Abstract
While exteroceptive sensory processing is a hallmark of autism spectrum disorder, how interoceptive processing may impact and contribute to symptomatology remains unclear. In this comprehensive narrative review on interoception in autism, we discuss: 1) difficulties with assessing interoception; 2) potential interoceptive differences; 3) interactions between neural systems for interoception, attention, sensorimotor processing, and cognition; and 4) potential differences in neural circuits involved in interoception. In general, there are mixed findings on potential interoception differences in autism. Nevertheless, some data indicate differences in integration of interoceptive and exteroceptive information may contribute to autism symptomatology. Neurologically, interoceptive processing in autism may be impacted by potential differences in the development, morphometry, and connectivity of key interoceptive hubs (vagal processing, brainstem, thalamus, insula), though much work is needed on this topic.
Keywords: autism, interoception, insula, brainstem, thalamus, thermosensation
Introduction
Interoception refers to the sensation of internal bodily sensations and processes, such as the heartbeat, respiration, gut sensations, and blood vessel activity.1–6 Internal body stimuli classically consisted of input from the internal organs (eg, heart and gut); however, more recently, some definitions also include skin-mediated interoception, such as thermosensation (perception of temperature, affective touch, and pain).7–9 Further, interoception is processed not only from afferent input, but may also involve feedback and feedforward loops from the brain to the internal organs.10–12
Interoception may also contribute to the genesis of one’s emotional states,2,13,14 which, in turn, give rise to feelings – the conscious experience of emotions.15 Interoception is essential for feelings of malaise and maintaining homeostasis of the body. In addition, interoception is thought to contribute to consciousness,1 action understanding and imitation in early infancy,16 decision making,17,18 sense of agency,19 spatial perspective-taking,20 and social judgment.21 For example, our initial impressions of others tend to be influenced by visceral states, such as cardiac afferent signals.22,23 Thus, interoception interacts with many other processes, including exteroception, cognition, and motor, social, and emotional processing.24,25
While exteroceptive sensory processing differences such as visual and auditory hypo- or hyper-sensitivities are part of the diagnostic criteria for autism in the DSM 5,26 how interoceptive processing is related to autism symptomatology remains to be determined. However, recently, difficulties with interoception have been hypothesized to be related to, or even underlie, some symptomatology in autism,27–34 but the presence of interoception differences in autism remains unresolved, due to mixed findings in prior studies.35 Discrepancies may stem from measurement issues, lack of statistical power, and variability in studied populations. In addition, high co-occurrence of mental and physical health conditions in autism, such as anxiety and gastrointestinal issues, could alter interoceptive functioning and may act as confounding variables in studies of interoception.36–38
Here, we aim to provide a neurobiological perspective to help better understand the potential association between interoceptive processing and aspects of some autism symptomatology. To better explore these associations, we first present a review of the literature related to interoception and autism. Second, we outline neurobiological models of the interoceptive nervous system2,3,6,13,39 and discuss their application to autism.
Potential Interoception Difficulties in Autism: Measurement Issues
To date, there is an inconsistency of evidence for a general interoceptive difference in autism.35,40,41 Some studies identify various interoceptive challenges faced by autistic individuals, including difficulties with awareness of hunger, thirst, heartbeat detection, pain, and affective touch.29,30,36,42–46 Other studies indicate interoceptive difficulties in autistic children but not in adults,47 while other studies do not find any differences.48–50
Discrepancies between studies may stem from issues with how interoception is measured. There are currently several ways to assess interoceptive ability, including: behavioral accuracy (the correspondence between objectively measured physiological events and an individual’s reported self measurement, i.e., heart rate); interoceptive attention (purposefully attending to interoceptive signals when instructed), interoceptive sensibility (i.e., metacognitive self-reflections and self-report measures), and attribution of a cause of interoceptive changes within the self, such as perceived threat.45,51 However, all of these methods draw attention to one’s bodily states, which can change the amplitude of interoceptive signals, thereby potentially augmenting or diminishing neural activation to interoceptive signals.51
While self-report tools are commonly used to assess interoceptive sensibility or perceived accuracy,52 their effectiveness in gathering accurate information from autistic individuals presents unique difficulties.53 Previous studies have reported challenges with self-evaluation in autism, as autistic individuals may have limited insight into their anxious thoughts and feelings, leading to difficulties in accurately identifying and reporting internalizing symptoms.49,54,55 Additionally, it may be that, similar to exteroception, autistic individuals may have hyper- or hypo-interoceptive reactivity, or combined patterns, making it difficult to interpret a mean score.45,46 Thus, when assessing interoceptive accuracy, it has been suggested to incorporate multiple measures.35,56
Moreover, in autism, there is an increased co-occurrence of alexithymia, a subclinical condition characterized by challenges in recognizing, interpreting, and describing one’s emotions (see Kinnaird et al, for a review).57 Reduced interoceptive accuracy may contribute to alexithymia in autistic individuals that could overestimate or underestimate the bodily sensations, which could further contribute to difficulties in recognizing and expressing their own emotions.48,58,59 Additionally, alexithymia is significantly associated with difficulties in processing and associating bodily sensations with emotions, leading to a disparity between objective and subjective experiences of bodily sensations.49 Additional research is needed to better understand the relationship between interoception and alexithymia in autism.
To summarize, there is a great deal of inconsistency in data exploring potential interoception difficulties in autism. Measurement issues and sample differences (i.e., age range, intelligence, sex, and co-occurring conditions) are perhaps the largest source of these discrepancies. Thus, studies with stratification by age and validated tools with multiple measures are needed.35,60 Also, Crucianelli et al8 suggest that interoception at perceptual levels should be investigated as a set of independent processes rather than a single construct. Specifically, they suggest that the capacity to perceive different kinds of interoceptive signals (eg, cardiac, thermosensory, nociceptive) may vary within an individual and thus distinct interoceptive submodalities may need to be probed separately.
Models of the Interoceptive System
As behavioral measurement is an issue in understanding potential differences in interoception in autism, neural differences related to the interoceptive system may be another avenue to explore for better understanding. Here, we first describe different models of the interoceptive system.
The interoceptive system is a network of neural structures that includes viscerosensory, autonomic, peripheral, and central components that continuously monitor and regulate the body’s visceral internal state.2,61,62 The unique anatomical structures and physiology of the interoceptive system are believed to play a critical role in the generation of feelings, the conscious mental events that represent the body’s states as it undergoes homeostatic regulation.15 Feelings can be spontaneously internally generated as a result of interoceptive regulation processes, which are called homeostatic feelings (i.e., hunger, thirst and pain, well-being, malaise, desire). Alternatively, emotional feelings may be largely prompted by external conditions (i.e., fear, anger, disgust, or joy).1 Therefore, interoception is a key factor in determining the nature and content of feelings, regardless of whether they arise from internal or external sources.
