Abstract
Background
Penile prosthetic devices are the standard treatment for erectile dysfunction (ED) after failure of maximum medical therapy and conservative options. Several penile lengthening procedures (PLPs) can be performed concurrently with penile prosthesis (PP) insertion in patients with severe ED, penile shortening, and/or Peyronie’s disease to help combat negative emotional and psychological concerns from penile length loss with penile prosthetic device placement.
Methods
An extensive, systematic literature review of the various pre-, intra-, and post-operative techniques that can be applied to preserve, restore or enhance penile length at the time of penile prosthetic implantation.
Results
Numerous pre-operative and post-operative inflation protocols exists with vacuum erection devices and penile traction therapy. Intraoperative surgical techniques include cavernosal sparing and channeling without dilatation, subcoronal incision with circumferential penile degloving and grafting, the sliding technique, the modified sliding technique, the multiple-slit technique, the tunical expansion procedure (TEP), modified TEP, and the auxetic expansion procedure. These approaches can be meaningful to restore and/or preserve length for patients undergoing PP insertion.
Conclusions
PLPs can be performed by surgeons who have extensive penile reconstruction experience and have been trained to do these procedures, as there is significant risk to the patient and limitations to what can be expected. Each patient must be counseled in detail about the risks and benefits of these procedures and have their expectations managed as the average postoperative penile length recovery is around 3 cm and can range from 0–4.0 cm. Future research is needed to identify the appropriate candidate for each approach, and how much length gain the patient can expect.
Keywords: Penile prosthesis (PP), penile lengthening procedures (PLPs), erectile dysfunction (ED)
Highlight box.
Key findings
• Penile lengthening procedures can be performed with concurrent penile prosthesis insertion in patients, though there is significant risk to the patient that requires extensive counselling and limitations to what can be safely expected in average postoperative penile length recovery.
What is known and what is new?
• We identified numerous studies addressing penile lengthening procedures, reflecting the evolving and expanding literature interest of both physicians and patients to address penile length recovery.
• Notable updates include advancements with penile traction therapy with the development of the RestoreX (Pathright Medical, Plymouth, MN, USA) for use in the pre-operative setting prior to penile prosthesis implantation and the introduction of the tunica expansion procedure and auxetic expansion strategies for achieving increased corporal length and girth.
What is the implication, and what should change now?
• Through this review, providers can more appropriately counsel patients on penile lengthening techniques available while placing a penile prosthesis as well as appropriately manage expectations on post-operative results.
Introduction
Penile prosthetic devices are the gold standard treatment for erectile dysfunction (ED) after failure of maximum medical therapy and conservative options. Penile shortening is the most prevalent long-term complaint and cause of patient dissatisfaction after successful placement of either an inflatable penile prosthesis (IPP) or malleable penile prosthesis (MPP) (1,2). After penile prosthesis (PP), patient disappointment ranges between 0–28% as a result of perceived length loss, diminished sensation, and appearance and malpositioning of the prosthetic components (2-6). Many of these concerns such as concealment of the components can be reduced with improved surgical technique. Additionally, various adjuvant techniques can be applied to enhance penile length at the time of PP surgery (2).
One approach to address patient dissatisfaction with PP or in those patients specifically requesting additional or restoration of penile length, is offering a concomitant penile lengthening procedure (PLP). Penile shortening can be associated with several comorbid medical conditions including ED, Peyronie’s disease (PD), priapism with corporal fibrosis, and treatment modalities for prostate cancer (radical prostatectomy, radiation therapy, androgen deprivation therapy) (2,7-9). Those men who present seeking PLP oftentimes overestimate ‘normal’ penile length (10). A pharmacologically induced erection and stretched penile length (SPL) measurement must be performed to set realistic expectations for surgery (11).
PD with associated ED is a scenario where PLP is currently accepted as a treatment option, yet even in those cases there is no consensus on the optimal procedure amongst the experts (12,13). When correcting PD deformities, there are numerous approaches and techniques, including penile plication or corporoplasty, plaque incision or partial excision with grafting, and PP placement with straightening maneuvers. Implantation of a PP is typically reserved for treatment of PD in patients with more severe penile curvature (>60° and/or significant indentation deformity resulting in shaft instability or hinge effect) who also have or are at increased the risk of developing ED post-operatively. Additionally, PP placement is suggested for those with severe ventral curvature, as ventral grafting poses a significant risk of postoperative ED (14,15). If the curvature after implantation is >30° and the patient wishes optimum straightening, first-line supplemental treatment includes manual modeling. If persistent residual curvature (>30°) remains after manual modeling, further surgical procedures such as tunical plication, plaque incision or excision with or without grafting may be indicated (16-21).
Regardless of the pathophysiology leading to the need for PP, we aim to review and provide an update on the expanding literature regarding techniques to preserve and enhance penile length with PLP during PP. As a whole, the quality of studies published in the literature over the last decade remains low. Scientific evidence regarding efficacy and safety of intervention is lacking. The majority of scientific evidence is based on studies with poor internal validity (observational designs, non-standardized methodologies, heterogeneous populations) and single surgeon experiences. Additionally, most reviews analyze changes in penile dimensions inconsistently, underscoring the lack of consensus regarding safety and efficacy outcomes as well as patient satisfaction, all of which are inconsistently reported (22).
Currently there is no consensus among experts on a particular PLP or when they should be performed to optimize outcomes. Additionally, the concept of penile lengthening is confusing as numerous procedures that do not increase corpora cavernosa length exist in the literature. Previously, attempts have been made to classify PLP as only those that actually increase corpora cavernosal length. Other procedures that only lengthen the shortened side to straighten the erect penis without actual elongation of the total penile length can be classified as penile restoration procedures (PRPs). PRP aim to equalize corpora cavernosa asymmetry and include plaque incision and partial plaque excision and grafting (PEG), with a variety of different grafts with or without PP (1). We present this article in accordance with the PRISMA reporting checklist (available at https://tau.amegroups.com/article/view/10.21037/tau-23-354/rc).
Methods
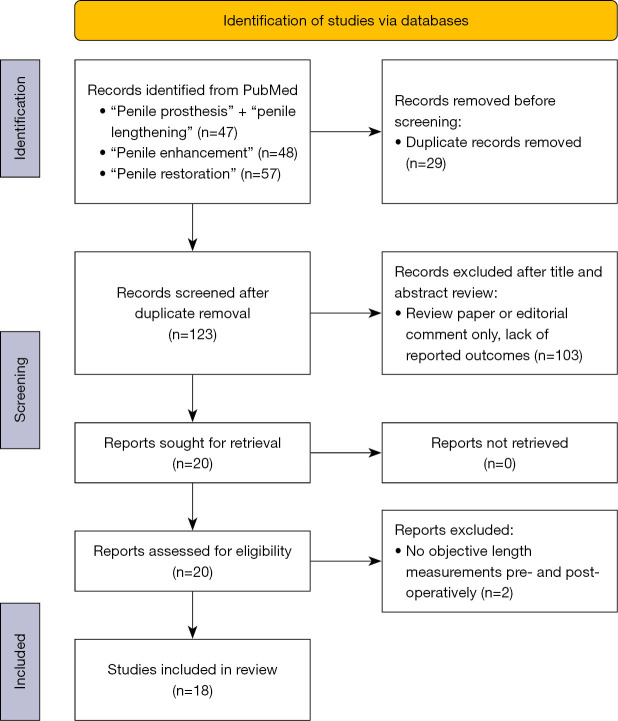
This review article presents a description of reports within the literature as well as the authors’ experience with pre-operative, intra-operative, and post-operative protocols that allow for enhancement of penile length while undergoing PP implantation. An extensive, systematic literature review was performed using PubMed over the past 10 years. Search timeline included all results from March 2013 to March 2023. Only studies published in English were included in this systematic review. Keywords used included “penile prosthesis” with “penile lengthening”, “penile enhancement”, and “penile restoration”. The search was intentionally broad to allow for wide-review of peer-reviewed papers. All authors reviewed and discussed studies to be included. To meet inclusion, all articles had to have new patient reported outcomes with subjective and/or objective penile length outcomes. At completion of reading each included study, we manually reviewed references to ensure additional publications were not excluded. These were then reviewed, and we include only those procedures that are designed to lengthen the penile shaft and not just give the perception of length gain. Additional studies with subject matter for historical referencing of PLP in this manuscript were included with their contemporary comparison, even if original publication was before 2013. A Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) flow diagram of the study selection process is presented in Figure 1 (23).
Figure 1.
PRISMA 2020 flow diagram of the systematic review study selection process.
