Abstract
Background:
The purpose of this study was to conduct a systematic review on the cost-effectiveness of enhanced recovery after surgery (ERAS) protocols in abdominally based autologous breast reconstruction. Further, we reviewed the use of liposomal bupivacaine transversus abdominis plane (TAP) blocks in abdominal autologous reconstruction.
Methods:
PubMed, Embase, Cochrane, and Scopus were used for literature review, and PRISMA guidelines were followed. Included articles had full-text available, included cost data, and involved use of TAP block. Reviews, case reports, or comparisons between immediate and delayed breast reconstruction were excluded. Included articles were reviewed for data highlighting treatment cost and associated length of stay (LOS). Cost and LOS were further stratified by treatment group (ERAS versus non-ERAS) and method of postoperative pain control (TAP versus non-TAP). Incremental cost-effectiveness ratio (ICER) was used to compare the impact of the above treatments on cost and LOS.
Results:
Of the 381 initial articles, 11 were included. These contained 919 patients, of whom 421 participated in an ERAS pathway. The average ICER for ERAS pathways was $1664.45 per day (range, $952.70–$2860). Average LOS of ERAS pathways was 3.12 days versus 4.57 days for non-ERAS pathways. The average ICER of TAP blocks was $909.19 (range, $89.64–$1728.73) with an average LOS of 3.70 days for TAP blocks versus 4.09 days in controls.
Conclusions:
The use of ERAS pathways and postoperative pain control with liposomal bupivacaine TAP block during breast reconstruction is cost-effective. These interventions should be included in comprehensive perioperative plans aimed at positive outcomes with reduced costs.
Takeaways
Question: Are enhanced recovery after surgery (ERAS) protocols and liposomal bupivacaine transversus abdominis plane blocks cost-saving measures in patients undergoing abdominally based autologous breast reconstruction?
Findings: In this systematic review, multiple studies reported that patients who were enrolled in ERAS pathways or received liposomal bupivacaine transversus abdominis plane blocks experienced lower health care costs and shortened hospital length of stay compared with control groups.
Meaning: ERAS protocols and analgesic regimens involving liposomal bupivacaine transversus abdominal plane blocks can effectively prevent unnecessary spending and healthcare resource utilization in abdominally based autologous breast reconstruction.
INTRODUCTION
In recent years, health care systems have increasingly shifted toward value-based models in which patient outcomes are compared with overall cost of care.1 Therefore, there is a growing incentive for institutions to increase the cost-effectiveness of interventions. Breast reconstruction is a unique procedure because of the wide variety of interventions available depending on patient needs and preference.2 Although this lends more flexibility in a particular patient scenario, it can contribute to wide variations in cost between patients with similar presenting problems.2 Breast reconstruction is commonly performed after mastectomy for breast cancer, with 19% of these reconstructions coming from autologous donor sites.3 Although autologous breast reconstruction has been shown to achieve aesthetic results and is associated with higher patient satisfaction than implant-based techniques, autologous reconstruction has been linked to longer postoperative length of stay (LOS) when compared with alloplastic procedures.4–6 LOS is a metric that is being increasingly scrutinized in the shift to value-based models because it is directly correlated with cost.7 Enhanced recovery after surgery (ERAS) protocols are pathways used to achieve faster recovery after surgery.8
Implementing ERAS pathways encourages shorter postoperative LOS and lower postoperative morbidity in multidisciplinary surgical procedures.9 ERAS pathways aim to shorten recovery times without increased risk of readmission while improving cost and clinical efficiency.9 The multimodal perioperative care pathways involved in ERAS protocols optimize recovery after surgery by addressing influential postoperative outcomes associated with prolonged hospitalization.10 Although clinical implementations of ERAS pathways are variable, common interventions included in the protocols are preoperative consultations, multimodal analgesia, nausea and vomiting prophylaxis, venous thrombosis prophylaxis, intraoperative analgesia, and targeted discharge planning.11,12 Pain management methods in ERAS pathways, including the liposomal bupivacaine transversus abdominis plane (TAP) blocks, are easily performed, are cost-effective, and attempt to reduce postoperative opioid consumption.13
Published ERAS recommendations from the ERAS society for breast reconstruction include detailed preoperative counseling, minimized preoperative fasting, assessing for VTE risk, preoperative and intraoperative multimodal medications to mitigate postoperative nausea and vomiting, opioid-sparing postoperative pain management methods, mobilization within 24 hours, and others.8 In the present study, we performed a systematic review to (1) analyze cost efficiency of ERAS implementation after receiving either deep inferior epigastric perforator (DIEP), pedicle transverse rectus abdominal muscle (TRAM), free muscle-sparing TRAM (MS-TRAM), or latissimus dorsi flap during breast reconstruction procedures and (2) analyze cost efficiency of liposomal bupivacaine TAP block use.