Changes in the body’s state trigger both automatic physiological reactions and mental experiences.2,6 These processes may occur via action programs or physiological mechanisms that are largely instinctual and stereotypical, primarily without the need for conscious experience.6 Specifically, when we experience homeostatic feelings like thirst, hunger, or pain, our body prompts us to engage in behaviors that address those needs. Further, the addition of conscious feelings increases behavioral flexibility and facilitates learning by allowing the organism to associate specific circumstances with changes in body states, and this knowledge can be applied to adapt to future situations.2,15
One model of interoception proposes an integration of aspects of somatosensory perception (pressure, temperature, and pain) and visceral information.5,9 For example, some exteroceptive signals, such as affective touch, can be mapped also by interoceptive structures, specifically by unmyelinated C-fibers in cutaneous skin.2 This suggests that the perception of affective touch and the processing of internal bodily sensations are interconnected, blurring the distinction between interoceptive and the exteroceptive senses.2 Additionally, proprioception and vestibular sensation may also contribute to interoception processes.6
Recently, some have proposed that interoception should also include regulating signals from the brain.10–12 This model of interoception has been integrated with prediction coding (Embodied Predictive Interoceptive Coding [EPIC]).39,63–65 From a Bayesian perspective that inferences and predictions of interoceptive processes regulate body states, the EPIC model posits that the brain forms a prediction-sensation loop that minimizes exteroception/interoceptive unexpectedness, contributing to homeostasis.63,65,66 The prediction-sensation loop can be divided into three parts: (1) interoceptive and exteroceptive information (from internal organs, and external sensory organs); (2) body regulation – the process of executing actions that affect the internal state of the body (eg, hormone release, motor commands, adjusting feedback loops); and (3) the prediction of the future consequences of bodily actions, known as forecasting.63 This regulative system is based on processing of current interoception and exteroception signals and comparing them to past experiences.65 The predictions are then tested against incoming sensory and interoceptive signals, and the brain adjusts its predictions accordingly (prediction error). However, whether these interoceptive predictions occur and, if so, how they function remain debated. Some of the empirical research on predictive processing models has focused on algorithmic theories, and still needs more work to evaluate the adequacy and explanatory power of these algorithms.67
It should be noted that predictive processing models were first suggested for motor and exteroceptive processes (eg, “Forward Model”;68 “Free Energy Principle”69,70). In particular, a large focus for these predictive models and experimental validation has been based on the visual system where it is thought that there is a predominant top-down prediction of visual processing,71 or, for example, at the cognitive level, for actively predicting the actions and intentions of others.72 We note that the interoceptive system, however, may be widely different from the visual and motor system in many aspects, including the mode of signal transmission, blood–brain barrier, and neurotransmitters/neuromodulators.2 For example, interoceptive neurons tend to be slow and unmyelinated, as opposed to the exteroceptive and motor system’s highly myelinated fast neurons.2 Additionally, interoception is associated with neurotransmitters such as monoamines (ie, dopamine, noradrenaline, serotonin), acetylcholine, and neuropeptides, many of which are involved in emotional regulation, attention, learning, and autonomic functions. By contrast, exteroception, movement, and cognition are associated with neurotransmitters such as glutamate and GABA, excitatory and inhibitory neurotransmitters. These neurobiological differences indicate that it may be difficult to transfer models of predictive modeling designed for the exteroceptive/motor systems to the interoceptive system.
Nevertheless, it is widely accepted that the interoceptive system orchestrates automatic responses through efferent signals, ensuring that the body can adapt and respond appropriately to maintain its well-being.2,25 Thus, Chen et al11 posit that it is necessary to include body regulation as a component of the interoceptive system, recognizing the interconnectedness of regulatory signals.10 Still, in the literature, some have considered interoception and body regulation as separate concepts,11 and further work is needed. In summary, there is a debate on what stimuli constitute interoceptive responses, how interoception and exteroception may interact neuronally, whether predictive models may exist for interoception as they do for exteroception, and how regulatory systems may be integrated into interoceptive systems.
Interoceptive Processing and Autism
There are several theories of how interoceptive processing may be different in autism. First, scholars have suggested that individuals with autism have a reduced ability to integrate interoceptive stimuli. Specifically, Hatfield et al73 apply the interoceptive system to the weak central coherence theory (difficulty seeing the whole picture and focusing instead on individual elements of a stimulus).74 They posit that the physiological state of thirst, for example, can only be inferred by integrating several distinct interoceptive sensations, such as dry mouth, increased heart rate, and a feeling of discomfort that are combined to form a coherent understanding of thirst. They propose that autistic individuals have a weakened global interoceptive integration, leading to difficulties in recognizing and addressing their thirst, suggesting they may have a heightened awareness of internal signals but difficulties interpreting and integrating them. However, this hypothesis has not been tested with empirical research yet.
Further, autistic individuals may have difficulties in accurately perceiving the timing of sensory signals.33 These temporal-binding windows are more prominent when the pairings of stimuli involve both external and internal sensory information, suggesting a lack of temporal acuity and disrupted integration of exteroceptive and interoceptive signaling.33 Additionally, autistic individuals might show a stronger focus on their own exteroceptive and interoceptive sensations with less habituation.75,76 Such differences may cascade downstream as social processing differences,28 and may be compounded by disrupted behavioral regulation (eating and sleeping patterns).27 Thus, there is some evidence for poor integration of exteroceptive and interoceptive signals in autism.33
In line with the latter idea, Proff et al28 proposed a unified theoretical framework of differences in autistic perception, which integrates interoceptive and exteroceptive domains, such as visceral, visual, and tactile. They propose that divergent patterns of sensory processing in autism can be explained by difficulties in integrating and interpreting these various exteroceptive and interoceptive sensory information. Utilizing a bottom-up and a top-down predictive model, they suggest that weak neural synchronization and an atypical perceptual inference of interoceptive and exteroceptive signals may give rise to difficulties in both interpreting bodily needs and alexithymia. This could lead to an overestimation or underestimation of the bodily sensations, which could further contribute to difficulties in recognizing and expressing their emotions. The authors suggested that in autism, there is an increased focus on sensory error signals in both exteroceptive and interoceptive domains, which may be inferred as an increased influence of error signals when generating predictions based on sensory input.28,77 However, as previously discussed, predictive models remain untested and debated for the interoception (and also debated for exteroception in autism; see Sapey-Triomphe et al;78 Cannon et al;79 Finnemann et al;80 Ward et al81). Thus, this unified theoretical framework remains empirically untested.
As mentioned earlier, recent definitions of interoception include skin-mediated stimuli, such as pain and affective touch.7,8 Atypical pain perception, expression, and difficulties in pain assessment have been previously described in autistic people.44,76,82–85 These may manifest as allodynia (extreme sensitivity to normal non-painful tactile stimulation that causes intense pain), paradoxical heat sensation (where gentle cooling is perceived as hot or burning), or abnormal sensitivity to pain (altered pain responses or lower thresholds to thermal or pain stimuli).84,86 One biological theory of these discrepancies suggests that autistic people experience most stages of pain processing differently (pain perception, transmission, expression, modulation, and/or suppression),42,76,83 and these differences may relate to unmyelinated small fiber density87 and attenuated thalamocortical signaling. Such pain processing differences may significantly affect their perception of and responses to somatosensory stimuli, such as hypoesthesia (reduced sensitivity to touch).44 In autism, pain processing differences have been found for pain processing, pain coping, and attenuation of pain.76,83,85 Attenuation of pain, in particular, is an important element of the interoceptive-visceromotor loop, an aberrance on this loop could lead to downstream attentional, social and behavioral symptomatology.42,88 Thus to summarize, there is evidence for pain processing differences in autism, and such differences may have cascading effects, though further work is needed.
Interoceptive Neural Processing
Here, we first discuss specific neural pathways for interoception, and then describe potential differences in these pathways in autism. The interoceptive system has poorly myelinated fibers which can lead to slower nerve transmission and localized gaps in the blood–brain barrier. These allow for ephaptic transmission, synchronization of membrane potential across neurons, detection of subthreshold potentials, chemosensation along the axonal trunk, and direct exposure to metabolites and blood-borne proteins (for more on this topic, see Damasio & Carvalho;6 Carvalho & Damasio2).
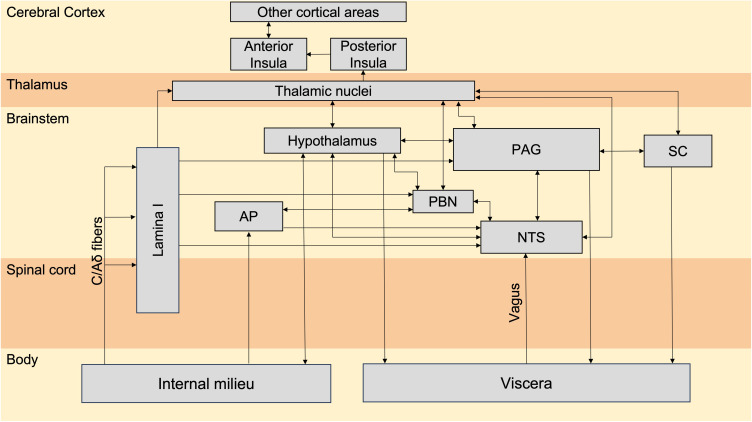
The neural networks involved in interoception are summarized in Figure 1. Much of interoceptive processing, including first-order integrated maps of interoceptive signals from the entire body, is completed at the level of the brainstem.6 Indeed, lesion studies show that interoceptive perception is intact even without the insula, further indicating that interoception may be largely processed in non-cortical neural regions.6
Figure 1.
