Abstract
Objective: This study aims to evaluate the clinical efficacy and short-term prognosis of using flexible cystoscopy with percutaneous nephrolithotomy to treat complex renal stones. Methods: A retrospective analysis was conducted on patients with complex kidney stones treated at Gansu Provincial Hospital of TCM and Lanzhou City No. 2 People’s Hospital from July 2019 to July 2022. The study divided the patients into a control group (n=95), who underwent percutaneous nephrolithotomy alone, and an observation group (n=109), who received additional holmium laser lithotripsy and cystoscopy. We compared stone clearance rates at 5 days and 1 month post-surgery, analyzed patient prognosis over a year based on stone recurrence, and assessed risk factors through logistic regression. Perioperative data, changes in renal function indiex 3 days post-surgery, and complication rates were also evaluated. Results: The observation group exhibited a significantly higher stone clearance rate at 5 days post-surgery (P=0.002) compared to the control group, although no significant difference was observed at 1 month (P=0.823). The operative time was significantly shorter (P<0.001), and postoperative levels of BUA, Cys-c, and β2-BMG were lower (P<0.05) in the observation group. Additionally, treatment regimen, BMI, and STONE score were influencing factors for stone recurrence within 1 year. Conclusion: Flexible cystoscopy combined with percutaneous nephrolithotomy offers superior short-term outcomes in the treatment of complex renal stones, including enhanced stone clearance, reduced operative time, and minimized renal function impairment shortly after surgery. Moreover, treatment approach, BMI, and STONE score play pivotal roles in predicting stone recurrence.
Keywords: Flexible cystoscopy, percutaneous nephrolithotomy, complex kidney stones, clinical efficacy, short-term prognosis
Introduction
Urologic stones are a significant global health concern, with a prevalence ranging from 7% to 13% in North America, 5% to 9% in Europe, and 1% to 5% in Asia, as reported in epidemiological studies [1,2]. These differences highlight the influence of lifestyle, dietary habits, and genetic predisposition across different populations. Specifically, the rising incidence of kidney stones is closely linked to factors such as population growth, increasing rates of obesity, and diabetes mellitus [3]. Notably, in China, the prevalence rate stands at approximately 6.4%, with a discernible pattern of higher occurrence rates in the southern regions, rural areas, among males, and individuals with a familial history [4]. These demographic and geographical variations underscore the necessity for region-specific research, especially in Asia and Africa, to elucidate the intricate dynamics of stone prevalence and risk. In the realm of urologic stones, complex renal stones represent a particularly challenging subset. These stones are characterized by attributes that complicate standard treatment protocols, necessitating more advanced and nuanced surgical intervention. Specifically, complex renal stones are delineated by their considerable size (often exceeding 2 cm), problematic locations such as lower pole stones or stones within anatomically abnormal kidneys, resistant composition (e.g., cystine or brushite stones), or the presence of multiple calculi. The complexity introduced by these characteristics is not merely a matter of physical attributes but significantly impacts treatment outcome, raising the likelihood of failure and recurrence [5,6]. This complexity underscores the imperative for innovative surgical techniques tailored to effectively manage and mitigate the unique challenges posed by complex renal stones.
The primary treatment for complex renal stones is surgical, complemented by non-surgical approaches like dietary modification, medications for stone dissolution, and extracorporeal shock wave lithotripsy [7-9]. Minimally invasive surgery, increasingly favored over traditional open surgery, includes percutaneous nephrolithotomy (PCNL) [10], retrograde intrarenal surgery [11], laparoscopic lithotripsy, and multi-scope combined surgery [12]. While laparoscopic lithotripsy offers a high stone clearance rate with few complications, its complexity and duration often discourage its preference. Moreover, despite improving stone clearance rates, the use of multiple channels in lithotripsy raises the risk of renal parenchymal injury and associated complications due to the difficulty in clearing stones through a single channel [13]. The introduction of flexible cystoscopy offers a precise method for locating and addressing stones in areas of the kidney that are traditionally difficult to reach. Its flexibility enables access to regions that pose challenges for conventional rigid endoscopy, facilitating the removal of residual stones. However, the combined use of the flexible cystoscopy with PCNL presents its own set of challenges, particularly in navigating areas that are inaccessible with rigid scopes alone [10]. Despite these challenges, this combination is proposed as a supplementary single surgical option that could improve prognostic outcome by promoting the clearance of residual stones. Currently, there is a scarcity of research on the combined application of PCNL and flexible cystoscopy, highlighting the need for further investigation into its efficacy and procedural optimization.
This study evaluated the efficacy and short-term outcome of integrating flexible cystoscopy with PCNL for complex renal stone treatment. The focus is on assessing the combined approach’s ability to enhance stone clearance, reduce renal damage, and decrease complications. Its innovation lies in merging two minimally invasive techniques to overcome limitations of conventional surgery by using flexible cystoscopy to access difficult renal areas, thereby improving clearance rates and reducing the need for multichannel procedures.
