Abstract
Multiple evanescent white dot syndrome (MEWDS) is a rare fundus disease, characterized by acute vision loss and visual field defects. Many previous studies have explained the possible pathogenesis and clinical features of primary MEWDS. However, as the number of reported cases increases, secondary MEWDS occurs in other related retinal diseases and injuries, exhibiting some special characteristics. The associated retinal diseases include multifocal choroiditis/punctate inner choroidopathy (MFC/PIC), acute zonal occult outer retinopathy, best vitelliform macular dystrophy, pseudoxanthoma elasticum, and ocular toxoplasmosis. The related retinal injury is laser photocoagulation, surgery, and trauma. Although primary MEWDS often have a self-limiting course, secondary MEWDS may require treatment in some cases, according to the severity of concomitant diseases and complications. Notably, MEWDS secondary to MFC/PIC that is prone to forming choroidal neovascularization and focal choroidal excavation, needs positive treatment with corticosteroids. The possible underlying pathogenesis of secondary MEWDS is the exposure of choroidal antigen after the disruption of Bruch's membrane. The MEWDS-related features in secondary MEWDS are still evanescent under most circumstances. Its prognosis and treatment depend on the severity of complications. Current studies propose that the etiology is associated with immune factors, including viral infection, inflammation in choroid and Bruch's membrane, and antigen exposure caused by retinal and/or choroidal insults. More pathogenic studies should be conducted in the future. Accurate diagnosis for secondary MEWDS could benefit patients in aspects of management and prognosis.
Keywords: multiple evanescent white dot syndrome, punctate inner choroidopathy, multifocal choroiditis, secondary multiple evanescent white dot syndrome
INTRODUCTION
Multiple evanescent white dot syndrome (MEWDS) is an evanescent and multifocal chorioretinopathy first reported by Jampol et al[1] in 1984. This disorder typically occurs in young healthy individuals, particularly in women, with its incidence estimated to be 0.22 per 100 000 population annually[2]–[3]. Patients with MEWDS usually present with multiple symptoms, such as moderate-to-severe vision loss, photopsia, and enlargement of physiologic scotoma. Clinically, MEWDS (primary MEWDS) is typically characterized by small white dots at the deep retina of the posterior pole and peripheral retina, papillary edema, foveal granularity, and retinal vascular sheathing[2]. Sometimes vitreous inflammation also could be observed (Figure 1)[4]. In addition, more than half of patients have myopia. Approximately 50% of patients have a history of respiratory tract infection, viral infection, vaccination, or show prodromes of systematic infection before the occurrence of MEWDS (about 4wk before onset)[1],[5]–[8].
Figure 1. Anterior segment photographs of a 25-year-old female who complained of decreased vision with fixed scotoma for one week and presented with vitreous cells in the right eye (A and B).

She was diagnosed with MEWDS in the right eye. MEWDS: Multiple evanescent white dot syndrome.
The etiology of MEWDS remains elusive. It is suspected that MEWDS is associated with viral infection. The diagnosis primarily relies on medical history, clinical features, and ancillary multimodal imaging (MMI)[9]. Generally, MEWDS exhibits a self-limiting course with a duration of 6 to 8wk, mostly without permanent complications. Therefore, local/retinal steroids and/or systemic steroid therapy have not been regularly recommended, except for some complications that require symptomatic treatment and related supportive therapy[2]. With the rapid advancement of diagnostic techniques and profound awareness of the disease, more and more patients with MEWDS secondary to or cooccurring with other retinal diseases or ocular events have been reported in the era of MMI. Essilfie et al[10] recently proposed a term, secondary MEWDS, that may be triggered by a macular disease or iatrogenic injury, distinguishing from the primary MEWDS described by Jampol[1]. Secondary MEWDS refers to classical MEWDS features triggered by choroidal antigen exposure after varied causes and diseases possibly disrupting the retinal pigment epithelium-Bruch membrane-choriocapillaris-complex (RPE-BrM-CC)[11]–[14]. They believed that secondary MEWDS seems to be an epiphenomenon that may be seen in diseases disruptive to RPE-BrM-CC. On our review of current literature, secondary MEWDS could be seen in other else white dot syndromes[15]–[19], such as punctate inner choroidopathy (PIC), multifocal choroiditis (MFC), acute zonal occult outer retinopathy (AZOOR), and etc., retinal diseases like best vitelliform macular dystrophy (BVMD), pseudoxanthoma elasticum (PXE), and retinal insults induced by ocular events (history of scleral buckle for retinal detachment, idiopathic retinochoroiditis, traumatic subretinal hemorrhage, choroidal rupture, penetrating trauma of the fellow eye or the choroid insults)[20]–[25]. What's more, MEWDS secondary to MFC/PIC is prone to form focal choroidal excavation (FCE)[26]–[28] and choroidal neovascularization (CNV)[23],[29]–[34]. In secondary MEWDS, the manifestations affiliated with primary MEWDS are still evanescent, and treatment and prognosis depend on the severity of concomitant diseases. Herein, the accurate diagnosis of secondary MEWDS can guide the treatment and evaluation of prognosis to avoid severer complications. In this article, we summarized the features, clinical manifestations, and possible pathogenesis of secondary MEWDS in the aforementioned entities.
Overview of Primary Multiple Evanescent White Dot Syndrome
It is necessary to have an understanding of primary MEWDS before describing secondary MEWDS. The primary MEWDS commonly occurs in young and mid-aged females. The male-to-female ratio is 1:5. The patients often present with acute or subacute vision loss, enlarged blind spots, photopsia, and floaters. We reviewed previous studies and reports about MEWDS and summarized the imaging features in different examinations as follows: 1) Color fundus photograph (CFP) shows that multifocal, round, and grayish-white spots, 100-200 µm in diameter, were located in proximity to areas of the posterior pole, macula, and optic disc. The lesions could extend from the posterior pole to the mid-peripheral retina at occurrence (Figure 2) and fade from the periphery to the posterior pole in the phase of resolution (Figure 3). Foveal granularity is another characteristic manifestation of CFP and is associated with the unique anatomical structure of the fovea[2],[35]–[37]. 2) Fluorescein angiography (FFA) helps the diagnosis of MEWDS. Early FFA shows varying sizes of tip-like hyperfluorescence arranged in a wreath-like shape in 80% of patients. On late FFA, no significant fluorescence leaks from the capillaries around the disc. The hyperfluorescence of the optic disc is noted in a few patients[2],[35],[38]. Finn and Khurana[39] first defined the lesions in MEWDS as dots and spots on FFA and indocyanine green angiography (ICGA). They defined dots as small lesions of approximately 100 µm and spots as larger lesions of more than 200 µm. Dots are correlated to the wreath-like hyperfluorescence on early FFA, and spots showed ill-defined and uneven hyperfluorescence on FFA (Table 1). 3) ICGA is also a significant auxiliary examination to provide better visualization of choroidal vessels. Early-ICGA shows no abnormalities of choroidal background fluorescence and medium-to-large vessels. But in the middle and late stages (after roughly 10min), multiple and scattered hypofluorescent spots in varying sizes and with poorly-defined borders were seen in the macula and mid-peripheral choroid as well as around the optic disc, surrounded by a light gray halo in the boundary. Subsequently, the hypofluorescence was fused in sheet-like patterns on late-ICGA[2]. 4) Fundus autofluorescence (FAF) imaging is a rapid and noninvasive technique to evaluate retinal pigment epithelium (RPE) function. On FAF, mottled and scattered hyperautofluorescent lesions are in the vicinity of the optic disc and in the posterior pole with scattered hyperautofluorescent dots at the edges of lesions. 5) Optical coherence tomography (OCT) is an important and non-invasive tool to observe the structure of the retina in vivo. The OCT shows disruption of the ellipsoid zone (EZ) in the fovea and dome-like accumulation of subretinal hyperreflective material (SHRM) overlying RPE. The SHRM has been considered debris of the insulted outer segments in previous studies. En-face OCT noted the dots in the outer nuclear layer and spots in the EZ/interdigitation zone (IZ), and also show ‘dots on spots’ in proximity to the optic disc (Figure 4)[2]. 6) OCT angiography (OCTA) is an advanced imaging technique to produce high-resolution images of blood flow of all the vascular layers in a rapid and non-invasive fashion[40]–[41]. In the acute phase of MEWDS, OCTA shows completely normal choriocapillary morphology. The hypofluorescent areas on ICGA also show no dilation or occlusion of choriocapillary, inferring that the lesions in the acute phase of MEWDS are limited to the outer segment of the photoreceptor[42]. 7) The visual field examination exhibits an enlarged physiological scotoma in MEWDS. The aforementioned imaging features help us make an acute diagnosis clinically.
