Abstract
Background
Airway management is a core component of the treatment of cardiac arrest. Where a rescuer cannot establish a patent airway to provide oxygenation and ventilation using standard basic and advanced airway techniques, there may be a need to consider emergency front-of-neck airway access (eFONA, e.g., cricothyroidotomy), but there is limited evidence to inform this approach.
Objectives
This scoping review aims to identify the evidence for the use of eFONA techniques in patients with cardiac arrest.
Methods
In November 2023, we searched Medline, Embase, and Cochrane Central to identify studies on eFONA in adults. We included randomised controlled trials, non-randomised studies, and case series with at least five cases that described any use of eFONA. We extracted data, including study setting, population characteristics, intervention characteristics, and outcomes. Our analysis focused on four key areas: incidence of eFONA, eFONA success rates, clinical outcomes, and complications.
Results
The search identified 21,565 papers, of which 18,934 remained after de-duplication. After screening, we included 69 studies (53 reported incidence, 40 reported success rate, 38 reported clinical outcomes; 36 studies reported complications). We identified only one randomised controlled trial. Across studies, there was a total of 4,457 eFONA attempts, with a median of 31 attempts (interquartile range 16–56.5) per study. There was marked heterogeneity across studies that precluded any pooling of data. There were no studies that included only patients in cardiac arrest.
Conclusion
The available evidence for eFONA is extremely heterogeneous, with no studies specifically focusing on its use in adults with cardiac arrest.
Keywords: Heart arrest, Out-of-hospital cardiac arrest, Emergency front-of-neck access, Endotracheal intubation, Cricothyroidotomy
Introduction
Airway management is a core component of cardiac arrest management.1 During cardiac arrest, airway management by healthcare providers typically begins with bag-mask ventilation, followed by a stepwise escalation to more definitive strategies such as supraglottic airway insertion or tracheal intubation.2 Traditionally, tracheal intubation has been considered the gold standard for airway management in cardiac arrest, but out-of-hospital cardiac arrest randomised controlled trials of tracheal intubation during cardiopulmonary resuscitation during out-of-hospital cardiac arrest have shown that it is not superior to bag mask ventilation or supraglottic airway use.3, 4 There are ongoing studies on the role of tracheal intubation during CPR in-hospital cardiac arrest setting.5, 6
In some patients, standard basic and advanced airway techniques may not be effective leading to a cannot oxygenate scenario. The rescue strategy is the use of emergency front-of-neck access (eFONA) techniques, such as surgical cricothyroidotomy and needle cricothyroidotomy.7 A recent systematic review showed that pre-hospital use of eFONA had a very high success rate.8.
To date, the International Liaison Committee on Resuscitation (ILCOR) has not incorporated eFONA in its treatment recommendations for airway management in adult cardiac arrest. On this basis, the ILCOR Advanced Life Support (ALS) Task Force prioritised the need for a scoping review to explore the role of eFONA in adult cardiac arrest.
Methods
The overarching objective of this scoping review was to explore the optimum airway management in cardiac arrest where initial strategies to achieve adequate ventilation and oxygenation have been unsuccessful, based on the following PICO (Population, Intervention, Comparator, Outcome) question:
In adult patients in cardiac arrest in any setting where adequate ventilation cannot be rapidly achieved using basic/advanced airway management strategies, does using a front-of-neck airway access attempt compared with ongoing attempts at basic/advanced airway management strategies change any clinical outcome?
We anticipated limited evidence in this specific area, so planned a scoping review that explored eFONA use in critically ill patients in the in-hospital and out-of-hospital settings, focussing on four key areas:
-
(1)
Incidence of eFONA.
-
(2)
Success rates of eFONA attempts.
-
(3)
Clinical outcomes in patients with an eFONA attempt.
-
(4)
Complications associated with eFONA attempts.
This scoping review was undertaken in line with ILCOR’s methodology for scoping reviews. This review paper is written in line with PRISMA checklist extension for scoping reviews.9 The ILCOR protocol template is available in the supplementary materials.
Eligibility criteria
We included randomised controlled trials, non-randomised studies (e.g., interrupted time series, controlled before-and-after studies, and cohort studies), and case series with at least five patients that described any use of eFONA in the pre-hospital or in-hospital setting. We excluded paediatric studies where all patients aged < 18 years old, simulation studies, studies that describe non-emergency surgical airways, animal studies, case series/reports with fewer than five patients, editorials, protocols, review papers, and letters. Grey literature was eligible for inclusion. In studies that included adults and children, we extracted only adult data where possible.
Information sources and search
We originally searched MEDLINE, Embase, and the Cochrane Library in June 2022, with search updates completed in January 2023 and November 2023. Search strategies were developed iteratively in collaboration with an information specialist (SJ). The searches combined keywords and index terms to describe the population, setting, and intervention of interest. The final search strategy is included in the supplementary materials. We did not limit the search by year of publication or language. We identified additional relevant studies, including grey literature, through liaison with subject experts and ILCOR Advanced Life Support Task Force members. We did not undertake specific searches for grey literature.
Selection of sources of evidence
Following the completion of searches, the list of citations was deduplicated using Endnote X9 and X9.3.3, and Rayyan software (https://www.rayyan.ai/). Following deduplication, two reviewers (MA/AA) independently screened the titles and abstracts of the papers to exclude clearly irrelevant citations. The same two reviewers then independently reviewed the full text of potentially relevant studies. At each stage, reviewer conflicts were resolved through discussion or referral to a third reviewer.
Data charting, items and critical appraisal
After developing and piloting a bespoke online form for data extraction, two reviewers (MA/AA) independently extracted data items, including study setting, population characteristics, intervention characteristics, and outcomes. An overview of extracted data items is included in the supplementary materials. Conflicts between reviewers were resolved through discussion or referral to a third reviewer. We did not undertake a critical appraisal of the evidence, as the primary focus of this scoping review was to describe the volume, type, and key findings of the available evidence.
Synthesis of results
In line with the focus of this scoping review, we describe the findings in a narrative style for each of our four areas of focus. We present the results broken down for each key study setting (pre-hospital, in-hospital, pre-hospital/in-hospital, and battlefield) and summarise the findings of studies that focus specifically on cardiac arrest. Quantitative analysis consisted of descriptive analyses, including the frequencies and ranges of the outcomes for the included studies. The qualitative analysis comprised descriptions of the overall results and outcomes. For both methods, Microsoft Excel supported data analysis. Where appropriate, we calculated a 95% confidence interval for relevant outcomes in each study.
Results
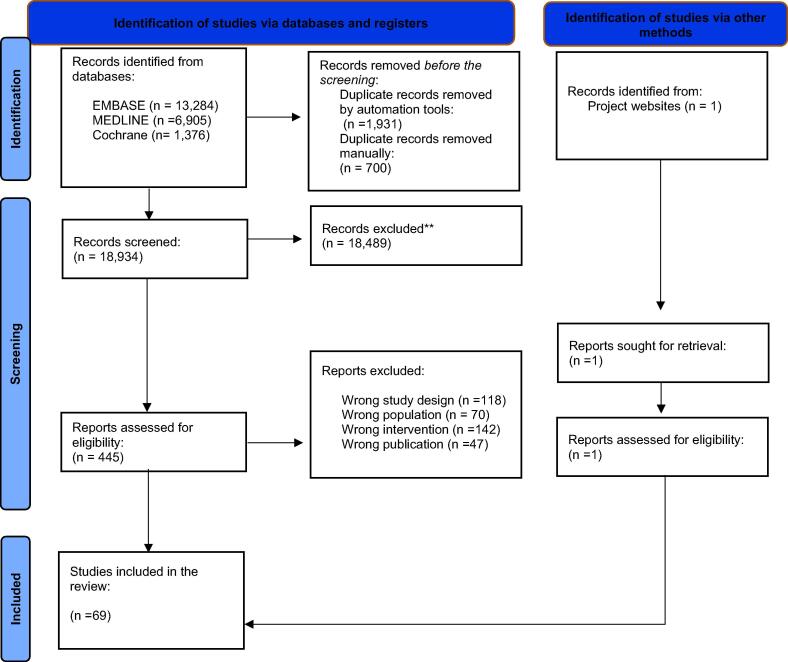
In total, our initial and updated searches identified 21,565 papers. Following the removal of duplicates, we screened 18,934 in the title/abstract stage, and then 445 full-text papers were retrieved for review (Fig. 1). In total, we included 69 studies.10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78 Of the 69 included studies, there was one randomised controlled trial and 68 observational studies. 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78 The randomised controlled trial compared emergency cricothyrotomy and emergency percutaneous dilatational tracheotomy.50 Of the observational studies, 59 were retrospective, 7 were prospective, and 2 were case series. Forty-eight percent of the studies were conducted in the USA, and the rest were conducted in the UK, the Netherlands, Afghanistan, Iraq, Israel, Syria, Singapore, Germany, Denmark, Egypt, Korea, Japan, India, Australia and/or New Zealand.
