Key Clinical Message
This clinical case report focuses on a case of surgery performed on a patient with the aim of cutting the dental apices in the patient's upper jaw. Mineral trioxide aggregate (MTA) was used as a filling material, and monitoring the condition showed that the operation was successful.
Keywords: apices, jaw, prosthodontics, surgery, teeth
1. INTRODUCTION
Dental root apicectomies are considered one of the important operations in preserving teeth. The process of cutting the apex of the dental roots in the jaws is one of the important surgical procedures performed by the dentist for many purposes, such as failure to treat teeth using traditional endodontic methods. 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 The dentist resorts to performing vertebral surgeries as one of the available methods for endodontically treating teeth. The dentist resorts to performing vertebral surgeries as one of the available methods for endodontically treating teeth. For example, an interesting consideration regarding the diagnosis of these events and their management in a currently minimally invasive manner studied in the reference in the reference. 11 It is known how much endodontic diagnosis can be facilitated by the availability of 3D examinations, which allow us to obtain, even if performed at low dosage and large FOV, all the useful information to proceed with treatment, whether orthograde or retrograde endodontic. In this case report, we present a dental maxillary treatment performed in the dental clinics at the International University of Science and Technology (https://iust.edu.sy/en/, https://iust.edu.sy/ar/%D8%A7%D9%84%D8%B9%D9%8A%D8%A7%D8%AF%D8%A7%D8%AA‐%D8%A7%D9%84%D8%B3%D9%86%D9%8A%D8%A9/). 12 , 13 After preparing the apex, a filling material is used to close the cavity at the root end. Several materials have been suggested and tested for this purpose: silver amalgam, gutta‐hanger, Cavit (3 M ESPE, St Paul, MN, USA), glass‐ionomer cements, zinc‐eugenol oxide‐reinforced cements (IRM, Super EBA), composite resin materials (Retroplast), compomers, polymers (Diaket, 3 M ESPE, St Paul, MN, USA), polycarboxylate cements, and bio‐ceramic cements (mineral trioxide aggregate [MTA]), Bio‐dentine or calcium phosphate silicate cements. 14 , 15 , 16 , 17 Where in this report, the return filling was performed in the spaces after the operation with MTA material. Mineral trioxide aggregate (MTA) (Pro Root MTA; Dentsply, Tulsa, OK, USA) was the first calcium silicate‐based retro filling material characterized by its biocompatibility, excellent sealing ability, and antibacterial properties. 18 , 19
2. CASE PRESENTATION
In this case report, we report patient Syrian woman, 40 years. Patient B N visited the dental clinics at the International University of Science and Technology when he was 40 years old in order to fully treat her teeth. The patient B N showed a complaint of swelling in the front of the upper jaw. When radiographs were taken of the patient B N, using X‐rays imaging, it was found that there was a large, radiolucent lesion that included several teeth.
3. METHOD
In this case report, the method of treatment for a 40‐year‐old Syrian woman, patient B N, with a complaint of swelling in the front of the upper jaw is described. The patient sought treatment at the dental clinics of the International University of Science and Technology. Radiographs were taken of the patient using X‐ray imaging, which revealed the presence of a large radiolucent lesion involving multiple teeth in the upper jaw. Based on this finding, surgery was deemed necessary to address the condition. Following the lesion resection, the apex was closed using MTA backfill. These measures were taken to promote healing and restoration in the affected area. After the surgical procedure was completed, the patient, B N, was monitored for a period ranging from one and a half to 2 months to evaluate the progress and ensure successful treatment. The patient's status was assessed through regular check‐ups and reviews of clinical findings. X‐ray images showed that the treatment had been successful and completed, with no evidence of the previously observed lesion. In summary, the method employed in this case report involved the use of X‐ray imaging for diagnosis, a wide flap technique for surgical access, and a sequence of steps including bone removal, apical resection, and lesion resection. The surgical area was then closed using MTA backfill, artificial bone graft, and a growth guide membrane. The patient's progress was monitored over a period of one and a half to 2 months, with positive results indicated by the X‐ray radiograph image after 3 weeks of monitoring.
Surgery was performed within the patient's upper jaw using a wide flap, as shown in the upper two images of Figure 1. Bone removal, apical resection, and lesion resection were performed as shown in the middle two images of Figure 1. Then, as shown in the bottom two images of Figure 1, the apex was closed with MTA backfill and an artificial bone graft and collagen‐absorbed growth guide membrane was placed. The patient B N was reviewed and monitored for a period ranging from one and a half to 2 months after the surgical procedure. In the Figure 2, we represent the X‐ray radiograph image of the patients before and after monitoring the case for 3 weeks. As it can be seen from the X‐ray image, the treatment was successful and completed.
