Abstract
Probiotics currently available on the market generally belong to a narrow range of microbial species. However, recent studies about the importance of the gut microbial commensals on human health highlighted that the gut microbiome is an unexplored reservoir of potentially beneficial microbes. For this reason, academic and industrial research is focused on identifying and testing novel microbial strains of gut origin for the development of next-generation probiotics. Although several of these are promising for the prevention and treatment of many chronic diseases, studies on human subjects are still scarce and approval from regulatory agencies is, therefore, rare. In addition, some issues need to be overcome before implementing their wide application on the market, such as the best methods for cultivation and storage of these oxygen-sensitive taxa. This review summarizes the most recent evidence related to NGPs and provides an outlook to the main issues that still limit their wide employment.
Keywords: Next-generation probiotics, Live biotherapeutics, Gut microbiome, Faecalibacterium prausnitzii, Akkermansia muciniphila, Prevotella copri
Introduction
The importance of the gut microbiome in influencing human health is widely recognized [1]. Indeed, an alteration in the gut microbiome composition (dysbiosis) has been linked to several intestinal and systemic diseases, such as inflammatory bowel and Crohn’s disease, obesity, diabetes and metabolic syndrome, allergies, immune and cardiovascular diseases [2, 3]. Although a causative effect is yet to be demonstrated, independent observational studies highlighted the presence of common microbial signatures, specific for each disease.
Microbiome-targeted intervention to promote host health
Dietary interventions for the modulation of the gut microbiome
Diet is considered as one of the main factors influencing the gut microbiome. Long-term, habitual diet shapes the gut microbiome composition and activities. Several studies demonstrated that the gut microbiome of non-Westernized populations living in Africa or South-America and habitually consuming a diet richer in undigestible fiber and phytochemicals compared to urbanized, Western subjects, show higher abundance of fiber-degrading microbial taxa in their gut microbiome [4]. These microbes are able to degrade complex polysaccharides and phytochemicals entrapped in the matrix, producing health-promoting metabolites from their catabolism, such as short-chain fatty acids (SCFA) from fiber fermentation, isothiocyanates or urolithins from polyphenols, that are usually enriched in the metabolome of these subjects [5, 6]. Consistently, Western subjects consuming a habitual diet rich in products of vegetable origin (e.g., vegetarian/vegan diet, Mediterranean diet) present features in their gut microbiome similar to non-Western populations, such as higher Bacteroidetes/Firmicutes ratio and higher levels of fiber-degrading bacteria (e.g., Prevotella, Faecalibacterium, Roseburia, Lachnospira) [5, 7–10]. In addition, these studies demonstrated that a dietary pattern rich in vegetable-based products is associated with a beneficial metabolome and positive health effects, such as a reduced inflammation, lower cardiometabolic risk and an improved glucose homeostasis [6, 9, 10]. However, it was highlighted that both the type of fibre and its structure may influence the effect of the gut microbiome and metabolome [11, 12]. In recent years, the possibility of manipulating the gut microbiome composition and activities as a therapeutic or preventive approach was explored. Dietary interventions targeting the gut microbiome in healthy and diseased populations were carried out, either evaluating the effect of a supplementation with specific foods (e.g., products rich in fiber or polyphenols) or the influence of a more complex dietary pattern (e.g., Mediterranean or vegan diets). Despite the differences in the study design, target population and methods used, most of these studies highlighted the strong impact of the dietary intervention on the gut microbiome and on the host health. A recent study evaluated the effect of a 2-month intervention with a Mediterranean diet in obese/overweight adults [8]. The intervention promoted the increase of Faecalibacterium prausnitzii, a microbial species well known for the ability to degrade complex polysaccharides and produce beneficial SCFA. On the contrary, a decrease in the pro-inflammatory Ruminococcus gnavus was observed. These changes were associated with a decrease in plasma cholesterol, inflammatory markers and insulin resistance [8]. Consistently, Ghosh et al. [11] observed a similar effect in a longer intervention (1 year) with the Mediterranean diet on elder subjects. However, these and other studies highlighted that the effect of the dietary intervention cannot be generalized. Indeed, the effects of a dietary treatment differ inter-individually and may be influenced by a combination of host and microbiome features [12, 13]. It was suggested that the baseline composition of the gut microbiome may be responsible for the individualized response to the same meal. In addition, building a complex model integrating the microbiome and host-specific features, it was possible to predict the individual’s metabolic response with good accuracy [14, 15], demonstrating that dietary recommendations should not be generalized. Therefore, the individual’s microbiome should be considered to inform the design of a personalized diet.
Modulation of the gut microbiome by probiotics
Probiotics are defined as “live microorganisms that, when administered in adequate amounts, confer a health benefit on the host” [16]. Probiotic microorganisms may interact with the host and its microbiome through different mechanisms, directly interplaying with human intestinal cells or producing active metabolites, that can indirectly act on the host microbiome by changing the gastrointestinal environment (e.g., pH lowering). In addition, ingested probiotics may compete with commensal microbes for nutrients and binding sites, or by producing antimicrobial compounds (organic acids, bacteriocins). Metabolites produced by probiotic microbes can act at the interface of human cell, binding to receptors on intestinal epithelial, immune, endocrine, and nervous cells [17, 18]. Probiotic strains may explicate their activity in different ways. Some strains promote the production of β-defensin and immunoglobulin A (IgA), thus suppressing the growth of pathogens or reducing the permeability of the intestinal barrier, inducing mucin production and strengthening tight junctions [17–20]. Other strains have an immunomodulatory activity, stimulating the production of anti-inflammatory cytokine, or can produce neuroactive molecules from dietary precursors, such as γ-aminobutyric acid (GABA), kynurenic acid, serotonin, catecholamines and acetylcholine [19–21].
Most of the probiotic strains available on the market belong to a limited number of genera, mainly Lactic Acid Bacteria (LAB; e.g., Lactobacillus, Lactococcus) or Bifidobacterium spp. and the main isolation sources are fermented foods or the human gut [18, 22]. These taxa have been granted the status of Generally Regarded as Safe (GRAS) in the United States or of Qualified Presumption of Safety by the European Food Safety Authority. Although their activity is strain-specific, the influence on human health and on the human microbiome has been widely studied in animals and humans and was recently and extensively reviewed [22–24]. However, recent advances in the knowledge of the gut microbiome suggested that the range of potentially beneficial microbes is much wider, and the human gut microbiome may be considered as an unexplored reservoir of novel probiotics.
Mining the gut microbiome for next-generation probiotics
Next-generation probiotics (NGPs) are microbial taxa that conform to the traditional definition of probiotics, but do not have an history of use for health promotion. They also fit well in the definition of live biotherapeutic products (LBP) given by the US Food and Drug Administration: “a biological product that: (1) contains live organisms, such as bacteria; (2) is applicable to the prevention, treatment, or cure of a disease or condition of human beings; and (3) is not a vaccine” [25]. Regulation about NGPs is still lacking and varies across countries. In Europe, all microorganisms that have not been used in foods before 1997, must be carefully evaluated by EFSA before being admitted on the market, either as a novel food or as a drug [26].
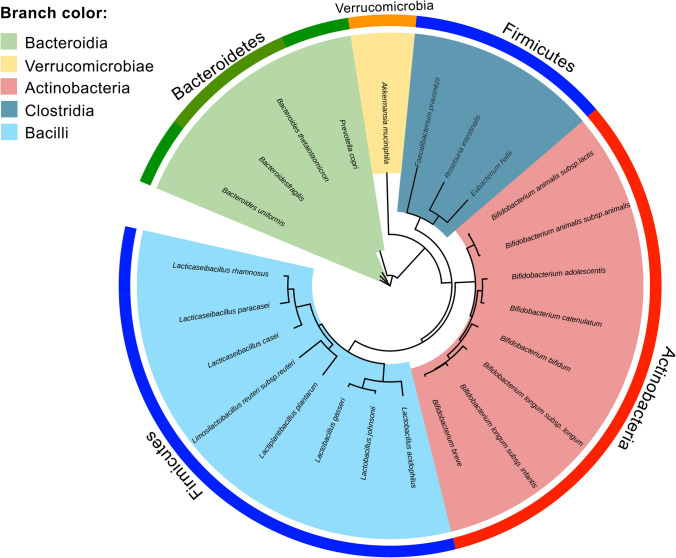
Several microbial commensals have been evaluated as NGPs. Of these, Akkermansia muciniphila, Faecalibacterium prausnitzii, Eubacterium hallii, Prevotella copri, Bacteroides spp. are the most promising. NGPs are phylogenetically distant from LAB, that belong to Firmicutes (Bacilli class) or Actinobacteria phyla (Fig. 1). Most of these taxa (Prevotella, Bacteroides, Akkermansia) are from different phyla (Bacteroidetes, Verrucomicrobia), while others (Faecalibacterium, Roseburia and Eubacterium) belong to the Firmicutes phylum but are from a different class (Clostridia; Fig. 1).