Methods and data
Sample collection
Data of patients diagnosed with complex kidney stones and admitted to the Department of Urology at Gansu Provincial Hospital of TCM and Lanzhou City No. 2 People’s Hospital between July 2019 and July 2022 were retrospectively analyzed. This study was conducted with the approval of the medical ethics committee of Gansu Provincial Hospital of TCM.
Inclusion exclusion criteria
Inclusion criteria: (1) Patients with complex kidney stones diagnosed according to the Diagnostic and Therapeutic Guidelines for Urologic Diseases, confirmed by urologic imaging such as intravenous pyelography [14]; (2) Patients with an American Society of Anesthesiologists (ASA) classification between I and III; (3) Patients experiencing their first occurrence of renal stone symptoms; (4) Patients with comprehensive clinical records; (5) Patients who underwent PCNL or a combination of PCNL with flexible cystoscopy.
Exclusion criteria: (1) Individuals with abnormal coagulation function; (2) Patients with concurrent severe hydronephrosis and infection; (3) Those with a documented history of pelvic trauma; (4) Patients with malignant tumors.
Patient screening
Based on the inclusion criteria, we initially screened 258 cases. After applying the exclusion criteria, 204 cases qualified for the study. Patient surgical programs were sourced from medical records. The included patients were categorized into two groups: a control group (n=95) underwent PCNL, and an observation group (n=109) received additional treatment of holmium laser lithotripsy and cystoscopy.
Surgical program
The surgeries were conducted under general anesthesia. The combined treatment team employed both PCNL and flexible cystoscopy. The process began by placing a 5F ureteral stent on the affected side to facilitate artificial hydronephrosis. After the patient was positioned prone with an elevated renal area, water was injected through the stent to induce hydronephrosis. Ultrasound guided the puncture into the renal calyx, confirmed when fluid emerged from the puncture needle. Following the removal of the puncture needle, an ultra-smooth guidewire was inserted. Progressive dilation was achieved using various sizes of stripping dilatation sheaths, culminating in positioning a 20F dilatation sheath for stone extraction. The holmium laser fragmented the stones through the nephroscope, while perfusion pump adjustments helped dislodge them. Each renal calyx was examined for residual stones. If any were unreachable by the nephroscope, they were addressed with an Olympus CYF-V2 cystoscope. Following confirmation of no remaining stones, a double J-tube and nephrostomy tube were inserted. The PCNL team followed a similar procedure but without the cystoscopy, and additional operative channels were established as needed for complete stone removal. It should be noted that the decisions regarding the treatment methods were made by the same team of doctors to ensure consistency and comparability between patient groups. Initially, from July 2019 to July 2020, the department primarily utilized PCNL alone. Subsequently, with the aim of exploring potential improvements in clinical outcomes, we introduced a combined treatment approach of PCNL with flexible cystoscopy. This strategic evolution in our surgical protocols allowed for a direct comparison between the two methodologies.
Data collection
Patient data were collected from outpatient reviews, electronic medical records, and intraoperative records. Collected clinical data included age, gender, body mass index (BMI), affected side, Stone Treatment Outcome Prediction Engine (STONE) system score [15], family history of stones, preoperative history of urinary tract infection, hypertension, diabetes, stone type, and stone clearance.
Laboratory tests encompassed blood uric acid (BUA), serum cystatin-c (Cys-c), and β2 microglobulin (β2-BMG). BUA and Cys-c levels were determined using the sarcosine oxidase method (Beckman Coulter, AU5800), while β2-BMG was measured by a double antibody sandwich enzyme-linked immunosorbent assay (Shanghai Enzyme-linked Biological Co., Ltd., ml092626). Data collection was conducted from pre- to post-operative 7 days.
Perioperative data included surgery duration, intraoperative bleeding, and hospital stay. We observed complications comprising fever, hematuria, perirenal hematoma, and uremic sepsis. Stone clearance was evaluated using CT scans on postoperative day 5, considering stones cleared if no residues were present or residual stones were less than 4 mm in diameter.
Criteria for reoccurrence
1. Patients confirmed stone-free post-surgery but with new stones detected in subsequent routine physical examination. 2. Patients with clinical symptoms, such as low back pain, abdominal pain, or hematuria during follow-up, confirmed as new stone formations by imaging. 3. Patients with residual stones less than 2 mm were detected 2 to 4 weeks post-surgery, exhibiting a significant size or number increase in follow-up.
Outcome measures
Primary outcome measures: The stone clearance rate was compared between the two groups at two post-operative intervals: 5 days and 1 month. Additionally, the incidence of stone recurrence within one year post-surgery served as a prognostic indicator. In addition, risk factors influencing patient prognosis were identified through logistic regression.
