Abstract
Objectives:
Proximal humerus fractures (PHFs) are common fractures in the elderly and are typically treated conservatively with immobilization. However, there is no consensus on whether to choose early or late conventional mobilization, taking their outcomes into account. This paper reviews comparative studies on the clinical outcomes of one- and three-week immobilization periods in terms of limb function, pain intensity, and complications following the adoption of the non-surgical treatment of PHF.
Methods:
The current systematic review started with searching PubMed, Scopus, and Web of Science databases for randomized clinical trials (RCTs) on PHF patients to compare the clinical outcomes between patients receiving the one-week mobilization (early mobilization) and those receiving the three-week mobilization (late mobilization). We also performed a meta-analysis to compare the two groups’ limb function and pain levels at three and six months of follow-up.
Results:
Five of the seven RCTs had adequate data to be included in the meta-analysis. The quantitative results showed that the early mobilized patients had improved limb function at three [weighted mean difference (WMD): 5.15 (CI 95%: 0.68-9.62)] and six [WMD: 3.51 (CI 95%: 0.43-6.60)] months, but not at 12 months of follow-up. At either three, six, or 12 months, there was no difference in pain intensity between the two groups.
Conclusion:
This review supports the adoption of early mobilization at one week for the non-operative management of PHFs. However, to compare the long-term effects, more clinical trials with longer follow-ups are needed.
Key Words: Early mobilization, Immobilization, Non-operative treatment, Proximal humerus fracture, Systematic review
Introduction
Proximal humerus fractures (PHFs) comprise an estimated 5% of all fractures, which primarily affect the elderly.1,2 Being among fragility fractures, PHFs frequently result in major morbidity in osteoporotic individuals in the growing geriatric population.2 The majority of fractures now being considered for surgical treatment are those with the potential to develop nonunion or symptomatic malunion in active individuals.3-5 PHF, which is most frequently brought on by a minor fall in an elderly person with osteoporosis, results in two-part fractures with or without partial dislocation and is usually treated conservatively with fixation in a splint.6 The trend has been changing in recent years, with even more severely displaced fractures being treated non-surgically. This is due to the growing evidence that there is no clinically significant difference between surgical and non-surgical treatments with regard to patient-reported shoulder function at one-year follow-ups.7-9 However, there is controversy over the appropriate immobilization period when nonsurgical treatment is considered.
Consequently, the next key issue is to investigate the non-surgical treatment approach for PHFs. Immobilization is usually suggested for a period of one to three weeks. Early mobilization is believed to have some benefits, such as a quicker return to normal activities and less financial burden. There is a recent perception, supported by some studies, that hypothesizes early mobilization is more beneficial for upper extremity functions.10 However, some issues, such as pain during rehabilitation and non-unions, can result in decreased patient compliance. Therefore, to have a clear understanding, we planned to review previous clinical trial studies on this topic.
In this systematic review and meta-analysis study, we aimed to compare the clinical outcomes of pain and functional status between two groups of patients with PHFs who were treated conservatively with early and late (conventional) mobilization.
Materials and Methods
Study Setting
We conducted a systematic search of the literature using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) principles.
Search Strategy
In July 2022, the following search phrases were entered into the Medline, Scopus, Web of Science, and the Cochrane Library databases: (“proximal”) AND (“humerus” OR “humeral”) AND (“fracture”) AND (“immobilization” OR “mobilization” OR “rehabilitation” OR “physiotherapy”) AND (“immediate” OR “early” OR “late” OR “conventional” OR “duration” OR “period” OR “week”). To make sure we did not leave out any relevant publications, we also checked the references in the articles.