Fig. 1.
Phylogenetic tree of species from common probiotics Lactic Acid Bacteria ore recently investigated next-generation probiotics. Outer ring is colored according to the phylum, while branch background is colored according to the class. Phylogenetic tree was based on concatenated marker genes as inferred by PhyloPhlAn 3.0 (https://github.com/biobakery/phylophlan) and visualized using iTOL v6 (https://itol.embl.de). Genomes used are from strains: Eubacterium hallii DSM3353; Akkermansia muciniphila DSM22959; Bacteroides fragilis NCTC9343; B. thetaiotaomicron DSM2079; B. uniformis ATCC8492; Faecalibacterium prausnitzii A2165; Prevotella copri DSM18205; Roseburia intestinalis R1.82; Bifidobacterium adolescentis ATCC15703; Bif. animalis subsp. animalis ATCC25527; Bif. animalis subsp. lactis BLC1; Bif. bifidum ATCC29521; Bif. breve DSM20213; Bif. catenulatum DSM16992; Bif. longum subsp. infantis ATCC15697; Bif. longum subsp. longum KCTC3128; Lacticaseibacillus casei DSM20011; Lc. paracasei ATCC25302; Lc. rhamnosus DSM20021; Lactiplantibacillus plantarum DSM20174; Lactobacillus acidophilus DSM20079; Lb. gasseri ATCC33323; Lb. johnsonii GHZ10a; Limosilactobacillus reuteri subsp. reuteri DSM20016
Akkermansia muciniphila
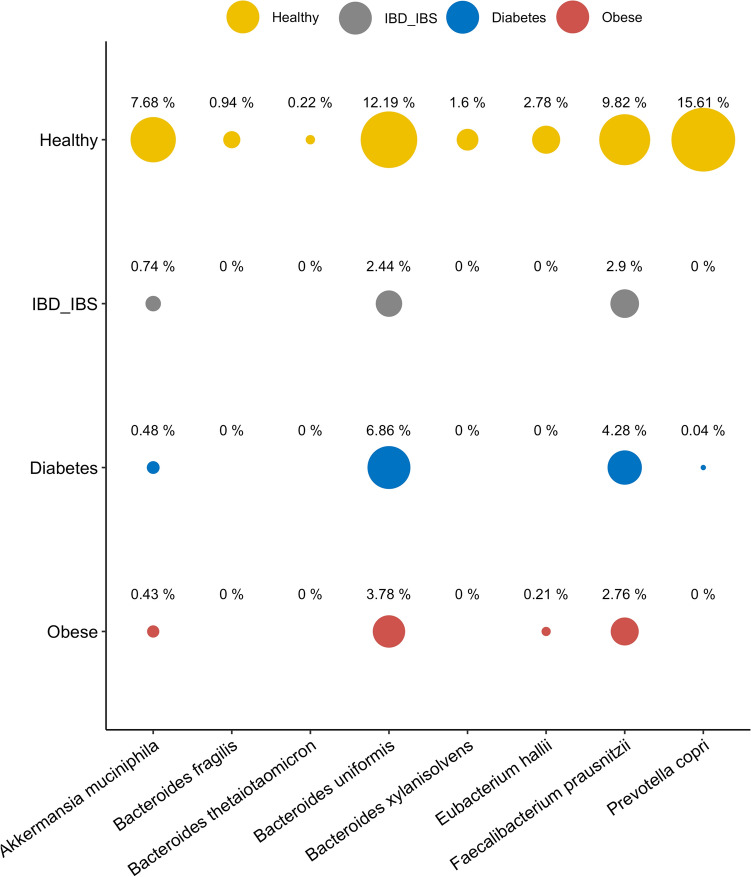
Akkermansia muciniphila is the only cultured member of Verrucomicrobia phylum. It can degrade the intestinal mucus layer to obtain energy [27], which has been suggested as one of the factors giving it a competitive advantage in the animal gut niche [28]. Evidence from several independent studies suggested that it is usually depleted in gut inflammatory conditions (Inflammatory Bowel Diseases, IBD and inflammatory bowel syndrome, IBS), as well as in obesity and diabetes (Fig. 2). Indeed, several studies reported a negative correlation of A. muciniphila abundance and obesity [29, 30] and detected an increase in its abundance during weight-loss [31]. However, a recent genome-based study reported the presence of five putative different species, closely related to A. muciniphila [32]. Interestingly, only one species was negatively associated with Body Mass Index, highlighting the need of an accurate taxonomic classification within Akkermansia genus [32]. The possibility to modulate A. muciniphila abundance by diet was also observed: A. muciniphila increased upon an intervention with prebiotic fructo-oligosaccharides (FOS) in obese mice and rats [33–35], as well as upon the consumption of a polyphenols-rich pomegranate extract [36]. In addition, the presence of A. muciniphila was associated with an improved metabolic response upon a 6-weeks calorie restriction diet: Dao et al. [30] demonstrated that only the group of subjects with higher abundance of A. muciniphila displayed an improvement in insulin sensitivity upon the diet [30], while the group with low A. muciniphila received the same diet, but did not display the same beneficial effects. All these data supported the role of A. muciniphila in human health, particularly in glucose homeostasis, and fostered studies on its use as probiotic supplementation (Table 1). Several studies carried out on mice models demonstrated an effect of A. muciniphila supplementation on reducing chronic inflammation (endotoxemia) and fat mass gain, improving glucose homeostasis and insulin sensitivity, and increasing energy expenditure, either consuming a normal or a high-fat diet (Table 1). Therefore, most of the existing evidence suggests the use of A. muciniphila as probiotic to ameliorate the metabolic state associated with obesity and diabetes. However, a recent study also highlighted that A. muciniphila was able to reduce the decline associated with aging, attenuating inflammation, immune disorders, and intestinal mucus layer thinning, thus promoting healthy aging [37]. Moreover, the positive effect of the consumption of A. muciniphila on experimentally induced periodontitis was also suggested: the gavage with A. muciniphila in mice infected by Porphyromonas gingivalis (a primary periodontal pathogen), reduced the bone loss typical of this condition compared with controls not receiving the microbial supplement [38]. Finally, the positive effect on reducing colitis and associated tumorigenesis was also suggested [39, 40].
Fig. 2.
Average relative abundance in the human gut of species investigated as Next-Generation Probiotics. Data were extracted from curatedMetagenomicData Bioconductor package on July 2021 (https://waldronlab.io/curatedMetagenomicData/). IBD, Inflammatory Bowel Disease; IBS, Inflammatory Bowel Syndrome
Table 1.