Fig. 1.
Of the 69 studies, there were no studies that included only patients in cardiac arrest. In addition, 99% used surgical cricothyroidotomy as the eFONA technique, with or without using needle cricothyroidotomy or emergency tracheostomy in some cases. The included studies described a total of 4,457 eFONA attempts, with a median of 31 attempts (interquartile range 16–56.5) per study. Across studies, there was a range of reported rescuers, including emergency medicine physicians, anaesthetists, surgeons, paramedics, and nurses. Study duration ranged from several months to 20 years. Table 1 summarises the included studies.
Table 1.
Characteristic of included studies.
| Study (Date) | Design | Setting (Length) | Population | Intervention (Providers)† | Patients (Sex, Age)† | Reported Outcomes |
|---|---|---|---|---|---|---|
| Pre-hospital studies | ||||||
| Spaite (1990) | RC | USA (1985–1987) |
Trauma, CA | Surgical cric (ALS paramedics) | 16 | Success; clinical outcomes; complications |
| Boyle (1993) | RC | USA (1983–1988) |
Trauma, CA | Surgical cric (air ambulance nurses) | 69 (Sex: 78% M; Age: Mean 22 y) |
Incidence; success rate; clinical outcomes complications |
| Xeropotamos (1993) | RC | UK (1991–1992) |
Trauma, CA | Surgical cric (HEMS staff, physicians, surgeons) | 11 (Age: Range 24–64 y) |
Incidence eFONA; success rate; ROSC; clinical outcomes |
| Jacobson (1996) | RC | USA (1990–1994) |
Trauma, CA | Surgical cric, needle cric (paramedics) | 50 (Sex: 76% M; Age: Mean 32 y) |
Incidence; success rate; ROSC; clinical outcomes; complications |
| Gerich (1998) | PC | Germany (1993–1997) |
Trauma, Medical | Surgical cric (HEMS) | 8 (Sex: 75% M; Age: Mean 40 y) |
Incidence; success rate; clinical outcomes; complications |
| Thomas (1999) | RC | USA (1995–1997) | Trauma, Medical | Surgical cric (HEMS) | 10 | Incidence; success rate |
| Robinson (2001) | RC | USA (1985–1997) | Trauma, Medical | Surgical cric (nurses, physicians) | 8 | Incidence; success rate |
| Bulger (2002) | RC | USA (1997–1999) | Trauma, Medical, CA | Surgical cric, needle cric (paramedics) | 30 (Sex: 70% M; Age: Range 18–99 y) |
Incidence; clinical outcomes |
| Germann (2009) | RC | USA (1998–2006) | Trauma, CA | Surgical cric (paramedics, registered nurses) | 6 (Sex: 100% M) |
Incidence; success rate |
| Warner (2009) | PC | USA (2001–2005) | Trauma, CA | Surgical cric (paramedic, critical-care, advanced paramedics) | 11 | Incidence; success rate; clinical outcomes; complications |
| Wang (2011) | RC | USA (2008–2008) | Trauma, CA | Surgical cric, needle cric (standard paramedic physicians, surgeons) | 88 (Sex: 75%M) |
Incidence; success rate; complications |
| Shapey (2012) | RC | UK (2003–2010) | Trauma, Medical, CA | Surgical cric, needle cric (paramedics, doctors, HEMS) | 16 | Incidence; ROSC; complications |
| Kamiutsuri (2013) | RC | Japan (2004–2011) | Trauma, CA | Surgical cric (physicians) | 13 | Incidence; success rate |
| Brown (2014) | RC | USA (2007–2009) | Trauma, Medical | Surgical cric, needle cric (HEMS, paramedics, nurses) | 35 | Incidence; success rate |
| Prekker (2014) | RC | USA (2006–2011) | NA | Surgical cric, needle cric (paramedics) | 30 | Incidence; ROSC; clinical outcomes |
| Diggs (2014) | RC | USA (2012–2012) | NA | Surgical cric, needle cric (paramedics) | 1,332 | Incidence; success rate |
| Peters (2015) | RC | Netherlands (2007–2012) | NA | Surgical cric (HEMS physicians, paramedics, nurses) | 19 | Incidence |
| Peters (2015) | RC | Netherlands (2007–2013) | Trauma, Medical, CA | Surgical cric (anaesthesiologists, HEMS physicians, surgeons) | 29 (Sex: 80% M) |
Incidence; ROSC; clinical outcomes |
| Sunde (2015) | PC | Multicentre (2012–2013) | Trauma, Medical, CA | Surgical cric (HEMS physicians, paramedics) | 6 | Incidence |
| Gellerfors (2018) | RC | Multicentre (2015–2016) | Trauma, CA | Surgical cric (physicians, nurses) | 14 | Incidence |
| Schober (2019) | RC | Netherlands (2011–2018) | Trauma, Medical | Surgical cric, needle cric (HEMS) | 18 | Incidence; success rate; clinical outcomes; complications |
| Aziz (2021) | RC | UK (2000–2019) | Trauma, CA | Surgical cric, needle cric (physicians, paramedics) | 72 | Incidence; success rate |
| Himmler (2023) | RC | USA (2008–2020) | Medical, Surgery | Surgical cric | 95 | Incidence |
| Malkan (2023) | RC | USA (2007–2020) | Trauma | Surgical cric | 251 (Sex: 98% M; Age: Median 25 y) | Incidence; clinical outcomes; complications |
| In-hospital setting | ||||||
| McGill (1982) | RC | USA (1977–1980) | Trauma, Medical, CA | Surgical cric (ER physicians, surgeons) | 38 (Age: Average 41 y) |
Incidence; clinical outcomes; |
| Erlandson (1989) | RC | USA (1981–1985) | Trauma, Medical, CA | Surgical cric (ER physicians, anaesthesiologists, surgeons) | 39 | Incidence; clinical outcomes; complications |
| Delaurier (1990) | RC | USA (1984–1988) | Trauma | Surgical cric (ER physicians) | 34 | Clinical outcomes; complications |
| Gillespie (1999) | RC | USA (1993–1998) | Trauma, Medical, CA | Surgical cric, needle cric, tracheostomy (ER physicians, surgeons) | 35 (Sex: 69% M; Age: Mean 50 y) |
Success rate; complications |
| Isaacs (2001) | RC | USA (1996) | Trauma, Medical | Surgical cric | 27 (Sex: 70% M; Age: Range 20–81 y) | Clinical outcomes; complications |
| Bair (2002) | RC | USA (1998–2001) | Trauma, Medical | Surgical cric, needle cric, tracheostomy (ER physicians surgeons) | 44 | Incidence |
| Wong (2008) | PC | Singapore (2000–2006) | Trauma, Medical, CA | Surgical cric, tracheostomy (ER physicians, anaesthesiologists, Surgeons) | 7 | Incidence; success rate |
| Cook (2011) | RC | UK (2008–2009) | Trauma, Medical, CA | Surgical cric, needle cric, tracheostomy (ER physicians, anaesthesiologists, surgeons) | 75 (Sex: 58% M) | Incidence; success rate; complications |
| NAP4 (2011) | PC | UK (2008–2009) | Trauma, Medical, CA | Surgical cric, needle cric (ER physicians, anaesthesiologists, surgeons) | 58 | Incidence; success rate clinical outcomes; complications |
| Beshey (2014) | RCT | Egypt (2011–2011) | Trauma, Medical, CA | Surgical cric | 169 (Percutaneous cricothyroidotomy = 85 and Percutaneous dilational tracheostomy = 84); (Age: Mean 46 ± 32 y) | Incidence; success rate; complications |
| Rosenstock (2016) | RC | Denmark (2008–2014) | Trauma, Medical, CA | Surgical cric (anaesthesiologists, surgeons) | 27 (Sex: 78% M; Age: Mean 57 y) | Incidence; success rate; complications |
| Darby (2018) | RC | USA (2008–2012) | Trauma, Medical, CA | Surgical cric, needle cric (physicians, anaesthesiologists, surgeons) | 22 (Sex: 77% M; Age: Mean 61 ± 11) | Incidence; success rate; Clinical outcomes; Complications |