METHODS
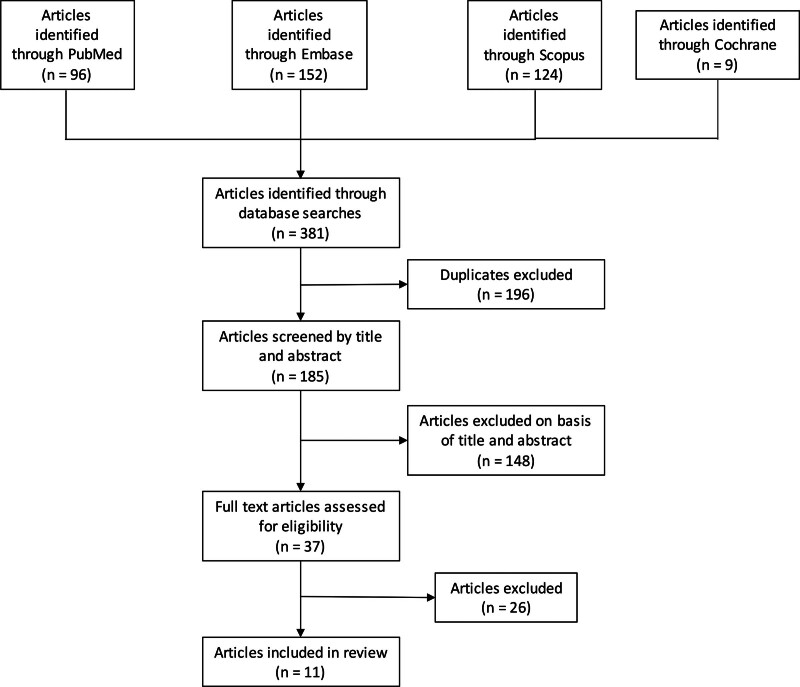
A systematic review was performed according to the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines to investigate cost analyses of ERAS pathways or TAP liposomal bupivacaine blocks. PubMed MEDLINE (National Library of Medicine), Embase (Elsevier), Cochrane (Wiley), and Scopus (Elsevier) were searched on September 9, 2022 from inception until present using keywords, including “ERAS” and “cost analysis” (Fig. 1). The protocol for this systematic review was not registered.
Fig. 1.
PRISMA flow diagram outlining article selection process.
All resultant articles were then filtered, and duplicates were excluded. Remaining articles were then screened by title and abstract for relevance. Articles proceeding to full-text review were screened for final inclusion (A.B., P.S., A.Y., M.A.L.), based on prespecified inclusion and exclusion criteria. Inclusion criteria included articles written or translated into the English language, with full-text available, use of DIEP, TRAM, MS-TRAM, or latissimus dorsi flap, use of liposomal bupivacaine TAP block, inclusion of cost data, or cost analysis. Exclusion criteria included articles that were conference abstracts with no full-text article, case reports (n = 1, n = 2), reviews, systematic reviews, meta-analyses, comparison between two different types of flaps or immediate and delayed reconstruction, and studies not meeting inclusion criteria. The primary outcome examined was incremental cost effectiveness ratio (ICER) of early discharge from hospital after either DIEP, TRAM, MS-TRAM, or latissimus dorsi flap; secondary outcome was ICER of liposomal bupivacaine TAP block use. Disagreements were reconciled before data extraction. Some included studies referred to their early discharge protocols as enhanced recovery pathways (ERP) or other unspecified clinical pathway, but all these pathways will be referred to as ERAS/ERP in this review.
