Abstract
Background
Only a few cases have been reported about active foreign body implantation in the cavernous body of the penis.
Case presentation
A 47-year-old man inserted two needles from the glans penis into the bilateral penile sponge body. Subsequently, two needles migrated through the penile cavernous body into the pelvic cavity. Attempts to remove the needles through the penis were unsuccessful. Eventually, after a duration exceeding one month, the displaced needles were removed in stages from the buttocks.
Conclusion
A few cases of intracavernosal-injection-therapy-associated needle breakage and retention have been reported globally. And this is the first case in China documenting the migration of foreign bodies within the penile region. In this condition, it is of utmost importance to engage the expertise of experienced andrologists to minimize the risk of excessive manipulation, thereby ensuring that inadvertent deep penetration of the needle into the penile tissue is prevented. In case the foreign body has migrated deeper into the tissues and the patient does not exhibit any specific symptoms or risks of macrovascular injury-related bleeding, close surveillance of its movement can be implemented. Surgical intervention can be initiated once the foreign body has reached a suitable position. Moreover, a psychiatric evaluation should be recommended for patient to discover any underlying mental health disorders.
Keywords: Foreign body, Retained penile needles, Urologic emergency, Case report, Literature review
Résumé
Contexte
Seuls quelques cas ont été rapportés concernant l’implantation active d’un corps étranger dans le corps caverneux du pénis.
Présentation du cas
Un homme de 47 ans a inséré deux aiguilles, par le gland du pénis, dans les corps spongieux du pénis. Par la suite, les deux aiguilles ont migré à travers le corps caverneux du pénis jusque dans la cavité pelvienne. Les tentatives pour retirer les aiguilles à travers le pénis ont été infructueuses. Finalement, après une durée de plus d’un mois, les aiguilles déplacées ont été retirées, par étapes, au niveau des fesses.
Conclusion
Quelques cas de rupture et de rétention d’aiguille associés au traitement par injection intracaverneuse ont été signalés dans le monde. Il s’agit ici du premier cas en Chine qui documente la migration de corps étrangers dans la région du pénis. Dans cette situation, il est de la plus haute importance de faire appel à l’expertise d’andrologues expérimentés pour minimiser le risque de manipulation excessive, garantissant ainsi que la pénétration profonde par inadvertance de l’aiguille dans le tissu pénien est prévenue. Dans le cas où le corps étranger a migré plus profondément dans les tissus et que le patient ne présente pas de symptômes spécifiques ou de risques de saignements liés à une lésion macrovasculaire, une surveillance étroite du mouvement du corps étranger peut être mise en œuvre. L’intervention chirurgicale peut être initiée une fois que le corps étranger a atteint une position appropriée. Enfin, une évaluation psychiatrique devrait être recommandée à la recherche de tout trouble sous-jacent de santé mentale.
Mots-clés: Corps étranger, Rétention d’Aiguilles péniennes, Urgence urologique, Cas clinique, Revue de la Littérature
Introduction
Occasional reports have emerged regarding needle breakage within the penis during intracavernosal injection therapy (ICI) for patients afflicted with erectile dysfunction (ED). Nevertheless, there is a scarcity of documented cases regarding voluntary self-needle insertion into the penis and the ensuing displacement. In July 2023, our hospital encountered a unique case involving the self-insertion of two needles into the bilateral cavernous body.
Case presentation
A 47-year-old married male, with a history of hypospadias and normal erectile function, independently inserted 10 steel balls of varying sizes subcutaneously through small incisions of the foreskin into the coronal sulcus, root of the penis, and the scrotum three months ago. Despite this behavior, the patient denied any previous history of mental disorders. Recently, the patient procured several elongated hollow needles via online sources, typically utilized for ICI, but he denied any usage for injection purposes. The needles had a length of 5 cm and a diameter of 0.5 mm. Approximately 18 h prior to admission, the patient experienced a nocturnal erection and self-inserted two needles along the long axis of the penis into the bilateral penile sponge body from the glans penis. He complained of mild pain during the insertion of the foreign objects, but did not experience any significant pain or discomfort thereafter. Urination remained normal without any presence of blood. However, due to an intolerable level of distress localized at the base of the penis, the patient made the decision to seek medical attention in the emergency room roughly 11 h subsequent to the needle insertion. He underwent a pelvic Computed Tomography (CT) examination, which revealed needle-shaped foreign bodies within the cavernous bodies bilaterally in the penis. In addition, a total of 10 nodular dense shadows were observed within the penis and scrotum (Fig. 1). The patient requested the extraction of the needles, yet declined surgical intervention due to apprehensions regarding potential postoperative ED. Following 7 h of hesitancy and careful consideration, the patient was admitted to the hospital on an emergency basis due to intensifying unbearable pain at the base of the penis and perineum.
