1000 impulses, and a total of 2000 impulses were applied. A total of 0.08mJ/mm2 energy flux density was applied, with a pressure of 2.5 bars and a frequency of 6 Hz |
5 w Shock wave therapy was administered once a week for a total of 5 sessions |
VAS, ROM, UCLA, ASES, SNQ |
| Xi 2022 | 31/31 | 69.21 ± 4.83/69.21 ± 4.83 | 18. 02 ± 8. 64/18. 64 ± 9. 11m | ESWT + Routine rehabilitation training | Routine rehabilitation training | Focused shock wave, Zimmer Company, enPuls Version 2.0, Germany | The probe is 15 mm straight, the frequency was 10 Hz, the energy flow density was 0.08 mJ/mm2, and the total number of shocks was 2000 times |
4 w Shock wave therapy was administered once a week, for a total of 4 weeks |
VAS, TER, ROM, UCLA |
| Fatima 2022 [24] | 20/20 | 48.7 ± 6.74/49.8 ± 7.54 | - | ESWT + Routine rehabilitation training | Routine rehabilitation training | Radial SWT BLT-6000 device (UK) | Each ESWT session was given for 15–20 min in which patients have been treated by 2000 shocks with 120 Hz. The procedure could be slightly painful in the first session, so a low-energy density of 0.03mJ/mm2 was given for the first five minutes and then progressively increasing to 0.32mJ/mm2 |
6 w Shock wave therapy was administered twice a week for six weeks |
CMS, VAS, WORC |
| Xu 2022 | 34/40 | 52.69 ± 6.10/53.04 ± 6.33 | 10.49 ± 2.77/10.26 ± 2.70d | ESWT + Routine rehabilitation training | Routine rehabilitation training | Radial shock wave, Swiss Dolor-Clast, EMS | The probe is 15 mm straight, the frequency is 5 Hz, the impact times of each pain point is 2500 times |
3 w Shock wave therapy was administered once every 2 days, a total of 10 times |
CMS, UCLA, ASES |
| Zhang 2021 | 60/60 | 61.02 ± 1.07/60.53 ± 1.49 | - | ESWT + Routine rehabilitation training | Routine rehabilitation training | Focused shock wave | Low energy shock wave, energy range: 0.08–0.28mJ/mm2, 1200–1500 times |
4 w Shock wave therapy was administered once a week, for a total of 4 weeks |
VAS, CMS, TER |
| Luo 2021 | 80/80 | 57.1 ± 6.9/56.5 ± 6.4 | - | ESWT + Routine rehabilitation training | Routine rehabilitation training | CJB divergent extracorporeal shock wave | The treatment pressure was 3.5 ~ 5.0 Bar, the number of shocks was 2000 ~ 3500, and the frequency was 12 ~ 15 Hz |
5 w Shock wave therapy was administered once a week, for a total of 5 weeks |
VAS, CMS, UCLA |
| Zhu 2021 | 20/20 | 57.60 ± 7.21/57.55 ± 6.48 | 48.05 ± 4.66/48.3 ± 3.76d | ESWT + Routine rehabilitation training | Routine rehabilitation training | Electromagnetic extracorporeal shock wave (Israeli Medispec series Radialspec model) | Select a 15 mm electrode head, use a low frequency of 5 Hz, energy level 1 (60 mJ), impact 2000 times, 500 times per point, and the rest of the uniform impact |
6 w Shock wave therapy was administered once a week, for a total of 6 weeks |
VAS |
| Zheng 2020 | 29/28 | 36.3 ± 5.6/38.5 ± 5.4 | 3 weeks to 3 months | ESWT + Routine rehabilitation training | Routine rehabilitation training | Radial shock wave, STORZ of Switzerland | The treatment probe with a diameter of 15 mm was fixed at 8 Hz and the intensity was controlled at 2.0 ~ 3.2 bar. Each treatment had a therapeutic impact of 4000r |
4 w Twice a week for 4 weeks, a total of 8 times a course of treatment |
UCLA, VAS, ROM |
| Zhao 2020 | 27/27 | 43.65 ± 3.27/42.34 ± 3.45 | 8.5 ± 1.02/8.86 ± 0.93m | ESWT + Floating needle therapy | Floating needle therapy | Focused shock wave | Set the pulse to 2000, set the energy to 0.25 mJ/mm2, and set the frequency to 3.0 Hz |
4 w Twice a week for 4 weeks, a total of 8 times a course of treatment |
VAS, ROM, SF-36, TER |
| Tian 2020 | 28/28 | 52.21 ± 6.47/55.07 ± 6.47 | 30.43 ± 17.91/32.60 ± 16.14d | ESWT + Routine rehabilitation training | Routine rehabilitation training | Radial shock wave, Swiss Dolor-Clast, EMS | The treatment probe with a diameter of 15 mm was fixed at 10 Hz and the intensity was controlled at 1.8 ~ 3.5 bar the energy flow density (0.12 ~ 0.25mJ/mm2), and the impact of each treatment is 2000 times |
8 w Each treatment interval was 1 week, and each patient in the observation group received 4 treatments |
VAS, UCLA, TER |
| Duymaz 2019 [22] | 40/40 | 54.33 ± 9.88/51.31 ± 8.86 | > 12m | ESWT + Routine rehabilitation training | Routine rehabilitation training | Radial shock wave, Shock Master 500 device, (GymnaUniphy NV, Bilzen, Belgium) | 1500 shocks with a frequency of 150 shocks per minute. Since pain could occur mostly during the first treatment, all patients were treated with a low energy density of 0.03 mJ/mm2 for the first five minutes, which was then progressively increased to 0.28 mJ/mm2 |
4 w Once a week for four weeks in total |
VAS, ROM |
| Chen 2018 | 22/16 | 19.14 ± 3.04/19.63 ± 3.05 | 2.16 ± 1.55/2.16 ± 1.09y | ESWT + Routine rehabilitation training | Routine rehabilitation training | Radial shock wave, Switzerland STORZ, DUOLITH® SD1 ultra | Pulse 2000, energy 0.25mJ/mm2, frequency 3.0Hz |
4 w Shock wave therapy was administered twice a week, for a total of 4 weeks |