Eligibility Criteria and Study Selection
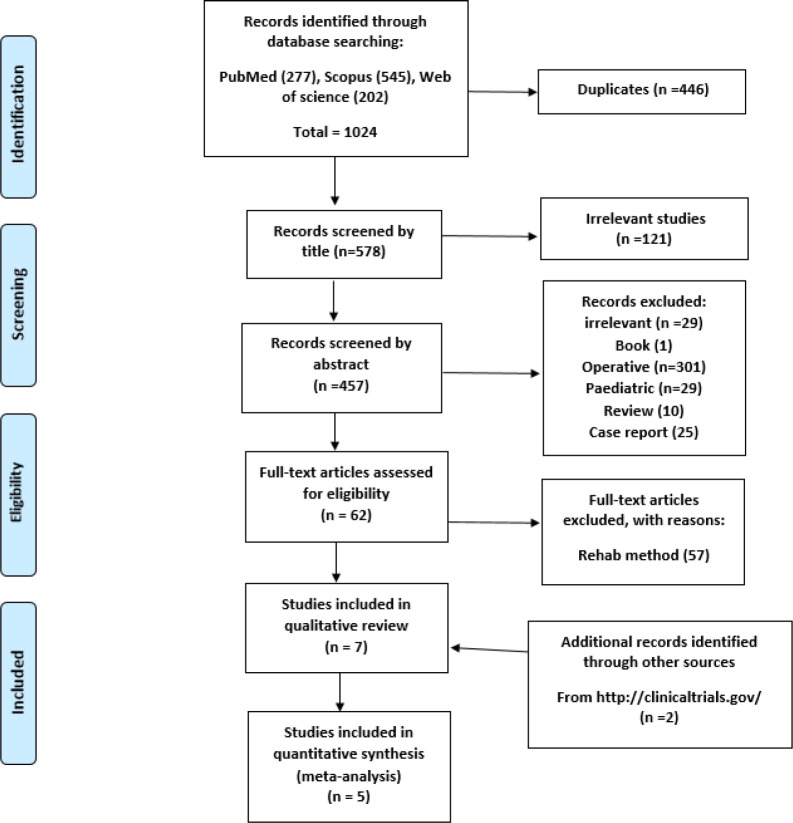
The purpose of the current study was to systematically review studies meeting the PICOS/TD methodological requirements [Table 1]. The exclusion criteria were operative treatment, chronic fractures, studies other than clinical trials, articles on the pediatric population, book chapters, studies without an available full text, and research comparing different rehabilitation techniques but not the timing of treatment [Figure 1].
Table 1.
PICOS/TD criteria for the inclusion of clinical trials
| Patients | Proximal humerus fracture in adults |
| Intervention | Early mobilization |
| Controls | Early and late (conventional) immobilization |
| Outcome | Pain and functional status |
| Timing | Follow-up of >3 months |
| Design | Clinical trial |
Figure 1.
Flowchart displaying the number of documents eliminated at each stage and the systematic search approach used
Data Extraction
The two authors used a pre-made data sheet to analyze the information extracted from each study, which included data on the study’s year of publication, design, the sample size in each group, follow-up intervals, the Neer classification of fractures, outcomes on patients’ pain scores, functional status [absolute Constant score (CS) or Neer score], and reported complications.
Quality Assessment
According to the modified Jadad scale, the quality of the included clinical trials was evaluated by the two authors (their names are removed for the sake of blinding the manuscript). The three main methodological criteria of randomization, blinding, and accountability were checked for each study. The scores ranged from 0 to 8 [Table 2]. Two trials scored 6/8 and one 7/8. The study by Kristiansen et al. scored 4/8 and was excluded from the meta-analysis. We could not assess two unpublished clinical trials due to unpublished details in the methodology.
Table 2.