All included articles were reviewed for bibliographic data, design, clinical data, intervention, and outcome data. Clinical data included variables such as flap used, LOS, pain regimen drugs and dosing, and cost-utility value (if reported). No meta-analysis was able to be performed due to heterogeneity of the data.
Statistical Analyses
Descriptive statistics were calculated using means, SDs, medians, and ranges using Microsoft Excel (Chicago, 2022). The ICER formulas for the primary and secondary outcome were calculated as follows:
ICER for primary (of early discharge from hospital following either DIEP, TRAM, MS-TRAM, or latissimus dorsi flap) outcome:
Control value was taken from patients not in the ERAS/ERP pathway.
ICER for secondary (of liposomal bupivacaine TAP block use after either DIEP, TRAM, MS-TRAM, or latissimus dorsi flap) outcome:
Control value was taken from patients who did not receive the liposomal bupivacaine TAP block and included patients either receiving no intervention,14 bupivacaine pain catheter,15 thoracic epidural,16 or injections of bupivacaine.17
Quality Assessment
Critical appraisal of included studies was conducted using the ROBINS-I18 and GRADE19 framework. A judgment for overall risk of bias for this systematic review was designated after weighing the risk of bias of included studies. (See table, Supplemental Digital Content 1, which displays characteristics and quality assessment of included studies. http://links.lww.com/PRSGO/D189.)
RESULTS
Demographics
The total number of patients who took part in the control pathway was 498, and the ERAS/ERP pathway was 421.
ERAS/ERP Pathway
The ICER calculated for ERAS/ERP pathway was an average of $1664.45 ± $851.28 per day and ranged from $952.70 per day to $2860 per day20–24 (Table 1). The LOS was an average of 3.12 ± 1.64 days in the ERAS/ERP pathways, and 4.57 ± 1.27 days in the control pathway.20–25
Table 1.
Average ICER and LOS for ERAS/ERP Pathways and TAP Block
| ERAS/ERP Pathways | ||
|---|---|---|
| Average ICER ($/Day) | Average LOS | |
| Control | — | 4.57 (1.27) |
| ERAS/ERP pathways | 1664.45 (851.28) | 3.12 (1.64) |
| TAP Block | ||
| Average ICER ($/Day) | Average LOS | |
| Control | — | 4.09 (0.22) |
| TAP block | 909.19 (1159.01) | 3.70 (0.30) |
Values shown as mean (SD).
ERAS/ERP pathway components differed across included studies. (See table, Supplemental Digital Content 2, which displays primary outcomes. http://links.lww.com/PRSGO/D190.) One common component included early discontinuation of the urinary catheter, either on POD122 or as soon as ambulation25 or adequate intake20 was possible. Another component included in several studies was early ambulation that either occurred on postoperative day 1,10,20 postoperative day 225 or as early as tolerated.22 In some cases, ambulation was even performed on the evening of surgery itself.23 Extensive preoperative counseling and education for patients was also a part of the pathway in multiple studies.10,21 This involved discussion of smoking cessation, healthy diet, weight stability, and glycemic control10,21 and avoidance of prolonged fasting.10 Other components of various pathways included immediate22 or postoperative day 123 start of general diet. With regard to analgesic regimens, many studies reported the use of multimodal analgesic regimens in their ERAS pathways and attempted to limit the use of patient-controlled analgesia (PCA) and opioid agents.20–23,26 Specific pharmacologic strategies included usage of acetaminophen, ketorolac, celecoxib, and gabapentin with opioids used in cases of breakthrough pain.20–23,26 Anti-emetics were also commonly used in the various pathways, and included agents such as scopolamine, dexamethasone, or ondansetron.20–23,26 Patients were also monitored with differing levels of care. Some studies used a Doppler check every hour for the first 24 hours with variability after this time point.20,25 In multiple studies, patients in control groups were sent directly to the surgical intensive care unit for up to 48 hours of monitoring.22,25 However, in multiple cases, patients in the ERAS pathway were sent directly to an inpatient unit or step-down unit for flap monitoring.20,22
