ABSTRACT
We provide estimates for (I) annual herpes zoster (HZ) cases, (II) carbon costs related to healthcare utilization, and (III) annual carbon emissions due to HZ among ≥50 years of age (YOA) United States (US) population. We estimated the annual number of HZ cases in the US based on available incidence data and demographic data of individuals ≥50 YOA. Both the healthcare resource utilization (HCRU) associated with HZ cases and the unit carbon dioxide equivalent (i.e. CO2e) costs associated with each type of HCRU in the US were estimated based on literature and studies available online. The carbon footprint associated with HZ annually among US adults ≥50 YOA was estimated by multiplying the unit carbon estimates by the HCRU. In the US population aged ≥50 YOA in 2020 (i.e. approximately 118 million), approximately 1.1 million cases of HZ occur annually assuming no vaccination. Based on 2 sources of HCRU the average kgCO2e per HZ patient ranged from 61.0 to 97.6 kgCO2e, with values by age group ranging from 40.9 kgCO2e in patients aged 50–59 to 195.9 kgCO2e in patients ≥80 YOA. The total annual HZ associated carbon ranged between 67,000 and 107,000 tons of CO2e in the US population aged ≥50 YOA. The impact of HZ on carbon footprint in the US results in considerable greenhouse gas (GHG)emissions. Assuming no vaccination, the burden of HZ is projected to rise over the coming years with the aging populations consequently worsening its impact on GHG emissions. (Figure 1)
KEYWORDS: Herpes zoster, healthcare resource, environmental sustainability, climate change
Introduction
Increasing scientific evidence shows that changes in the climate and the natural world are impacting human health.1,2 The World Health Organization noted climate change as one of the biggest risks to human health and consequently addressing climate change as a key public health opportunity in improving human health.3 Healthcare and the provision of healthcare also contribute to greenhouse gas (GHG) emissions and climate change, and as such, may contribute negatively to a population’s health.2 The health impacts of environmental change are well recognized,4 however, the environmental footprint of the healthcare sector is less well documented.
Lenzen et al.2 provided a global assessment of the environmental footprint of health care.2 Several detailed country-specific reports suggest that the carbon footprint attributed to health care ranges from 2% in Indonesia to 10% in Russia, of the total national carbon footprint.2 As such, the healthcare sector has a vital role to play in climate change mitigation efforts, which will not only result in substantial reductions in GHG emissions, but can often lead to enhanced patient care, staff satisfaction, and cost savings.5
Carbon footprints are traditionally measured in terms of global warming potential (GWP). GWP is the heat absorbed by any greenhouse gas in the atmosphere, and quantified as carbon dioxide equivalent (CO2e), whereby for any other gas, CO2e is the mass of CO2 that would warm the earth as much as the mass of that gas. As such CO2e emissions include the effects of greenhouse gases such as CO2, methane (CH4) and nitrous oxide (N2O).6 Hospitals and pharmaceuticals are considered to be major contributors to healthcare carbon footprints.7 In particular, hospitals are highly energy intensive, consume large amounts of resources, and produce a large amount of waste.8
Very limited data is available on the impact of specific diseases on carbon footprints. Desterbecq et al. provide a summary of environmental impacts of various disease areas and healthcare products.9 The number of studies included in their review increased from 1 in 2004 to 10 in 2022. Several studies were carried out on vaccine preventable disease including pertussis, influenza, respiratory syncytial virus and COVID-19.10–13 In this manuscript we explore the carbon footprint associated with another vaccine-preventable disease, i.e. herpes zoster (HZ), focusing on adults aged ≥50 years of age (YOA) in the United States (US). HZ typically manifests as a unilateral, painful dermatomal rash (Figure 1).14 In the US, approximately 30% of the population will develop HZ during their lifetime.15 The median duration of HZ is approximately 30 days,16 but up to 30% of HZ patients develop postherpetic neuralgia (PHN), a chronic condition of debilitating pain that may last for months or even years and is very difficult to treat.17,18 HZ contributes annually to GHG emissions through healthcare visits and treatment (e.g., hospitalizations, physician visits, HZ medication). We present estimates of (I) the annual number of HZ cases in the US, (II) the unit carbon costs associated with healthcare utilization in the US and (III) the carbon associated with HZ annually in the US in population aged ≥50 YOA.
Figure 1.
Plain language summary.