| Kwon (2019) | RC | Korea (2007–2018) | Trauma, Medical, CA | Surgical cric, needle cric (ER, ENT) | 23 (Sex: 78% M; Age: Mean 63 y) | Success rates; ROSC; clinical outcomes; complications |
| Alkhouri (2020) | RC | Australia, New Zealand (2010–2015) | Trauma, Medical, CA | Surgical cric, tracheostomy (ER-physicians, intensivists, anaesthetists, GP) | 15 (Sex: 93% M; Age: Mean 54 y) | Complications |
| Willinge (2021) | RC | Netherlands (2013–2018) | Trauma, Medical, CA | Surgical cric (surgeons) | 52 (Age: Median 54 y) | Complications |
| Okada (2022) | RC | Japan (2012–2020) | Trauma, Medical, CA | Surgical cric, needle cric, tracheostomy (physicians) | 31 (Sex: 74% M; Age: Median 53 y) | Incidence; clinical outcomes; complications |
| George (2022) | RC | USA (2009–2019) | Trauma | Surgical cric | 51 (Sex: 77% M; Age: Average 45 ± 19 y) | Incidence; clinical outcomes |
| Jansen (2023) | RC | Germany (2014–2019) | In-hospital emergencies | Surgical cric | 8 | Incidence |
| Arora (2023) | RC | India (2021–2022) | Medical | Needle cric, tracheostomy | 17 (Sex: 41% M; Age: Mean 64 y) | Clinical outcomes |
| Offenbacher (2023) | RC | USA (2016–2018) | Trauma, Medical, CA | Surgical cric | 49 (Sex:80% M; Age: Median 41 y) | Incidence; success rate; clinical outcomes |
| In-hospital/pre-hospital settings | ||||||
| Nugent (1991) | RC | USA (1987–1989) | Trauma, Medical, CA | Surgical cric (HEMS-nurses) |
55 (Sex: 78% M; Age: Range 9–76 y) | Incidence; success rate; clinical outcomes; complications |
| Salvino (1993) | RC | USA (1988–1991) | Trauma | Surgical cric (paramedics, HEMS-nurses and paramedics, anaesthesiologists, surgeons) | 30 (Sex: 90% M) | Incidence; success rate; clinical outcomes; complications |
| Hawkins (1995) | RC | USA (1989–1993) | Trauma | Surgical cric(ER-physicians) | 66 | Incidence; clinical outcomes; complications |
| Bair (2003) | RC | USA (1995–2000) | Trauma, Medical | Surgical cric (HEMS, ER-physicians, surgeons) |
50 | Incidence; success rate; complications |
| McIntosh (2008) | RC | USA (1995–2004) | Trauma, Medical | Surgical cric (paramedics, HEMS-nurses, and paramedics) |
17 | Incidence; success rate clinical outcomes; complications |
| Graham (2011) | RC | USA (1995–2010) | Trauma, Medical, CA | Surgical cric | 94 (Sex: 94% M) | Success rate; ROSC; clinical outcomes; complications |
| Paix (2012) | Case series | Australia (1992–2011) | Trauma, Medical, CA | Surgical cric, needle cric | 24 (Sex: 88% M) | Success rate; complication |
| King (2012) | RC | USA (2000–2010) | Trauma | Surgical cric (paramedics, ER-physicians, surgeons) | 54 (Sex: 80% M; Age: Mean 50 ± 15) | Complications |
| Katzenell (2013) | RC | Israel (1997–2010) | Trauma | Surgical cric (paramedics, physicians) | 46 | Incidence; success rate; clinical outcomes. |
| High (2018) | RC | USA (2006–2015) | Trauma, Medical | Surgical cric (HEMS) | 13 (Sex: 75% M) | Incidence; success rate |
| Duggan (2018) | RC | Multicentre (2016–2017) | Trauma, Medical, CA | Surgical cric, needle cric, tracheostomy (paramedics; ER-physicians, anaesthesiologists, surgeons) | 99 (Sex: 74% M) | Success rate |
| Morocco (2021) | Case series | USA (2010–2020) | Trauma | Surgical cric (paramedics, surgeons) | 12 (Sex: 92% M; Age: Average 43 y) | Incidence; success rate; clinical outcomes; complications |
| Battlefield | ||||||
| Leibovici (1997) | RC | Israel (1991–1995) | Trauma | Surgical cric | 29 (Age: Median 20 ± 6 y) | Success rate; clinical outcomes; complications |
| Adams (2008) | PC | Iraq (2005–2007) | Trauma, Medical, CA | Surgical cric | 17 (Sex: 95% M) | Incidence; success rate; complications |
| Mabry (2012) | RC | Iraq, Afghanistan (2007–2009) | Trauma | Surgical cric | 72 (Sex: 96% M) | Success rate; clinical outcomes; complications |
| Lairet (2012) | PC | Afghanistan (2009–2011) | NA | Surgical cric | 15 | Incidence; complications |
| Barnard (2014) | RC | Afghanistan (2009–2013) | Trauma | Surgical cric (ground and flight-medics) | 34 (Sex: 97% M; Age: median 24y) | Incidence; success rate; clinical outcomes |
| Pugh (2015) | RC | Afghanistan (2013–2013) | Trauma | Surgical cric (paramedics) | 14 | Incidence; clinical outcomes; complications |
| Schauer (2015)* | RC | USA (2010–2012) | Trauma | Surgical cric (military-physicians and physician-assistants) | 32 (Age: Range ]36–56 y [) | Incidence; clinical outcomes |
| Tobin (2015) | RC | Afghanistan (2010–2010) | Trauma, CA | Surgical cric, tracheostomy (military personnel, HEMS- critical care team). |
42 | Incidence |
| Kyle (2016) | RC | Afghanistan (2006–2014) | Trauma | Surgical cric (general medic, medical emergency response team, combat EMT) | 86 (Sex: 100% M; Age: Median 25 y) | Success rate; clinical outcomes |
| Schauer (2018) | RC | Iraq, Afghanistan (2007–2016) | Trauma | Surgical cric | 230 (Afghanistan = 178 and Iraq = 52); (Sex: Iraq: 96% M; Afghanistan: 99% M) | Clinical outcomes; complications |
| Benov (2019) | RC | Israel, Syria (2013–2017) | Trauma, Medical | Surgical cric | 30 (Male:93%; Age: Median 24 y) | Incidence; success rate |
| Hudson (2020) | RC | Afghanistan (2008–2014) | Trauma | Surgical cric, tracheostomy | 85 (Sex: 98% M; Age: Median 25 y IQR [23–30]) | Incidence; clinical outcomes. |
| Beit ner (2021) | RC | Israel (1998–2018) | Trauma | Surgical cric (paramedics, ER-physicians) | 153 (Age: Mean 27 y) | Incidence; success rate; clinical outcomes |
Key: ALS – Advanced Life Support, CA – cardiac arrest, Cric – cricothyroidotomy, EMT – Emergency medical technician, ENT – Ear-Nose-Throat surgeon, ER – emergency room, GP – General practitioner (primary care doctor), HEMS – Helicopter Emergency Medical Services, HRQoL – Health-related quality of life), M – Male, PC – prospective cohort RC – retrospective cohort-Year.
Provider/Age/sex information reported where available.
Incidence of eFONA
The incidence of eFONA was described in 53 studies.42, 45, 46, 54, 65, 69, 72, 10, 11, 12, 13, 14, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 36, 37, 38, 39, 40, 48, 49, 50, 51, 56, 57, 58, 60, 61, 62, 74, 75, 76, 77, 78 Studies were conducted across the pre-hospital setting (n = 23, 43%), in-hospital setting (n = 13, 25%), pre-hospital/in-hospital setting (n = 8, 15%), and on the battlefield (n = 9, 17%). There were important differences in the denominator used to calculate incidence across studies, including all EMS calls, patients in whom tracheal intubation was attempted, and undefined population types (Table 2). None of the studies reported an incidence rate for patients in cardiac arrest. The lowest reported incidence was 0.06 per 1,000 patients receiving general anaesthesia, and the highest incidence was 436 per 1,000 patients with an identified difficult airway.36, 37
Table 2.
