Abstract
While multi-level theories and frameworks have become a cornerstone in broader efforts to address HIV inequities, little is known regarding their application in adolescent and young adult (AYA) HIV research. To address this gap, we conducted a scoping review to assess the use and application of multi-level theories and frameworks in AYA HIV prevention and care and treatment empirical research. We systematically searched five databases for articles published between 2010 and May 2020, screened abstracts, and reviewed eligible full-text articles for inclusion. Of the 5890 citations identified, 1706 underwent full-text review and 88 met the inclusion criteria: 70 focused on HIV prevention, with only 14 on care and treatment, 2 on both HIV prevention and care and treatment, and 2 on HIV-affected AYA. Most authors described the theory-based multi-level framework as informing their data analysis, with only 12 describing it as informing/guiding an intervention. More than seventy different multi-level theories were described, with 38% utilizing socio-ecological models or the eco-developmental theory. Findings were used to inform the adaptation of an AYA World Health Organization multi-level framework specifically to guide AYA HIV research.
Keywords: HIV, Adolescents, Young adults, Multi-level theories, Review
Introduction
In an era where advances in HIV prevention, care, and treatment have led to calls for the end of the AIDS epidemic [1, 2], the disproportionate burden of HIV on adolescents and young adults (AYA) continues to grow. In 2020, an estimated 410,000 young people aged 10 to 24 years newly acquired HIV worldwide [3], and only slightly more than half of adolescents living with HIV (940,000/1.7 million) received antiretroviral therapy (ART) [4]. In response to these stark statistics, the Johns Hopkins University (JHU) Center for AIDS Research (CFAR) Adolescent and Young Adult Scientific Working Group (AYA SWG) was convened with the mission to promote interdisciplinary research collaborations across the intersecting domains of AYA health and HIV (https://hopkinscfar.org/science-cores/adolescent-young-adult-swg/). Early in the formation of the AYA SWG, members across the JHU schools of medicine, nursing, and public health, shared the different conceptual theories and frameworks they used in their work with young people. This process highlighted a gap with multi-level theories (defined here as theories and/or frameworks encompassing several tiers of influence), needed to guide research and programs for AYA HIV prevention, care, and treatment. The AYA SWG decided to address this gap as presented in this paper.
Multi-level theories, such as Socio-Ecological Models (SEMs), are an important tool for identifying how individuals interact with their environment, and how the interplay of risk and protective factors across levels (e.g., individual, interpersonal, environmental, macrosocial) influences and provides intervention points for health behaviors and outcomes. Several HIV-specific SEMs [5–11] provide a strong rationale and evidence that intervening on multiple levels can mitigate HIV acquisition more than individual-level approaches alone [12, 13]. However, these HIV-specific SEMs are not tailored to AYA and their distinct developmental stages. Furthermore, there are SEMs that focus on children and youth development, including Bronfenbrenner’s, [14]; Blum et al. [15], and the World Health Organization’s (WHO) Ecological Model of the Determinants of Adolescent Health and Development [16], but these broader AYA SEMs do not address HIV explicitly.
We need HIV specific, theory-based multi-level research and programs that address the profound growth that AYA experience. Adolescent development, from early, middle, and late adolescence through young adulthood, is characterized by an expanding ability to think abstractly, plan for the future, and establish a secure identity. Adolescence can also be a time for vulnerability due to an inability to link cause with effects of behavior and to incorporate risk perception into behavior [16]. These changes may influence AYA exposure to HIV risk and protective factors. At the same time, AYA access to services, social roles in different settings, and protections under the law may also be shifting. The extent to which AYA’s health and well-being are fostered or hindered during these years has consequences across the life course, as well as into the life of the next generation [17].
A first step toward achieving an AYA HIV specific multi-level framework is to review if and how researchers in the field of AYA HIV have applied such frameworks in their research; and in doing so, identify potential gaps. To address this need, we conducted a scoping review of the literature from 2010 to May 2020. The objectives of this paper are to present the findings of the scoping review of AYA HIV prevention and care and treatment empirical research that directly state use of named multi-level theories and frameworks, also describing how the theory or framework was used, and how it was applied in those studies assessed. Results of this scoping review were used by the JHU CFAR AYA SWG to adapt an existing AYA multi-level framework to further tailor it to AYA HIV prevention and care and treatment. The hope was that the revised framework could be used as an interdisciplinary tool to guide and generate thought related to AYA HIV prevention and treatment researchers in their analyses, study designs, and interventions. This AYA HIV specific framework is presented in this paper.
Methods
Data Source
We searched the following five electronic databases: PubMed, Embase, CINAHL Plus (Ebsco), PsycINFO, and Sociological Abstracts through May 2020. For each database, a search strategy was developed in collaboration with an Informationist at the JHU Welch Medical Library to identify articles that included multi-level approaches in the context of HIV prevention and care and treatment among AYA. MeSH terms, when available, were searched for HIV, adolescent, and theoretical frameworks. Otherwise, searches were restricted to titles and abstracts using the following algorithm: {“HIV” OR “human immunodeficiency virus” OR “AIDS”} AND {“adolescent” OR “youth” OR “young adult” OR “teen” OR “student”} AND {“theoretical model” OR “conceptual model” OR “theoretical framework” OR “conceptual framework” OR “social ecological model” OR “socio ecological model” OR “multi-level” OR “multilevel”}. Truncation was used as appropriate (see Appendix Table 4 for search terms). All search results were imported into an EndNote database prior to coding with duplicate articles deleted. Articles were then uploaded into Covidence [18] for screening and review.
Table 4.
Search terms
| Concept #1 HIV | Concept #2 Adolescent | Concept #3 Conceptual models | |
|---|---|---|---|
| PubMed | HIV[mesh] OR HIV[tiab] OR AIDS Virus*[tiab] | Adolescent[Mesh] OR Young Adult[Mesh] OR Adolescen*[tiab] OR Teen*[tiab] OR Youth*[tiab] OR young adult*[tiab] OR student*[tiab] | Models, theoretical[mesh] OR theoretical model*[tiab] OR conceptual model*[tiab] OR theoretical framework*[tiab] OR conceptual framework*[tiab] OR social-ecological model*[tiab] OR socio-ecological model*[tiab] OR multi-level[tiab] OR multilevel[tiab] Filters: from 2010/1/1 - 2020/5/31 |
| Embase | 'Human immunodeficiency virus'/exp OR (‘HIV’ OR ‘AIDS virus*’):ab,ti,kw | ‘Adolescent’/exp OR ‘Young Adult’/exp OR (‘Adolescen*’ OR ‘Teen*’ OR ‘Teen’ OR ‘Youth*’ OR ‘young adult*’ OR ‘student*’):ab,ti,kw | ‘Theoretical model’/exp OR ‘conceptual framework’/exp ’OR 'multilevel analysis'/exp OR 'social ecological model'/exp OR (‘theoretical model*’ OR ‘conceptual model*’ OR ‘theoretical framework*’ OR ‘conceptual framework*’ OR ‘social ecological model*’ OR ‘socio ecological model* OR multilevel OR 'multi level'):ab,ti,kw |
| CINHAL | (MM "Human Immunodeficiency Virus") OR “HIV” OR “AIDS virus*” | MM "Adolescent" OR MM "Young Adult" OR "Adolescen*” OR "Teen*" OR "Youth*" OR "young adult*" OR “student*” | (MM "Models, Theoretical") OR (MM "Conceptual Framework") OR "theoretical model*" OR "conceptual model*" OR "theoretical framework*" OR "conceptual framework*" OR “social ecological model*” OR “socio ecological model*” OR multilevel OR multi-level |
| PsycINFO | DE "HIV" OR DE "AIDS" OR “HIV” OR “AIDS virus*” | “adolescen*” OR “young adult*” OR “teen*” OR “youth*” OR “young adult*” | “theoretical model*” OR “conceptual model*” OR “theoretical framework*” OR “conceptual framework*” OR “social ecological model*” OR “socio ecological model” OR multilevel OR multi-level |
| Sociologic Abstracts | ab,ti,su(HIV) OR ab,ti,su(AIDS virus) | ab,ti,su(Adolescen*) OR ab,ti,su(Teen*) OR ab,ti,su(Youth*) OR ab,ti,su(young adult*) OR ab,ti,su(student*) | ab,ti,su(theoretical model*) OR ab,ti,su(conceptual model*) OR ab,ti,su (theoretical framework*) OR ab,ti,su(conceptual framework*) OR ab,ti,su(social ecological model*) OR ab,ti,su(socio ecological model*) OR ab,ti,su(multilevel) OR ab,ti,su(multi-level) |