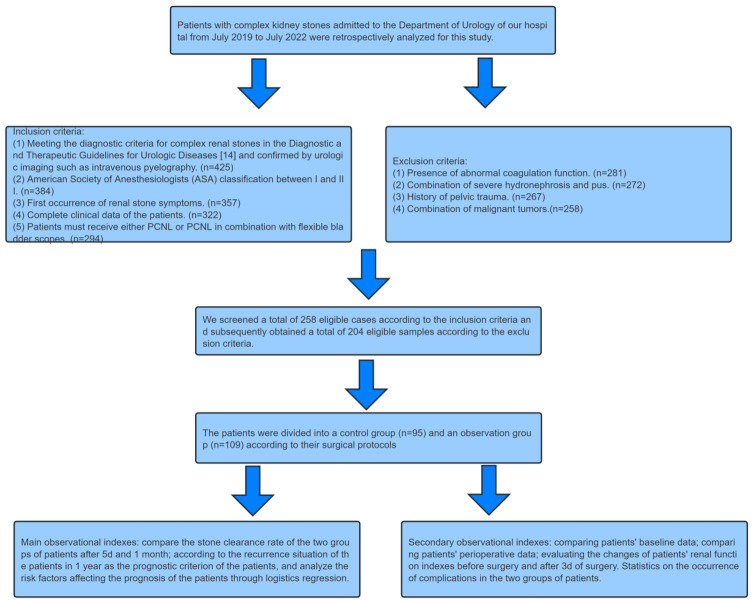
Secondary outcome measures: Baseline and perioperative patient data were compared between the two groups. Changes in renal function indices between before surgery and three days after the procedure were recorded. Furthermore, the occurrence of complications in both patient groups was statistically analyzed, as depicted in Figure 1.
Figure 1.
Study flow chart.
Statistical analysis
SPSS 26.0 software was used for data preprocessing. Counted data were expressed as a rate (%) and analyzed using the chi-square test. The Kolmogorov-Smirnov test was utilized to assess the normality of the distribution of continuous (measured) data. Data conforming to a normal distribution were expressed as mean ± standard deviation (Mean ± SD) and compared between groups using independent samples t-tests, while within groups using paired t-tests. Data that did not meet the normal distribution were expressed as P50 using quartiles (P25, P75) and processed using the Mann-Whitney U test. Risk factors affecting patients’ prognosis were analyzed using logistic regression. Independent variables included age, BMI, STONE score, and treatment regimen. A binary logistic regression model was used due to the dichotomous nature of the outcome variable (relapse: yes/no). Prior to analysis, the data were checked for missing values and outliers and standardized for continuous variables. The modeling process used a backward LR method to identify significant predictors. We considered the resultsignificant if the P value was less than 0.05.
Results
Comparison of baseline information
A comparison of the baseline data of the two groups of patients revealed that there were no significant differences between the two groups (P>0.05, Table 1).
Table 1.
Baseline information
| Items | Control group (n=95) | Observation group (n=109) | χ2/t value | P-value |
|---|---|---|---|---|
| Age (years) | 43.96±5.44 | 45.17±4.57 | 1.703 | 0.090 |
| Gender | ||||
| Male | 48 | 60 | 0.416 | 0.519 |
| Female | 47 | 49 | ||
| BMI (kg/m2) | 22.88±1.95 | 22.75±1.98 | -0.468 | 0.641 |
| Affected side | ||||
| Left side | 43 | 52 | 0.122 | 0.727 |
| Right side | 52 | 57 | ||
| STONE score | 8.00 [7.00, 9.00] | 8.00 [7.00, 9.00] | 0.657 | 0.496 |
| Family history of stones | ||||
| Yes | 11 | 16 | 0.425 | 0.515 |
| No | 84 | 93 | ||
| Preoperative urinary tract infection | ||||
| Yes | 22 | 27 | 0.072 | 0.788 |
| No | 73 | 82 | ||
| History of hypertension | ||||
| Yes | 8 | 5 | 1.251 | 0.263 |
| No | 87 | 104 | ||
| History of diabetes | ||||
| Yes | 10 | 7 | 1.119 | 0.290 |
| No | 85 | 102 | ||
| Type of stone | ||||
| Multiple calculus | 71 | 89 | 1.435 | 0.231 |
| Staghorn calculus | 24 | 20 |
Note: BMI, Body Mass Index; STONE score, Stone Treatment Outcome Prediction Engine.
Comparison of stone clearance rates at postoperative 5 d and 1 month
The postoperative 5 d stone clearance rate in the observation group was significantly higher than that in the control group (P=0.002, Table 2), while there was no statistical difference in the stone clearance rate between the two groups at 1 month after surgery (P=0.823, Table 2).
Table 2.
Comparison of stone clearance rates in patients at 5 d and 1 month postoperatively
| Group | 5 d stone removal rate | 1 month stone clearance rate |
|---|---|---|
| Control group (n=95) | 71 | 90 |
| Observation group (n=109) | 99 | 104 |
| χ2-value | 9.460 | 0.049 |
| P-value | 0.002 | 0.823 |
Comparison of perioperative indicators
The operative time in the control group was significantly longer than that in the observation group (P<0.001, Table 3). However, the two groups showed no statistical difference in the amount of intraoperative bleeding (P=0.351) and the length of hospitalization (P=0.777).