Methods
The carbon footprint of HZ was estimated using data from published literature and national data sources from the US. The US population estimates by age were taken from the United Nations Department of Economic and Social Affairs population estimates.19 Incidence rates of HZ were based on the publication of Johnson et al.20 and health care resource utilization for patients with HZ taken from 2 alternative sources (I) Table 2 of Johnson et al.21 and (II) Table 2 of Meyers et al.22 All 3 studies used claims data from the Truven Health Analytics MarketScan Commercial Claims and Encounters database and the Medicare Supplemental and Coordination of Benefits database. The annual number of HZ cases in the US was calculated by multiplying the US age-group specific population estimates by the annual incidence rates of HZ.
Table 2.
Estimated unit of kgCo2e by facility.
| Energy |
Equipment (PPE) | Diagnostic procedures | Return transport | ||||
|---|---|---|---|---|---|---|---|
| Energy Type | Consumption(kWh/patient) | Emissions factor(kgCO2e/unit) | Emissions (kgCO2e) | ||||
| Hospitalisation per day | Natural Gas | 194.653 | 0.181 | 35.278 | 3.37 | 0.73 | 4.18 |
| Electricity | 182.995 | 0.413 | 75.541 | ||||
| Total | 110.82 | ||||||
| Emergency department | Natural Gas | 3.633 | 0.181 | 0.658 | 1.20 | 0.73 | 7.82 |
| Electricity | 3.368 | 0.413 | 1.390 | ||||
| Total | 2.05 | ||||||
| Primary care physician | Natural Gas | 0.089 | 0.181 | 0.016 | 2.87 | ||
| Electricity | 0.146 | 0.413 | 0.060 | ||||
| Total | 0.08 | ||||||
| Outpatient | Natural Gas | 0.213 | 0.181 | 0.039 | 4.18 | ||
| Electricity | 0.303 | 0.413 | 0.125 | ||||
| Total | 0.16 | ||||||
| Pharmacy | Natural Gas | 0.097 | 0.181 | 0.018 | |||
| Electricity | 0.156 | 0.413 | 0.065 | ||||
| Total | 0.08 | 3.57 | |||||
CO2e, carbon dioxide equivalent; PPE, personal protective equipment. See supplementary text for further details
Unit carbon cost of all healthcare treatment steps that a typical patient affected by HZ undergoes was calculated, e.g., based on the average time spent in each facility apportioned to the area utilized per patient, energy consumption, and personal protective equipment (PPE). The facilities included in the analysis were: hospital inpatient, hospital outpatient, emergency department, primary care physician and pharmacy. The carbon cost of transport was calculated based on the average time taken to get to each facility split by type of facility, population density of a region and/or population density split by rural, suburban and urban. The carbon cost accounted for the type of transport, distance and mode of transport to the medical facility. The average distance to each facility was estimated as follows: hospital 5.62 miles (assuming 10% of patients arrived from the emergency department); emergency department 11.89 miles; pharmacy 5.36 miles, primary care physician 4.3 miles.
The calculations were based on average consumption data across the US. The analysis was conducted from a healthcare perspective (i.e., including direct and non-direct medical CO2e costs). Further details are provided in the supplementary material text.23–53
The per HZ patient CO2e for each age group was estimated by summing over i the product of the healthcare resource utilization per HZ case for healthcare facility type i and age group a, from Johnson et al.21 and Meyers et al.22 respectively and the unit kgCO2e costs per healthcare facility type i for age group a:
The total annual CO2e was subsequently calculated by summing over a the product of the annual number of HZ cases for age group a, and the per patient CO2e for age group a: Total annual CO2e = ∑a (HZcasesa × Per HZ patient CO2ea)
Results
Applying the annual incidence rates to the US population ≥50 YOA (i.e. approximately 118 million in 2020 (see Table 1)) yields an estimate of approximately 1.1 million cases of HZ in 2020 assuming no vaccination.
Table 1.
Estimated number of annual herpes zoster cases by age group and overall.
| Age | Population | Annual incidence | Annual cases |
|---|---|---|---|
| 50–59 YOA | 42,120,077 | 0.00674 | 283,889 |
| 60–64 YOA | 20,669,143 | 0.00932 | 192,636 |
| 65–69 YOA | 17,819,027 | 0.00932 | 166,073 |
| 70–79 YOA | 24,082,597 | 0.01202 | 289,473 |
| 80+ YOA | 13,147,182 | 0.01278 | 168,021 |
| Total | 117,838,026 | 1,100,093 |
YOA, years of age.
The estimated unit kgCO2e for each facility is presented in Table 2. Note, each day of hospitalization is associated with 110.82 kgCO2e. It was estimated that on average the length of stay in hospital due to a HZ episode in individuals aged ≥50 years was 7.4 days (see text in Supplementary Material for more details).