Incidence rate of eFONA.
| Study | eFONA attempts | Number in population (population definition) | Incidence per1000 (95% CI) |
|---|---|---|---|
| Pre-hospital | |||
| Boyle (1993) | 69 | 2,188 (air ambulance calls) | 31.53 (24.61–39.74) |
| Xeropotamos (1993) | 11 | 600 (treated by HEMS) | 18.33 (9.18–32.56) |
| Jacobson (1996) | 50 | 14,772 (transported by ambulance services) | 3.38 (2.51–4.46) |
| Gerich (1998) | 8 | 383 (airway management required) | 20.88 (9.05–40.74) |
| Thomas (1999) | 10 | 722 (airway management attempts) | 13.85 (6.66–25.32) |
| Robinson (2001) | 8 | 1,589 (tracheal intubation required) | 11.47 (7.75–16.34) |
| Bulger (2002) | 30 | 2,614 (tracheal intubation attempts) | 8.41 (5.28–12.71) |
| Germann (2009) | 6 | 369 (tracheal intubation attempts) | 16.26 (5.99–35.05) |
| Warner (2009) | 11 | 4,091 (tracheal intubation attempts) | 2.68 (1.34–4.80) |
| Wang (2011) | 88 | 88,180 (airway management attempts) | 0.99 (0.80–1.22) |
| Shapey (2012) | 16 | 5,490 (EMS calls) | 2.91 (1.66–4.72) |
| Kamiutsuri (2013) | 13 | 3,719 (treated by EMS) | 3.49 (1.86–5.97) |
| Brown (2014) | 35 | 4,871 (tracheal intubation attempts) | 7.18 (5.01–9.97) |
| Prekker (2014) | 30 | 7,523 (advanced airway attempts) | 3.98 (2.69–5.68) |
| Diggs (2014) | 1332 | 136,980 (airway management attempts) | 9.72 (9.21–10.25) |
| Peters (2015) | 19 | 1,399 (airway management required) | 13.58 (8.19–21.12) |
| Peters (2015) | 29 | 1,871 (airway management required) | 15.49 (10.40–22.18) |
| Sunde (2015) | 6 | 2,327 (tracheal intubation required) | 2.57 (0.94–5.60) |
| Gellerfors (2018) | 9 | 2,054 (tracheal intubation required) | 4.38 (2.01–8.30) |
| Schober (2019) | 18 | 10,252 (air ambulance Calls) | 1.75 (1.04–2.77) |
| Aziz (2021) | 72 | 37,725 (EMS calls) | 1.90 (1.49–2.40) |
| Himmler (2023) | 95 | 953 (critical airway team activations) | 99.68(81.40–120.49) |
| Malkan (2023) | 251 | 258,976 (cases registered) | 0.96 (0.85–1.09) |
| In-hospital | |||
| McGill (1982) | 38 | 1,362 (tracheal intubation required) | 27.90 (19.81–38.09) |
| Erlandson (1989) | 39 | 2,287 (tracheal intubation required) | 17.05 (12.15–23.23) |
| Bair (2002) | 22 | 7,712 (tracheal intubation attempts) | 2.85 (1.78–4.31) |
| Wong (2008) | 8 | 2,343 (advanced airway required) | 3.41 (1.47–6.72) |
| NAP4 (2011) | 58 | 133 (difficult airway cases) | 436.09 (350.34–524.74) |
| Cook (2011) | 75 | 286 (major complications of airway management reports) | 262.23 (212.21–317.26) |
| Beshey (2014) | 163 | 3,785 (advanced airway required) | 43.06 (36.82–50.03) |
| Rosenstock (2016) | 27 | 452,461 (general anaesthesia patients) | 0.06 (0.03–0.08) |
| Darby (2016) | 22 | 266 (difficult airway cases) | 82.70 (52.55–122.54) |
| George (2022) | 51 | 29,213 (tracheal intubation required) | 1.75 (1.30–2.29) |
| Okada (2022) | 31 | 75,529 (emergency cases) | 0.41 (0.27–0.58) |
| Jansen (2023) | 8 | 14,166(emergency interventions) | 0.56 (0.24–1.11) |
| Offenbacher (2023) | 49 | 17,720 (tracheal intubation attempts) | 2.76 (2.05–3.65) |
| Pre-hospital /in-hospital | |||
| Nugent (1991) | 55 | 302 (airway management required) | 185.43 (143.21–233.93) |
| Salvino (1993) | 30 | 8,320 (trauma admissions) | 3.61 (2.43–5.14) |
| Hawkins (1993) | 66 | 525 (airway management required) | 125.71 (98.57–157.14) |
| Bair (2003) | 50 | 2,730 (tracheal intubation attempts) | 18.31 (13.62–24.07) |
| McIntosh (2008) | 17 | 712 (advanced airway required) | 23.87 (13.96–37.95) |
| Katzenell (2012) | 46 | 406 (tracheal intubation attempts) | 113.31 (84.15–148.22) |
| High (2018) | 13 | 22,434 (EMS calls) | 0.57 (0.31–0.99) |
| Moroco (2021) | 12 | 1,642 (trauma cases identified) | 7.30 (3.78–12.73) |
| Battlefield | |||
| Adams (2008) | 17 | 293 (advanced airway attempts) | 58.02 (34.15–91.27) |
| Lairet (2012) | 15 | 1,003 (combat cases) | 14.95 (8.39–24.54) |
| Barnard (2014) | 34 | 1,927 (cases identified) | 17.64 (12.24–24.56) |
| Pugh (2015) | 14 | 57 (advanced airway attempts) | 245.61 (141.26–377.61) |
| Schauer (2015) | 32 | 14,233 (trauma admissions) | 2.24 (1.53–3.17) |
| Tobin (2015) | 42 | 1,198 (transportation events) | 35.05 (25.38–47.09) |
| Benov (2019) | 30 | 134 (advanced airway attempts) | 223.88 (156.43–303.92) |
| Hudson (2020) | 85 | 890 (airway management attempts) | 95.51 (76.99–116.74) |
| Beit Ner (2021) | 153 | 17,702 (recorded casualties) | 8.64 (7.33–10.11) |
EMS: Emergency medical services; HEMS: Helicopter emergency medical services.
eFONA success rates
The eFONA success rate was reported in 40 studies.15, 17, 18, 23, 24, 26, 27, 29, 36, 37, 41, 44, 60, 61, 70, 71, 73, 10, 11, 12, 13, 31, 32, 33, 34, 48, 49, 50, 54, 55, 56, 57, 58, 63, 64, 65, 75, 76, 77, 78 The most common location was the pre-hospital setting (n = 15, 38%), followed by in-hospital setting (n = 8, 20%), pre-hospital/in-hospital setting (n = 10, 25%) and in the battlefield (n = 7, 18%). Six studies reported a success rate of less than 70%.12, 18, 29, 49, 57, 70 However, 22% of the studies reported a 100% success rate of the performed eFONA.10, 27, 54, 58, 61, 63, 65 The median success rate of eFONA among all settings was 91% (Table 3). None of the studies reported a success rate for patients in cardiac arrest.
Table 3.
Efona success rate.
| Study | Number of eFONA cases | Number of successful eFONA | Success rate% (95% CI) |
|---|---|---|---|
| Pre-hospital | |||
| Spaite (1990) | 16 | 14 | 88% (62–98) |
| Boyle (1993) | 69 | 68 | 99% (92–99) |
| Xeropotamos (1993) | 11 | 11 | 100% (71–100*) |
| Jacobson (1996) | 50 | 47 | 94% (83–98) |
| Gerich (1998) | 8 | 8 | 100% (63–100*) |
| Thomas (1999) | 10 | 9 | 90% (55–99) |
| Robinson (2001) | 8 | 5 | 63% (24–91) |
| Warner (2009) | 10 | 9 | 90% (55–99) |
| Germann (2009) | 6 | 6 | 100% (54–100*) |
| Wang (2011) | 88 | 61 | 69% (58–78) |
| Kamiutsuri (2013) | 13 | 11 | 85% (54–98) |
| Diggs (2014) | 1332 | 457 | 34% (31–36) |
| Brown (2014) | 35 | 34 | 97% (85–99) |
| Schober (2019) | 230 | 216 | 94% (89–96) |
| Aziz (2021) | 11 | 10 | 91% (58–99) |
| In-hospital | |||
| Gillespie (1999) | 35 | 34 | 97% (85–99) |
| Wong (2008) | 8 | 7 | 88% (47–99) |
| Cook (2011) | 58 | 21 | 36% (23–49) |
| NAP4 (2011) | 58 | 50 | 86% (74–93) |
| Beshey (2014) | 169 | 163 | 96% (92–98) |
| Darby (2016) | 22 | 20 | 91% (70–98) |
| Rosenstock (2016) | 27 | 21 | 78% (57–91) |
| Kwon (2019) | 23 | 17 | 74% (51–89) |
| Pre-hospital/In-hospital | |||
| Nugent (1991) | 55 | 53 | 96% (87–99) |
| Salvino (1993) | 30 | 30 | 100% (88–100*) |
| Bair (2003) | 50 | 50 | 100% (92–100*) |
| McIntosh (2008) | 17 | 17 | 100% (80–100*) |
| Graham (2011) | 94 | 94 | 100% (96–100*) |
| Paix (2012) | 24 | 24 | 100% (85–100*) |
| Katzenell (2012) | 46 | 43 | 93% (82–98) |
| Duggan (2018) | 99 | 71 | 72% (61–80) |
| High (2018) | 13 | 13 | 100% (75–100*) |
| Moroco (2021) | 12 | 7 | 58% (27–84) |
| Battlefield | |||
| Leibovici (1997) | 29 | 26 | 90% (72–97) |
| Adams (2008) | 17 | 13 | 76% (50–93) |
| Mabry (2012) | 72 | 49 | 68% (56–78) |
| Barnard (2014) | 34 | 28 | 82% (65–93) |
| Kyle (2016) | 86 | 79 | 92% (83–96) |
| Benov (2019) | 30 | 25 | 83% (65–94) |
| Beit Ner (2021) | 153 | 135 | 88% (82–92) |
One-sided, 97.5% confidence interval.