Table 3.
Comparison of perioperative indicators in patients
| Group | Surgical time (min) | Intraoperative bleeding (mL) | Length of hospitalization (d) |
|---|---|---|---|
| Control group (n=95) | 136.48±11.19 | 74.00 [67.50, 79.00] | 7.00 [6.00, 8.00] |
| Observation group (n=109) | 121.75±14.37 | 74.00 [71.00, 79.00] | 7.00 [6.00, 8.00] |
| χ2-value | -8.219 | 0.932 | -0.273 |
| P-value | <0.001 | 0.351 | 0.777 |
Changes in renal function before and after treatment
There were no statistical differences in BUA, Cys-c, or β2-BMG levels between the two groups before treatment (P>0.05). During treatment, renal function deteriorated in both groups of patients, showing a significant increase compared to pre-treatment levels (P<0.001), but the postoperative BUA, Cys-c, and β2-BMG levels in the observation group were significantly lower than those in the control group (P<0.05, Figure 2).
Figure 2.
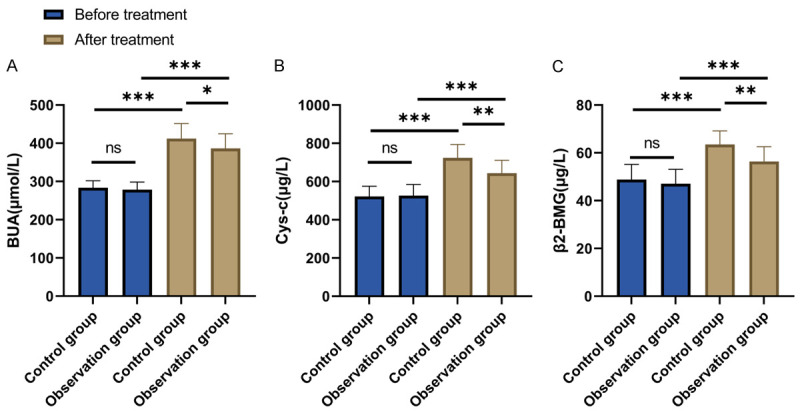
Changes in renal function of patients before and after treatment. A. Comparison of BUA changes before and after treatment between the two groups of patients; B. Comparison of Cys-c changes before and after treatment between the two groups of patients; C. Comparison of changes in β2-BGM before and after treatment between the two groups of patients. Note: nsP>0.05, *P<0.05, **P<0.01, ***P<0.001; BUA, blood uric acid; Cys-c, serum cystatin-c; β2-BMG, β2 microglobulin.
Incidence of postoperative complications
No statistical difference was found in the incidence of each complication between the two groups (P>0.05). However, the total incidence rate in the control group was significantly higher than that in the observation group (P=0.043, Table 4).
Table 4.
Complications
| Group | Fever (38.5°C) | Hematuria (≥100 mL) | Perirenal hematoma | Uremic sepsis | Total incidence |
|---|---|---|---|---|---|
| Control group (n=95) | 5 | 7 | 4 | 2 | 18 |
| Observation group (n=109) | 3 | 4 | 2 | 1 | 10 |
| χ2-value | 0.849 | 1.361 | 1.004 | 0.494 | 4.094 |
| P-value | 0.356 | 0.243 | 0.317 | 0.482 | 0.043 |
Analysis of factors influencing the reoccurrence
Using patients’ outpatient review records and electronic medical records, we tracked stone recurrence within 1 year. Among the 204 patients, 25 experienced recurrence, with a recurrence rate of 12.25%. Univariate analysis revealed that treatment regimen (P=0.009), BMI (P<0.001), STONE score (P<0.001), and family history of stones (P=0.001) were risk factors for recurrence (Table 5). Then, these indicators were assigned values after the measures were dichotomized based on cut-off values (Table 6). Subsequent multivariate analysis revealed that treatment regimen (P=0.010), BMI (P<0.001), and STONE score (P<0.001) were independent risk factors for recurrence (Table 7).
Table 5.