Key findings and potential impacts
We identified numerous studies addressing PLP, reflecting the evolving and expanding literature interest of both physicians and patients to address penile length recovery. There is significant updates and modernizations over the last decade to the various pre-, intra-, and post-operative techniques utilized for PLP. Through this review, providers can more appropriately counsel patients on techniques available as well as appropriately manage expectations on post-operative results. Notable updates include advancements with penile traction therapy with the development of the RestoreX (Pathright Medical, Plymouth, MN, USA) for use in the pre-operative setting prior to PP implantation and the introduction of the tunica expansion procedure (TEP) and auxetic expansion strategies for achieving increased corporal length and girth.
All clinical procedures described in this study were conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethical approval was not required as no human subjects or animals were involved in this literature review. All images in publication are completely unidentified and there are no details on persons mentioned within the text.
Results
PLPs
Many different surgical techniques have been developed over the last decade. The initial PubMed search returned 152 articles, 29 were excluded for duplication. Abstracts and titles were read for 123 remaining papers. The majority of these articles were review papers without original data or patient reported outcomes. Additionally, many articles were not specific to PP surgery. A total of 18 articles were ultimately included the pre-operative, post-operative and PLP comparison of study results and parameters are summarized in Table 1. When looking at only those techniques that increase true penile length, several intraoperative surgical techniques have been reported. These include cavernosal sparing and channeling without dilatation, subcoronal incision with circumferential penile degloving and grafting, the sliding technique, the modified sliding technique (MoST), the multiple-slit technique (MuST), the tunical expansion procedure (TEP), modified TEP, and the auxetic expansion procedure.
Table 1. Pre-operative, post-operative and penile lengthening procedure comparison of mean penile length gain.
| Techniques | Mean length gain | Description | Publication(s) |
|---|---|---|---|
| Pre-operative/post-operative | |||
| Penile traction therapy | 1.5 cm | 30–90 min daily (RestoreX), 2–4 hours daily for 2–4 months | Ziegelmann et al. 2019, Levine and Rybak 2011 |
| Penile traction therapy and CCH injections | 1.9 cm | CCH alone versus CCH and PTT (non RestoreX) versus CCH and RestoreX | Alom et al. 2019 |
| Vacuum erection device | 0.8–3.5 cm | 10 min at least once daily 2 months pre-op | Sellers et al. 2013 |
| 10–15 min twice daily for minimum 3-months in patients with severe corporal fibrosis | Tsambarlis et al. 2017 | ||
| 10–15 min daily for 30 days pre-op | Canguven et al. 2017 | ||
| Post-operative inflation protocols | 1 cm | 6–12 months post-operative inflation of prosthesis for 1–2 hours a day | Henry et al. 2015 |
| Penile lengthening procedures | |||
| Cavernosal sparing | 1.2–2.0 cm | No cavernosal dilation, or only up to 8-Fr dilation at time of PP implantation | Moncada et al. 2010, ZaaZaa et al. 2019 |
| Sub-coronal incision | 0.6–2.8 cm | Circumcising incision with circumferential penile degloving to penoscrotal junction for IPP implantation | Sansalone et al. 2012, Weinberg et al. 2016 |
| Sliding technique | 3.2 cm | NVB and corpora spongiosum raised off corpora cavernosa, lateral longitudinal semilunar dorsal and ventral incisions made in corpora, then incisions patch grafted | Rolle et al. 2016 |
| MoST | 3.1 cm | Sliding technique without grafts | Egydio and Kuehhas 2015 |
| MuST | 3.1 cm | Multiple pairs of dorsal and ventral semilunar incisions, instead of two with classic sliding technique | Egydio and Kuehhas 2018 |
| Sliding technique and MuST (nondegloving ventral incision) | 2.6 cm | Nondegloving technique to potentially avoid vascular complications to the glans penis | Clavell-Hernández and Wang, 2018 |
| TEP (subcoronal incision) | 3.3 cm | Subcoronal approach with IPP cylinders intentionally upsized 2 cm larger than measurements, multiple small, staggered incisions in mesh pattern along tunica albuginea | Egydio 2020 |
| TEP (scrotal incision) | 2.8 cm | Scrotal approach with complete eversion of the penis with multiple small, staggered incisions along tunica albuginea | Razdan et al. 2024 |
| Auxetic expansion | 1.4 cm | Star-shaped TA incision (auxetic) principle to simultaneously increase length, girth, and volume | Miranda 2022 (J Urol) |
CCH, collagenase clostridium histolyticum; PTT, penile traction therapy; IPP, inflatable penile prosthesis; NVB, neurovascular bundle; MoST, modified sliding technique; MuST, multiple-slit technique; TEP, tunica expansion procedure; TA, tunica albuginea.
Cavernosal sparing and channeling without dilatation
Corporal preservation during IPP surgery was described by Moncada et al. in 100 patients undergoing IPP surgery with increase in penile length and improvements in the mean International Index of Erectile Function scores at 3- and 6-month post-operatively. Penile non-dilation resulted in greater penile length in the immediate post-operative period (10.2 vs. 8.5 cm), 3-month post-operative (10.1 vs. 8.3 cm), and 6-months post-operative (10.0 vs. 8.0 cm), although activated PP length was not obtained (24). Later, this was studied in a prospective randomized fashion in 92 patients by ZaaZaa et al. comparing minimal dilation of the corpora with an 8-Fr dilator vs. serial dilation during MPP placement. While their primary end point was improved spontaneous tumescence, they did identify improved penile girth (11.2 vs. 10.1 cm) (25). Cavernosal sparing and channeling without dilatation remains an option primarily for those who desire sensation of spontaneous tumescence, and while strong evidence is lacking, there may also be some limited penile length and girth benefits.
Subcoronal incision with circumferential penile degloving and grafting
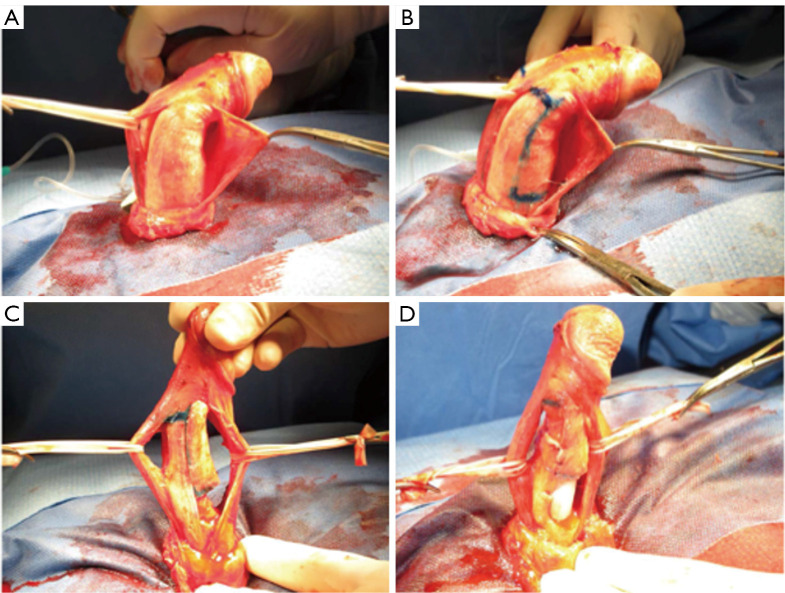
It has been suggested that long-standing ED can lead to loss of penile elasticity and as a result, dartos fascia tethering onto the underlying tunica albuginea (TA) resulting in loss of erect penile length (26). The subcoronal approach to IPP placement allows for complete penile degloving and release of the underlying dartos attachments. The subcoronal approach begins with a distal circumcising incision 2 cm proximal to the coronal sulcus of the glans. The penis is completely degloved proximal to the penoscrotal junction. A corporotomy is made, followed by proximal and distal dilation dorsally to the level of the mid-glans. The entire urethra and corporal bodies are visualized throughout device insertion, and penile modeling, plication sutures, relaxing incisions with or without grafting, and glans fixation can be performed to correct curvature, indentation deformities, or a hypermobile glans (Figure 2) (27).
Figure 2.