FIGURE 1.
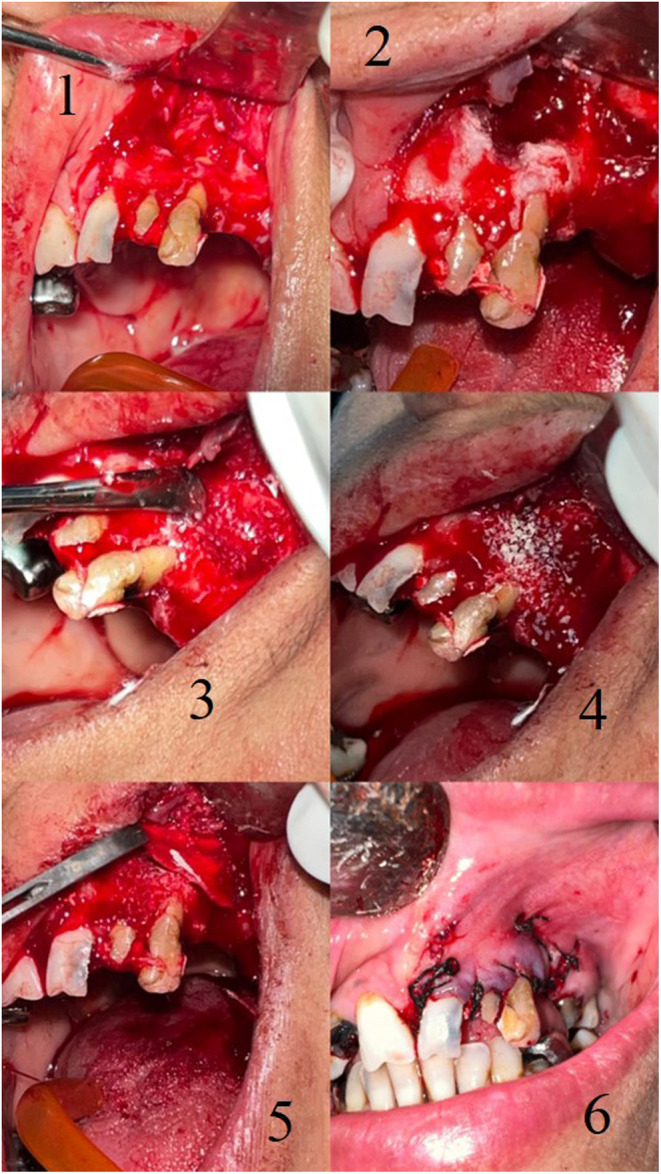
The case in which surgery was performed (before and after the surgical removal of the apices). 1, 2 at the beginning of surgical procedure. 3, 4, 5 during the removing of apices and inserting the MTA filler. 6 after stitching the wound in the patient mouse.
FIGURE 2.
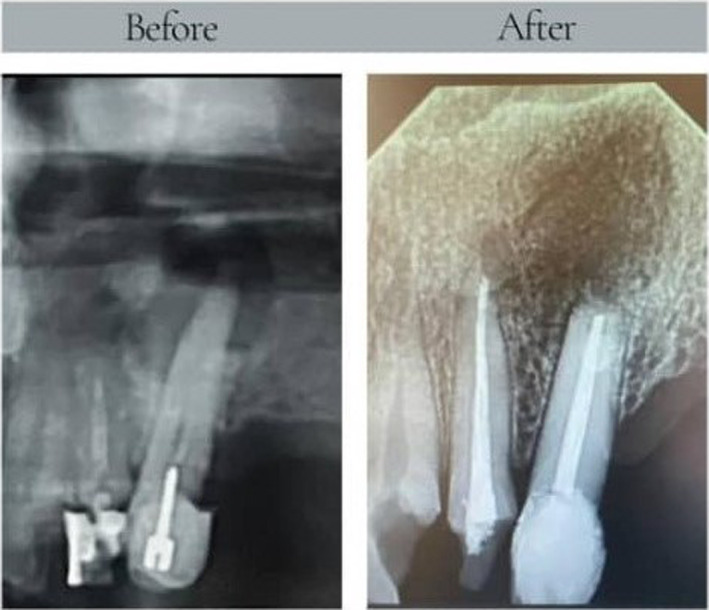
The radiograph image of the case in which surgery was performed (before and after the surgical removal of the apices).