Fig. 1.
July 26, 2023, plain CT of the pelvis. The arrows show needles in the cavernous body of the penis on both sides
Physical examination revealed pinhole-like marks on the surface of both sides of the glans, along with the combination of glans cleft and anterior hypospadias, and external urethral opening in the ventral coronal groove (Fig. 2). Numerous bead-like foreign bodies, approximately 5–10 mm in diameter, were perceptible within the subcutaneous tissues of the coronal groove, root of the penis, and scrotum. The needles could not be detected through palpation of the penis.
Fig. 2.

Appearance of the patient’s penis: glans cleft combined with anterior hypospadias, external urethral opening in the ventral coronal sulcus. The metal beads hidden beneath the foreskin are indicated by the arrow
Twenty two h following the incident, the patient underwent surgical exploration in urology department. Intraoperative X-ray guidance was employed to successfully locate the needles in the posterior section of the penile body, with their anterior ends extending beyond the pubic symphysis (Fig. 3). Under general anesthesia, a circular incision was made on the foreskin, 1 cm away from the base of the penile body’s surface. Through dissection of the superficial fascia towards its proximal end, the tunica albuginea of the corpus cavernosum was exposed up to the pubic symphysis. A longitudinal incision was made on the lateral side of the tunica albuginea of the right cavernosum; however, no foreign body was detected within the cavernous tissue of the penis. Following the verification of adequate hemostasis, the incision was meticulously closed in a layered manner. On the second postoperative day, a pelvic CT scan was conducted, revealing significant displacement of the needles into the deep tissues (Figs. 4 and 5). The needles pierced the cavernous body of the penis and reached the pelvic floor, thereby inducing a gradual amelioration of the patient’s distress. Instead of pursuing trans-perineal surgery, close surveillance was selected as the foreign body was primarily situated within the soft tissues of the pelvic floor, distanced from major blood vessels and the rectum. On the fifth day following the surgical procedure, a subsequent pelvic CT scan revealed further migration of the two needles into the sacrococcygeal region (Fig. 6). However, on the seventh postoperative day, the patient began experiencing deteriorating perineal pain and unbearable acupuncture-like sensation in the right buttock when seated. Physical examination revealed an elevation of the cutaneous surface in the right buttock proximal to the gluteal cleft, with noticeable tenderness and a palpable sensation of a foreign body beneath the skin. Therefore, an emergency procedure was performed under local anesthesia. Intraoperative X-ray revealed the presence of one needle within the deep soft tissue of the pelvic floor, while another needle was oriented perpendicular to the body’s surface in the right buttock. With intraoperative X-ray guidance, an incision of 1 cm in length was made on the skin, which was then probed downward for 2 cm, resulting in the complete extraction of a hollow needle with a length of 5 cm and a diameter of 0.5 mm (Fig. 7). Following the surgery, the localized pain symptoms were reduced. Pelvic CT examination on the 12th postoperative day confirmed the stability of the residual needle’s position. The patient was instructed to closely observe it and await an appropriate opportunity for the removal of the foreign body (Fig. 8).
Fig. 3.
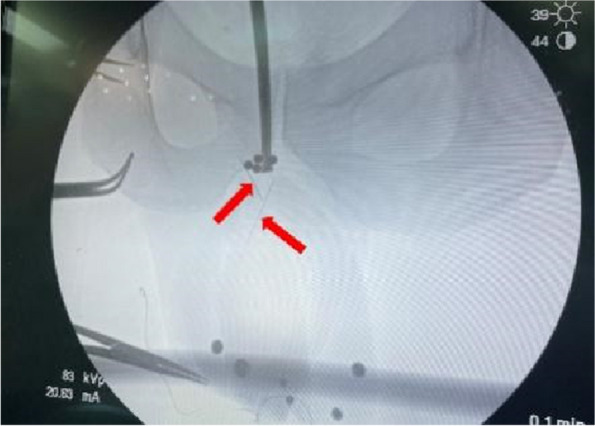
Intraoperative X-ray of the patient’s first surgery on July 26, 2023. The arrows show the needles
Fig. 4.