Interoceptive pathways, adapted from Damasio & Carvalho (2013),6 involve two main routes that run alongside for conveying information from the body’s internal environment to the central nervous system; lamina I and vagus.
Note: Adapted from Damasio A, Carvalho GB. The nature of feelings: evolutionary and neurobiological origins. Nat Rev Neurosci. 2013;14(2):143–152, Springer Nature.6
Abbreviations: PAG, periaqueductal grey; SC, superior colliculus; AP, area postrema; PBN, parabrachial nucleus; NTS, nucleus tractus solitarius.
Bottom-up interoceptive signals, important for sensing homeostatic change, primarily originate from internal organs, such as from the bladder for detecting bladder stretch and coordinating urination.2 The first pathway consists of C and Aδ fibers that carry information related to various body states, and these afferents converge in the spinal cord and the trigeminal nucleus. The vagus nerve and the spinothalamocortical pathway then transmit the interoceptive information to the central nervous system. Viscerosensory inputs are carried to brainstem structures, including the nucleus tractus solitarius, parabrachial nucleus, and periaqueductal gray (PAG).61 The upper brainstem plays a crucial role in assembling and integrating this interoceptive afferent information.
Also, in the brainstem, the deep layers of the superior colliculus receive inputs from different sensory modalities, including visual, auditory, and somatosensory information. This unique arrangement suggests that both exteroceptive and interoceptive information converge in the superior colliculus to form an integrated sensory map of internal and external afferent information.6,89 Inputs to the PAG are linked to motivated behaviors (i.e., appetitive and aversive control) and gating autonomic visceromotor activity (i.e., escape behavior).90,91 Further processing is sent from the brainstem to the thalamus and the insular cortex, which we discuss next.
Thalamus
The intralaminar nuclei of the thalamus, which are immediately rostral to the brainstem, play a role in orienting and attention while the midline nuclei of the thalamus are responsible for arousal and visceral sensation.92,93 Specifically, thalamic nuclei and subthalamic nucleus modulate cardiorespiratory activity.94 In addition, pain and temperature information is transmitted from lamina I from the C and Aδ fibers directly to the thalamus without a synapse in the brainstem.6 It has been suggested that this direct pathway from lamina I to the thalamus (and then to the anterior cingulate cortex [ACC]) may play a role in mediating the emotional experience of pain.92 The thalamus is also involved in nociceptive discrimination. It is responsible for distinguishing ascending signals evoked by both innocuous or noxious heat. In tandem with the PAG and the amygdala, the thalamus triggers a descending inhibitory pathway that reduces pain (see You et al, for a review).95 Additionally, the combination of excitatory and inhibitory thalamocortical interactions can dynamically shape large-scale cortical dynamics, which are important for regulating arousal levels in the brain. For example, during sleep there is an increased connectivity between the thalamus and sensorimotor networks.96
Insula
The insula is a major cortical hub for finer-grain late interoceptive processing such as the integration of interoception, feelings, and cognition, for top-down cognitive control.62 Specific to interoception, the insula is involved in developing controlled action plans6 in response to interoceptive stimuli (eg, the experience of cardiac pain leads one to call the doctor). Thus, the insula has a modulatory role in the processing and experience of the body state and integrating interoception with feelings and other cognitive processes.
The insula receives multiple sensory (exteroceptive and interoceptive) information about the body’s internal state, such as visceral, pain, temperature, vestibular, gustatory and somatosensory (related to touch and pressure) information. The posterior insula is mainly responsible for processing the perception of visceral/bodily signals while the anterior insula may integrate bodily sensations with subjective feelings and awareness.97,98 The anterior insula cortex and the ACC have Von Economo neurons (VENs) which are unique cells found only in these areas. It is hypothesized that their function is to relay information from the insula and ACC to frontal and temporal regions and are related to the ability to make adaptive responses to changing environmental conditions.99
The left anterior insula commonly shows convergent coactivation patterns with the dorsal ACC and bilateral thalamus, together constituting the mid-cingulo-insular “salience network”.12,100–102 The anterior insula also strongly interacts with other functional brain networks including the medial frontoparietal “default mode network” and lateral frontoparietal “central executive network”.101 These findings suggest that the large-scale connectivity of the insular cortex plays a critical role in integrating internal and external multisensory stimuli in the service of initiating higher-order control functions, acting as a gatekeeper to other brain regions and networks.101
Efferent Pathways
Regulatory top-down signals of interoception may be transmitted through both non-neural and neural pathways. Non-neural pathways include the blood and lymphatic system. Neural pathways can be either spinal (sympathetic) or vagal (parasympathetic) efferents. The sympathetic chain ganglia are specifically involved in the body’s fight-or-flight response, preparing the body to respond to stress or danger, and may be considered part of the top-down pathway for the interoceptive system. Vagal efferents, also known as parasympathetic efferents of the autonomic nervous system, travel through the nodose or jugular ganglia bundles, helping to regulate interoceptive signals and organ functions (e.g., regulating rest and digestion).11,12 Further, subcortical brain regions including the amygdala, nucleus accumbens, ventral striatum, and ventral pallidum are involved in generating homeostatic actions, such as valence modulation and the triggering of motor behaviors.6,61
Neural Characteristic of Autism: Implications on Interoception
There have been limited studies on potential differences in the interoceptive nervous system in autism. To investigate differences, one could look for differences in afferent tracts from the viscera (e.g., vagus nerve), efferent parasympathetic processing, and/or changes in the brainstem or other interoceptive system tracts. With regard to afferent visceral tracts, there is ample evidence that signaling by the vagus nerve may be impacted by microbial and metabolite differences commonly found in autism (see Chernikova et al;103 Taniya et al104, for reviews). Such signaling differences from gut dysbiosis may impact not only interoceptive processes, but also socio-emotional processes.105
Further, autistic individuals show differences in physiological responses in the autonomic nervous system. A recent meta-analysis investigated the physiological response in autistic individuals in comparison to a non-autistic group, focusing on two key factors: (a) the type of physiological measure used, particularly its connection to the autonomic nervous system branches (sympathetic and parasympathetic); and (b) the social context in which the measurements were taken.106 The findings revealed significant differences between groups, particularly in relation to the activity of the parasympathetic nervous system and the combined activity of the sympathetic and parasympathetic systems during social interactions. Specifically, respiratory sinus arrhythmia, a common measure of peripheral nervous system activity, showed reduced activity during exposure to environmental stimuli. This may suggest that in autism, there may be differences in inhibitory mechanisms needed to reallocate physiological resources in response to external factors.106 Along this line, in both autistic and non-autistic children, Bufo et al107 collected autonomic parameters during gentle tactile stimulation in two skin regions, one corresponding to high-intensity C fibers (forearm), and the other to low-intensity C fibers l (palm of the hand). In response to tactile stimuli on both skin regions, non-autistic children had an increase in pupil diameter and skin conductance, along with a decrease in heart rate. However, autistic children exhibited reduced autonomic responses overall, and their baseline autonomic nervous system activity was significantly different to non-autistic children. These findings suggest autonomic dysregulation and lower tactile autonomic evoked responses in autistic children in response to affective stimulation.
With regard to the brainstem, several studies indicate differences in autism.108–111 These include significant differences in brainstem volume,112 brainstem gray matter volume,109 and lower white matter volume.113–115 Additionally, studies have shown that impairments in the superior colliculus have been observed in autistic individuals.116,117 Furthermore, a longitudinal study found that youth with autism displayed atypical brainstem development.110 Longitudinal, histology, psychophysiology and neuroimaging studies have shown atypical brainstem development in autism though differences in autism may be attenuated with age.110,111 Burstein et al116 posit that early life brainstem-mediated markers related to autonomic/arousal regulation, sleep-wake homeostasis, and sensorimotor integration and reactivity (including interoception), may contribute to the early autism symptomatology. Furthermore, it is posited that differences in neuromodulation by the brainstem (which releases neuromodulators such as dopamine, norepinephrine, and serotonin) may also contribute to autistic symptomatology.118
In addition, in autism, changes in the development of the brainstem during early life stages could have a cascading effect on the formation of the cortex and cerebellum.111,119 Epidemiology findings and data from animal models of autism provide support for this hypothesis, particularly during the peak formation of the brainstem’s monoaminergic centers.119 These differences in brainstem development and maturation may be related to specific autistic symptoms, such as atypical sensorimotor features. Specifically, a diffusion-weighted imaging (DWI) study examined the sensory-brainstem relationship in 133 children between the ages of 6 and 11, including 61 autistic children and 72 non-autistic children. In autistic children, sensory hypo-responsiveness and heightened response to touch were specifically associated with the microstructure of white matter in brainstem tracts.120 However, other studies have not found any significant brainstem differences in autism.121,122 Discrepancies between studies may arise from the vast age ranges of participants studied121 or the inclusion of only adults.122 Taken together, some studies indicate brainstem differences in autism, and that they may play a role in the behavioral responses of autistic children to sensory stimuli. How these may also relate to interoceptive processing, however, remains to be determined.