Animal trials using next-generation probiotics
| Number of animals | Age | Study details | Condition of the microorganism | Method of administration | Dose | Frequency | Treatment length | Results | References | |
|---|---|---|---|---|---|---|---|---|---|---|
| A. muciniphila ATTC BAA-835 | 54 | 6 weeks | Accelerated aging | N.A | Oral gavage | 2 × 108 | Three times a week | 10 weeks | Improvement of immune system and gut permeability | [41] |
| A. muciniphila p2261 | 245 | 7 weeks | Fecal transplant from cancer patients | Live or pasteurized | Oral gavage | 1 × 108–1 × 109 | Three times in 2 weeks | 14 days | Reduced inflammation; production of anticancer metabolites | [42] |
| A. muciniphila ATCC BAA-835 | N.A | 6–8 weeks | Acute colitis | Pasteurized and purified membrane protein | Oral gavage | 1.5 × 108 of pasteurised A. muciniphila; 3 µg of Amuc_1100 protein | N.A | From 2 weeks before treatment to sacrifice | Pasteurised A. muciniphila and Amuc_1100 relieved colon shortening and splenomegaly and attenuated histological injuries in the proximal colon | [43] |
| A. muciniphila ATTC BAA835 | 24 | 6–7 weeks | Colitis | Live | Oral gavage | 3 × 109 | Daily | 14 days | Colon histological damage and mucosal barrier improvement; Reduced inflammation | [44] |
| A. muciniphila ATTC BAA835 | 53 | 10 weeks | Obesity and type 2 diabetes | Live and heat-killed | Oral gavage | 2 × 108 | N.A | 4 weeks | Reduced body weight, improved body composition; Improved gut barrier and metabolic parameters | [34] |
| A. muciniphila ATCC BAA-835 | 20 | 6 weeks | Healthy | Live | Oral gavage | 2 × 108 | Daily | 5 weeks | Reduced fat mass and increased lean mass; Improved glucose homeostasis; Reduced metabolic endotoxemia and inflammation | [45] |
| A. muciniphila ATCC-BAA-835 | 24 | 6 weeks | High-fat diet | Live, supernatant or purified protein | Oral gavage | 4 × 108 | Daily | 14 weeks | Reduced body mass; Improved glucose tolerance; increased serum concentrations of insulin and glucagon-like peptide-1 (GLP-1) | [46] |
| A. muciniphila ATTC BAA-835 | 21 | 8 weeks | Obese | Pasteurized | Oral gavage | 2 × 108 | Daily | 5 weeks | Reduced body weight gain and fat mass gain without affecting cumulative food intake | [47] |
| A. muciniphila ATTC BAA-835 | 125 | 10–11 weeks | Obesity and diabetes | Live, pasteurized and purified protein Amuc_1100 | Oral gavage | 1 × 109–1 × 1010 for live Akkermansia; 1 × 1010 for pasteurized Akkermasia; 3 µg of purified protein | Daily | 1st experiment 4 weeks, 2nd and 3rd experiment 5 weeks | Live and pasteurized A. muciniphila reduces body weight, fat mass gain, improve glucose intolerance and insulin resistance | [48] |
| A. muciniphila ATCC BAA-835 | 36 | 20 weeks | Porphiromonas gingivalis induced periodontitis | Live and purified protein Amuc_1100 | Oral gavage | 1 × 109 | Three times a week | 6 weeks | A. muciniphila and Amuc_1100 reduces alveolar bone loss and periodontal inflammation | [49] |
| A. muciniphila ATCC BAA-835 | 24 | 22 weeks | Obesity | Live | Oral gavage | 1 × 109 | Daily | 2 weeks | Inflammation reduction; reduced soft and hard tissue damage and alveolar bone loss | [50] |
| A. muciniphila ATCC BA-835 | 36 | 6–8 weeks | Diabetes | A. muciniphila-derived extracellular vesicles | Oral gavage | 10 µg | Daily | 2 weeks | Reduction of gut permeability | [51] |
| A. muciniphila CIP 107961 T | 24 | 25 weeks | Diabetes | Centrifugated | Oral gavage | 2 × 108 | Three times a week | From 3 weeks of age to 10 weeks | Delayed onset of diabetes; reduced serum endotoxin levels | [52] |
| A. muciniphila BAA-835 | 36 | 8 weeks | Endotoxemia-Induced Inflammation in Apoe − / − | Live and heat killed | Oral gavage | 5 × 109 | Daily | 8 weeks | A muciniphila improved both aortic and systemic inflammation, reduced gut permeability | [53] |
| B. fragilis ATCC 25285 | 40 | N.A | Graft-versus-host disease (GVHD) | Live | Oral gavage | 1 × 109 | Three times a week for 1 week and weekly for 30 days | 33 days | Improved acute and chronic GVHD development | [54] |
| B. acidifaciens JCM10556 | 38 | 24 weeks | Obese | Live | Oral gavage | 5 × 109 | Daily | 10 weeks | Reduced body weight and fat mass; Improved hepatic and peripheral insulin sensitivity | [55] |
| B. uniformis CECT 7771 | 28 | 6–8 weeks | High-fat diet induced obesity | Live | Oral gavage | 5 × 108 | Daily | 7 weeks | Reduced body weight gain, liver steatosis; improved immune system and glucose oral tolerance | [56] |
| B. uniformis CECT 7771 | 30 | 6–8 weeks | Obese | Live | Oral gavage | 5 × 107 | Daily | 17 weeks | Body weight and adiposity reduction; improved oral glucose tolerance; reduced gut permeability, plasma cholesterol and triglycerides | [57] |
| B. uniformis CECT 7771 | 40 | 6–8 weeks | Obese | Centrifuged and re-suspended in 10% skimmed milk | Oral gavage | 1 × 108 | Daily | 14 weeks | Reduced body weight gain, plasma cholesterol, triglycerides, glucose and leptin | [58] |
| B. thetaiotaomicron DSM 2079 | 75 | 8 weeks | High-fat diet | Live | Oral gavage | 1 × 1010 | Daily | 8 days | Decrease of body weight, serum triglycerides, insulin | [59] |
| B. thetaiotaomicron VPI-5482 | 60 | 8 weeks | High-fat diet | Live and heat killed | Oral gavage | 5 × 108 | Three times a week | 7 weeks | Alleviated diet-induced body-weight gain and adiposity | [60] |
| F. prausnitzii A2–165 | 30 | 6 weeks | Asthma | Live, supernatant and dead | Oral gavage | 1 × 109 | Daily | 22 days | Decreased inflammation; increased fecal short-chain fatty acids | [61] |
| F. prausnitzii A2–165 (DSM 17677) or B. thetaiotaomicron VPI-5482 (ATCC 29148) | 64 | N.A | Gnotobiotic animals | Live | Oral gavage | B. thetaiotaomicron 1 × 107; F. prausnitzii 7 × 109 | Once a week | Until F. prausnitzii was established in a donor rat | Increased colonic mucus production | [62] |
| F. prausnitzii A2–165 | 80 | 6 weeks | Induced inflammation | Live | Intragastrical | 1 × 109 | Daily | 10 days | Reduction of inflammation | [63] |
| F. prausnitzii ATCC 27766 | 60 | N.A | Induced colitis | Live and supernatant concentrated | Oral gavage | 1 × 109 | Daily | 7 days | Reduced weight loss and inflammation in colitis | [64] |
| F. prausnitzii A2–165 | 96 | 6–8 weeks | Induced colitis | Bacterial strains or supernatant | Intragastrical | 1 × 109 | Daily | 7 days for sever protocol and 10 days for moderate protocol | Reduced weight loss and inflammation in colitis | [65] |
| F. prausnitzii ATCC27766 | 35 | 6 weeks | Induced colitis | Fresh and fresh culture supernatant | Oral gavage | 1 × 109 | Daily | 7 days | Reduced inflammation; increased short-chain fatty acids | [66] |
| F. prausnitzii A2-165; HTF-F | 50 | 2 months | Induced colitis | Live and its extracellular polymeric matrix | Intrarectal | 3 × 109 of F. prausnitzii; 50 µg of its extracellular polymeric matrix | Daily | For ten days prior the DSS exposure and during the eight days of DSS treatment | Attenuated clinical symptoms in DSS-colitis; decreased inflammation | [67] |
| F. prausnitzii strain N.A | 24 | 8 weeks | Diabetes | Purified microbial anti-inflammatory molecule (MAM) from F. prausnitzii | N.A | 200 μL at a concentration of 1 μg/μL | Daily | 4 weeks | Restoration of the intestinal barrier; decreased inflammation | [68] |
| F. prausnitzii strain N.A | 30 calves | Newborn | Healthy | Live culture | Oral gavage and intrarectal | 40 mL | One dose in the first week of life and a second dose 1 week later | 2 weeks | Decreased incidence of severe diarrhea and related mortality rate | [69] |
| F. prausnitzii A2–165 | 80 | 6–8 weeks | Acute induced colitis | Live and supernatant | Intragastrical | 1 × 109 | Daily | 10 days | Decreased intestinal permeability; decreased inflammation | [70] |
| F. prausnitzii A2–165 | 29 | 7–8 weeks | Gnotobiotic animals | Concentrated colture | Intragastrical and intrarectal | 1 × 109 | N.A | 4 weeks | Reduced weight loss and inflammation | [71] |
| F. prausnitzii ATCC 27766 | 18 | 8 weeks | High-fat diet | N.A | Intragastrical | 2 × 108 | Twice a week every 2 weeks | 13 weeks | Increased insulin sensitivity; decreased inflammation in the visceral adipose tissue | [72] |
| F. prausnitzii A2–165 | 102 | N.A | Radiation-induced inflammation | Live | Intragastrical | 1 × 109 | Daily | 6 days | Reduced severity of the histological damage and epithelial permeability | [73] |
| E. hallii L2–7 | 32 | 12 weeks | Obesity and diabetes | Active and heat-inactivated | Oral gavage | 1 × 108 | Daily | 4 weeks | Reduced blood glucose levels; reduced hepatic triglyceride levels; increased fecal butyrate | [74] |
| C. butyricum MIYAIRI 588 | 18 | 5 weeks | High-fat diet | Spores | Oral gavage | 1.4 × 109 | Daily | 12 weeks | Decreased plasma cholesterol levels and enhanced bile acid excretion | [75] |
| R. intestinalis DSMZ-14610 | 24 | 6 weeks | Induced colitis | Supernatant | Oral gavage | 0.2 mL of 5× concentrated growth supernatant | Daily | 7 days | Reduced intestinal inflammation; increased short-chain fatty acids | [76] |
| P. copri DSM 18205 | 12 | 12–14 weeks | High-fat/high-sucrose diet + fructo-oligosaccharides | Live | Oral gavage | N.A | Daily | 7 days | Improved glucose homeostasis and insulin tolerance | [77] |
| P. copri DSM 18205 | 20 | 6–8 weeks | Healthy | Live | Oral gavage | 1 × 108 | Daily | 4 weeks | Increased production of Th17 cells in the gut (improved immune response) | [78] |
| P. copri DSM 18205 | 10 | 10 to 12 weeks | High-fat diet | Live or heat-killed | Oral gavage | 1 × 108 | Daily | 1st experiment: 7 days 2nd:7 days 3rd: single gavage | Improved of glucose tolerance only with live P. copri | [79] |
| P. copri CB7 | 12 | 10 weeks | High-fat diet | Live | Oral gavage | 5 × 108 | Twice a week | 3 weeks | Increased insulin resistance | [80] |
| P. copri CB7 | N.A | N.A | Induced colitis | Live | Oral gavage | 1 × 107 | Single gavage | Single gavage | Increased inflammation, more severe colitis | [81] |
The mechanisms leading to these beneficial outcomes have not been fully elucidated yet. A primary role in mediating these effects was given to the protein Amuc_1100, present on the bacterium outer membrane, that seems to be able to interact with the intestinal Toll-like receptors (TRL2) and promote tight junctions occlusion, thus restoring the gut barrier function. Interestingly, some studies highlighted that the positive effects mediated by A. muciniphila supplementation were also obtained by the pasteurized bacterial cells [41, 49] or the purified Amuc_1100 protein [40, 49], supporting the important role played by the cell membrane components. In addition, a recent study identified a novel peptide secreted by A. muciniphila (named P9) that can improve glucose homeostasis and promote thermogenesis, thus counteracting obesity in high-fat fed mice [44].