July 27, 2023, CT of the pelvis. The arrows point to the needles
Fig. 5.
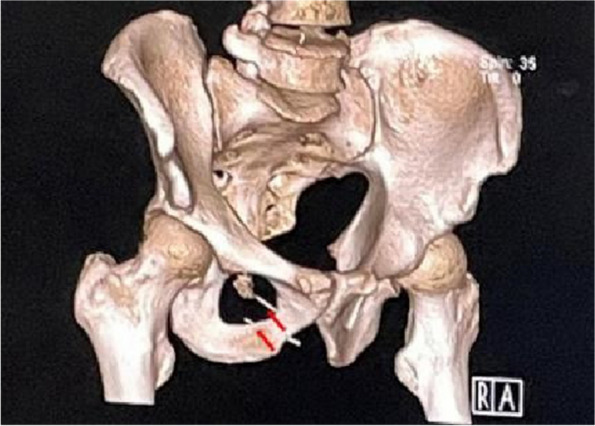
July 27, 2023, a 3D reconstruction of pelvis. The arrows point to the needles
Fig. 6.
July 31, 2023, CT of the pelvis. The arrows point to the needles
Fig. 7.
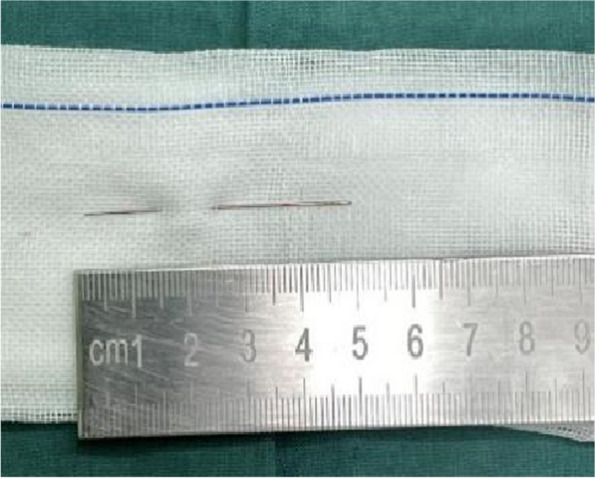
August 2, 2023, a needle extracted from the patient’s right buttock
Fig. 8.
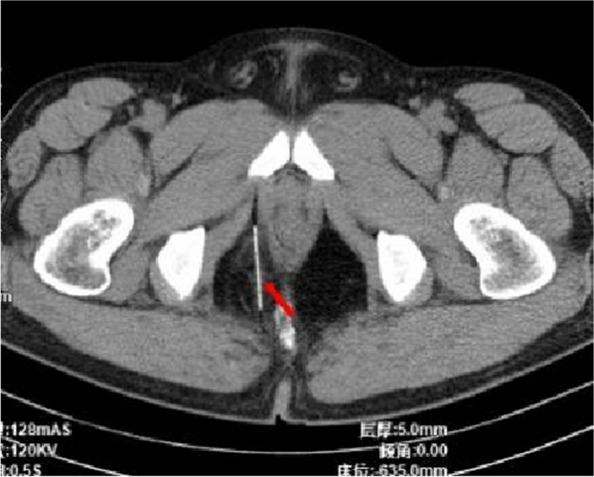
August 7, 2023, CT scan of the pelvis. The arrow points to the residual needle
On the 45th day following surgery, the patient presented with a noticeable bulge and pronounced tenderness in the localized area of the right buttock. Physical examination revealed a localized skin bulge, situated approximately 5 cm above the surgical scar on the right buttock, accompanied by tenderness and a sensation of a foreign object upon palpation (Fig. 9). An emergent local anesthetic examination was conducted. Intraoperative X-ray found that the residual needle was located within the right buttock, perpendicular to the surface of the body, and approximately 1.5 cm away from the skin. Subsequently, the needle was completely extracted through a local incision (Fig. 10) and the patient experienced a complete resolution of pain the day after the procedure. During the follow-up, the patient noted a slight decrease in the length and rigidity of the penis during erections compared to the preoperative state.