Figure 2. Ultrawide fundus images of a 33-year-old female who was diagnosed with MEWDS in the left eye with a complaint of decreased vision for 1wk.
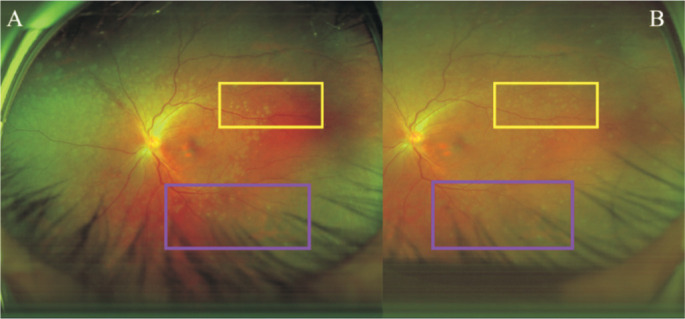
A: Plenty of white dots and spots; B: Increased numbers of dots and spots from the posterior pole to the peripheral over time (yellow and purple box). MEWDS: Multiple evanescent white dot syndrome.
Figure 3. Ultrawide fundus images of a 33-year-old female who is diagnosed with MEWDS in the left eye with a complaint of decreased vision for one week.

A: White spots and dots in the peripheral after one week; B: White spots start to fade from the peripheral after 2wk. MEWDS: Multiple evanescent white dot syndrome.
Table 1. Difference between spots and dots.
| Definition | Size | Location | Features |
| Dots | 100 µm | Abmormal extension of the inner retina | Superficial, small and dense |
| Spots | 200 µm | EZ (including IZ) | Big, located at the posterior pole and fused spots formed a bigger hypofluorescence |
| Meaning | Dots and spots commonly occur around the optic disc and is associated with the enlarged scotoma | ||
EZ: Ellipsoid zone; IZ: Interdigitation zone.
Figure 4. En-face OCTA of a 28-year-old female who complained of acute vision loss for one week and was diagnosed with MEWDS in the left eye.

En-face OCTA shows the typical dots and spots. A: Dots are located in the outer nuclear layer (red oval); B: Spots represent EZ disruption (yellow ovals). OCTA: Angio optical coherence tomography; EZ: Ellipsoid zone; MEWDS: Multiple evanescent white dot syndrome.
As for the prognosis, due to its self-limiting course, the vision will return to the pre-onset level in 95% of the patients with primary MEWDS, with a resolution of structural change on MMI[2]. However, enlargement of the scotoma, photopsia, and chromatic aberration may persist in a minority of patients[23],[29]–[34],[43].
Multiple Evanescent White Dot Syndrome Secondary to Retinal Diseases
Multiple evanescent white dot syndrome secondary to multifocal choroiditis/punctate inner choroidopathy
In addition to the already recognized manifestations of primary MEWDS, secondary MEWDS is referred to classical MEWDS features triggered by choroidal antigen exposure after varied causes and diseases possibly disrupting the RPE-BrM-CC. Cases of MEWDS secondary to MFC/PIC have been reported in the recent literature. MFC mostly affects bilaterally and occurs in young myopic women presented with photopsia, blurred vision and visual field defects[44]–[45]. When inflammation infiltrates deep choroid, the affected eyes may be presented with inflammatory cells of the vitreous cavity and anterior chamber, macular serous detachment, optic disc edema or congestion, electroretinogram (ERG) changes, and so forth. Idiopathic MFC is a generic term encompassing all three diseases, including PIC (Figure 5), MFC with panuveitis and progressive subretinal fibrosis. Despite sharing demographic features and symptoms, MFC differs from MEWDS in several aspects[1]. White spots in MEWDS are usually unilateral and present clinically in the deep retina or RPE layer, rather than the choroid. Vitreous inflammation could occur, but it is milder and more evanescent than MFC. Besides, leakage and macular detachment usually do not occur in MEWDS. Compared to MFC, white spots and visual field defects usually resolve spontaneously within 4 to 6wk with no significant residual lesions. Visual acuity usually remains good, although macular granularity tends to persist.
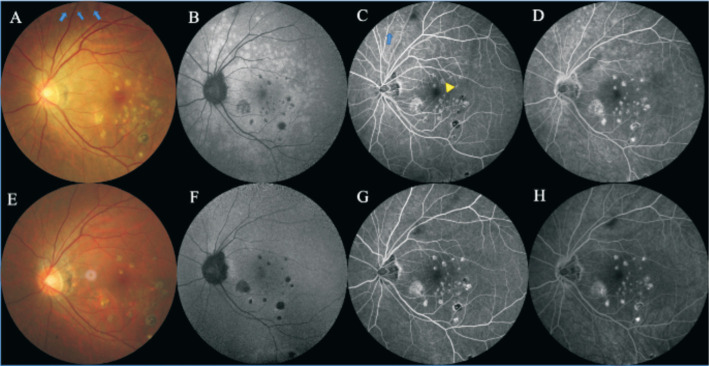
Figure 5. Color fundus photographs and FFA of a 35-year-old male presented with bilateral floating shadows and complained of vision decline. He was diagnosed with PIC and MEWDS in the left eye.
A-D: The fundus imaging at the first visit. A: Varying sizes of whitish-yellow lesions with pigmentation in the posterior pole and mottled yellow lesions in the mid-peripheral (blue arrows); B: Diffused hyperautofluorescence in the posterior pole with scattered hypoautofluorescence on FAF; C: Wreath-like hyperfluorescence on early FFA (blue arrows) and hypofluorescent PIC lesions with hyperfluorescent margin (yellow triangle); D: Fluorescence staining of PIC lesions in the posterior pole on late FFA. E-H: The follow-up at the time of 3wk later. E: The disappearance of the mid-peripheral lesions; F: Hypoautofluorescent PIC lesions in the posterior pole on FAF, and some of them are surrounded by the hyperautofluorescence at the border, while the diffused hyperautofluorescence in the posterior pole faded; G: Hypofluorescent lesions with a hyperfluorescent border in the posterior pole; H: Fluorescence staining of PIC lesions in the posterior pole on late-FFA. PIC: Punctate inner chorioretinopathy; MEWDS: Multiple evanescent white dot syndrome; FAF: Fundus autofluorescence; FFA: Fundus fluorescence angiography.
Regarding the similar demographic features and symptoms of MEWDS and MFC, a common host susceptibility likely exists between these two distinct entities. The overlap seen in these 2 entities can be explained in several ways. Kuznetcova et al[46] hypothesized a collective mechanism of episodes of choriocapillaris before MEWDS and MFC, and then this recurrent asymptomatic choriocapillaris may eventually evolve into MFC or other entities of WDS. Regarding MEWDS and MFC, previous literature has reported several cases of patients with MEWDS who subsequently exhibited typical manifestations of MFC with/without CNV during continuous observation[15],[47]. However, the opposite sequence is rarely seen (MFC evolving to MEWDS), with only two cases identified in the literature. In these two cases, MEWDS occurred in patients with pre-existing peripheral retinal scars that may be induced by prior MFC[15]. Whether the manifestation of inflammatory diseases is initially of MFC pattern or MEWDS pattern, most likely depends on the identity of the stimulating antigen or infectious agent and the host susceptibility. Some patients with MEWDS may be presented with overlapping MFC in the same or fellow eye[18]. Whether the two entities in the same patient exhibit a common susceptibility or common pathological mechanisms, there is considerable evidence of overlap among many idiopathic inflammatory choroidal entities, not just MFC and MEWDS[18]. MFC and MEWDS may be affiliated with the same disease spectrum and are more closely related to each other than other entities of WDS. MFC and MEWDS may be mediated by the same immune process that triggers one or the other, or both[48]. An MEWDS-like reaction may be triggered by the previous or simultaneous damage to the outer retina. Therefore, more studies about the genetic predisposition and molecular basis of MEWDS-like reactions will help to further understand this disease.