Univariate analysis of factors influencing recurrence
| Item | β | Standard error | χ2 | P-value | OR value | 95% confidence interval for EXP (B) | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Lower limit | Upper limit | ||||||
| Treatment plan | 1.226 | 0.47 | 6.791 | 0.009 | 3.406 | 1.355 | 8.563 |
| Age | -0.031 | 0.043 | 0.529 | 0.467 | 0.969 | 0.891 | 1.054 |
| BMI | 1.235 | 0.223 | 30.548 | <0.001 | 3.439 | 2.219 | 5.329 |
| STONE score | 1.288 | 0.243 | 28.021 | <0.001 | 3.625 | 2.250 | 5.840 |
| Surgical time | 0.003 | 0.014 | 0.051 | 0.822 | 1.003 | 0.975 | 1.032 |
| Intraoperative bleeding | 0.029 | 0.033 | 0.782 | 0.376 | 1.029 | 0.966 | 1.097 |
| Length of hospitalization | 0.223 | 0.207 | 1.155 | 0.283 | 1.25 | 0.832 | 1.877 |
| Distinguishing between the sexes | -0.043 | 0.427 | 0.01 | 0.920 | 0.958 | 0.414 | 2.214 |
| Affected side | -0.911 | 0.47 | 3.759 | 0.053 | 0.402 | 0.16 | 1.010 |
| Family history of stones | 1.616 | 0.485 | 11.09 | 0.001 | 5.031 | 1.944 | 13.021 |
| Preoperative urinary tract infection | 0.460 | 0.464 | 0.982 | 0.322 | 1.584 | 0.638 | 3.934 |
| History of hypertension | -0.545 | 1.063 | 0.263 | 0.608 | 0.58 | 0.072 | 4.662 |
| History of diabetes | 0.889 | 0.617 | 2.076 | 0.150 | 2.432 | 0.726 | 8.149 |
| Type of stone | -0.158 | 0.503 | 0.099 | 0.753 | 0.853 | 0.319 | 2.286 |
| BUA | 0.002 | 0.011 | 0.035 | 0.852 | 1.002 | 0.98 | 1.024 |
| Cys-c | 0.002 | 0.004 | 0.405 | 0.525 | 1.002 | 0.995 | 1.010 |
| β2-BGM | 0.063 | 0.035 | 3.252 | 0.071 | 1.065 | 0.995 | 1.141 |
Note: BMI, Body mass index; STONE score, Stone Treatment Outcome Prediction Engine; BUA, blood uric acid; Cys-c, serum cystatin-c; β2-BMG, β2 microglobulin.
Table 6.
Assignment table
| Consideration | Assignment of values |
|---|---|
| Treatment plan | Control group =1, observation group =0 |
| BMI (kg/m2) | ≥24.035 =1, <24.035 =0 |
| Stone score | ≥9.5 =1, <9.5 =0 |
| Family history of stones | Yes =1, no =0 |
| Relapse | Recurrence =1, no recurrence =0 |
Note: BMI, Body Mass Index; STONE score, Stone Treatment Outcome Prediction Engine.
Table 7.
Multifactorial analysis of factors influencing recurrence
| Consideration | β | Standard error | χ2 | P-value | OR value | 95% confidence interval for EXP (B) | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Lower limit | Upper limit | ||||||
| Treatment plan | 2.950 | 1.145 | 6.639 | 0.010 | 4.330 | 1.597 | 7.501 |
| BMI | 4.862 | 1.231 | 15.597 | <0.001 | 7.025 | 3.653 | 10.496 |
| STONE score | 4.681 | 1.126 | 17.277 | <0.001 | 6.767 | 3.686 | 9.940 |
| Family history of stones | -0.173 | 1.313 | 0.017 | 0.895 | 0.880 | 0.089 | 3.588 |
Note: BMI, Body Mass Index; STONE score, Stone Treatment Outcome Prediction Engine.
Discussion
Complex renal stones pose a significant challenge in treatment due to their size, morphology, and associated patient factors [16]. PCNL, a primary method for large stones, often results in unsatisfactory clearance rates, with a clearance rate of 56.9% for staghorn calculi reported in the CROES database [17,18]. Lower success rates, especially with antler stones, prompt the exploration of enhanced techniques, including multichannel and flexible scopes, alongside more efficient lithotripsy methods like pneumatic ballistic lithotripsy, to improve outcome [19].
Our study explored the synergistic application of flexible cystoscopy with PCNL for complex renal stones and uncovered substantial procedural benefits. This combination not only achieved higher stone clearance rates within 5 days post-surgery and offered shorter operation time, but also ensured improved renal function recovery and minimized complications compared to traditional PCNL alone. These findings echo the challenges highlighted in existing literature regarding PCNL’s limitations in fully addressing complex stones, where studies like those in the CROES database have shown suboptimal clearance rates [20,21]. The integration of flexible cystoscopy can enhance precision and accessibility, addressing the intricate stone morphology and distribution that occur in single-method approaches. Notably, the technique’s effectiveness in accessing difficult renal areas and the holmium laser’s efficiency in stone fragmentation suggest a promising avenue for reducing renal cortical bleeding and hastening recovery, aligning with the safety and efficacy reported by Nedbal et al. and Selmi et al. [22,23]. The observed reduction in surgery duration of PCNL plus flexible cystoscopy can be attributed to several efficiency-enhancing factors. First, the precise targeting and fragmentation capabilities of flexible scopes streamline the process of stone removal, particularly for complex stones, thereby reducing surgery time. Second, this approach minimizes complications, lessening the need for intraoperative management and further shortening surgery duration. Thirdly, the superior accessibility of flexible scopes allows for direct access to difficult renal calyces, eliminating the need for additional punctures. Also, advancements in endoscopic technology have improved procedural control and speed. These elements together enhance procedural efficiency and underscore the clinical benefits of the combined approach for complex renal stone management. While our immediate post-surgical outcomes revealed the method’s superiority, the similar stone clearance rates observed one month postoperatively between both groups underscore the enduring value of this combined therapy. By bridging the gap between traditional PCNL limitations and the need for more effective stone management strategies, our study advocates for a nuanced reevaluation of treatment protocols for complex renal stones, suggesting that integrating these innovative surgical techniques could revolutionize standard practices. Further research, particularly with larger, multi-centered studies, is crucial for validating these preliminary findings and potentially establishing a new standard of care that could significantly impact patients’ long-term health and quality of life.