*MM major concept, DE subject {exact} (explode), MH explode
Inclusion Criteria
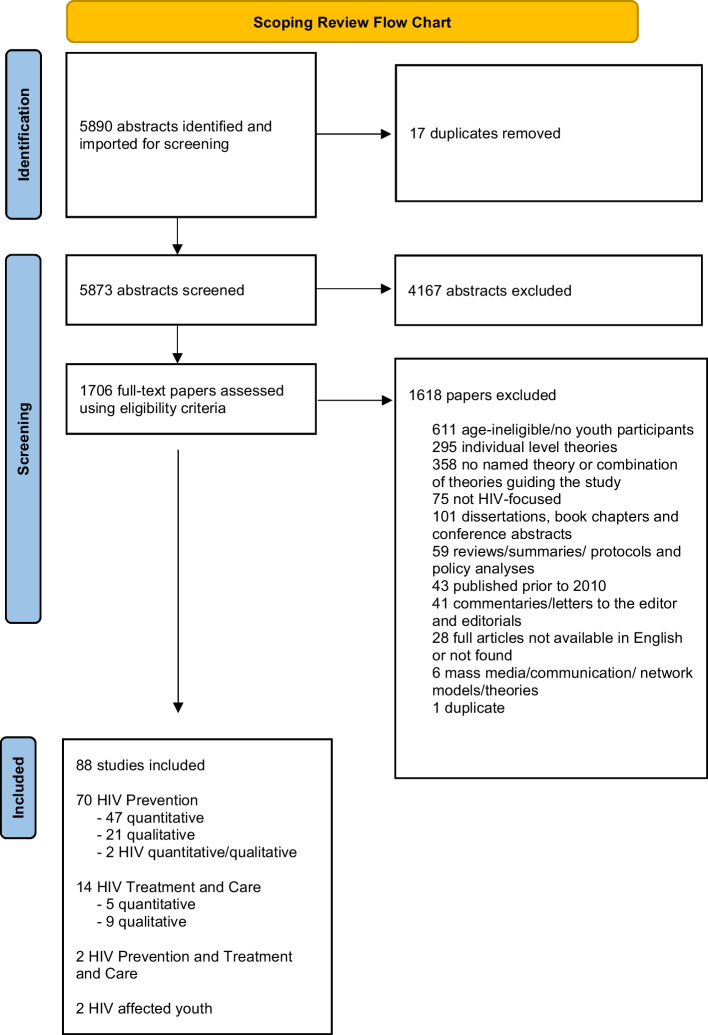
The review of records for inclusion was sequential. After initial screening in Covidence to exclude articles not related to HIV or with a mean participant age > 25 years, a full text double review was conducted (by authors SD, JAD, KW, CY, KMS) to ensure the remaining articles met the following inclusion criteria: (1) the study population consisted predominantly of AYA aged 10–24 years based on the WHO definition (mean or median age fell between 10 and 24 years or 50% or more of the study population were AYA); (2) were HIV-focused; (3) presented a named multi-level theory (defined here as theories and/or frameworks encompassing several tiers of influence); and (4) were published in 2010–May 2020. Figure 1 details the reasons for exclusions, with most articles excluded based on age of participants, presenting only individual-level theories (e.g., Health Belief Model, Theory of Planned Behavior, Social Cognitive Theory), and not having a named theory or combination of theories that addressed factors on multiple levels. We reviewed articles published from 2010 to May 2020 to account for the following advances: (1) the availability of some prominent AYA—general health SEMs [15, 16]; (2) an increasing focus and awareness of AYA as a critical population to achieve the UNAIDS 90-90-90 HIV goals [19, 20]; and (3) the emerging application of multi-level theories and frameworks to HIV, including advances in technology and the push for combination interventions. Discrepancies between the two reviewers were then resolved by a third reviewer and, if needed, discussion and consensus among all three reviewers.
Fig. 1.
Scoping review prisma flow chart
Data Extraction
Two independent reviewers extracted data from each article that met the inclusion criteria. Discrepancies were resolved by a third reviewer to check for consistency. Data extracted from each article included author name; year of publication; location(s) of the study; whether the article focused on HIV prevention or care and treatment, or both; the names of the multi-level approach(es) used; and a concise description on how the approaches were used in the article as described by the authors. Data were extracted using a standard extraction form in Excel.
Results
Of the initial 5890 articles of the search, 1706 underwent full text review, after which 88 met the inclusion criteria. Details of the search and screening results are presented in Figure 1, and details of the included articles are provided in Tables 1, 2, 3. Altogether, 70 of the 88 included articles focused on HIV prevention [21–89
Table 1.
List of HIV prevention quantitative articles identified (n = 47)
| Year | Location(s) | Name of multi-level theory/framework | How multi-level theory/framework was used | |
|---|---|---|---|---|
| Babalola | 2011 | Multiple countries in SSA | • Boerma and Weir’s proximate determinants framework | Informed data analysis |
| Bauermeister | 2011 | USA | • Social disorganization theory | Informed measure creation and data analysis |
| Brennan | 2012 | USA | • Syndemic theory | Informed measures and data analysis |
| Burton | 2019 | Canada | • Social ecological model | Informed measure selection and data analysis |
| Carlson | 2012 | Tanzania | • Sen’s capability theory | Informed intervention development and analysis |
| • Habermas’ communication action theory | ||||
| • Boal’s participatory drama method | ||||
| • Bronfenbrenner’s ecological theory | ||||
| • Bandura’s theory of self and collective efficacy | ||||
| Cheruiyot | 2019 | Kenya | • Andersen and Newman’s framework of healthcare utilization | Informed measures selected and data analysis |
| Cho | 2019 | Kenya | • The four bases of gendered power | Informed data analysis |
| Cluver | 2013 | South Africa | • Interactive theoretical model developed by the research team | Study tested the interactive theoretical model that was informed by the other named theories/models |
| • Sameroff’s transactional theory of impacts of parental psychopathology | ||||
| • Cicchetti’s ecological/transactional model of impacts of child maltreatment | ||||
| • Rutter’s pathways theory to identify direct and indirect chain effects of childhood adversity | ||||
| Cordova | 2016 | USA | • Ecodevelopmental theory | Informed analysis and testing of the parent-adolescent family functioning discrepancy hypotheses |
| Cordova | 2020 | USA | • Empowerment theory | Informed intervention |
| • Ecodevelopmental theory | ||||
| Coyle | 2019 | USA | • Positive youth development framework | Informed intervention and data analysis |
| • Social cognitive theory | ||||
| DeAtley | 2020 | South Africa | • Bronfenbrenner’s ecological systems theory | Guided the study and data analysis |
| Eisenberg | 2013 | USA | • Social ecological frameworks | Guided study and data analysis |
| Folayan | 2016 | Nigeria | • Lazarus and Folkman’s conceptual framework of stress and coping | Informed data analysis |
| Halkitis (1) | 2013 | USA | • Fundamental causes theory | Informed data analysis |
| • Syndemic theory | ||||
| Halkitis (2) | 2013 | USA | • Singer’s syndemic theory | Informed data analysis |
| Huebner | 2014 | USA | • Diaz’s model of social oppression | Tested the model |
| James | 2018 | USA | • Social ecological model | Guided the study |
| Johns | 2010 | USA | • Social disorganization theory (SDT) | SDT informed hypothesis 2, TGP used to interpret a finding |
| • Theory of gender and power (TGP) | ||||
| Karamagi | 2018 | Uganda | • Quality improvement for behavior change model (QBC) | Tested the model’s effectiveness on outcome |
| Li | 2019 | USA | • Szapocznik and Coatsworth’s ecodevelopmental theory | Guided the study and data analysis |
| Logie | 2017 | Jamaica | • Baral’s social ecological model | Guided the study and data analysis |
| Mathur | 2020 | Kenya, Malawi, Zambia | • Proximate determinants theoretical framework | Informed analysis |
| Maticka-Tyndale | 2010 | Kenya | • Information motivation behavioral skills model | Informed analysis |
| • Campbell’s identification of community influence on HIV risk reduction model | ||||
| Miller | 2018 | USA | • Bernard et al.’s conceptual work on community opportunity structures | Informed analysis |
| • Hatzenbuehler et al.’s conceptual work on structural stigma | ||||
| Mmari | 2013 | Uganda | • Risk and protective factor framework | Informed analysis |
| • Ecological model | ||||
| Mustanski | 2019 | USA | • National Institute of minority health and health disparities multilevel research framework | Informed analysis |
| Moodley | 2017 | South Africa | • Secularization theory | Informed analysis |
| Nakazwe | 2019 | Zambia | • Proximate determinants framework | Informed analysis |
| Njoroge | 2010 | Kenya | • McLeroy’s social ecological model | Provided multilevel context for the study and for interpretation of findings |
| Pilgrim | 2015 | Uganda | • Bronfenbrenner’s ecological system theory | Informed analysis |
| Placek | 2019 | India | • McLeroy’s socioecological model | Informed parts of analysis |
| • Maternal fetal protection model | ||||
| Prado | 2010 | USA | • Ecodevelopmental theory | Theory tested |
| Prado | 2011 | USA | • Ecodevelopmental theory | Guided intervention |
| Robertson | 2010 | Multiple countries in SSA | • Expanded Boerma and Weir’s proximate determinants framework | Informed hypothesis development and analysis |
| Ruisenor-Escudero | 2017 | Togo | • Modified social ecological model | Informed study conceptualization and analysis |
| Salud | 2014 | USA | • AIDS risk reduction model | Informed conceptual framework for the study |
| • Acculturation | ||||
| • Theory of gender and power | ||||
| Schwandt | 2013 | Botswana, Malawi, and Mozambique | • Social ecological framework and ideation | Informed intervention and implementation |
| Ssewamala | 2012 | Uganda | • Asset theory | Guided study |
| • Resilience theory | ||||
| Stock | 2013 | USA | • Prototype/willingness model | Informed analysis |
| Tenkorang | 2014 | Kenya | • Information motivation behavioral skills model | Informed analysis |
| • Campbell’s community characteristics framework | ||||
| Tomita | 2017 | South Africa | • Social disorganization theory | Guided study and analysis |
| Tozan | 2019 | Uganda | • Asset theory | Informed intervention |
| Tyler | 2016 | Zambia | • Bronfenbrenner’s ecological framework | Guided study and analysis |
| Underwood | 2015 | Multiple countries in SSA | • Theory of economic and social organization | Informed analysis |
| Waldrop-Valverde | 2013 | USA | • Socio-ecological model | Informed analysis |
| Ward-Peterson | 2018 | Malawi | • Conceptual framework adapted from work by Barnett and Whiteside (2006) and [5] | Guided study and analysis |
Table 2.