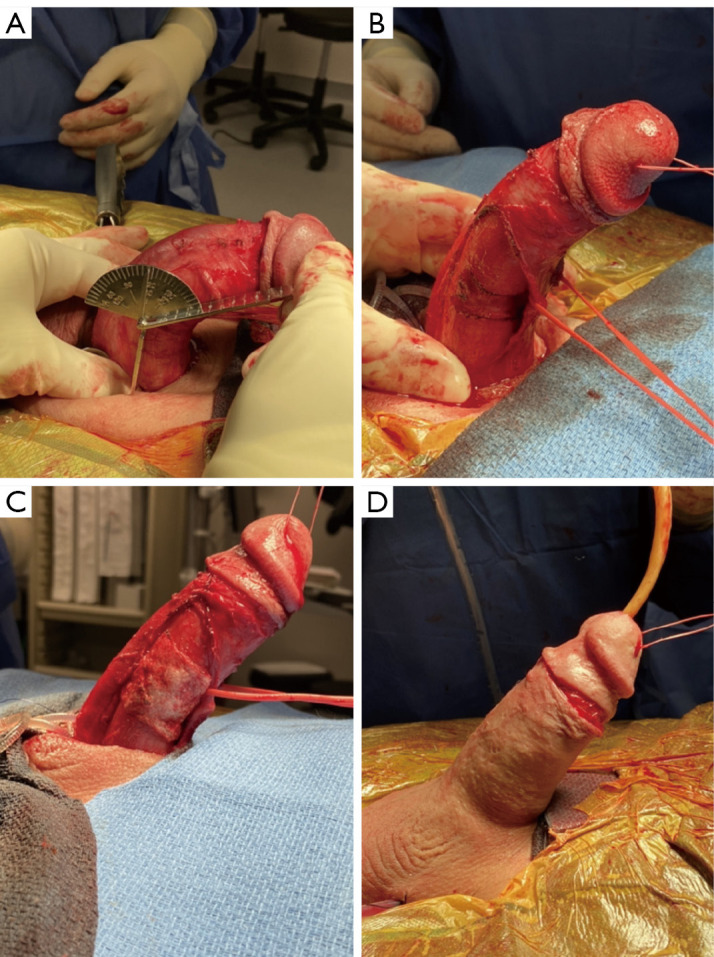
The subcoronal approach to IPP placement. (A) After complete penile degloving and release of the underlying dartos attachments a reassessment of deformity with goniometer is obtained. (B) After mobilization of the neurovascular bundle, and device implantation, the area of maximum deformity is marked prior to incision and grafting. (C) After prosthesis and excision and graft placement, a functionally straight penis with IPP in place is shown. (D) An approximation prior to closure of a cosmetic circumcision line. IPP, inflatable penile prosthesis.
In 2012, Sansalone et al. described 23 patients with PD and ED with severe penile shortening who underwent subcoronal penile degloving, neurovascular bundle (NVB) elevation, and ventral urethral release with improved post-operative penile length. After artificial erection was induced, a bisector line was incised circumferentially in the TA at the area of maximum curvature allowing expansion of the cavernosal tissue limited by the length of the NVB. The IPP was then inserted and the exposed tunical defect was covered with a graft. Outcomes included, a mean 2.8-cm penile length gain, with 20% reporting decreased glans sensitivity, 15% with residual curvature, and an overall patient satisfaction rate of 90% (28). Weinberg et al. later published their series of 200 patients undergoing subcoronal IPP. Additional reconstructive procedures were performed in 46% of patients who had concurrent PD and ED with 24% of patients undergoing tunical plication and 22% undergoing relaxing incisions, with no patients undergoing grafting. Overall, they saw a mean gain in penile length of 0.6 cm, with no patients having a measured length loss (27). In addition, the subcoronal incision allows for multiple different PLP by providing access to the entire shaft, which will be further described in subsequent sections.
Double dorsal-ventral patch graft: “Sliding Technique”
Utilizing a subcoronal penile degloving incision, this approach raises the NVB off the entire penile shaft. Similarly, the corpus spongiosum is elevated from the corpora cavernosa. Bilateral 4-cm longitudinal incisions are made through the TA at 3 and 9 o’clock. Then, a semicircular proximal incision is made dorsally, and a similar distal incision is made ventrally connecting the two longitudinal incisions. Gentle traction on the glans is placed to allow for penile lengthening resulting in two rectangular defects. The longitudinal incisions of the TA are then secured with absorbable sutures and the tunical defects are covered with grafts. A PP is then placed through the proximal incision in standard fashion with a drain left before closure (29).
In 2012, Rolle et al. first published their series on the sliding technique to achieve penile lengthening in patients with PD and severe penile shortening. The study was limited to only 3 patients with no major complications reported and an average increase in penile length of 3.2 cm. In a subsequent larger series of 28 patients (7 with MPP and 21 with IPP), they looked at both porcine small intestinal submucosa and acellular porcine dermal matrix to cover the tunical defects. In this series, mean penile length gain was 3.2 cm at a mean follow-up of 37 months. Post-operative complications included 1 patient (3.5%) required a blood transfusion, and 1 had a MPP device infection requiring removal (30).
MoST
Initially introduced in 2015, MoST is a modification of the previously described sliding technique, which allows penile lengthening and widening without grafting. Again, this approach uses a subcoronal incision. Elevation of Buck fascia, urethra, and cavernosal incisions are the same as the sliding technique. However, in this approach, the ventral semicircular incision (from 3 to 9 o’clock) is performed 2 cm proximal to the coronal sulcus (ventral incision is distal) and the dorsal incision is 1–2 cm distal to the penoscrotal junction (dorsal incision is proximal). The prosthesis is then placed through two separate corporotomies that are created proximal to the dorsal semilunar incision. These corporotomies ensure a proximal point of exit of the implant cylinder tubing. The modification avoids grafts at the sites of the tunical defects. The proximal defect is covered by Buck fascia using 4-0 running Monocryl suture and the distal defect is covered by compression of the corpus cavernosum and spongiosum (31).
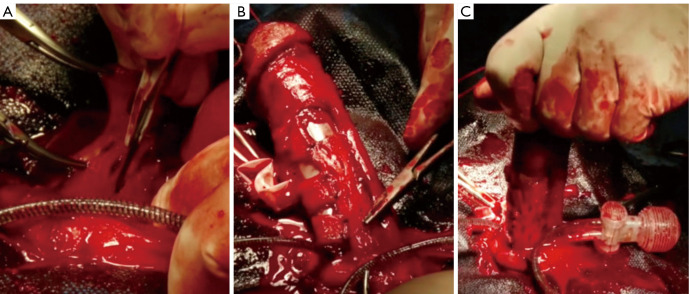
The initial series had a median 9.7-month follow-up of 143 patients (133 with MPP and 10 with IPP) with a mean penile length gain of 3.1 cm (32). Representative images from their series and technical steps are detailed in Figure 3. The most feared complication with this approach, and the original sliding technique, is glans necrosis. Wilson et al. published on a series of 21 patients with glans necrosis after undergoing PP using a variety of advanced techniques. Of the 21 patients, 7 (33%) had extensive urethral and NVB mobilization that the authors believed compromised distal penile circulation. Additionally, 7 (33%) patients had undergone sliding-technique or MoST procedures for penile lengthening. The authors recommended if there are signs of impending glans necrosis (usually presenting with a dusky glans <24 hours post-operatively), immediate PP removal may prevent subsequent glans necrosis (33).
Figure 3.
Modified from ref. (32). (A) Mobilization of the neurovascular bundle and urethra in preparation for sliding technique. (B) Incisions marked for sliding technique. (C) Stretched penis after incisions for sliding to restore penile length. (D) Malleable penile prosthesis inserted into corpora through tunical defects.
MuST
The next modification of the MoST technique, included multiple pairs of dorsal and ventral hemi-circumferential incisions. This allowed for multiple sliding sections to distribute the expansion of tunical tissues instead of a single set of dorsal and ventral longitudinal incisions and two hemi-circumferential tunical incisions. MuST tries to overcome the potential bulging of cylinders through larger tunical defects by dispersing the pressure amongst multiple small tunical defects, thus avoiding grafting, cylinder bulging and tunic gap sensation at the tunical defects. Another distinctive feature of the MuST is the placement of multiple small longitudinal slits on the TA. These longitudinal slits help restore girth of the penile shaft in areas where an indentation or narrowing is present (34). An additional modification of the tunical incisions consists of multiple forked transverse incisions on the side of the curvature rather than using the sliding technique (35).