The recurrent nature of kidney stones post-surgery significantly affects patients, leading to repeated episodes of pain, discomfort, and hematuria that severely impair their quality of life and daily activities [24]. This cycle of recurrence necessitates frequent medical interventions and long-term treatment strategies, substantially increasing the financial burden on patients. Moreover, these recurring conditions might culminate in chronic pain and renal impairment, exacerbating the patient’s overall health status [25]. The psychological impact of recurrent kidney stones is profound, as it escalates stress levels and emotional burdens, adversely affecting mental health and well-being [26]. Given the high risk of stone recurrence, it is imperative to implement effective preventive and therapeutic measures for those identified at high risk. Our one-year follow-up analysis pinpointed the treatment regimen, BMI, and STONE score as significant independent risk factors for the recurrence of kidney stones. A higher BMI, commonly associated with obesity, contributes to metabolic diseases and may increase urinary concentrations of stone-forming components such as calcium and uric acid, thus elevating the risk of stone formation [27]. Additionally, obesity is linked to chronic, low-grade inflammation that could alter urinary characteristics and exacerbate stone formation [28]. The STONE score, by evaluating stone complexity through factors like size, location, number, renal anatomy, and function, serves as a predictive tool for assessing the likelihood of recurrence. Higher STONE scores indicate greater complexity, posing significant challenges for non-surgical removal and may require more sophisticated surgical interventions [29-31]. In response to these challenges, our study explored the efficacy of combining PCNL with flexible cystoscopy for a more comprehensive management of kidney stones, especially those located in hard-to-reach areas. This approach ensures a thorough clearance of stones, potentially reducing the likelihood of residual stones and, consequently, the risk of recurrence. The synergistic use of these techniques not only promises to mitigate the physical, financial, and psychological impacts of recurrent kidney stones but also suggests a shift in treatment protocols, aiming for improved patient outcomes and quality of life. Emphasizing the integration of innovative surgical techniques highlights the need for a detailed understanding of stone management, urging further research into long-term prevention and management strategies for kidney stone recurrence.
In this study, we explored the effectiveness of using flexible cystoscopy in conjunction with PCNL for the treatment of complex renal stones, highlighting its potential benefits in reducing operative time and minimizing renal function damage. Despite the promising outcomes, the study’s limitations include a one-year follow-up period and its single-center, small sample size nature. The short follow-up duration limits our understanding of the long-term efficacy and recurrence rates, while the single-center approach restricts the generalizability of our findings across diverse patient populations. Recognizing these limitations, we aim to pursue further research through larger, multicenter clinical trials with extended follow-up periods. Such studies would not only provide a more comprehensive understanding of long-term impacts but also enhance the validity and applicability of findings, contributing to improved management strategies for patients with complex renal stones.
In conclusion, combining flexible cystoscopy with PCNL is a safe and effective surgical procedure for managing complex renal stones. In addition, the combined treatment may reduce short-term stone recurrence in patients.
Acknowledgements
This study was supported by the Lanzhou Science and Technology Development Guidance Plan Project (2019-ZD-113).
Disclosure of conflict of interest
None.