Table 3 presents the estimated annual kgCO2e associated with HZ cases by age group and overall based on 2 alternative sources of healthcare resource utilization estimates. Based on the healthcare resource utilization (HCRU) estimates of Johnson et al.21 the average kgCO2e per HZ patient was estimated as 61.0, ranging from 40.9 kgCO2e in patients aged 50–59 to 121.7 kgCO2e in patients aged 80 years and older. Similarly, based on the HCRU estimates of Meyers et al.22 the average kgCO2e per HZ patient was estimated as 97.6, ranging from 63.6 kgCO2e in patients aged 50–59 to 195.9 kgCO2e in patients aged 80 and older. Based on these estimates, the overall emissions kgCO2e associated with HZ in the US in adults aged ≥50 years was approximately between 67,000 and 107,000 tons CO2e.
Table 3.
Estimated annual kgCo2e associated with herpes zoster cases by age group and overall.
| Based on Johnson et al.21 |
Based on Meyers et al.22 |
||||
|---|---|---|---|---|---|
| Age | HZ cases | Per patient kgCO2e | Total tons CO2e | Per patient kgCO2e | Total tons CO2e |
| 50–59 YOA | 283,889 | 40.9 | 11,602 | 63.6 | 18,052 |
| 60–64 YOA | 192,636 | 46.5 | 8,959 | 62.0 | 11,951 |
| 65–69 YOA | 166,073 | 51.4 | 8,538 | 73.2 | 12,159 |
| 70–79 YOA | 289,473 | 60.6 | 17,536 | 111.5 | 32,278 |
| 80+ YOA | 168,021 | 121.7 | 20,450 | 195.9 | 32,921 |
| Total | 1,100,093 | 61.0 | 67,085 | 97.6 | 107,362 |
CO2e, carbon dioxide equivalent; HZ, herpes zoster; kg, kilogram; YOA, years of age.
Figure 2 presents the percent annual kgCO2e associated with HZ cases by healthcare resource. Based on both sources of HCRU estimates, hospitalization is associated with the largest contribution of CO2e.
Figure 2.
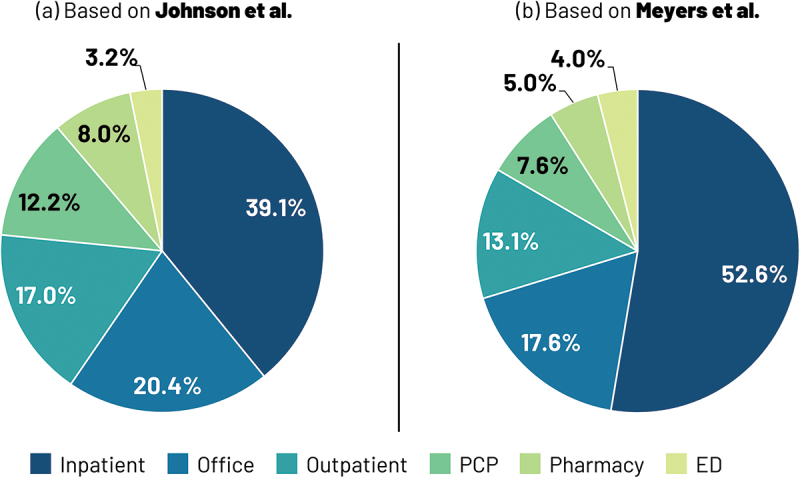
Annual total kgCo2e associated with herpes zoster cases by healthcare resource based on (a) Johnson et al.21 (b) Meyers et al.22
Note. ED, emergency department; PCP, primary care physician
Discussion
In this manuscript, we describe the first estimates of the healthcare related carbon footprint associated with HZ in the US in adults aged 50 years and older. We estimated 1.1 million cases of HZ annually, in line with previous publications,54–56 resulting in between 67,000 and 107,000 tons of CO2e in the US, which is equivalent to between 41,000 return flights and 65,000 return flights from London to New York.57
Many decision-making bodies, such as the National Health Service (NHS) in the United Kingdom, are putting in place plans and targets to make the healthcare sector, including hospitals, more sustainable.7 For example, several solutions are proposed to improve the environmental impact of hospitals, including engineering solutions to upgrade buildings; use of renewable energy and energy savings schemes; improved waste segregation facilities and recycling rates; travel and transport (e.g., use of public transport and cycle to work and lift-share schemes for staff); education on sustainability and waste management.
Given that transport is one of the main contributors to carbon emissions associated with HZ visits, alternative solutions such as telehealth could circumvent the need for face-to-face visits including emergency department, outpatient and/or primary care physician visits. It may be feasible for diagnosis and monitoring of HZ patients to be performed remotely thus reducing the carbon footprint associated with face-to-face visits.