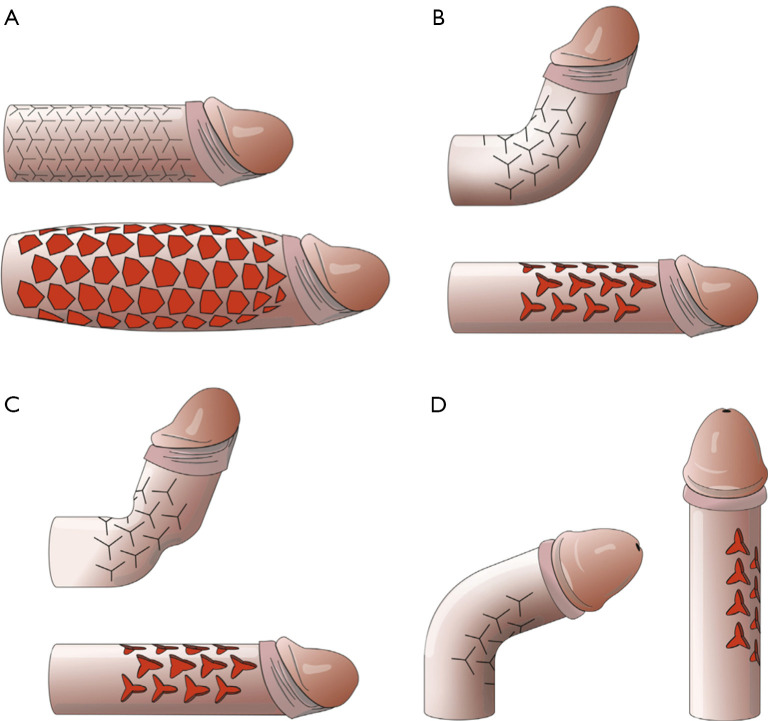
The initial series on the MuST procedure included 138 patients (103 with MPP and 35 with IPP) with a mean penile length gain of 3.1 cm. Follow-up was a median 15.2 months with 1-major complication of glans necrosis despite urethral dissection being minimized. Zero devices were explanted for infection (34). Representative images from their series and technical steps are detailed in Figure 4. A separate cohort reviewed their experience with the sliding technique in 7 patients, using a combination of subcoronal degloving (2 patients) and non-degloving ventral incisions (5 patients). They believed the non-degloving ventral incision would offer better preserving blood flow to the glans penis. The study used a combination of the original sliding technique (5 patients) and the MuST approach (2 patients). In this series, the mean degree of curvature was 66° pre-operatively with no residual curvature at the end for 6-patient, and 15° in 1-patient at mean 15.5 months post-operatively. Mean penile length gain from pre-operative SPL was 2.6 cm, though breakdown between approaches was not reported. There were no reported explanted devices for infection, nor cases of glans necrosis (36).
Figure 4.
From ref. (34). Multiple small relaxing tunical incisions are performed in a rhomb-like configuration, allowing for penile girth restoration from lost tunical elasticity in the setting of inflatable penile prosthesis implantation.
TEP
Initially described in 2018, TEP is another non-grafting technique to achieve penile lengthening. After penile degloving and dissection of the NVB and urethra, a three-piece IPP is inserted through the standard approach, but the cylinders are intentionally upsized 2 cm from the original corporal measurements. The TA is then expanded in girth and length by performing multiple small incisions in a mesh pattern until satisfactory curvature correction is achieved and adequate girth and length are restored. As all tunical incisions are less than 1 cm in length, the risk of aneurysm of the cylinders is minimal and grafting of the defect was felt by the author to not be necessary (37).
In 2020, Egydio described a modification of the TEP approach. At a mean follow-up of 12 months in 416 patients with ED (361 with MPP, 55 with IPP), of which 287 (69%) had concurrent PD they found an estimated intraoperative penile length gain of 3.3 cm. As compared to previous studies, in these patients, there was no urethral separation performed. Complications included postoperative hematoma (20%), temporary partial glans numbness (4%), temporary anorgasmia (up to 4 months) (7%), and PP infection (0.2%) (38).
In 2024, Razdan et al. described another modification of the TEP. Their series via a scrotal approach involves complete eversion of the penis with dissection of Buck fascia off the underlying TA. Then staggered incisions of the TA are performed to allow circumferential girth enhancement and lengthening. In those with PD, the staggered full-thickness tunical incisions are preferentially on the side of the plaque to straighten without loss of length. In their series, 32 patients with concurrent ED and PD underwent modified TEP with a mean increase in length of 2.8 cm (measured using Furlow before and after penile eversion with TEP). Additionally, they found a mean increase in girth of 1.6 cm. They reported no complications (39).
Overall, the TEP strategy is based on recovery of tissue by expansion instead of substitution, which allows penile enlargement to the limit of the dissected NVB. The multiple, small (5–8 mm in length), staggered incisions (spaced 2–3 mm apart) positioned on the TA in a meshed pattern promote length and girth enlargement in the TEP strategy (11). Additional care must be made to avoid compromising tunical strength with cross-mesh. To avoid this, vertical and horizontal cuts must be made independently, with only vertical cuts used to correct narrowing, indentations and hourglass deformity. Then in a second stage, only horizontal cuts may be used to treat shortening by elongation of the penis but only in areas adjacent to the cuts made in the first stage (40). The largest possible cylinders and the smallest possible rear tip extenders should be used to avoid diminished axial rigidity (11). The average reported length gain following these procedures is around 3 cm. However, it is impossible to anticipate pre-operatively as it depends on the laxity of the NVB and Buck Fascia once it is elevated off the TA. This must be discussed pre-operatively so patients can clearly understand that while length can be provided, it is not without limitations.
Auxetic expansion
Originally conceptualized in 2021, a research article introduced the experimental technique of a star-shaped TA incision (auxetic) principle to correct fibrotic penile alterations with knotted cotton fabric models (simulating a straight corpus cavernosum). This approach was proposed to simultaneously increase length, girth and volume. At the time, this was only a conceptual and experimental technique awaiting clinical evidence. They compared the auxetic incisions to the mesh pattern model previously discussed. In their article, the fabric cylinders lengthened by 40% in both incision techniques (longitudinal expansion from 10 to 14 cm). The mesh cohort however had a girth reduction of 12% (from 8 to 7 cm). The auxetic technique however resulted in girth expansion of 50% (from 8 to 12 cm). The results of this study demonstrated auxetic incisions expanded the fabric cylinder in both penile length and circumference, while the mesh incisions only expanded in length or circumference. The resulting final volume obtained using the auxetic technique was 2.9-fold greater than that of the mesh technique (41). Illustrated images from their series are provided in Figure 5. A video with the auxetic technique in two patients is available, but a full-text article has yet to be published showing long-term results in cases (42).
Figure 5.
From ref. (41). An illustrated version of auxetic technique: (A) circumferential auxetic incisions simultaneously enhance length and girth. (B) Unilateral auxetic incisions to correct dorsal curvature. (C) Unilateral auxetic incisions to simultaneously correct dorsal curvature with an hourglass deformity. (D) Unilateral auxetic incisions to correct lateral curvature.
More recently in 2022, a case series of 7-patients was published in abstract form regarding their outcomes using the auxetic technique with the auxetic guide device prior to PP implantation to correct any penile curvature without a graft. They found a mean resultant length gain of 1.4 cm. All patients were able to have corporal dilation to 13 mm in diameter, despite reported extensive corporal fibrosis initially. Post-operatively one uncircumcised patient developed paraphimosis requiring surgical correction, but no additional complications were reported. All curvature was reported corrected at a mean follow-up of 10.1 months (43). While safety and efficacy data in both the short and long-term is limited, the auxetic technique may be an additional PLP that can be performed concurrently with PP insertion, especially in those with extensive fibrosis. However, until more data is released on this largely experimental technique, implementation of this approach should be used with caution.
Pre-operative and post-operative protocols
In addition to the actual PLP, there are numerous pre-operative and post-operative protocols that can be used to augment PLP for optimal outcomes. Vacuum erection devices (VEDs) and penile traction therapy (PTT) are non-surgical treatment options that have been used in the treatment of PD and ED for penile lengthening, and as adjunct to surgical interventions such as PP surgery and radical prostatectomy (44). Several pre-operative protocols using a VED as well as PTT were found for penile length preservation and enhancement. In non-operative management of PD patients, traction duration was shown to play an important role in outcomes where patients who utilized PTT for ≥3 hours daily, in conjunction with intralesional verapamil (every other week for 24 weeks, 12 injections) and oral therapies (L-arginine/pentoxifylline), had mean curvature improvement of 26.9° (compared to 20.9° without, P=0.22), mean SPL improvement of 0.6 cm compared with 0.7 cm loss in those who used PTT <3 hours (P=0.09) (45). Another study found PTT use was associated with improved SPL for men receiving concurrent intralesional interferon when PTT was used for at least 3 hours/day. Patients had curvature improvement of 8.1° with treatment (compared to 9.9° without, P=0.49). In those receiving intralesional interferon and utilizing PTT, they had a measured 4.4 mm increase in SPL vs. a 1.3 mm increase in the injection-only group (P=0.04) and a 2.4 mm increase in SPL in the group with any use of PTT at all (P=0.56), thus emphasizing with strict adherence, concomitant PTT therapy causes a small increase in SPL among PD patients receiving interferon α-2b injections (46). In contrast, when looking at PTT duration in patients who underwent intralesional collagenase clostridium histolyticum (CCH), no significant difference was identified in SPL between PTT group and non-PTT group, though there was a mean +0.4 cm in the PTT group and −0.35 cm in the non-PTT group (P=0.21). Patients had curvature improvements from baseline curvature of 66.7° to 20.9° post CCH (P<0.0001). Calcified plaque was present in 16% of patients included in the cohort, not statistically different between groups (P=0.38). They did note the difficulties with real-world implementation of PTT, as just 25% of patients used PTT for the recommended >3 hours/day and they found no significant difference in SPL based on PTT duration (47).
