Abstract
A core concept of the Integral Theory System is that “ligaments are for structure; vagina is for function”. The vagina and uterus should be conserved. Because the vagina is an organ, its collagen and elastin, which are so necessary for its function, cannot regenerate once they are removed. Removing the uterus involves severing the descending uterine artery, which is the principal blood supply of the proximal part of the uterosacral ligaments (USLs), and so may cause atrophy, which can cause future incontinence problems because of collagen loss after menopause. The diagnostic algorithm guides which of the five pelvic ligaments need repair. Native ligament plication can be adequate for prolapse/symptom cure, but only in premenopausal women. Postmenopausal women are usually collagen deficient and require collagen-creating tapes or wide-bore polyester sutures to restore structural collagen in the ligaments. Of extreme importance, vaginal tissue excision should be avoided, as consequent scarring may cause “tethered vagina syndrome” (TVS). TVS can cause massive uncontrolled urine loss because the scar tissue in the bladder neck area of the vagina can link the more powerful posterior muscles to the anterior, so the posterior urethra wall is forcibly pulled open, when given the signal to close. Instead of vaginal excision, a “concertina” suture technique re-assigns and shrinks excess vaginal tissue to normal anatomy by 6 weeks. In conclusion, the five key surgical principles of the Integral Theory System are: ligaments are for structure, vagina is for function; structure (prolapse) and function (symptoms) are related; repair the structure and you will restore the function; avoid vaginal excision and hysterectomy; create new collagen to reinforce the damaged ligaments.
Keywords: Surgery principles, ligaments, vagina, collagen, polyester sutures
Highlight box.
Key findings
• “Ligaments for structure, vagina for function.” Ligament plications are effective for pelvic organ prolapse and symptoms in premenopausal women. Older women need collagen-creating methods such as slings.
What is known and what is new?
• Conventional native vaginal repairs for organ prolapse have high recurrence rates.
• It is the ligaments which must be reconstructed for prolapse repair.
What is the implication, and what should change now?
• Older women, have high surgical failure rates because their tissues are more deficient in collagen. In older women, repairing the ligaments with slings or collagen-creating wide-bore polyester sutures will result in much higher cure rates. The vagina and uterus should be conserved.
Introduction
The key points of the article are summarized in the video abstract (Video S1).
Video S1.
Video abstract.
“Precise, almost mathematical knowledge of anatomy is a highly fertile source of surgical applications, suggesting new techniques and helping perfect and simplify existing surgical methods, making them less mutilating and more benign and, in short, raising surgery to the rank of true science.” Salvador Gil Vernet.
What is it for? Salvador Gil Vernet [1892–1987], a famous Spanish anatomist/surgeon, and Nobel Prize Nominee.
The aim of this review is to share basic surgical principles developed over 30 years by surgeons who follow the Integral Theory Paradigm (ITP) surgical system. We have found that these methods vastly reduce intraoperative blood loss, the need for catheterization postoperatively, problems with scar tissue from vaginal excision, and generally allow same-day discharge from hospital. Subsequent contributions will describe repair of each of the five pelvic ligaments, native tissue repair for younger women, collagen-creating slings, or wide-bore polyester sutures for ligaments structurally weakened by collagen loss.
Ligaments are for structure; vagina is for function
Traditionally, at least in the pelvic floor Anglosphere, vaginal repairs involving excision of vaginal tissue have been the mainstay of surgery for pelvic organ prolapse (POP), sometimes (Kelly operation) even for stress urinary incontinence (SUI). In addition to excising tissue during a posterior repair, some surgeons excise large V-shaped segments from the perineal body (PB) as part of a PB repair.