The United Nations has developed 17 Sustainable Development Goals many of which are directly applicable to the health sector including: Good Health and Well-being, Affordable and Clean Energy, Industry, Innovation and Infrastructure, Sustainable Cities and Communities, Responsible Consumption and Reduction, Climate Action, Life on Land, and Partnerships for the Goals.58
As in other sectors and industries, progress needs to be tracked in the healthcare sector by integrating sustainability indices into existing forms of reporting (e.g., financial and healthcare outcomes reports). Integrated reporting allows better monitoring of progress and identification of areas of improvement. Life cycle analyses, e.g., of medical interventions, which provide in-depth reports of the energy and resources needed to create, package, ship, administer and dispose of an item, are substantially lacking for products in the medical field.59 The lack of measurable information often limits potential approaches to guide future improvements in the carbon footprint associated with an intervention.
In 2022 the United States signed into law the Inflation Reduction Act (IRA), which directs new federal spending toward reducing carbon emissions, including grants and incentives for lowering emissions.60 The IRA is projected to reduce US GHG emissions by 42% (3.3 Gigatons) by 2030, compared to 2005. A consequence of the legislation and ambitious targets is that evaluation of environmental impacts of disease and healthcare products is likely to be incorporated into future health technology assessment (HTA). Some HTA bodies, including Canada’s Drug and Health Technology Agency (CADTH) and the National Institute for Health and Care Excellence (NICE) in England, have developed guidance on how this may be achieved.61,62
HZ and related complications are estimated to result in approximately $1.3 billion in medical care costs annually in adults ≥50 YOA.63 HZ healthcare medical costs therefore represent approximately 0.03% of the total US national health expenditures (i.e.: $3.8 trillion).64 Given that US national health GHG emissions represents 7.9% of the total GHG emissions in the US (i.e. 5,981 million tons), our estimates of overall tons of CO2e associated with HZ in adults ≥50 YOA range from 0.01% to 0.02% of the total US national health GHG emissions (see text in Supplementary Material for more details).65,66 Assuming healthcare financial costs and healthcare environmental costs are correlated, this would suggest that our estimates are conservative, especially considering that the latter includes travel to healthcare facilities.
Assuming no vaccination, the burden of HZ is projected to rise over the coming years due to the aging populations.67 Zoster vaccines that substantially reduce the risk of HZ in older adults could be carbon saving given the small number of subjects (i.e., less than 10) who need to be vaccinated to prevent 1 HZ case.68,69
One limitation of our study is that calculations are based on average consumption data across the US, and may not be specific to a HZ patient, i.e., a HZ patient may have higher or lower CO2e consumption. A limitation of carbon footprint analyses is that although data is available overall for healthcare facilities, it is not always possible to separate out the carbon footprint for different disease types in particular where areas are shared for multiple disease types, e.g. where HZ, cardiovascular, diabetic, rheumatology patients share the same facilities (e.g. waiting areas/emergency rooms/wards, GP offices, clinics). In addition, we have not provided estimates broken down by health status, e.g. HZ patients without PHN/complications versus HZ patients with PHN or with other non-pain complications. The carbon footprint is likely to be 4 to 5 times higher in HZ patients with PHN/complications compared to HZ patients without PHN/complications, given the relative differences in healthcare resource utilization observed between those two groups.70
Another limitation of our study is that we focused on CO2e. Our study did not comprise a wider range of environmental indicators known to harm human health, e.g., scarce water use, air pollution, reactive nitrogen in water. On the rare occasions that US data was not available (e.g. waiting times) we used global or other country information (see text in Supplementary Material).
Conclusions
The impact and complications of HZ are substantial, particularly in older adults resulting in substantial greenhouse gas emissions. Assuming no vaccination, the burden of HZ is projected to rise over the coming years due to the aging populations, consequently worsening its impact on greenhouse gas emissions. Human health is intricately linked to the health of the planet we all share.
Supplementary Material
Acknowledgments
The authors would also like to thank the Business & Decision Life Sciences platform for editorial assistance and manuscript coordination.
Funding Statement
GlaxoSmithKline Biologicals SA funded this study [VEO-000026].
Disclosure statement
DC, JB and SW are employed by/hold shares in GSK. JB declares participation on a Data Safety Monitoring Board/Advisory Board and financial services from GSK, outside of the submitted work. IC is an employee of Carbon Trust, who was engaged by GSK to complete part of the work related to this manuscript. All authors declare no other financial and non-financial relationships and activities.