Other studies on the neural correlates of autism indicate differences in thalamic connectivity in autism. For example, resting state fMRI studies comparing neural activity in infants with high likelihood (have an older sibling with autism; HL) and low likelihood of autism (no siblings with ASD; LL) indicate increased thalamo-limbic connectivity between the bilateral thalamus and the hippocampus, parahippocampus, left amygdala, and left olfactory cortex at 1.5 months of age compared to the lower likelihood (LL) group. In addition, at 9 months, the HL group showed thalamo-cortical hypoconnectivity with several prefrontal regions, including the medial prefrontal cortex (mPFC) and motor areas.123 These results indicate alterations in functional thalamic networks involved in sensory processing may be present in the first nine months of life in HL infants. These results are consistent with Nair et al,124 which also found reduced connectivity between: 1) the prefrontal cortex and the anterior/dorsal nuclei of the thalamus; 2) thalamic-occipital regions; and 3) thalamic-motor regions in HL infants relative to LL group. Further, at 6 weeks of age, aberrant thalamocortical connectivity, at both the functional and structural level, predicted atypical social development assessed with eye-tracking and clinical measures between 9 and 36 months of age. Taken together, these studies seem to indicate that HL infants may be on a delayed and/or differential maturational neural trajectory for thalamocortical connectivity and sensory responsivity as early as 1.5 months of age, though more work is needed to verify these findings and connect them to potential differences in interoception.123,124
Furthermore, evidence suggests that the thalamocortical and thalamo-subcortical pain-processing pathways play a role in reduced pain awareness in autistic individuals.83 During aversive sensory stimulation, autistic individuals also exhibit attenuated thalamocortical connectivity between the thalamus and the cortex. However, there is enhanced connectivity between the thalamus and subcortical areas such as the putamen, hippocampus, and amygdala. These results suggest that modified thalamus connectivity may contribute to attributing pain to benign tactile stimuli in autistic individuals.83
The insula is a “hub” for coordinating brain network dynamics. In autism, structural and functional changes in the insula, as well as alterations in connectivity, have additionally been observed.125–128 Specifically, hyperconnectivity has been observed in the anterior insula and ACC, which are both part of the salience network.129 This hyperconnectivity pattern can differentiate autistic children from typically developing children and can also predict the severity of symptomatology, such as restricted and repetitive behaviors.126 Indeed, many connectivity differences have been found in autism, including between network connectivity (DMN, salience-executive network and fronto-parietal network);99,126,130,131 and aberrant connectivity in attention networks (ventral and dorsal attention networks).132–134 These results are in line with the proposals that autism may, in part, arise from differences in neural connectivity, with atypical connections between and within multiple intrinsic functional networks involved from salience, to sensory, to attentional, to cognitive and socio-emotional processes.134–136
Taken together, there is limited work on how neural differences are specifically related to potential differences in the interoceptive nervous system in autism. However, there is indication that many hubs of the interoceptive nervous system – vagal processing, brainstem, thalamus, and insula, may have differences in development, morphometry, and connectivity, all of which may impact interoceptive processing and intero-exteroceptive sensory integration and interpretation in autism. Nevertheless, much more research on this topic is needed.
Conclusion
Here we aimed to explore the potential relationships between interoceptive processing in autism. Interoception plays a central role in normative functioning by providing the brain the internal sensory states of the body. Additionally, the interoceptive network interplays bidirectionally with exteroceptive sensory, motor, and cognitive networks. A crucial characteristic of interoception is its intrinsic valence and arousal that have influence in attention allocation, shaping how individuals perceive and interact with the world around them.6
There still remains a debate about whether or not there are differences in interoceptive processing in autism. Measurement issues remain as one of the greatest barriers, making it difficult to assess potential differences in autism. To better understand different levels of interoceptive processing, it may help to divide the concept of interoception into different components, including attention, discrimination, accuracy, insight, and integration.51,52,60,137–139 This would lessen the burden of metacognitive ability and alexithymia on current measures of interoception. In addition, methodology for the study of non-conscious interoceptive processing may be an important step in future autism research and different kinds of interoceptive signals (e.g., cardiac, thermosensory, nociceptive) may be probed separately. Further, there remains a need to better understand how interoceptive and exteroceptive signals are integrated and how this process may differ in autism.
Neurobiologically, we discussed how afferent pathways from the viscera may have aberrant signaling from microbial and metabolite differences common to autism.103 In addition, brain regions, such as brainstem nuclei, the thalamus, and insula implicated in interoceptive processing show differential integrity, activity patterns, and/or connectivity patterns in autism.83,101,111,123,124 These patterns have been correlated with sensory sensitivities, but further studies on their relationship to interoceptive ability remain to be determined. Additionally, in autism, differences in the thalamocortical and thalamo-subcortical pathways may lead to differences in interoceptive processing such as pain and/or attributing pain to sensory experiences.83 Future research on interoception at early processing levels, such as the function of peripheral small fibers and the relation to the autonomic regulation, could also contribute to the understanding of some behavioral and social symptomatology experienced by autistic individuals.107,140
In conclusion, there still remains a debate on the differences in interoception in autism. In this narrative review, we provide evidence to explain why there are discrepancies in past research and suggestions for future research directions to help scholars obtain a better understanding of behavioral and neurobiological impacts of interoceptive processing across the autism spectrum.
Acknowledgments
We thank Carissa Cascio for her feedback on an earlier version of this manuscript. Additionally, we thank Tarun Seera for her assistance with this manuscript.