MEWDS secondary to MFC/PIC exhibits not only features of primary MEWDS but also includes additional conditions as below: 1) Isolated juxtafoveal yellowish-white inflammatory PIC lesion is visible on CFP. 2) Bruch's membrane (BrM) disruption and SHRM are visible on OCT. Choroidal thickening can be observed on enhanced depth imaging OCT (EDI-OCT) in the acute phase, suggesting the presence of inflammation in the outer retina and choriocapillaris. 3) The neovascularization in the optic disc or macula could be seen at the initial presentation on FFA, ICGA, and OCTA. A detailed description of MEWDS secondary PIC/MFC could be found in our team's previous work[13]. The common complications of MFC/PIC have been referred to as FCE and CNV[26]–[34],[43]. Therefore, some previous cases showed cooccurrence of MEWDS and FCE/CNV. We reviewed these cases and summarized them as follows.
Secondary MEWDS with focal choroidal excavation
FCE was first identified on time-domain OCT and then named by Margolis et al[49]. FCE mostly exhibits a stable state during a 1-year or 3-year follow-up period[50]. Although the pathogenesis remains hypothetical, it is suspected that FCE is in association with congenital or acquired abnormalities of choroidal capillary, including the choroidal malformation and developmental defects , inflammatory diseases[27]–[28],[51] and choroidal vascular disease[52]. There are three reported cases of secondary MEWDS with yellowish-white lesions developing into FCE[26]–[28] . Their common features are the increased choroidal thickness at the lesion's site initially, and the separation of the RPE from BrM with SHRM with/without mild BrM disruption subsequently. A case of FCE succeeding occurrence of MEWDS, reported by Jabbarpoor Bonyadi et al[27], was given a small dose of short-term steroid therapy and then BrM returned to structural integrity at the last follow-up, whereas the excavation was gradually deepened and morphologically stabilized. It is suggested that the severity of inflammation-induced damage and the plasticity of the RPE-BrM-CC may be related to the different types of acquired FCE. The mechanisms underlying MEWDS with FCE seem to consist of the following pathogenic events. First, inflammation occurring in the outer retina/inner choroid causes impairment of RPE-BrM-CC leading to adhesion of retinal and choroidal tissues through the RPE-BrM-CC ruptures with the increase of choroidal thickness. Then, contraction of the fibrotic lesions in combination with intraocular pressure leads to retinal herniation into the choroid. In addition, it has also been suggested that focal choroidal scar is the starting point for the pathogenesis of FCE and the imbalance of intraocular pressure and choroidal pressure may play a role in the formation of FCE[52].
Secondary MEWDS with choroidal neovascularization
CNV is caused by perturbation of RPE, presented with vision loss due to intraretinal exudate, subretinal fluid, hemorrhage, or fibrosis. CNV is an uncommon complication of primary MEWDS and usually occurs in secondary cases, such as the recurrent forms or MEWDS with marked inflammatory symptoms[15],[29]–[34],[43],[47],[53]–[58]. In the evolution of recurrent forms, infiltration and persistence of inflammation may lead to the formation of chorioretinal scar, then predisposing to CNV. On the review of the literature, we found that CNV occurred ranging from 4wk before to 13y after the occurrence of MEWDS, especially concurred with CNV in 6 cases[15],[29]–[34],[43],[47],[53]–[58]. The CNV is mainly located in the juxtafovea, with two cases located around the optic disc[29],[33]. It is suggested that acute changes of CNV are related to the occurrence of MEWDS. Of note, there are six atypical cases of MEWDS in three publications presented with juxtafoveal yellowish-white lesions[29],[32]–[33]. Our team reported a case series of MFC/PIC cases with MEWDS-like features[13]. In our study, all the cases showed the MEWDS features of multifocal deep retinal grayish-white spots, with the addition of juxtafoveal yellowish-white lesions (determined as CNV by OCTA), increased choroidal thickness, and SHRM.
The reason why MEWDS concurred with CNV is uncertain. It is suspected that the ischemia at the RPE-BrM-CC may trigger neovascularization. The evanescent choroidal hypoperfusion corresponding to hypofluorescence on late-ICGA in typical MEWDS[2], is not sufficient to cause permanent structural damage to the RPE and outer retina. Nonetheless, in secondary MEWDS cases, inflammation in the choroid leads to the formation of pachyvessels in the Haller layer and ruptures of BrM, and then choriocapillaris and scatter layer suffer a sufficient compression exerted by pachyvessels to produce a local ischemic microenvironment in conjunction with BrM ruptures predisposing to CNV.
Treatment is needed in cases of inflammatory CNV followed by secondary MEWDS. It is suspected that timely and effective steroid treatment is beneficial to the repair of elastic and collagen fibers of BrM, reducing the pulling of fibrous tissue against the formation of CNV[13],[59]. The inflammatory CNV preceding MEWDS suggests an asymptomatic phase of choriocapillaris. CNV may trigger the occurrence of MEWDS, probably due to the pro-inflammatory environment generated by the retinal tissue surrounding CNV. The pro-inflammatory environment acts as a trigger effect in susceptible eyes. These triggers can induce CNV and inflammatory changes in choriocapillaris or evanescent ischemia of choriocapillaris. Secondary MEWDS occurs more likely in patients with chorioretinitis with BrM ruptures[24]–[25]. The yellowish-white lesion in the juxtafovea may be the precursor of inflammatory CNV, and that timely and effective glucocorticoid treatment may reduce the progression of inflammatory lesions transforming into FCE or CNV and protect visual function as much as possible.
MEWDS with Acute Zonal Occult Outer Retinopathy
AZOOR is an outer retinal dysfunction extending from the optic disc, mainly characterized by acute vision loss or enlargement of a blind spot with photopsia, unilateral presentation, and often combined with myopia[33]. In the early stage of AZOOR, the ocular examination in 90% of patients, is almost completely normal, whereas atrophy of RPE and choroidal formed in the later stage. Different from MEWDS, AZOOR has a progressive course and a relatively aggressive prognosis. MMI is a helpful tool in diagnosing and differentiating MEWDS and AZOOR. FAF shows the characterized pattern of zonal fused hyperautofluorescence surrounding the optic disc. FFA shows no abnormalities in AZOOR patients, and ERG contributes to assessing if there is rod or cone cell dysfunction by evaluating the function of the outer retina. OCT shows the disappearance of EZ, corresponding to areas of visual field defect[24].
The presence of MEWDS and AZOOR in the same eye implies a common environmental or genetic susceptibility, or that these white dot syndrome (WDS) have a common etiology. However, the probability of incidental concurrence of 2 rare diseases is very small. It is difficult to determine whether the clinical manifestations of MEWDS precede AZOOR or appear simultaneously. Although the prognosis of MEWDS is better than that of AZOOR, the subsequent onset of AZOOR succeeding MEWDS may predict a worse outcome[16]. The overlapping manifestations in different WDS have also been reported. AZOOR also occurred in patients with a prior diagnosis of other types of WDS, including PIC[60] and MFC[61], suggesting a common genetic association with the pathogenesis[62].
In some patients, MEWDS and AZOOR may share common features, including gender (mostly female), unilaterality, low-to-moderate myopia, punctate or confluent hyperautofluorescence in the active phase on FAF, hypofluorescent lesions on late-ICGA. However, as being 2 distinct entities, there are some differences in different examinations as follows helping to differentiate. First, MEWDS is mainly seen in young women aged 15 to 30 years old, whereas AZOOR occurs mostly in their 30s to 40s. Second, MEWDS shows obvious white dots mostly located in the posterior pole on CFP, also seen in the midperiphery. However, when it comes to AZOOR, there is no visible abnormality in the early phase of CFP, and atrophic changes are only seen around the optic disc in the late phase. Third, in MEWDS, ERG commonly shows no abnormalities, with the abnormality of a wave occasionally, while in AZOOR, ERG could show abnormality in some cases. Most importantly, FAF plays an important role in differentiating these 2 entities. FAF is a noninvasive means of assessing RPE function[63]. Inflammation in the acute phase tends to cause the accumulation of autofluorescence so that hyper-autofluorescence is seen in active lesions or at the edges of the chorioretinal scar. In chronic disease, the apoptosis of RPE may result in hypo-autofluorescence. In MEWDS, it has a self-limiting course and a good prognosis, and the lesions on FAF could restore spontaneously in MEWDS. Yet, in AZOOR, the prognosis varies depending on the site of lesions, and the lesions could not recover on FAF. AZOOR usually has a more severe outer retinal impairment and may be associated with thinning of the inner nuclear layer. IS/OS was restored during the recovery phase of MEWDS, which is uncommon in AZOOR.