Our thesis is that the vagina needs to be conserved, and the uterus, also, whenever possible. Biomechanically, the vagina is a weak elastic membrane (1,2). The vagina gains its strength through stretching by the opposite stretching forces, the pubococcygeus muscle (PCM) anteriorly and the levator plate (LP) and conjoint longitudinal muscle of the anus (LMA) posteriorly (Figure 1). With reference to Figure 1, like the traffic road of a suspension bridge, the anterior vaginal wall [pubocervical fascia (PCF)] is suspended anteriorly by the pubourethral ligament (PUL), laterally by the arcus tendineus fascia pelvis (ATFP) and at the cervix, by the cardinal ligament (CL). The posterior vaginal wall [rectovaginal fascia (RVF)] is suspended inferiorly by the PB, superiorly by uterosacral ligaments (USLs), and laterally by the ATFP. The vagina is stretched to help open and close the urethra, and to support the bladder base stretch receptors, “N” (Figure 1). Excising the vagina reduces its quantum of elastin and collagen III, which reduces all these functions. Furthermore, excess vaginal excision will either narrow the vagina, or shorten it. If scarring at the bladder neck area of the vagina is sufficient, the patient may develop “tethered vagina syndrome” (TVS), classically, massive uncontrollable urine loss on getting out of bed in the morning (this is described later in this series).
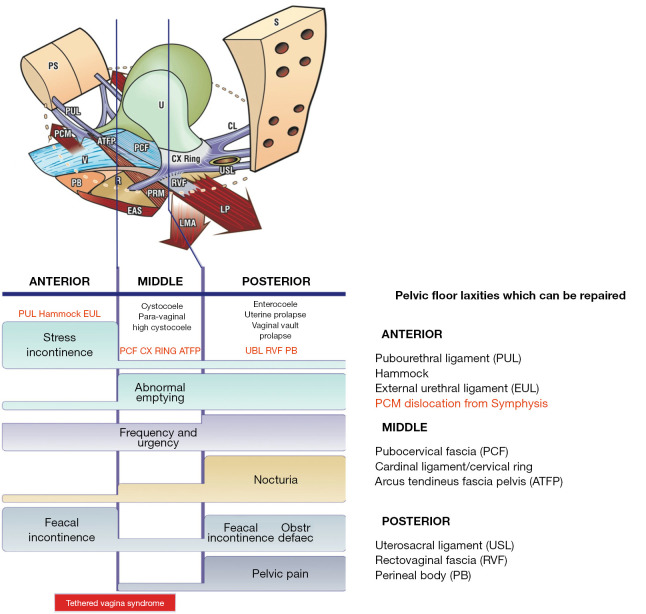
Figure 1.
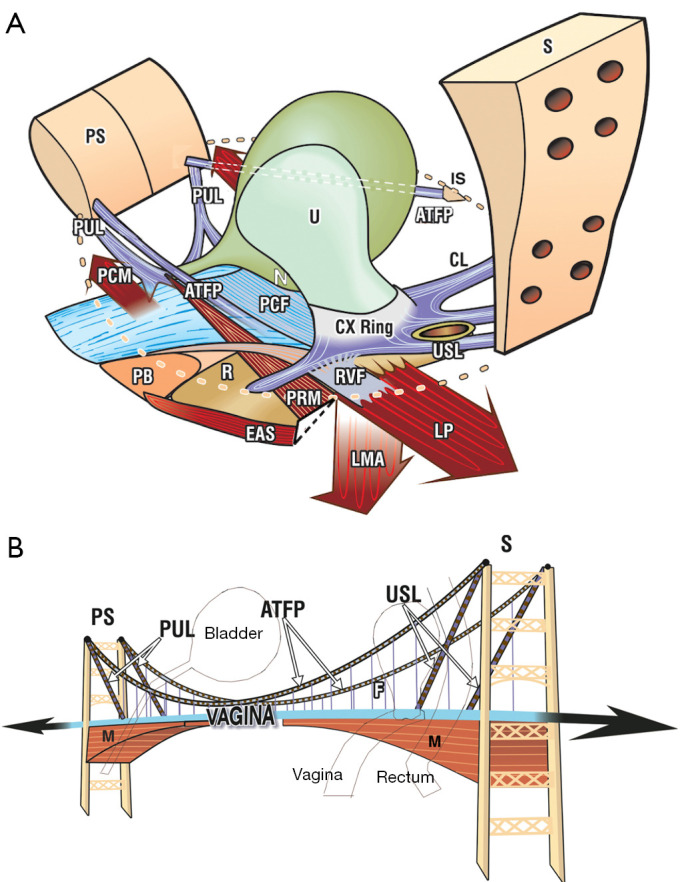
The suspension bridge analogy for pelvic organ support. (A) The vagina is suspended by ligaments like a suspension bridge. Both walls of the vagina, PCF anteriorly, and RVF posteriorly, are suspended like the traffic part of a suspension bridge, by suspensory ligaments, PUL, CL, USL, ATFP laterally and PB inferiorly. The opposite muscle forces “M” (PCM, LP, and conjoint LMA), lie below the ligaments, and impart strength to the vaginal membrane by stretching it in opposite directions like a trampoline. (B) The suspension bridge analogy. Ligaments suspend the vagina from above and the pelvic muscles support it from below. The opposite muscle forces (arrows) stretch the vagina in opposite directions to tension it. Both images reused from Petros P. The female pelvic floor function, dysfunction and management according to the Integral Theory. 3rd ed. Heidelberg: Springer Berlin; 2010. With permission from Peter Petros; retains ownership of the copyright. PS, pubic symphysis; PUL, pubourethral ligament; PCM, pubococcygeus muscle; PB, perineal body; ATFP, arcus tendineus fascia pelvis; R, rectum; U, urethra; N, bladder base stretch receptors; PCF, pubocervical fascia; CX, cervix; RVF, rectovaginal fascia; PRM, puborectalis muscle; EAS, external anal sphincter; S, sacrum; IS, ischial spine; CL, cardinal ligament; USL, uterosacral ligament; LP, levator plate; LMA, longitudinal muscle of the anus; PS, pubic symphysis; M, muscle; F, fascia.