To date, only one pilot A. muciniphila intervention study on human exists. Depommier et al. [43] carried out a randomized, double-blind, placebo-controlled study in overweight/obese volunteers with metabolic syndrome, that consumed live or pasteurized A. muciniphila (1010 CFU/day) for 3 months [43]. The authors demonstrated that both the formulas were safe and well tolerated by humans, and that the intervention reduced inflammation and improved insuline sensitivity, with the pasteurized bacteria showing a better effect than live cells [43]. Indeed, the use of the pasteurized A. muciniphila as novel food was recently approved by EFSA, making this species the first next-generation probiotic that will be soon available on the market (https://open.efsa.europa.eu/questions/EFSA-Q-2019-00767). This result will surely boost further investigations on this microbe as NGP directed to the prevention or treatment of diabetes and metabolic syndrome.
Faecalibacterium prausnitzii
Faecalibacterium prausnitzii is a Gram-positive bacterium belonging to the Ruminococcaceae family, also known as Clostridium cluster IV (phylum Firmicutes). F. prausnitzii is considered as extremely sensitive to oxygen and is the only isolated species of the Faecalibacterium genus [47]. However, a recent study based on genomes reconstruction from human gut metagenomes highlighted the presence of at least 12 different species commonly found in the human gut, most of them never isolated, and suggested the definition of Faecalibacterium complex [48]. The interest in F. prausnitzii is associated with its capacity to produce beneficial metabolites, mainly the short-chain fatty acid butyrate, that is known to play several health-promoting effects. SCFAs have an anti-inflammatory, anti-carcinogenic and immunomodulatory activity, it is an energy source for the colonocytes, and it can improve the metabolic syndrome [46, 82]. Consistently, F. prausnitzii is usually considered as a biomarker of intestinal health, since it is depleted in inflammatory states, such as IBD/IBS (Fig. 2) [46], while a diet rich in complex fiber can promote its growth [5, 8, 11]. Indeed, several trials on mice demonstrated a protective role of F. prausnitzii in experimentally induced colitis (Table 1). A treatment with F. prausnitzii or concentrated growth supernatant were able to reduce inflammation and tissue damage in mice with induced colorectal colitis [83–85]. In addition, F. prausnitzii gavage in high-fat fed mice was also associated with a reduction of visceral adipose tissue inflammation and fibrosis [86]. Besides butyrate, several other metabolites may be implicated in these beneficial effects. An uncharacterized peptide [66] or salicylic acid [64] were both identified in F. prausnitzii culture supernatant and were shown to exert an anti-inflammatory activity and to prevent colitis in mice. Nevertheless, contrasting results about this species are present in literature. In fact, higher F. prausnitzii abundance has been reported in allergic diseases [65, 72]. However, these discrepancies might be due to the presence of different and unidentified species/strains. As reported above, at least 12 different species closely related to F. prausnitzii were recently identified [48]. The same study also suggests that a misidentification of some F. prausnitzii strains likely occurred and some of them may belong to different species [48]. These species may be differently linked with health and disease [48]. In addition, different Faecalibacterium species may co-occur in the same subject. A decrease in Faecalibacterium diversity was found in obesity and inflammatory diseases, while the consumption of a diet rich in fiber may promote it [48]. These considerations should guide the development of NGPs, that should include more than one strain to take advantage of the wide diversity existing in this species. Therefore, although further investigations are needed, F. prausnitzii can be considered as a promising NGP for IBD/IBS and other inflammatory conditions.
Prevotella copri
Prevotella copri (Bacteroidetes phylum) is an obligate anaerobic Gram-negative rod and it is one of the dominant taxa in the human gut microbiome. P. copri is traditionally considered as a beneficial microbe, since it is often associated with a diet rich in fiber from vegetable products and normally shows higher levels in non-Western populations [87]. The interest in P. copri is due to the proposed positive effect in modulating glucose homeostasis, as recently demonstrated in a cohort of more than 1000 subjects [71]. Indeed, subjects with higher basal levels of P. copri showed higher glucose tolerance and insulin sensitivity upon a 3-day intervention with barley kernel fiber [88]. This mechanism seems to be linked with the ability to promote glycogen storage in the liver, probably activated by the production of succinate [89]. In addition, other studies demonstrated that a Prevotella-rich microbiome predisposes to higher weight loss [77, 79, 90, 91] or cholesterol decrease [92] upon the consumption of a fibre-rich diet. Consistently, mice gavaged daily with P. copri showed improved glycemic control [88, 89] (Table 1). However, also in this case literature data about the role of P. copri in relation to human health are contrasting [93]. Subjects with higher P. copri abundance reported higher serum levels of branched-chain amino acids (BCAA) that promote insulin resistance [94]. The same authors demonstrated that P. copri was able to produce BCAA and that mice fed with one P. copri strain for 3 weeks aggravated glucose tolerance, increased insulin resistance and showed higher circulating levels of BCAA [94] (Table 1). In addition, higher baseline abundance of P. copri was associated with a lower decrease in insulin resistance in obese subjects following a Mediterranean diet intervention [8]. P. copri was also linked with arthritis onset [95] and gavage with P. copri in mice with experimentally induced colitis exacerbated colitis gravity and inflammation [95] (Table 1). Interestingly, the same P. copri strain (P. copri CB7, Table 1) was tested in these two studies [94, 95], demonstrating that different strains may explicate totally opposite effects. Indeed, a recent study highlighted that different P. copri strains have a specific functional potential and may be selected by diet [96]. In addition, it was demonstrated the presence of at least four different species closely related to P. copri (P. copri complex) [97], suggesting that isolated strains previously identified as P. copri might belong to different species. Specific P. copri strains may be selected by diet [80, 96] and display a different polysaccharides utilization pattern [80]. Therefore, although P. copri might be a promising taxon to be used as NGP for glucose metabolism regulation, this beneficial activity cannot be generalized to all strains and further investigations are needed.
Bacteroides spp.
Bacteroides spp. are anaerobic, non-spore-forming, Gram-negative rods and some species (B. uniformis, B. fragilis, B. xylanisolvens, B. thetaiotaomicron) are considered interesting as NGP [81]. B. fragilis has been considered a pathogen for several years. Indeed, some B. fragilis strains can produce a zinc-dependent metalloprotease that is considered a toxin and can disrupt the intestinal mucosa. Therefore, according to the occurrence of the toxin-encoding gene bft, B. fragilis has been classified into two subgroups: non-enterotoxigenic (NTBF, lack of bft) and enterotoxigenic (ETBF, with bft) B. fragilis. Other pathogenic factors are associated with the presence of lipopolysaccharide (LPS) or ferritin that should also be considered in B. fragilis safety evaluation [98]. However, NTBF strains may exert several beneficial effects owing to an anti-inflammatory and immunomodulatory activity [99] (Table 1). This activity seems to be mediated by the production of a capsular polysaccharide A that showed these properties even when purified and administered to mice [100].
Among other Bacteroides species, B. uniformis and B. thetaiotaomicron were suggested as NGP for the management of metabolic syndrome, glucose homeostasis, and obesity in mice fed with high-fat diet (Table 1). Indeed, oral gavage with B. uniformis can reduce liver steatosis, weight gain, and immune dysfunctions associated with obesity [101], while an intervention with B. thetaiotaomicron reduced adiposity and weight gain [102]. However, a B. thetaiotaomicron isolate was reported to induce colitis in mice [103].
All these findings suggest that, although Bacteroides spp. are potentially interesting as NGP, the strains should be carefully evaluated for safety both in vitro and in vivo.