List of HIV prevention qualitative and multi-methods articles identified
| Year | Location(s) | Name of multi-level theory/framework | How multi-level theory/framework | |
|---|---|---|---|---|
| HIV prevention (Qualitive n = 21) | ||||
| Bird | 2017 | USA | • Theory of emerging adulthood | Data used to create the Emergent Conceptual Model, named theories provide rationale and used in the interpretation of the new model |
| • Developmental approaches to family life-cycle | ||||
| • Family system theory | ||||
| • Structural family therapy | ||||
| • Emergent conceptual model developed by the research team | ||||
| Burch | 2018 | Malaysia | • Modified social-ecological model based on Mustanaski et al. (2011) | Guided study |
| Casale | 2011 | South Africa | • Critical social science approach | To develop an interview guide for focus group discussions and data analysis |
| • Conceptual framework developed by the research team | ||||
| Conn | 2013 | Uganda | • Framework of gender empowerment and positive sexuality | Framed the narrative analysis; applied to HIV prevention paradigms |
| Darlington | 2012 | Jamaica | • Socio-ecological model | Guided focus group discussions; organized themes that emerged from the data |
| Dyson | 2018 | USA | • Socio-ecological model | Informed data analysis |
| Enah | 2014 | USA | • Model of adolescent sexual risk behaviors | Informed semi-structured interviews and data analysis |
| • Elaboration likelihood model | ||||
| Harper | 2014 | Kenya | • Bronfenbrenner’s bioecological systems theory | Informed development of focus group guide and analysis |
| Hudson | 2012 | USA | • Comprehensive health seeking and coping paradigm | Guided data interpretation |
| Hutchinson | 2012 | Jamaica | • Theory of planned behavior | Informed semi-structure interview guides |
| • Parental expansion of theory of planned behavior | ||||
| Katz | 2013 | Uganda | • Explanatory framework of adolescent sexual decision-making | Data used to create the Explanatory Framework |
| Khan | 2018 | India | • Structural violence | Informed interpretation of data |
| • Moral pragmatics | ||||
| • Foucault state power and discourse | ||||
| Kubicek | 2015 | USA | • Resource theory | Informed framing of research question |
| Logie | 2018 | Jamaica | • Syndemics theoretical framework | Guided the study and data analysis |
| Lyons | 2013 | USA | • Syndemic theory | Informed research questions |
| Newman | 2013 | Thailand | • Socio-ecological models based on Bronfenbrenner’s ecological systems theory | Informed semi-structured interview guide; guided conceptual map and presentation of results |
| Nwokocha | 2015 | Nigeria | • Conceptual framework based on structural functionalism, rational choice, and differential association theories | Guided the study |
| Rahangdale | 2010 | India | • Modified Steward’s framework on stigma | Informed data analysis and interpretation of results |
| Richardson | 2013 | USA | • Anderson’s code of the street | Informed focus group discussion guide and analysis |
| Stevens | 2013 | USA | • Integrative model of behavior change | Used to develop the focus group script and Informed analysis |
| • Ecological systems theory | ||||
| Underwood | 2011 | Botswana, Malawi, and Mozambique | • Stokol’s social ecological perspective | Informed the analysis |
| • Social ecology | ||||
| HIV prevention (Multi-methods—quantitative and qualitative n = 2) | ||||
| Arrington-Sanders | 2016 | USA | • Bronfenbrenner’s ecological systems theory | Informed analysis |
| Cordova | 2019 | USA | • Empowerment theory | Informed intervention |
| • Ecodevelopmental theory | ||||
Table 3.
List of HIV ‘care and treatment’ and ‘prevention and care and treatment’ articles identified
| Year | Location(s) | Name of multi-level theory/framework | How multi-level theory/framework was used | |
|---|---|---|---|---|
| HIV treatment and care (Quantitative n = 5) | ||||
| Jeffries | 2017 | USA | • Social ecological theory | Informed study analysis |
| Mutumba | 2017 | Uganda | • Transactional model of stress and coping | Informed multilevel factors |
| Naar-King | 2013 | USA | • Socio ecological model | Hypothesized the association among multilevel factors and non-adherence; assessed analysis |
| Pantelic | 2017 | South Africa | • Hypothesized risk pathways from HIV-related disability to internalized HIV stigma | Informed study hypothesis |
| Nestadt | 2019 | Thailand | • Modified social action theory | Informed intervention |
| HIV treatment and care (Qualitative n = 9) | ||||
| Ashaba | 2019 | Uganda | • Conceptual model | Informed the relationship of the study variables |
| Crowley | 2019 | South Africa | • Self-management conceptual framework | Guided the study |
| • Individual and family self-management theory | ||||
| • Bronfenbrenner’s ecological systems theory | ||||
| Galea | 2018 | Peru | • Social ecological systems theory | To guide analysis and conceptualization of the data |
| Harper | 2019 | Kenya | • Disability-stress-coping model | To guide inquiry and analysis |
| Mutumba | 2019 | Uganda | • Self-management of chronic diseases framework | Informed multilevel factors |
| Rutakumwa | 2015 | Uganda | • Family systems circular causality | Informed interpretation of study findings; guided study implications and future research |
| Skovdal | 2012 | Kenya | • Peer social capital framework | Informed study methodology |
| Wolf | 2019 | Kenya | • Socio-ecological model | Informed study |
| Wong | 2017 | China | • Conceptual model of sexual health disclosure | Guided semi-structured interviews; informed results |
| HIV prevention and care and treatment (Mixed methods n = 2) | ||||
| McKay | 2014 | USA | • Social action theory | Informed the “CHAMP+” intervention components |
| Vu | 2017 | Uganda | • Human rights framework | Guided the “Link Up” intervention |
| HIV affected youth (Quantitative n = 2) | ||||
| Li | 2019 | China | • Social action theoretical framework | Informed the intervention |
| Li | 2017 | China | • Socioecological theories of child development | Informed the intervention |
| • Psychological resilience theories | ||||
90], 14 on HIV care and treatment [91–104], 2 on both HIV prevention and care and treatment [105, 106] and 2 with HIV affected youth [107, 108]. Out of the 70 HIV prevention-focused articles (Tables 1, 2, 3), 31 were studies conducted in sub-Saharan Africa (SSA), 30 in North America, 5 in South Asia, and 4 in the Caribbean Islands. For the HIV care and treatment-focused articles, 9 were from SSA, 2 from North America, 2 from Asia and 1 from South America. In terms of methods, 54 articles presented quantitative data only, 30 articles presented qualitative data only, and 4 articles presented both quantitative and qualitative data. Nine of the fourteen (64%) articles on care and treatment only presented findings from qualitative research, in comparison to 21 of 70 (30%) of the HIV prevention articles. Additionally, most care and treatment articles (79%) were published in 2017 or later, while a smaller proportion (37%) of the prevention articles were published during those years, with most published prior to 2017. In terms of gender, 52 of the 88 articles enrolled both male and female AYA, 17 studies enrolled females only, 13 studies enrolled males only, and 7 studies included transgender youth (data not shown).