VAS, ASES, TER |
| Su 2018 | 32/30 | 56.88 ± 10.45/57.87 ± 12.43 | > 3m | ESWT + Routine rehabilitation training | Routine rehabilitation training | Focused shock wave | The parameter is 0.08 mJ/mm2, 2000 times, and the frequency is 8 Hz |
4 w Shock wave therapy was administered once a week, for a total of 4 weeks |
VAS, CMS |
| Xie 2017 | 30/30 | 68.7 ± 6.9/67.5 ± 9.3 | 111.8 ± 69.8/104.6 ± 53.4m | ESWT + Routine rehabilitation training | Routine rehabilitation training | Radial shock wave, Switzerland, STORZ | The treatment frequency was 14 Hz, the pressure was 1.0 ~ 2.5 bar, the energy flux density (EFD) was 0.38 mJ/mm2, the treatment probe was 15 mm, and each shock was 2,000 times |
8 w Shock wave therapy was administered once a week, for a total of 8 weeks |
VAS, CMS, TER |
| Wang 2013 | 40/40 | 49.2 ± 10.6/47.6 ± 9.8 | 12.8 ± 4.2/12.3 ± 3.8w | ESWT + Routine rehabilitation training | Routine rehabilitation training | Radial shock wave, MASTERPULS MP-100 is produced by STORZ, Switzerland | Voltage 15 ~ 25 kV, 2000 shocks per time, power energy density 0.16 mJ/mm2 |
4 w Shock wave therapy was administered once a week, for a total of 4 weeks |
CMS, VAS, ROM |
| Galasso 2012 [25] | 11/9 | 50.7 ± 8.44/51.11 ± 13.26 | 45.36 ± 34.33/61.22 ± 24.04m | ESWT + Routine rehabilitation training | Routine rehabilitation training | ModulithW SLK system (Storz Medical AG, Tagerwilen, Switzerland) | The treatment regimen required administration of two treatment sessions, each consisting of 3000 shockwaves at an energy flux density of 0.068 mJ/mm2 |
6 w Shock wave therapy was administered once a week, for a total of 6 weeks |
CMS |
| Cacchio 2006 [20] | 45/45 | 56.12 ± 1.98/56.42 ± 2.09 | 14 ± 4.95/13 ± 5.03m | ESWT + Routine rehabilitation training | Routine rehabilitation training | Radial shock wave | 2500 impulses per session (500 impulses with a pressure of 1.5 bar and a frequency of 4.5 Hz and 2000 impulses with a pressure of 2.5 bar and a frequency of 10 Hz), an EFD of 0.10 mJ/mm2, and a fixed impulse time of 2 ms |
4 w Each subject in the treatment group received 4 sessions at 1-week intervals |
UCLA, VAS, SPADI |
T Trial group; C Control group; ESWT Extracorporeal shock wave therapy; VAS Visual Analogue Scale/Score; CMS Constant-Murley score; UCLA University of California Los Angeles score; ROM Range of motion; TER Total effective rate; ASES American Shoulder and Elbow Surgeons form; SPADI Shoulder Pain & Disability Index; EFD Energy flux density; WORC Western Ontario Rotator Cuff; SF-36 36-item Short-Form; SNQ Signal/Noise Quotient
Risk of bias in studies
All studies were assessed using the ROB 2.0. It was found that five studies were of low-risk bias [20, 22, 23, 25, 29], and twelve studies were conducted as controlled clinical trials, raising concerns about potential bias in several criteria [21, 24, 26–28, 30–36]. The risk of bias assessed by the study are shown in Table 2.
Table 2.
The risk of bias of RCTs included and evaluated through Rob 2.0
| Author, year | Randomization process | Deviation from intended interventions | Missing Outcome data | Measurement of the outcome | Selection of the reported result | Overall |
|---|---|---|---|---|---|---|
| Shao 2023 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Xi 2022 | Some concerns | Low risk | Low risk | Low risk | Low risk | Some concerns |
| Fatima 2022 [24] | Low risk | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Xu 2022 | Some concerns | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Zhang 2021 | Some concerns | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Luo 2021 | Some concerns | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Zhu 2021 | Low risk | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Zheng 2020 | Low risk | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Zhao 2020 | Some concerns | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Tian 2020 | Some concerns | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Duymaz 2019 [22] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Chen 2018 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Su 2018 | Low risk | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Xie 2017 | Some concerns | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Wang 2013 | Low risk | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Galasso 2012 [25] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Cacchio 2006 [20] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
Results of syntheses
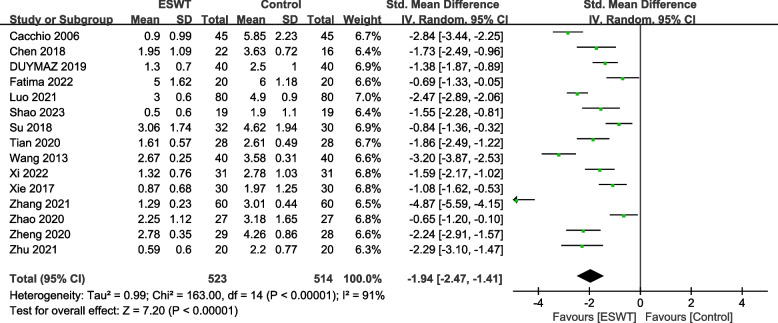
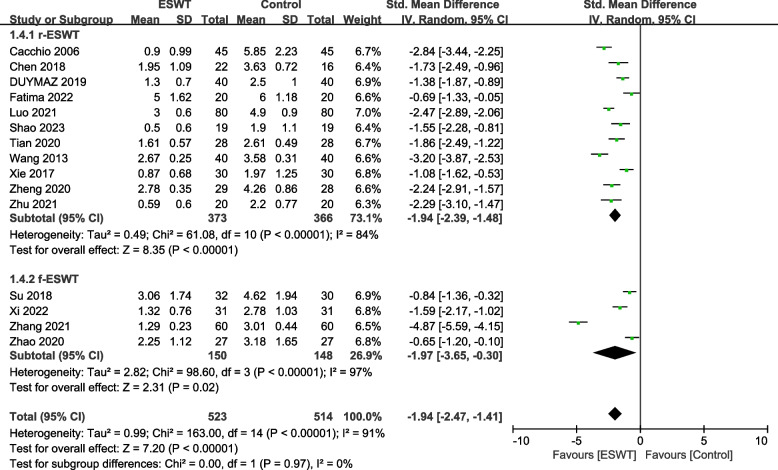
VAS
Fifteen studies [20–24, 26–29, 31–36] involving 1037 patients used the VAS to assess the pain relief effect. The heterogeneity results showed that there was heterogeneity among the studies (P < 0.00001, I2 = 91%), and the random effects model was used for meta-analysis. The results showed that there was a significant difference in pain reduction between the ESWT group and the control group (SMD = -1.94, 95% CI -2.47, -1.41, P < 0.00001) (Fig. 2).
Fig. 2.