Funding Statement
This publication was supported by the Department of Defense through the Idea Development Award under award number AR170062. Opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the Department of Defense.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Damasio A, Damasio H. Feelings are the source of consciousness. Neural Comput. 2022;35(3):277–286. doi: 10.1162/neco_a_01521 [DOI] [PubMed] [Google Scholar]
- 2.Carvalho GB, Damasio A. Interoception and the origin of feelings: a new synthesis. BioEssays. 2021;43(6):2000261. doi: 10.1002/bies.202000261 [DOI] [PubMed] [Google Scholar]
- 3.Craig AD. How do you feel? Interoception: the sense of the physiological condition of the body. Nat Rev Neurosci. 2002;3(8):655–666. doi: 10.1038/nrn894 [DOI] [PubMed] [Google Scholar]
- 4.Craig A B. Interoception: the sense of the physiological condition of the body. Curr Opin Neurobiol. 2003;13(4):500–505. doi: 10.1016/S0959-4388(03)00090-4 [DOI] [PubMed] [Google Scholar]
- 5.Cameron OG. Interoception: the inside story—a model for psychosomatic processes. Psychosom Med. 2001;63(5):697–710. doi: 10.1097/00006842-200109000-00001 [DOI] [PubMed] [Google Scholar]
- 6.Damasio A, Carvalho GB. The nature of feelings: evolutionary and neurobiological origins. Nat Rev Neurosci. 2013;14(2):143–152. doi: 10.1038/nrn3403 [DOI] [PubMed] [Google Scholar]
- 7.Crucianelli L, Ehrsson HH. The role of the skin in interoception: a neglected organ? Perspect Psychol Sci. 2023;18(1):224–238. doi: 10.1177/17456916221094509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crucianelli L, Enmalm A, Ehrsson HH. Interoception as independent cardiac, thermosensory, nociceptive, and affective touch perceptual submodalities. Biol Psychol. 2022;172:108355. doi: 10.1016/j.biopsycho.2022.108355 [DOI] [PubMed] [Google Scholar]
- 9.Craig A. A new view of pain as a homeostatic emotion. Trends Neurosci. 2003;26(6):303–307. doi: 10.1016/S0166-2236(03)00123-1 [DOI] [PubMed] [Google Scholar]
- 10.Khalsa SS, Adolphs R, Cameron OG, et al. Interoception and Mental Health: a Roadmap. Biol Psychiatry Cogn Neurosci Neuroimaging. 2018;3(6):501–513. doi: 10.1016/j.bpsc.2017.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen WG, Schloesser D, Arensdorf AM, et al. The emerging science of interoception: sensing, integrating, interpreting, and regulating signals within the self. Trends Neurosci. 2021;44(1):3–16. doi: 10.1016/j.tins.2020.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berntson GG, Khalsa SS. Neural circuits of interoception. Trends Neurosci. 2021;44(1):17–28. doi: 10.1016/j.tins.2020.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barrett LF. The theory of constructed emotion: an active inference account of interoception and categorization. Soc Cogn Affect Neurosci. 2017;nsw154. doi: 10.1093/scan/nsw154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.James W. The Principles of Psychology. Vol. 1. Henry Holt and Co; 1890. doi: 10.1037/10538-000 [DOI] [Google Scholar]
- 15.Damasio AR. Feeling & Knowing: Making Minds Conscious. 1st ed. Pantheon Books; 2021. [DOI] [PubMed] [Google Scholar]
- 16.Zhou H, Gao Q, Chen W, Wei Q. Action understanding promoted by interoception in children: a developmental model. Front Psychol. 2022;13:724677. doi: 10.3389/fpsyg.2022.724677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bechara A, Damasio AR. The somatic marker hypothesis: a neural theory of economic decision. Games Econ Behav. 2005;52(2):336–372. doi: 10.1016/j.geb.2004.06.010 [DOI] [Google Scholar]
- 18.Pollatos O, Mönkemöller K, Groppe K, Elsner B. Interoceptive accuracy is associated with benefits in decision making in children. Front Psychol. 2023;13:1070037. doi: 10.3389/fpsyg.2022.1070037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koreki A, Goeta D, Ricciardi L, et al. The relationship between interoception and agency and its modulation by heartbeats: an exploratory study. Sci Rep. 2022;12(1):13624. doi: 10.1038/s41598-022-16569-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baiano C, Job X, Kirsch LP, Auvray M. Interoceptive abilities facilitate taking another’s spatial perspective. Sci Rep. 2023;13(1):10064. doi: 10.1038/s41598-023-36173-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Feldman MJ, MacCormack JK, Bonar AS, Lindquist KA. Interoceptive ability moderates the effect of physiological reactivity on social judgment. Emotion. 2023. doi: 10.1037/emo0001210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Von Mohr M, Finotti G, Esposito G, Bahrami B, Tsakiris M. Social interoception: perceiving events during cardiac afferent activity makes people more suggestible to other people’s influence. Cognition. 2023;238:105502. doi: 10.1016/j.cognition.2023.105502 [DOI] [PubMed] [Google Scholar]
- 23.Azevedo RT, Von Mohr M, Tsakiris M. From the viscera to first impressions: phase-dependent cardio-visual signals bias the perceived trustworthiness of faces. Psychol Sci. 2023;34(1):120–131. doi: 10.1177/09567976221131519 [DOI] [PubMed] [Google Scholar]
- 24.Engelen T, Solcà M, Tallon-Baudry C. Interoceptive rhythms in the brain. Nat Neurosci. 2023. doi: 10.1038/s41593-023-01425-1 [DOI] [PubMed] [Google Scholar]
- 25.Quadt L, Critchley H, Nagai Y. Cognition, emotion, and the central autonomic network. Auton Neurosci. 2022;238:102948. doi: 10.1016/j.autneu.2022.102948 [DOI] [PubMed] [Google Scholar]
- 26.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. DSM-5-TR. American Psychiatric Association Publishing; 2022. [Google Scholar]
- 27.Djerassi M, Ophir S, Atzil S. What is social about autism? The role of allostasis-driven learning. Brain Sci. 2021;11(10):1269. doi: 10.3390/brainsci11101269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Proff I, Williams GL, Quadt L, Garfinkel SN. Sensory processing in autism across exteroceptive and interoceptive domains. Psychol Neurosci. 2022;15(2):105–130. doi: 10.1037/pne0000262 [DOI] [Google Scholar]
- 29.Yang H, Zhou H, Li Y, et al. Decreased interoceptive accuracy in children with autism spectrum disorder and with comorbid attention deficit/hyperactivity disorder. Autism Res. 2022;15(4):729–739. doi: 10.1002/aur.2679 [DOI] [PubMed] [Google Scholar]
- 30.Palser ER, Fotopoulou A, Pellicano E, Kilner JM. Dissociation in how core autism features relate to interoceptive dimensions: evidence from cardiac awareness in children. J Autism Dev Disord. 2020;50(2):572–582. doi: 10.1007/s10803-019-04279-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Palser ER, Fotopoulou A, Pellicano E, Kilner JM. The link between interoceptive processing and anxiety in children diagnosed with autism spectrum disorder: extending adult findings into a developmental sample. Biol Psychol. 2018;136:13–21. doi: 10.1016/j.biopsycho.2018.05.003 [DOI] [PubMed] [Google Scholar]
- 32.Arnaud S. Self‐consciousness in autism: a third‐person perspective on the self. Mind Lang. 2022;37(3):356–372. doi: 10.1111/mila.12356 [DOI] [Google Scholar]
- 33.Noel J, Lytle M, Cascio C, Wallace MT. Disrupted integration of exteroceptive and interoceptive signaling in autism spectrum disorder. Autism Res. 2018;11(1):194–205. doi: 10.1002/aur.1880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schauder KB, Mash LE, Bryant LK, Cascio CJ. Interoceptive ability and body awareness in autism spectrum disorder. J Exp Child Psychol. 2015;131:193–200. doi: 10.1016/j.jecp.2014.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Williams ZJ, Suzman E, Bordman SL, et al. Characterizing interoceptive differences in autism: a systematic review and meta-analysis of case–control studies. J Autism Dev Disord. 2023;53(3):947–962. doi: 10.1007/s10803-022-05656-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Garfinkel SN, Tiley C, O’Keeffe S, Harrison NA, Seth AK, Critchley HD. Discrepancies between dimensions of interoception in autism: implications for emotion and anxiety. Biol Psychol. 2016;114:117–126. doi: 10.1016/j.biopsycho.2015.12.003 [DOI] [PubMed] [Google Scholar]
- 37.Lai MC, Kassee C, Besney R, et al. Prevalence of co-occurring mental health diagnoses in the autism population: a systematic review and meta-analysis. Lancet Psychiatry. 2019;6(10):819–829. doi: 10.1016/S2215-0366(19)30289-5 [DOI] [PubMed] [Google Scholar]