Multi-level Approaches
Altogether, the 88 included articles presented a total of 72 different multi-level theories, with about a quarter of the published manuscripts presenting multiple theories. Specifically, 33 (38%) utilized socio-ecological models (SEMs) or the eco-developmental theory. These multi-level approaches often described the components of Bronfenbrenner’s (i.e., macrosystem, exosystem, mesosystem, microsystem) [109] or McLeroy’s (intrapersonal, interpersonal, organizational, community, and public policy) SEMs [110, 111]. Other articles included sociological and structural theories such as the Theory of Gender and Power and Social Disorganization, as well as adolescent-specific theories such as the Theory of Emerging Adulthood. Other examples of theories this review found include Foucault State Power and Discourse, Family System Theory, and the Disability-Stress-Coping Model. Most authors described the approach as informing their data analysis, and 12 out of the 88 articles described the approach as informing or guiding an intervention.
Discussion
We found 88 articles published between 2010 and May 2020 that fulfilled the criteria for this scoping review, suggesting an opportunity for increased use of multi-level theories and frameworks among researchers in the field of AYA HIV prevention and care and treatment. Most of these articles also focused on AYA HIV prevention, with fewer addressing AYA care and treatment. Most of the included care and treatment literature was published in 2017 and later. This overall lag in HIV care and treatment research may be in part due to the initial focus on advancing treatment options and availability. As treatment has become more widely available, efforts have turned to the behavioral and multi-level aspects of supporting AYAs’ engagement with the care continuum, as reflected in some recent National Institutes for Health requests for applications [112, 113].
This scoping review also highlights a lack of AYA intervention focused research that utilized a named multi-level theory or framework. The view that conducting multi-level interventions is challenging due to its complexity and expense is summarized by Kaufman et al.: “multi-level approaches…are in many ways at odds with contemporary HIV-related policy, which often favors brief, replicable, and easily disseminated interventions” (p. S251) [7]. Such challenges may be amplified when working with AYA whose continued development may result in changing HIV risks and resiliencies across the various levels of a multi-level approach. For example, identity development, puberty, cognitive growth, and age may all lead to greater AYA risk (e.g., alcohol use) as well as resiliencies and protection (e.g., access to clinics/understanding of information). However, given the evolving nature of adolescence, it is critical that we use multi-level theories and frameworks to improve AYA HIV-related health outcomes. Such approaches can be achieved by designing and adapting interventions at selected levels that allow for and are responsive to AYA developmental needs. For example, Denison et al. pilot-tested the “Family Connections” family-based intervention among AYAs, ages 15 to 19 years, living with HIV in Zambia. Based on positive youth development, Family Connections moved beyond individual level factors to engage the family caregivers (interpersonal level) and health care providers (environmental level) [114]. To expand on this pilot study, the team is now conducting a National Institute for Mental Health—funded R01 to examine both the impact of Family Connections on youth achieving an undetectable viral load, and if developmental differences among participants (e.g., cognitive functioning, emotional regulation and impulse control) moderate any impact found. Studies that combine multi-level theory and incorporate developmental factors into intervention testing illustrate how we may strengthen our AYA HIV research to engage and address the needs of AYAs.
Our scoping review findings also highlight the ways researchers creatively drew upon different theories and frameworks to examine multi-level factors within their respective studies. This practice of drawing upon different theoretical perspectives is an important contribution and supports the recommendation of Kaufman et al. to utilize existing theories at various levels until a new theory is needed [7]. In the scoping review, we found that authors sometimes combined individual and/or structural theories with SEMs. This process can help translate SEMs, which tend to be broadly applied, to specific populations and factors, explicitly detailing proposed hypotheses of how change occurs. We recommend researchers continue to combine theories to clearly link and measure multi-level variables and their interactive effects on behavior change.
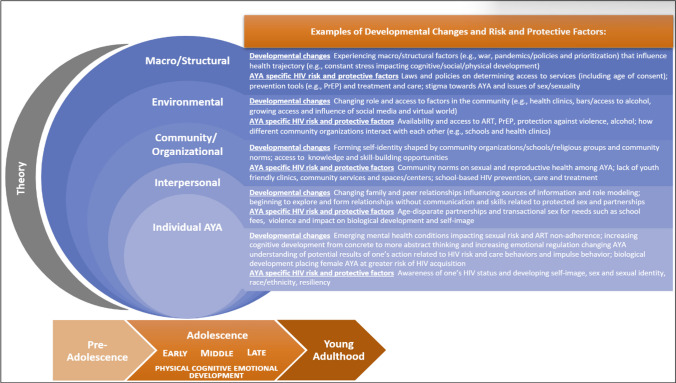
Adapted AYA HIV Multi-level Framework
Given the importance of multi-level theories and frameworks for advancing AYA HIV research, and the lessons learned from this scoping review, the interdisciplinary JHU CFAR AYA SWG adapted the WHO’s Adolescent Health Ecological Model to HIV specifically. In this adapted framework we explicitly emphasize the dynamic and changing nature of adolescence within the context of HIV (Figure 2). The arrow across the bottom underscores the broad developmental stages of adolescence and young adulthood within a life course perspective. To make the framework more parsimonious and accessible, we also collapsed four of the original seven levels. We combined community and organizational levels into one level to group the social norms (e.g., values, networks) and institutions (e.g., schools) that may exist within an AYA’s broader community. We also combined the macro/structural levels that encompass super structural (e.g., war, racism) and structural (e.g., policies, laws) factors. Within each level, we highlight AYA developmental changes and provide examples of the HIV-specific risk and protective factors that may be at play. In the adapted framework, we also remind researchers to use theory, as shown in the grey moon-shaped sliver in the figure, to guide intervention design, measures, and analyses, and to explicitly state how factors across levels are hypothesized to interact and impact AYA HIV outcomes. Overall, the goal of this adapted framework is to provide interdisciplinary teams of AYA HIV researchers with a tool for conceptualizing the developmental changes and the corresponding HIV risk and protective factors they could consider in their interventions and to state the theoretical relationship among these variables guiding their analyses across levels.
Fig. 2.
A tool to support multi-level approaches in AYA HIV research
Adapted from the WHO Adolescent Health Ecological Model (16)
Limitations
There are limitations to the scoping review. First, only published articles in English that had the search terms, such as theoretical framework, in the title/abstract or as a MeSH term, were included. This process may have missed articles that used multi-level theories or frameworks that did not include the terms we used to search. This process also excluded grey literature and any published article in a language other than English, potentially resulting in publication and language biases respectively. Finally, we did not assess the use of multi-level analytic models, interventions, or study designs in the absence of a named theory, or the quality of the research in the included articles.
Conclusions
This scoping review highlights a paucity of published articles that utilized a named multi-level theory or framework, particularly in HIV care and treatment. The scoping review also found that researchers who have used multi-level theories or frameworks have taken creative approaches to integrate theories and/or have relied on socio-ecological models. Use of multi-level approaches by AYA HIV researchers is greatly needed, and we offer an adapted model to facilitate these efforts.
Appendix
See Table 4
Author contributions
All authors substantially contributed to project conception, reviewed and edited the manuscript, gave final approval of the version to be published, and agreed to be accountable for all aspects of this review. JAD, KW, and SD led the scoping review process including conceptualization, abstract and full-text review, data extraction, and writing the manuscript. KMS contributed to full-text review, data extraction and contributed to writing and editing the final draft. AA, RS, MK, SP, EF, KA, LL, and CY contributed to the conceptualization of the study and edited and contributed to the final draft. All authors have read and approved the final manuscript and agreed to be accountable for all aspects of this review. The authors are current or former members of the Johns Hopkins University (JHU) Center for AIDS Research (CFAR) Adolescent and Young Adult (AYA) Scientific Working Group (SWG).