Forest plot of VAS on shoulder pain
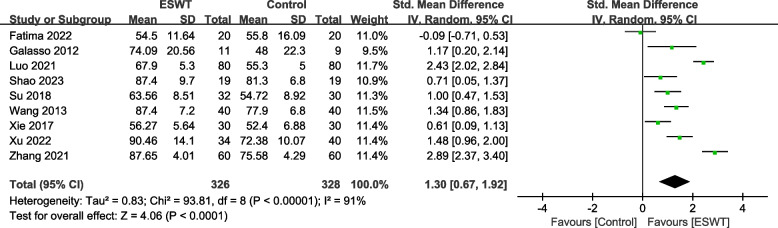
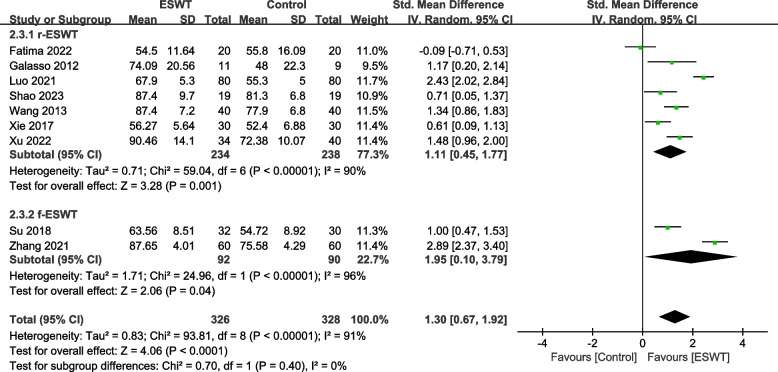
CMS
Nine studies [21, 24–26, 28–30, 32, 35] involving 654 patients used the CMS to assess the effect of shoulder function. The heterogeneity results showed that there was heterogeneity among the studies (P < 0.00001, I2 = 91%), and the random effects model was used for meta-analysis. The results showed that there was a significant difference in the improvement of shoulder function between the ESWT group and the control group (SMD = 1.30, 95% CI 0.67, 1.92, P <0.0001) (Fig. 3).
Fig. 3.
Forest plot of CMS on shoulder function
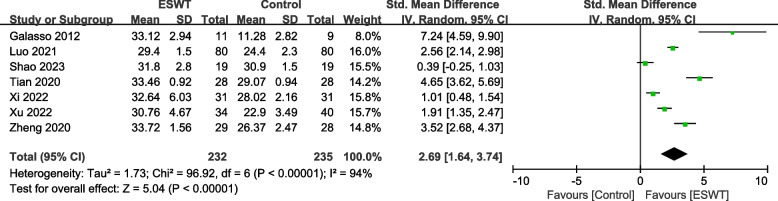
UCLA
Seven studies [25, 27, 29, 30, 33–35] involving 467 patients used the UCLA to assess the effect of shoulder function. The heterogeneity results showed that there was heterogeneity among the studies (P < 0.00001, I2 = 94%), and the random effects model was used for meta-analysis. The results showed that there was a significant difference in the improvement of shoulder function between the ESWT group and the control group (SMD = 2.69, 95% CI 1.64, 3.74, P < 0.00001) (Fig. 4).
Fig. 4.
Forest plot of UCLA on shoulder function
ROM
Four studies [27, 29, 33, 36] involving 211 patients used the ROM-Abduction to assess the Angle of motion of the shoulder joint. The heterogeneity results showed that there was heterogeneity among the studies (P < 0.00001, I2 = 90%), and the random effects model was used for meta-analysis. The results showed that there was no significant difference in the improvement of shoulder abduction angle between the ESWT group and the control group (SMD = 0.72, 95% CI -0.22, 1.66, P = 0.13) (Fig. 5).
Fig. 5.
Forest plot of ROM on shoulder function
Three studies [27, 29, 33] involving 157 patients used the ROM-External rotation to assess the Angle of motion of the shoulder joint. The heterogeneity results showed that there was heterogeneity among the studies (P < 0.00001, I2 = 90%), and the random effects model was used for meta-analysis. The results showed that there was a significant difference in the improvement of shoulder external rotation angle between the ESWT group and the control group (SMD = 1.00, 95% CI 0.29, 1.72, P = 0.02) (Fig. 5).
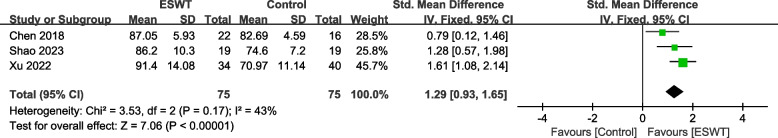
ASES
Three studies [23, 29, 30] involving 150 patients used the ASES to assess the effect of shoulder function. The heterogeneity results showed that there was low heterogeneity among the studies (P = 0.17, I2 = 43%), and the fixed effects model was used for meta-analysis. The results showed that there was a significant difference in the improvement of shoulder function between the ESWT group and the control group (SMD = 1.29, 95% CI 0.93, 1.65, P < 0.00001) (Fig. 6).
Fig. 6.
Forest plot of ASES on shoulder function
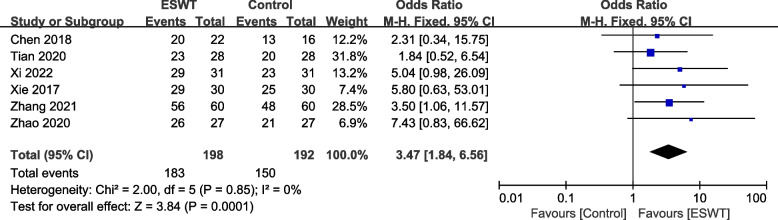
TER
Six studies [23, 28, 32–34, 36] involving 390 subjects reported the TER of RCT recovery. Meta-analysis showed that there was no heterogeneity among the studies (P = 0.85, I2 = 0%), and there was a significant difference in the effective rate of RCT treatment between the ESWT group and the control group (OR = 3.47, 95% CI: 1.84, 6.56, P = 0.0001), indicating that the ESWT group intervention is more effective than the control group (Fig. 7).
Fig. 7.
Forest plot of TER on shoulder function
Subgroup analysis
Subgroup analysis was carried out according to the intensity of the shock wave in each study, and those with a shock wave intensity less than or equal to 0.1mj/mm2 were divided into one group, and those with an intensity greater than 0.1mj/mm2 were divided into a group. Subgroup analysis of VAS and CMS indicators was performed.
VAS by intensity
Among the VAS indicators, 4 studies [20, 21, 29, 33] involved 252 patients with shock wave intensity less than or equal to 0.1mj/mm2, and 4 studies [23, 26, 28, 36] involved 232 patients with shock wave intensity greater than 0.1mj/mm2. There was a statistically significant difference between the experimental group and the control group using a shock wave intensity of 0.1mj/mm2 or less (SMD = -1.70, 95% CI -2.57, -0.84, P = 0.0001, I2 = 88%). The difference between the experimental group and the control group using shock wave intensity greater than 0.1mj/mm2 was statistically significant (SMD = -1.65, 95% CI -2.73, -0.57, P = 0.003, I2 = 92%) (Fig. 8).