Possible pathogenesis of MEWDS with white dot syndromes
The patients initially diagnosed with MEWDS finally develop into other types of WDS, further complicating our understanding of MEWDS (Table 2)[15]–[16],[46]–[47]. Investigating atypical cases of MEWDS may provide profound insights into understanding the underlying mechanisms of MEWDS. For example, according to the different manifestations of varying severity of inflammatory diseases, these overlapping entities probably have two completely distinct progressions (e.g., photoreceptor inflammation secondary to choroiditis or a primary choriocapillaris). It is suggested that these diseases may share a common genetic susceptibility and/or pathological factors. All these patients have relatively common nonspecific gene clusters at specific loci that predispose patients to immune dysregulation and autoimmune diseases. In addition, common susceptibilities (including immune dysregulation, interactions between specific environmental triggers, and other genes) lead to the overlapping occurrence of one or more diseases. What's more, environmental triggers and major histocompatibility antigens explain some changes in clinical course. Finally, retinal specialists must study the differentiation between MEWDS and other entities of WDS, because appropriate evaluation allows clinicians to estimate whether patients with MEWDS will develop into other overlapping entities of WDS and helps to determine the treatment and evaluate the prognosis.
Table 2. Literature review of MEWDS with other types of WDS.
| Year | Journal | Sex | Age | Affected eye | Medical history | Refractive status | Primary diagnosis | Chief complaint | First VA | Duration | Primary treatment | VA in follow-up | Chief complaint in follow-up | Final diagnosis | Follow-up treatment | Last VA | Follow-up time |
| 2009 | Arch Ophthalmol | F | 29 | R | - | N/A | MEWDS | Blurred vision with oribital pain | 20/100 | 3wk | Observation | 20/20 | Vision field defect progress after 14mo | AZOOR | Oral steroid, MMF and AZA | 20/20 | 26mo |
| M | 51 | R | Flu | N/A | MEWDS | Enlarged scotoma | FC | 1mo | Observation | FC | Dcreased vision after 11mo | AZOOR | N/A | HM | 11mo | ||
| F | 32 | R | - | N/A | MEWDS | Photopsia with transient shadow and headache | 20/20 | 1mo | Observation | 20/20 | Vision field defect progress after 15mo | AZOOR | N/A | 20/20 | 15mo | ||
| 2002 | Retina | F | 32 | R | Orbital lymphoma | N/A | MFC | Decreased vision | 20/20 | N/A | Oral steroid | 20/20 | Dcreased vision with photopsia after 5y | MEWDS | Observation | 20/20 | 5y |
| F | 29 | L | - | N/A | MFC&BVMD | Acute vision field defect with photopsia | 20/200 | 2mo | Observation | 20/200 | Photopsia disappeared | MEWDS | Observation | 20/200 | 2mo | ||
| F | 32 | R | - | N/A | MFC | Decreased vision | 20/40 | N/A | LP | 20/25 | Decreased vision follow flu after 2mo | MEWDS | Observation | N/A | 2y | ||
| F | 29 | L | - | N/A | MFC | Decreased vision with scotoma | 20/50 | N/A | N/A | 20/20 | Decreased vision with scotoma | MEWDS | Observation | 20/20 | 4wk | ||
| 2012 | J Ophthalmic Vis Res | F | 40 | L | - | High myopia | MEWDS | Central scotoma | 20/25 | 4mo | Observation | 20/25 | Dcreased vision | MFC | Retrobulbar injection of TA | 20/25 | 1y |
| 2019 | Int J Retina Vitreous | F | 39 | R | - | Emmetropia | MEWDS | N/A | 20/20 | N/A | Anti-VEGF; oral sulfamethoxazole and steroid | 20/20 | N/A | MEWDS | Anti-VEGF; oral sulfamethoxazole and steroid | 20/20 | 11y |
| L | MFC&CNV | N/A | 20/25 | N/A | 20/25 | N/A | MFC/CNV | 20/25 | |||||||||
| R | MFC | Paracentral scotoma for 2d | 20/20 | 4mo | 20/20 | Paracentral scotoma | MFC | 20/20 |
MEWDS: Multiple evanescent white dot syndrome; WDS: White dot syndrome; -: None; N/A: Not available; FC: Finger count; F: Female; M: Male; R: Right; L: Left; VA: Visual acuity; AC: Anterior chamber; HM: Hand move; MFC: Multifocal chorioditis; CNV: Choroidal neovascularization; BVMD: Best vitelliform macular dystrophy; LP: Laser photocoagulation; TA: Triamcinolone acetonide; MMF: Mycophenolate mofetil; AZA: Azathioprine; VEGF: Vascular endothelial growth factor; AZOOR: Acute zonal occult outer retinopathy; PIC: Punctate inner choroidopathy.
Secondary MEWDS with PXE, BVMD, History of Surgery, Trauma, or Photocoagulation
In the traditional recognition of MEWDS, it is an inflammatory disease with a self-limiting course. Although the characterized presentation, reports have described MEWDS occurring in conjunction with other, apparently unrelated, ocular diseases, either concurrently or over the course of follow-up. We comprehensively reviewed the related literatures of secondary MEWDS with other ocular diseases and previous therapeutic history probably inducing retinal insults, and then summarize the features to help differentiate and discuss the underlying mechanisms of MEWDS occurring in the setting of posterior segment abnormalities mentioned above.
Secondary MEWDS with PXE
PXE is a rare autosomal recessive multisystem disease characterized by skin lesions, premature calcification, occlusive vascular disease and complications such as angina pectoris, claudication, hypertension, fundus angioid streaks changes, especially occurring in young women. Mutations in ABCC6 gene are responsible for PXE, although no clear genotype-phenotype relationship has been elucidated yet. Retinal features of PXE include several alterations as a peaud'orange-like appearance, comet lesions, angioid streaks, and peripapillary drusen. In particular, the calcification of BrM may be in association with the alternation of the fundus and finally lead to retinal atrophy with vision loss. Of note, the disruption of the calcified BrM corresponds to the angioid streaks in the ophthalmoscope and gives rise to the development of CNV and exposure of the retinal, RPE and choroidal antigens. Although the pathogenesis is elusive, there are several literatures suggesting that the underlying mechanism is associated with exposure to retinal antigens and the subsequent immune response to these antigens. Gliem et al[24], who conducted a study enrolling 9 patients with acute retinopathy (frequency of 5%) in a cohort with PXE, hypothesized that PXE may be due to serum anti-retinal autoantibodies and anti-RPE autoantibodies, and found that these features of acute outer retinopathy and the frequency of 5% suggested a true association between PXE and MEWDS, rather than a coincidental coexistence. In addition, Marchese et al[64] also reported two young PXE patients presented with features MEWDS and MFC. In the PXE-associated acute outer retinopathy, the lesions (BrM rupture) along vessels are most evidently seen, where antigens of the retina, RPE, and BrM to the immune system may trigger autoimmune processes. Meanwhile, acute outer retinopathy could also explain the previously reported undetected ERG response in PXE patients. The literature reported that autoantibodies against the anti-RPE protein (anti-62-kDa protein) were found in 4 of the 6 cases (67%). Only two cases were tested during the acute phase of retinopathy and the antibodies were tested up to 4y after the onset of acute outer retinopathy. However, if the antigens stimulate the immune system, autoantibodies can persist in the circulation for a long time[24]. Therefore, further investigation on the association between RPE as well as retinal antibodies and etiopathology of MEWDS should be conducted.
Secondary MEWDS with BVMD
With regard to BVMD, there is a case report documenting the presentation of MEWDS in a patient with BVMD, yet without persistent lesions other than the foveal lesion of BVMD[16]. We conclude that BrM disruption, RPE changes, and angioid streaks (disruption of calcified BrM) are likely causes of acute outer retinopathy. Additionally, although fibrotic proliferation is a common complication of angioid streaks, it may also play a pathogenic role in the development of inflammatory-like reactions.