An additional study by Ziegelmann et al. evaluated outcomes with a second-generation traction device known as RestoreX (Pathright Medical, Plymouth, MN, USA) in a randomized, controlled, single-blinded intention-to-treat analysis where 100 patients were randomized to PTT daily for 30–90 minutes versus no traction for 3 months. This device differs from the original class of traction devices by providing a dynamic adjustment system and ensures appropriate traction is being applied with a counterbending component, and a modified clamp that allows for increased displacement of force. The authors found a significant improvement in penile curvature (−11.7° vs. +1.3°, P<0.01) and SPL (+1.5 vs. 0 cm, P<0.001) when comparing treatment arms with controls, and this was the first study to show improvements with PTT duration <3 hours daily (48). Follow-up data on this study included a 3-month open-label phase following the previous treatment phase, where all patients (control and treatment) were given the option to use RestoreX. Follow-up data taken over the next 6-month showed the PTT group had an additional length gain of +0.6–0.8 cm without further curvature improvements, and those in the original control group had length gain of +1.7–2.0 cm and curvature improvements of 18–20%. Of men treated for 6-month, 95% of men experienced penile length gains (mean 2.0–2.2 cm, P<0.001) and 61% had curvature improvements of 16.8–21.4° (32.8–35.8%, P<0.001) (49). A subsequent study compared RestoreX to other PTT devices and found that in 113 PD patients, those undergoing treatment with RestoreX with CCH had a mean +1.9 cm penile length increase compared to −0.4 cm (CCH + other PTT devices) and −0.7 cm (CCH alone) (P<0.001). The RestoreX group also demonstrated significantly improved curvature of 33.8° (49%) (CCH + RestoreX) vs. 19.2° (30%) (CCH + other PTT devices) vs. 20.3° (31%) (CCH alone) (P<0.001) (50). In our experience, in patients deferring or delaying operative intervention and when patients are compliant with usage recommendations, PTT can aid in some length restoration typically not exceeding 1.5–2.0 cm.
When looking at operative outcomes, pre-operative use of PTT and VED have been shown to have a positive effect on post-IPP penile length. PTT as monotherapy or as part of a treatment protocol was first published in 2008 involving 10 patients who utilized PTT for 2–8 hours daily for 6 months with objective curvature improvements (10–45°) and increase in SPL (0.5–2.0 cm) (51). Additional literature on PTT before PP surgery resulted in length gain in 70% of men with daily use for 2–4 hours a day for up to 4 months. Compared to pre-traction pre-operative SPL, there was up to 1.5 cm post-operative measured erect length gain, with no patients having perceived length loss after surgery (52). Rybak et al. also found that in PD patients who underwent tunica albuginea plication (TAP), or partial plaque excision and grafting (PEG) and PTT use for >2 hours daily for 3 months starting 3–4 weeks post-operatively, had positive changes in penile length compared to the control group. TAP patients gained +0.85 cm compared to −0.53 cm in the control group (P<0.001) and PEG patients gained +1.48 cm compared to +0.24 cm in the PEG non-PTT control group (P<0.001) (53).
When looking specifically at VED use, Sellers et al. introduced a protocol that involves preoperative use of a VED in an effort to limit penile length reduction after IPP surgery in hopes that it will restore corporal length and girth from disuse atrophy pre-operatively. In their protocol, patients were instructed to use VED for 10 minutes at least once daily for up to 2 months before surgery. After IPP placement, the prosthesis remained 50% inflated for 48 hours, and then to 25% inflation for 9–12 days. Additionally, they were instructed to inflate the device within 2 weeks of surgery and to remain inflated for approximately 1 hour before deflating it to allow pseudocapsule formation around the inflated cylinder rather than the deflated one. Following this protocol, the authors reported an average cylinder length increase by 3.5 cm (54). Whether this increase also resulted in a measured increase in shaft length was not reported. A retrospective study of 13 patients with severe corporal fibrosis prior to IPP placement that used a daily VED pre-operatively for at least 10–15 minutes/twice daily for a minimum of 3-month had softening of corporal fibrosis facilitating placement of prosthesis with a mean average SPL increase of +0.92 cm with VED and prosthesis compared to pre-operative SPL (P=0.20) (55). In a later randomized study of 51 patients, Canguven et al. reported a mean increase in SPL of 0.8 cm when a VED was used 10–15 minutes daily for 30 days prior to insertion of IPP (P<0.05) (56).
Additionally, many high-volume implanters would suggest that aggressive prosthesis sizing with detailed post-operative inflation protocols can help preserve penile length. A multi-center study by Henry et al. in 2015 examined men who underwent aggressive cylinder sizing followed by a 6- to 12-month post-operative protocol that involved post-operative inflation of their prosthesis for at least 1–2 hours a day. They reported an approximate 1 cm increase in length (P=0.006) and girth (P=0.001) at 1-year follow-up, and 74.2% of these patients perceived longer penile length (57). In our experience, those men who express concern about losing more length pre-operatively are encouraged to use PTT daily for up to 3 months to optimize length prior to IPP placement, followed by a post-operative protocol similar to the one reported by Henry et al. (57). In summary, VED and PTT have shown marginal, but real benefits as nonsurgical therapies to elongate the penis prior to PP implantation.
Discussion
Comorbidities associated with ED, including PD, prior prostate cancer treatment, diabetes, and obesity are associated with loss of penile length (2). In this setting, PP surgery can adjunct as a cosmetic procedure to improve distress associated with reduced penile length as well as optimize penile functionality. In the last decade, there have been numerous studies addressing PLP, reflecting the evolving interest of both physicians and patients to address penile length recovery. This technique moved from large corporal defects with or without grafting (29,32,34) to small defects using the skin mesh principle (37-39). For patients with shortening of their true corporal length, particularly in the setting of concurrent PD, a variety of approaches have been developed. All 3 sliding techniques (sliding technique, MoST, and MuST) as well as the TEP, are typically performed via a subcoronal approach, but can also be done via an infrapubic or penoscrotal approach by inverting the penis (2). All of the described PLP’s are quite complex to perform and can be associated with devastating complications. Therefore, these procedures should only be performed in centers of excellence with experience in performing them. These institutions will be responsible to train surgeons who would like to offer these procedures to their patients.
We have adopted the TEP, performed via a subcoronal incision, but we have modified the approach in two ways, first to limit vascular compromise to the glans we only elevate Buck fascia and NVB to correct dorsal and dorso-lateral curves, or the urethra and leave the NVB in situ for ventral deformities. We do not recommend elevating both structures. We also cover our tunical incisions with one or more Tachosil grafts (Baxter Healthcare, Deerfield, IL, USA), to reduce post-operative bleeding and provide additional shaft support during the healing phase. Second, we make the majority of our releasing incisions prior to placement of the IPP so we can more accurately measure the expanded intra-cavernosal length (Figure 6). In our experience, we have seen from as little as no length gain to as much as 4 cm. Typically, we see around 3 cm of length gain. We always discuss pre-operatively the limitations of length recovery with this procedure. We are now injecting diluted papaverine into the glans, proximal corpus spongiosum, and at the base of the penis dorsally near the NVB to enhance blood flow to these structures and to reduce the risk of distal ischemia. The use of papaverine injection was a modification of technique suggested by Dr. Egydio to attempt to vasodilate the vasculature in the structures supporting blood flow to the glans and thereby reduce the most dreaded risk of glans ischemia. We recommend doing this in addition to our modifications to only elevate Buck fascia and NVB to correct dorsal and dorso-lateral curves, or the urethra and leave the NVB in situ for ventral deformities. Again, we do not recommend elevating both structures.