Fig. 8.
Subgroup by strength–Forest plot of VAS on shoulder pain
CMS by intensity
Among the CMS indicators, 3 studies [21, 25, 29] involved 120 patients with shock wave intensity less than or equal to 0.1mj/mm2, and 2 studies [26, 28] involved 140 patients with shock wave intensity greater than 0.1mj/mm2. There was a statistically significant difference between the experimental group and the control group using a shock wave intensity of 0.1mj/mm2 or less (SMD = 0.93, 95% CI 0.55, 1.31, P < 0.00001, I2 = 0%). The difference between the experimental group and the control group using shock wave intensity greater than 0.1mj/mm2 was statistically significant (SMD = 0.98, 95% CI 0.26, 1.70, P = 0.008, I2 = 76%) (Fig. 9).
Fig. 9.
Subgroup by strength–Forest plot of CMS on shoulder function
According to each type of shock wave, which can be divided into radial-ESWT (r-ESWT) and focused-ESWT (f-ESWT). Subgroup analysis of VAS and CMS indicatiors was performed.
VAS by type
Among the VAS indicators, 11 studies [20, 22–24, 26–29, 31, 34, 35] involved 739 patients with r-ESWT, and 4 studies [21, 32, 33, 36] involved 298 patients with f-ESWT. There was a statistically significant difference between the experimental group and the control group using r-ESWT (SMD = -1.94, 95% CI -2.39, -1.48, P < 0.00001, I2 = 84%). The difference between the experimental group and the control group using f-EAWT was statistically significant (SMD = -1.97, 95% CI -3.65, -0.30, P = 0.02, I2 = 97%) (Fig. 10).
Fig. 10.
Subgroup by type–Forest plot of VAS on shoulder pain
CMS by type
Among the CMS indicators, 7 studies [24–26, 28–30, 35] involved 472 patients with r-ESWT, and 2 studies [21, 32] involved 182 patients with f-ESWT. There was a statistically significant difference between the experimental group and the control group using r-ESWT (SMD = 1.11, 95% CI 0.45, 1.77, P = 0.001, I2 = 90%). The difference between the experimental group and the control group using f-ESWT was statistically significant (SMD = 1.95, 95% CI 0.10, 3.79, P = 0.04, I2 = 96%) (Fig. 11).
Fig. 11.
Subgroup by type–Forest plot of CMS on shoulder function
Reporting biases
Funnel plot was drawn for the studies on VAS with more outcome indicators in the included studies. Most of the VAS studies were distributed within the 95% CI range of the inverted funnel plot. The results show that the distribution is vertically symmetrical, indicating that the publication bias is small (Fig. 12).
Fig. 12.

Funnel plot for comparison of VAS between the two groups
Discussion
RCT is one of the most common musculoskeletal degenerative diseases of aging. The etiology is complex and diverse, with varying clinical treatment approaches. The best treatment method is still uncertain. Surgical treatment has the possibility of secondary infection, and conservative drug treatment is also prone to various adverse reactions, especially for the elderly, who have a higher risk of drug use [37]. Therefore, it is particularly important to choose a safer and more effective treatment method for elderly patients with RCT. Extracorporeal shock waves transmit sound waves to the affected area through the skin. As a non-invasive treatment, it has been gradually used in the treatment of RCT in recent years. The main mechanism of action includes: extracorporeal shock wave can directly use the mechanical effect generated between the local mechanical vibration effect and cavitation to cause changes in human tissues and cells, stimulate blood vessel expansion, and promote regeneration of tendon and soft tissue [38]. inhibit the high-frequency pulse emitted by pain receptors and the transmission of pain signals, improve the water and electrolyte circulation and the metabolism of the treatment area, evacuate local inflammation, and then reduce the load and relieve pain, improve the function of the shoulder joint and increase the ROM of the shoulder joint [39].
To the best of our knowledge, this study represents the first meta-analysis focusing on the impact of ESWT on pain and function among patients with RCT. Our findings indicate that the noninvasive nature of ESWT renders it an efficacious treatment modality for alleviating pain and enhancing function following RCT. These results offer the most robust current evidence regarding the utilization of ESWT in RCT, drawing from available randomized controlled trials. Specifically, our analysis reveals that ESWT significantly reduces shoulder pain and enhances function post-RCT. However, the improvement in shoulder abduction ROM does not exhibit statistically significant differences compared to the control group. Subgroup analyses further demonstrate that ESWT remains effective in mitigating shoulder pain and enhancing shoulder function, irrespective of the administered energy dose.
The goals of RCT treatment are pain control and maintenance of function. Once pain is under control, the function can be maintained with exercises to increase ROM and strengthen the rotator cuff. This meta-analysis demonstrated the superiority of ESWT in terms of clinical pain relief and recovery of shoulder function. Results regarding ESWT on RCT were similar to a previous study by Fatima et al., in which pain was reduced and the effect was maintained for 12 weeks. Although the mechanism by which ESWT improves pain effects is unclear, it has been suggested that ESWT produces oscillations in tissues that improve microcirculation and metabolic activity [40]. The immediate pain reduction after ESWT can be explained by the results of overstimulation analgesia [41]. Furthermore, gender may also influence the effectiveness of ESWT in pain relief. In a retrospective study examining the subjects influenced by RCT, it was observed that among individuals undergoing ESWT alone, males reported higher benefits in pain relief compared to females [42].
Various etiologies of RCT including rotator cuff tendonitis, partial rotator cuff tears, adhesive capsulitis, subscapular bursitis, and complex regional pain syndrome are thought to lead to antifibrotic, anti-inflammatory, and pain-modulating effects [43]. Since RCT includes an inflammatory response, ESWT can eliminate inflammatory factors in the patient's body, relieve pain, promote the early recovery of shoulder joint function, and improve the curative effect. Ko et al. employed a single session of high-energy extracorporeal shockwave therapy (ESWT) with long-term follow-up and demonstrated its efficacy in improving the functional outcome of rotator cuff lesions accompanied by shoulder stiffness. These findings suggest that ESWT represents a simple, effective, and non-invasive treatment option for such a condition [44]. Similar results were also observed in other studies, with significant improvement in pain reduction and shoulder function in the ESWT group compared with the sham group [45, 46]. In addition, the adverse effects of ESWT were dose-dependent and usually limited to temporary increases in pain and local reactions, such as swelling, erythema, petechiae, or small hematomas, and no serious adverse events were reported [47].