References
- 1.Hao Y, Shen X, Han D, Hao Z, Chen D. Tubeless PCNL versus standard PCNL for the treatment of upper urinary tract stones: a propensity score matching analysis. Int Urol Nephrol. 2024;56:1281–1288. doi: 10.1007/s11255-023-03872-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sorokin I, Mamoulakis C, Miyazawa K, Rodgers A, Talati J, Lotan Y. Epidemiology of stone disease across the world. World J Urol. 2017;35:1301–1320. doi: 10.1007/s00345-017-2008-6. [DOI] [PubMed] [Google Scholar]
- 3.Yuan S, Larsson SC. Assessing causal associations of obesity and diabetes with kidney stones using Mendelian randomization analysis. Mol Genet Metab. 2021;134:212–215. doi: 10.1016/j.ymgme.2021.08.010. [DOI] [PubMed] [Google Scholar]
- 4.Yuan S, Shi Y, Li M, Hu X, Bai R. Trends in incidence of urinary tract infection in mainland China from 1990 to 2019. Int J Gen Med. 2021;14:1413–1420. doi: 10.2147/IJGM.S305358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Large T, Assmus MA, Valadon C, Emmott A, Forbes CM, Agarwal D, Nottingham C, Scotland K, Rivera M, Chew B, Krambeck A. A multi-institutional review of single-access percutaneous nephrolithotomy for complex staghorn stones. Eur Urol Focus. 2021;7:1170–1175. doi: 10.1016/j.euf.2020.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Sahan A, Dincer E, Ozkaptan O, Cubuk A, Ertas K, Eryildirim B, Akca O. The impact of anterior calyceal stones on the outcomes of percutaneous nephrolithotomy for complex kidney stones: a comparative study. Minerva Urol Nephrol. 2021;73:815–822. doi: 10.23736/S2724-6051.20.04002-3. [DOI] [PubMed] [Google Scholar]
- 7.Kim SC, Tinmouth WW, Kuo RL, Paterson RF, Lingeman JE. Using and choosing a nephrostomy tube after percutaneous nephrolithotomy for large or complex stone disease: a treatment strategy. J Endourol. 2005;19:348–352. doi: 10.1089/end.2005.19.348. [DOI] [PubMed] [Google Scholar]
- 8.O’Connor CJ, Kinnear N, Browne G, Hennessey DB. Bilateral staghorn kidney stones in megacalycosis: non operative management of complex kidney stone disease. Urol Case Rep. 2022;44:102146. doi: 10.1016/j.eucr.2022.102146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bayne D, Maru J, Srirangapatanam S, Hicks C, Neuhaus J, Scales C, Chi T, Stoller M. Effects of delayed surgical intervention following emergency department presentation on stone surgery complexity. J Endourol. 2023;37:729–737. doi: 10.1089/end.2022.0843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liang T, Zhao C, Wu G, Tang B, Luo X, Lu S, Dong Y, Yang H. Multi-tract percutaneous nephrolithotomy combined with EMS lithotripsy for bilateral complex renal stones: our experience. BMC Urol. 2017;17:15. doi: 10.1186/s12894-017-0205-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ding Q, Zhu H, Fan Z, Li F, Tu W, Jin X, Fan B. Comparative analysis of super-mini percutaneous nephrolithotomy combined with flexible ureteroscopic lithotripsy versus flexible ureteroscopic lithotripsy alone for treating complex kidney stones: a retrospective study of 205 patients. Med Sci Monit. 2023;29:e941012. doi: 10.12659/MSM.941012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hu L, Zhang N, Zhang X, Liang H, Fan Y, Chen J. Laparoscopic pyelotomy combined with ultrasonic lithotripsy via a nephroscope for the treatment of complex renal stones. Urolithiasis. 2024;52:22. doi: 10.1007/s00240-023-01522-7. [DOI] [PubMed] [Google Scholar]
- 13.Chen H, Qiu X, Du C, Xie D, Liu T, Wang G, Song L. The comparison study of flexible ureteroscopic suctioning lithotripsy with intelligent pressure control versus minimally invasive percutaneous suctioning nephrolithotomy in treating renal calculi of 2 to 3 cm in size. Surg Innov. 2019;26:528–535. doi: 10.1177/1553350619849782. [DOI] [PubMed] [Google Scholar]
- 14.Fang D, Hu Y, Wang C, Tang C. Diagnostic value of urinary Tamm-Horsfall protein and 24 h urine osmolality for recurrent calcium oxalate stones of the upper urinary tract: cross-sectional study. Open Med (Wars) 2023;18:20230848. doi: 10.1515/med-2023-0848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sirirak N, Sangkum P, Phengsalae Y, Kongchareonsombat W, Leenanupunth C, Ratanapornsompong W, Ketsuwan C. External validation of the S.T.O.N.E. score in predicting stone-free status after rigid ureteroscopic lithotripsy. Res Rep Urol. 2021;13:147–154. doi: 10.2147/RRU.S304221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen D, Jiang C, Liang X, Zhong F, Huang J, Lin Y, Zhao Z, Duan X, Zeng G, Wu W. Early and rapid prediction of postoperative infections following percutaneous nephrolithotomy in patients with complex kidney stones. BJU Int. 2019;123:1041–1047. doi: 10.1111/bju.14484. [DOI] [PubMed] [Google Scholar]