- 38.Micai M, Fatta LM, Gila L, et al. Prevalence of co-occurring conditions in children and adults with autism spectrum disorder: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2023;155:105436. doi: 10.1016/j.neubiorev.2023.105436 [DOI] [PubMed] [Google Scholar]
- 39.Barrett LF, Simmons WK. Interoceptive predictions in the brain. Nat Rev Neurosci. 2015;16(7):419–429. doi: 10.1038/nrn3950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Failla M D, Bryant L K, Heflin B H, Mash L E, Schauder K, Davis S, Gerdes M B, Weitlauf A, Rogers B P and Cascio C J. (2020). Neural Correlates of Cardiac Interoceptive Focus Across Development: Implications for Social Symptoms in Autism Spectrum Disorder. Autism Research, 13(6), 908–920. 10.1002/aur.2289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Palser ER, Galvez-Pol A, Palmer CE, et al. Reduced differentiation of emotion-associated bodily sensations in autism. Autism. 2021;25(5):1321–1334. doi: 10.1177/1362361320987950 [DOI] [PubMed] [Google Scholar]
- 42.Failla MD, Gerdes MB, Williams ZJ, et al. Increased pain sensitivity and pain-related anxiety in individuals with autism. Pain Reports. 2020;5():1–10. doi: 10.1097/PR9.0000000000000861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Failla MD, Peters BR, Karbasforoushan H, et al. Intrainsular connectivity and somatosensory responsiveness in young children with ASD. Mol Autism. 2017;8(1):25. doi: 10.1186/s13229-017-0143-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vaughan S, McGlone F, Poole H, Moore DJ. A quantitative sensory testing approach to pain in autism spectrum disorders. J Autism Dev Disord. 2020;50(5):1607–1620. doi: 10.1007/s10803-019-03918-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Trevisan DA, Parker T, McPartland JC. First-hand accounts of interoceptive difficulties in autistic adults. J Autism Dev Disord. 2021;51(10):3483–3491. doi: 10.1007/s10803-020-04811-x [DOI] [PubMed] [Google Scholar]
- 46.DuBois D, Ameis SH, Lai M, Casanova MF, Desarkar P. Interoception in Autism Spectrum Disorder: a review. Int J Dev Neurosci. 2016;52(1):104–111. doi: 10.1016/j.ijdevneu.2016.05.001 [DOI] [PubMed] [Google Scholar]
- 47.Nicholson T, Williams D, Carpenter K, Kallitsounaki A. Interoception is impaired in children, but not adults, with autism spectrum disorder. J Autism Dev Disord. 2019;49(9):3625–3637. doi: 10.1007/s10803-019-04079-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shah P, Hall R, Catmur C, Bird G. Alexithymia, not autism, is associated with impaired interoception. Cortex. 2016;81:215–220. doi: 10.1016/j.cortex.2016.03.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Butera CD, Harrison L, Kilroy E, et al. Relationships between alexithymia, interoception, and emotional empathy in autism spectrum disorder. Autism. 2022;27(3):690–703. doi: 10.1177/13623613221111310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ben Hassen N, Molins F, Garrote-Petisco D, Serrano MÁ. Emotional regulation deficits in autism spectrum disorder: the role of alexithymia and interoception. Res Dev Disabil. 2023;132:104378. doi: 10.1016/j.ridd.2022.104378 [DOI] [PubMed] [Google Scholar]
- 51.Suksasilp C, Garfinkel SN. Towards a comprehensive assessment of interoception in a multi-dimensional framework. Biol Psychol. 2022;168:108262. doi: 10.1016/j.biopsycho.2022.108262 [DOI] [PubMed] [Google Scholar]
- 52.Murphy J, Brewer R, Plans D, Khalsa SS, Catmur C, Bird G. Testing the Independence of self-reported interoceptive accuracy and attention. Q J Exp Psychol. 2020;73(1):115–133. doi: 10.1177/1747021819879826 [DOI] [PubMed] [Google Scholar]
- 53.Nicolardi V, Fanizza I, Accogli G, Macchitella L, Scoditti S, Trabacca A. Pain assessment in autism: updating the ethical and methodological challenges through a state-of-The-art review. Neurol Sci. 2023;44(11):3853–3861. doi: 10.1007/s10072-023-06942-2 [DOI] [PubMed] [Google Scholar]
- 54.Trevisan DA, Mehling WE, McPartland JC. Adaptive and maladaptive bodily awareness: distinguishing interoceptive sensibility and interoceptive attention from anxiety-induced somatization in autism and alexithymia. Autism Res. 2021;14(2):240–247. doi: 10.1002/aur.2458 [DOI] [PubMed] [Google Scholar]
- 55.Shipkova M, Butera CD, Flores GD, et al. Caregiver and youth inter‐rater assessment agreement in autism spectrum disorder, developmental coordination disorder, and typical development. Autism Res. 2024:aur.3110. doi: 10.1002/aur.3110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Adams KL, Murphy J, Catmur C, Bird G. The role of interoception in the overlap between eating disorders and autism: methodological considerations. Eur Eat Disord Rev. 2022;30(5):501–509. doi: 10.1002/erv.2905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kinnaird E, Stewart C, Tchanturia K. Investigating alexithymia in autism: a systematic review and meta-analysis. Eur Psychiatry. 2019;55:80–89. doi: 10.1016/j.eurpsy.2018.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bonaz B, Lane RD, Oshinsky ML, et al. Diseases, disorders, and comorbidities of interoception. Trends Neurosci. 2021;44(1):39–51. doi: 10.1016/j.tins.2020.09.009 [DOI] [PubMed] [Google Scholar]
- 59.Brewer R, Cook R, Bird G. Alexithymia: a general deficit of interoception. R Soc Open Sci. 2016;3(10):150664. doi: 10.1098/rsos.150664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Desmedt O, Luminet O, Walentynowicz M, Corneille O. The new measures of interoceptive accuracy: a systematic review and assessment. Neurosci Biobehav Rev. 2023;153:105388. doi: 10.1016/j.neubiorev.2023.105388 [DOI] [PubMed] [Google Scholar]
- 61.Critchley HD, Harrison NA. Visceral influences on brain and behavior. Neuron. 2013;77(4):624–638. doi: 10.1016/j.neuron.2013.02.008 [DOI] [PubMed] [Google Scholar]
- 62.Critchley HD, Wiens S, Rotshtein P, Öhman A, Dolan RJ. Neural systems supporting interoceptive awareness. Nat Neurosci. 2004;7(2):189–195. doi: 10.1038/nn1176 [DOI] [PubMed] [Google Scholar]
- 63.Petzschner FH, Garfinkel SN, Paulus MP, Koch C, Khalsa SS. Computational models of interoception and body regulation. Trends Neurosci. 2021;44(1):63–76. doi: 10.1016/j.tins.2020.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Quigley KS, Kanoski S, Grill WM, Barrett LF, Tsakiris M. Functions of interoception: from energy regulation to experience of the self. Trends Neurosci. 2021;44(1):29–38. doi: 10.1016/j.tins.2020.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sennesh E, Theriault J, Brooks D, Van De Meent JW, Barrett LF, Quigley KS. Interoception as modeling, allostasis as control. Biol Psychol. 2022;167:108242. doi: 10.1016/j.biopsycho.2021.108242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Seth AK, Friston KJ. Active interoceptive inference and the emotional brain. Philos Trans R Soc B Biol Sci. 2016;371(1708):20160007. doi: 10.1098/rstb.2016.0007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hodson R, Mehta M, Smith R. The empirical status of predictive coding and active inference. Neurosci Biobehav Rev. 2024;157:105473. doi: 10.1016/j.neubiorev.2023.105473 [DOI] [PubMed] [Google Scholar]
- 68.Haruno M, Wolpert DM, Kawato M. MOSAIC model for sensorimotor learning and control. Neural Comput. 2001;13(10):2201–2220. doi: 10.1162/089976601750541778 [DOI] [PubMed] [Google Scholar]
- 69.Friston K. The free-energy principle: a unified brain theory? Nat Rev Neurosci. 2010;11(2):127–138. doi: 10.1038/nrn2787 [DOI] [PubMed] [Google Scholar]
- 70.Friston K. A theory of cortical responses. Philos Trans R Soc B Biol Sci. 2005;360(1456):815–836. doi: 10.1098/rstb.2005.1622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ortiz-Tudela J, Nicholls VI, Clarke A. Parameters of prediction: multidimensional characterization of top-down influence in visual perception. Neurosci Biobehav Rev. 2023;153:105369. doi: 10.1016/j.neubiorev.2023.105369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Qin C, Michon F, Onuki Y, et al. Predictability alters information flow during action observation in human electrocorticographic activity. Cell Rep. 2023;42(11):113432. doi: 10.1016/j.celrep.2023.113432 [DOI] [PubMed] [Google Scholar]