Characteristics of the included studies
| Author (year) | Study design | Neer Fracture type (N) | Group | Sample size | Age (mean±SD) | Gender ratio (percentage of females) | Follow-up (month) | Jadad Score |
|---|---|---|---|---|---|---|---|---|
| Raquel Martínez (2021) | RCT | Nondisplaced (37) Two-part greater tuberosity (17) Two-part surgical neck (37) Three-part (19) Four-part (1) |
Early | 55 | 69.5±10.1 | 81 | 3, 6, 12 | 7 |
| Late | 56 | 71.3±10.4 | 76 | |||||
| B. Kristiansen (1989) | RCT | Minimally displaced fractures | Early | 42 | 72 (median) | 71 | 3, 6, 12 | 4 |
| Late | 43 | 70 (median) | 68 | |||||
| S. A. Hodgson (2007) | RCT | Minimally displacedtwo-part fractures | Early | 37 | 68.6±12.2 | 78.3 | 12, 24 | |
| Late | 37 | 68.2±11.4 | 86.4 | 6 | ||||
| S. A. Hodgson (2003) | RCT | Minimally displacedtwo-part fractures | Early | 44 | 70.7±12.5 | 75 | 2, 4, 12 | 6 |
| Late | 42 | 69.6±11.6 | 88 | |||||
| M.M. Lefevre-Colau (2007) | RCT | Nondisplaced (34) Two-part greater tuberosity (1) Two-part surgical neck (15) Three-part (24) 4 part (0) |
Early | 37 | 63.2±18.4 | 65 | 1.5, 3, 6 | 6 |
| Late | 37 | 63.4±17.5 | 81 | |||||
| Chen et al. (unpublished) | RCT | 82% non- or minimallydisplaced | Early | 26 | 63±13 | 19.2 | 3, 6 | -------- |
| Late | 24 | 62±12 | 37.5 | -------- | -------- | |||
| Torrens et al. (unpublished) | RCT | Minimally displaced or displaced two- or three-part | Early | 20 | -------- | -------- | 3, 6, 12 | -------- |
| Late | 22 | -------- | -------- | -------- |
Statistical Meta-Analysis
The main purpose of this meta-analysis was to compare pain and functional status scores between two groups of PHF patients conservatively treated by protocols of early and late mobilization. Forest plots were depicted to assess heterogeneity and calculate the pooled weighted mean difference (WMD) with corresponding 95% confidence intervals (WMD with a 95% CI was used as the pooled estimation of efficacy outcomes) for visual inspection across studies. Due to the conceptual heterogeneity, a random-effects meta-analysis was conducted to account for the heterogeneity of the study populations. Pooled estimates with their corresponding 95% CIs were calculated using the inverse-variance weights methods.11 The I2 statistics was used to assess heterogeneity across studies12 (I2=0% indicates no observed heterogeneity, and I2≥50% indicates substantial heterogeneity). Cochran’s Q test was also used to analyze the statistical significance of heterogeneity.13 The WMD was plotted against the inverse of the squared standard error. All statistical tests were two-tailed, and the significance level was set at less than 0.05 for all tests, except for the heterogeneity test. Statistical analyses were performed using Stata (version 17.0; Stata Corp., College Station, Texas, USA).
Results
Study Characteristics
Five published and two unpublished clinical trials were reviewed. The two unpublished clinical trials whose data were available were also included in this review: Carlos Torrens, personal communication, March 2019, Hospital del Mar, and Neal Chung-Jen Chen, personal communication, June 2019, Massachusetts General Hospital [Table 2].
There were 182 and 181 patients in the early and late groups, with mean ages of 66.6 and 66.57 years, respectively. The percentage of women in the early and late groups was 60% and 70.6%, respectively. The study by Kristiansen et al. lacked the necessary follow-up information to run any statistical test.14 The results of the three- and six-month follow-ups after the treatment were reported in five studies with a quantitative methodology. Three studies applied visual analogue scale (VAS) to evaluate pain intensity15,16 (Carlos Torrens, personal communication, March 2019, Hospital del Mar). The pain section from Neer and SF36 general health questionnaires were used in the studies by Kristiansen14 and Hodgson et al.,17 respectively. Pain scores are reported out of 100 in this review. Except for the study by Kristiansen et al., others evaluated limb function using the CS. The functional scores are also reported out of 100 in this review.
Quantitative Analysis (Clinical Outcomes)
The demographic characteristics of the patients in each study were analyzed. The age and gender ratio parameters were not different between the two groups (P>0.05).
Comparison of Functional Outcomes between Early and Late Mobilization Groups
According to the analysis of the four clinical trials and the comparison of the functional outcomes between early and late mobilization at the three-month follow-up after PHF, the WMD was 5.15 (CI 95%: 0.68-9.62) [Figure 2]. The results revealed the notable superiority of early mobilization. The heterogeneity index (I2) was 21.1% (P=0.28).
Figure 2.
Forest plot comparing functional outcomes between early and late mobilization groups at the three-month follow-up. The horizontal lines represent the confidence intervals for the studies included in the meta-analysis. The solid squares indicate the mean difference and are proportional to the weights used in the meta-analysis. The diamond represents the aggregated pooled effect. The diamond does not cross the line of null effect, indicating an overall significant improvement with early mobilization
The analysis of four clinical trials comparing early and late mobilization functional outcomes at the six-month follow-up after PHF showed that the WMD was 3.51 (CI 95%: 0.43-6.60) [Figure 3]. The results revealed the notable superiority of early mobilization. The heterogeneity index (I2) was 0% (P=0.58).