Fig. 9.

The departure positions of the two foreign bodies are indicated by the arrows. The thick arrow represents the first exit position and the thin arrow represents the second exit position. Both needles were removed from the right buttock
Fig. 10.

August 30, 2023, the second needle extracted from the patient’s right buttock
Literature review
We searched the PubMed and Embase databases for similar cases and compared the findings across all the cases. 15 articles were finally included and 17 cases were extracted. All included cases were self-insertion of needle-like foreign bodies into the cavernous body of the penis (see Table 1).
Table 1.
Comprehensive comparison among all reported cases of retained penile needles
| first author | No. of patients | age | cause | Palpable needle on PE | Interval of needle retrieval | Imaging modality | needle location | Remove location | Local vs. general anesthesia |
|---|---|---|---|---|---|---|---|---|---|
| this case | 1 | 47 | Self implantation | NO | 22 h | CT | pelvic cavity | pygal | General anesthesia |
| Mark (1991) [1] | 1 | 67 | ICI | YES | Immediate | X-ray | NA | Local area of the penis | Local anesthesia |
| Beer (1992) [2] | 1 | 61 | ICI | NO | 2 d | X-ray. Ultrasound failed to localize the needle | Intracorporal. At the base of the left corpus cavernosum | Local area of the penis | Local anesthesia (penile block) |
| Nazli (1993) [3] | 1 | 58 | ICI | YES | Immediate | X-ray | Intracorporal. Left corpus cavernosum | Local area of the penis | Local anesthesia |
| Greenstein(1997) [4] | 2 case 1 | 69 | ICI | NO | 6 wk | X-ray to confirm needle presence on initial presentation | NA | Local area of the penis | Needle was palpable at time of retrieval. No anesthesia used at all. |
| case 2 | 81 | ICI | NO | 4 d | X-ray to confirm needle presence on initial presentation | NA | Local area of the penis | Needle was palpable at time of retrieval. No anesthesia used at all. | |
| Iacono (1998) [5] | 1 | 50 | ICI | NO | Immediate | Ultrasound | Intracorporal. Distal third of the right corpus cavernosum | Local area of the penis | No anesthesia used at all |
| Bandi (2005) [6] | 1 | 44 | ICI | N0 | 2 wk, nonoperative management | X-ray | NA | Local area of the penis | No |
| Shamloul(2005) [7] | 1 | 32 | ICI | N0 | Immediate | X-ray | Intracorporal. Midshaft of left corpus cavernosum | Local area of the penis | Local anesthesia (penile block) |
| Hsiao (2013) [8] | 1 | 42 | ICI | No, only superficial palpation performed due to fear of needle stick | Immediate | X-ray | Intracorporal. Midshaft of right corpus cavernosum | Local area of the penis | General anesthesia |
| Banerji(2016) [9] | 1 | 62 | ICI | YES | Immediate | X-ray | Under Buck’s fascia (right midshaft) | Local area of the penis | General anesthesia |
| Wren (2018) [10] | 1 | 55 | ICI | NO | 3 d | X-ray | Intracorporal. Left corpus cavernosum | Local area of the penis | General anesthesia, penile degloving |
| Pan (2019) [11] | 1 | 51 | ICI | NO | Several months | Ultrasound and CT scan | Under Dartos fascia (right side of penile base) | Local area of the penis | General anesthesia |
| Collaço(2020) [12] | 1 | 54 | ICI | NO | Immediate | X-ray and ultrasound | Intracorporal. Left corpus cavernosum | Local area of the penis | General anesthesia |
| Lazaraviciute(2021) [13] | 1 | 82 | ICI | NO | 1 d | X-ray and ultrasound | Intracorporal. Left corpus cavernosum | Local area of the penis | General anesthesia |
| Mai (2021) [14] | 1 | 64 | ICI | YES | Immediate | X-ray and ultrasound | Under Dartos fascia (left midshaft) | Local area of the penis | General anesthesia |
| Kirolos(2023) [15] | 1 | 70 | ICI | NO | 2 d | Ultrasound | Intracorporal. Midshaft of right corpus cavernosum | Local area of the penis | General anesthesia |
ICI intracavernosal injection therapy
Discussion
Penile foreign bodies, such as those in the foreskin, are relatively common [16]. A small number of individuals usually surgically implant beads of various materials and shapes beneath the foreskin through a dorsal foreskin incision, as elucidated in existing literature [16]. One optional remedy for ED is ICI. Since 1982, some ED sufferers have been consistently self-administering injections of medications, such as botulinum toxin, directly into the corpus cavernosum as a means of treatment. However, this self-injection method poses significant challenges, and the use of ICI in China remains relatively limited due to the requirement for specialized expertise and associated discomfort [17]. Through the literature review, there have been 16 reported cases of self-insertion of needle-like foreign bodies into the cavernous body of the penis. And they were all ICI-associated needle breakage and retention abroad, with the needle being inserted into the penile body rather than the glans at the time of injection. And the longer the delay, the easier it is for the needle to move its position. Finally, the needles all be removed through a local incision in the penis. As of yet, no similar case has been reported in China [15]. In particular, this case encompasses the simultaneous presence of two uncommon clinical conditions: foreign bodies within the penile cavernous body, and the coexistence of glans cleft and hypospadias in the patient.