MEWDS with toxoplasmosis
Gass[62] first described deep retinal involvement for toxoplasmosis, then, Friedmann and Knox[65] described more typical presentations, including punctate inner retinopathy and deep punctate lesions with subretinal fluid, mostly involving the macula or peripapillary area[65]. Furthermore, Doft and Gass[66] documented the features in detail and named this condition as ‘punctate outer retinal toxoplasmosis. In reviewing literatures, 3 cases of ocular toxoplasmosis followed by MEWDS, proposing the assumption of the possibility that infection triggers an immune response[67]. The authors deemed that whether the succedent MEWDS was related to the patient's ocular toxoplasmosis infection remained elusive. Alternatively, it may also be due to impaired immune defenses associated with steroid treatment or the immunosuppression related to toxoplasmosis (toxoplasma could also suppress immune function). The state of immunosuppression induced by the former 2 causes could lead patients to be susceptible to an inflammatory condition. Ocular toxoplasmosis can trigger fleeting disruption of the outer retina with photoreceptor loss in the absence of choroidal ischemia. This disruption has been also described in MEWDS and may occur in the setting of inflammatory conditions typically affecting young and healthy patients. However, further studies are needed to better understand the link between the transient disruption of the outer retina triggered by MEWDS and ocular toxoplasmosis[67]. In all, toxoplasma gondii is a possible pathogen or may be a pathogen of immunoreaction in some cases of inflammatory diseases. Animal studies also verified that toxoplasmosis can cause defect and migration of RPE cells[68]. Taken together, hypothetically, toxoplasmosis is possibly a triggering factor of immune response which ultimately leads to the MEWDS.
MEWDS after surgery, trauma, laser photocoagulation
Patients with MEWDS who have an ocular history positive for previous or concurrent ocular events have been described in recent literatures. These ocular events in the published reports include ocular surgery (most being repairment for retinal detachment), trauma, and laser photocoagulation. In our review of the literatures, we identified patients diagnosed with overlapping features of MEWDS and MFC after retinal detachment in the same eye[69] or in the contralateral eye[46]. One of two cases of retinal detachment preceding the manifestation of MFC was attributed to a hypersensitive response to the scleral buckling material[70]. According to the authors' hypothesis, it is possible that the retinal damage of retinal detachment and subsequent surgical repair commonly serve to trigger a local inflammatory response. Other reports in the literature also support the theory, and it seems that MEWDS-like reactions are also associated with ocular trauma, including laser photocoagulation treatment of peripheral retinal tears[71], choroidal rupture[22], penetrating trauma[21], and history of orbital lymphangioma resections[25]. Fung et al[22] reported a case of a 24-year-old female with blunt trauma to the right eye combined with choroidal rupture, who presented 10wk after the initial trauma with gray deep retinal spots, foveal granularity, mild vitreous inflammation, optic disc congestion and edema, and retinal vasculitis. FFA, ICGA, and OCT showed overlapping features consistent with MEWDS. Given the duration after damage and the anatomical location of the injury, retinal damage at the time of detachment and subsequent surgical repair may have played a role in triggering the local inflammatory response. Therefore, the authors concluded that exposure to choroidal antigens or dehemoglobinized blood was the trigger for the fundus manifestation. Overall, in light of the findings reported previously, it is speculated that the co-existence of ocular events and inflammatory retinal diseases may not be coincidental, but rather due to susceptibility or trigger for the local inflammatory response and immune-mediated process, including immunogenic triggers and host genetic susceptibility.
Possible pathogenesis of secondary MEWDS with PXE, BVMD, history of surgery, trauma, or photocoagulation
All in all, the ocular diseases or ocular events mentioned above have a greater or lesser role in triggering the concurrent or following MEWDS. Although etiopathology remains to be determined, we have summarized several aspects of triggers according to the previous literature, including infection, genetic susceptibilities to autoimmune diseases, and traumatic events. Taken together, all the triggers seem to contribute to impairing the outer retina or inner choroid and disruption of BrM leading to more exposure to retina and RPE antigens. In macular diseases, although the simultaneous presence of macular diseases (e.g., CNV or BVMD) and MEWDS in the same eye may be coincidental, it is hypothesized that macular RPE or BrM damage is associated with acute inflammatory events. The presence of MEWDS-like features attributed to prior or concurrent ocular injury events may trigger a local nonspecific inflammatory response. Concerning PXE-associated acute retinopathy, the lesions are usually along angioid streaks (disruption of calcified BrM), also supporting the theory of antigen exposure. What's more, traumatic subretinal hemorrhage, choroidal rupture, penetrating trauma of the fellow eye, or choroid insults also imply the role of antigen exposure as a possible cause. At the site of BrM disruption, more antigens of the outer retina or RPE are exposed to the immune system, which may contribute to the development of secondary MEWDS. Additionally, individuals with outer retinopathy are prone to MEWDS, and the overlapping manifestations indicate a common pathogenic pathway, too[71]. Although the underlying mechanism remains speculative, it is found to be strongly relevant to the immunoreaction and pathological progress of inner choroid, RPE, and photoreceptor, suggesting that antigen exposure is a possible trigger[62]. Literature about MEWDS concurrently with PXE, BVMD, and MEWDS-like change after surgery, trauma, photocoagulation, and OT were summarized in Table 3.
Table 3. Literature review of MEWDS concurrently with PXE, BVMD and MEWDS-like change after surgery, trauma, photocoagulation and OT.
| Year | Journal | Sex | Age | Affected eye | Medical history | Refractive status | Diagnosis | Chief complaint | First VA | Treatment | Last VA | Follow-up time |
| 1997 | Arch Ophthalmol | M | 23 | R | N/A | N/A | BVMD with MEWDS | Regular follow-up for BVMD | 20/25 | Observation | 20/60 | 1mo |
| 2004 | Retina | F | 17 | L | PPV for ophthalmorrhexis 8wk ago | Myopia | Post-trama with MEWDS-like reaction | Decreased vision for 1wk | 20/25 | Steroid and MTX | 20/20 | 18mo |
| 2011 | Retina | N/A | 27 | N/A | N/A | N/A | OT with MEWDS | N/A | 20/20 | Steroid and antibiotic | 20/20 | 4wk |
| 2012 | Retin Cases Brief Rep | F | 24 | R | N/A | N/A | Choroidal rupture with MEWDS | Scotoma and floating shadow | 20/70 | Steroid | 20/50 | 8wk |
| 2016 | BMC Ophthalmol | F | 20 | L | N/A | N/A | ASs with MEWDS | Decreased vision | 20/100 | Steroid and anti-VEGF | 20/60 | 1mo |
| 2017 | Retina | F | 67 | B | Viral infection 2mo ago | N/A | Retinal tears and post-LP | Decreased vision with floating shadow | 20/40 | Observation | 20/20 | 8wk |
| N/A | 20/80 | |||||||||||
| 2019 | JAMA Ophthalmol | N/A | N/A | R | - | N/A | PXE with MEWDS | Decreased vision with central scotoma | 20/40 | Steroid and anti-VEGF | 20/80 | 64mo |
| F | N/A | R | N/A | N/A | PXE with MEWDS | Decreased vision with photopsia | 20/32 | Anti-VEGF | 20/25 | 48mo | ||
| F | 32 | R | N/A | N/A | PXE with MEWDS | N/A | 20/400 | Steroid, anti-VEGF and retrobulbar infection of TA | 20/640 | 20mo | ||
| 2020 | Retina | N/A | 14 | N/A | N/A | N/A | OT with MEWDS | N/A | 20/50 | Steroid and antibiotic | 20/30 | 32d |
| 2021 | Ophthalmol Retina | M | 19 | R | BVMD with CNV | N/A | BVMD with MEWDS | Decreased vision with photopsia | 20/40 | Steroid | 20/32 | 4mo |
| F | 81 | R | P+I and LP | N/A | PXE with MEWDS | Decreased vision after 2wk of P+I | FC | Anti-VEGF | N/A | 1mo | ||
| F | 38 | R | SB for RD 14y ago | High myopia | post-SB with MEWDS | Floating shadow in the peripheral | 20/30 | Steroid and anti-VEGF | 20/40 | 4mo | ||
| M | 16 | L | N/A | N/A | Idiopathic retinochoroiditis with MEWDS | Decreased vision with photopsia | 20/50 | Observation | 20/20 | 4wk |
-: None; N/A: Not available; FC: Finger count; F: Female; M: Male; R: Right; L: Left; B: Binocular; MEWDS: Multiple evanescent white dot syndrome; MFC: Multifocal chorioditis; CNV: Choroidal neovascularization; BVMD: Best vitelliform macular dystrophy; TA: Triamcinolone acetonide; VEGF: Vascular endothelial growth factor; MTX: Methotrexate; LP: Laser photocoagulation; SB: Scleral buckling; PXE: Pseudoxanthoma elasticum; PPV: Pars plana vitrectomy; P+I: Phaco, and intraocular lens implantation; ASs: Angioid streaks; OT: Ocular toxoplasmosis; RD: Retinal detachment; CSCR: Central serous chorioretinopathy; VA: Visual acuity.