Figure 3.
Forest plot comparing functional outcomes between early and late mobilization groups at the six-month follow-up. The horizontal lines represent the confidence intervals for the studies included in the meta-analysis. The solid squares indicate the mean difference and are proportional to the weights used in the meta-analysis. The diamond represents the aggregated pooled effect. The diamond does not cross the line of null effect, indicating an overall significant improvement with early mobilization
The analysis of the three clinical trials comparing early and late mobilization functional outcomes at the 12-month follow-up after PHF revealed that the WMD was 1.84 (CI 95%: -2.63-6.30) [Figure 4]. The results revealed the notable superiority of early mobilization. The heterogeneity index (I2) was 0% (P=0.52).
Figure 4.
Forest plot comparing functional outcomes between early and late mobilization groups at the 12-month follow-up. The horizontal lines represent the confidence intervals for the studies included in the meta-analysis. The solid squares indicate the mean difference and are proportional to the weights used in the meta-analysis. The diamond represents the aggregated pooled effect. The diamond does not cross the line of null effect, indicating an overall significant improvement with early mobilization
Comparison of Pain Intensity between Early and Late Mobilization Groups
In the analysis of four clinical trials comparing early and late mobilization pain intensity at the three-month follow-up after PHF, the WMD was 1.84 (CI 95%: -5.34-9.01) [Figure 5]. The results revealed no superiority regarding early mobilization. The heterogeneity index (I2) was 48.1% (P=0.12).
Figure 5.
Forest plot comparing pain intensity between early and late mobilization groups at the three-month follow-up. The horizontal lines represent the confidence intervals for the studies included in the meta-analysis. The solid squares indicate the mean difference and are proportional to the weights used in the meta-analysis. The diamond represents the aggregated pooled effect. The diamond crosses the line of the null effect, indicating no significant improvement with early mobilization
In the analysis of four clinical trials comparing early and late mobilization pain intensity at the six-month follow-up after PHF, the weighted mean difference was -0.14 (CI 95%: -4.98-4.70) [Figure 6]. The results revealed no notable superiority regarding early mobilization. The heterogeneity index (I2) was 0% (P=0.62).
Figure 6.
Forest plot comparing pain intensity between early and late mobilization groups at the six-month follow-up. The horizontal lines represent the confidence intervals for the studies included in the meta-analysis. The solid squares indicate the mean difference and are proportional to the weights used in the meta-analysis. The diamond represents the aggregated pooled effect. The diamond crosses the line of the null effect, indicating no significant improvement with early mobilization
In the analysis of three clinical trials comparing early and late mobilization pain intensity at the 12-month follow-up after PHF, the WMD was 1.44 (CI 95%: -3.03-5.92) [Figure 7]. The results revealed no notable superiority regarding early mobilization. The heterogeneity index (I2) was 2.4% (P=0.36).
Figure 7.
