Abstract
Introduction
Heterotopic ossification (HO) develops when bone formation appears in soft tissues, usually after an injury or major surgery. Timely and accurately diagnosing of this rare event is essential due to the possibility of misdiagnosis as a maintained foreign body, infection, incisional neoplastic recurrence, and metastatic or primary neoplasms.
Case presentation
In this study, we present a 57-year-old man who was operated for peritonitis due to perforated appendicitis, and an asymptomatic HO was accidentally found on an incisional line of previous open prostatectomy about 5 years earlier due to benign prostatic hyperplasia. A bone density lesion was seen in the fascia and on the incisional scar of previous surgery.
Discussion
HO rarely occurs within an abdominal incision due to surgery. It is reported only within vertical midline incisions and mainly within the first year after the operation. Imaging confirms the diagnosis of HO in previous abdominal surgery scars, which reveals dense vertical calcification along the previous incisional scar. In the case of HO, the exclusive effective management is the entire surgical excision with primary closure, and NSAIDs are the preventive choices.
Conclusion
HO should be considered in patients presenting with discomfort or palpable mass or even asymptomatic patients with previous abdominal surgeries besides considering relative history such as surgical complications or neoplasms.
Keywords: Heterotopic ossification, Abdominal incision, Appendectomy, Bone reaction, Surgical scar, Case report
Highlights
-
•
Heterotopic ossification (HO) may be accidentally found on the incisional scar of previous abdominal surgery in asymptomatic patients.
-
•
Computed Tomography (CT) scan is useful in distinguishing HO from other similar surgical complications such as infection and maintained foreign body, intra-incisional mass, and metastatic or primary neoplasms with considering the patient’s history, and is useful in deciding on surgical management.
-
•
The main HO management is the entire surgical excision with primary closure.
-
•
For prevention of HO post abdominal midline incision surgeries or recurrence after primary excisional management of previous HO, non-steroidal anti-inflammatories or external radiotherapy, can be considered.
1. Introduction
Heterotopic ossification (HO) is a benign and uncommon occurrence that develops when trabecular bone tissue appears outside the usual skeletal system, including skin, subcutaneous, joints, muscles, and mesentery tissues [[1], [2], [3], [4]]. Risk factors contributed to this formation are burns, trauma, arthroplasty, and abdominal surgery [5]. HO consists of the formation of osseous, cartilaginous, and rarely myelogenous components along an abdominal scar and may be misdiagnosed as a maintained foreign body, infection, incisional neoplastic recurrence, and metastatic or primary neoplasms [6]. HO may cause severe and lifelong disabilities, depending on the involved structures [7]. In this study, we present a 57-year-old man who was operated on for peritonitis due to perforated appendicitis, and the asymptomatic bony lesion was accidentally found on the incisional line of a previous open prostatectomy and also been conducted through the SCARE checklist [8].
2. Case presentation/examination
2.1. General data
A 57-year-old Iranian man who has complained of abdominal pain, nausea and vomiting, and loss of appetite since two days ago was referred to our academic hospital. He had a history of open prostatectomy due to benign prostatic hyperplasia (BPH) about 5 years earlier. The patient had no smoking history, and familial or personal medical history was not significant.
2.2. Physical examination
The vital signs were stable. On abdominal physical examination, there was rebound tenderness in the right lower quadrant (RLQ) with rigidity and guarding. Bowel sounds were normal.
2.3. Laboratory assessment
In clinical tests, he had leukocytosis (WBC = 15,000), CRP = 3+, and ESR = 25. Further tests showed no abnormalities.
2.4. Medical imaging
Due to suspicion of peritonitis caused by perforated appendicitis, an abdominal Computed Tomography (CT) scan was requested in which peritonitis and perforated appendicitis were confirmed. The patient was prepared for appendectomy.
2.5. Treatment and follow-up
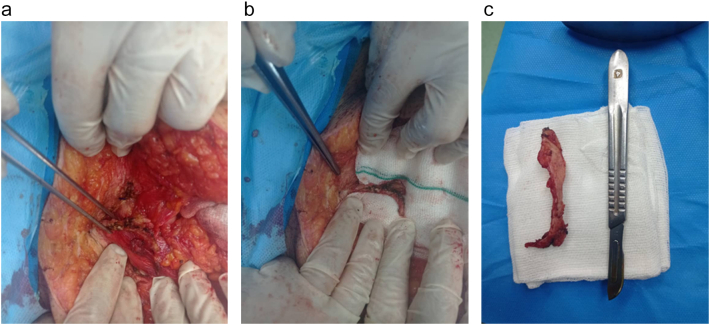
At the operation, the patient's abdomen was opened with a midline incision. A bone density lesion was found in the fascia along the incisional scar of a previous open prostatectomy. A bone reaction occurred, and new bone was formed, which has the same density as other bone structures. In our case, the lesion was excised (Fig. 1), and appendectomy was performed, and preventive ibuprofen was recommended. The histopathology evaluation of the resected specimen revealed normal osseous tissue and also confirmed HO. The patient was examined about a year after the surgical excision of the previous HO, and no signs of recurrence were found.