Collagen
Traditionally, women with prolapse are treated with native tissue repair which reconstructs the vagina and/or supporting ligaments by native tissue repair. In a comparative study, Shkarupa et al. achieved high cure rates for prolapse and overactive bladder (OAB) symptoms by cardinal and USL repair at 18 months, but only in premenopausal women (3); there was a catastrophic drop in cure rates for both symptoms and prolapse in postmenopausal women at 18 months (Table 1). Based on their department’s data, Shkarupa et al. recommended polypropylene slings for postmenopausal women who had surgery for prolapse and/or symptoms.
Table 1. Cure rate (%) of POP and OAB symptoms in different points of follow-up using native tissue cardinal/uterosacral plication.
| POP/OAB symptoms | Premenopausal group (n=49) | Postmenopausal group (n=39) |
|---|---|---|
| 3 months | ||
| Frequency | 71.5 | 64.1 |
| Urgency | 85.7 | 82 |
| Nocturia | 96 | 64.1 |
| POP | 98 | 89.7 |
| 6 months | ||
| Frequency | 77.5 | 48.7 |
| Urgency | 85.7 | 64.1 |
| Nocturia | 98 | 59 |
| POP | 85.7 | 48.7 |
| 12 months | ||
| Frequency | 63.3 | 38.5 |
| Urgency | 81.6 | 33.3 |
| Nocturia | 71.5 | 25.6 |
| POP | 85.7 | 20.5 |
| 18 months | ||
| Frequency | 59.2 | 15.4 |
| Urgency | 67.3 | 17.9 |
| Nocturia | 87.7 | 20.5 |
| POP | 79.6 | 15.4 |
Reused from reference (3). Copyright 2021, with permission Central European Journal of Urology. POP, pelvic organ prolapse; OAB, overactive bladder.
The key to whether a surgical operation succeeds or fails is understanding that structural strength derives from ligament collagen and that function derives from elasticity in the vagina (1). The vagina is an elastic organ which is structurally weak. The vagina has a breaking strength of only 60 mg/mm2 as opposed to a ligament’s 300 mg/mm2 (2). The vagina needs to be conserved, because excising the vagina only reduces its quantum of elastin and collagen III, neither of which can be recreated: the vagina is an organ and so cannot regenerate. Collagen breaks down in bones and ligaments after the menopause and is excreted as hydroxyproline in the entire postmenopausal period (3). The prospect trial in the Lancet unequivocally demonstrated that vaginal surgery as practiced in the United Kingdom, whether “native tissue” repair by vaginal excision, or insertion of mesh sheets behind the vaginal wall, gave very poor cure rates, in the region of 20% by 12 months (4). The Lancet Prospect Trial results reinforced a core thesis of the ITP, that, “ligaments are for structure; vagina is for function” (1).