- 73.Hatfield TR, Brown RF, Giummarra MJ, Lenggenhager B. Autism spectrum disorder and interoception: abnormalities in global integration? Autism. 2019;23(1):212–222. doi: 10.1177/1362361317738392 [DOI] [PubMed] [Google Scholar]
- 74.Happé F, Frith U. The weak coherence account: detail-focused cognitive style in autism spectrum disorders. J Autism Dev Disord. 2006;36(1):5–25. doi: 10.1007/s10803-005-0039-0 [DOI] [PubMed] [Google Scholar]
- 75.Puts NAJ, Wodka EL, Harris AD, et al. Reduced GABA and altered somatosensory function in children with autism spectrum disorder. Autism Res. 2017;10(4):608–619. doi: 10.1002/aur.1691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Failla MD, Moana-Filho EJ, Essick GK, Baranek GT, Rogers BP, Cascio CJ. Initially intact neural responses to pain in autism are diminished during sustained pain. Autism. 2018;22(6):669–683. doi: 10.1177/1362361317696043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Quattrocki E, Friston K. Autism, oxytocin and interoception. Neurosci Biobehav Rev. 2014;47:410–430. doi: 10.1016/j.neubiorev.2014.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sapey-Triomphe LA, Pattyn L, Weilnhammer V, Sterzer P, Wagemans J. Neural correlates of hierarchical predictive processes in autistic adults. Nat Commun. 2023;14(1):3640. doi: 10.1038/s41467-023-38580-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Cannon J, O’Brien AM, Bungert L, Sinha P. Prediction in Autism spectrum disorder: a systematic review of empirical evidence. Autism Res. 2021;14(4):604–630. doi: 10.1002/aur.2482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Finnemann JJS, Plaisted-Grant K, Moore J, Teufel C, Fletcher PC. Low-level, prediction-based sensory and motor processes are unimpaired in Autism. Neuropsychologia. 2021;156:107835. doi: 10.1016/j.neuropsychologia.2021.107835 [DOI] [PubMed] [Google Scholar]
- 81.Ward EK, Buitelaar JK, Hunnius S. Autistic and nonautistic adolescents do not differ in adaptation to gaze direction. Autism Res. 2024;aur.3118. doi: 10.1002/aur.3118 [DOI] [PubMed] [Google Scholar]
- 82.Moore DJ. Acute pain experience in individuals with autism spectrum disorders: a review. Autism. 2015;19(4):387–399. doi: 10.1177/1362361314527839 [DOI] [PubMed] [Google Scholar]
- 83.Bogdanova OV, Bogdanov VB, Pizano A, et al. The current view on the paradox of pain in autism spectrum disorders. Front Psychiatry. 2022;13:910824. doi: 10.3389/fpsyt.2022.910824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ortiz Rubio A, de María Romero Ayuso DN, Torres Sánchez I, et al. Pain experiences of people diagnosed with autism spectrum disorder: a systematic review of case–control studies. Am J Occup Ther. 2023;77(2):7702185020. doi: 10.5014/ajot.2023.050050 [DOI] [PubMed] [Google Scholar]
- 85.Hoffman T, Bar-Shalita T, Granovsky Y, et al. Indifference or hypersensitivity? Solving the riddle of the pain profile in individuals with autism. Pain. 2023;164(4):791–803. doi: 10.1097/j.pain.0000000000002767 [DOI] [PubMed] [Google Scholar]
- 86.Riquelme I, Hatem SM, Sabater-Gárriz Á, Montoya P. A multidimensional investigation of the relationship between skin-mediated somatosensory signals, emotion regulation and behavior problems in autistic children. Front Neurosci. 2023;17:1227173. doi: 10.3389/fnins.2023.1227173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chien YL, Chao CC, Wu SW, et al. Small fiber pathology in autism and clinical implications. Neurology. 2020;95(19). doi: 10.1212/WNL.0000000000010932 [DOI] [PubMed] [Google Scholar]
- 88.Courtemanche AB, Black WR, Reese RM. The relationship between pain, self-injury, and other problem behaviors in young children with autism and other developmental disabilities. Am J Intellect Dev Disabil. 2016;121(3):194–203. doi: 10.1352/1944-7558-121.3.194 [DOI] [PubMed] [Google Scholar]
- 89.Stein BE, Stanford TR, Rowland BA. Development of multisensory integration from the perspective of the individual neuron. Nat Rev Neurosci. 2014;15(8):520–535. doi: 10.1038/nrn3742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lefler Y, Campagner D, Branco T. The role of the periaqueductal gray in escape behavior. Curr Opin Neurobiol. 2020;60:115–121. doi: 10.1016/j.conb.2019.11.014 [DOI] [PubMed] [Google Scholar]
- 91.Silva C, McNaughton N. Are periaqueductal gray and dorsal raphe the foundation of appetitive and aversive control? A comprehensive review. Prog Neurobiol. 2019;177:33–72. doi: 10.1016/j.pneurobio.2019.02.001 [DOI] [PubMed] [Google Scholar]
- 92.Venkatraman A, Edlow BL, Immordino-Yang MH. The brainstem in emotion: a review. Front Neuroanat. 2017;11. doi: 10.3389/fnana.2017.00015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Agashkov K, Krotov V, Krasniakova M, et al. Distinct mechanisms of signal processing by lamina I spino-parabrachial neurons. Sci Rep. 2019;9(1):19231. doi: 10.1038/s41598-019-55462-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.De Falco E, Solcà M, Bernasconi F, et al. Single neurons in the thalamus and subthalamic nucleus process cardiac and respiratory signals in humans. Proc Natl Acad Sci. 2024;121(11):e2316365121. doi: 10.1073/pnas.2316365121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.You HJ, Lei J, Pertovaara A. Thalamus: the ‘promoter’ of endogenous modulation of pain and potential therapeutic target in pathological pain. Neurosci Biobehav Rev. 2022;139:104745. doi: 10.1016/j.neubiorev.2022.104745 [DOI] [PubMed] [Google Scholar]
- 96.Shine JM, Lewis LD, Garrett DD, Hwang K. The impact of the human thalamus on brain-wide information processing. Nat Rev Neurosci. 2023;24(7):416–430. doi: 10.1038/s41583-023-00701-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Scarpazza C, Zangrossi A, Huang YC, Sartori G, Massaro S. Disentangling interoceptive abilities in alexithymia. Psychol Res. 2022;86(3):844–857. doi: 10.1007/s00426-021-01538-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Dobrushina OR, Arina GA, Dobrynina LA, et al. Sensory integration in interoception: interplay between top-down and bottom-up processing. Cortex. 2021;144:185–197. doi: 10.1016/j.cortex.2021.08.009 [DOI] [PubMed] [Google Scholar]
- 99.Uddin LQ. Idiosyncratic connectivity in autism: developmental and anatomical considerations. Trends Neurosci. 2015;38(5):261–263. doi: 10.1016/j.tins.2015.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tan Y, Yan R, Gao Y, Zhang M, Northoff G. Spatial-topographic nestedness of interoceptive regions within the networks of decision making and emotion regulation: combining ALE meta-analysis and MACM analysis. NeuroImage. 2022;260:119500. doi: 10.1016/j.neuroimage.2022.119500 [DOI] [PubMed] [Google Scholar]
- 101.Molnar-Szakacs I, Uddin LQ. Anterior insula as a gatekeeper of executive control. Neurosci Biobehav Rev. 2022;139:104736. doi: 10.1016/j.neubiorev.2022.104736 [DOI] [PubMed] [Google Scholar]
- 102.Azzalini D, Rebollo I, Tallon-Baudry C. Visceral signals shape brain dynamics and cognition. Trends Cognit Sci. 2019;23(6):488–509. doi: 10.1016/j.tics.2019.03.007 [DOI] [PubMed] [Google Scholar]
- 103.Chernikova MA, Flores GD, Kilroy E, Labus JS, Mayer EA, Aziz-Zadeh L. The brain-gut-microbiome system: pathways and implications for autism spectrum disorder. Nutrients. 2021;13(12):4497. doi: 10.3390/nu13124497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Taniya MA, Chung HJ, Al Mamun A, et al. Role of gut microbiome in autism spectrum disorder and its therapeutic regulation. Front Cell Infect Microbiol. 2022;12:915701. doi: 10.3389/fcimb.2022.915701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Morais LH, Schreiber HL, Mazmanian SK. The gut microbiota–brain axis in behaviour and brain disorders. Nat Rev Microbiol. 2021;19(4):241–255. doi: 10.1038/s41579-020-00460-0 [DOI] [PubMed] [Google Scholar]
- 106.Zadok E, Golan O, Lavidor M, Gordon I. Autonomic nervous system responses to social stimuli among autistic individuals: a systematic review and meta-analysis. Autism Res. 2023;aur.3068. doi: 10.1002/aur.3068 [DOI] [PubMed] [Google Scholar]