Clinical outcomes
Clinical outcomes in patients who received eFONA were reported in 38 studies.10, 11, 15, 17, 19, 21, 22, 24, 27, 30, 32, 36, 43, 52, 54, 60, 62, 63, 73, 74, 76, 39, 40, 41, 45, 46, 47, 48, 56, 57, 58, 67, 68, 69, 70, 71 Of these, 11 (29%) were pre-hospital studies, 11 (29%) were in-hospital studies, seven (18%) were in-hospital/pre-hospital, and nine (24%) were battlefield studies.
Nine studies reported the rate of return of spontaneous circulation (ROSC) in patients who had a cardiac arrest and who received eFONA at some point during their treatment.10, 16, 18, 19, 21, 24, 32, 41, 63 Across studies, the return of spontaneous circulation rate ranged from 0% to 64% (Table 4).
Table 4.
Summary of outcomes in patients with eFONA that sustained a cardiac arrest.
Eleven studies (seven pre-hospital, one in-hospital, and three battlefield) reported the outcome of survival to hospital admission.11, 17, 19, 21, 27, 30, 32, 39, 69, 71, 74 Across studies, the survival rate of hospital admission ranged from 19% to 73% (Table 5).
Table 5.
Clinical outcomes across all patients with eFONA.
| Setting | Number of patients (number of studies) | Clinical outcome |
|---|---|---|
| Survival to hospital admission | ||
| Pre-hospital | 195 (seven studies)11, 17, 19, 21, 27, 30, 32 | 29% (range 19–91%) |
| In-hospital | 49 (One study)39 | 73% |
| Pre-hospital and in-hospital | NA | NA |
| Battlefield | 127 (Three studies)69, 71, 74 | 53% (range 46–55%) |
| Survival to hospital discharge/30-days | ||
| Pre-hospital | 423(Seven studies)10, 15, 17, 22, 24, 27, 32 | 64% (range 7–98%) |
| In-hospital | 255 (Eight studies)38, 40, 41, 46, 47, 48 | 42% (range 13–82%) |
| Pre-hospital and in-hospital | 227 (Six studies) 54, 60, 57, 58 | 32% (range 27–75%) |
| Battlefield | 692 (Seven studies)67, 68, 70, 73, 74, 76, 77 | 45% (range 4–67%) |
| Survival to hospital discharge/30-days with good functional outcome | ||
| Pre-hospital | 77 (Three studies)10, 15, 24 | 5% (range 0–27%) |
| In-hospital | 158 (Four studies)36, 43, 46, 47 | 44% (range 5–69%) |
| Pre-hospital and in-hospital | 112 (Two studies)58, 63 | 33% (range 29–34%) |
| Battlefield | 34 (One study)77 | 9% |
Twenty-eight studies (seven pre-hospital, eight in-hospital, six pre-hospital/in-hospital, and seven battlefield) reported the outcome of survival until hospital discharge or 30-days. 10, 15, 17, 22, 24, 27, 32, 38, 40, 41, 52, 54, 60, 62, 67, 68, 70, 73, 74, 76, 46, 47, 48, 56, 57, 58 In these studies, survival ranged from 4 to 98%. Most studies reported a survival rate of less than 67% (Table 5).
Ten studies (three pre-hospital, four in-hospital, two pre-hospital/in-hospital, and one battlefield) reported survival to hospital discharge or 30 days with favourable neurological outcomes.10, 15, 24, 36, 43, 46, 47, 58, 63, 77 The survival to hospital discharge or 30 days with favourable neurological outcome ranged from 0% to 69%. One study used the Glasgow Coma Scale (GCS) to assess neurological outcomes (Table 5).63.
Five studies (three pre-hospital and two in-hospital setting studies) reported health-related quality-of-life outcomes. None of the studies specified which scales or parameters were used to measure the results. Two studies reported that patients could speak normally after discharge.40, 46 Poor patient health after eFONA was reported in one study, but another reported good recovery after the procedure.10, Finally, one study reported that patients could care for themselves and were in an ambulatory status.32
Complications
Overall, 36 studies (eight (22%) pre-hospital, 13 (36%) in-hospital, nine (25%) combined in-hospital and pre-hospital, six (17%) in the battlefield setting) reported complications with eFONA.11, 12, 20, 22, 24, 27, 32, 40, 41, 43, 44, 53, 54, 62, 63, 65, 67, 70, 71, 16, 17, 35, 36, 37, 38, 46, 47, 48, 49, 50, 56, 57, 58, 59 Four studies reported immediate complications, including incorrect site of tube placement, procedure time greater than 3 min, and haemorrhage.32, 40, 56, 63 One study reported a long-term complication: laryngeal fracture with permanent dysphonia.40 Other studies reported a range of other complications, such as bleeding, tracheal erosion and supraglottic inflammation.
Discussion
Our scoping review, which included total of 4,457 eFONA attempts across 69 studies, provides important information on eFONA incidence, success rates, clinical outcomes, and complications. We identified no studies specific to adults in cardiac arrest. We found marked variation in the denominator used to calculate eFONA incidence with associated marked variation in incidence across studies. The reported success rates of eFONA were generally high and clinical outcomes appear to be influenced by the study setting.
Our scoping review builds on Morton and colleague’s recently published systematic review and meta-analysis that focused on success rates of eFONA in the pre-hospital setting.8 Morton et al.’s systematic review included 69 studies and found an overall eFONA success rate of 88%, with higher success rates reported with surgical techniques (92%) than needle techniques (52%). In contrast to that review, our review had a broader scope and we chose to exclude small case series due to their high risk of selection bias, such that we included fewer pre-hospital studies. Nevertheless, the reported overall success rate in our review (91%) was comparable to that reported by Morton et al (88%).
The European Resuscitation Council and American Heart Association both recognise that there may be a need for eFONA during cardiac arrest.1, 79 There are likely two main patient groups in which eFONA may need to be considered. First, a patient might have a hypoxic cardiac arrest in an established “cannot intubate, cannot oxygenate” scenario, where face-mask ventilation and placement of a supraglottic airway device has already been unsuccessful. In this case, UK Difficult Airway Society guidelines provide a clear framework for progression to eFONA as a ‘Plan D’ airway management strategy.7
The second patient group is patients in cardiac arrest in which providers are unable to successfully site a tracheal tube or supraglottic airway, due to patient anatomy, cardiac arrest aetiology, or environmental factors. In such cases, UK Difficult Airway Society guidelines recommend that providers attempt face-mask ventilation.7 However, the adequacy of face-mask ventilation can be challenging to assess during cardiac arrest due to ongoing chest compressions and because standard strategies for determining adequate oxygenation, such as pulse oximetry, are unreliable in cardiac arrest.1, 80 In such cases, healthcare providers will need to make a clinical judgement regarding the need for eFONA. Recent qualitative research with UK critical care paramedics described the stress associated with making a decision to perform eFONA.81 Our review findings provide reassurance that when appropriately skilled healthcare providers attempt eFONA, the success rate is usually high in all clinical settings, although index studies rarely provided information on provider training or exposure to eFONA. There is a need for further studies that report the incidence, success rate, and outcomes of patients in cardiac arrest that receive eFONA. However, undertaking high-quality studies is likely to be extremely challenging due to the low incidence of eFONA in this population.