Fig. 1.
Macroscopic specimens removed from patient intraoperatively.
3. Discussion
HO is the abnormal deposition of mature, lamellar osseous tissue in soft tissues such as skin, subcutaneous fat, mesenteric tissue, and scars [9,10]. This dystrophic soft tissue calcification rarely occurs within an abdominal incision due to surgery, which has been reported only within vertical midline incisions and mainly within the first year after operation [11,12]. Kim et al. conducted a study that revealed an incidence of about 25 % for HO after abdominal incisions [13]. HOs are more likely to develop in males (89 %) [14]. In our 57-year-old male patient, HO was found 5 years after the BPH surgical procedure. In the current case, a bone density lesion was observed in the fascia along the incisional scar of a previous open prostatectomy, which was accidentally found during a midline incision for peritonitis caused by perforated appendicitis.
Three main theories have been proposed for the occurrence of this ossification [11,12,15,16]. The first is that tiny pieces of periosteum or perichondrium of the pubis symphysis or xiphoid process are inculcated into surgical incisions during surgery, leading to ossification. So, this theory explains the fact that all reported HOs are from vertical scars, whereas it doesn't sufficiently support HOs without closeness with bone tissue or infrequent formation in orthopedic operation wounds, which are associated with more osseous particles. In our patient, this theory seems to be the leading cause due to a lower midline incision in the previous surgery. The other theory explains that HO is formed due to the differentiation of immature pluripotent mesenchymal cells to osteoblasts or chondroblasts caused by local damage. This one is unable to justify the exclusive formation in vertical incisions. In the third one, extra tension on the suture scar may cause implantation of periosteal components in muscular tissue from torn regions of bone and muscular insertion. Although the formation mechanism is incompletely understood, both local and systemic agents are considered to stimulate pro-inflammatory conditions that lead to HO development. The literature also demonstrated no correlation between surgical incision site complications such as hyperplastic, keloid, or infection and the HO.
Computed Tomography (CT) scan of HO in abdominal midline incisions demonstrated ossified components with tubular bone density as well as fatty components representative of marrow in scar site between bilateral rectus abdominis muscles that are used in distinguishing HO from other similar surgical complications including infection and maintained foreign body, intra-incisional mass, and metastatic or primary neoplasms with considering the patient's history, and may help in deciding for surgical resection (Fig. 2) [11].
Fig. 2.
Computerized Tomography (CT) scan reveals ossified tissue at the site of the midline incision scar.
The HO management in abdominal scars is restricted to symptomatic patients presenting with discomfort. The main sufficient surgical management is complete excision with primary closure. For prevention of HO post-midline abdominal incision surgeries or recurrence after excisional management, a non-steroidal anti-inflammatory scan be considered [17]. Herein, we present a 57-year-old male patient with suspected signs of peritonitis 5 years after open prostatectomy due to benign prostatic hyperplasia (BPH). A bone density lesion was found in the fascia and on the incisional scar of a previous open prostatectomy. A bone reaction occurred, and new bone was formed, which has the same density as other bone structures. The ossified lesion was excised.
4. Conclusion
HO should be considered in patients presenting with discomfort or palpable mass or even asymptomatic patients with previous abdominal surgeries besides considering relative history such as surgical complications or neoplasms. The diagnosis of HO in previous abdominal surgery scars is confirmed by imaging, which reveals dense vertical calcification along the previous incisional scar. In the case of HO, the exclusive effective management is complete excision with primary closure, and non-steroidal anti-inflammatories, are the preventive choices.
Consent for publication
The patient provided written informed consent for the publication of this case report and accompanying images. The editor-in-chief of this journal can review a copy of the written consent upon request.
Ethical approval
This research was approved by the research ethics committee of our institution.
Funding
Not applicable.
Guarantor
Corresponding author is Dr. Javad Zebarjadi Bagherpour and accept full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Research registration number
-
1.
Name of the registry: N/A
-
2.
Unique identifying number or registration ID: N/A
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): N/A.
CRediT authorship contribution statement
J.Z.B. and S.H.H. were actively involved in the patient follow-up and the acquisition, analysis and interpretation of data. J.Z.B. and H.S. designed and organized the study. H.S., F.F., S.Kh., and M.D. wrote the manuscript. All authors reviewed, edited and approved the final manuscript.
J.Z.B: Conceptualization, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – review & editing.