Figure 6.
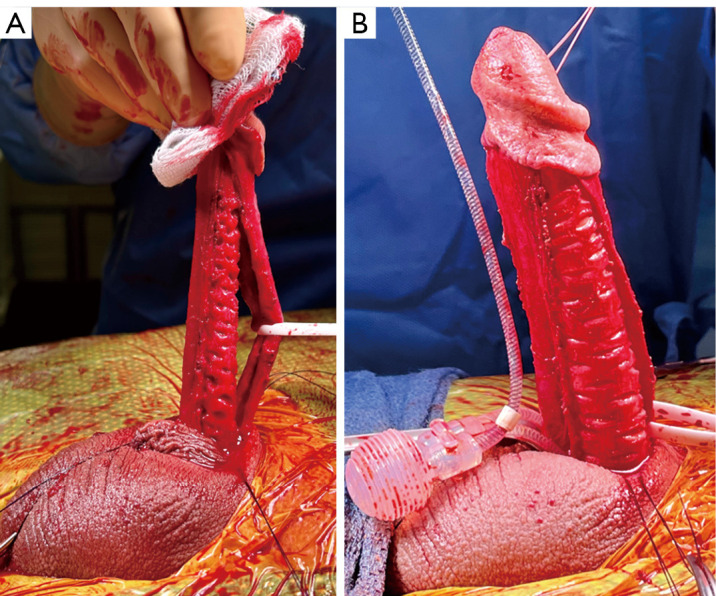
The tunica expansion procedure. (A) After subcoronal incision with penile degloving and dissection of the neurovascular bundle, the tunica expansion procedure is performed with transverse “lengthening” (5–8 mm in length) and staggered incisions (spaced 2–3 mm apart) positioned on the tunica albuginea in a meshed pattern before an inflatable penile prosthesis placement and Tachosil grafting (Baxter Healthcare, Deerfield, IL, USA). (B) A representative tunica expansion procedure patient with IPP in place. IPP, inflatable penile prosthesis.
This review aims to provide an update on the expanding literature regarding techniques to preserve and enhance penile length. Notable updates include advancements with penile traction therapy with the development of the RestoreX (Pathright Medical, Plymouth, MN, USA) (28) for use in the pre-operative setting prior to IPP implantation and the introduction of the TEP and auxetic expansion strategies for achieving increased corporal length and girth (52).
Patient selection and setting realistic expectations are imperative prior to treatment selection (1). Preoperative discussion may reveal more generalized psychiatric problems such as body dysmorphic disorder, and in these cases, involvement of a mental health specialist would be of great value (58). Furthermore, extensive patient and partner counseling is paramount to set proper expectations before surgery. The use of pre-operative and post-operative protocols are not well studied in a randomized manner; however, published reports suggest improvement in outcomes of length and girth. These protocols are largely patient driven, and when appropriately performed with patient compliance, positive results have been seen. Additionally, device selection is an important component of PP surgery. Numerous devices exist, but the two traditional manufacturers for penile implant in the USA are Coloplast and Boston Scientific (59). From these companies, devices include the Titan (Coloplast, Minneapolis, MN, USA), Genesis Malleable (Coloplast), AMS 700 LGX (Boston Scientific, Marlborough, MA, USA), AMS 700 CX (Boston Scientific), AMS 700 CXR (Boston Scientific), Tactra (Boston Scientific). Also, a 2-piece IPP exists the AMS Ambicor (Boston Scientific). While the nuances of each device are out of the scope of this paper, and all devices, can be used during concurrent PLP, 1 device emphasizes length expansion in those without fibrosis or scarring, the AMS 700 LGX (Boston Scientific). In a prospective study of 45 patients, those who underwent AMS 700 LGX (Boston Scientific) implantation had a mean 10% increase (1.3±0.4 cm) from baseline to 12 months, and an 80% satisfaction rate with penile length without concomitant PLP’s (60). However, another prior, single armed, prospective, two-center study, this device was able to maintain SPL in only 23.1% of patients. They suggest that implantation of the AMS 700 LGX (Boston Scientific) cylinders alone are not sufficient for increasing SPL, but acknowledge that this was prior to their post-operative inflation protocol being implemented that may have improved outcomes (61). More recently a newer company Rigicon (Ronkonkoma, NY, USA) is offering an IPP that also promotes length and girth expansion, the Infla10 AX. Initial studies with all of their implants have shown freedom from revision comparable to the existing devices, however they are still in the process of obtaining Food and Drug Administration (FDA) clearance in the US (59,62). The Rigicon implants are already available in many countries outside the US, however, initial published studies report on the first 545 patients implanted with all Rigicon Infla10 devices (34.7% of which are Infla 10 AX), and report similar safety data for mechanical failure, device infection, but do not report on real world impact on penile length preservation (62). The discussion of which PP should be utilized is another of the many nuances involved in these operations, unfortunately, most manuscripts at this time do not publish their specific device utilization, so direct comparisons is difficult to perform. Future papers on PLP can hopefully be transparent on specific device usage to allow for further evaluation and insight on optimal implant for selected PLP approaches. In combination with device selection, the intraoperative PLP approaches discussed can restore and/or preserve length for patients undergoing PP insertion and although low complication rates are reported, those that have been seen can be devastating.
This review is not without limitations, primarily owing to a limited number of patients in reported studies, and the non-randomized retrospective approach to those studies. Statistical analysis in this review was not performed given the fact that studies reported different metrics for penile length evaluation and outcomes. Additionally, many of the studies referenced are very small clinical outcomes series, with great heterogeneity of interventions and parameters of outcome reporting. Therefore study-level or outcome-level statistical analysis between surgical approaches is not feasible. This affected the ability to assess for risk of bias, which can be a limitation in systematic reviews (63). Also, this review reports the senior author’s experience without statistical data supporting clinical outcomes and complications. The feasibility and safety of these approaches in all settings cannot be concluded from this article, as it summarizes numerous prior reports, many of which were not randomized with appropriately selected controls, nor prospective.
Conclusions
Significant penile length loss and ED create tremendous negative impact on patients’ emotional and psychological well-being. Several PLP can be performed concurrently with PP insertion in patients with severe ED and penile shortening to help combat negative emotional and psychological concerns from penile length loss with penile prosthetic device placement. Many pre-operative, intra-operative, and post-operative techniques can be performed by surgeons who have extensive penile reconstruction experience and have been trained to do these procedures, as there is significant risk to the patient and limitations to what can be expected. Proper patient selection, extensive patient and partner counseling, and setting realistic penile length and girth expectations are essential to prevent patient dissatisfaction post-operatively. Penile length enhancement can only be achieved by the longitudinal increase of the corpora cavernosa during PP implantation. In the hands of experienced, high-volume implanters, these approaches can provide meaningful length recovery for patients undergoing PP insertion. However, it should be understood that the expected length gain cannot be predicted preoperatively. The average reported length recovery is limited to around 3 cm, but can be less than 1.0 cm. Future research is needed to identify the appropriate technique for each approach, ideal candidates, and the length gain that can be safely expected.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: None.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring the questions related to the accuracy or integrity of a part of the work are appropriately investigated and resolved. All clinical procedures described in this study were conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethical approval was not required as no human subjects or animals were involved in this literature review. All images in publication are completely unidentified and there are no details on persons mentioned within the text.
Footnotes
Provenance and Peer Review: This article was commissioned by the Guest Editors (Martin Gross, Jay Simhan, and David Barham) for the series “Complex Penile Prosthesis Surgery” published in Translational Andrology and Urology. The article has undergone external peer review.
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://tau.amegroups.com/article/view/10.21037/tau-23-354/rc
Peer Review File: Available at https://tau.amegroups.com/article/view/10.21037/tau-23-354/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-23-354/coif). The series “Complex Penile Prosthesis Surgery” was commissioned by the editorial office without any funding or sponsorship. L.A.L. is on the Speakers Bureau for Boston Scientific, Advisory Board for Absorption Pharmaceutical, International Medical Devices, and Hybrid Medical, and a Company stockholder in Absorption Pharmaceutical. The authors have no other conflicts of interest to declare.