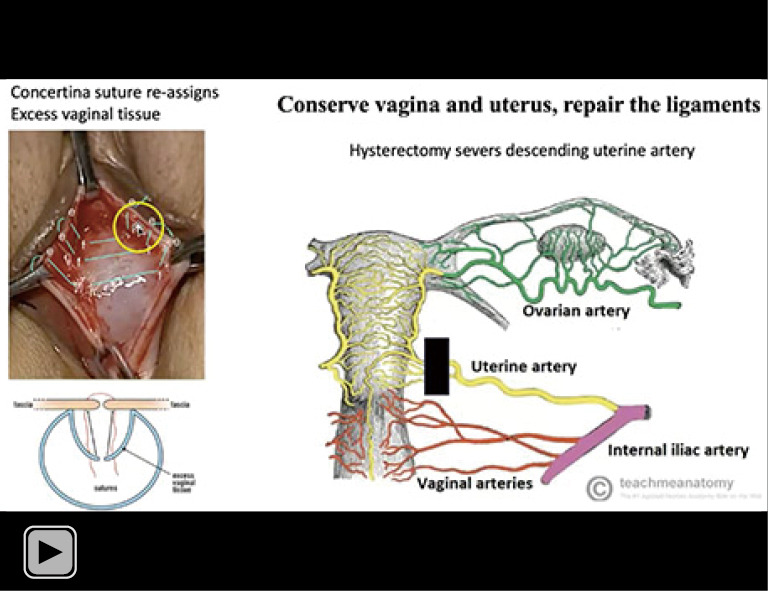
Another major review in Lancet showed that women with prior hysterectomy had higher prolapse and pelvic symptom rates after the menopause (5). The pathogenesis of hysterectomy/prolapse relationship was later explained by reference to data from another study also published in Lancet (6), “A constant intraoperative finding in this other study (6), was laxity and atrophy of the uterosacral ligaments, which may give a clue to causation. The descending uterine artery supplies the uterosacral ligaments, and ligation during hysterectomy may cause atrophy” (6).
In contrast to the Lancet Prospect Trial (4), Inoue et al. (7) following the ITP’s system, avoided vaginal excision and hysterectomy, and used the Tissue Fixation System (TFS) minisling tapes to repair suspensory ligaments. Inoue et al. achieved 87% anatomical cure for POP at 12 months, falling (minimally) to 79% at 60 months (7). Ten-year data from Japan, for 960 women (mean age 70 years), of 3,100 TFS implants for ligament repair with vaginal and uterine conservation, broadly confirmed Inoue et al.’s data (8). The patient ages in the Lancet Prospect Trial (4) and Inoue et al.’s (8) trials were comparable. The difference in results, we believe, can be mainly attributed to the collagen-creating tapes used by Inoue et al. (8).
Creating new collagen for postmenopausal ligaments
Another important discovery in 1990 was a new surgical principle, how to create an artificial collagenous neoligament by harnessing the collagen 1 wound reaction to an implanted tape (9) (Figure 2). Collagen I has a breaking strength of 18,000 lbs/sq inch. Whereas ligament reinforcement with tapes is still the gold standard for the midurethral (pubourethral) and posterior (uterosacral) slings, the enormous strength of neocollagen they created (9) led to the question whether wide bore No. 2 or No. 3 polyester sutures would create sufficient collagen to repair weak ligaments, and so eliminate tapes altogether (10). Initial results indicate that this may be so (10).
Figure 2.
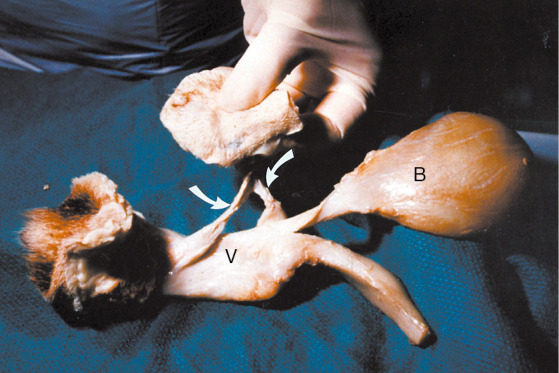
Formation of artificial collagenous neoligaments. Specimen of vagina (V), vulva bladder (B) dissected from a dog, 2 weeks after the implanted tape had been removed. Note the significant artificial collagenous neoligament created by tissue reaction against the tape (white arrows). Reused from Petros P. The female pelvic floor function, dysfunction and management according to the Integral Theory. 3rd ed. Heidelberg: Springer Berlin; 2010. With permission from Peter Petros; retains ownership of the copyright.