Eubacterium hallii
Eubacterium hallii (Firmicutes, Clostridium cluster XIVa) includes non-spore forming, obligately anaerobic rods and is considered a beneficial microorganism since it can produce several SCFAs [104], that play a major role in the modulation of gut inflammation, promoting epithelial integrity and regulating the immune response. Several studies report a decrease in E. hallii abundance in IBD/IBS and a reduction of SCFA producers, including Eubacterium, in diabetic subjects (Fig. 2) [56, 60]. Consistently, oral administration of E. hallii to obese and insulin-resistant mice improved insulin sensitivity and energy metabolism [105]. In addition, it was reported an increase in Eubacterium spp. and an improvement in insulin sensitivity after a fecal microbiota transplantation from lean to obese donors [106]. Although the mechanism was not yet fully elucidated, it seems that SCFA can bind to receptors, regulating satiety hormones such as ghrelin and glucagon-like peptide-1 (GLP-1), thus, inhibiting food intake [107].
Current issues and future paths
NPGs are attracting more and more interest both at academic and industrial research levels. However, several points should be addressed before proceeding to their introduction on the market.
First of all, wider and thorough studies about safety and tolerability of these novel microbial taxa need to be carried out, by both animal and human trials. Trials involving humans are still not available for most of the candidate NGPs and when performed, they are mainly exploratory, with small sample sizes and do not include sensitive populations (frailty subjects, elderly, or children). These studies should also consider that different subjects may show a specific response to the same strain. Indeed, the same drug, dietary treatment or probiotic supplementation may have a subject-specific effect, that may be caused by several factors, including genetics and gut microbiome composition. Therefore, a personalized application of NGPs should also be considered. In addition, an update in current regulation would be necessary. Indeed, the introduction of new taxa on the market may follow the novel foods framework or the pharmaceutical path, being commercialized as LBPs. In both cases, a thorough characterization of several strains from these new species will be required, including phenotypic and genomic analyses, with a focus on the research for the presence of genes related to antibiotic resistance, toxin production, virulence factors, and mobile elements. For this purpose, large-scale culturomics studies are extremely important [74, 108], not only to discover novel interesting strains, but also to highlight the wide diversity existing within each species and characterize the largest possible number of strains of the candidate NGP species. Finally, our knowledge about NGP mode of action is still scarce. In vitro and in vivo trials, as well as genomic screening, are needed, to understand the functional mechanisms leading to a positive effect on human health.
Another issue is related to NGP cultivation and stabilization for storage. Indeed, all these taxa are extremely sensitive to oxygen, much more than common probiotic LAB, that constitute the major hurdle to be overcome for their production and commercialization. Microbial biomass production usually takes place in bioreactors that can work anaerobically. However, guaranteeing strict anaerobiosis in the following phases, such as during microbial cells collection, freeze-drying and storage during the product shelf life, can be more challenging. In addition, the viability of the strains after the gastrointestinal passage should also be evaluated, as well as the number of cells to be assumed to obtain the desired effects. The use of appropriately designed coating systems might be tested to protect cell viability during shelf life and gastrointestinal transit [109].
Although there are several obstacles that need to be overcome before these products can be introduced into the probiotics products market, the development of NGPs hold promises for innovation in both food and pharmaceutical industry and it will be possible in following years as an output of interaction between research centers, regulatory boards, and industry.
Author contributions
DE and FDF conceived the review; FDF and AE researched data and prepared figures and table; FDF wrote the first draft; all authors reviewed and edited the manuscript before submission.
Funding
This study was supported by the project MASTER (Microbiome Applications for Sustainable food systems through Technologies and Enterprise). This project has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No 818368. This manuscript reflects only the authors’ views and the European Commission is not responsible for any use that may be made of the information it contains. The work was also supported by the projects Linking environmental pollution and gut microbiota in individuals living in contaminated settlements, funded by the Italian Ministry of Health (GR-2016-02362975) and PRIN2017-Microbiome-tailored food products based on typical Mediterranean Diet components, granted by the Italian Ministry of University and Research (20174FHBWR_005). A.E. PhD fellowship (PhD in Food Science, XXXVII cycle) was granted by the Italian Ministry of University within the Programme “PON R&I 2014-2020 - AZIONI IV.4 DOTTORATI E CONTRATTI DI RICERCA SU TEMATICHE DELL'INNOVAZIONE” (DOT1718749; CUP E65F21003630003).
Availability of data and materials
Not applicable.
Code availability
Not applicable.
Declarations
Conflict of interest
The authors declare that they do not have competing interests.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Manor O, Dai CL, Kornilov SA, Smith B, Price ND, Lovejoy JC, Gibbons SM, Magis AT. Health and disease markers correlate with gut microbiome composition across thousands of people. Nat Commun. 2020;11(1):5206. doi: 10.1038/s41467-020-18871-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fan Y, Pedersen O. Gut microbiota in human metabolic health and disease. Nat Rev Microbiol. 2021;19(1):55–71. doi: 10.1038/s41579-020-0433-9. [DOI] [PubMed] [Google Scholar]
- 3.De Filippis F, Vitaglione P, Cuomo R, Berni Canani R, Ercolini D. Dietary interventions to modulate the gut microbiome—how far away are we from precision medicine. Inflamm Bowel Dis. 2018;24(10):2142–2154. doi: 10.1093/ibd/izy080. [DOI] [PubMed] [Google Scholar]
- 4.Ecklu-Mensah G, Gilbert J, Devkota S. Dietary selection pressures and their impact on the gut microbiome. Cell Mol Gastroenterol Hepatol. 2021 doi: 10.1016/j.jcmgh.2021.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Filippis F, Pellegrini N, Vannini L, et al. High-level adherence to a Mediterranean diet beneficially impacts the gut microbiota and associated metabolome. Gut. 2016;65(1):63–72. doi: 10.1136/gutjnl-2014-308209. [DOI] [PubMed] [Google Scholar]
- 6.Wu GD, Compher C, Chen EZ, et al. Comparative metabolomics in vegans and omnivores reveal constraints on diet-dependent gut microbiota metabolite production. Gut. 2016;65(1):63–72. doi: 10.1136/gutjnl-2014-308209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Angelis M, Ferrocino I, Calabrese FM, et al. Diet influences the functions of the human intestinal microbiome. Sci Rep. 2020;10(1):4247. doi: 10.1038/s41598-020-61192-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meslier V, Laiola M, Roager HM, et al. Mediterranean diet intervention in overweight and obese subjects lowers plasma cholesterol and causes changes in the gut microbiome and metabolome independently of energy intake. Gut. 2020;69(7):1258–1268. doi: 10.1136/gutjnl-2019-320438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang DD, Nguyen LH, Li Y, et al. The gut microbiome modulates the protective association between a Mediterranean diet and cardiometabolic disease risk. Nat Med. 2021;27(2):333–343. doi: 10.1038/s41591-020-01223-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bolte LA, Vila AV, Imhann F, et al. Long-term dietary patterns are associated with pro-inflammatory and anti-inflammatory features of the gut microbiome. Gut. 2021;70(7):1287–1298. doi: 10.1136/gutjnl-2020-322670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deehan EC, Yang C, Perez-Muñoz ME, et al. Precision microbiome modulation with discrete dietary fiber structures directs short-chain fatty acid production. Cell Host Microbe. 2020;27(3):389–404. doi: 10.1016/j.chom.2020.01.006. [DOI] [PubMed] [Google Scholar]