Conclusion and Future Prospects
In conclusion, typical fundus manifestations of MEWDS can be diagnosed by MMI (CFP, OCT, FFA, ICGA, OCTA, FAF), and the main diagnostic criteria contain multiple, small, white spots in the posterior pole and deep layers of the peripheral retina, yellow-white foveal granularity; wreath-like hyperfluorescence on early-FFA and SHRM in RPE, EZ, and outer nuclear layer on OCT; and mild anterior chamber and vitreous cells. Secondary MEWDS was diagnosed by the aforementioned criteria of primary MEWDS, meanwhile with a cause/disease resulting in RPE-BrM-CC disruption. Due to its self-limiting course, MEWDS patients aren't often given specific treatment. However, in recent years, reports of secondary MEWDS combined with other diseases increased, especially CNV and FCE secondary to MEWDS with juxtafoveal isolated yellow-white lesion, MEWDS with BVMD and PXE, and secondary MEWDS after surgery, trauma or photocoagulation. Those diseases involving macula have a poor prognosis and cause irreversible damage to vision. Some studies suggested that early steroid treatment is effective for the diseases, suggesting ophthalmologists perceive the occurrence of secondary MEWDS with other diseases in the early stage. Although the manifestations are still evanescent, the prognosis and treatment of secondary MEWDS are determined by the severity of the complications. The etiology and pathogenesis of secondary MEWDS remain undetermined. Current studies support the association of secondary MEWDS pathogenesis with immune factors, including a history of viral infection, inflammation of the choroidal vessels and BrM, traumatic subretinal hemorrhage, choroidal rupture, contralateral eye penetrating injury, or combined choroidal insults, resulting in antigen exposure. More etiologic and pathogenic studies are urgently needed in the future such as the research on retinal antigens and antibodies. Accurate diagnosis could guide clinical management and prognostic assessment to avoid more serious complications.
Footnotes
Authors' contributions: Chen CL: Conceptualization, drafting the original manuscript. Cheng YZ: Drafting the original manuscript, editing, visualization. Zhang ZH: Editing. Peng XY: Visualization, reviewing. All authors read and approved the final manuscript.
Foundations: Supported by the National Natural Science Foundation of China (No.82171073; No.82101147).
Conflicts of Interest: Chen CL, None; Cheng YZ, None; Zhang ZH, None; Wang G, None; Peng XY, None.
REFERENCES
- 1.Jampol LM. Multiple evanescent white dot syndrome. Arch Ophthalmol. 1984;102(5):671. doi: 10.1001/archopht.1984.01040030527008. [DOI] [PubMed] [Google Scholar]
- 2.Marsiglia M, Gallego-Pinazo R, de Souza EC, Munk MR, Yu S, Mrejen S, Cunningham ET, Jr, Lujan BJ, Goldberg NR, Albini TA, Gaudric A, Francais C, Rosen RB, Freund KB, Jampol LM, Yannuzzi LA. Expanded clinical spectrum of multiple evanescent white dot syndrome with multimodal imaging. Retina. 2016;36(1):64–74. doi: 10.1097/IAE.0000000000000685. [DOI] [PubMed] [Google Scholar]
- 3.Cicinelli MV, Ramtohul P, Marchese A, Bandello F, Bailey Freund K, Miserocchi E, Jampol LM. Latest advances in white spot syndromes: new findings and interpretations. Prog Retin Eye Res. 2023;97:101207. doi: 10.1016/j.preteyeres.2023.101207. [DOI] [PubMed] [Google Scholar]
- 4.Classification criteria for multiple evanescent white dot syndrome. Am J Ophthalmol. 2021;228:198–204. doi: 10.1016/j.ajo.2021.03.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ng HW, Niederer RL. Lightning can strike twice: recurrent multiple evanescent white dot syndrome (MEWDS) following both COVID-19 vaccination and subsequent COVID-19 infection. J Ophthalmic Inflamm Infect. 2023;13(1):36. doi: 10.1186/s12348-023-00355-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yu J, Ji YY, Zeng YK, Li HH, Liao HL, Wen F. Multimodal imaging in diagnosing multiple evanescent white dot syndrome following human papillomavirus vaccine immunization. Case Rep Ophthalmol Med. 2024;2024:9600771. doi: 10.1155/2024/9600771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kashyap H, Manoharan A, Mahendradas P, Agarwal A, Majumder PD. A COVID-19 perspective of multiple evanescent white dot syndrome (MEWDS) Indian J Ophthalmol. 2024 doi: 10.4103/IJO.IJO_2029_23. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zou YR, Kamoi K, Zong Y, Zhang J, Yang MM, Ohno-Matsui K. Ocular inflammation post-vaccination. Vaccines. 2023;11(10):1626. doi: 10.3390/vaccines11101626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Standardization of Uveitis Nomenclature Working Group. Classification criteria for multiple evanescent white dot syndrome. Am J Ophthalmol. 2021;228:198–204. doi: 10.1016/j.ajo.2021.03.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Essilfie J, Bacci T, Abdelhakim AH, Ramtohul P, Turchi F, Freund KB, Yannuzzi LA. Are there two forms of multiple evanescent white dot syndrome? Retina. 2022;42(2):227–235. doi: 10.1097/IAE.0000000000003288. [DOI] [PubMed] [Google Scholar]
- 11.Serrar Y, Cahuzac A, Gascon P, Langlois-Jacques C, Mauget-Faÿsse M, Wolff B, Sève P, Kodjikian L, Mathis T. Comparison of primary and secondary forms of multiple evanescent white dot syndrome. Retina. 2022;42(12):2368–2378. doi: 10.1097/IAE.0000000000003609. [DOI] [PubMed] [Google Scholar]
- 12.Meng Y, Zhang Q, Li L, Yi Z, Xu YS, Su Y, Liang CB, Xiao D, Zhang L, Chen CZ. Primary multiple evanescent white dot syndrome and multiple evanescent white dot syndrome secondary to multifocal choroiditis/punctate inner choroidopathy: a comparative study. Retina. 2023;43(7):1122–1131. doi: 10.1097/IAE.0000000000003776. [DOI] [PubMed] [Google Scholar]
- 13.Chen CL, Cheng YZ, Zhang ZH, Zhang Y, Hou SM, Wang G, Peng XY. The multimodal imaging features and outcomes of multifocal choroiditis/punctate inner choroidopathy lesion with multiple evanescent white dot syndrome-like features: a retrospective study. BMC Ophthalmol. 2024;24(1):3. doi: 10.1186/s12886-023-03277-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ong AY, Birtel J, Agorogiannis E, Sharma SM, Charbel Issa P. Topographic patterns of retinal lesions in multiple evanescent white dot syndrome. Graefes Arch Clin Exp Ophthalmol. 2023;261(8):2257–2264. doi: 10.1007/s00417-023-06032-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Callanan D, Gass JD. Multifocal choroiditis and choroidal neovascularization associated with the multiple evanescent white dot and acute idiopathic blind spot enlargement syndrome. Ophthalmology. 1992;99(11):1678–1685. doi: 10.1016/s0161-6420(92)31755-5. [DOI] [PubMed] [Google Scholar]
- 16.Fine HF, Spaide RF, Ryan EH, Jr, Matsumoto Y, Yannuzzi LA. Acute zonal occult outer retinopathy in patients with multiple evanescent white dot syndrome. Arch Ophthalmol. 2009;127(1):66–70. doi: 10.1001/archophthalmol.2008.530. [DOI] [PubMed] [Google Scholar]
- 17.Schaal S, Schiff WM, Kaplan HJ, Tezel TH. Simultaneous appearance of multiple evanescent white dot syndrome and multifocal choroiditis indicate a common causal relationship. Ocul Immunol Inflamm. 2009;17(5):325–327. doi: 10.3109/09273940903043923. [DOI] [PubMed] [Google Scholar]