References
- 1.Khalil MI, Machado B, Miranda A, et al. Penile shortening complaints in males with erectile dysfunction: a narrative review on penile lengthening procedures during penile prosthesis surgery. Transl Androl Urol 2021;10:2658-68. 10.21037/tau-21-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shah BB, Kent M, Valenzuela R. Advanced Penile Length Restoration Techniques to Optimize Penile Prosthesis Placement Outcomes. Sex Med Rev 2021;9:641-9. 10.1016/j.sxmr.2020.05.007 [DOI] [PubMed] [Google Scholar]
- 3.Lee KC, Brock GB. Strategies for maintaining penile size following penile implant. Transl Androl Urol 2013;2:67-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akin-Olugbade O, Parker M, Guhring P, et al. Determinants of patient satisfaction following penile prosthesis surgery. J Sex Med 2006;3:743-8. 10.1111/j.1743-6109.2006.00278.x [DOI] [PubMed] [Google Scholar]
- 5.Deveci S, Martin D, Parker M, et al. Penile length alterations following penile prosthesis surgery. Eur Urol 2007;51:1128-31. 10.1016/j.eururo.2006.10.026 [DOI] [PubMed] [Google Scholar]
- 6.Anaissie J, Yafi FA. A review of surgical strategies for penile prosthesis implantation in patients with Peyronie’s disease. Transl Androl Urol 2016;5:342-50. 10.21037/tau.2016.04.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dillon BE, Chama NB, Honig SC. Penile size and penile enlargement surgery: a review. Int J Impot Res 2008;20:519-29. 10.1038/ijir.2008.14 [DOI] [PubMed] [Google Scholar]
- 8.Haliloglu A, Baltaci S, Yaman O. Penile length changes in men treated with androgen suppression plus radiation therapy for local or locally advanced prostate cancer. J Urol 2007;177:128-30. 10.1016/j.juro.2006.08.113 [DOI] [PubMed] [Google Scholar]
- 9.Vasconcelos JS, Figueiredo RT, Nascimento FL, et al. The natural history of penile length after radical prostatectomy: a long-term prospective study. Urology 2012;80:1293-6. 10.1016/j.urology.2012.07.060 [DOI] [PubMed] [Google Scholar]
- 10.Vardi Y, Har-Shai Y, Gil T, et al. A critical analysis of penile enhancement procedures for patients with normal penile size: surgical techniques, success, and complications. Eur Urol 2008;54:1042-50. 10.1016/j.eururo.2008.07.080 [DOI] [PubMed] [Google Scholar]
- 11.Wilson SK, Wen L, Egydio PH. Evolution of techniques for aesthetic penile enlargement during prosthesis placement: a chronicle of the Egydio non-grafting strategy. Int J Impot Res 2023;35:1-8. 10.1038/s41443-020-00379-3 [DOI] [PubMed] [Google Scholar]
- 12.Nehra A, Alterowitz R, Culkin DJ, et al. Peyronie’s Disease: AUA Guideline. J Urol 2015;194:745-53. 10.1016/j.juro.2015.05.098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alei G, Letizia P, Ricottilli F, et al. Original technique for penile girth augmentation through porcine dermal acellular grafts: results in a 69-patient series. J Sex Med 2012;9:1945-53. 10.1111/j.1743-6109.2012.02744.x [DOI] [PubMed] [Google Scholar]
- 14.Mulhall J, Anderson M, Parker M. A surgical algorithm for men with combined Peyronie’s disease and erectile dysfunction: functional and satisfaction outcomes. J Sex Med 2005;2:132-8. 10.1111/j.1743-6109.2005.20113.x [DOI] [PubMed] [Google Scholar]
- 15.Ralph DJ. Long-term results of the surgical treatment of Peyronie’s disease with plaque incision and grafting. Asian J Androl 2011;13:797. 10.1038/aja.2011.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ziegelmann MJ, Bajic P, Levine LA. Peyronie’s disease: Contemporary evaluation and management. Int J Urol 2020;27:504-16. 10.1111/iju.14230 [DOI] [PubMed] [Google Scholar]
- 17.Papagiannopoulos D, Yura E, Levine L. Examining Postoperative Outcomes after Employing a Surgical Algorithm for Management of Peyronie’s Disease: A Single-Institution Retrospective Review. J Sex Med 2015;12:1474-80. 10.1111/jsm.12910 [DOI] [PubMed] [Google Scholar]
- 18.Leungwattanakij S, Bivalacqua TJ, Reddy S, et al. Long-term follow-up on use of pericardial graft in the surgical management of Peyronie’s disease. Int J Impot Res 2001;13:183-6. 10.1038/sj.ijir.3900676 [DOI] [PubMed] [Google Scholar]
- 19.Allen MS, Walter EE. Erectile Dysfunction: An Umbrella Review of Meta-Analyses of Risk-Factors, Treatment, and Prevalence Outcomes. J Sex Med 2019;16:531-41. 10.1016/j.jsxm.2019.01.314 [DOI] [PubMed] [Google Scholar]
- 20.Levine LA, Lenting EL. A surgical algorithm for the treatment of Peyronie’s disease. J Urol 1997;158:2149-52. 10.1016/S0022-5347(01)68184-9 [DOI] [PubMed] [Google Scholar]
- 21.978-94-92671-16-5., E.G.E.p.a.t.E.A.C.A.I., EAU Guidelines. 2022, EAU Annual Congress Amsterdam. Available online: https://uroweb.org/guidelines/sexual-and-reproductive-health/chapter/penile-curvature
- 22.Romero-Otero J, Manfredi C, Ralph D, et al. Non-invasive and surgical penile enhancement interventions for aesthetic or therapeutic purposes: a systematic review. BJU Int 2021;127:269-91. 10.1111/bju.15145 [DOI] [PubMed] [Google Scholar]
- 23.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moncada I, Martínez-Salamanca JI, Jara J, et al. Inflatable penile prosthesis implantation without corporeal dilation: a cavernous tissue sparing technique. J Urol 2010;183:1123-6. 10.1016/j.juro.2009.11.048 [DOI] [PubMed] [Google Scholar]
- 25.Zaazaa A, Mostafa T. Spontaneous Penile Tumescence by Sparing Cavernous Tissue in the Course of Malleable Penile Prosthesis Implantation. J Sex Med 2019;16:474-8. 10.1016/j.jsxm.2019.01.012 [DOI] [PubMed] [Google Scholar]
- 26.Tran H, Goldfarb R, Ackerman A, et al. Penile Lengthening, Girth, and Size Preservation at the Time of Penile Prosthesis Insertion. Sex Med Rev 2017;5:403-12. 10.1016/j.sxmr.2016.11.005 [DOI] [PubMed] [Google Scholar]
- 27.Weinberg AC, Pagano MJ, Deibert CM, et al. Sub-Coronal Inflatable Penile Prosthesis Placement With Modified No-Touch Technique: A Step-by-Step Approach With Outcomes. J Sex Med 2016;13:270-6. 10.1016/j.jsxm.2015.12.016 [DOI] [PubMed] [Google Scholar]
- 28.Sansalone S, Garaffa G, Djinovic R, et al. Simultaneous penile lengthening and penile prosthesis implantation in patients with Peyronie’s disease, refractory erectile dysfunction, and severe penile shortening. J Sex Med 2012;9:316-21. 10.1111/j.1743-6109.2011.02509.x [DOI] [PubMed] [Google Scholar]
- 29.Rolle L, Ceruti C, Timpano M, et al. A new, innovative, lengthening surgical procedure for Peyronie’s disease by penile prosthesis implantation with double dorsal-ventral patch graft: the “sliding technique”. J Sex Med 2012;9:2389-95. 10.1111/j.1743-6109.2012.02675.x [DOI] [PubMed] [Google Scholar]
- 30.Rolle L, Falcone M, Ceruti C, et al. A prospective multicentric international study on the surgical outcomes and patients’ satisfaction rates of the ‘sliding’ technique for end-stage Peyronie’s disease with severe shortening of the penis and erectile dysfunction. BJU Int 2016;117:814-20. 10.1111/bju.13371 [DOI] [PubMed] [Google Scholar]
- 31.Egydio PH, Kuehhas FE, Valenzuela RJ. Modified Sliding Technique (MoST) for Penile Lengthening with Insertion of Inflatable Penile Prosthesis. J Sex Med 2015;12:1100-4. 10.1111/jsm.12911 [DOI] [PubMed] [Google Scholar]
- 32.Egydio PH, Kuehhas FE. Penile lengthening and widening without grafting according to a modified ‘sliding’ technique. BJU Int 2015;116:965-72. 10.1111/bju.13065 [DOI] [PubMed] [Google Scholar]
- 33.Wilson SK, Mora-Estaves C, Egydio P, et al. Glans Necrosis Following Penile Prosthesis Implantation: Prevention and Treatment Suggestions. Urology 2017;107:144-8. 10.1016/j.urology.2017.06.020 [DOI] [PubMed] [Google Scholar]
- 34.Egydio PH, Kuehhas FE. The Multiple-Slit Technique (MUST) for Penile Length and Girth Restoration. J Sex Med 2018;15:261-9. 10.1016/j.jsxm.2017.11.223 [DOI] [PubMed] [Google Scholar]
- 35.Gaffney CD, Pagano MJ, Weinberg AC, et al. Lengthening strategies for Peyronie’s disease. Transl Androl Urol 2016;5:351-62. 10.21037/tau.2016.04.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Clavell-Hernández J, Wang R. Penile Size Restoration With Nondegloving Approach for Peyronie’s Disease: Initial Experience. J Sex Med 2018;15:1506-13. 10.1016/j.jsxm.2018.07.003 [DOI] [PubMed] [Google Scholar]
- 37.Garaffa G, CM, Chiriaco G, et al. Peyronie’s Disease: Tunical String-vest Incisions for Girth and Length Restoration after Penile Prosthesis Implantation 2018.