An additional consideration when analyzing pathways and their impact on LOS is if a pedicled or free flap was used. This could potentially serve as a confounder; however, Hwang et al controlled for this in their analysis and still found that the addition of an ERAS pathway was independently associated with shorter LOS and reduced resource utilization.24 Although Stein et al included only patients with pedicled LD flaps and both patients in the ERAS and traditional group had shorter LOS than in other studies, the LOS was significantly lower in the ERAS group than in the traditional pathway (P = 0.003).21
Pain Control
The ICER calculated for use of a liposomal bupivacaine TAP block was an average of $909.19 ± $1159.01 per day and ranged from $89.64 per day to $1728.73 per day.14,17
The LOS was an average of 3.70 ± 0.30 days in the liposomal bupivacaine pathways and 4.09 ± 0.22 days in the control pathway.14–17 The control pathways used in the different studies included thoracic epidurals and traditional bupivacaine mixtures.16,17 Additionally, there was variation in TAP block procedure with studies using ultrasound14,16,17,25 or tactile confirmation,17 along with regional anesthesia pain teams16 or operating surgeons performing the TAP block.25
The cost of other pain management methods were bupivacaine ($3153.55), OnQ pump ($3686.21 and $3655.95).14,15 The ICER for these pain modalities was $−14,357 per day for the OnQ pump and $509.75 per day for the bupivacaine.14 (See table, Supplemental Digital Content 3, which displays secondary outcomes. http://links.lww.com/PRSGO/D191.) Usage of the TAP block resulted in decreased use of postoperative narcotics or PCA,10,25 with only 21% of TAP block patients requiring PCA postoperatively compared with 98% in the traditional recovery after surgery group.10 Moreover, Salibian et al found that TAP blocks were independent predictors of decreased total narcotic usage (P < 0.0001),17 and Knackstedt et al found that patients receiving TAP blocks with liposomal bupivacaine had significantly lower total postoperative narcotic utilization compared with the OnQ group (105.6 mg versus 165.4 mg, P = 0.005).15 On the other hand, Clary et al16 did not find a significant difference in total postoperative consumption of oral morphine equivalents (OME) between the TAP block liposomal bupivacaine group (205.4 OME) and the thoracic epidural group (253.1 OME). Another study reported that days of PCA use among patients in the ERAS/ERP pathway were lower at 2.83 days compared with 3.15 days in the control.24
Aside from PCA, another common modality of pain control is use of an OnQ pump (pain catheter) that was used in two included studies.14,15 Gatherwright et al14 reported that use of the OnQ pump resulted in a higher cost of stay than the control group ($3686.21 versus $3255.50) as well as little decrease in LOS (3.8 days versus 3.83 days, respectively). This same study reported that patients receiving a TAP block with liposomal bupivacaine compared with those receiving conventional bupivacaine via TAP block required less overall narcotic consumption (P = 0.002), had a decreased LOS (P = 0.08), and had similar overall costs (liposomal bupivacaine: $3215.16 versus bupivacaine: $3153.55). In Knackstedt et al,15 LOS did not differ between the TAP block and the OnQ pain catheter groups (both at 4 days) although the cost of the OnQ pain catheter was lower. Between these two studies, the cost of the OnQ pain catheter was similar at $3686 for Gatherwright et al14 and $3656 for Knackstedt et al.15 Jablonka et al25 used a nonnarcotic protocol and compared patients receiving no local analgesia, continuous bupivacaine infusion TAP catheters (OnQ pump model P400X4D, Halyard Health Global Headquarters, Alpharetta, Ga.), and a single-dose TAP blockade with liposomal bupivacaine solution. Their LOS in the single-dose liposomal bupivacaine TAP block was 2.65 versus 3.52 in the pain catheter group. Opioid consumption was significantly lower on postoperative day 1 and 2 for those with the TAP block and, although not significant, was still lower on postoperative day 3.25
DISCUSSION
The overall average ICER for the ERAS/ERP pathways was $1664.45, and LOS for the ERAS/ERP pathways was lower than the traditional pathway. These findings suggest that the ERAS/ERP pathways were more cost-effective and reduced the LOS for patients.