Ultrasound, X-ray, and CT are viable diagnostic options for the detection and localization of foreign bodies within the penile cavernous body. 3D reconstruction of CT proves highly beneficial in precisely locating deeply embedded foreign tissues, enabling surgeons to devise effective surgical plans aimed at protecting the cavernous body tissues and minimizing the risk of postoperative ED [18].
Specifically, in cases involving parenchymal organs, the retention and removal of needle-like foreign entities can be very challenging and present surgeons with “needle in a haystack” situation. Preoperative 3D reconstruction of CT and intraoperative X-ray can be instrumental in precisely locating the needles. The unpredictable displacement trajectory of the foreign body represents the primary challenge. In this case, the complete removal of the needles from the patient required over a month as they migrated proximally within the cavernous body before penetrating the subcutaneous tissue of the sacrococcygeal region. It is thought that variations in intra-abdominal pressure, penile tissue deformation, hemodynamics, and muscular activity collectively contribute to the movement of the needles. In case the foreign body has migrated deeper into the tissues as a result of muscle movement, and the patient does not exhibit any specific symptoms or risks of macrovascular injury-related bleeding, close surveillance of its movement can be implemented. Surgical intervention should only be initiated once the foreign body has reached a suitable position to prevent excessive tissue damage and functional impairment. The second difficulty pertains to the challenge of the control of hemorrhage and the prevention of substantial harm to erectile tissue during the incision of the penile cavernosa for needle extraction. The third dilemma is related to the spongy tissue structure of penis, which may reduce the surgeon’s tactile feedback and increase the likelihood of missing thin needles even with intraoperative fluoroscopic guidance. Therefore, to prevent excessive manipulation that could potentially push the needle further into deeper penile tissues and consequently complicate its retrieval, it is recommended that emergency departments seek assistance from experienced andrologists first in cases of intracorporeal needle break in the penile cavernous body [15].
When the anatomical structure of the penis is normal, inserting a needle from the glans to the corpus cavernosum can result in excruciating agony. The patient in this case presented with a penile deformity and experienced only mild discomfort during needle insertion. It remains unclear whether the presence of this deformity is correlates with decreased penile nociception [18]. It is known that individuals with mental health issues may occasionally engage in deviant sexual activity, such as inserting foreign objects into the urethra [19]. The reasons for the insertion of foreign bodies into the genitourinary tract could be sexual gratification, psychiatric, accidental, curiosity, especially among children, or therapeutic [20]. The individual involved in this case, despite engaging in a behavior that may appear peculiar to the majority, is obviously a normal, mature member of society, without any known psychiatric abnormalities. However, it is only speculative at present regarding the psychological issues underlying the patient’s abnormal behavior, as the patient refused any discussions pertaining to this matter. Nevertheless, when dealing with such unconventional circumstances, it is essential for clinicians to be mindful of the potential psychological issues that the patient may be experiencing. Communication approaches should be carefully considered when interacting with the patient and their family. Additionally, it is suggested that a psychiatric evaluation should be recommended to discover any underlying mental health disorders, thus reducing the risk of recurrence [21] .