Forest plot comparing pain intensity between early and late mobilization groups at the 12-month follow-up. The horizontal lines represent the confidence intervals for the studies included in the meta-analysis. The solid squares indicate the mean difference and are proportional to the weights used in the meta-analysis. The diamond represents the aggregated pooled effect. The diamond crosses the line of the null effect, indicating no significant improvement with early mobilization
Complications
In the study by Kristiansen et al., each group had one patient with complex regional pain syndrome type 1 (CRPS-1).14 There was also one case of frozen shoulder in the late mobilization group in the study by Hodgson and Martinez.16,17 Subacromial impingement was observed in one patient in each group.15 Martinez et al. reported four displacements in the early group versus one in the late group.16 Two osteonecrosis cases happened in the early group, and two nonunion occurred in the late group.16
Discussion
Recent investigations have failed to demonstrate any notable differences between the outcomes of conservative and surgical treatments for PHF, despite the fact that some researchers have emphasized the need to treat displaced fractures surgically.7-9,18 There is a disagreement over the required duration of shoulder immobilization in non-operative treatment cases. Formerly, a method of progressive rehabilitation after a period of three weeks of immobilization was adopted. However, early and late mobilization had comparable results in terms of pain and functional disability at baseline and follow-up in a recent clinical trial investigation.16 Another two trials pointed out more favorable results for immediate mobilization.15,17
The findings of this systematic review showed that when nonsurgical management is considered, a one-week immobilization period can be more efficient than a three-week immobility period for PHF in terms of the functional outcomes at three- and six-month follow-ups. The overall WMDs were 7.6 and 5.23 at the three- and six-month follow-ups, respectively, as reviewed by Dabija et al.,19 showing clinically significant differences at three months (MCID range of 5.4-11.6 for Constant score) in shoulder functional outcomes. Early mobilization following PHF has not been proven to significantly improve the range of motion (ROM) or pain. However, it did not cause any new difficulties. An essential factor to take into account is the probable side effects of keeping the elderly who have experienced a PHF immobilization for longer than necessary, which may result in compromised general well-being. 20
Limitations
One limitation was the variability of fracture patterns within a subgroup of the Neer classification, which could have affected the results of the functional outcome. The value of adding two unpublished datasets seems limited, as we could not assess the two trials due to unpublished details in the methodology.
Discussion of Key Findings
Clinical Outcomes
During a recent randomized clinical trial (RCT) study, non-operatively treated patients with PHFs were investigated in terms of mobilization time. The two groups of patients who began rehabilitation within one or three weeks following the injury showed no difference in functional scores, daily activities, CS, shoulder ROM, or the pain VAS score.16 Another RCT by Lefevre-Colau et al. resulted in a notably better functional score in patients treated by immediate mobilization (within three days) after 1.5 and 3 months of follow-up (P=0.02).15 Compared to the group receiving standard care, the early mobilization group had significantly less pain after three months (P=0.04) but not after six months (P=0.9).15 The early mobilization group exhibited greater active and passive abduction, as well as anterior elevation, in the assessments after 1.5 and 3 months.15 At the six-month follow-up, active ROM, as assessed in relation to the unaffected arm, did not substantially differ between the two groups.15 In the study by Hodgson et al., patients with immediate mobilization experienced enhanced shoulder function (P=0.001) after four months following the fracture compared to patients with a conventional immobilization period of three weeks.17 Participants in the early mobilization group had significantly higher scores on the SF36 health-related quality-of-life components for pain and physical role-limitation at 16 weeks.17 However, the significant differences were not observed after 13 months.17 With a longer follow-up, Hodgson et al. showed a trend toward decreased disability, as measured by the Croft Shoulder Disability Questionnaire, at one year in the early mobilization group (42.8% versus 72.5% in early and late mobilization, respectively)21. It is believed that patients who start rehabilitation early recover more quickly, which is often complete after a year.21 Similarly, Kristiansen et al. showed that significantly improved scores of pain and functional assessments after three months in the early mobilization group decreased after six months of follow-up.14 They identified no conclusive proof of a difference in ROM between the groups.14 Different PHF types have been reported by Martinez et al. and Colau et al. In the first study, secondary displacement occurred in four patients, three of whom had surgical neck PHF, while the latter reported no problems in either group.
Torrens et al. studied and followed 42 patients at 3, 6, and 12 months, and at all three follow-up points, participants in the late mobilization group consistently scored higher on the EuroQol 5D quality-of-life scale. In terms of the function score, pain score, or patient satisfaction, there were no differences between the two groups (Carlos Torrens, personal communication, March 2019, Hospital del Mar). Chen et al.’s trial evaluated shoulder ROM in both groups and found that flexion, external rotation, and abduction were higher among the early mobilized group (Neal Chung-Jen Chen, personal communication, June 2019, Massachusetts General Hospital) [Table 3].
Table 3.