Principles of surgery according to the ITP
The ITP successfully cures or improves major symptoms, where there is only minor prolapse, using the same operations as for major prolapse; however, any such symptom-based surgery must first undergo a screening test (simulated operation; see paper No. 8 in this ATM series) where the damaged ligament in question is mechanically supported per vaginam while observing change in symptoms. Examples are: a hemostat applied vaginally to the midurethra in women with stress incontinence; a speculum applied to support USLs in women with urge or chronic pelvic pain symptoms.
Symptom-based surgery
The ITP indications for pelvic surgery are symptom-based. The Pictorial Diagnostic Algorithm guides which ligaments and fascia to repair (Figure 3).
Figure 3.
Diagnostic algorithm. A “short-hand” diagnostic method where symptoms indicate which ligaments are causing which prolapse and which symptoms. The connective tissue structures fall naturally into three zones of causation. Symptoms, even if occurring “sometimes”, are ticked in each box where they occur. The ticked boxes also serve as a guide to surgery. For example, nocturia and pelvic pain are almost exclusively caused by the “USL” laxity; stress incontinence, by pubourethral laxity “PUL”. Reused from Petros P. The female pelvic floor function, dysfunction and management according to the Integral Theory. 3rd ed. Heidelberg: Springer Berlin; 2010. With permission from Peter Petros; retains ownership of the copyright. PS, pubic symphysis; PUL, pubourethral ligament; PCM, pubococcygeus muscle; V, vagina; PB, perineal body; ATFP, arcus tendineus fascia pelvis; R, rectum; U, urethra; PCF, pubocervical fascia; CX, cervix; RVF, rectovaginal fascia; PRM, puborectalis muscle; EAS, external anal sphincter; S, sacrum; IS, ischial spine; CL, cardinal ligament; USL, uterosacral ligament; LP, levator plate; LMA, longitudinal muscle of the anus; EUL, external urethral ligament.
Ligaments and the vagina have different roles
Ligaments and the vagina have a different role in pelvic floor function, and so require very different surgeries. Ligaments are structural. They require shortening and reinforcement so as to act as firm insertion points for the muscles which contract against them (Figure 1). Excellent results are achieved for anatomical and symptomatic cure by native plication of cardinal and USLs (3), with vaginal conservation, but only in premenopausal women (Table 1).
The vagina’s role is primarily functional (1). It mediates closure and opening of the urethra, and it has a key role in controlling the afferent output of the urothelial stretch receptors which lead to inappropriate urgency (“OAB”). Vaginal excision removes a quantum of the collagen and elastin required for optimal functioning of the vagina. The vagina must be conserved.
Postmenopausal women suffer from collagen breakdown
Collagen breaks down after the menopause and is excreted as hydroxyproline (3,11). Older, postmenopausal women have very poor results from “native tissue” repair (3,4) and require new collagen to strengthen their ligaments (3) (Table 1). In older women, ligaments require reinforcing with collagen-creating tapes for longer term results (7,8). More recently, wide-bore polyester sutures show promise of providing sufficient collagen to reinforce ligaments without the need for implanted tapes (10).
Vaginal conservation
Avoiding mesh sheets is key to retaining the elasticity which is so important for bladder function postoperatively. The elasticity issue is even more acute in older women, whose vagina is usually collagen and elastin deficient. Excision can cause scar tissue and fibrosis, which may lead to “TVS” (12). (TVS will be more extensively presented later in this series). The cardinal TVS symptom is sudden massive urine loss on getting out of bed in the morning. Generally, there is little, if any, SUI. The same rationale, preservation of vaginal elasticity, holds for mesh sheets placed behind the vagina, as mesh causes immense fibrosis to reduce elasticity.