Differences in ERAS Pathways
An ERAS pathway for breast reconstruction has been established by the ERAS society,8 but in our review, ERAS/ERP pathway components differed across included studies.
One significant finding was the drastic decrease in cost between the ERAS/ERP protocol and control groups when preoperative counseling was paired with a comprehensive postoperative follow-up plan, including wound management and drain care from wound nurses. This pairing21 of interventions resulted in a $3200 decrease in cost of the ERAS/ERP pathway. The difference in LOS was also drastic, with protocol patients spending only one-third of a day in the hospital and control patients almost eight times that (2.4 days). This suggests that preoperative counseling and access to postoperative care like wound nurses can be extremely cost-effective and part of a successful ERAS/ERP protocol.
Approaches to Pain Management
The average ICER value for the use of a TAP block compared with other pain modalities was $909.19 ± $1159.01, indicating that this process was overall more cost-effective than the other pain modalities. LOS for TAP block patients was also on average lower than traditional pain methods. Notably, the SD for the ICER of TAP block was greater than the ICER value itself, indicating great variability in the cost of use of this block. The highest cost of stay for a TAP block patient was $1728.73 per day17 and lowest was $89.64 per day.14 Both studies were from the United States and published in the same year, although the former was performed in a New York City hospital, whereas the latter was in a Cleveland, Ohio hospital, which could potentially explain some of the discrepancy but does not account for the full difference.
In most cases, the TAP block was less expensive than the control pain treatment and resulted in a shorter LOS, suggesting that use of the TAP block can be a cost-effective form of pain relief postoperatively during breast reconstruction. In only one included study,14 the TAP block group costed more than the control by approximately $500 and reduced LOS by only 0.03 days, resulting in a negative ICER. This could also be a possible explanation for the high SD of the ICER values for the TAP block group.
One study24 provided detailed charges and relative value units for each of the separate services that account for cost of care (supplies, pharmacy, laboratory). With implementation of the ERAS/ERP pathway, the cost and relative value units were lower for all the aforementioned sections.
A study done in an ERAS pathway for laparoscopic colorectal surgery found that patients who received a TAP block had lower postoperative nausea and vomiting rates.27 They also reported that despite an opioid-sparing protocol in the ERAS pathway, there was no difference in pain intensity between the control and the ERAS pathway.27 For abdominally based autologous breast reconstruction, there is evidence from one RCT, two prospective cohort studies,28,29 and two retrospective studies24,30 that TAP blocks are safe and reduce postoperative opioid use. With TAP blocks being both safe and cost-effective, they should be considered as part of a comprehensive postoperative pain management plan for breast reconstruction independent of an ERAS/ERP pathway, although they should also be included in ERAS/ERP pathways.
Limitations
There are several limitations to this study. Most importantly, studies varied in study design, preventing standardization of data obtained. No meta-analysis was conducted, given heterogeneity in cost-reporting and protocols used. This prevented us from drawing statistically significant conclusions. Additionally, only published studies with full-text articles in the English-language were included, placing results at risk for publication bias and limiting data that may be published in a different language. Another key limitation is that many of the included studies span across many years with the use of historical controls, and thus, the groups may have received dynamically evolving postoperative care protocols. This may introduce unaccounted for advancements in technology that have the ability to impact the studied outcomes.
Some of the studies included were of low quality with high risk of bias due to methods and low sample sizes, introducing bias into this review. This is likely due to the low number of studies on the cost-effectiveness of ERAS/ERP pathways currently in the literature. More high-quality, large sample-size studies with rigorous methodology will help allay this gap in the literature.
Despite these limitations, we used the rigor of a systematic review to assess cost-effectiveness of ERAS/ERP pathways after breast reconstruction. To our knowledge, our study is the first to examine these outcomes and provides a valuable complement to existing studies examining the overall safety and cost-effectiveness of ERAS/ERP pathways to assist plastic surgeons in the management of this patient population.