Role of the sponsor
GlaxoSmithKline Biologicals SA funded this study (VEO-000026) and took in charge all costs associated with the development and publication of this manuscript.
Author contributions
DC, JB and SW were involved in the conception and/or the design of the study and participated in the collection/generation of the study data. All authors had full access to the data and gave approval before submission. All authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The work described was carried out in accordance with the recommendations of the International Committee of Medical Journal Editors for conduct, reporting, editing, and publication of scholarly work in medical journals.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2024.2335722.
References
- 1.Costello A, Abbas M, Allen A, Ball S, Bell S, Bellamy R, Friel S, Groce N, Johnson A, Kett M, et al. Managing the health effects of climate change: lancet and University College London Institute for Global health Commission. Lancet. 2009;373(9676):1693–7. doi: 10.1016/S0140-6736(09)60935-1. [DOI] [PubMed] [Google Scholar]
- 2.Lenzen M, Malik A, Li M, Fry J, Weisz H, Pichler P-P, Chaves LSM, Capon A, Pencheon D.. The environmental footprint of health care: a global assessment. Lancet Planet Health. 2020;4(7):271–9. doi: 10.1016/S2542-5196(20)30121-2. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization . Climate change: an opportunity for public health; 2014. [accessed 2023 Jan 17]. https://www.who.int/news-room/commentaries/detail/climate-change-an-opportunity-for-public-health.
- 4.Landrigan PJ, Fuller R, Acosta NJR, Adeyi O, Arnold R, Basu N, Baldé AB, Bertollini R, Bose-O’Reilly S, Boufford JI, et al. The Lancet commission on pollution and health. Lancet. 2018;391(10119):462–512. doi: 10.1016/S0140-6736(17)32345-0. [DOI] [PubMed] [Google Scholar]
- 5.Tennison I, Roschnik S, Ashby B, Boyd R, Hamilton I, Oreszczyn T, Owen A, Romanello M, Ruyssevelt P, Sherman JD, et al. Health care’s response to climate change: a carbon footprint assessment of the NHS in England. Lancet Planet Health. 2021;5(2):84–92. doi: 10.1016/S2542-5196(20)30271-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gavurova B, Rigelsky M, Ivankova V.. Greenhouse gas emissions and health in the countries of the European Union. Front Public Health. 2021;9:756652. doi: 10.3389/fpubh.2021.756652.eCollection2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Health Service . Delivering a ‘Net zero’. National Health Service; 2020. [accessed 2023 Jan 17]. https://www.england.nhs.uk/greenernhs/wp-content/uploads/sites/51/2020/10/delivering-a-net-zero-national-health-service.pdf.
- 8.Malik A, Lenzen M, McAlister S, McGain F. The carbon footprint of Australian health care. Lancet Planet Health. 2018;2(1):27–35. doi: 10.1016/S2542-5196(17)30180-8. [DOI] [PubMed] [Google Scholar]
- 9.Desterbecq C, Tubeuf S. Inclusion of environmental spillovers in applied economic evaluations of healthcare products. Value Health. 2023;26(8):1270–81. doi: 10.1016/j.jval.2023.03.008. [DOI] [PubMed] [Google Scholar]
- 10.Terlinden A, Renson B, Ponder C, Poirrier JE, Curran D. Carbon cost-effectiveness of cocooning immunization against pertussis in England and wales: an ecological perspective. Value In Health. 2013;16(7):A578. doi: 10.1016/j.jval.2013.08.1575. [DOI] [Google Scholar]
- 11.Bozorgi A, Fahimnia B. Micro array patch (MAP) for the delivery of thermostable vaccines in Australia: a cost/benefit analysis. Vaccine. 2021;39(41):6166–73. doi: 10.1016/j.vaccine.2021.08.016. [DOI] [PubMed] [Google Scholar]
- 12.Hudson R, Rigoine de Fougerolles T, Leadley F, Chetty M, de la Tour P. HSD76 assessing the carbon intensity profile of an immunization program against RSV in infants in the United Kingdom to show the reduction in emissions versus standard of care. Value Health. 2023;26(12):S308. doi: 10.1016/j.jval.2023.09.1627. [DOI] [Google Scholar]
- 13.Signorini SG, Brugnoni D, Levaggi R, Garrafa E. Less is more: an ecological and economic point of view on appropriate use of lab testing for COVID-19 patients. Bioanalysis. 2021;13(24):1781–3. doi: 10.4155/bio-2021-0064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johnson RW, Bouhassira D, Kassianos G, Leplège A, Schmader KE, Weinke T. The impact of herpes zoster and post-herpetic neuralgia on quality-of-life. BMC Med. 2010;8(37). doi: 10.1186/1741-7015-8-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harpaz R, Ortega-Sanchez IR, Seward JF. Prevention of herpes zoster: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2008;57:1–30; quiz CE2–4. [PubMed] [Google Scholar]
- 16.Drolet M, Brisson M, Levin MJ, Schmader KE, Oxman MN, Johnson RW, Camden S, Mansi JA. A prospective study of the herpes zoster severity of illness. Clin J Pain. 2010;26(8):656–66. doi: 10.1097/AJP.0b013e3181eef686. [DOI] [PubMed] [Google Scholar]
- 17.Kawai K, Gebremeskel BG, Acosta CJ. Systematic review of incidence and complications of herpes zoster: towards a global perspective. BMJ Open. 2014;4(6):e004833. doi: 10.1136/bmjopen-2014-004833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cohen JI. Herpes zoster. N Engl J Med. 2013;369:255–63. doi: 10.1056/NEJMcp1302674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.United Nations Department of Economic and Social Affairs . World population prospects, standard projections; 2022. [accessed 2023 Jan 17]. https://population.un.org/wpp/Download/Standard/Population/.