- 17.Kalkanli A, Cilesiz NC, Fikri O, Ozkan A, Gezmis CT, Aydin M, Tandoğdu Z. Impact of anterior kidney calyx involvement of complex stones on outcomes for patients undergoing percutaneous nephrolithotomy. Urol Int. 2020;104:459–464. doi: 10.1159/000505822. [DOI] [PubMed] [Google Scholar]
- 18.Desai M, De Lisa A, Turna B, Rioja J, Walfridsson H, D’Addessi A, Wong C Jean Rosette On Behalf Of The Croes Pcnl Study Group. The clinical research office of the endourological society percutaneous nephrolithotomy global study: staghorn versus nonstaghorn stones. J Endourol. 2011;25:1263–1268. doi: 10.1089/end.2011.0055. [DOI] [PubMed] [Google Scholar]
- 19.Armitage JN, Irving SO, Burgess NA British Association of Urological Surgeons Section of Endourology. Percutaneous nephrolithotomy in the United Kingdom: results of a prospective data registry. Eur Urol. 2012;61:1188–1193. doi: 10.1016/j.eururo.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 20.Xu K, Ding J, Shi B, Wu Y, Huang Y. Flexible ureteroscopic holmium laser lithotripsy with PolyScope for senile patients with renal calculi. Exp Ther Med. 2018;16:1723–1728. doi: 10.3892/etm.2018.6369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jinhua D, Wanlin D. Retrospective analysis of stone basket combined with flexible ureteroscope holmium laser lithotripsy in the treatment of lower calyceal stones. Eur Rev Med Pharmacol Sci. 2022;26:3430–3436. doi: 10.26355/eurrev_202205_28836. [DOI] [PubMed] [Google Scholar]
- 22.Nedbal C, Jahrreiss V, Cerrato C, Castellani D, Kamal WK, Hameed Z, Gauhar V, Juliebo-Jones P, Tzelves L, Kallidonis P, Tokas T, Somani BK. Current role of endoscopic combined intrarenal surgery in the management of renal stones: a scoping review. Indian J Urol. 2023;39:274–284. doi: 10.4103/iju.iju_249_23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Selmi V, Sarı S, Caniklioğlu M, Öztekin Ü, Taspinar MS, Işıkay L. Effect of endoscopic ureteral stone treatment on kidney function. Cureus. 2021;13:e12883. doi: 10.7759/cureus.12883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baowaidan F, Zugail AS, Lyoubi Y, Culty T, Lebdai S, Brassart E, Bigot P. Incidence and risk factors for urolithiasis recurrence after endourological management of kidney stones: a retrospective single-centre study. Prog Urol. 2022;32:601–607. doi: 10.1016/j.purol.2022.02.010. [DOI] [PubMed] [Google Scholar]
- 25.Raizenne BL, Deyirmendjian C, Lafontaine ML, Balde M, Bechis SK, Sur RL, Nakada SY, Antonelli JA, Streeper NM, Sivalingam S, Viprakasit DP, Averch TD, Landman J, Chi T, Pais VM, Chew BH, Bird VG, Andonian S, Canvasser NE, Harper JD, Penniston KL, Bhojani N. The impact of bilateral stone disease on patients’ disease progression and health-related quality of life. J Endourol. 2023;37:1289–1294. doi: 10.1089/end.2023.0132. [DOI] [PubMed] [Google Scholar]
- 26.Li S, Iremashvili V, Vernez SL, Penniston KL, Jhagroo RA, Best SL, Hedican SP, Nakada SY. Effect of stone composition on surgical stone recurrence: single center longitudinal analysis. Can J Urol. 2021;28:10744–10749. [PubMed] [Google Scholar]
- 27.Laurenius A, Sundbom M, Ottosson J, Näslund E, Stenberg E. Incidence of kidney stones after metabolic and bariatric surgery-data from the scandinavian obesity surgery registry. Obes Surg. 2023;33:1564–1570. doi: 10.1007/s11695-023-06561-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Campschroer T, Van Balken MR, Deden LN, Hazebroek EJ, De Boer H. Effect of preoperative metabolic profiling to reduce the risk of kidney stones after bariatric surgery in patients with a history of stone formation. Surg Obes Relat Dis. 2023;19:633–639. doi: 10.1016/j.soard.2022.12.023. [DOI] [PubMed] [Google Scholar]
- 29.Wang K, Ge J, Han W, Wang D, Zhao Y, Shen Y, Chen J, Chen D, Wu J, Shen N, Zhu S, Xue B, Xu X. Risk factors for kidney stone disease recurrence: a comprehensive meta-analysis. BMC Urol. 2022;22:62. doi: 10.1186/s12894-022-01017-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kavoussi NL, Da Silva A, Floyd C, McCoy A, Koyama T, Hsi RS. Feasibility of stone recurrence risk stratification using the recurrence of kidney stone (ROKS) nomogram. Urolithiasis. 2023;51:73. doi: 10.1007/s00240-023-01446-2. [DOI] [PubMed] [Google Scholar]
- 31.Rule AD, Lieske JC, Li X, Melton LJ 3rd, Krambeck AE, Bergstralh EJ. The ROKS nomogram for predicting a second symptomatic stone episode. J Am Soc Nephrol. 2014;25:2878–2886. doi: 10.1681/ASN.2013091011. [DOI] [PMC free article] [PubMed] [Google Scholar]