This review has two important limitations. First, the index studies were extremely heterogeneous, in relation to study design, healthcare provider, and setting. Second, we chose not to undertake a risk or bias assessment as our overriding objective was to characterise the volume and type of existing evidence, rather than draw conclusions to inform clinical practice.82 Third, we chose to focus our scoping review on eFONA in adults. eFONA placement in children may be more challenging due to both patient factors and provider confidence and expertise, limiting the generalisability of our findings to children.83 A recent review highlighted that few data are available on eFONA in children.83
Conclusion
Our scoping review found no studies specifically focusing on the use of eFONA during adult cardiac arrest. The available evidence suggests that the incidence of eFONA is generally low, but that, when attempted, the success rate is typically high.
Funding
MA and AAA are undertaking PhDs which are financially supported by Prince Sultan College for Emergency Medical Services, King Saud University, Riyadh, Saudi Arabia.
CRediT authorship contribution statement
Mohammed Aljanoubi: Writing – review & editing, Writing – original draft, Methodology, Formal analysis, Conceptualization. Abdulkarim A. Almazrua: Writing – review & editing, Investigation. Samantha Johnson: Writing – review & editing, Investigation. Ian R Drennan: Writing – review & editing, Investigation, Conceptualization. Joshua C. Reynolds: Writing – review & editing, Investigation, Conceptualization. Jasmeet Soar: Writing – review & editing, Investigation, Conceptualization. Keith Couper: Writing – review & editing, Writing – original draft, Supervision, Methodology, Conceptualization.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: ‘JS is an Editor of the journal Resuscitation (payment received from the publisher, Elsevier) and Editorial Board member of Resuscitation Plus. KC is an Associate Editor of Resuscitation Plus (payment received from the publisher, Elsevier). IRD, JCR, JS, and KC are current or former members of the ILCOR ALS task force.’.
Footnotes
Supplementary material to this article can be found online at https://doi.org/10.1016/j.resplu.2024.100653.
Contributor Information
Keith Couper, Email: k.couper@warwick.ac.uk.
International Liaison Committee on Resuscitation Advanced Life Support Taskforce:
Katherine M. Berg, Bernd W. Böttiger, Yew Woon Chia, Conor Crowley, Sonia D'Arrigo, Charles D. Deakin, Shannon M. Fernando, Rakesh Garg, Asger Granfeldt, Brian Grunau, Karen G. Hirsch, Mathias J. Holmberg, Eric Lavonas, Carrie Leong, Peter J. Kudenchuk, Peter Morley, Ari Moskowitz, Robert Neumar, Tonia C. Nicholson, Nikolaos Nikolaou, Jerry P. Nolan, Brian O'Neil, Shinichiro Ohshimo, Michael Parr, Helen Pocock, Claudio Sandroni, Tommaso Scquizzato, Markus Skrifvars, Neville Vlok, Michelle Welsford, and Carolyn Zelop
Appendix A. Supplementary material
The following are the Supplementary material to this article:
References
- 1.Soar J., Böttiger B.W., Carli P., et al. European resuscitation council guidelines 2021: adult advanced life support. Resuscitation. 2021;161:115–151. doi: 10.1016/j.resuscitation.2021.02.010. [DOI] [PubMed] [Google Scholar]
- 2.Newell C., Grier S., Soar J. Airway and ventilation management during cardiopulmonary resuscitation and after successful resuscitation. Critical Care. 2018;22:190. doi: 10.1186/s13054-018-2121-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benger J.R., Kirby K., Black S., et al. Effect of a strategy of a supraglottic airway device vs tracheal intubation during out-of-hospital cardiac arrest on functional outcome: The AIRWAYS-2 randomized clinical trial. JAMA. 2018;320:779–791. doi: 10.1001/jama.2018.11597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang H.E., Schmicker R.H., Daya M.R., et al. Effect of a strategy of initial laryngeal tube insertion vs endotracheal intubation on 72-hour survival in adults with out-of-hospital cardiac arrest: A randomized clinical trial. JAMA. 2018;320:769–778. doi: 10.1001/jama.2018.7044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Watkins S., Chowdhury F.J., Norman C., et al. Randomised trial of the clinical and cost effectiveness of a supraglottic airway device compared with tracheal intubation for in-hospital cardiac arrest (AIRWAYS-3): Protocol, design and implementation. Resusc Plus. 2023;15 doi: 10.1016/j.resplu.2023.100430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moskowitz A., Andrea L., Shiloh A.L., et al. Design and implementation of the hospital airway resuscitation trial. Resusc Plus. 2024;17 doi: 10.1016/j.resplu.2023.100512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Frerk C., Mitchell V.S., McNarry A.F., et al. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015;115:827–848. doi: 10.1093/bja/aev371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morton S., Avery P., Kua J., et al. Success rate of prehospital emergency front-of-neck access (FONA): a systematic review and meta-analysis. Br J Anaesth. 2023;130:636–644. doi: 10.1016/j.bja.2023.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tricco A.C., Lillie E., Zarin W., et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 10.Xeropotamos N.S., Coats T.J., Wilson A.W. Prehospital surgical airway management: 1 year's experience from the Helicopter Emergency Medical Service. Injury. 1993;24:222–224. doi: 10.1016/0020-1383(93)90172-3. [DOI] [PubMed] [Google Scholar]
- 11.Warner K.J., Bulger E.M., Sharar S.R., et al. Prehospital management of the difficult airway: A prospective cohort study. J Emerg Med. 2009;36:257–265. doi: 10.1016/j.jemermed.2007.10.058. [DOI] [PubMed] [Google Scholar]
- 12.Wang H.E., Mann N.C., Jacobson K., et al. Out-of-hospital airway management in the United States. Resuscitation. 2011;82:378–385. doi: 10.1016/j.resuscitation.2010.12.014. [DOI] [PubMed] [Google Scholar]
- 13.Thomas S.H., Harrison T.H., Wedel S.K. Flight crew airway management in four settings: a six-year review. Prehosp Emerg Care. 1999;3:310–315. doi: 10.1080/10903129908958960. [DOI] [PubMed] [Google Scholar]
- 14.Sunde G.A., Heltne J.K., Lockey D., et al. Airway management by physician-staffed Helicopter Emergency Medical Services – a prospective, multicentre, observational study of 2,327 patients. Scand J Trauma Resusc Emerg Med. 2015;23:57. doi: 10.1186/s13049-015-0136-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spaite D.W., Joseph M. Prehospital cricothyrotomy: an investigation of indications, technique, complications, and patient outcome. Ann Emerg Med. 1990;19:279–285. doi: 10.1016/s0196-0644(05)82045-1. [DOI] [PubMed] [Google Scholar]
- 16.Shapey I.M., Kumar D.S., Roberts K. Invasive and surgical procedures in pre-hospital care: what is the need? Eur J Trauma Emerg Surg. 2012;38:633–639. doi: 10.1007/s00068-012-0207-9. [DOI] [PubMed] [Google Scholar]
- 17.Schober P., Biesheuvel T., de Leeuw M.A., et al. Prehospital cricothyrotomies in a helicopter emergency medical service: analysis of 19,382 dispatches. BMC Emerg Med. 2019;19:12. doi: 10.1186/s12873-019-0230-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Robinson K.J., Katz R., Jacobs L.M. A 12-year experience with prehospital cricothyrotomies. Air Med J. 2001;20:27–30. [PubMed] [Google Scholar]