- 18.Kang HG, Kim TY, Kim M, Byeon SH, Kim SS, Koh HJ, Lee SC, Lee CS. Expanding the clinical spectrum of multiple evanescent white dot syndrome with overlapping multifocal choroiditis. Ocul Immunol Inflamm. 2022;30(1):81–89. doi: 10.1080/09273948.2020.1795206. [DOI] [PubMed] [Google Scholar]
- 19.Mizuuchi K, Saito W, Namba K, Ishida S. Multiple evanescent white dot syndrome and panuveitis: a case report. J Ophthalmic Inflamm Infect. 2020;10(1):26. doi: 10.1186/s12348-020-00221-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Park DW. Multiple evanescent white dot syndrome in a patient with best disease. Arch Ophthalmol. 1997;115(10):1342. doi: 10.1001/archopht.1997.01100160512031. [DOI] [PubMed] [Google Scholar]
- 21.Landolfi M, Bhagat N, Langer P, Rescigno R, Mirani N, Grigorian RA, Zarbin MA. Penetrating trauma associated with findings of multiple evanescent white dot syndrome in the second eye: coincidence or an atypical case of sympathetic ophthalmia? Retina. 2004;24(4):637–645. doi: 10.1097/00006982-200408000-00029. [DOI] [PubMed] [Google Scholar]
- 22.Fung AT, Sorenson JA, Freund KB. An atypical white dot syndrome after traumatic subretinal hemorrhage. Retin Cases Brief Rep. 2012;6(4):339–344. doi: 10.1097/ICB.0b013e318260af4a. [DOI] [PubMed] [Google Scholar]
- 23.Pece A, Allegrini D, Kontadakis S, Querques G, Rossetti L. Intravitreal ranibizumab for choroidal neovascularization in a patient with angioid streaks and multiple evanescent white dots. BMC Ophthalmol. 2016;16:122. doi: 10.1186/s12886-016-0307-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gliem M, Birtel J, Müller PL, Hendig D, Faust I, Herrmann P, Holz FG, Adamus G, Charbel Issa P. Acute retinopathy in pseudoxanthoma elasticum. JAMA Ophthalmol. 2019;137(10):1165–1173. doi: 10.1001/jamaophthalmol.2019.2910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cicinelli MV, Hassan OM, Gill MK, Goldstein D, Parodi MB, Jampol LM. A multiple evanescent white dot syndrome-like reaction to concurrent retinal insults. Ophthalmol Retina. 2021;5(10):1017–1026. doi: 10.1016/j.oret.2020.12.007. [DOI] [PubMed] [Google Scholar]
- 26.Hashimoto Y, Saito W, Noda K, Ishida S. Acquired focal choroidal excavation associated with multiple evanescent white dot syndrome: observations at onset and a pathogenic hypothesis. BMC Ophthalmol. 2014;14:135. doi: 10.1186/1471-2415-14-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jabbarpoor Bonyadi MH, Hassanpour K, Soheilian M. Recurrent focal choroidal excavation following multiple evanescent white dot syndrome (MEWDS) associated with acute idiopathic blind spot enlargement. Int Ophthalmol. 2018;38(2):815–821. doi: 10.1007/s10792-017-0511-9. [DOI] [PubMed] [Google Scholar]
- 28.Matsubara H, Uchiyama E, Suzuki K, Matsuda Y, Kondo M. A case of focal choroidal excavation development associated with multiple evanescent white dot syndrome. Case Rep Ophthalmol. 2018;9(2):388–394. doi: 10.1159/000492747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McCollum CJ, Kimble JA. Peripapillary subretinal neovascularization associated with multiple evanescent white-dot syndrome. Arch Ophthalmol. 1992;110(1):13–14. doi: 10.1001/archopht.1992.01080130015007. [DOI] [PubMed] [Google Scholar]
- 30.Papadia M, Herbort CP. Idiopathic choroidal neovascularisation as the inaugural sign of multiple evanescent white dot syndrome. Middle East Afr J Ophthalmol. 2010;17(3):270–274. doi: 10.4103/0974-9233.65490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mathis T, Delaunay B, Cahuzac A, Vasseur V, Mauget-Faÿsse M, Kodjikian L. Choroidal neovascularisation triggered multiple evanescent white dot syndrome (MEWDS) in predisposed eyes. Br J Ophthalmol. 2018;102(7):971–976. doi: 10.1136/bjophthalmol-2017-311005. [DOI] [PubMed] [Google Scholar]
- 32.Chen KC, Marsiglia M, Dolz-Marco R, Zahid S, Mrejen S, Pulido JS, Cohen SY, Freilich B, Yannuzzi LA, Freund KB. Foveal exudate and choroidal neovascularization in atypical cases of multiple evanescent white dot syndrome. Retina. 2017;37(11):2025–2034. doi: 10.1097/IAE.0000000000001486. [DOI] [PubMed] [Google Scholar]
- 33.Savastano MC, Rispoli M, Lumbroso B. Choroidal juxtapapillary neovascularization regression in multiple evanescent white dot syndrome by optical coherence tomography angiography: a case report. J Med Case Rep. 2019;13(1):274. doi: 10.1186/s13256-019-2211-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Demirel S, Yalçındağ N, Yanık Ö, Temel E, Batıoğlu F, Özmert E. Unusual presentation of multiple evanescent white dot syndrome and importance of optical coherence tomography angiography to diagnose choroidal neovascularization under inflammed choriocapillaris. Indian J Ophthalmol. 2020;68(9):1948–1950. doi: 10.4103/ijo.IJO_1115_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dell'Omo R, Pavesio CE. Multiple evanescent white dot syndrome (MEWDS) Int Ophthalmol Clin. 2012;52(4):221–228. doi: 10.1097/IIO.0b013e31826647ed. [DOI] [PubMed] [Google Scholar]
- 36.Hua R, Chen K, Liu LM, Liu NN, Chen L, Teng WP. Multi-modality imaging on multiple evanescent white dot syndrome-a Spectralis Study. Int J Ophthalmol. 2012;5(5):644–647. doi: 10.3980/j.issn.2222-3959.2012.05.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zicarelli F, Mantovani A, Preziosa C, Staurenghi G. Multimodal imaging of multiple evanescent white dot syndrome: a new interpretation. Ocul Immunol Inflamm. 2020;28(5):814–820. doi: 10.1080/09273948.2019.1635169. [DOI] [PubMed] [Google Scholar]
- 38.Dell'omo R, Wong R, Marino M, Konstantopoulou K, Pavesio C. Relationship between different fluorescein and indocyanine green angiography features in multiple evanescent white dot syndrome. Br J Ophthalmol. 2010;94(1):59–63. doi: 10.1136/bjo.2009.163550. [DOI] [PubMed] [Google Scholar]
- 39.Finn AP, Khurana RN. Multiple evanescent white dot syndrome: bilateral disease may be silent and asymmetric. Am J Ophthalmol Case Rep. 2021;21:101004. doi: 10.1016/j.ajoc.2020.101004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mebsout-Pallado C, Orès R, Terrada C, et al. Review of the current literature and our experience on the value of OCT-angiography in white dot syndromes. Ocul Immunol Inflamm. 2022;30(2):364–378. doi: 10.1080/09273948.2020.1837185. [DOI] [PubMed] [Google Scholar]
- 41.Khochtali S, Dridi T, Abroug N, Ksiaa I, Lupidi M, Khairallah M. Swept-source optical coherence tomography angiography shows choriocapillaris flow reduction in multiple evanescent white dot syndrome. J Curr Ophthalmol. 2020;32(2):211–215. doi: 10.4103/JOCO.JOCO_107_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pereira F, Lima LH, de Azevedo AGB, Zett C, Farah ME, Belfort R., Jr Swept-source OCT in patients with multiple evanescent white dot syndrome. J Ophthalmic Inflamm Infect. 2018;8(1):16. doi: 10.1186/s12348-018-0159-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Desira M, Fitoussi R, Comet A, Denis D, Stolowy N, David T. Choroidal neovascularization and MEWDS like reaction in a child: A rare case. Eur J Ophthalmol. 2023:11206721231206440. doi: 10.1177/11206721231206440. [DOI] [PubMed] [Google Scholar]