Extracorporeal shock waves can also effectively loosen adhesion tissue and relieve soft tissue spasms, thereby increasing the ROM of the shoulder joint. The results of the Meta-analysis showed that the ROM of external rotation of the two groups was significantly improved compared with that before treatment, and the experimental group was significantly better than that of the control group, but the difference in the ROM of abduction was not statistically significant. Firstly, consider that this may be related to the fact that extracorporeal shock waves can effectively improve pain, thereby improving the patient’s exercise time and effect. Secondly, it may also be because extracorporeal shock waves can damage local tissues, promote the production and accumulation of repair factors, and accelerate the vascularization of rotator cuff ischemia. regeneration, thereby speeding up the repair process and improving the stability of the shoulder joint [48, 49]. In short, extracorporeal shock waves can not only effectively improve the pain of RCT, but also improve the ROM of joints more effectively. Admittedly, the improvement in some symptoms in the control group may have been the expected result of the natural healing process.
In a meta-analysis by Steuri et al., ESWT was found to be more effective than sham ESWT in improving function, pain, and active ROM. Studies have shown that ESWT at doses equal to or greater than 0.28 mJ/mm2 is more effective in improving shoulder function and reducing pain [50]. In another related study, the experimental group received ESWT in addition to conventional PT intervention, while the control group only underwent conventional PT intervention. Patients receiving ESWT treatment demonstrated a significant improvement in shoulder function compared to the control group [22]. A study comparing ESWT with a placebo treatment also showed a statistically significant improvement in outcomes for the ESWT group [51]. In this study, the control group also showed pain improvement after the intervention, but the pain improvement was negligible compared with the ESWT group, where the difference was statistically significant.
However, in a study comparing placebo ESWT with ESWT in patients with subacromial pain syndrome with supervised exercise, there were no significant differences in primary or secondary outcomes (VAS, CMS) between the two treatment groups. These results suggest that ESWT has no additional effect on supervised exercise in this patient group in the short, medium, or long term. Analyzing causes with negative outcome expectations, frequent use of pain medication, not working from baseline, marital status (single), low self-reported general health, and participation in infrequent supervised exercise classes all predicted poor SPADI results after one year [52]. In a study comparing placebo ESWT and ESWT to RCT, Kolk et al. found that VAS, CMS, and SST scores improved significantly in both groups at 3 and 6 months after treatment, compared with placebo at low doses ESWT does not appear to be effective in reducing symptoms in patients with chronic rotator cuff tendinitis. Therefore, a beneficial effect of ESWT in patients with shoulder tendonitis could not be demonstrated [53]. These results support a previous study by Schmitt et al. ESWT did not improve CMS, SPADI, or pain in patients with noncalcified cuff tendonitis [54].
There may be several explanations for these inconsistent results, such as the high number of variables in the ESWT application (frequency, pressure, treatment interval, etc.), the large heterogeneity of the reported treatment regimens, and the large variation in shock wave intensity. The reliability of blinding in each study is questionable, and although ESWT has been extensively studied, the exact mechanism by which ESWT reduces tendon-related pain is unknown. Theoretical benefits are promoting tissue healing and breaking down calcifications. The intensity of ESWT is measured by energy flux density (EFD), which is generally divided into low-energy, intermediate-energy, and high-energy shockwave therapy, and may also affect the outcome of the treatment. Currently, there is no consensus on the exact dividing point between low-energy and high-energy shockwaves. In general, an EFD of less than 0.08 mJ/mm2 corresponds to low energy, while an EFD of a high-energy extracorporeal shock wave is greater than 0.28 mJ/mm2. Although the dose–response relationship between low-energy and high-energy ESWT has not been established, studies have shown that high-energy ESWT (> 0.28 mJ/mm2) is more likely than low-energy ESWT (< 0.08 mJ/mm2) to improve shoulder joints in patients with chronic calcific tendinopathy function and pain relief [55]. The advantage of high-energy ESWT is that it is widely applicable in out-of-hospital settings and is relatively inexpensive. The clinical effect is good, and the treatment has no serious side effects and long-term complications. Generally, however, patients require multiple ESWT treatments to achieve these results. Therefore, further research is needed to better understand the relative efficacy of these treatments.
Previous research findings indicate that both f-ESWT and r-ESWT are superior to placebo in alleviating pain and improving knee joint function [56]. In this study, we conducted a subgroup analysis based on the type of shock wave, revealing that both rESWT and fESWT groups exhibited superior improvements in VAS and CMS compared to the control group. However, Raffaello et al. found, in their investigation of the safety and efficacy of fESWT and rESWT in Lateral elbow tendinopathy (LET) symptoms and wrist extensor strength, that both fESWT and rESWT could potentially improve LET symptoms. ESWT appears to be an effective alternative to conventional therapeutic modalities for treating pain, disability, and muscle injuries associated with LET. Nonetheless, rESWT seems to be less effective and requires more time for pain relief and functional recovery [42, 57]. Therefore, further research is needed to compare the effects of rESWT and fESWT specifically in the context of RCT.
Prospects
Since extracorporeal shock wave is still a relatively new treatment method, many aspects of ESWT for RCT still need further clinical research and improvement, including the determination of the dose of shock therapy and the formulation of a unified treatment prescription. Therefore, further research and clinical trials may be required to elucidate the ideal parameters conducive to ESWT. The efficacy and safety of ESWT for RCT still need further research and clinical trials to confirm. Accumulating more scientific evidence will help clarify its strengths and limitations in specific cases. The treatment of RCT is an individualized process, and treatment plans need to be formulated according to the specific conditions of patients. Future research will pay more attention to individualized treatment methods. Doctors should consider the patient's condition, symptom severity, physical condition and other factors, and choose the most appropriate treatment based on the latest clinical guidelines and research results. Additionally, ESWT may be combined with other treatments, such as physical therapy, medication, or surgery, for better results. In addition to treatment, future research may pay more attention to the prevention and rehabilitation of RCT. It is possible to reduce the incidence of RCT through preventive measures such as strengthening exercise, improving posture, and avoiding overuse. At the same time, the rehabilitation program for RCT will also be further optimized to improve the effect of rehabilitation and prevent recurrence.
Limitations
There are certain limitations in this study: (1) There are differences in the brand, and intensity (For example, the energy of rESWT is relatively weaker, with a broader range of wave propagation. The energy of fESWT is stronger but concentrated within a smaller area, enabling deeper penetration into tissues) and the dose of extracorporeal shock waves used in each study, may affect the accuracy of the results. (2) Some studies did not use correct random allocation and concealment methods, which may cause selection bias. (3) Due to language limitations, we only included Chinese and English literature. Therefore, to obtain conclusive evidence, we need to expand the sample and include studies in more languages.
Conclusions
In summary, the current evidence supports the effectiveness of ESWT for the clinical efficacy of shoulder pain and functional recovery in patients with RCT. ESWT provided better pain relief, functional recovery, and maintenance compared with controls. ESWT may be a promising approach for the treatment of RCT. Due to the limited quality and number of included trials, additional high-quality prospective clinical studies are needed to verify these conclusions.