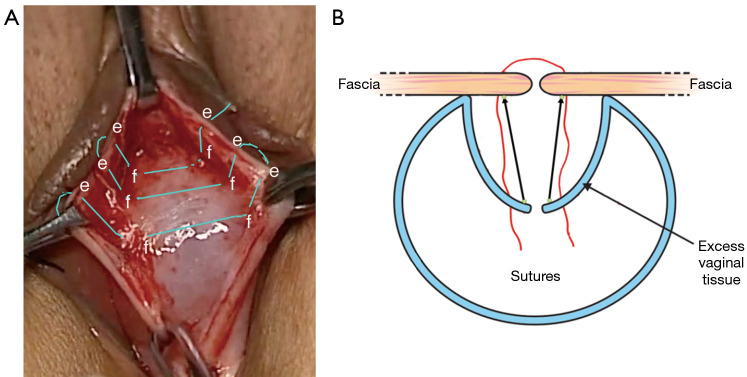
Re-assigning excess vaginal tissue instead of excision
In their 10-year experience with 3,100 minisling tape implants, most with 3rd or 4th degree organ prolapse, Inoue et al. did not excise vaginal tissue (8). They repaired only ligaments. Instead of excising “excess” vaginal tissue, we recommend the “concertina” technique which shrinks and flattens excess vaginal epithelium by re-attaching it to the underlying fascial layer (Figure 4). Over the ensuing 6 weeks, the intraepithelial collagen and glycoaminoglycans re-adjust to the forces acting on them to give a very pleasing result post-operatively. Performed on a glove model, Video S2 outlines how to shrink the excess vaginal tissue, using the “concertina suture”, as in Figure 4. A 00 vicryl suture is inserted 2 mm from the cut vaginal edge, from the outside in. Next, it is inserted into the deep fascial layer on the same side. The forefinger and 2nd finger then are placed around the suture from the outside, and the vaginal edge is compressed down onto the fascia. The suture is then inserted into the fascia on the other side, then inserted 2 mm from the vaginal edge, taken to the outside and pulled through. The suture is placed between the fingers as before and pushed down onto the deep fascia. It can be tied as an interrupted suture or continued as a continuous suture.
Figure 4.
The concertina method. The “concertina” method of re-attaching ballooned vaginal epithelium to the underlying fascial layer. Using a continuous (or interrupted) 00 vicryl suture, a suture “e” is placed 2 mm from the vaginal edge and sutured deep into the fascia “f”. The 1st and 2nd fingers are placed around the suture to push the epithelium down onto the fascia “f” after each suture. Then the suture is placed through the contralateral fascia, then into the vaginal edge “e”. The vaginal edge “e” is pushed down onto “f” as before, and the suture is continued. (A) The concertina method. Published with permission from Peter Petros: Personal Collection. (B) The concertina method. Reused from Petros P. The female pelvic floor function, dysfunction and management according to the Integral Theory. 3rd ed. Heidelberg: Springer Berlin; 2010. With permission from Peter Petros; retains ownership of the copyright.
Video S2.
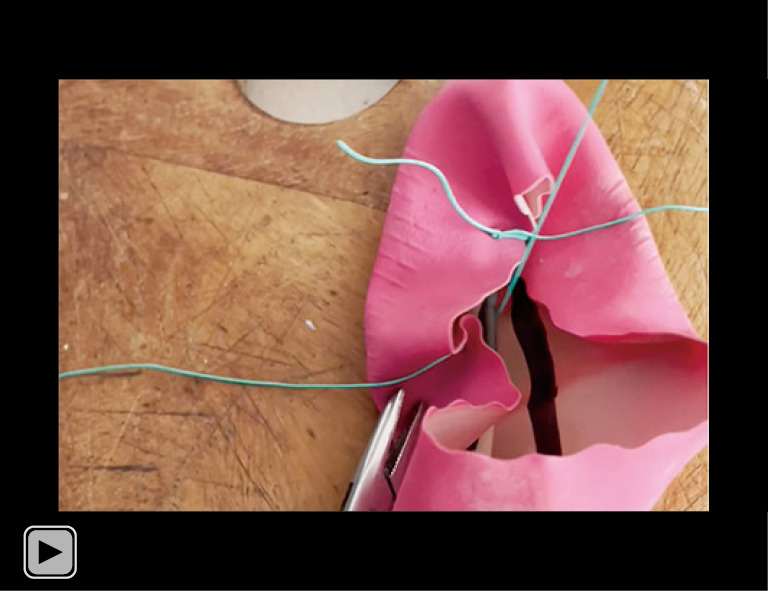
Demonstrates the principle of compressing thin vaginal epithelium to the underlying fascia, in order to avoid excision of vaginal tissue. By permission Professor Peter Petros.