Funding
The authors gratefully acknowledge youth globally who continue to teach and inspire the JHU CFAR AYA SWG. We also acknowledge the technical input and guidance from Claire Twose, a JHU Welch Medical Library Informationist, who contributed substantially to the search strategy and guided the team on Covidence. We also wish to thank Eileen Martin for her editorial skills. This publication resulted (in part) from research supported by the JHU CFAR, an NIH funded program (P30AI094189), which is supported by the following NIH Co-Funding and Participating Institutes and Centers: NIAID, NCI, NICHD, NHLBI, NIDA, NIA, NIGMS, NIDDK, NIMHD. Funding for Julie Denison came from the National Center for Complementary and Integrative Health (5K01AT009049). Funding for Stephanie M. DeLong came from the NIH/NIAID T32AI102623. This article was also made possible (in part) by the support of the American people through the United States Agency for International Development (USAID) under the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR). Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH, USAID, or PEPFAR.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article.
Code availability
Not applicable.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.United Nations. Transforming our world: The 2030 agenda for sustainable development. 2016. https://stg-wedocs.unep.org/bitstream/handle/20.500.11822/11125/unepswiosm1inf7sdg.pdf?sequence=1.
- 2.World Health Organization. HIV/AIDS: framework for action in the WHO African region, 2016–2020. 2017. https://apps.who.int/iris/bitstream/handle/10665/259638/EndAIDS-eng.pdf;sequence=1.
- 3.UNICEF. HIV and AIDS in adolescents. 2021. https://data.unicef.org/topic/adolescents/hiv-aids/.
- 4.UNICEF. Coverage of antiretroviral treatment (ART) among adolecents aged 10–19 living with HIV, 2010–2020. 2021. https://data.unicef.org/topic/hivaids/adolescents-young-people/#.
- 5.Sweat MD, Denison JA. Reducing HIV incidence in developing countries with structural and environmental interventions. AIDS. 1995;9:251–7. [PubMed] [Google Scholar]
- 6.Baral S, Logie CH, Grosso A, Wirtz AL, Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. 2013;13(1):1–8. doi: 10.1186/1471-2458-13-482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaufman MR, Cornish F, Zimmerman RS, Johnson BT. Health behavior change models for HIV prevention and AIDS care: practical recommendations for a multi-level approach. J Acquir Immune Defic Syndr. 2014;66(Suppl 3):S250. doi: 10.1097/QAI.0000000000000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DiClemente RJ, Wingood GM. Expanding the scope of HIV prevention for adolescents: beyond individual-level interventions. J Adolesc Health. 2000;26(6):377–8. doi: 10.1016/S1054-139X(00)00126-9. [DOI] [PubMed] [Google Scholar]
- 9.Bekker L-G, Beyrer C, Quinn TC. Behavioral and biomedical combination strategies for HIV prevention. Cold Spring Harbor Perspect Med. 2012;2(8):a007435. doi: 10.1101/cshperspect.a007435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Auerbach JD, Coates TJ. HIV prevention research: accomplishments and challenges for the third decade of AIDS. Am J Public Health. 2000;90(7):1029. doi: 10.2105/AJPH.90.7.1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coates TJ, Richter L, Caceres C. Behavioural strategies to reduce HIV transmission: how to make them work better. The Lancet. 2008;372(9639):669–84. doi: 10.1016/S0140-6736(08)60886-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kerrigan D, Moreno L, Rosario S, Gomez B, Jerez H, Barrington C, et al. Environmental–structural interventions to reduce HIV/STI risk among female sex workers in the Dominican Republic. Am J Public Health. 2006;96(1):120–5. doi: 10.2105/AJPH.2004.042200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lippman SA, Chinaglia M, Donini AA, Diaz J, Reingold A, Kerrigan DL. Findings from encontros: a multi-level STI/HIV intervention to increase condom use, reduce STI, and change the social environment among sex workers in Brazil. Sex Transm Dis. 2012;39(3):209. doi: 10.1097/OLQ.0b013e31823b1937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bronfenbrenner U. The ecology of human development: experiments by nature and design. Cambridge: Harvard university press; 1979. [Google Scholar]
- 15.Blum RW, McNeely C, Nonnemaker J. Vulnerability, risk, and protection. J Adolesc Health. 2002;31(1):28–39. doi: 10.1016/S1054-139X(02)00411-1. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization. Health for the world’s adolescents: a second chance in the second decade. 2014. https://apps.who.int/iris/bitstream/handle/10665/112750/WHO_FWC_MCA_14.05_eng.pdf.
- 17.Patton GC, Sawyer SM, Santelli JS, Ross DA, Afifi R, Allen NB, et al. Our future: a Lancet commission on adolescent health and wellbeing. The Lancet. 2016;387(10036):2423–78. doi: 10.1016/S0140-6736(16)00579-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Veritas Health Innovation. Covidence systematic review software Melbourne Australia. https://www.covidence.org.
- 19.UNAIDS. 90-90-90. Ambitious treatment target to help end the AIDS epidemic: UNAIDS. 2014. https://www.unaids.org/sites/default/files/media_asset/90-90-90_en.pdf.
- 20.UNAIDS. Understanding fast-track accelerating action to end the AIDS epidemic by 2030. 2015. https://www.unaids.org/sites/default/files/media_asset/201506_JC2743_Understanding_FastTrack_en.pdf.
- 21.Babalola S. Factors associated with HIV Infection among sexually experienced adolescents in Africa: a pooled data analysis. Afr J AIDS Res. 2011;10(4):403–14. doi: 10.2989/16085906.2011.646655. [DOI] [PubMed] [Google Scholar]
- 22.Bauermeister JA, Zimmerman MA, Caldwell CH. Neighborhood disadvantage and changes in condom use among African American adolescents. J Urb Health. 2011;88(1):66–83. doi: 10.1007/s11524-010-9506-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brennan J, Kuhns LM, Johnson AK, Belzer M, Wilson EC, Garofalo R, et al. Syndemic theory and HIV-related risk among young transgender women: the role of multiple, co-occurring health problems and social marginalization. Am J Public Health. 2012;102(9):1751–7. doi: 10.2105/AJPH.2011.300433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Burton K, Ayangeakaa S, Kerr J, Kershner S, Maticka-Tyndale E. Examining sexual concurrency and number of partners among African, Caribbean, and black women using the social ecological model: results from the ACBY study. Can J Hum Sexuality. 2019;28(1):46–56. doi: 10.3138/cjhs.2018-0033. [DOI] [Google Scholar]
- 25.Carlson M, Brennan RT, Earls F. Enhancing adolescent self-efficacy and collective efficacy through public engagement around HIV/AIDS competence: a multilevel, cluster randomized-controlled trial. Soc Sci Med. 2012;75(6):1078–87. doi: 10.1016/j.socscimed.2012.04.035. [DOI] [PubMed] [Google Scholar]
- 26.Cheruiyot C, Magu D, Mburugu P, Sagwe D. Uptake and utilization of institutional voluntary HIV testing and counseling services among students aged 18–24 in Kenya’s public universities. Afr Health Sci. 2019;19(4):3190–9. doi: 10.4314/ahs.v19i4.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cluver L, Orkin M, Boyes ME, Sherr L, Makasi D, Nikelo J. Pathways from parental AIDS to child psychological, educational and sexual risk: developing an empirically-based interactive theoretical model. Soc Sci Med. 2013;87:185–93. doi: 10.1016/j.socscimed.2013.03.028. [DOI] [PubMed] [Google Scholar]