- 38.Egydio PH. An Innovative Strategy for Non-Grafting Penile Enlargement: A Novel Paradigm for Tunica Expansion Procedures. J Sex Med 2020;17:2093-103. 10.1016/j.jsxm.2020.05.010 [DOI] [PubMed] [Google Scholar]
- 39.Razdan S, Zisman A, Valenzuela R. Scrotal approach for tunica expansion procedure (TEP) for penile girth and length restoration during penile prosthesis implantation in patients with penile angulation due to Peyronie’s disease and erectile dysfunction: technique and outcomes. Int J Impot Res 2024;36:146-50. 10.1038/s41443-022-00652-7 [DOI] [PubMed] [Google Scholar]
- 40.Henderson J, Arya R, Gillespie P. Skin graft meshing, over-meshing and cross-meshing. Int J Surg 2012;10:547-50. 10.1016/j.ijsu.2012.08.013 [DOI] [PubMed] [Google Scholar]
- 41.Miranda A. Auxetic Expansion of the Tunica Albuginea for Penile Length and Girth Restoration Without a Graft: A Translational Study. Sex Med 2021;9:100456. 10.1016/j.esxm.2021.100456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Miranda A. Auxetic Technique Application in Cases of Corpora Cavernosa Fibrosis. Video Journal of Prosthetic Urology and Sexual Medicine Surgery 2022. Available online: https://www.vjsm.info/videos/all/auxetic-technique-application-in-cases-of-corpora-cavernosa-fibrosis
- 43.Miranda A. PD23-09 Auxetic expansion of the tunica albuginea for penile length and girth restoration without a graft: a case series. J Urol 2022;207:e412. 10.1097/JU.0000000000002565.09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mehr J, Santarelli S, Green TP, et al. Emerging Roles of Penile Traction Therapy and Vacuum Erectile Devices. Sex Med Rev 2022;10:421-33. 10.1016/j.sxmr.2021.12.003 [DOI] [PubMed] [Google Scholar]
- 45.Abern MR, Larsen S, Levine LA. Combination of penile traction, intralesional verapamil, and oral therapies for Peyronie’s disease. J Sex Med 2012;9:288-95. 10.1111/j.1743-6109.2011.02519.x [DOI] [PubMed] [Google Scholar]
- 46.Yafi FA, Pinsky MR, Stewart C, et al. The Effect of Duration of Penile Traction Therapy in Patients Undergoing Intralesional Injection Therapy for Peyronie’s Disease. J Urol 2015;194:754-8. 10.1016/j.juro.2015.03.092 [DOI] [PubMed] [Google Scholar]
- 47.Ziegelmann MJ, Viers BR, Montgomery BD, et al. Clinical Experience With Penile Traction Therapy Among Men Undergoing Collagenase Clostridium histolyticum for Peyronie Disease. Urology 2017;104:102-9. 10.1016/j.urology.2017.01.054 [DOI] [PubMed] [Google Scholar]
- 48.Ziegelmann M, Savage J, Toussi A, et al. Outcomes of a Novel Penile Traction Device in Men with Peyronie’s Disease: A Randomized, Single-Blind, Controlled Trial. J Urol 2019;202:599-610. 10.1097/JU.0000000000000245 [DOI] [PubMed] [Google Scholar]
- 49.Joseph J, Ziegelmann MJ, Alom M, et al. Outcomes of RestoreX Penile Traction Therapy in Men With Peyronie’s Disease: Results From Open Label and Follow-up Phases. J Sex Med 2020;17:2462-71. 10.1016/j.jsxm.2020.10.003 [DOI] [PubMed] [Google Scholar]
- 50.Alom M, Sharma KL, Toussi A, et al. Efficacy of Combined Collagenase Clostridium histolyticum and RestoreX Penile Traction Therapy in Men with Peyronie’s Disease. J Sex Med 2019;16:891-900. 10.1016/j.jsxm.2019.03.007 [DOI] [PubMed] [Google Scholar]
- 51.Levine LA, Newell M, Taylor FL. Penile traction therapy for treatment of Peyronie’s disease: a single-center pilot study. J Sex Med 2008;5:1468-73. 10.1111/j.1743-6109.2008.00814.x [DOI] [PubMed] [Google Scholar]
- 52.Levine LA, Rybak J. Traction therapy for men with shortened penis prior to penile prosthesis implantation: a pilot study. J Sex Med 2011;8:2112-7. 10.1111/j.1743-6109.2011.02285.x [DOI] [PubMed] [Google Scholar]
- 53.Rybak J, Papagiannopoulos D, Levine L. A retrospective comparative study of traction therapy vs. no traction following tunica albuginea plication or partial excision and grafting for Peyronie’s disease: measured lengths and patient perceptions. J Sex Med 2012;9:2396-403. 10.1111/j.1743-6109.2012.02849.x [DOI] [PubMed] [Google Scholar]
- 54.Sellers T, Dineen M, Salem EA, et al. Vacuum Preparation, Optimization of Cylinder Length and Postoperative Daily Inflation Reduces Complaints of Shortened Penile Length Following Implantation of Inflatable Penile Prosthesis. Advances in Sexual Medicine 2013;3:5. 10.4236/asm.2013.31003 [DOI] [Google Scholar]
- 55.Tsambarlis PN, Chaus F, Levine LA. Successful Placement of Penile Prostheses in Men With Severe Corporal Fibrosis Following Vacuum Therapy Protocol. J Sex Med 2017;14:44-6. 10.1016/j.jsxm.2016.11.304 [DOI] [PubMed] [Google Scholar]
- 56.Canguven O, Talib RA, Campbell J, et al. Is the daily use of vacuum erection device for a month before penile prosthesis implantation beneficial? A randomized controlled trial. Andrology 2017;5:103-6. 10.1111/andr.12258 [DOI] [PubMed] [Google Scholar]
- 57.Henry GD, Carrion R, Jennermann C, et al. Prospective evaluation of postoperative penile rehabilitation: penile length/girth maintenance 1 year following Coloplast Titan inflatable penile prosthesis. J Sex Med 2015;12:1298-304. 10.1111/jsm.12833 [DOI] [PubMed] [Google Scholar]
- 58.Veale D, Miles S, Read J, et al. Penile Dysmorphic Disorder: Development of a Screening Scale. Arch Sex Behav 2015;44:2311-21. 10.1007/s10508-015-0484-6 [DOI] [PubMed] [Google Scholar]
- 59.Wilson SK, Wen L, Rossello M, et al. Initial safety outcomes for the Rigicon Infla10® inflatable penile prosthesis. BJU Int 2023;131:729-33. 10.1111/bju.15960 [DOI] [PubMed] [Google Scholar]
- 60.Negro CL, Paradiso M, Rocca A, et al. Implantation of AMS 700 LGX penile prosthesis preserves penile length without the need for penile lengthening procedures. Asian J Androl 2016;18:114-7. 10.4103/1008-682X.154311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wallen JJ, Madiraju SK, Wang R, et al. Implementation of length expanding inflatable penile prosthesis is not sufficient to prevent postsurgical penile shortening. Asian J Androl 2018. [Epub ahead of print]. doi: . 10.4103/aja.aja_77_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wilson SK, Haxhimolla H, Kua B, et al. Survival From Revision Surgery for New Rigicon Infla10 Three-piece Inflatable Penile Prosthesis Is Comparable to Preceding Devices. Urology 2023;180:257-61. 10.1016/j.urology.2023.06.031 [DOI] [PubMed] [Google Scholar]
- 63.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as