Uterine conservation
The uterus and its USL attachments provide a firm, structural anchoring point for the downward muscle vectors which are so important for bladder/anorectal function. Hysterectomy requires sectioning the descending uterine arteries which supply the USLs at their insertion points into the cervix (6). Therefore, it is not uncommon to find atrophic USLs at this point after a hysterectomy. In fact, women who have had a hysterectomy are known to have more serious bladder/bowel/incontinence after the menopause (5,6).
Surgery in the time of banned tape kits
In 2011, a major drive against any type of mesh implantation, whether tapes for midurethral slings or mesh sheets for prolapse, began in the mass media and gathered sufficient political momentum for a complete ban of slings and meshes for prolapse in many countries worldwide. These decisions have left the vast majority of older women with only one surgical option, native tissue repair with its high failure rates (3,4). We present below some surgical options suitable for an individual patient by an individual doctor.
Tension-free artisan tapes
Postmenopausal women almost invariably have depleted collagen in their ligaments, and this may be the principal cause of cystocele, rectocele and uterine prolapse. These prolapses, and also, SUI, can be repaired using the artisan tape technique (13). Thin strips of polypropylene tapes 8–10 mm wide, 10 cm long, are cut from a large sheet of type 1 polypropylene mesh and are applied directly in the position of the damaged ligaments (Figure 5). The symptoms in the three zones of the vagina are a good guide as to what ligaments may need repairing (Figure 3). Where kits are not allowed, artisan tapes can create neocollagen to reinforce the weakened ligaments, potentially, all five main pelvic ligaments, as in Figure 5. The ligament is located; a tunnel is made along the ligament on each side; the tape is inserted “tension-free” equivalently on each side with a Crile (or other) hemostat, and the vagina is closed with vicryl sutures (13).
Figure 5.
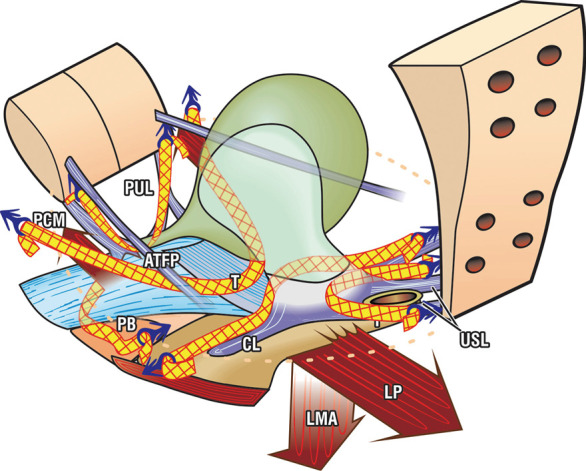
Precisely placed tapes create new collagen to repair five damaged ligaments and restore muscle function. Reused from Petros P. The female pelvic floor function, dysfunction and management according to the Integral Theory. 3rd ed. Heidelberg: Springer Berlin; 2010. With permission from Peter Petros; retains ownership of the copyright. PUL, pubourethral ligament; PCM, pubococcygeus muscle; ATFP, arcus tendineus fascia pelvis; PB, perineal body; T, tape; CL, cardinal ligament; USL, uterosacral ligament; LP, levator plate; LMA, longitudinal muscle of the anus.
Wide bore No. 2 or No. 3 polyester sutures as alternatives to mesh tapes
Initial results using wide-bore polyester sutures for ligament repair are highly promising. The ligament is shortened along its length with the polyester sutures. It has been calculated that sufficient collagen would be created to structurally reinforce the ligament (10). To date, No. 2 or No. 3 polyester sutures have been used for PULs, for SUI, CL for cystocele, USL for uterine prolapse, and also, for the deep transversus perinei ligaments which suspend the PB, for rectocele.
Conclusions
The five key surgical principles of the Integral Theory System are: ligaments are for structure and the vagina is for function. Prolapse and symptoms are related; repair the structure and you will restore the function. Avoid vaginal excision and hysterectomy. Especially in postmenopausal women, create new collagen to reinforce damaged ligaments.
Supplementary
The article’s supplementary files as
Acknowledgments
We would like to express our thanks to Editors Professor Peter Petros and Vani Bardetta for their tremendous help in designing and modifying the article.