- 20.Johnson BH, Palmer L, Gatwood J, Lenhart G, Kawai K, Acosta CJ. Annual incidence rates of herpes zoster among an immunocompetent population in the United States. BMC Infect Dis. 2015;15:502. doi: 10.1186/s12879-015-1262-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Johnson BH, Palmer L, Gatwood J, Lenhart G, Kawai K, Acosta CJ. Healthcare resource utilization and costs associated with herpes zoster in the US. J Med Econ. 2016;19:928–35. 10.1080/13696998.2016.1187150. [DOI] [PubMed] [Google Scholar]
- 22.Meyers JL, Madhwani S, Rausch D, Candrilli SD, Krishnarajah G, Yan S. Analysis of real-world health care costs among immunocompetent patients aged 50 years or older with herpes zoster in the United States. Hum Vaccine Immunother. 2017;13:1861–72. doi: 10.1080/21645515.2017.1324373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cohen B, Hyman S, Rosenberg L, Larson E. Frequency of patient contact with health care personnel and visitors: implications for infection prevention. J Comm J Qual Patient Saf. 2012;38:560–5. doi: 10.1016/S1553-7250(12)38073-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Becker G, Kempf DE, Xander CJ, Momm F, Olschewski M, Blum HE. Four minutes for a patient, twenty seconds for a relative - an observational study at a university hospital. BMC Health Serv Res. 2010;10(1):94. doi: 10.1186/1472-6963-10-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Friendly Power . Hospitals; 2020. [accessed 2023 Jan 19]. https://esource.bizenergyadvisor.com/article/hospitals.
- 26.Fairbanks P. Hospital energy use: taking advantage of energy efficiency; 2018. [accessed 2023 Jan 19]. https://electricenergyonline.com/energy/magazine/1147/article/Hospital-Energy-Use-Taking-Advantage-of-Energy-Efficiency.htm.
- 27.E source . Managing energy costs in hospitals; 2010. [accessed 2023 Jan 19]. https://www.dsoelectric.com/sites/dsoelectric/files/My%20Business/hospitals.pdf.
- 28.Bawaneh K, Ghazi Nezami F, Rasheduzzaman M, Deken B. Energy consumption analysis and characterization of hHealthcare facilities in the United States. Energies. 2019;12(19):3775. doi: 10.3390/en12193775. [DOI] [Google Scholar]
- 29.U.S. Energy Information Administration . Commercial buildings energy consumption survey. Energy characteristics and energy consumed in large hospital buildings in the United States in 2007; 2012. [accessed 2023 Jan 19]. https://www.eia.gov/consumption/commercial/reports/2007/large-hospital.php.
- 30.Skolnick C. Oversized healthcare: how did we get here and how do we right-size? 2013. [accessed 2023 Jan 19]. https://www.bdcnetwork.com/oversized-healthcare-how-did-we-get-here-and-how-do-we-right-size.
- 31.U.S. Energy Information Administration . Commercial buildings energy consumption survey. Electricity consumption totals and conditional intensities by building activity subcategories, 2012; 2012. [accessed 2023 Jan 19]. https://www.eia.gov/consumption/commercial/data/2012/c&e/cfm/pba4.php.
- 32.Dyrda L. 25 facts and statistics on emergency departments in the US; 2016. [accessed 2023 Jan 19]. http://www.designcollaborative.com/design-blog/hospital-planning-emergency-departments/.