- 12.Patnode ML, Beller ZW, Han ND, et al. Interspecies competition impacts targeted manipulation of human gut bacteria by fiber-derived glycans. Cell. 2019;179(1):59–73. doi: 10.1016/j.cell.2019.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ghosh TS, Rampelli S, Jeffery IB, et al. Mediterranean diet intervention alters the gut microbiome in older people reducing frailty and improving health status: the NU-AGE 1-year dietary intervention across five European countries. Gut. 2020;69(7):1218–1228. doi: 10.1136/gutjnl-2019-319654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kolodziejczyk AA, Zheng D, Elinav E. Diet–microbiota interactions and personalized nutrition. Nat Rev Microbiol. 2019;17(12):742–753. doi: 10.1038/s41579-019-0256-8. [DOI] [PubMed] [Google Scholar]
- 15.Leeming ER, Louca P, Gibson R, Menni C, Spector TD, Le Roy CI. The complexities of the diet–microbiome relationship: advances and perspectives. Genome Med. 2021;13(1):10. doi: 10.1186/s13073-020-00813-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zeevi D, Korem T, Zmora N, et al. Personalized nutrition by prediction of glycemic responses. Cell. 2015;163(5):1079–1094. doi: 10.1016/j.cell.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 17.Berry SE, Valdes AM, Drew DA, et al. Human postprandial responses to food and potential for precision nutrition. Nat Med. 2020;26(6):964–973. doi: 10.1038/s41591-020-0934-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hill C, Guarner F, Reid G, et al. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. 2014;11(8):506–514. doi: 10.1038/nrgastro.2014.66. [DOI] [PubMed] [Google Scholar]
- 19.Cowan CSM, Dinan TG, Cryan JF. Annual research review: critical windows—the microbiota-gut-brain axis in neurocognitive development. J Child Psychol Psychiatry. 2020;61(3):353–371. doi: 10.1111/jcpp.13156. [DOI] [PubMed] [Google Scholar]
- 20.Cryan JF, O’Riordan KJ, Cowan CSM, et al. The microbiota-gut-brain axis. Physiol Rev. 2019;99(4):1877–2013. doi: 10.1152/physrev.00018.2018. [DOI] [PubMed] [Google Scholar]
- 21.Hemarajata P, Versalovic J. Effects of probiotics on gut microbiota: mechanisms of intestinal immunomodulation and neuromodulation. Therap Adv Gastroenterol. 2013;6(1):39–51. doi: 10.1177/1756283X12459294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cunningham M, Azcarate-Peril MA, Barnard A, et al. Shaping the future of probiotics and prebiotics. Trends Microbiol. 2021;29(8):667–685. doi: 10.1016/j.tim.2021.01.003. [DOI] [PubMed] [Google Scholar]
- 23.Wall R, Cryan JF, Ross RP, Fitzgerald GF, Dinan TG, Stanton C. Bacterial neuroactive compounds produced by psychobiotics. Adv Exp Med Biol. 2014;817:221–239. doi: 10.1016/j.tim.2021.01.003. [DOI] [PubMed] [Google Scholar]
- 24.Roager HM, Licht TR. Microbial tryptophan catabolites in health and disease. Nat Commun. 2018;9(1):3294. doi: 10.1038/s41467-018-05470-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yahfoufi N, Alsadi N, Jambi M, Matar C. The immunomodulatory and anti-inflammatory role of polyphenols. Nutrients. 2018;10(11):1618. doi: 10.3390/nu10111618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.De Filippis F, Pasolli E, Ercolini D. The food-gut axis: lactic acid bacteria and their link to food, the gut microbiome and human health. FEMS Microbiol Rev. 2020;44(4):454–489. doi: 10.1093/femsre/fuaa015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khalesi S, Bellissimo N, Vandelanotte C, Williams S, Stanley D, Irwin C. A review of probiotic supplementation in healthy adults: helpful or hype? Eur J Clin Nutr. 2019;73(1):24–37. doi: 10.1038/s41430-018-0135-9. [DOI] [PubMed] [Google Scholar]
- 28.McFarland LV, Evans CT, Goldstein EJC. Strain-specificity and disease-specificity of probiotic efficacy: a systematic review and meta-analysis. Front Med. 2018;5:124. doi: 10.3389/fmed.2018.00124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.O’Toole PW, Marchesi JR, Hill C. Next-generation probiotics: the spectrum from probiotics to live biotherapeutics. Nat Microbiol. 2017;2:17057. doi: 10.1038/nmicrobiol.2017.57. [DOI] [PubMed] [Google Scholar]
- 30.Martín R, Langella P. Emerging health concepts in the probiotics field: streamlining the definitions. Front Microbiol. 2019;10:1047. doi: 10.3389/fmicb.2019.01047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Berry D, Stecher B, Schintlmeister A, et al. Host-compound foraging by intestinal microbiota revealed by single-cell stable isotope probing. Proc Natl Acad Sci USA. 2013;110(12):4720–4725. doi: 10.1073/pnas.1219247110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Derrien M, Belzer C, de Vos WM. Akkermansia muciniphila and its role in regulating host functions. Microb Pathog. 2017;106:171–181. doi: 10.1016/j.micpath.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 33.Zhou Q, Zhang Y, Wang X, et al. Gut bacteria Akkermansia is associated with reduced risk of obesity: evidence from the American Gut Project. Nutr Metab (Lond) 2020;17:90. doi: 10.1186/s12986-020-00516-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dao MC, Everard A, Aron-Wisnewsky J, et al. Akkermansia muciniphila and improved metabolic health during a dietary intervention in obesity: relationship with gut microbiome richness and ecology. Gut. 2016;65(3):426–436. doi: 10.1136/gutjnl-2014-308778. [DOI] [PubMed] [Google Scholar]
- 35.Stenman LK, Burcelin R, Lahtinen S. Establishing a causal link between gut microbes, body weight gain and glucose metabolism in humans towards treatment with probiotics. Benef Microbes. 2016;7(1):11–22. doi: 10.3920/BM2015.0069. [DOI] [PubMed] [Google Scholar]
- 36.Karcher N, Nigro E, Punčochář M, et al. Genomic diversity and ecology of human-associated Akkermansia species in the gut microbiome revealed by extensive metagenomic assembly. Genome Biol. 2021;22(1):209. doi: 10.1186/s13059-021-02427-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Everard A, Lazarevic V, Derrien M, Girard M, Muccioli GM, Neyrinck AM, Cani PD. Responses of gut microbiota and glucose and lipid metabolism to prebiotics in genetic obese and diet-induced leptin-resistant mice. Diabetes. 2011;60(11):2775–2786. doi: 10.2337/db11-0227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Everard A, Belzer C, Geurts L, Ouwerkerk JP, Druart C, Bindels LB, Cani PD. Cross-talk between Akkermansia muciniphila and intestinal epithelium controls diet-induced obesity. Proc Natl Acad Sci USA. 2013;110(22):9066–9071. doi: 10.1073/pnas.1219451110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reid DT, Eller LK, Nettleton JE, Reimer RA. Postnatal prebiotic fibre intake mitigates some detrimental metabolic outcomes of early overnutrition in rats. Eur J Nutr. 2015;55(8):2399–2409. doi: 10.1007/s00394-015-1047-2. [DOI] [PubMed] [Google Scholar]
- 40.Henning SM, Summanen PH, Lee RP, Yang J, Finegold SM, Heber D, Li Z. Pomegranate ellagitannins stimulate the growth of Akkermansia muciniphila in vivo. Anaerobe. 2017;43:56–60. doi: 10.1016/j.anaerobe.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 41.Van der Lugt B, Van Beek AA, Aalvink S, et al. Akkermansia muciniphila ameliorates the age-related decline in colonic mucus thickness and attenuates immune activation in accelerated aging Ercc1-/Δ7 mice. Immun Ageing. 2019;16:6. doi: 10.1186/s12979-019-0145-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Grajeda-Iglesias C, Durand S, Daillère R, et al. Oral administration of Akkermansia muciniphila elevates systemic antiaging and anticancer metabolites. Aging (Albany NY) 2021;13(5):6375–6405. doi: 10.18632/aging.202739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang L, Tang L, Feng Y, et al. A purified membrane protein from Akkermansia muciniphila or the pasteurised bacterium blunts colitis associated tumourigenesis by modulation of CD8+T cells in mice. Gut. 2020;69(11):1988–1997. doi: 10.1136/gutjnl-2019-320105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bian X, Wu W, Yang L, et al. Administration of Akkermansia muciniphila ameliorates dextran sulfate sodium-induced ulcerative colitis in mice. Front Microbiol. 2019;10:2259. doi: 10.3389/fmicb.2019.02259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhao S, Liu W, Wang J, et al. Akkermansia muciniphila improves metabolic profiles by reducing inflammation in chow diet-fed mice. J Mol Endocrinol. 2017;58(1):1–14. doi: 10.1530/JME-16-0054. [DOI] [PubMed] [Google Scholar]
- 46.Yoon HS, Cho CH, Yun MS, et al. Akkermansia muciniphila secretes a glucagon-like peptide-1-inducing protein that improves glucose homeostasis and ameliorates metabolic disease in mice. Nat Microbiol. 2021;6(5):563–573. doi: 10.1038/s41564-021-00880-5. [DOI] [PubMed] [Google Scholar]