Funding: None.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All clinical procedures described in this study were performed in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for the publication of this article and accompanying images. Human participation in the video was by patient permission on the basis it was deidentified.
Footnotes
Provenance and Peer Review: This article was commissioned by the International Society for Pelviperineology for the series “Integral Theory Paradigm” published in Annals of Translational Medicine. Peter Petros (Editor) and Vani Bardetta (Assistant Editor) served as the unpaid Guest Editors of the series. The article has undergone external peer review.
Peer Review File: Available at https://atm.amegroups.com/article/view/10.21037/atm-23-1769/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-23-1769/coif). The series “Integral Theory Paradigm” was commissioned by the International Society for Pelviperineology without any funding or sponsorship. M.N. reports stocks and stock options at Momentis and Femselect. The authors have no other conflicts of interest to declare.
References
- 1.An integral theory of female urinary incontinence. Experimental and clinical considerations. Acta Obstet Gynecol Scand Suppl 1990;153:1-78. [PubMed] [Google Scholar]
- 2.Yamada H. Aging rate for the strength of human organs and tissues. In: Evans FG. editor. Strength of biological materials. Baltimore: Williams & Wilkins; 1970:272-80. [Google Scholar]
- 3.Shkarupa D, Zaytseva A, Kubin N, et al. Native tissue repair of cardinal/uterosacral ligaments cures overactive bladder and prolapse, but only in pre-menopausal women. Cent European J Urol 2021;74:372-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Glazener CM, Breeman S, Elders A, et al. Mesh, graft, or standard repair for women having primary transvaginal anterior or posterior compartment prolapse surgery: two parallel-group, multicentre, randomised, controlled trials (PROSPECT). Lancet 2017;389:381-92. 10.1016/S0140-6736(16)31596-3 [DOI] [PubMed] [Google Scholar]
- 5.Brown JS, Sawaya G, Thom DH, et al. Hysterectomy and urinary incontinence: a systematic review. Lancet 2000;356:535-9. 10.1016/S0140-6736(00)02577-0 [DOI] [PubMed] [Google Scholar]
- 6.Petros P. Influence of hysterectomy on pelvic-floor dysfunction. Lancet 2000;356:1275. 10.1016/S0140-6736(05)73879-4 [DOI] [PubMed] [Google Scholar]
- 7.Inoue H, Kohata Y, Fukuda T, et al. Repair of damaged ligaments with tissue fixation system minisling is sufficient to cure major prolapse in all three compartments: 5-year data. J Obstet Gynaecol Res 2017;43:1570-7. 10.1111/jog.13413 [DOI] [PubMed] [Google Scholar]
- 8.Inoue H, Nakamura R, Sekiguchi Y, et al. Tissue Fixation System ligament repair cures major pelvic organ prolapse in ageing women with minimal complications - a 10-year Japanese experience in 960 women. Cent European J Urol 2021;74:552-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Petros PE, Ulmsten UI, Papadimitriou J. The autogenic ligament procedure: a technique for planned formation of an artificial neo-ligament. Acta Obstet Gynecol Scand Suppl 1990;153:43-51. 10.1111/j.1600-0412.1990.tb08031.x [DOI] [PubMed] [Google Scholar]
- 10.Petros P, Palma P. Conceptualizing stress urinary incontinence surgery beyond midurethral slings: Very early results from simplified ligament repair without tapes. Neurourol Urodyn 2023;42:383-8. 10.1002/nau.25049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sone T, Miyake M, Takeda N, et al. Urinary excretion of type I collagen crosslinked N-telopeptides in healthy Japanese adults: age- and sex-related changes and reference limits. Bone 1995;17:335-9. 10.1016/S8756-3282(95)00243-X [DOI] [PubMed] [Google Scholar]
- 12.Goeschen K, Müller-Funogea A, Petros P. Tethered vagina syndrome: cure of severe involuntary urinary loss by skin graft to the bladder neck area of vagina. Pelviperineology 2010;29:100-2. [Google Scholar]
- 13.Piñango-Luna S, Level-Córdova L, Petros PE, et al. A low cost artisan tension-free tape technique cures pelvic organ prolapse and stress urinary incontinence - proof of concept. Cent European J Urol 2020;73:490-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as