Supplementary Information
Acknowledgements
Not applicable.
Authors' contributions
All authors conceived and designed the study. Conceptualization: XLX. Literature search: XLX. Screening and study selection: QFS and HF. Data extraction: XWY and XLX. performed the data analysis. XLX and XWY wrote the manuscript. XLX, XWY, and AK revisions to the manuscript. GQC is the guarantor. All authors approved the final version of the manuscript.
Funding
The project is supported by the National Natural Science Foundation of China (82172423), the Bejing Municipal Natural Science Foundation (7222209), the Clinical queue construction project of Peking University Third Hospital (BYSYDL2022006), and the Key Laboratory of Sports Medicine of Sichuan Province and the Key Laboratory of The General Administration of Sport of China (2023-A033).
Availability of data and materials
All data analysed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
The original version of this article was revised: Yulei Liu (one of the corresponding authors) has been added to the author group.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xiali Xue, Qingfa Song and Xinwei Yang contributed equally to this work.
Change history
7/1/2024
A Correction to this paper has been published: 10.1186/s12891-024-07611-x
Contributor Information
Yulei Liu, Email: liuyuleiok@sina.com.
Guoqing Cui, Email: drcuiguoqing1964@126.com.
References
- 1.Rhee SM, Youn SM, Park JH, Rhee YG. Biceps Rerouting for Semirigid Large-to-Massive Rotator Cuff Tears. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2021;37(9):2769–2779. doi: 10.1016/j.arthro.2021.04.008. [DOI] [PubMed] [Google Scholar]
- 2.Fitzpatrick LA, Atinga A, White L, Henry PDG, Probyn L. Rotator Cuff Injury and Repair. Seminars in musculoskeletal radiology. 2022;26(5):585–596. doi: 10.1055/s-0042-1756167. [DOI] [PubMed] [Google Scholar]
- 3.Hu Y, Wu L, He L, Luo X, Hu L, Wang Y, Zhao X. Bibliometric and visualized analysis of scientific publications on rehabilitation of rotator cuff injury based on web of science. Front Public Health. 2023;11:1064576. doi: 10.3389/fpubh.2023.1064576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Longo UG, Candela V, Berton A, Salvatore G, Guarnieri A, DeAngelis J, Nazarian A, Denaro V. Genetic basis of rotator cuff injury: a systematic review. BMC Med Genet. 2019;20(1):149. doi: 10.1186/s12881-019-0883-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rodriguez-Santiago B, Castillo B, Baerga-Varela L, Micheo WF. Rehabilitation Management of Rotator Cuff Injuries in the Master Athlete. Curr Sports Med Rep. 2019;18(9):330–337. doi: 10.1249/JSR.0000000000000628. [DOI] [PubMed] [Google Scholar]
- 6.Weber S, Chahal J. Management of Rotator Cuff Injuries. J Am Acad Orthop Surg. 2020;28(5):e193–e201. doi: 10.5435/JAAOS-D-19-00463. [DOI] [PubMed] [Google Scholar]
- 7.Dang A, Davies M. Rotator Cuff Disease: Treatment Options and Considerations. Sports Med Arthrosc Rev. 2018;26(3):129–133. doi: 10.1097/JSA.0000000000000207. [DOI] [PubMed] [Google Scholar]
- 8.Ramme AJ, Robbins CB, Patel KA, Carpenter JE, Bedi A, Gagnier JJ, Miller BS. Surgical Versus Nonsurgical Management of Rotator Cuff Tears: A Matched-Pair Analysis. The Journal of bone and joint surgery American. 2019;101(19):1775–1782. doi: 10.2106/JBJS.18.01473. [DOI] [PubMed] [Google Scholar]
- 9.Sciarretta FV, Moya D, List K. Current trends in rehabilitation of rotator cuff injuries. Sicot-j. 2023;9:14. doi: 10.1051/sicotj/2023011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Auersperg V, Trieb K. Extracorporeal shock wave therapy: an update. EFORT open reviews. 2020;5(10):584–592. doi: 10.1302/2058-5241.5.190067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheng JH, Wang CJ. Biological mechanism of shockwave in bone. International journal of surgery (London, England) 2015;24(Pt B):143–146. doi: 10.1016/j.ijsu.2015.06.059. [DOI] [PubMed] [Google Scholar]
- 12.Lv F, Li Z, Jing Y, Sun L, Li Z, Duan H. The effects and underlying mechanism of extracorporeal shockwave therapy on fracture healing. Front Endocrinol. 2023;14:1188297. doi: 10.3389/fendo.2023.1188297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Frizziero A, Vittadini F, Barazzuol M, Gasparre G, Finotti P, Meneghini A, Maffulli N, Masiero S. Extracorporeal shockwaves therapy versus hyaluronic acid injection for the treatment of painful non-calcific rotator cuff tendinopathies: preliminary results. J Sports Med Phys Fitness. 2017;57(9):1162–1168. doi: 10.23736/S0022-4707.16.06408-2. [DOI] [PubMed] [Google Scholar]
- 14.Gerdesmeyer L, Wagenpfeil S, Haake M, Maier M, Loew M, Wörtler K, Lampe R, Seil R, Handle G, Gassel S, et al. Extracorporeal shock wave therapy for the treatment of chronic calcifying tendonitis of the rotator cuff: a randomized controlled trial. JAMA. 2003;290(19):2573–2580. doi: 10.1001/jama.290.19.2573. [DOI] [PubMed] [Google Scholar]