. Results of the included studies
| Author (year) | Group | Functional Score (tool) | Pain score (tool) | ON | Secondary displacement | NU | Stiffness | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Follow-up 1 | Follow-up 2 | Follow-up 3 | P1 | P2 | P3 | Follow-up 1 | Follow-up 2 | Follow-up 3 | P1 | P2 | P3 | ||||||
| Raquel Martínez (2021) | Early | 50±15.4 (CS) | 61.3±16.7 (CS) | 68.1±16.2 (CS) | 0.663 | 0.352 | 0.93 | 20±19 (VAS) | 10±16 (VAS) | 6.5±15 (VAS) | 0.372 | 0.605 | 0.718 | 2 | 4 | 0 | 0 |
| Late | 48.5±18.1 (CS) | 58.6±17.9 (CS) | 68±17.4 (CS) | 24±23 (VAS) | 12±18 (VAS) | 6.6±14 (VAS) | 1 | 1 | 2 | 1 | |||||||
| B. Kristiansen (1989) | Early | 75.5 (Neer) | 86.6 (Neer) | 88.8 (Neer) | 0.001 | >0.05 | >0.05 | 77.1 (Neer) | 85.7 (Neer) | 91.4 (Neer) | 0.01 | >0.05 | >0.05 | 0 | 0 | 0 | 0 |
| Late | 65.5 (Neer) | 84.4 (Neer) | 87.7 (Neer) | 57.1 (Neer) | 80 (Neer) | 85.7 (Neer) | 0 | 0 | 0 | 0 | |||||||
| S. A. Hodgson (2007) | Early | 18 (42.8%) | 16 (43.2%) | <0.01 | >0.06 | ||||||||||||
| Late | 29 (72.5%) | 22 (59.5%) | |||||||||||||||
| S. A. Hodgson (2003) | Early | 57±26 (CS) | 70±21 (CS) | 82±23 (CS) | 0.001 | 0.001 | 0.002 | 65.8±19 (SF36) | 72±20.6 (SF36) | 69.2±27.2 (SF36) | <0.01 | <0.01 | 0.01 | 0 | 0 | 0 | 0 |
| Late | 39±19 (CS) | 54±20 (CS) | 75±25 (CS) | 50.5±18.6 (SF36) | 59.9±20 (SF36) | 65.6±26.6 (SF36) | 0 | 0 | 0 | 1 | |||||||
| M.M. Lefevre-Colau (2007) | Early | 44±16.5 (CS) | 71±14.6 (CS) | 81.5±11.2 (CS) | 0.02 | 0.02 | 0.07 | 22.9±34.1 (VAS) | 34.9±25.8 (VAS) | 38.8±25.5 (VAS) | 0.68 | 0.04 | 0.97 | 0 | 0 | 0 | 0 |
| Late | 33.9±16.5 (CS) | 61.1±17 (CS) | 75.4±14.4 (CS) | 19.3±35.9 (VAS) | 19.2±35.4 (VAS) | 39±32 (VAS) | 0 | 0 | 0 | 0 | |||||||
| Chen et al. (unpublished) | Early | 33±25 (DASH) | 18±12 (DASH) | 30±20 (Likert) | 20±10 (Likert) | 0 | 0 | 0 | 0 | ||||||||
| Late | 24±15 (DASH) | 14±7 (DASH) | 30±10 (Likert) | 20±30 (Likert) | |||||||||||||
| Torrens et al. (unpublished) | Early | 58.6±12 (CS) | 66.2±11.6 (CS) | 74.63±13.4 (CS) | 37±18.1 (VAS) | 38±20 (VAS) | 33.1±23 (VAS) | 2 | 0 | ||||||||
| Late | 56.2±16.3 (CS) | 66.7±13.1 (CS) | 73.17±13.7 (CS) | 35±23 (VAS) | 30±24 (VAS) | 22.3±26 (VAS) | 1 | 0 | |||||||||
Abbreviations: CS: constant score, P: P-value, VAS: visual analogue scale, ON: osteonecrosis, NU: nonunion
As measured by the CS, early mobilization was found to be more beneficial for regaining the fractured shoulder’s function than the usual three-week immobilization time. In Colau et al.’s study, only impacted fractures were included; however, this trial’s validity was limited by the rigorous physiotherapy program that was administered to both groups.15 Ten patients left the trial due to attendance issues. Kristiansen et al. observed that, compared to a three-week immobilization period, a one-week immobilization for minimally displaced PHFs resulted in less pain and greater function after three months of follow-up. At the 12- and 24-month follow-up, these disparities were no longer present.14 When evaluating outcomes on displaced PHFs with long-term follow-ups, short and long periods of immobilization produce similar outcomes, regardless of the fracture pattern.16 Initial immobilization prior to physiotherapy has been proposed for better pain management and the prevention of fracture displacement. Having the arm immobilized in a sling for three to four weeks can significantly interrupt everyday activities, especially in the elderly who are more susceptible to PHF due to osteoporosis. Pain intensity scores were almost similar between the two groups. However, it might be advantageous to take into account extending the immobilization time according to an individual’s pain.