- 47.Depommier C, Van Hul M, Everard A, Delzenne NM, De Vos WM, Cani PD. Pasteurized Akkermansia muciniphila increases whole-body energy expenditure and fecal energy excretion in diet-induced obese mice. Gut Microbes. 2020;11(5):1231–1245. doi: 10.1080/19490976.2020.1737307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Plovier H, Everard A, Druart C, et al. A purified membrane protein from Akkermansia muciniphila or the pasteurized bacterium improves metabolism in obese and diabetic mice. Nat Med. 2017;23(1):107–113. doi: 10.1038/nm.4236. [DOI] [PubMed] [Google Scholar]
- 49.Mulhall H, DiChiara JM, Deragon M, Iyer R, Huck O, Amar S. Akkermansia muciniphila and its pili-like protein Amuc_1100 modulate macrophage polarization in experimental periodontitis. Infect Immun. 2020;89(1):e00500–e520. doi: 10.1128/IAI.00500-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Huck O, Mulhall H, Rubin G, et al. Akkermansia muciniphila reduces Porphyromonas gingivalis-induced inflammation and periodontal bone. J Clin Periodontol. 2020;47(2):202–212. doi: 10.1111/jcpe.13214. [DOI] [PubMed] [Google Scholar]
- 51.Chelakkot C, Choi Y, Kim DK, et al. Akkermansia muciniphila-derived extracellular vesicles influence gut permeability through the regulation of tight junctions. Exp Mol Med. 2018;50(2):e450. doi: 10.1038/emm.2017.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hänninen A, Toivonen R, Pöysti S, et al. Akkermansia muciniphila induces gut microbiota remodelling and controls islet autoimmunity in NOD mice. Gut. 2018;67(8):1445–1453. doi: 10.1136/gutjnl-2017-314508. [DOI] [PubMed] [Google Scholar]
- 53.Li J, Lin S, Vanhoutte PM, Woo CW, Xu A. Akkermansia Muciniphila protects against atherosclerosis by preventing metabolic endotoxemia-induced inflammation in Apoe−/− Mice. Circulation. 2016;133(24):2434–2446. doi: 10.1161/CIRCULATIONAHA.115.019645. [DOI] [PubMed] [Google Scholar]
- 54.Sofi MH, Wu Y, Ticer T, et al. A single strain of Bacteroides fragilis protects gut integrity and reduces GVHD. JCI Insight. 2021;6(3):e136841. doi: 10.1172/jci.insight.136841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yang JY, Lee YS, Kim Y, et al. Gut commensal Bacteroides acidifaciens prevents obesity and improves insulin sensitivity in mice. Mucosal Immunol. 2017;10(1):104–116. doi: 10.1038/mi.2016.42. [DOI] [PubMed] [Google Scholar]
- 56.Gauffin Cano P, Santacruz A, Moya Á, Sanz Y. Bacteroides uniformis CECT 7771 ameliorates metabolic and immunological dysfunction in mice with high-fat-diet induced obesity. PLoS One. 2012;7(7):e41079. doi: 10.1371/journal.pone.0041079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.López-Almela I, Romaní-Pérez M, Bullich-Vilarrubias C, Benítez-Páez A, Gómez Del Pulgar EM, Francés R, Liebisch G, Sanz Y. Bacteroides uniformis combined with fiber amplifies metabolic and immune benefits in obese mice. Gut Microbes. 2021;13(1):1–20. doi: 10.1080/19490976.2020.1865706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fabersani E, Portune K, Campillo I, López-Almela I, Montserrat-de la Paz S, Romaní-Pérez M, Benítez-Páez SY. Bacteroides uniformis CECT 7771 alleviates inflammation within the gut-adipose tissue axis involving TLR5 signaling in obese mice. Sci Rep. 2021;11(1):11788. doi: 10.1038/s41598-021-90888-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Olli K, Saarinen MT, Forssten SD, Madetoja M, Herzig KH, Tiihonen K. Independent and combined effects of lactitol, polydextrose, and Bacteroides thetaiotaomicron on postprandial metabolism and body weight in rats fed a high-fat diet. Front Nutr. 2016;3:15. doi: 10.3389/fnut.2016.00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Liu R, Hong J, Xu X, et al. Gut microbiome and serum metabolome alterations in obesity and after weight-loss intervention. Nat Med. 2017;23(7):859–868. doi: 10.1038/nm.4358. [DOI] [PubMed] [Google Scholar]
- 61.Hu W, Lu W, Li L, Zhang H, Lee YK, Chen W, Zhao J. Both living and dead Faecalibacterium prausnitzii alleviate house dust mite-induced allergic asthma through the modulation of gut microbiota and short-chain fatty acid production. J Sci Food Agric. 2021;101(13):5563–5573. doi: 10.1002/jsfa.11207. [DOI] [PubMed] [Google Scholar]
- 62.Wrzosek L, Miquel S, Noordine ML. Bacteroides thetaiotaomicron and Faecalibacterium prausnitzii influence the production of mucus glycans and the development of goblet cells in the colonic epithelium of a gnotobiotic model rodent. BMC Biol. 2013;11:61. doi: 10.1186/1741-7007-11-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Laval L, Martin R, Natividad JN. Lactobacillus rhamnosus CNCM I-3690 and the commensal bacterium Faecalibacterium prausnitzii A2–165 exhibit similar protective effects to induced barrier hyper-permeability in mice. Gut Microbes. 2015;6(1):1–9. doi: 10.4161/19490976.2014.990784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Qiu X, Zhang M, Yang X, Hong N, Yu C. Faecalibacterium prausnitzii upregulates regulatory T cells and anti-inflammatory cytokines in treating TNBS-induced colitis. J Crohns Colitis. 2013;7(11):e558–e568. doi: 10.1016/j.crohns.2013.04.002. [DOI] [PubMed] [Google Scholar]
- 65.Martín R, Chain F, Miquel S, et al. The commensal bacterium Faecalibacterium prausnitzii is protective in DNBS-induced chronic moderate and severe colitis models. Inflamm Bowel Dis. 2014;20(3):417–430. doi: 10.1097/01.MIB.0000440815.76627.64. [DOI] [PubMed] [Google Scholar]
- 66.Zhang M, Qiu X, Zhang H, Yang X, Hong N, Yang Y, Chen H, Yu C. Faecalibacterium prausnitzii inhibits interleukin-17 to ameliorate colorectal colitis in rats. PLoS One. 2014;9(10):e109146. doi: 10.1371/journal.pone.0109146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rossi O, Khan MT, Schwarzer M, et al. Faecalibacterium prausnitzii strain HTF-F and its extracellular polymeric matrix attenuate clinical parameters in DSS-induced colitis. PLoS One. 2015;10(4):e0123013. doi: 10.1371/journal.pone.0123013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Xu J, Liang R, Zhang W, Tian K, Li J, Chen X, Yu T, Chen Q. Faecalibacterium prausnitzii-derived microbial anti-inflammatory molecule regulates intestinal integrity in diabetes mellitus mice via modulating tight junction protein expression. J Diabetes. 2020;12(3):224–236. doi: 10.1111/1753-0407.12986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Foditsch C, Pereira RVV, Ganda EK, Gomez MS, Marques EC, Santin T, Bicalho RC. Oral administration of Faecalibacterium prausnitzii decreased the incidence of severe diarrhea and related mortality rate and increased weight gain in preweaned dairy heifers. PLoS One. 2015;10(12):e0145485. doi: 10.1371/journal.pone.0145485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Martín R, Miquel S, Chain F, et al. Faecalibacterium prausnitzii prevents physiological damages in a chronic low-grade inflammation murine model. BMC Microbiol. 2015;15:67. doi: 10.1186/s12866-015-0400-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Miquel S, Leclerc M, Martin R, et al. Identification of metabolic signatures linked to anti-inflammatory effects of Faecalibacterium prausnitzii. MBio. 2015;6(2):e00300–e315. doi: 10.1128/mBio.00300-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Munukka E, Rintala A, Toivonen R. Faecalibacterium prausnitzii treatment improves hepatic health and reduces adipose tissue inflammation in high-fat fed mice. ISME J. 2017;11(7):1667–1679. doi: 10.1038/ismej.2017.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lapiere A, Geiger M, Robert V. Prophylactic Faecalibacterium prausnitzii treatment prevents the acute breakdown of colonic epithelial barrier in a preclinical model of pelvic radiation disease. Gut Microbes. 2020;12(1):1–15. doi: 10.1080/19490976.2020.1812867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Udayappan S, Manneras-Holm L, Chaplin-Scott A. Oral treatment with Eubacterium hallii improves insulin sensitivity in db/db mice. NPJ Biofilms Microbiomes. 2016;2:16009. doi: 10.1038/npjbiofilms.2016.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Seo M, Inoue I, Tanaka M, et al. Clostridium butyricum MIYAIRI 588 improves high-fat diet-induced non-alcoholic fatty liver disease in rats. Dig Dis Sci. 2013;58(12):3534–3544. doi: 10.1007/s10620-013-2879-3. [DOI] [PubMed] [Google Scholar]