- 28.Córdova D, Schwartz SJ, Unger JB, Baezconde-Garbanati L, Villamar JA, Soto DW, et al. A longitudinal test of the parent–adolescent family functioning discrepancy hypothesis: a trend toward increased HIV risk behaviors among immigrant hispanic adolescents. J Youth Adolesc. 2016;45(10):2164–77. doi: 10.1007/s10964-016-0500-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Folayan MO, Harrison A, Brown B, Odetoyinbo M, Stockman JK, Ajuwon AJ, et al. Associations between forced sexual initiation, HIV status, sexual risk behavior, life stressors, and coping strategies among adolescents in Nigeria. PLoS ONE. 2016;11(5):e0155210. doi: 10.1371/journal.pone.0155210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Halkitis PN, Figueroa RP. Sociodemographic characteristics explain differences in unprotected sexual behavior among young HIV-negative gay, bisexual, and other YMSM in New York City. AIDS Patient Care STDs. 2013;27(3):181–90. doi: 10.1089/apc.2012.0415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Halkitis PN, Moeller RW, Siconolfi DE, Storholm ED, Solomon TM, Bub KL. Measurement model exploring a syndemic in emerging adult gay and bisexual men. AIDS Behav. 2013;17(2):662–73. doi: 10.1007/s10461-012-0273-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huebner DM, Kegeles SM, Rebchook GM, Peterson JL, Neilands TB, Johnson WD, et al. Social oppression, psychological vulnerability, and unprotected intercourse among young Black men who have sex with men. Health Psychol. 2014;33(12):1568. doi: 10.1037/hea0000031. [DOI] [PubMed] [Google Scholar]
- 33.James TG, Ryan SJ. HIV knowledge mediates the relationship between HIV testing history and stigma in college students. J Am Coll Health. 2018;66(7):561–9. doi: 10.1080/07448481.2018.1432623. [DOI] [PubMed] [Google Scholar]
- 34.Johns MM, Bauermeister JA, Zimmerman MA. Individual and neighborhood correlates of HIV testing among African American youth transitioning from adolescence into young adulthood. AIDS Educ Prev. 2010;22(6):509–22. doi: 10.1521/aeap.2010.22.6.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Karamagi E, Sensalire S, Nabwire J, Byabagambi J, Awio AO, Aluma G, et al. Quality improvement as a framework for behavior change interventions in HIV-predisposed communities: a case of adolescent girls and young women in northern Uganda. AIDS Res Therapy. 2018;15(1):1–11. doi: 10.1186/s12981-018-0190-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Maticka-Tyndale E, Tenkorang EY. A multi-level model of condom use among male and female upper primary school students in Nyanza, Kenya. Soc Sci Med. 2010;71(3):616–25. doi: 10.1016/j.socscimed.2010.03.049. [DOI] [PubMed] [Google Scholar]
- 37.Mmari KN, Kaggwa E, Wagman J, Gray R, Wawer M, Nalugoda F. Risk and protective correlates of young women’s first sexual experiences in Rakai, Uganda. Int Perspec Sex Reprod Health. 2019;39:153–62. doi: 10.1363/3915313. [DOI] [PubMed] [Google Scholar]
- 38.Moodley CG. Perceptions of South African emerging adult FET College students on sexual practices in relation to religion. J Relig Health. 2017;56(5):1515–36. doi: 10.1007/s10943-016-0312-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Njoroge KM, Olsson P, Pertet AM, Ahlberg BM. Voices unheard: youth and sexuality in the wake of HIV prevention in Kenya. Sex Reproductive Healthc. 2010;1(4):143–8. doi: 10.1016/j.srhc.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 40.Pilgrim NA, Ahmed S, Gray RH, Sekasanvu J, Lutalo T, Nalugoda F, et al. Multiple sexual partnerships among female adolescents in rural Uganda: the effects of family structure and school attendance. Int J Adolesc Med Health. 2015;27(3):319–28. doi: 10.1515/ijamh-2014-0032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Placek CD, Nishimura H, Hudanick N, Stephens D, Madhivanan P. Reframing HIV stigma and fear. Hum Nat. 2019;30(1):1–22. doi: 10.1007/s12110-018-09335-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Prado G, Huang S, Maldonado-Molina M, Bandiera F, Schwartz SJ, de la Vega P, et al. An empirical test of ecodevelopmental theory in predicting HIV risk behaviors among hispanic youth. Health Educ Behav. 2010;37(1):97–114. doi: 10.1177/1090198109349218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Prado G, Pantin H. Reducing substance use and HIV health disparities among hispanic youth in the USA: the Familias Unidas program of research. Psychosocial Intervention. 2011;20(1):63–73. doi: 10.5093/in2011v20n1a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Robertson L, Gregson S, Garnett GP. Sexual risk among orphaned adolescents: is country-level HIV prevalence an important factor? AIDS Care. 2010;22(8):927–38. doi: 10.1080/09540121003758622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ruiseñor-Escudero H, Grosso A, Ketende S, Pitche V, Simplice A, Tchalla J, et al. Using a social ecological framework to characterize the correlates of HIV among men who have sex with men in Lomé, Togo. AIDS Care. 2017;29(9):1169–77. doi: 10.1080/09540121.2017.1280122. [DOI] [PubMed] [Google Scholar]
- 46.Salud MC, Marshak HH, Natto ZS, Montgomery S. Exploring HIV-testing intentions in young Asian/Pacific Islander (API) women as it relates to acculturation, theory of gender and power (TGP), and the AIDS risk reduction model (ARRM) AIDS Care. 2014;26(5):642–7. doi: 10.1080/09540121.2013.841836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stock ML, Gibbons FX, Peterson LM, Gerrard M. The effects of racial discrimination on the HIV-risk cognitions and behaviors of black adolescents and young adults. Health Psychol. 2013;32(5):543. doi: 10.1037/a0028815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tenkorang EY, Maticka-Tyndale E. Individual-and community-level influences on the timing of sexual debut among youth in Nyanza, Kenya. Int Perspect Sex Reproductive Health. 2014;40(2):68–78. doi: 10.1363/4006814. [DOI] [PubMed] [Google Scholar]
- 49.Underwood C, Schwandt HM. Community support and adolescent girls’ vulnerability to HIV/AIDS: evidence from Botswana, Malawi, and Mozambique. Int Q Community Health Educ. 2015;35(4):317–34. doi: 10.1177/0272684X15592762. [DOI] [PubMed] [Google Scholar]
- 50.Waldrop-Valverde DG, Davis TL, Sales JM, Rose ES, Wingood GM, DiClemente RJ. Sexual concurrency among young African American women. Psychol Health Med. 2013;18(6):676–86. doi: 10.1080/13548506.2013.764462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bird JD, LaSala MC, Hidalgo MA, Kuhns LM, Garofalo R. I had to go to the streets to get love: pathways from parental rejection to HIV risk among young gay and bisexual men. J Homosex. 2017;64(3):321–42. doi: 10.1080/00918369.2016.1179039. [DOI] [PubMed] [Google Scholar]
- 52.Casale M, Rogan M, Hynie M, Flicker S, Nixon S, Rubincam C. Gendered perceptions of HIV risk among young women and men in a high-HIV-prevalence setting. Afr J AIDS Res. 2011;10(sup1):301–10. doi: 10.2989/16085906.2011.637728. [DOI] [PubMed] [Google Scholar]
- 53.Conn C. Young African women must have empowering and receptive social environments for HIV prevention. AIDS Care. 2013;25(3):273–80. doi: 10.1080/09540121.2012.712659. [DOI] [PubMed] [Google Scholar]
- 54.Darlington K-A, Basta T, Obregon R. Cross-generational relationships in rural Jamaica. Vulnerable Child Youth Stud. 2012;7(2):128–38. doi: 10.1080/17450128.2011.647729. [DOI] [Google Scholar]
- 55.Dyson YD, Mobley Y, Harris G, Randolph SD. Using the social-ecological model of HIV prevention to explore HIV testing behaviors of young Black college women. J Assoc Nurses AIDS Care. 2018;29(1):53–9. doi: 10.1016/j.jana.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 56.Enah C, Moneyham L, Vance DE, Gakumo CA, Chandler M. Make it like the real world: adolescents’ recommendations for the design of a digital HIV prevention game. J HIV/AIDS Social Serv. 2014;13(2):163–78. doi: 10.1080/15381501.2012.749821. [DOI] [Google Scholar]
- 57.Harper GW, Riplinger AJ, Neubauer LC, Murphy AG, Velcoff J, Bangi AK. Ecological factors influencing HIV sexual risk and resilience among young people in rural Kenya: implications for prevention. Health Educ Res. 2014;29(1):131–46. doi: 10.1093/her/cyt081. [DOI] [PubMed] [Google Scholar]
- 58.Hudson AL. Where do youth in foster care receive information about preventing unplanned pregnancy and sexually transmitted infections? J Pediatr Nurs. 2012;27(5):443–50. doi: 10.1016/j.pedn.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 59.Katherine Hutchinson M, Kahwa E, Waldron N, Hepburn Brown C, Hamilton PI, Hewitt HH, et al. Jamaican mothers’ influences of adolescent girls’ sexual beliefs and behaviors. J Nurs Scholarsh. 2012;44(1):27–35. doi: 10.1111/j.1547-5069.2011.01431.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Katz IT, Ybarra ML, Wyatt MA, Kiwanuka JP, Bangsberg DR, Ware NC. Socio-cultural and economic antecedents of adolescent sexual decision-making and HIV-risk in rural Uganda. AIDS Care. 2013;25(2):258–64. doi: 10.1080/09540121.2012.701718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Khan S, Lorway R, Chevrier C, Dutta S, Ramanaik S, Roy A, et al. Dutiful daughters: HIV/AIDS, moral pragmatics, female citizenship and structural violence among devadasis in northern Karnataka, India. Glob Public Health. 2018;13(8):1065–80. doi: 10.1080/17441692.2017.1280070. [DOI] [PubMed] [Google Scholar]