Conclusion
This article presents a unique case involving the self-insertion of needles into the cavernous body of the penis, which were eventually removed in a staged procedure from the buttocks. To our knowledge, this is the first case of migrating foreign bodies within penis in China. In such cases, it is of utmost importance to engage experienced andrologists to prevent excessive manipulation and further needle penetration into the penile tissue. In case the foreign body has migrated deeper into the tissues and the patient does not exhibit any specific symptoms or risks of macrovascular injury-related bleeding, close surveillance of its movement can be implemented. Surgical intervention can be initiated once the foreign body has reached a suitable position to prevent excessive tissue damage and functional impairment. Moreover, a psychiatric evaluation should be recommended for patient to discover any underlying mental health disorders.
Acknowledgements
We sincerely thank Professor Bo Yang for performing the surgery.
Abbreviations
- CT
Computed Tomography
- ED
Erectile dysfunction
- ICI
Intracavernosal injection therapy
Authors’ contributions
Bo Yang, Yue Zhang and Ying Ke created and presented the published work; Yue Zhang and Ying Ke from the original research group created and presented the published work; Aixin Qiu participated to the revisions; Lijie Wen and Xiaolong Xv provided study materials; Bo Yang performed the surgery; Yue Zhang and Xiaoyun Liu took charge of coordination and management.
Funding
This study was supported by the “1 + X” program for Cross-disciplinary Innovation Projects of the Second Hospital of Dalian Medical University (2022JCXKZD05), In-Hospital Training Fund of the Second Hospital of Dalian Medical University (dy2yynpy202220), Liaoning Provincial Department of Education 2021 Scientific Research Funding Project (LJKZ0873), the Second Hospital of Dalian Medical University - Dalian Institute of Chemical Physics, Chinese Academy of Sciences “Collaborative Innovation Centre for Individualized Diagnosis and Treatment” Jointly Funded Project(UF-ZD-202014).
Availability of data and materials
No dataset was generated or analyzed during this study.
Declarations
Ethics approval and consent to participate
This study was awarded the Ethics Committee of the Second Affiliated Hospital of Dalian Medical University.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Competing interests
All the authors have no potential conflicts of interest to disclose.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Bo Yang and Ying Ke contribute equally to this work.
Contributor Information
Xiaoyun Liu, Email: 15940988776@163.com.
Yue Zhang, Email: zhangyueliaoning@163.com.
References
- 1.Mark SD, Gray JM. Iatrogenic penile foreign body. Br J Urol. 1991;67(5):555–556. doi: 10.1111/j.1464-410X.1991.tb15211.x. [DOI] [PubMed] [Google Scholar]
- 2.Beer SJ, See WA. Intracorporeal needle breakage: an unusual complication of papaverine injection therapy for impotence. J Urol. 1992;147(1):148–150. doi: 10.1016/S0022-5347(17)37167-7. [DOI] [PubMed] [Google Scholar]
- 3.Nazli O, Ateşci YZ, Girgin C, Günaydin G, Erhan O. An unusual complication of intracavernous self-injection of papaverine. Br J Urol. 1993;72(1):126–127. doi: 10.1111/j.1464-410X.1993.tb06481.x. [DOI] [PubMed] [Google Scholar]
- 4.Greenstein A, Sofer M, Chen J. Delayed retrieval of fragment after needle breakage during intracavernous self-injection. J Urol. 1997;157(3):953. doi: 10.1016/S0022-5347(01)65097-3. [DOI] [PubMed] [Google Scholar]
- 5.Iacono F, Barra S. Intracorporeal needle breakage as an unusual complication of intracavernous self-injection. Tech Urol. 1998;4(1):54–55. [PubMed] [Google Scholar]