Complication
After a three-week immobilization period, problems such as non-union, stiffness, and frozen shoulder were noted.16,17 In both groups, osteonecrosis and secondary displacement were reported, with early immobilized patients experiencing them more.16 There is no consistency in the type(s) of non-operatively treated PHFs that should be immobilized for longer periods. In the present study, most patients in the reviewed reports were non-displaced or minimally displaced. Colau et al. and Martinez et al. studied various PHF Neer types.22 While the first study did not disclose any issues in either group, secondary displacement occurred in four patients in the latter, three of whom had surgical neck PHFs. The possible explanation might be the longer follow-up in the study by Martinez et al., which did not take the impacted parameter into consideration, while Colau et al. defined all of the displaced fractures as impacted. However, a humeral head can be impacted in an anatomical position or in a (variably) displaced position. Therefore, impaction in itself cannot be regarded as the only classification discussing results after conservative treatment.
Uncertainty exists regarding our study’s findings due to the small number of trials and heterogeneous or unclear inclusion and exclusion criteria. There are some ongoing clinical trials whose data are not yet available (https://clinicaltrials.gov/ct2/show/NCT03786679), and after completion, more robust conclusions would be possible to draw.
Conclusion
Comparing early mobilization to the three-week immobilization for the non-surgical treatment of PHFs at the end of a six-month follow-up showed that early mobilization appears to be beneficial in terms of limb function, which remains to be proven. The level of pain was similar whether mobilization lasted one week or three weeks following the fracture. In the future, other factors, including psychological and social status, are suggested to be considered as risks for impaired function.23,24
Acknowledgment
We are grateful to Dr. Ramin Sadeghi for his assistance with the statistical meta-analysis. We appreciate the assistance with the submission from Shahryar Hashemi.
Conflict of interest:
None
Funding:
None
References
- 1.Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37(8):691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 2.Palvanen M, Kannus P, Niemi S, Parkkari J. Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res. 2006;442:87–92. doi: 10.1097/01.blo.0000194672.79634.78. [DOI] [PubMed] [Google Scholar]
- 3.Hageman MG, Jayakumar P, King JD, Guitton TG, Doornberg JN, Ring D. The factors influencing the decision making of operative treatment for proximal humeral fractures. J Shoulder Elbow Surg. 2015;24(1):e21–6. doi: 10.1016/j.jse.2014.05.013. [DOI] [PubMed] [Google Scholar]
- 4.Lanting B, MacDermid J, Drosdowech D, Faber KJ. Proximal humeral fractures: a systematic review of treatment modalities. J Shoulder Elbow Surg. 2008;17(1):42–54. doi: 10.1016/j.jse.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 5.Okike K, Lee OC, Makanji H, Harris MB, Vrahas MS. Factors associated with the decision for operative versus non-operative treatment of displaced proximal humerus fractures in the elderly. Injury. 2013;44(4):448–455. doi: 10.1016/j.injury.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 6.Davey MS, Hurley ET, Anil U, et al. Management options for proximal humerus fractures–A systematic review & network meta-analysis of randomized control trials. Injury. 2022;53(2):244–249. doi: 10.1016/j.injury.2021.12.022. [DOI] [PubMed] [Google Scholar]