- 19.Prekker M.E., Carlbom D., Kwok H., et al. The process of prehospital airway management: Challenges and solutions during paramedic endotracheal intubation. Crit Care Med. 2014;42:1372–2138. doi: 10.1097/CCM.0000000000000213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peters J., van Wageningen B., Hendriks I., et al. First-pass intubation success rate during rapid sequence induction of prehospital anaesthesia by physicians versus paramedics. Eur J Emerg Med. 2015;22:391–394. doi: 10.1097/MEJ.0000000000000161. [DOI] [PubMed] [Google Scholar]
- 21.Peters J., Bruijstens L., van der Ploeg J., et al. Indications and results of emergency surgical airways performed by a physician-staffed helicopter emergency service. Injury. 2015;46:787–790. doi: 10.1016/j.injury.2014.11.024. [DOI] [PubMed] [Google Scholar]
- 22.Malkan R.M., Borelli C.M., Fairley R.R., et al. Outcomes after prehospital cricothyrotomy. Med J. 2023:70–73. [PubMed] [Google Scholar]
- 23.Kamiutsuri K., Okutani R., Kozawa S. Analysis of prehospital endotracheal intubation performed by emergency physicians: retrospective survey of a single emergency medical center in Japan. J Anesth. 2013;27:374–379. doi: 10.1007/s00540-012-1528-x. [DOI] [PubMed] [Google Scholar]
- 24.Jacobson L.E., Gomez G.A., Sobieray R.J., et al. Surgical cricothyroidotomy in trauma patients: analysis of its use by paramedics in the field. J Trauma Acute Care Surg. 1996;41:15–20. doi: 10.1097/00005373-199607000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Himmler A., McDermott C., Martucci J., et al. Code critical airway: A collaborative solution to a catastrophic problem. Am Surg. 2023;89:2460–3247. doi: 10.1177/00031348221101485. [DOI] [PubMed] [Google Scholar]
- 26.Germann C.A., Baumann M.R., Kendall K.M., et al. Performance of endotracheal intubation and rescue techniques by emergency services personnel in an air medical service. Prehosp Emerg Care. 2009;13:44–49. doi: 10.1080/10903120802474505. [DOI] [PubMed] [Google Scholar]
- 27.Gerich T.G., Schmidt U., Hubrich V., et al. Prehospital airway management in the acutely injured patient: the role of surgical cricothyrotomy revisited. J Trauma. 1998;45:312–314. doi: 10.1097/00005373-199808000-00017. [DOI] [PubMed] [Google Scholar]
- 28.Gellerfors M., Fevang E., Bäckman A., et al. Pre-hospital advanced airway management by anaesthetist and nurse anaesthetist critical care teams: a prospective observational study of 2028 pre-hospital tracheal intubations. Br J Anaesth. 2018;120:1103–1119. doi: 10.1016/j.bja.2017.12.036. [DOI] [PubMed] [Google Scholar]
- 29.Diggs L.A., Yusuf J.E., De Leo G. An update on out-of-hospital airway management practices in the United States. Resuscitation. 2014;85:885–892. doi: 10.1016/j.resuscitation.2014.02.032. [DOI] [PubMed] [Google Scholar]
- 30.Bulger E.M., Copass M.K., Maier R.V., et al. An analysis of advanced prehospital airway management. J Emerg Med. 2002;23:183–189. doi: 10.1016/s0736-4679(02)00490-0. [DOI] [PubMed] [Google Scholar]
- 31.Brown Iii C.A., Walls R.M., Cox K., et al. 4,871 Emergency airway encounters by air medical providers: A report of the Air Transport Emergency Airway Management (NEAR VI: “A-TEAM”) project. West J Emerg Med. 2014;15:188–193. doi: 10.5811/westjem.2013.11.18549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boyle M.F., Hatton D., Sheets C. Surgical cricothyrotomy performed by air ambulance flight nurses: A 5-year experience. J Emerg Med. 1993;11:41–45. doi: 10.1016/0736-4679(93)90008-u. [DOI] [PubMed] [Google Scholar]
- 33.Aziz S., Foster E., Lockey D.J., et al. Emergency scalpel cricothyroidotomy use in a prehospital trauma service: a 20-year review. Emerg Med j. 2021;38:349–354. doi: 10.1136/emermed-2020-210305. [DOI] [PubMed] [Google Scholar]
- 34.Wong E., Ng Y.-Y. The difficult airway in the emergency department. Int J Emerg. 2008;1:107–111. doi: 10.1007/s12245-008-0030-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Willinge G.J.A., Hietbrink F., Leenen L.P.H. Surgical airway procedures in emergency surgical patients: Results of what has become a back-up procedure. World J Surg. 2021;45:2683–2693. doi: 10.1007/s00268-021-06110-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cook T, Woodall N, Frerk C (Eds). 4th National Audit Project of The Royal College of Anaesthetists and The Difficult Airway Society: Major complications of airway management in the United Kingdom: Report and findings, March 2011. 2011 (Accessed 15 April 2024 at https://www.rcoa.ac.uk/media/32521). [DOI] [PubMed]
- 37.Rosenstock C.V., Norskov A.K., Wetterslev J., et al. Emergency surgical airway management in Denmark: a cohort study of 452 461 patients registered in the Danish Anaesthesia Database. Br J Anaesth. 2016;117:i75–i82. doi: 10.1093/bja/aew190. [DOI] [PubMed] [Google Scholar]
- 38.Okada A., Okada Y., Kandori K., et al. Adverse events of emergency surgical front of neck airway access: an observational descriptive study. Acute Med Surg. 2022;9:e750. doi: 10.1002/ams2.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Offenbacher J., Nikolla D.A., Carlson J.N., et al. Incidence of rescue surgical airways after attempted orotracheal intubation in the emergency department: A National Emergency Airway Registry (NEAR) Study. Am j Emerg Med. 2023;68:22–27. doi: 10.1016/j.ajem.2023.02.020. [DOI] [PubMed] [Google Scholar]
- 40.McGill J., Clinton J.E., Ruiz E. Cricothyrotomy in the emergency department. Ann Emerg Med. 1982;11:361–364. doi: 10.1016/s0196-0644(82)80362-4. [DOI] [PubMed] [Google Scholar]
- 41.Kwon Y.S., Lee C.A., Park S., et al. Incidence and outcomes of cricothyrotomy in the “cannot intubate, cannot oxygenate” situation. Medicine. 2019;98:e17713. doi: 10.1097/MD.0000000000017713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jansen G., Scholz S.S., Rehberg S.W., et al. Indications and measures of medical emergency teams: a retrospective evaluation of in-hospital emergency operations of the German Resuscitation Register. Minerva Anestesiol. 2023;89:56–65. doi: 10.23736/S0375-9393.22.16665-4. [DOI] [PubMed] [Google Scholar]
- 43.Isaacs J.H., Jr. Emergency cricothyrotomy: long-term results. Am Surg. 2001;67:346–350. [PubMed] [Google Scholar]
- 44.Gillespie M.B., Eisele D.W. Outcomes of emergency surgical airway procedures in a hospital-wide setting. The Laryngoscope. 1999;109:1766–1769. doi: 10.1097/00005537-199911000-00008. [DOI] [PubMed] [Google Scholar]
- 45.George N., Consunji G., Storkersen J., et al. Comparison of emergency airway management techniques in the performance of emergent Cricothyrotomy. Int j Emerg. 2022;15:24. doi: 10.1186/s12245-022-00427-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Erlandson M.J., Clinton J.E., Ruiz E., et al. Cricothyrotomy in the emergency department revisited. J Emerg Med. 1989;7:115–118. doi: 10.1016/0736-4679(89)90254-0. [DOI] [PubMed] [Google Scholar]
- 47.DeLaurier G.A., Hawkins M.L., Treat R.C., et al. Acute airway management. Role of cricothyroidotomy. Am Surg. 1990;56:12–15. [PubMed] [Google Scholar]
- 48.Darby J.M., Halenda G., Chou C., et al. Emergency surgical airways following activation of a difficult airway management team in hospitalized critically Ill patients: A case series. J Intensive Care Med. 2018;33:517–526. doi: 10.1177/0885066616680594. [DOI] [PubMed] [Google Scholar]
- 49.Cook T.M., Woodall N., Harper J., et al. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 2: Intensive care and emergency departments. Br J Anaesth. 2011;106:632–642. doi: 10.1093/bja/aer059. [DOI] [PubMed] [Google Scholar]
- 50.Beshey B.N., Helmy T.A., Asaad H.S., et al. Emergency percutaneous tracheotomy in failed intubation. Egypt J Chest Dis Tuberc. 2014;63:939–945. [Google Scholar]