- 15.Dedes V, Tzirogiannis K, Polikandrioti M, Dede AM, Nikolaidis C, Mitseas A, Panoutsopoulos GI. Comparison of Radial Extracorporeal Shockwave Therapy versus Ultrasound Therapy in the Treatment of Rotator Cuff Tendinopathy. Folia Med. 2019;61(4):612–619. doi: 10.3897/folmed.61.e47916. [DOI] [PubMed] [Google Scholar]
- 16.Kim JY, Lee JS, Park CW. Extracorporeal shock wave therapy is not useful after arthroscopic rotator cuff repair. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2012;20(12):2567–2572. doi: 10.1007/s00167-012-1923-8. [DOI] [PubMed] [Google Scholar]
- 17.Efe T, Felgentreff M, Heyse TJ, Stein T, Timmesfeld N, Schmitt J, Roessler PP. Extracorporeal shock wave therapy for non-calcific supraspinatus tendinitis - 10-year follow-up of a randomized placebo-controlled trial. Biomedizinische Technik Biomedical engineering. 2014;59(5):431–437. doi: 10.1515/bmt-2013-0135. [DOI] [PubMed] [Google Scholar]
- 18.Kamonseki DH, da Rocha GM, Mascarenhas V, de Melo Ocarino J, Pogetti LS: Extracorporeal shock-wave therapy for the treatment of non-calcific rotator cuff tendinopathy: A systematic review and meta-analysis. American journal of physical medicine & rehabilitation 2023. [DOI] [PubMed]
- 19.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (Clinical research ed) 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cacchio A, Paoloni M, Barile A, Don R, de Paulis F, Calvisi V, Ranavolo A, Frascarelli M, Santilli V, Spacca G. Effectiveness of radial shock-wave therapy for calcific tendinitis of the shoulder: single-blind, randomized clinical study. Phys Ther. 2006;86(5):672–682. [PubMed] [Google Scholar]
- 21.Xiangzheng S, Zhongli L, Ji L, Hao Z, Chunhui L. Effect of extracorpeal shock wave combined with functional exercise on rotator cuff injury. Academic Journal of Chinese PLA Medical School. 2018;39(5):408–410. [Google Scholar]
- 22.Duymaz T, Sindel D. Comparison of Radial Extracorporeal Shock Wave Therapy and Traditional Physiotherapy in Rotator Cuff Calcific Tendinitis Treatment. Archives of rheumatology. 2019;34(3):281–287. doi: 10.5606/ArchRheumatol.2019.7081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fan C, Cong L, Hui P. Therapeutic effect of extracorporeal shock wave combined with exercise therapy on rotator cuff injury of weightlifters. Chinese Manipulation & Rehabilitation Medicine. 2018;9(10):5–7. [Google Scholar]
- 24.Fatima A, Ahmad A, Gilani SA, Darain H, Kazmi S, Hanif K. Effects of High-Energy Extracorporeal Shockwave Therapy on Pain, Functional Disability, Quality of Life, and Ultrasonographic Changes in Patients with Calcified Rotator Cuff Tendinopathy. Biomed Res Int. 2022;2022:1230857. doi: 10.1155/2022/1230857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Galasso O, Amelio E, Riccelli DA, Gasparini G. Short-term outcomes of extracorporeal shock wave therapy for the treatment of chronic non-calcific tendinopathy of the supraspinatus: a double-blind, randomized, placebo-controlled trial. BMC Musculoskelet Disord. 2012;13:86. doi: 10.1186/1471-2474-13-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guowei W, Yongjie L, Junsheng M, Shui S, Jiying C, Xunkai H, Qingshan S. Efficacy of extracorporeal shock wave in the treatment of chronic rotator cuff injury. Chinese Journal of Physical Medicine and Rehabilitation. 2013;35(6):479–480. [Google Scholar]
- 27.Junfan Z, Feng G, Shurong C, Shaoyun S, Xin C. The Effect of the Diffuse Shock Wave Combined with Joint Mobilization on No Serious Rotator Cuff Injury. Chinese and Foreign Medical Research. 2020;18(33):22–24. [Google Scholar]
- 28.Qiuen X, Qian W, Xinjun X, Yonggui X, Xiong Z. Effect of Extracorporeal Shock Wave Therapy combined with Xujin JieguLiquid and Sinew Adjusting Manipulationon Rotator Cuff Injury. Guiding Journal of Traditional Chinese Medicine and Pharmacy. 2017;23(20):93–95. [Google Scholar]
- 29.Hong S, Shurong Z, Jun C, Aizhen W, Ziying W, Mingru H, Wei Y, Zifan L, Chang L, Zhengbiao J, et al. Radial extracorporeal shockwave therapy reduces pain and promotes proximal tendon healing after rotator cuff repair: Randomized clinical trial. Ann Phys Rehabil Med. 2023;66(4):101730. doi: 10.1016/j.rehab.2023.101730. [DOI] [PubMed] [Google Scholar]
- 30.Weibin X, Jia D, Mei Z, Hu W. Effect of extracorporeal shock wave assisted local acupuncture aspiration on joint function in middle-aged and elderly patients with acute calcifying rotator cuff tendinitis. Contemporary Medicine. 2022;28(2):169–171. [Google Scholar]
- 31.Weiwei Z, Wei C, Jingjie Z, Ming Z, Xinyu L, Xiuyan L. A randomized controlled clinical study of electromagnetic extracorporeal shock waveon shoulder dysfunction after arthroscopic repair of rotator cuff degeneration. Journal of Hebei Medical University. 2021;42(4):390–394. [Google Scholar]
- 32.Xuping Z, Baihong C, Yunxiang Y, Rongfang S: shock wave therapy on arthroscopic rotator cuff repair Perioperative intervention effect of accelerated rehabilitation combined with extracorporeal. Journal of Logistics University of PAP ( Medical Sciences ) 2021, 30(12):159–160+163.