- 33.Xie Z, Or C. Associations between waiting times, Service times, and patient satisfaction in an endocrinology outpatient department: a time study and questionnaire survey. Inquiry. 2017;54:46958017739527. doi: 10.1177/0046958017739527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Blakemore E. Why are wait times so long in emergency rooms? 2020. [accessed 2023 Jan 19]. https://www.washingtonpost.com/health/why-are-wait-times-so-long-in-emergency-rooms/2020/05/29/405204b8-a056-11ea-81bb-c2f70f01034b_story.html.
- 35.Maciag M. Emergency room wait times: state averages; 2015. [accessed 2023 Jan 19]. https://www.governing.com/archive/hospital-emergency-room-wait-times-by-state.html.
- 36.AIMS Education . US vs UK: Allied Healthcare at Home and Abroad; 2015. [accessed 2023 Jan 19]. https://aimseducation.edu/blog/us-vs-uk-allied-healthcare.
- 37.Hood L. Wait times remain stubbornly long in hospital emergency rooms; 2020. [accessed 2023 Jan 19]. https://theconversation.com/wait-times-remain-stubbornly-long-in-hospital-emergency-rooms-136314.
- 38.Esposito L. Enduring really long waits at the emergency room; 2015. [accessed 2023 Jan 19]. https://health.usnews.com/health-news/patient-advice/articles/2015/05/08/enduring-really-long-waits-at-the-emergency-room.
- 39.Finnegan J. Report outlines the business perils of long patient wait times; 2018. [accessed 2023 Jan 19]. https://www.fiercehealthcare.com/practices/ppatients-switched-doctors-long-wait-times-vitals.
- 40.Ahmad BA, Khairatul K, Farnaza A. An assessment of patient waiting and consultation time in a primary healthcare clinic. Malays Fam Physician. 2017;12:14–21. doi: 10.4066/AMJ.2014.1936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Irving G, Neves AL, Dambha-Miller H, Oishi A, Tagashira H, Verho A, Holden J. International variations in primary care physician consultation time: a systematic review of 67 countries. BMJ Open. 2017;7:e017902. doi: 10.1136/bmjopen-2017-017902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Michas F. Amount of time U.S. primary care physicians spent with each patient as of 2018; 2019. [accessed 2023 Jan 19]. https://www.statista.com/statistics/250219/us-physicians-opinion-about-their-compensation/.
- 43.Tai-Seale M, McGuire TG, Zhang W. Time allocation in primary care office visits. Health Serv Res. 2007;42:1871–94. doi: 10.1111/j.1475-6773.2006.00689.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hurt A. How much space do you really need? 2018. [accessed 2023 Jan 19]. https://www.physicianspractice.com/view/how-much-space-do-you-really-need.
- 45.Crist C. The doctor will see you now - but often not for long; 2017. [accessed 2023 Jan 19]. https://www.reuters.com/article/us-doctor-checkup-duration/the-doctor-will-see-you-now-but-often-not-for-long-idUSKBN1DS2Z2.
- 46.Young RA, Burge SK, Kumar KA, Wilson JM, Ortiz DF. A time-motion study of primary care physicians’ work in the electronic health record era. Fam Med. 2018;50:91–9. doi: 10.22454/FamMed.2018.184803. [DOI] [PubMed] [Google Scholar]
- 47.National Institute of Building Sciences . Clinic/Health unit; 2018. [accessed 2023 Jan 19]. https://www.wbdg.org/space-types/clinic-health-unit.
- 48.Wells JE. Efficient office design for a successful practice. Fam Pract Manag. 2007;14:46–50. [PubMed] [Google Scholar]
- 49.Oche M, Adamu H. Determinants of patient waiting time in the general outpatient department of a tertiary health institution in north Western Nigeria. Ann Med Health Sci Res. 2013;3:588–92. doi: 10.4103/2141-9248.122123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Janssen A, Kafetz A. What is the cost of outpatient appointments? 2020. [accessed 2023 Jan 19]. https://www.zpb-associates.com/what-is-the-cost-of-outpatient-appointments/.
- 51.International Health Facility Guidelines . Part B – health facility briefing & design, 245- outpatient unit; 2016. [accessed 2023 Jan 19]. https://healthfacilityguidelines.com/ViewPDF/ViewIndexPDF/iHFG_part_b_outpatients_unit.
- 52.Midmark . Rethink the outpatient clinical space: efficient exam room design; 2011. [accessed 2023 Jan 19]. https://cdn2.hubspot.net/hubfs/350655/White_Paper_Rethink_Outpatient_Clinical_Space_Rev_4_LR.pdf.