- 7.Handoll HH, Elliott J, Thillemann TM, Aluko P, Brorson S. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev. 2022;6(6):CD000434. doi: 10.1002/14651858.CD000434.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Handoll H, Keding A, Corbacho B, Brealey S, Hewitt C, Rangan A. Five-year follow-up results of the PROFHER trial comparing operative and non-operative treatment of adults with a displaced fracture of the proximal humerus. Bone Joint J. 2017;99-B(3):383–392. doi: 10.1302/0301-620X.99B3.BJJ-2016-1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rangan A, Handoll H, Brealey S, et al. Surgical vs nonsurgical treatment of adults with displaced fractures of the proximal humerus: the PROFHER randomized clinical trial. JAMA. 2015;313(10):1037–1047. doi: 10.1001/jama.2015.1629. [DOI] [PubMed] [Google Scholar]
- 10.Østergaard HK, Mechlenburg I, Launonen AP, Vestermark MT, Mattila VM, Ponkilainen VT. The benefits and harms of early mobilization and supervised exercise therapy after Non-surgically treated proximal humerus or distal radius fracture: a systematic review and meta-analysis. Curr Rev Musculoskelet Med. 2021;14(2):107–129. doi: 10.1007/s12178-021-09697-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 12.Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. London, UK: The Cochrane Collaboration; 2011. [Google Scholar]
- 13.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Stat Med. 2002;21(11):1539–58. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 14.Kristiansen B, Angermann P, Larsen T. Functional results following fractures of the proximal humerus: a controlled clinical study comparing two periods of immobilization. Arch Orthop Trauma Surg. 1989;108(6):339–41. doi: 10.1007/BF00932441. [DOI] [PubMed] [Google Scholar]
- 15.Lefevre-Colau M, Babinet A, Fayad F, et al. Immediate mobilization compared with conventional immobilization for the impacted nonoperatively treated proximal humeral fracture: a randomized controlled trial. J Bone Joint Surg Am. 2007;89(12):2582–90. doi: 10.2106/JBJS.F.01419. [DOI] [PubMed] [Google Scholar]
- 16.Martínez R, Santana F, Pardo A, Torrens C. One versus 3-week immobilization period for nonoperatively treated proximal humeral fractures: a prospective randomized trial. J Bone Joint Surg Am. 2021;103(16):1491–1498. doi: 10.2106/JBJS.20.02137. [DOI] [PubMed] [Google Scholar]
- 17.Hodgson S, Mawson S. Rehabilitation after two-part fractures of the neck of the humerus. J Bone Joint Surg Br. 2003;85(3):419–22. doi: 10.1302/0301-620x.85b3.13458. [DOI] [PubMed] [Google Scholar]
- 18.Lopiz Y, Alcobía-Díaz B, Galán-Olleros M, García-Fernández C, Picado AL, Marco F. Reverse shoulder arthroplasty versus nonoperative treatment for 3-or 4-part proximal humeral fractures in elderly patients: a prospective randomized controlled trial. J Shoulder Elbow Surg. 2019;28(12):2259–2271. doi: 10.1016/j.jse.2019.06.024. [DOI] [PubMed] [Google Scholar]
- 19.Dabija DI, Jain NB. Minimal clinically important difference of shoulder outcome measures and diagnoses: a systematic review. Am J Phys Med Rehabil. 2019;98(8):671–676. doi: 10.1097/PHM.0000000000001169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cunningham C, O'Sullivan R, Caserotti P, Tully MA. Consequences of physical inactivity in older adults: A systematic review of reviews and meta‐analyses. Scand J Med Sci Sports. 2020;30(5):816–827. doi: 10.1111/sms.13616. [DOI] [PubMed] [Google Scholar]
- 21.Hodgson S, Mawson S, Saxton J, Stanley D. Rehabilitation of two-part fractures of the neck of the humerus (two-year follow-up) J Shoulder Elbow Surg. 2007;16(2):143–5. doi: 10.1016/j.jse.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 22.S II NC. Displaced Proximal Humeral Fractures Part II Treatment of three-part and four-part displacement. J Bone Joint Surg Am. 1970;52(6):1090–103. [PubMed] [Google Scholar]
- 23.Jayakumar P, Teunis T, Williams M, Lamb S, Ring D, Gwilym S. Factors associated with the magnitude of limitations during recovery from a fracture of the proximal humerus: predictors of limitations after proximal humerus fracture. Bone Joint J. 2019;101-B(6):715–723. doi: 10.1302/0301-620X.101B6.BJJ-2018-0857.R1. [DOI] [PubMed] [Google Scholar]
- 24.Johnson NA, Dias J. The effect of social deprivation on fragility fracture of the distal radius. Injury. 2019;50(6):1232–1236. doi: 10.1016/j.injury.2019.04.025. [DOI] [PubMed] [Google Scholar]