- 107.Bufo MR, Guidotti M, Mofid Y, et al. Atypical response to affective touch in children with autism: multi-parametric exploration of the autonomic system. J Clin Med. 2022;11(23):7146. doi: 10.3390/jcm11237146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Baizer JS. Functional and neuropathological evidence for a role of the brainstem in autism. Front Integr Neurosci. 2021;15:748977. doi: 10.3389/fnint.2021.748977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Jou RJ, Minshew NJ, Melhem NM, Keshavan MS, Hardan AY. Brainstem volumetric alterations in children with autism. Psychol Med. 2009;39(8):1347–1354. doi: 10.1017/S0033291708004376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Jou RJ, Frazier TW, Keshavan MS, Minshew NJ, Hardan AY. A two-year longitudinal pilot MRI study of the brainstem in autism. Behav Brain Res. 2013;251:163–167. doi: 10.1016/j.bbr.2013.04.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Seif A, Shea C, Schmid S, Stevenson RA. A systematic review of brainstem contributions to autism spectrum disorder. Front Integr Neurosci. 2021;15:760116. doi: 10.3389/fnint.2021.760116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Fredo ARJ, Kavitha G, Ramakrishnan S. Segmentation and morphometric analysis of subcortical regions in autistic MR brain images using fuzzy Gaussian distribution model-based distance regularised multi-phase level set. Int J Biomed Eng Technol. 2014;15(3):211. doi: 10.1504/IJBET.2014.064647 [DOI] [Google Scholar]
- 113.Cheung C, Chua SE, Cheung V, et al. White matter fractional anisotropy differences and correlates of diagnostic symptoms in autism. J Child Psychol Psychiatr. 2009;50(9):1102–1112. doi: 10.1111/j.1469-7610.2009.02086.x [DOI] [PubMed] [Google Scholar]
- 114.Hanaie R, Mohri I, Kagitani‐Shimono K, et al. White matter volume in the brainstem and inferior parietal lobule is related to motor performance in children with autism spectrum disorder: a voxel-based morphometry study. Autism Res. 2016;9(9):981–992. doi: 10.1002/aur.1605 [DOI] [PubMed] [Google Scholar]
- 115.Hyde KL, Samson F, Evans AC, Mottron L. Neuroanatomical differences in brain areas implicated in perceptual and other core features of autism revealed by cortical thickness analysis and voxel-based morphometry. Hum Brain Mapp. 2010;31(4):556–566. doi: 10.1002/hbm.20887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Burstein O, Geva R. The brainstem-informed autism framework: early life neurobehavioral markers. Front Integr Neurosci. 2021;15:759614. doi: 10.3389/fnint.2021.759614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Jure R. The “Primitive Brain Dysfunction” theory of autism: the superior colliculus role. Front Integr Neurosci. 2022;16:797391. doi: 10.3389/fnint.2022.797391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.London EB. Neuromodulation and a reconceptualization of autism spectrum disorders: using the locus coeruleus functioning as an exemplar. Front Neurol. 2018;9:1120. doi: 10.3389/fneur.2018.01120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Dadalko OI, Travers BG. Evidence for brainstem contributions to autism spectrum disorders. Front Integr Neurosci. 2018;12:47. doi: 10.3389/fnint.2018.00047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Surgent O, Riaz A, Ausderau KK, et al. Brainstem white matter microstructure is associated with hyporesponsiveness and overall sensory features in autistic children. Mol Autism. 2022;13(1):48. doi: 10.1186/s13229-022-00524-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Hardan AY, Minshew NJ, Harenski K, Keshavan MS. Posterior fossa magnetic resonance imaging in autism. J Am Acad Child Adolesc Psychiatry. 2001;40(6):666–672. doi: 10.1097/00004583-200106000-00011 [DOI] [PubMed] [Google Scholar]
- 122.Chaddad A, Desrosiers C, Toews M. Multi-scale radiomic analysis of sub-cortical regions in MRI related to autism, gender and age. Sci Rep. 2017;7(1):45639. doi: 10.1038/srep45639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Wagner L, Banchik M, Okada NJ, et al. Associations between thalamocortical functional connectivity and sensory over-responsivity in infants at high likelihood for ASD. Cereb Cortex. 2023;33(12):8075–8086. doi: 10.1093/cercor/bhad100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Nair A, Jalal R, Liu J, et al. Altered thalamocortical connectivity in 6-week-old infants at high familial risk for autism spectrum disorder. Cereb Cortex. 2021;31(9):4191–4205. doi: 10.1093/cercor/bhab078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Butera C, Kaplan J, Kilroy E, et al. The relationship between alexithymia, interoception, and neural functional connectivity during facial expression processing in autism spectrum disorder. Neuropsychologia. 2023;180:108469. doi: 10.1016/j.neuropsychologia.2023.108469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Uddin LQ, Supekar K, Lynch CJ, et al. Salience network–based classification and prediction of symptom severity in children with autism. JAMA Psychiatry. 2013;70(8):869. doi: 10.1001/jamapsychiatry.2013.104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Nomi JS, Molnar-Szakacs I, Uddin LQ. Insular function in autism: update and future directions in neuroimaging and interventions. Prog Neuropsychopharmacol Biol Psychiatry. 2019;89:412–426. doi: 10.1016/j.pnpbp.2018.10.015 [DOI] [PubMed] [Google Scholar]
- 128.Odriozola P, Uddin LQ, Lynch CJ, Kochalka J, Chen T, Menon V. Insula response and connectivity during social and non-social attention in children with autism. Soc Cogn Affect Neurosci. 2016;11(3):433–444. doi: 10.1093/scan/nsv126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Uddin LQ, Kinnison J, Pessoa L, Anderson ML. Beyond the Tripartite Cognition–Emotion–Interoception Model of the human insular cortex. J Cogn Neurosci. 2013;26(1):16–27. doi: 10.1162/jocn_a_00462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Roy D, Uddin LQ. Atypical core-periphery brain dynamics in autism. Netw Neurosci. 2021;5(2):295–321. doi: 10.1162/netn_a_00181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Uddin LQ, Menon V. The anterior insula in autism: under-connected and under-examined. Neurosci Biobehav Rev. 2009;33(8):1198–1203. doi: 10.1016/j.neubiorev.2009.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Farrant K, Uddin LQ. Atypical developmental of dorsal and ventral attention networks in autism. Dev Sci. 2016;19(4):550–563. doi: 10.1111/desc.12359 [DOI] [PubMed] [Google Scholar]
- 133.Baez AC, Dajani DR, Voorhies W, et al. Parsing heterogeneity of executive function in typically and atypically developing children: a conceptual replication and exploration of social function. J Autism Dev Disord. 2020;50(3):707–718. doi: 10.1007/s10803-019-04290-9 [DOI] [PubMed] [Google Scholar]
- 134.Xiao J, Chen H, Shan X, et al. Linked social–communication dimensions and connectivity in functional brain networks in autism spectrum disorder. Cereb Cortex. 2021;31(8):3899–3910. doi: 10.1093/cercor/bhab057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Sigar P, Uddin LQ, Roy D. Altered global modular organization of intrinsic functional connectivity in autism arises from atypical node-level processing. Autism Res. 2023;16(1):66–83. doi: 10.1002/aur.2840 [DOI] [PubMed] [Google Scholar]
- 136.Liu Y, Wang H, Ding Y. The dynamical biomarkers in functional connectivity of autism spectrum disorder based on dynamic graph embedding. Interdiscip Sci Comput Life Sci. 2023. doi: 10.1007/s12539-023-00592-w [DOI] [PubMed] [Google Scholar]
- 137.Garfinkel SN, Schulz A, Tsakiris M. Addressing the need for new interoceptive methods. Biol Psychol. 2022;170:108322. doi: 10.1016/j.biopsycho.2022.108322 [DOI] [PubMed] [Google Scholar]
- 138.Gabriele E, Spooner R, Brewer R, Murphy J. Dissociations between self-reported interoceptive accuracy and attention: evidence from the Interoceptive Attention Scale. Biol Psychol. 2022;168:108243. doi: 10.1016/j.biopsycho.2021.108243 [DOI] [PubMed] [Google Scholar]
- 139.Murphy J, Catmur C, Bird G. Classifying individual differences in interoception: implications for the measurement of interoceptive awareness. Psychon Bull Rev. 2019;26(5):1467–1471. doi: 10.3758/s13423-019-01632-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Rehbein T, Herrmann DN. Sensory processing in autism spectrum disorder: insights from the periphery? Neurology. 2020;95(19):851–852. doi: 10.1212/WNL.0000000000010931 [DOI] [PubMed] [Google Scholar]