- 44.Nozik RA, Dorsch W. A new chorioretinopathy associated with anterior uveitis. Am J Ophthalmol. 1973;76(5):758–762. doi: 10.1016/0002-9394(73)90573-4. [DOI] [PubMed] [Google Scholar]
- 45.Dreyer RF, Gass DJ. Multifocal choroiditis and panuveitis. A syndrome that mimics ocular histoplasmosis. Arch Ophthalmol. 1984;102(12):1776–1784. doi: 10.1001/archopht.1984.01040031440019. [DOI] [PubMed] [Google Scholar]
- 46.Kuznetcova T, Jeannin B, Herbort CP. A case of overlapping choriocapillaritis syndromes: multimodal imaging appraisal. J Ophthalmic Vis Res. 2012;7(1):67–75. [PMC free article] [PubMed] [Google Scholar]
- 47.Wyhinny GJ, Jackson JL, Jampol LM, Caro NC. Subretinal neovascularization following multiple evanescent white-dot syndrome. Arch Ophthalmol. 1990;108(10):1384–1385. doi: 10.1001/archopht.1990.01070120030013. [DOI] [PubMed] [Google Scholar]
- 48.Morizot E, Schiavo Froner C. Neovessel as first manifestation of relapse of associated multifocal choroiditis and MEWDS. Int J Retina Vitreous. 2019;5:25. doi: 10.1186/s40942-019-0175-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Margolis R, Mukkamala SK, Jampol LM, Spaide RF, Ober MD, Sorenson JA, Gentile RC, Miller JA, Sherman J, Freund KB. The expanded spectrum of focal choroidal excavation. Arch Ophthalmol. 2011;129(10):1320–1325. doi: 10.1001/archophthalmol.2011.148. [DOI] [PubMed] [Google Scholar]
- 50.Lim FPM, Loh BK, Cheung CMG, Lim LS, Chan CM, Wong DWK. Evaluation of focal choroidal excavation in the macula using swept-source optical coherence tomography. Eye (Lond) 2014;28(9):1088–1094. doi: 10.1038/eye.2014.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ramakrishnan MS, Patel AP, Melles R, Vora RA. Multiple evanescent white dot syndrome: findings from a large northern California cohort. Ophthalmol Retina. 2021;5(9):850–854. doi: 10.1016/j.oret.2020.11.016. [DOI] [PubMed] [Google Scholar]
- 52.Gan YH, Ji YY, Zuo CG, Su YY, Liao NY, Zhang XZ, Zeng YK, Wen F. Correlation between focal choroidal excavation and underlying retinochoroidal disease: a pathological hypothesis from clinical observation. Retina. 2022;42(2):348–356. doi: 10.1097/IAE.0000000000003307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Oh KT, Christmas NJ, Russell SR. Late recurrence and choroidal neovascularization in multiple evanescent white dot syndrome. Retina. 2001;21(2):182–184. doi: 10.1097/00006982-200104000-00017. [DOI] [PubMed] [Google Scholar]
- 54.Rouvas AA, Ladas ID, Papakostas TD, Moschos MM, Vergados I. Intravitreal ranibizumab in a patient with choroidal neovascularization secondary to multiple evanescent white dot syndrome. Eur J Ophthalmol. 2007;17(6):996–999. doi: 10.1177/112067210701700623. [DOI] [PubMed] [Google Scholar]
- 55.Battaglia Parodi M, Iacono P, Zucchiatti I, Bandello F. Choroidal neovascularization associated with multiple evanescent white dot syndrome treated with intravitreal ranibizumab. Ocul Immunol Inflamm. 2018;26(4):608–611. doi: 10.1080/09273948.2016.1247175. [DOI] [PubMed] [Google Scholar]
- 56.Löw U, Palmowski AM, Weich CM, Ruprecht KW. Choroidal neovascularization followed in a patient with “Multiple Evanescent White Dot Syndrome” (MEWDS) —a case report. Klin Monbl Augenheilkd. 2004;221(12):1051–1053. doi: 10.1055/s-2004-813823. [DOI] [PubMed] [Google Scholar]
- 57.Fernández-Barrientos Y, Díaz-Valle D, Méndez-Fernández R, Benítez-Del-Castillo JM. Possible recurrent multiple evanescent white dot syndrome and chroroidal neovascularization. Arch Soc Esp Oftalmol. 2007;82(9):587–590. doi: 10.4321/s0365-66912007000900016. [DOI] [PubMed] [Google Scholar]
- 58.Battaglia Parodi M, Iacono P, Zucchiatti I, Bandello F. Regarding comments by mathis T and kodjikian L on “choroidal neovascularization associated with multiple evanescent white dot syndrome treated with intravitreal ranibizumab”. Ocul Immunol Inflamm. 2018;26(4):614. doi: 10.1080/09273948.2017.1312097. [DOI] [PubMed] [Google Scholar]
- 59.Norooznezhad AH, Mohammadzadeh V, Kadivar S, Ghassemi F. Multiple evanescent white dot syndrome: a case report and experience with corticosteroid therapy. Iran J Allergy Asthma Immunol. 2020;19(S1):91–94. doi: 10.18502/ijaai.v19i(s1.r1).2865. [DOI] [PubMed] [Google Scholar]
- 60.Taira K, Nakazawa M, Takano Y, Ota T. Acute zonal occult outer retinopathy in the fellow eye 5y after presentation of punctate inner choroidopathy. Graefes Arch Clin Exp Ophthalmol. 2006;244(7):880–882. doi: 10.1007/s00417-005-0172-7. [DOI] [PubMed] [Google Scholar]
- 61.Zweifel SA, Kim E, Freund BK. Simultaneous presentation of multifocal choroiditis and acute zonal occult outer retinopathy in one eye. Br J Ophthalmol. 2011;95(2):288,297–288,298. doi: 10.1136/bjo.2008.153254. [DOI] [PubMed] [Google Scholar]
- 62.Gass JD. Are acute zonal occult outer retinopathy and the white spot syndromes (AZOOR complex) specific autoimmune diseases? Am J Ophthalmol. 2003;135(3):380–381. doi: 10.1016/s0002-9394(03)00030-8. [DOI] [PubMed] [Google Scholar]
- 63.Lee GE, Lee BW, Rao NA, Fawzi AA. Spectral domain optical coherence tomography and autofluorescence in a case of acute posterior multifocal placoid pigment epitheliopathy mimicking Vogt-Koyanagi-Harada disease: case report and review of literature. Ocul Immunol Inflamm. 2011;19(1):42–47. doi: 10.3109/09273948.2010.521610. [DOI] [PubMed] [Google Scholar]
- 64.Marchese A, Romano F, Cicinelli MV, Bandello F, Battaglia Parodi M. Chorioretinal punched-out lesions in pseudoxanthoma elasticum. Retina. 2018;38(6):e43–e44. doi: 10.1097/IAE.0000000000002052. [DOI] [PubMed] [Google Scholar]
- 65.Friedmann CT, Knox DL. Variations in recurrent active toxoplasmic retinochoroiditis. Arch Ophthalmol. 1969;81(4):481–493. doi: 10.1001/archopht.1969.00990010483005. [DOI] [PubMed] [Google Scholar]
- 66.Doft BH, Gass DM. Punctate outer retinal toxoplasmosis. Arch Ophthalmol. 1985;103(9):1332–1336. doi: 10.1001/archopht.1985.01050090084037. [DOI] [PubMed] [Google Scholar]
- 67.Mathis T, Delaunay B, Favard C, Denis P, Kodjikian L. Hyperautofluorescent spots in acute ocular toxoplasmosis: a new indicator of outer retinal inflammation. Retina. 2020;40(12):2396–2402. doi: 10.1097/IAE.0000000000002759. [DOI] [PubMed] [Google Scholar]
- 68.Tedesco RC, Smith RL, Corte-Real S, Calabrese KS. Ocular toxoplasmosis: the role of retinal pigment epithelium migration in infection. Parasitol Res. 2004;92(6):467–472. doi: 10.1007/s00436-003-1031-2. [DOI] [PubMed] [Google Scholar]
- 69.Baílez C, Pastor JC. Outer retinal edema or multifocal choroiditis after retinal detachment surgery. A case report. Arch Soc Esp Oftalmol. 2001;76(6):379–384. [PubMed] [Google Scholar]
- 70.Woldoff HS, Dooley WJ., Jr Multifocal choroiditis after retinal detachment surgery. Ann Ophthalmol. 1979;11(8):1182–1184. [PubMed] [Google Scholar]
- 71.Golshani C, Gal-Or O, Giovinazzo V, Freund KB. An elderly patient with acute transient outer retinal disruption resembling bilateral multiple evanescent white dot syndrome. Retin Cases Brief Rep. 2020;14(2):131–136. doi: 10.1097/ICB.0000000000000665. [DOI] [PubMed] [Google Scholar]