- 76.Luo W, Shen Z, Deng M, et al. Roseburia intestinalis supernatant ameliorates colitis induced in mice by regulating the immune response. Mol Med Rep. 2019;20(2):1007–1016. doi: 10.3892/mmr.2019.10327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.De Vadder F, Kovatcheva-Datchary P, Zitoun C, Duchampt A, Bäckhed F, Mithieux G. Microbiota-produced succinate improves glucose homeostasis via intestinal gluconeogenesis. Cell Metab. 2016;24(1):151–157. doi: 10.1016/j.cmet.2016.06.013. [DOI] [PubMed] [Google Scholar]
- 78.Huang Y, Tang J, Cai Z, Zhou K, Chang L, Bai Y, Ma Y. Prevotella Induces the Production of Th17 Cells in the Colon of Mice. J Immunol Res. 2020;2020:9607328. doi: 10.1155/2020/9607328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kovatcheva-Datchary P, Nilsson A, Akrami R, et al. Dietary fiber-induced improvement in glucose metabolism is associated with increased abundance of Prevotella. Cell Metab. 2015;22(6):971–982. doi: 10.1016/j.cmet.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 80.Pedersen HK, Gudmundsdottir V, Nielsen HB, et al. Human gut microbes impact host serum metabolome and insulin sensitivity. Nature. 2016;535(7612):376–381. doi: 10.1038/nature18646. [DOI] [PubMed] [Google Scholar]
- 81.Scher JU, Sczesnak A, Longman RS, et al. Expansion of intestinal Prevotella copri correlates with enhanced susceptibility to arthritis. Elife. 2013;2:e01202. doi: 10.7554/eLife.01202.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Depommier C, Everard A, Druart C, et al. Supplementation with Akkermansia muciniphila in overweight and obese human volunteers: a proof-of-concept exploratory study. Nat Med. 2019;25(7):1096–1103. doi: 10.1038/s41591-019-0495-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lopez-Siles M, Duncan SH, Garcia-Gil LJ, Martinez-Medina M. Faecalibacterium prausnitzii: from microbiology to diagnostics and prognostics. ISME J. 2017;11(4):841–852. doi: 10.1038/ismej.2016.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.De Filippis F, Pasolli E, Ercolini D. Newly explored Faecalibacterium diversity is connected to age, lifestyle, geography, and disease. Curr Biol. 2020;30(24):4932–4943.e4. doi: 10.1016/j.cub.2020.09.063. [DOI] [PubMed] [Google Scholar]
- 85.Parada Venegas D, De la Fuente MK, Landskron G, et al. Short chain fatty acids (SCFAs)-mediated gut epithelial and immune regulation and its relevance for inflammatory bowel diseases. Front Immunol. 2019;10:277. doi: 10.3389/fimmu.2019.00277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ríos-Covián D, Ruas-Madiedo P, Margolles A, Gueimonde M, De Los Reyes-gavilán CG, Salazar N. Intestinal short chain fatty acids and their link with diet and human health. Front Microbiol. 2016;7:185. doi: 10.3389/fmicb.2016.00185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Quévrain E, Maubert MA, Michon C, et al. dentification of an anti-inflammatory protein from Faecalibacterium prausnitzii, a commensal bacterium deficient in Crohn’s disease. Gut. 2016;65(3):415–425. doi: 10.1136/gutjnl-2014-307649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.De Filippis F, Paparo L, Nocerino R, et al. Specific gut microbiome signatures and the associated pro-inflamatory functions are linked to pediatric allergy and acquisition of immune tolerance. Nat Commun. 2021;12:1–11. doi: 10.1038/s41467-021-26266-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Song H, Yoo Y, Hwang J, Na YC, Kim HS. Faecalibacterium prausnitzii subspecies-level dysbiosis in the human gut microbiome underlying atopic dermatitis. J Allergy Clin Immunol. 2016;137(3):852–860. doi: 10.1016/j.jaci.2015.08.021. [DOI] [PubMed] [Google Scholar]
- 90.Tett A, Pasolli E, Masetti G, Ercolini D, Segata N. Prevotella diversity, niches and interactions with the human host. Nat Rev Microbiol. 2021;19(9):585–599. doi: 10.1038/s41579-021-00559-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Asnicar F, Berry SE, Valdes AM, et al. Microbiome connections with host metabolism and habitual diet from 1098 deeply phenotyped individuals. Nat Med. 2021;27(2):321–332. doi: 10.1038/s41591-020-01183-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Christensen L, Roager HM, Astrup A, Hjorth MF. Microbial enterotypes in personalized nutrition and obesity management. Am J Clin Nutr. 2018;108(4):645–651. doi: 10.1093/ajcn/nqy175. [DOI] [PubMed] [Google Scholar]
- 93.Hjorth MF, Roager HM, Larsen TM, Poulsen SK, Licht TR, Bahl MI, Astrup A. Pre-treatment microbial Prevotella-to-Bacteroides ratio, determines body fat loss success during a 6-month randomized controlled diet intervention. Int J Obes. 2018;42(2):284. doi: 10.1038/ijo.2017.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hjorth MF, Blædel T, Bendtsen LQ, et al. Prevotella-to-Bacteroides ratio predicts body weight and fat loss success on 24-week diets varying in macronutrient composition and dietary fiber: results from a post-hoc analysis. Int J Obes. 2019;43(1):149–157. doi: 10.1038/s41366-018-0093-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ortega-Santos CP, Whisner CM. The key to successful weight loss on a high-fiber diet may be in gut microbiome Prevotella abundance. J Nutr. 2019;149(12):2083–2084. doi: 10.1093/jn/nxz248. [DOI] [PubMed] [Google Scholar]
- 96.Eriksen AK, Brunius C, Mazidi M, et al. Effects of whole-grain wheat, rye, and lignan supplementation on cardiometabolic risk factors in men with metabolic syndrome: a randomized crossover trial. Am J Clin Nutr. 2020;111(4):864–876. doi: 10.1093/ajcn/nqaa026. [DOI] [PubMed] [Google Scholar]
- 97.Claus SP. The strange case of Prevotella copri: Dr. Jekyll or Mr. Hyde? Cell Host Microbe. 2019;26(5):577–578. doi: 10.1016/j.chom.2019.10.020. [DOI] [PubMed] [Google Scholar]
- 98.De Filippis F, Pasolli E, Tett A, et al. Distinct genetic and functional traits of human intestinal Prevotella copri strains are associated with different habitual diets. Cell Host Microbe. 2019;25(3):444–4453.e3. doi: 10.1016/j.chom.2019.01.004. [DOI] [PubMed] [Google Scholar]
- 99.Tett A, Huang KD, Asnicar F, et al. The Prevotella copri complex comprises four distinct clades underrepresented in westernized populations. Cell Host Microbe. 2019;26(5):666–679.e7. doi: 10.1016/j.chom.2019.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Gálvez EJ, Iljazovic A, Amend L, et al. Distinct polysaccharide utilization determines interspecies competition between intestinal Prevotella spp. Cell Host Microbe. 2020;28(6):838–852.e6. doi: 10.1016/j.chom.2020.09.012. [DOI] [PubMed] [Google Scholar]
- 101.Douillard FP, de Vos WM. Biotechnology of health-promoting bacteria. Biotechnol Adv. 2019;37(6):107369. doi: 10.1016/j.biotechadv.2019.03.008. [DOI] [PubMed] [Google Scholar]
- 102.Sun F, Zhang Q, Zhao J, Zhang H, Zhai Q, Chen W. A potential species of next-generation probiotics? The dark and light sides of Bacteroides fragilis in health. Food Res Int. 2019;126:108590. doi: 10.1016/j.foodres.2019.108590. [DOI] [PubMed] [Google Scholar]
- 103.Wang C, Zhao J, Zhang H, Lee YK, Zhaia Q, Chen W. Roles of intestinal bacteroides in human health and diseases. Crit Rev Food Sci Nutr. 2020 doi: 10.1080/10408398.2020.1802695. [DOI] [PubMed] [Google Scholar]
- 104.Ramakrishna C, Kujawski M, Chu H, Li L, Mazmanian SK, Cantin EM. Bacteroides fragilis polysaccharide A induces IL-10 secreting B and T cells that prevent viral encephalitis. Nat Commun. 2019;10(1):2153. doi: 10.1038/s41467-019-09884-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hansen JJ, Huang Y, Peterson DA, Goeser L, Fan TJ, Chang EB, Sartor RB. The colitis-associated transcriptional profile of commensal Bacteroides thetaiotaomicron enhances adaptive immune responses to a bacterial antigen. PLoS One. 2012;7(8):e42645. doi: 10.1371/journal.pone.0042645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Engels C, Ruscheweyh HJ, Beerenwinkel N, Lacroix C, Schwab C. The common gut microbe Eubacterium hallii also contributes to intestinal propionate formation. Front Microbiol. 2016;7:713. doi: 10.3389/fmicb.2016.00713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Bach Knudsen KE. Microbial degradation of whole-grain complex carbohydrates and impact on short-chain fatty acids and health. Adv Nutr. 2015;6(2):206–213. doi: 10.3945/an.114.007450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Karlsson FH, Tremaroli V, Nookaew I, Bergström G, Behre CJ, Fagerberg B, Nielsen J, Bäckhed F. Gut meta-genome in European women with normal, impaired and diabetic glucose control. Nature. 2013;498(7452):99–103. doi: 10.1038/nature12198. [DOI] [PubMed] [Google Scholar]
- 109.Vrieze A, Van Nood E, Holleman F, et al. Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology. 2012;143(4):913–6.e7. doi: 10.1053/j.gastro.2012.06.031. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.
Not applicable.