- 62.Kubicek K, McNeeley M, Collins S. Same-sex relationship in a straight world individual and societal influences on power and control in young men’s relationships. J Interpers Violence. 2015;30(1):83–109. doi: 10.1177/0886260514532527. [DOI] [PubMed] [Google Scholar]
- 63.Lyons T, Johnson AK, Garofalo R. What could have been different: a qualitative study of syndemic theory and HIV prevention among young men who have sex with men. J HIV/AIDS Social Serv. 2013;12(3–4):368–83. doi: 10.1080/15381501.2013.816211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Newman PA, Roungprakhon S, Tepjan S. A social ecology of rectal microbicide acceptability among young men who have sex with men and transgender women in Thailand. J Int AIDS Soc. 2013;16(1):18476. doi: 10.7448/IAS.16.1.18476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Nwokocha E, Isiugo-Abanihe I, Omololu F, Isiugo-Abanihe U, Udegbe B. Implementation of family life and HIV/AIDS education in Nigerian schools: a qualitative study on scope, delivery and challenges. Afr J Reprod Health. 2015;19(2):63–78. [PubMed] [Google Scholar]
- 66.Rahangdale L, Banandur P, Sreenivas A, Turan JM, Washington R, Cohen CR. Stigma as experienced by women accessing prevention of parent-to-child transmission of HIV services in Karnataka, India. AIDS Care. 2010;22(7):836–42. doi: 10.1080/09540120903499212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Richardson J, Robillard A. The least of these: chronic exposure to violence and HIV Risk behaviors among African American Male Violent Youth offenders detained in an adult jail. J Black Psychol. 2013;39(1):28–62. doi: 10.1177/0095798412447645. [DOI] [Google Scholar]
- 68.Stevens R, Bernadini S, Jemmott JB. Social environment and sexual risk-taking among gay and transgender African American youth. Cult Health Sex. 2013;15(10):1148–61. doi: 10.1080/13691058.2013.809608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Burch WJ, Hart GJ, Lim SH. A qualitative study of young men who have sex with men and multilevel factors related to HIV risks in Malaysia. AIDS Educ Prev. 2018;30(2):85–95. doi: 10.1521/aeap.2018.30.2.85. [DOI] [PubMed] [Google Scholar]
- 70.Cho H, Deming ME, Park J-H, Iritani B. Gender differences in HIV/HSV-2: evidence from a school support randomized controlled trial among orphaned adolescents in Kenya. AIDS Behav. 2019;23:2396–406. doi: 10.1007/s10461-019-02518-4. [DOI] [PubMed] [Google Scholar]
- 71.Cordova D, Munoz-Velazquez J, Mendoza Lua F, Fessler K, Warner S, Delva J, et al. Pilot study of a multilevel mobile health app for substance use, sexual risk behaviors, and testing for sexually transmitted Infections and HIV among youth: Randomized controlled trial. JMIR mHealth and uHealth. 2020;8(3):e16251. doi: 10.2196/16251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Coyle KK, Anderson P, Franks HM, Walker JD, Glassman JR. You-Me-Us: results of a cluster randomized trial of a healthy relationships approach to sexual risk reduction. J Prim Prev. 2019;40:607–29. doi: 10.1007/s10935-019-00569-w. [DOI] [PubMed] [Google Scholar]
- 73.DeAtley T, Mathews C, Stein DJ, Grelotti D, Brown LK, Giovenco D, et al. Risk and protective factors for whoonga use among adolescents in South Africa. Addict Behav Rep. 2020;11:100277. doi: 10.1016/j.abrep.2020.100277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Eisenberg ME, Hannan PJ, Lust KA, Lechner KE, Garcia C, Frerich EA. Sexual health resources at Minnesota colleges: associations with students’ sexual health behaviors. Perspect Sex Reprod Health. 2013;45(3):132–8. doi: 10.1363/4513213. [DOI] [PubMed] [Google Scholar]
- 75.Li Y-H, Mgbere O, Abughosh S, Chen H, Cuccaro P, Smesny A, et al. Assessment of sexually transmitted disease/HIV risk among young African Americans: comparison of self-perceived and epidemiological risks utilizing ecodevelopmental theory. HIV/AIDS Res Palliative Care. 2019;11:31–44. doi: 10.2147/HIV.S189482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mathur S, Pilgrim N, Patel SK, Okal J, Mwapasa V, Chipeta E, et al. HIV vulnerability among adolescent girls and young women: a multi-country latent class analysis approach. Int J Public Health. 2020;65:399–411. doi: 10.1007/s00038-020-01350-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mustanski B, Morgan E, D’Aquila R, Birkett M, Janulis P, Newcomb ME. Individual and network factors associated with racial disparities in HIV among young men who have sex with men: results from the RADAR cohort study. J Acquir Immune Defic Syndr. 2019;80(1):24. doi: 10.1097/QAI.0000000000001886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Nakazwe C, Michelo C, Fylkesnes M, Sandoy I. An association between HIV prevalence and socioeconomic factors among young people in Zambia: do neighbourhood contextual effects play a role. In: Nakazwe C, Michelo C, Fylkesnes M, Sandoy I, editors. Transactions of the royal society of tropical medicine and hygiene. England: Oxford Univ Press; 2019. [Google Scholar]
- 79.Schwandt HM, Underwood C. Making a difference in adult–child relationships: evidence from an adult–child communication intervention in Botswana, Malawi, and Mozambique. J Adolesc. 2013;36(6):1177–86. doi: 10.1016/j.adolescence.2013.09.005. [DOI] [PubMed] [Google Scholar]
- 80.Ssewamala FM, Neilands TB, Waldfogel J, Ismayilova L. The impact of a comprehensive microfinance intervention on depression levels of AIDS-orphaned children in Uganda. J Adolesc Health. 2012;50(4):346–52. doi: 10.1016/j.jadohealth.2011.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Tozan Y, Sun S, Capasso A, Shu-Huah Wang J, Neilands TB, Bahar OS, et al. Evaluation of a savings-led family-based economic empowerment intervention for AIDS-affected adolescents in Uganda: a four-year follow-up on efficacy and cost-effectiveness. PLoS ONE. 2019;14(12):e0226809. doi: 10.1371/journal.pone.0226809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tomita A, Vandormael AM, Bärnighausen T, de Oliveira T, Tanser F. Social disequilibrium and the risk of HIV acquisition: a multilevel study in rural KwaZulu-Natal Province, South Africa. J Acquir Immune Defic Syndr. 2017;75(2):164. doi: 10.1097/QAI.0000000000001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tyler KA, Handema R, Schmitz RM, Phiri F, Kuyper KS, Wood C. Multi-level risk and protective factors for substance use among Zambian street youth. Subst Use Misuse. 2016;51(7):922–31. doi: 10.3109/10826084.2016.1156702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ward-Peterson M, Fennie K, Baird S, Coxe S, Trepka MJ, Madhivanan P. Association between HIV awareness factors, health facility characteristics and risky sexual behaviour among young women in Zomba district, Malawi. J Biosoc Sci. 2018;50(6):853–67. doi: 10.1017/S0021932017000694. [DOI] [PubMed] [Google Scholar]
- 85.Logie CH, Wang Y, Lacombe-Duncan A, Jones N, Ahmed U, Levermore K, et al. Factors associated with sex work involvement among transgender women in Jamaica: a cross‐sectional study. J Int AIDS Soc. 2017;20(1):21422. doi: 10.7448/IAS.20.01/21422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Underwood C, Skinner J, Osman N, Schwandt H. Structural determinants of adolescent girls’ vulnerability to HIV: views from community members in Botswana, Malawi, and Mozambique. Soc Sci Med. 2011;73(2):343–50. doi: 10.1016/j.socscimed.2011.05.044. [DOI] [PubMed] [Google Scholar]