4. CONCLUSION AND RESULTS
In this report, we presented the case of a patient who visited the specialized dental clinics at the International University for Science and Technology and were suffering from severe swelling in her upper jaw. Using X‐ray imaging of the patient's upper jaw, it was demonstrated that it was impossible to treat her with regular endodontic methods. A dental apex cut was performed in the patient's upper jaw in specialized dental clinics. Then, the apex was closed with MTA, a retrograde filling, an artificial bone graft was placed, and a growth‐directing membrane absorbed from collagen. The patient was found to have recovered after monitoring her condition for a period of one and a half to 2 months after completing the operation. The main conclusion remark of this surgical case report is that the surgical operation was performed successfully, and the patient had her lesions treated using a root apex procedure in her upper jaw.
5. DISCUSSION
In this case report, we presented the successful treatment of a Syrian woman, patient B N, who visited our dental clinics at the International University of Science and Technology at the age of 40. The patient presented with a complaint of swelling in the front of her upper jaw. Initial radiographic examination revealed a large, radiolucent lesion encompassing multiple teeth. To address this issue, surgery was performed in the patient's upper jaw using a wide flap approach. The surgical procedure involved bone removal, apical resection, and lesion resection. The images in Figure 1 demonstrate the various stages of the surgical procedure. The upper two images show the wide flap used to access the affected area. The middle two images depict the bone removal, apical resection, and lesion resection. Finally, the bottom two images illustrate the closure of the apex with MTA backfill and the placement of an artificial bone graft and collagen‐absorbed growth guide membrane. Following the surgical intervention, the patient B N was closely monitored for a period ranging from one and a half to 2 months. During this period, her recovery and progress were assessed and documented. After 3 weeks of monitoring, an X‐ray radiograph image was obtained and presented in Figure 2. This image clearly demonstrates the successful completion of the treatment. The lesion is no longer visible, and the affected area appears to have healed well. From this case report, it can be concluded that the surgical approach employed in the treatment of the patient B N's condition was effective in resolving the radiolucent lesion and restoring the health of her teeth. The successful outcome highlights the importance of accurate diagnosis, appropriate surgical techniques, and post‐operative monitoring in achieving favorable results in such cases.
AUTHOR CONTRIBUTIONS
Issa Saad: Conceptualization; data curation; formal analysis; funding acquisition; resources; writing – original draft; writing – review and editing. Marwan Al‐Raeei: Conceptualization; data curation; formal analysis; writing – original draft; writing – review and editing. Mohamad Salem Rkab: Conceptualization; data curation; formal analysis; funding acquisition; writing – original draft; writing – review and editing. Ahmad Al Manadili: Resources; writing – original draft; writing – review and editing. Chadi Azmeh: Writing – original draft; writing – review and editing. Tala Alkhori: Conceptualization; data curation; formal analysis; writing – review and editing. Remon Alhaja: Conceptualization; data curation; formal analysis. Rama Kabani: Conceptualization; data curation; formal analysis. Joudi Albokaii: Data curation; formal analysis; writing – original draft; writing – review and editing. Maya Saad: Conceptualization; data curation; formal analysis; funding acquisition.
FUNDING INFORMATION
This research is funded by International University for Science and Technology, http://iust.edu.sy and Damascus University https://damascusuniversity.edu.sy/.
CONFLICT OF INTEREST STATEMENT
No conflict of interests.
ETHICS STATEMENT
The authors have gotten the ethical approval document from the university (https://iust.edu.sy/) with the number 2023145120, and the authors have followed all of the ethics publishing terms.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
PERMISSION TO REPRODUCE MATERIAL FROM OTHER SOURCES
Not applicable.
CLINICAL TRIAL REGISTRATION
The authors have the clinical trial registration in the IUST clinic.
Saad I, Al‐Raeei M, Rikab MS, et al. A specific surgical procedure to remove the apices in the upper jaw. Clin Case Rep. 2024;0:e8799. doi: 10.1002/ccr3.8799
DATA AVAILABILITY STATEMENT
All data are included in the manuscript.