H.S: Data curation, Investigation, Project administration, Visualization, Writing – original draft, Writing – review & editing.
S.H.H.: Data curation, Investigation, Writing – review & editing.
F.F., S.Kh., and M.D.: Investigation, Writing – original draft, Writing – review & editing.
Declaration of Generative AI and AI-assisted technologies in the writing process
The authors declare that they don't have used AI in scientific writing.
Declaration of competing interest
The authors declare that they have no competing interests.
Acknowledgments
Not applicable.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on request, with the approval of the patients' legal guardians.
References
- 1.Hogan N.M., et al. Heterotopic ossification of the abdominal wall. Int. J. Surg. Case Rep. 2012;3(10):489–491. doi: 10.1016/j.ijscr.2012.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hallock J., Field L.D. Surgical management of shoulder heterotopic ossification. Arthrosc. Tech. 2019;8(9):e1057–e1062. doi: 10.1016/j.eats.2019.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Edwards D.S., et al. Heterotopic ossification: a review of current understanding, treatment, and future. J. Orthop. Trauma. 2016;30 doi: 10.1097/BOT.0000000000000666. [DOI] [PubMed] [Google Scholar]
- 4.Hakim M., McCarthy E.F. Heterotopic mesenteric ossification. Am. J. Roentgenol. 2001;176(1):260–261. doi: 10.2214/ajr.176.1.1760260. [DOI] [PubMed] [Google Scholar]
- 5.Brady R.D., et al. Neurological heterotopic ossification: current understanding and future directions. Bone. 2018;109:35–42. doi: 10.1016/j.bone.2017.05.015. [DOI] [PubMed] [Google Scholar]
- 6.Yoo Y.S., N.K., Hwang I.K., Kim H.C. Heterotopic ossification in abdominal incision: a case report. J Korean Radiol Soc. Aug 2001;45(2):191–193. [Google Scholar]
- 7.Koolen P.G., Schreinemacher M.H., Peppelenbosch A.G. Heterotopic ossifications in midline abdominal scars: a critical review of the literature. Eur. J. Vasc. Endovasc. Surg. 2010;40(2):155–159. doi: 10.1016/j.ejvs.2010.03.010. [DOI] [PubMed] [Google Scholar]
- 8.Sohrabi C., M.G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg Lond Engl. 2023;109(5):1136. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McCarthy E.F., Sundaram M. Heterotopic ossification: a review. Skeletal Radiol. 2005;34(10):609–619. doi: 10.1007/s00256-005-0958-z. [DOI] [PubMed] [Google Scholar]
- 10.Myers M.A., Minton J.P. Heterotopic ossification within the small-bowel mesentery. Arch. Surg. 1989;124(8):982–983. doi: 10.1001/archsurg.1989.01410080118020. [DOI] [PubMed] [Google Scholar]
- 11.Jacobs J.E., Birnbaum B.A., Siegelman E.S. Heterotopic ossification of midline abdominal incisions: CT and MR imaging findings. AJR Am. J. Roentgenol. 1996;166(3):579–584. doi: 10.2214/ajr.166.3.8623631. [DOI] [PubMed] [Google Scholar]
- 12.Reardon M.J., et al. Heterotopic calcification in abdominal wounds. Am. J. Surg. 1997;173(2):145–147. doi: 10.1016/S0002-9610(96)00415-1. [DOI] [PubMed] [Google Scholar]
- 13.Kim J., et al. Heterotopic ossification developing in surgical incisions of the abdomen: analysis of its incidence and possible factors associated with its development. J. Comput. Assist. Tomogr. 2008;32(6):872–876. doi: 10.1097/RCT.0b013e318159c617. [DOI] [PubMed] [Google Scholar]
- 14.Goff A.K., Reichard R. A soft-tissue calcification: differential diagnosis and pathogenesis. J. Forensic Sci. 2006;51(3):493–497. doi: 10.1111/j.1556-4029.2006.00109.x. [DOI] [PubMed] [Google Scholar]
- 15.Marteinsson B.T., Musgrove J.E. Heterotopic bone formation in abdominal incisions. Am. J. Surg. 1975;130(1):23–25. doi: 10.1016/0002-9610(75)90449-3. [DOI] [PubMed] [Google Scholar]
- 16.Apostolidis N.S., et al. Heterotopic bone formation in abdominal operation scars. Report of six cases with review of the literature. Am. J. Surg. 1981;142(5):555–559. doi: 10.1016/0002-9610(81)90424-4. [DOI] [PubMed] [Google Scholar]
- 17.McLaren A.C. Prophylaxis with indomethacin for heterotopic bone. After open reduction of fractures of the acetabulum. J. Bone Joint Surg. Am. 1990;72(2):245–247. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on request, with the approval of the patients' legal guardians.