CONCLUSIONS
Implementation of the ERAS/ERP pathways resulted in lower costs and decreased LOS compared with controls. This suggests that implementation of an ERAS/ERP pathway for breast reconstruction can be cost effective. The use of a TAP block as part of a multimodal analgesic protocol for breast reconstruction is also cost effective. ERAS/ERP pathways for breast reconstruction should be considered to help appropriately allocate healthcare resources and improve quality of care.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Supplementary Material
Footnotes
Published online 6 May 2024.
Presented in part at Midwestern Association of Plastic Surgeons 2023 in Lake Geneva, Wisconsin and at Plastic Surgery The Meeting 2023 in Austin, Texas.
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Teisberg E, Wallace S, O’Hara S. Defining and implementing value-based health care: a strategic framework. Acad Med. 2020;95:682–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sheckter CC, Matros E, Lee GK, et al. Applying a value-based care framework to post-mastectomy reconstruction. Breast Cancer Res Treat. 2019;175:547–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saldanha IJ, Broyles JM, Adam GP, et al. Autologous reconstruction after mastectomy for breast cancer. Plast Reconstr Surg Glob Open. 2022;10:e4181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pirro O, Mestak O, Vindigni V, et al. Comparison of patient-reported outcomes after implant versus autologous tissue breast reconstruction using the BREAST-Q. Plast Reconstr Surg Glob Open. 2017;5:e1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fischer JP, Nelson JA, Cleveland E, et al. Breast reconstruction modality outcome study: a comparison of expander/implants and free flaps in select patients. Plast Reconstr Surg. 2013;131:928–934. [DOI] [PubMed] [Google Scholar]
- 6.Frey JD, Salibian AA, Karp NS, et al. Examining length of hospital stay after microsurgical breast reconstruction: evaluation in a case-control study. Plast Reconstr Surg Glob Open. 2017;5:e1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Billig JI, Lu Y, Momoh AO, et al. A nationwide analysis of cost variation for autologous free flap breast reconstruction. JAMA Surg. 2017;152:1039–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Temple-Oberle C, Shea-Budgell MA, Tan M, et al. ; ERAS Society. Consensus review of optimal perioperative care in breast reconstruction: enhanced recovery after surgery (ERAS) society recommendations. Plast Reconstr Surg. 2017;139:1056e–1071e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Altman AD, Helpman L, McGee J, et al. ; Society of Gynecologic Oncology of Canada’s Communities of Practice in ERAS and Venous Thromboembolism. Enhanced recovery after surgery: implementing a new standard of surgical care. CMAJ. 2019;191:E469–E475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Afonso AM, McCormick PJ, Assel MJ, et al. Enhanced recovery programs in an ambulatory surgical oncology center. Anesth Analg. 2021;133:1391–1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Offodile AC, II, Gu C, Boukovalas S, et al. Enhanced recovery after surgery (ERAS) pathways in breast reconstruction: systematic review and meta-analysis of the literature. Breast Cancer Res Treat. 2019;173:65–77. [DOI] [PubMed] [Google Scholar]
- 12.Melnyk M, Casey RG, Black P, et al. Enhanced recovery after surgery (ERAS) protocols: time to change practice? Can Urol Assoc J. 2011;5:342–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Colonna AL, Bellows BK, Enniss TM, et al. Reducing the pain: a cost-effectiveness analysis of transversus abdominis plane block using liposomal bupivacaine for outpatient laparoscopic ventral hernia repair. Surg Open Sci. 2020;2:75–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gatherwright J, Knackstedt RW, Ghaznavi AM, et al. Prospective, randomized, controlled comparison of bupivacaine versus liposomal bupivacaine for pain management after unilateral delayed deep inferior epigastric perforator free flap reconstruction. Plast Reconstr Surg. 2018;141:1327–1330. [DOI] [PubMed] [Google Scholar]