- 51.Bair A.E., Filbin M.R., Kulkarni R.G., et al. The failed intubation attempt in the emergency department: analysis of prevalence, rescue techniques, and personnel. J Emerg Med. 2002;23:131–140. doi: 10.1016/s0736-4679(02)00501-2. [DOI] [PubMed] [Google Scholar]
- 52.Arora R.D., Rao K.N., Satpute S., et al. Emergency tracheostomy in locally advanced anaplastic thyroid cancer. Indian J Surg Oncol. 2023;14:714–722. doi: 10.1007/s13193-023-01753-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Alkhouri H., Richards C., Miers J., et al. Case series and review of emergency front-of-neck surgical airways from The Australian and New Zealand Emergency Department Airway Registry. Emerg Med Australas. 2021;33:499–507. doi: 10.1111/1742-6723.13678. [DOI] [PubMed] [Google Scholar]
- 54.Salvino C.K., Dries D., Gamelli R., et al. Emergency cricothyroidotomy in trauma victims. J Trauma. 1993;34:503–505. doi: 10.1097/00005373-199304000-00006. [DOI] [PubMed] [Google Scholar]
- 55.Paix B.R., Griggs W.M. Emergency surgical cricothyroidotomy: 24 successful cases leading to a simple 'scalpel-finger-tube' method. Emerg Med Australas. 2012;24:23–30. doi: 10.1111/j.1742-6723.2011.01510.x. [DOI] [PubMed] [Google Scholar]
- 56.Nugent W.L., Rhee K.J., Wisner D.H. Can nurses perform surgical cricothyrotomy with acceptable success and complication rates? Ann Emerg Med. 1991;20:367–370. doi: 10.1016/s0196-0644(05)81656-7. [DOI] [PubMed] [Google Scholar]
- 57.Moroco A.E., Armen S.B., Goldenberg D. Emergency cricothyrotomy: A 10-year single institution experience. Am Surg. 2021 doi: 10.1177/0003134821995075. [DOI] [PubMed] [Google Scholar]
- 58.McIntosh S.E., Swanson E.R., Barton E.D. Cricothyrotomy in air medical transport. J Trauma. 2008;64:1543–2157. doi: 10.1097/TA.0b013e3181271b60. [DOI] [PubMed] [Google Scholar]
- 59.King D., Ogilvie M., Michailidou M., et al. Fifty-four emergent cricothyroidotomies: are surgeons reluctant teachers? Scand J Surg. 2012;101:13–15. doi: 10.1177/145749691210100103. [DOI] [PubMed] [Google Scholar]
- 60.Katzenell U., Lipsky A.M., Abramovich A., et al. Prehospital intubation success rates among Israel Defense Forces providers: epidemiologic analysis and effect on doctrine. J Trauma Acute Care Surg. 2013;75:S178–S183. doi: 10.1097/TA.0b013e318299d650. [DOI] [PubMed] [Google Scholar]
- 61.High K., Brywczynski J., Han J.H. Cricothyrotomy in helicopter emergency medical service transport. Air Med j. 2018;37:51–53. doi: 10.1016/j.amj.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 62.Hawkins M.L., Shapiro M.B., Cue J.I., et al. Emergency cricothyrotomy: a reassessment. Am Surg. 1995;61:52–55. [PubMed] [Google Scholar]
- 63.Graham D.B., Eastman A.L., Aldy K.N., et al. Outcomes and long term follow-up after emergent cricothyroidotomy: is routine conversion to tracheostomy necessary? Am Surg. 2011;77:1707–1711. doi: 10.1177/000313481107701248. [DOI] [PubMed] [Google Scholar]
- 64.Duggan L., Lockhart S., Cook T., et al. The Airway App: exploring the role of smartphone technology to capture emergency front-of-neck airway experiences internationally. Anaesthesia. 2018;73:703–710. doi: 10.1111/anae.14247. [DOI] [PubMed] [Google Scholar]
- 65.Bair A.E., Panacek E.A., Wisner D.H., et al. Cricothyrotomy: A 5-year experience at one institution. J Emerg Med. 2003;24:151–216. doi: 10.1016/s0736-4679(02)00715-1. [DOI] [PubMed] [Google Scholar]
- 66.Tobin J.M., Nordmann G.R., Kuncir E.J. Resuscitation During Critical Care Transportation in Afghanistan. J Spec Oper Med. 2015;15:72–75. doi: 10.55460/V3ZO-RG71. [DOI] [PubMed] [Google Scholar]
- 67.Schauer S.G., Naylor J.F., Maddry J.K., et al. Prehospital airway management in Iraq and Afghanistan: A descriptive analysis. South Med J. 2018;111:707–713. doi: 10.14423/SMJ.0000000000000906. [DOI] [PubMed] [Google Scholar]
- 68.Schauer S.G., Bellamy M.A., Mabry R.L., et al. A comparison of the incidence of cricothyrotomy in the deployed setting to the emergency department at a level 1 military trauma center: a descriptive analysis. Mil Med. 2015;180:60–63. doi: 10.7205/MILMED-D-14-00384. [DOI] [PubMed] [Google Scholar]
- 69.Pugh H.E.J., LeClerc S., McLennan J. A review of pre-admission advanced airway management in combat casualties, Helmand Province 2013. J R Army Med Corps. 2015;161:121–216. doi: 10.1136/jramc-2014-000271. [DOI] [PubMed] [Google Scholar]
- 70.Mabry R.L. An analysis of battlefield cricothyrotomy in Iraq and Afghanistan. J Spec Oper Med. 2012;12:17–23. doi: 10.55460/FYQG-8E49. [DOI] [PubMed] [Google Scholar]
- 71.Leibovici D., Gofrit O.N., Blumenfeld A., et al. Prehospital cricothyroidotomy by physicians. Am j Emerg Med. 1997;15:91–93. doi: 10.1016/s0735-6757(97)90059-0. [DOI] [PubMed] [Google Scholar]
- 72.Lairet J.R., Bebarta V.S., Burns C.J., et al. Prehospital interventions performed in a combat zone: a prospective multicenter study of 1,003 combat wounded. J Trauma Acute Care Surg. 2012;73:S38–S42. doi: 10.1097/TA.0b013e3182606022. [DOI] [PubMed] [Google Scholar]
- 73.Kyle T., le Clerc S., Thomas A., et al. The success of battlefield surgical airway insertion in severely injured military patients: a UK perspective. J R Army Med Corps. 2016;162:460–544. doi: 10.1136/jramc-2016-000637. [DOI] [PubMed] [Google Scholar]
- 74.Hudson I.L., Blackburn M.B., Staudt A.M., et al. Analysis of casualties that underwent airway management before reaching role 2 facilities in the Afghanistan conflict 2008–2014. Mil Med. 2020;185:10–18. doi: 10.1093/milmed/usz383. [DOI] [PubMed] [Google Scholar]
- 75.Benov A., Shkolnik I., Glassberg E., et al. Prehospital trauma experience of the Israel defense forces on the Syrian border 2013–2017. J Trauma Acute Care Surg. 2019;87:S165–S171. doi: 10.1097/TA.0000000000002217. [DOI] [PubMed] [Google Scholar]
- 76.Beit Ner E., Tsur A.M., Nadler R., et al. High success rate of prehospital and en route cricothyroidotomy performed in the Israel Defense Forces: 20 years of experience. Prehosp Disaster Med. 2021;36:713–778. doi: 10.1017/S1049023X21001199. [DOI] [PubMed] [Google Scholar]
- 77.Barnard E.B.G., Ervin A.T., Mabry R.L., et al. Prehospital and en route cricothyrotomy performed in the combat setting: a prospective, multicenter, observational study. J Spec Oper Med. 2014;14:35–39. doi: 10.55460/62V1-UIZC. [DOI] [PubMed] [Google Scholar]
- 78.Adams B.D., Cuniowski P.A., Muck A., et al. Registry of emergency airways arriving at combat hospitals. J Trauma. 2008;64:1548–1554. doi: 10.1097/TA.0b013e3181728c41. [DOI] [PubMed] [Google Scholar]
- 79.Panchal A.R., Bartos J.A., Cabañas J.G., et al. Part 3: Adult basic and advanced life support: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020;142:S366–S468. doi: 10.1161/CIR.0000000000000916. [DOI] [PubMed] [Google Scholar]
- 80.Spittal M.J. Evaluation of pulse oximetry during cardiopulmonary resuscitation. Anaesthesia. 1993;48:701–703. doi: 10.1111/j.1365-2044.1993.tb07185.x. [DOI] [PubMed] [Google Scholar]
- 81.Aldred D., Durham M., Prokop N., et al. Critical care paramedics' experiences of performing an emergency scalpel cricothyroidotomy: a qualitative study. Br Paramed J. 2022;7:3–8. doi: 10.29045/14784726.2022.06.7.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Munn Z., Peters M.D., Stern C., et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:1–7. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Haag A.-K., Tredese A., Bordini M., et al. Emergency front-of-neck access in pediatric anesthesia: A narrative review. Paediatr Anaesth. 2024 doi: 10.1111/pan.14875. Epub ahead of print 11 March 2024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.