- 87.Arrington-Sanders R, Morgan A, Oidtman J, Gomez MC, Ogunbajo A, Trent M, et al. Context of first same‐sex condom use and nonuse in Young Black Gay and Bisexual males. J Res Adolescence. 2016;26(4):1009–21. doi: 10.1111/jora.12255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cordova D, Mendoza Lua F, Muñoz-Velázquez J, Street K, Bauermeister JA, Fessler K, et al. A multilevel mHealth drug abuse and STI/HIV preventive intervention for clinic settings in the United States: a feasibility and acceptability study. PLoS ONE. 2019;14(8):e0221508. doi: 10.1371/journal.pone.0221508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Logie CH, Abramovich A, Schott N, Levermore K, Jones N. Navigating stigma, survival, and sex in contexts of social inequity among young transgender women and sexually diverse men in Kingston. Jamaica Reproductive Health Matters. 2018;26(54):72–83. doi: 10.1080/09688080.2018.1538760. [DOI] [PubMed] [Google Scholar]
- 90.Miller RL, Strzyzykowski T, Lee KS, Chiaramonte D, Acevedo-Polakovich I, Spring H, et al. Structural effects on HIV risk among youth: A multi-level analysis. AIDS and Behavior. 2018;22:3451–67. [DOI] [PMC free article] [PubMed]
- 91.Jeffries IVWL, Gelaude DJ, Torrone EA, Gasiorowicz M, Oster AM, Spikes PS, Jr, et al. Unhealthy environments, unhealthy consequences: experienced homonegativity and HIV Infection risk among young men who have sex with men. Glob Public Health. 2017;12(1):116–29. doi: 10.1080/17441692.2015.1062120. [DOI] [PubMed] [Google Scholar]
- 92.Mutumba M, Bauermeister JA, Harper GW, Musiime V, Lepkowski J, Resnicow K, et al. Psychological distress among Ugandan adolescents living with HIV: examining stressors and the buffering role of general and religious coping strategies. Glob Public Health. 2017;12(12):1479–91. doi: 10.1080/17441692.2016.1170871. [DOI] [PubMed] [Google Scholar]
- 93.Naar-King S, Montepiedra G, Garvie P, Kammerer B, Malee K, Sirois PA, et al. Social ecological predictors of longitudinal HIV treatment adherence in youth with perinatally acquired HIV. J Pediatr Psychol. 2013;38(6):664–74. doi: 10.1093/jpepsy/jst017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Pantelic M, Boyes M, Cluver L, Meinck F. HIV, violence, blame and shame: pathways of risk to internalized HIV stigma among South African adolescents living with HIV. J Int AIDS Soc. 2017;20(1):21771. doi: 10.7448/IAS.20.1.21771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ashaba S, Cooper-Vince CE, Vořechovská D, Rukundo GZ, Maling S, Akena D, et al. Community beliefs, HIV stigma, and depression among adolescents living with HIV in rural Uganda. Afr J AIDS Res. 2019;18(3):169–80. doi: 10.2989/16085906.2019.1637912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.van der Crowley T, Skinner D. Adolescent HIV self-management: lived experiences of adolescents, caregivers, and health care workers in a South African context. J Assoc Nurses AIDS Care. 2019;30(4):e7–e19. doi: 10.1097/JNC.0000000000000098. [DOI] [PubMed] [Google Scholar]
- 97.Galea JT, Wong M, Muñoz M, Valle E, Leon SR, Díaz Perez D, et al. Barriers and facilitators to antiretroviral therapy adherence among Peruvian adolescents living with HIV: a qualitative study. PLoS ONE. 2018;13(2):e0192791. doi: 10.1371/journal.pone.0192791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Harper GW, Lemos D, Mutumba M, Kumar M, Gikuni AW, Mustich I, et al. Resilience processes among youth newly diagnosed with HIV who live in urban informal settlements in Kenya: implications for intervention. J HIV/AIDS Social Serv. 2019;18(4):329–46. doi: 10.1080/15381501.2019.1657546. [DOI] [Google Scholar]
- 99.Mutumba M, Musiime V, Mugerwa H, Nakyambadde H, Gautam A, Matama C, et al. Perceptions of HIV self-management roles and challenges in adolescents, caregivers, and health care providers. J Assoc Nurses AIDS Care. 2019;30(4):415–27. doi: 10.1097/JNC.0000000000000011. [DOI] [PubMed] [Google Scholar]
- 100.Skovdal M, Ogutu VO. Coping with hardship through friendship: the importance of peer social capital among children affected by HIV in Kenya. Afr J AIDS Res. 2012;11(3):241–50. doi: 10.2989/16085906.2012.734983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wolf HT, Davidoff K, Auerswald CL, Halpern-Felsher BL, Bukusi EA, Lyon M, et al. Health care experiences of youth living with HIV who were lost to follow-up in Western Kenya. J Assoc Nurses AIDS Care. 2019;30(5):539–47. doi: 10.1097/JNC.0000000000000044. [DOI] [PubMed] [Google Scholar]
- 102.Wong WC, Holroyd E, Miu HY, Wong CS, Zhao Y, Zhang J. Secrets, shame and guilt: HIV disclosure in rural Chinese families from the perspective of caregivers. Vulnerable Child Youth Stud. 2017;12(4):292–303. doi: 10.1080/17450128.2017.1344343. [DOI] [Google Scholar]
- 103.Rutakumwa R, Zalwango F, Richards E, Seeley J. Exploring the care relationship between grandparents/older carers and children infected with HIV in south-western Uganda: implications for care for both the children and their older carers. Int J Environ Res Public Health. 2015;12(2):2120–34. doi: 10.3390/ijerph120202120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Nestadt DF, Saisaengjan C, McKay MM, Bunupuradah T, Pardo G, Lakhonpon S, et al. CHAMP + Thailand: pilot randomized control trial of a family-based psychosocial intervention for perinatally HIV-infected early adolescents. AIDS Patient Care STDs. 2019;33(5):227–36. doi: 10.1089/apc.2019.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.McKay MM, Alicea S, Elwyn L, McClain ZR, Parker G, Small LA, et al. The development and implementation of theory-driven programs capable of addressing poverty-impacted children’s health, mental health, and prevention needs: CHAMP and CHAMP+, evidence-informed, family-based interventions to address HIV risk and care. J Clin Child Adolesc Psychol. 2014;43(3):428–41. doi: 10.1080/15374416.2014.893519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Vu L, Burnett-Zieman B, Banura C, Okal J, Elang M, Ampwera R, et al. Increasing uptake of HIV, sexually transmitted infection, and family planning services, and reducing HIV-related risk behaviors among youth living with HIV in Uganda. J Adolesc Health. 2017;60(2):22–S8. doi: 10.1016/j.jadohealth.2016.09.007. [DOI] [PubMed] [Google Scholar]
- 107.Li L, Liang L-J, Lin C, Lan C-W, Ji G, Xiao Y. Changes in behavioral outcomes among children affected by HIV: results of a randomized controlled trial in China. J Health Psychol. 2019;24(11):1581–94. doi: 10.1177/1359105317746479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Li X, Harrison SE, Fairchild AJ, Chi P, Zhao J, Zhao G. A randomized controlled trial of a resilience-based intervention on psychosocial well-being of children affected by HIV/AIDS: effects at 6-and 12-month follow-up. Soc Sci Med. 2017;190:256–64. doi: 10.1016/j.socscimed.2017.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Bronfenbrenner U. Toward an experimental ecology of human development. Am Psychol. 1977;32(7):513. doi: 10.1037/0003-066X.32.7.513. [DOI] [Google Scholar]
- 110.McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351–77. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 111.Stokols D. Translating social ecological theory into guidelines for community health promotion. Am J Health Promotion. 1996;10(4):282–98. doi: 10.4278/0890-1171-10.4.282. [DOI] [PubMed] [Google Scholar]
- 112.NIH. RFA-HD-23-020. Adolescent medicine trials network for HIV/AIDS interventions (ATN) Scientific Leadership Center (UM2 Clinical Trial Optional). 2021. https://grants.nih.gov/grants/guide/rfa-files/RFA-HD-23-020.html.
- 113.NIH. RFA-MD-22-001. Innovative multi-level approaches and strategies to prevent, test and treat HIV in primary care settings in health disparity populations in geographic hot spots in the United States (R01 - Clinical Trial Required). 2021. https://grants.nih.gov/grants/guide/rfa-files/RFA-MD-22-001.html.
- 114.Denison JA, Packer C, Nyambe N, Hershow RB, Caldas S, Miti S, et al. Family connections randomized controlled trial: assessing the feasibility and acceptability of an intervention with adolescents living with HIV and their caregivers in Ndola, Zambia. AIDS Care. 2021;34:1–10. doi: 10.1080/09540121.2021.1902935. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article.
Not applicable.