- 15.Knackstedt R, Gatherwright J, Ghaznavi A, et al. Comparison of local anesthetic infusion pump bupivacaine versus transversus abdominis plane (TAP) block liposomal bupivacaine for pain management after bilateral deep inferior epigastric perforator free flap reconstruction. J Plast Reconstr Aesthet Surg. 2017;70:1779–1781. [DOI] [PubMed] [Google Scholar]
- 16.Clary Z, Nazir N, Butterworth J. Transversus abdominis plane block with liposomal bupivacaine versus thoracic epidural for postoperative analgesia after deep inferior epigastric artery perforator flap-based breast reconstruction. Ann Plast Surg. 2020;85:e24–e26. [DOI] [PubMed] [Google Scholar]
- 17.Salibian AA, Frey JD, Thanik VD, et al. Transversus abdominis plane blocks in microsurgical breast reconstruction: analysis of pain, narcotic consumption, length of stay, and cost. Plast Reconstr Surg. 2018;142:252e–263e. [DOI] [PubMed] [Google Scholar]
- 18.Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brozek JL, Canelo-Aybar C, Akl EA, et al. ; GRADE Working Group. GRADE Guidelines 30: the GRADE approach to assessing the certainty of modeled evidence—an overview in the context of health decision-making. J Clin Epidemiol. 2021;129:138–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.O’Neill AC, Mughal M, Saggaf MM, et al. A structured pathway for accelerated postoperative recovery reduces hospital stay and cost of care following microvascular breast reconstruction without increased complications. J Plast Reconstr Aesthet Surg. 2020;73:19–26. [DOI] [PubMed] [Google Scholar]
- 21.Stein MJ, Frank SG, Lui A, et al. Ambulatory latissimus dorsi flap breast reconstruction: a prospective cohort study of an enhanced recovery after surgery (ERAS) protocol. J Plast Reconstr Aesthet Surg. 2019;72:1950–1955. [DOI] [PubMed] [Google Scholar]
- 22.Oh C, Moriarty J, Borah BJ, et al. Cost analysis of enhanced recovery after surgery in microvascular breast reconstruction. J Plast Reconstr Aesthet Surg. 2018;71:819–826. [DOI] [PubMed] [Google Scholar]
- 23.Kaoutzanis C, Ganesh Kumar N, O’Neill D, et al. Enhanced recovery pathway in microvascular autologous tissue-based breast reconstruction: should it become the standard of care? Plast Reconstr Surg. 2018;141:841–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hwang TG, Wilkins EG, Lowery JC, et al. Implementation and evaluation of a clinical pathway for TRAM breast reconstruction. Plast Reconstr Surg. 2000;105:541–548. [DOI] [PubMed] [Google Scholar]
- 25.Jablonka EM, Lamelas AM, Kim JN, et al. Transversus abdominis plane blocks with single-dose liposomal bupivacaine in conjunction with a nonnarcotic pain regimen help reduce length of stay following abdominally based microsurgical breast reconstruction. Plast Reconstr Surg. 2017;140:240–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Afonso A, Oskar S, Tan KS, et al. Is enhanced recovery the new standard of care in microsurgical breast reconstruction? Plast Reconstr Surg. 2017;139:1053–1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pirrera B, Alagna V, Lucchi A, et al. Transversus abdominis plane (TAP) block versus thoracic epidural analgesia (TEA) in laparoscopic colon surgery in the ERAS program. Surg Endosc. 2018;32:376–382. [DOI] [PubMed] [Google Scholar]
- 28.Zhong T, Wong KW, Cheng H, et al. Transversus abdominis plane (TAP) catheters inserted under direct vision in the donor site following free DIEP and MS-TRAM breast reconstruction: a prospective cohort study of 45 patients. J Plast Reconstr Aesthet Surg. 2013;66:329–336. [DOI] [PubMed] [Google Scholar]
- 29.Hivelin M, Wyniecki A, Plaud B, et al. Ultrasound-guided bilateral transversus abdominis plane block for postoperative analgesia after breast reconstruction by DIEP flap. Plast Reconstr Surg. 2011;128:44–55. [DOI] [PubMed] [Google Scholar]
- 30.Wheble GA, Tan EK, Turner M, et al. Surgeon-administered, intra-operative transversus abdominis plane block in autologous breast reconstruction: a UK hospital experience. J Plast Reconstr Aesthet Surg. 2013;66:1665–1670. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.