- 6.Bandi G, Rajpurkar A, MacDonald MF, Dhabuwala CB. Multiple retained needles: an unusual complication of intracavernous self-injection[J/OL] Urology. 2005;65(4):797. doi: 10.1016/j.urology.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 7.Shamloul R, Kamel I. Case report: a broken intracavernous needle: successful ultrasound-guided removal. J Sex Med. 2005;2(1):147–148. doi: 10.1111/j.1743-6109.2005.20115.x. [DOI] [PubMed] [Google Scholar]
- 8.Hsiao W, Lian F, Goodgame B, Ritenour CW, Angell J, Master VA. Breakage of needle during intracavernosal injection and use of portable ultrasound guidance for removal. Case Rep Urol. 2013;2013:1–3. doi: 10.1155/2013/215492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Banerji JS, Govier FE. A “needling” complication. Urology. 2016;97:e5. doi: 10.1016/j.urology.2016.06.040. [DOI] [PubMed] [Google Scholar]
- 10.Wren J, Huang IS, Gillis V, Rizo-Palomera R, Brannigan R, Bennett N. A rare complication; retained needle during intracavernosal injection for erectile dysfunction[J/OL] Urol Case Rep. 2018;20:51–53. doi: 10.1016/j.eucr.2018.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pan S, D’Amico MJ, Munarriz R. Surgical management of retained needle in a transgender woman’s phallus. Can J Urol. 2019;26(4):9867–9870. [PubMed] [Google Scholar]
- 12.Collao BG, Cavalcante MDS, Miranda EP, Scafuri AG. Intracorporeal needle breakage during intracavernous injection therapy: a case report. SNCCM. 2020;2(10):1938–1940. doi: 10.1007/s42399-020-00472-0. [DOI] [Google Scholar]
- 13.Lazaraviciute G, Mckay AC, Massanova M, Hendry DS, Zreik A. Removal of retained intracavernous needle tip using intraoperative fluoroscopy. J Clin Urol. 2021;14(6):422–424. doi: 10.1177/2051415820961724. [DOI] [Google Scholar]
- 14.Mai Y, Kannady C, Wang R. Using portable ultrasound guidance and direct incision as reliable technique for retrieval of retained hypodermic needle: a rare complication of intracavernosal injection. J Sex Med. 2021;18(3):S43. doi: 10.1016/j.jsxm.2021.01.051. [DOI] [Google Scholar]
- 15.Meilika KN, Eid JF. Retained needles during intracavernosal self-injection for erectile dysfunction treatment: a case report and systematic literature review. Sex Med. 2023;11(2):qfad008. doi: 10.1093/sexmed/qfad008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kirkham CL, Monks SM, Crawford SB. Complications of subcutaneous penile modifications: a discussion of emergency department presentations and management. Int J Emerg Med. 2019;12(1):22. doi: 10.1186/s12245-019-0241-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abou Zahr R, Bou Kheir G, Mjaess G, Jabbour T, Chalhoub K, Diamand R, et al. Intra-cavernosal injection of botulinum toxin in the treatment of erectile dysfunction: a systematic review and meta-analysis. Urology. 2022;170:5–13. doi: 10.1016/j.urology.2022.08.039. [DOI] [PubMed] [Google Scholar]
- 18.Matsuzaka J, Aoki H, Banya Y, Fujioka T, Kubo T, Nagane Y. A foreign body of the corpus cavernosum in a patient with cleft glans penis: a case report. Hinyokika Kiyo. 1994;40(6):545–547. [PubMed] [Google Scholar]
- 19.Crawford SB, Lowry D, Watts SH. Evaluation and management of urethral foreign bodies and description of a novel ultrasound-guided catheter‐based extraction technique. J Am Coll Emerg Phys Open. 2021;2(2):e12398. doi: 10.1002/emp2.12398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Untan İ, Sabur V. Esferas magnéticas de neodimio agrupadas calcificadas como un cuerpo extraño intravesical: reporte de un caso y revisión de la literatura. Cir Cir. 2023:8905. 10.24875/CIRU.22000275. [DOI] [PubMed]
- 21.Untan I, Ersekerci E. A Sewing needle as a urethral foreign body: a case report and literature review[J/OL] Niger J Clin Pract. 2023;26(10):1588–1590. doi: 10.4103/njcp.njcp_168_23. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No dataset was generated or analyzed during this study.