REFERENCES
- 1. Schmid C, Lotz M, Pieralli S, Valdec S. Guided flapless apicoectomy of the palatal root of a maxillary molar: a case presentation. Quintessence Int. 2022;53(7):608‐614. [DOI] [PubMed] [Google Scholar]
- 2. Wang HH, Lam C, Myneni SR. Resolution of a cystic endodontic‐periodontal lesion utilizing combined apicoectomy and guided tissue regeneration: a case report. Clin Adv Periodontics. 2022;12(2):94‐100. [DOI] [PubMed] [Google Scholar]
- 3. Fehlberg BK, Bittencourt G. Parendodontic surgery—apicoectomy and simultaneous obturation of root canals with mineral trioxide aggregate (MTA): case report. Dental Press Endod. 2019;9(1):48‐57. [Google Scholar]
- 4. Manfro R, Garcia GF, Bortoluzzi MC, Fabris V, Bacchi A, Elias CN. Apicoectomy and scanning electron microscopy analysis of an implant infected by apical (retrograde) peri‐implantitis: a case letter. J Oral Implantol. 2018;44(4):287‐291. [DOI] [PubMed] [Google Scholar]
- 5. Jakse N, Ruckenstuhl M, Rugani P, Kirnbauer B, Sokolowski A, Ebeleseder K. Influence of extraoral apicoectomy on revascularization of an autotransplanted tooth: a case report. J Endod. 2018;44(8):1298‐1302. [DOI] [PubMed] [Google Scholar]
- 6. Saad I, Rkab MS, Al Manadili A, et al. A specific surgical operation for frenectomy in the upper lip of a young man in his forties: case report. Adv Oral Maxillofac Surg. 2023;12:100461. [Google Scholar]
- 7. Kalyvas D, Tarenidou M, Zorogiannidis G, Tsetsenekou E, Grous A. Deep peri‐implantitis: two cases treated with implant apicoectomy with follow‐up of at least 7 years. Oral Surg. 2015;8(4):200‐207. [Google Scholar]
- 8. Toma L, Scarani V, Heulfe I, Brevi BC. Removal of fractured implants using the apicoectomy technique and immediate replacement with new implants: case report. J Oral Implantol. 2012;38(1):71‐77. [DOI] [PubMed] [Google Scholar]
- 9. Al‐Raeei M. When AI goes wrong: fatal errors in oncological research reviewing assistance. Oral Oncol Rep. 2024;10:100292. [Google Scholar]
- 10. Saad I, Al‐Raeei M, Azmeh C, et al. A titanium dental implant in the lower jaw for replacing missing molar: a case report. Med Rep. 2023;2:100017. [Google Scholar]
- 11. Reda R, Zanza A, Bhandi S, Biase A, Testarelli L, Miccoli G. Surgical‐anatomical evaluation of mandibular premolars by CBCT among the Italian population. Dent Med Probl. 2022;59(2):209‐216. [DOI] [PubMed] [Google Scholar]
- 12. Saad I, Rkab MS, Al Manadili A, et al. Surgical removal of bone tumour from the jaws to prepare the jaws to receive full dental compensation: case report. Adv Oral Maxillofac Surg. 2023;12:100456. [Google Scholar]
- 13. Al‐Raeei M, Al‐Jabban MO, Azmeh C, Al‐Raeei A. Bibliometrics study of the cancer research in the faculties of medicine and dentistry during Syrian crisis. Oral Oncol Rep. 2023;8:100105. [Google Scholar]
- 14. Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review‐part I: chemical, physical, and antibacterial properties. J Endod. 2010;36:16‐27. [DOI] [PubMed] [Google Scholar]
- 15. Hauman CH, Love R. Biocompatibility of dental materials used in contemporary endodontic therapy: a review. Part 2. Root‐canal‐filling materials. Int Endod J. 2003;36:147‐160. [DOI] [PubMed] [Google Scholar]
- 16. Seedat H, Van Der Vyver P, De Wet F. Micro‐endodontic surgery part 2: root‐end filling materials‐a literature review. South Africa Dent J. 2018;73:336‐342. [Google Scholar]
- 17. Kohli MR, Berenji H, Setzer FC, Lee S‐M, Karabucak B. Outcome of endodontic surgery: a meta‐analysis of the literature—part 3: comparison of endodontic microsurgical techniques with 2 different root‐end filling materials. J Endod. 2018;44:923‐931. [DOI] [PubMed] [Google Scholar]
- 18. Saad I, Saad M, Darwich Z, et al. Assessment and treatment of large tumor from the jaws in a 55‐Syrian male patient: a case report. Adv Oral Maxillofac Surg. 2023;13:100476. [Google Scholar]
- 19. Saad I, Jokhadar M, Rkab MS, et al. Pedunculated oral fibroma in an 11‐year‐old patient: a case study. Oral Oncol Rep. 2024;100143:100143. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are included in the manuscript.