- 53.Cahnman S. Design guidelines for short-stay patient units; 2017. [accessed 2023 Jan 19]. https://www.hfmmagazine.com/articles/2841-design-guidelines-for-short-stay-patient-units.
- 54.Leung J, Harpaz R, Molinari N-A, Jumaan A, Zhou F. Herpes zoster incidence among insured persons in the United States, 1993–2006: evaluation of impact of varicella vaccination. Clin Infect Dis. 2011;52(3):332–40. doi: 10.1093/cid/ciq077. [DOI] [PubMed] [Google Scholar]
- 55.Cohen EJ, Jeng BH. Herpes zoster: a brief definitive review. Cornea. 2021;40(8):943–9. doi: 10.1097/ICO.0000000000002754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Harvey M, Prosser LA, Rose AM, Ortega-Sanchez IR, Harpaz R. Aggregate health and economic burden of herpes zoster in the United States: illustrative example of a pain condition. Pain. 2020;161(2):361–8. doi: 10.1097/j.pain.0000000000001718. [DOI] [PubMed] [Google Scholar]
- 57.Atmosfair . Emissions calculator; 2022. [accessed 2023 Jan 19]. https://www.atmosfair.de/en/standards/emissions_calculation/emissions_calculator/.
- 58.United Nations . Sustainable development goals: 17 goals to transform our world; [accessed 2023 Jan 19]. https://www.un.org/en/exhibits/page/sdgs-17-goals-transform-world.
- 59.Leonard N, McLean-Mandell R. A step toward environmental sustainability in mohs surgery. Dermatol surg. 2021;47:1504–5. doi: 10.1097/DSS.0000000000003169. [DOI] [PubMed] [Google Scholar]
- 60.Rajagopalan S, Landrigan PJ. The inflation reduction act – implications for climate change, air pollution, and health. Lancet Reg Health Am. 2023;23:100522. doi: 10.1016/j.lana.2023.100522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Canada’s Drug and Health Technology Agency . Reducing the environmental impact of clinical care; 2023. [accessed 2024 Mar 1]. https://www.cadth.ca/reducing-environmental-impact-clinical-care.
- 62.National Institute for Health and Care Excellence . NICE strategy 2021 to 2026; 2021. [accessed 2024 Mar 1]. https://www.nice.org.uk/Media/Default/Get-involved/Meetings-In-Public/Public-board-meetings/Mar-24-pbm-NICE-strategy-2021-2026.pdf.
- 63.McLaughlin JM, McGinnis JJ, Tan L, Mercatante A, Fortuna J. Estimated human and economic burden of four major adult vaccine-preventable diseases in the United States, 2013. J Prim Prev. 2015;36:259–73. doi: 10.1007/s10935-015-0394-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Centers for Disease Control and Prevention . Health expenditures; 2022. [accessed 2023 Jan 17]. https://www.cdc.gov/nchs/fastats/health-expenditures.htm.
- 65.Pichler P-P, Jaccard IS, Weisz U, Weisz H. International comparison of health care carbon footprints. Environ Res Lett. 2019;14:064004. 10.1088/1748-9326/ab19e1. [DOI] [Google Scholar]
- 66.U.S. Environmental Protection Agency . Overview of greenhouse gases; 2022. [accessed 2023 Jan 17]. https://www.epa.gov/ghgemissions/overview-greenhouse-gases.
- 67.Varghese L, Standaert B, Olivieri A, Curran D. The temporal impact of aging on the burden of herpes zoster. BMC Geriatr. 2017;17:30. doi: 10.1186/s12877-017-0420-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Curran D, Van Oorschot D, Matthews S, Hain J, Salem AE, Schwarz M. Long-term efficacy data for the recombinant zoster vaccine: impact on public health and cost effectiveness in Germany. Hum Vaccin Immunother. 2021;17:5296–303. doi: 10.1080/21645515.2021.2002085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Anderson TC, Masters NB, Guo A, Shepersky L, Leidner AJ, Lee GM, Kotton CN, Dooling KL. Use of recombinant zoster vaccine in immunocompromised adults aged ≥19 years: recommendations of the Advisory Committee on immunization practices - United States, 2022. Morb Mortal Wkly Rep. 2022;71:80–4. doi: 10.15585/mmwr.mm7103a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Yawn BP, Itzler RF, Wollan PC, Pellissier JM, Sy LS, Saddier P. Health care utilization and cost burden of herpes zoster in a community population. Mayo Clin Proc. 2009;84(9):787–94. doi: 10.4065/84.9.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