- 33.Yang X, Xiaomei G, Yimeng K, Guilin Z, Zhicheng S. Clinical effects of water-filtered infrared-A combined with extracorporeal shock wave in elderly patients with rotator cuff injury. Practical Geriatrics. 2022;36(9):948–951. [Google Scholar]
- 34.Yong T, Wenwu X, Shundong Z, Tongtong W. Clinical efficacy of medium energy focused extracorporeal shock wave in the treatment of rotator cuff calcific tendinitis. Zhongguo kang fu. 2020;35(9):472–475. [Google Scholar]
- 35.Xianzhe L, Jianliang S, Honghai Z, Qinghua L, Zhengwei Y, Liang Y. Clinical observation of extracorporeal shock wave combined with flubinofen gel paste in the treatment of rotator cuff injury. Journal of Clinical Anesthesiol. 2021;37(7):752–754. [Google Scholar]
- 36.Zhiyong Z, Ming Z, Junqu L, Shuye P. Clinical observation of extracorporeal shock wave therapy combined with floating needle therapy for rotator cuff injury. Chinese Journal of Modern Drug Application. 2020;14(22):226–227. [Google Scholar]
- 37.Gumucio JP, Korn MA, Saripalli AL, Flood MD, Phan AC, Roche SM, Lynch EB, Claflin DR, Bedi A, Mendias CL. Aging-associated exacerbation in fatty degeneration and infiltration after rotator cuff tear. J Shoulder Elbow Surg. 2014;23(1):99–108. doi: 10.1016/j.jse.2013.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ryskalin L, Morucci G, Natale G, Soldani P, Gesi M: Molecular Mechanisms Underlying the Pain-Relieving Effects of Extracorporeal Shock Wave Therapy: A Focus on Fascia Nociceptors. Life (Basel, Switzerland) 2022, 12(5):743. [DOI] [PMC free article] [PubMed]
- 39.Kim SH, Ha KW, Kim YH, Seol PH, Kwak HJ, Park SW, Ryu BJ. Effect of Radial Extracorporeal Shock Wave Therapy on Hemiplegic Shoulder Pain Syndrome. Ann Rehabil Med. 2016;40(3):509–519. doi: 10.5535/arm.2016.40.3.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schleusser S, Song J, Stang FH, Mailaender P, Kraemer R, Kisch T. Blood Flow in the Scaphoid Is Improved by Focused Extracorporeal Shock Wave Therapy. Clin Orthop Relat Res. 2020;478(1):127–135. doi: 10.1097/CORR.0000000000000993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yoon SY, Kim YW, Shin IS, Moon HI, Lee SC. Does the Type of Extracorporeal Shock Therapy Influence Treatment Effectiveness in Lateral Epicondylitis? A Systematic Review and Meta-analysis. Clin Orthop Relat Res. 2020;478(10):2324–2339. doi: 10.1097/CORR.0000000000001246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pellegrino R, Di Iorio A, Brindisino F, Paolucci T, Moretti A, Iolascon G. Effectiveness of combined extracorporeal shock-wave therapy and hyaluronic acid injections for patients with shoulder pain due to rotator cuff tendinopathy: a person-centered approach with a focus on gender differences to treatment response. BMC Musculoskelet Disord. 2022;23(1):863. doi: 10.1186/s12891-022-05819-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Notarnicola A, Moretti L, Tafuri S, Panella A, Filipponi M, Casalino A, Panella M, Moretti B Shockwave therapy in the management of complex regional pain syndrome in medial femoral condyle of the knee. Ultrasound Med Biol. 2010;36(6):874–879. doi: 10.1016/j.ultrasmedbio.2010.03.012. [DOI] [PubMed] [Google Scholar]
- 44.Ko JY, Siu KK, Wang FS, Wang CJ, Chou WY, Huang CC, Kuo SJ. The Therapeutic Effects of Extracorporeal Shock Wave Therapy (ESWT) on the Rotator Cuff Lesions with Shoulder Stiffness: A Prospective Randomized Study. Biomed Res Int. 2020;2020:6501714. doi: 10.1155/2020/6501714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cosentino R, De Stefano R, Selvi E, Frati E, Manca S, Frediani B, Marcolongo R. Extracorporeal shock wave therapy for chronic calcific tendinitis of the shoulder: single blind study. Ann Rheum Dis. 2003;62(3):248–250. doi: 10.1136/ard.62.3.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hsu CJ, Wang DY, Tseng KF, Fong YC, Hsu HC, Jim YF. Extracorporeal shock wave therapy for calcifying tendinitis of the shoulder. J Shoulder Elbow Surg. 2008;17(1):55–59. doi: 10.1016/j.jse.2007.03.023. [DOI] [PubMed] [Google Scholar]
- 47.Schroeder AN, Tenforde AS, Jelsing EJ. Extracorporeal Shockwave Therapy in the Management of Sports Medicine Injuries. Curr Sports Med Rep. 2021;20(6):298–305. doi: 10.1249/JSR.0000000000000851. [DOI] [PubMed] [Google Scholar]
- 48.Kenmoku T, Nemoto N, Iwakura N, Ochiai N, Uchida K, Saisu T, Ohtori S, Nakagawa K, Sasho T, Takaso M. Extracorporeal shock wave treatment can selectively destroy end plates in neuromuscular junctions. Muscle Nerve. 2018;57(3):466–472. doi: 10.1002/mus.25754. [DOI] [PubMed] [Google Scholar]
- 49.Frassanito P, Cavalieri C, Maestri R, Felicetti G. Effectiveness of Extracorporeal Shock Wave Therapy and kinesio taping in calcific tendinopathy of the shoulder: a randomized controlled trial. Eur J Phys Rehabil Med. 2018;54(3):333–340. doi: 10.23736/S1973-9087.17.04749-9. [DOI] [PubMed] [Google Scholar]
- 50.Steuri R, Sattelmayer M, Elsig S, Kolly C, Tal A, Taeymans J, Hilfiker R. Effectiveness of conservative interventions including exercise, manual therapy and medical management in adults with shoulder impingement: a systematic review and meta-analysis of RCTs. Br J Sports Med. 2017;51(18):1340–1347. doi: 10.1136/bjsports-2016-096515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Li W, Zhang SX, Yang Q, Li BL, Meng QG, Guo ZG. Effect of extracorporeal shock-wave therapy for treating patients with chronic rotator cuff tendonitis. Medicine. 2017;96(35):e7940. doi: 10.1097/MD.0000000000007940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kvalvaag E, Roe C, Engebretsen KB, Soberg HL, Juel NG, Bautz-Holter E, Sandvik L, Brox JI. One year results of a randomized controlled trial on radial Extracorporeal Shock Wave Treatment, with predictors of pain, disability and return to work in patients with subacromial pain syndrome. Eur J Phys Rehabil Med. 2018;54(3):341–350. doi: 10.23736/S1973-9087.17.04748-7. [DOI] [PubMed] [Google Scholar]
- 53.Kolk A, Yang KG, Tamminga R, van der Hoeven H: Radial extracorporeal shock-wave therapy in patients with chronic rotator cuff tendinitis: a prospective randomised double-blind placebo-controlled multicentre trial. The Bone Joint J. 2013, 95-b(11):1521–1526. [DOI] [PubMed]
- 54.Speed CA, Richards C, Nichols D, Burnet S, Wies JT, Humphreys H, Hazleman BL: Extracorporeal shock-wave therapy for tendonitis of the rotator cuff. A double-blind, randomised, controlled trial. J Bone Joint Surgery British 2002, 84(4):509–512. [DOI] [PubMed]
- 55.Kenmoku T, Iwakura N, Ochiai N, Saisu T, Ohtori S, Takahashi K, Nakazawa T, Fukuda M, Takaso M. Influence of different energy patterns on efficacy of radial shock wave therapy. Journal of orthopaedic science : official journal of the Japanese Orthopaedic Association. 2021;26(4):698–703. doi: 10.1016/j.jos.2020.07.009. [DOI] [PubMed] [Google Scholar]
- 56.Sayegh ET, Strauch RJ. Does nonsurgical treatment improve longitudinal outcomes of lateral epicondylitis over no treatment? A meta-analysis. Clin Orthop Relat Res. 2015;473(3):1093–1107. doi: 10.1007/s11999-014-4022-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pellegrino R, Di Iorio A, Filoni S, Mondardini P, Paolucci T, Sparvieri E, Tarantino D, Moretti A, Iolascon G: Radial or Focal Extracorporeal Shock Wave Therapy in Lateral Elbow Tendinopathy: A Real-Life Retrospective Study. Int J Environ Res Public Health 2023, 20(5)4371. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data analysed during this study are included in this published article.